Abstract
Purpose:
To report anterior-segment optical coherence tomography (ASOCT) characteristics of different types of corneal and anterior chamber (AC) foreign bodies (FBs) and their usefulness in diagnosis and management.
Methods:
This is a retrospective descriptive clinical study involving 11 eyes of 11 patients who presented at the outpatient department of a tertiary ophthalmic care center from January 2017 to January 2022. All patients had a diagnosed or suspected corneal FB. All participants underwent a comprehensive ophthalmological examination, followed by slit-lamp photography and ASOCT. FB removal was done where required by an external, internal, or combined approach.
Results:
The mean age of patients was 28.2 (7–53) years. Ten were male, and one was female. Seven patients had a definitive positive history of injury; in one, there was a history suggestive of trauma, one had the post-operative complication of scleral buckling surgery, and two patients had a history of insect fall in the eyes. Three patients had acute, four had sub-acute, and four had chronic presentations. Descemet’s membrane (DM) breach was suspected in three cases of deep FB, which was later confirmed on ASOCT. In two cases, DM was presumed to be intact clinically, but ASOCT showed an AC penetration. The FB was removed in seven patients, one via slit-lamp, one via an external approach, two via an internal approach, and three via a combined approach.
Conclusion:
ASOCT facilitates non-invasive rapid imaging of ocular tissue at various depths, provides an accurate assessment of FB characteristics, and thereby serves as an additional tool in our armamentarium for diagnosis and management of deep corneal and AC FBs.
Keywords: Anterior chamber foreign bodies, anterior-segment optical coherence tomography (ASOCT), deep corneal foreign bodies
Ocular injury is the most common cause of emergency interventions in ophthalmology departments across the world.[1] According to the World Health Organization (WHO) global estimates, the annual incidence of ocular trauma is approximately 55 million and ocular injuries account for 5–16% of ophthalmology consultations.[2] Among the ocular trauma, corneal foreign bodies (FBs) are the second most common type of ocular injury, accounting for approximately 30.8% of all eye injuries.[3] Although the diagnosis and management of corneal FBs (CFBs) are generally easily made based on the history and slit-lamp examination, there are some unusual cases that create difficulties in the diagnosis and choosing the most appropriate method of removal.[4,5,6,7] Anterior-segment optical coherence tomography (ASOCT) provides high-resolution cross-sectional images of CFBs and has the advantage of being a non-contact imaging system causing minimal discomfort, especially in trauma patients.[8] Tao Wang et al.[7] have described a study mostly involving superficial CFBs with a stress on its ASOCT characteristics only. Armanik et al.[9] described ASOCT characteristics of artificially embedded CFBs. A paucity of data exists regarding ASOCT for the evaluation of deeply embedded CFBs.[9] Ours is the first study describing ASOCT characteristics of deep intrastromal, Descemet’s membrane (DM) breaching, and anterior chamber (AC) FBs. The purpose of this study is to highlight the role and usefulness of ASOCT in the diagnosis and management of FBs as well as to describe different techniques and approaches of FB removal used in our study. The purpose of this study is to highlight the role and usefulness of ASOCT in the diagnosis and management of FBs as well as to describe different techniques and approaches of FB removal used in our study.[10,11,12,13,14]
Methods
This is a retrospective study involving 11 eyes of 11 patients who presented at the outpatient department of a tertiary ophthalmic care center from January 2017 to January 2022. All patients who were included in this study met the following criteria:
-
(1)
Had a confirmed or suspected corneal or AC FB.
-
(2)
Were able to complete the anterior segment examinations with clear anterior segment color photography and ASOCT scanning.
-
(3)
Had no apparent corneal infection.
The study was performed after approval from the Institutional Ethics Committee. Informed written consent was obtained from all the participants. The study confirms adherence to the Declaration of Helsinki.
All participants underwent comprehensive ophthalmological examination, including a detailed questionnaire (including age, sex, history of trauma, the onset of symptoms, occupation, general, and ocular disease history), visual acuity, refractive error, slit-lamp biomicroscopic examination of the anterior segment, and fundus examination using indirect ophthalmoscopy. Duration of the presentation was classified into acute (1–10 days), sub-acute (11–30 days), and chronic (>30 days). All patients were subjected to clinical slit-lamp photography for documentation before and after FB removal. ASOCT was done for all patients in raster and line scan using a Heidelberg spectralis (Germany) scanner focused on lesions using the anterior segment protocol.[15,16,17] One section of the clear image was used for evaluation and measurement. The results were interpreted by two different experienced ophthalmologists. We used the signal of the normal corneal tissue surrounding the lesions as a reference. If the signal of the lesion was stronger than the surrounding tissue signal, it was labeled as a hyper-reflective signal (high signal). When the signal of the lesion was weaker than the surrounding tissue, it was a hypo-reflective signal (low signal). When the signal deep in the FB was weaker or even disappeared, it was regarded as signal attenuation and was called a posterior shadowing effect. Total attenuation was called complete posterior shadowing. When the deep signal was weak or present at margins with total loss at the center, it was called partial posterior shadowing.
FBs were classified depending on the depth and breach of DM into.
(a) epithelial and sub-epithelial (up to Bowman’s layer), (b) superficial stromal (up to 40% of stroma), (c) deep stromal (beyond 40% of stroma but not breaching DM), (d) DM penetrating (primarily corneal but breaching DM and protruding into AC), and (e) AC FB (primarily or completely in AC).
Depending on various characteristics such as (1) type, (2) duration, (3) depth, and (4) DM breach, the decision for removing versus retaining the FB and if removing then on slit-lamp versus in the operation theater (OT) was taken. For removal in the OT, either of the below-mentioned three approaches was undertaken.
-
(1)
External approach: When the FB was up to the mid-stroma and not penetrating through DM, it was approached from the epithelial side with a 26 G hypodermic needle or picked up with microforceps.
-
(2)
Internal approach: When a FB was in the AC completely or predominantly, the AC was entered and the FB was picked up with the help of long microforceps.
-
(3)
Combined approach: When a FB was impacted mainly in the corneal stroma even though it was breaching the DM, a combined approach was preferred. The AC was entered, and the FB was held or supported with microforceps or a spatula. This served two purposes. It prevented accidental slippage of the FB in the AC and also provided counter-pressure or external push when required. The FB was then approached from the epithelial side and removed.
FB removal was supplemented with 10-0 non-absorbable monofilament nylon sutures in case of tissue loss or penetrating corneal wound or cyano-acrylate glue in case of thinning. Inert FBs which did not cause any significant symptoms were not removed. Inert FBs causing a decrease in the best-corrected visual acuity (BCVA) or endothelial decompensation were removed. The composition of the FB was noted in all cases where it was removed. Detailed clinical and slit-lamp characteristics of patients have been described in Table 1. The ASOCT characteristics of different FBs are described in Table 2.
Table 1.
Clinical characteristics of patients
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Case 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 26 | 53 | 17 | 45 | 28 | 52 | 26 | 31 | 17 | 8 | 7 |
| Gender | Male | Male | Male | Male | Male | Male | Male | Male | Male | Male | Female |
| Eye | Right | Left | Right | Left | Right | Left | Right | Left | Right | Right | Right |
| Mode of injury | Injury with glass fragment during a road accident | Accidental fall of the FB while working at a steel plant | Fall of the stone chip while cutting tiles | Injury by a glass of his own spectacles due to an accidental fall | Anterior migration through recti muscle and positioning in the corneoscleral limbus | Gunshot injury | Fall of insect | Fall of insect | Firecracker injury | Parents could not recall the mode of injury | History of trauma with pencil |
| Duration of Presentation | Chronic (2 years) | Acute (6 days) | Sub-acute (20 days) | Sub-acute (17 days) | Chronic (3 months) | Acute (3 days) | Sub-acute (20 days) | Sub-acute (13 days) | Chronic (5 years) | Acute (10 days) | Chronic (45 days) |
| BCVA on presentation | 6/18 | 6/6 | 6/9 | 6/9 | 6/9 | PL+, PR4+ | 6/6 | 6/6 | 6/6 | 6/6 | 6/15 |
| Sle findings | Diffuse, microcystic sectoral edema (4-6.30 o’clock) with few bullae. On treatment with hyperosmotic agents, edema subsided and some refractive structure stuck to the DM in the AC was suspected. [Fig. 1a] | One metallic FB at 6.30 o’clock with surrounding infiltration and pigmentation, overlying epithelial defect, impacted deep into the stroma, posterior extent not clearly delineated [Fig. 2a] | Small-brownish deep intrastromal FB with surrounding minimal scarring, intact overlying epithelium, clinically no breach in the DM [Fig . 1c] | A deep intrastromal refractive FB with surrounding scarring with an intact overlying epithelium and an intact DM [Fig. 2c] | Deep intrastromal silicon band at corneoscleral limbus from 2 to 4.30 o’clock with the overlying intact epithelium, posterior margin not clearly delineated [Fig. 3b] | 3 metallic corneal FB, one in the anterior mid-stroma, second in mid-stroma, and third in the deep stroma with possible AC penetration. | Multiple setae in upper tarsal conjunctiva and intrastromal in the cornea with no anterior chamber reaction | Few tarsal setae with one corneal deep stromal setae at 3.30 o’clock with possible AC penetration [Fig. 4a] | Multiple shiny powdery intrastromal deposits with a surrounding nebular scar [Fig. 3a] | Transparent FB in visual axis with intact overlying epithelium [Fig. 1b] | Human hair (eyelash) in the AC with its nasal end impacted in the stroma, 5×1 mm full thickness self-sealed corneal scar surrounding impacted part of the hair [Fig. 4b] |
| BCVA final | 6/6 | 6/6 | 6/6 | 6/6 | 6/9 | 6/9 | 6/6 | 6/6 | 6/6 | 6/6 | 6/15 |
FB: foreign body, DM: Descemet’s membrane, AC: anterior chamber, BCVA: best-corrected visual acuity, SLE: slit-lamp examination, PL: perception of light, PR: projection of rays
Table 2.
ASOCT characteristics and management of patients
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Case 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of foreign body | Glass (AC) | Metal | Stone chip | Glass (Intrastromal) | Silicon band | Gun pellets (metal) | Caterpillar hair | Caterpillar hair | Firecracker debris | Plastic sheet piece | Human hair eyelash (AC+corneal) |
| ASOCT findings | AC FB with well-defined hyper-reflective borders and hypo-reflective left, anterior border of FB resting on DM with no intervening space, no posterior shadowing, and intact overlying cornea. [Fig. 1d] | Hyper-reflective triangular anterior border with total posterior shadowing, posterior edge protruding in AC, curling of DM at the site of AC penetration, hyper-reflective anterior border of protruding part in AC. [Fig. 2c] | A triangular FB with hyper-reflective anterior apex, well-defined hyper-reflective sides, and complete central shadowing, Curling of DM (arrow in Fig. 2d) at the site of DM breach. [Fig. 2d] | Intrastromal FB with an area of hypo-reflectivity surrounded by hyper-reflective, well-delineated borders with the isoechoic left, no posterior shadowing, and no breach in the endothelium. [Fig. 1e] | Deep intrastromal FB at corneoscleral limbus on the nasal side with well-delineated hyper-reflective borders and internal area of isoechoic reflectivity with complete penetration of rays. Epithelium and Descemet’s layer were intact. [Fig. 3d] | ASOCT of deep corneal FBs showed hyper-reflective anterior margins with total posterior shadowing, hyper-reflective oblique border in the AC with overhanging tissue, surrounding tissue hyper-reflectivity due to associated tissue edema, scarring and damage due to heat associated with pellets, curling of the DM at the site of AC entry. [Fig. 2e] | Three hyper-reflective fine linear structures corresponding to setae at different corneal depths with no posterior shadowing as follows (1) 144 microns at 3 o’clock (2) 144 microns a 5 o’clock (3) 567 microns at 6 o’clock resting on DM but not penetrating AC. | (1) First visit- single hyper-reflective fine linear structure corresponding to setae at 3 o’clock, anchored to DM, temporal 2/3 in the stroma, and nasal 1/3 protruding in the AC. [Fig. 4c] (2) Follow-up ASOCT showed migration of setae into AC with a small segment anchored to the cornea. [Fig. 4d] | Multiple hyper-reflective clump echoes at different depths in the cornea from sub-epithelial to a mid-stromal level corresponding to intrastromal powdery debris with partial posterior shadowing. [Fig. 3c] | Hyper-reflective horizontal structure, sub-epithelial, corresponding to the plastic sheet, with no posterior shadowing. | Multiple hyper-reflective echoes due to stromal scar and deep stromal impacted hair with a well-defined linear hyper-reflective structure in AC corresponding to the hair shaft. A hypo-echoic area suggestive of a clear space between the DM and hair shaft is seen. Curling of the DM at the site of the DM breach. [Fig. 4e] |
| Approach to FB removal | Internal | Combined | Combined | External | Not removed as inert. Patient is under close observation for further stromal or AC migration of the band | Combined | Not removed and observed for setae migration and intraocular inflammation | Not removed as deep and observed for setae migration and intraocular inflammation | Not removed as inert | External under the slit lamp | Internal |
| Additional measures | Nil | Three interrupted 10-0 nylon sutures as it was penetrating the wound | Two interrupted 10-0 nylon sutures | Cyno-acrylate glue+bandage contact lens | Nil | Cyno-acrylate glue+bandage contact lens | Upper tarsal conjunctival setae were removed under the slit lamp under topical anesthesia | Upper tarsal conjunctival setae were removed using a slit lamp under topical anesthesia | Nil | Nil | Nil |
FB: foreign body, DM: Descemet’s membrane, AC: anterior chamber
Results
The mean age of patients in our series was 28.2 (7-53 years). Ten patients were male, and one was female. Seven patients had a definitive positive history of injury, one patient’s parents gave a history of trauma but could not elucidate the exact mechanism, one had a post-operative complication of scleral buckling surgery, and two patients had a history of fall of some insect in their eyes. Three patients had an acute presentation, four had a sub-acute presentation, and four had a chronic presentation. All four cases with chronic presentations were of inert FB. The presence of 10 FBs was confirmatory, whereas, in one, the FB was suspected on slit-lamp examination and was confirmed on ASOCT. DM breach was not definitive in three cases of deep CFB, which was later confirmed by ASOCT. In two cases, DM was presumed to be intact clinically, but ASOCT showed AC penetration. Out of 11 cases, in seven patients, the FB was removed, and in four cases, the FB was retained and the patient was kept on observation. In seven cases where FB removal was done, one was on slit-lamp, one via an external approach, two via an internal approach, and three via a combined approach. In four patients, additional intraoperative measures were required. All patients who underwent FB removal had complete wound healing with either improvement in BCVA or improvement in their symptoms. Patients in whom the FB was retained maintained their BCVA without the development of any other symptoms.
Discussion
A corneal FB is the most common type of occupational ocular injury accounting for almost 35% of all ocular trauma.[18,19] Such injuries are commonly seen in metal industry workers (welding, grinding, and cutting), construction industry workers, and agricultural workers.[19,20,21] Men in their active lifespan with the age range of 10–60 years are affected more.[22,23] Injury can also often occur at work and during domestic and leisure activities (home, garden, and playing), sports, or windy days.[24]
Metallic FBs and organic substances, such as vegetables and wood, are poorly tolerated by the cornea and must be promptly removed.[25] Materials such as glass, plastic, and silicon are inert in nature and can be left intrastromal under close monitoring.[8] Although if an inert CFB is in the visual axis and/or reduces visual acuity due to posterior astigmatism, prompt removal is indicated.[26] Depending on the location, CFBs can be divided into superficial, stromal, or deep.[27] FBs that are confined to the corneal epithelium can be considered superficial.[27] These are the most common types of CFBs, which cause minimal visual impairment and can be easily diagnosed and managed on a slit lamp.[24] However, deeply embedded CFBs cause significant morbidity and sequelae.[9]ASOCT is particularly useful for the management of deep CFBs, and its role can be divided broadly into the following sub-categories:
To know the exact location of the FB
The high resolution of ASOCT is ideal for evaluating the depth and location of the FB, which in turn dictates the optimal surgical technique to be employed. Superficial CFBs can be easily removed on a slit-lamp in a daycare setting under topical anesthesia with either a cotton tip, hypodermic 26-gauge needle, or 15-number blade. In case-7 and case-8, superficial corneal setae were removed using the slit lamp. In case-10, an 8-year-old child presented with a transparent CFB which was found to be just sub-epithelial on ASOCT [Fig. 1b], so it could be easily removed on a slit lamp, avoiding undue exposure to general anesthesia in a child. In six cases, the FB was either deep corneal or in the AC and therefore was removed in OT. In case-3, clinically, the DM appeared intact, but ASOCT showed a breach in the DM with AC penetration [Fig. 2b and d]. In cases with an intact DM, the FB can be removed via an external approach (26-G needle or forceps) like in case-4 [Fig. 1c] and case-6. Removal via a lamellar corneal pocket for an intrastromal FB is described by Au et al.,[28] for cases in which the entry wound had healed and epithelized. A lamellar dissection was extended centrally toward the CFB, and the corneal wound was closed with a circumferential mattress suture using a 10-0 nylon. In cases with a breach in the DM, an internal approach via the AC is preferred. CFBs lying in the posterior stroma and protruding in the AC can be grabbed with microforceps via a side port. When the FB is in the anterior or mid-stroma and protruding in AC, it can be directly grasped through forceps externally, if the overlying epithelium is loose or damaged, supporting from within the AC with a spatula to prevent slippage in AC, or it can even be pushed from inside out with the help of a spatula or reverse-Sinskey hook.
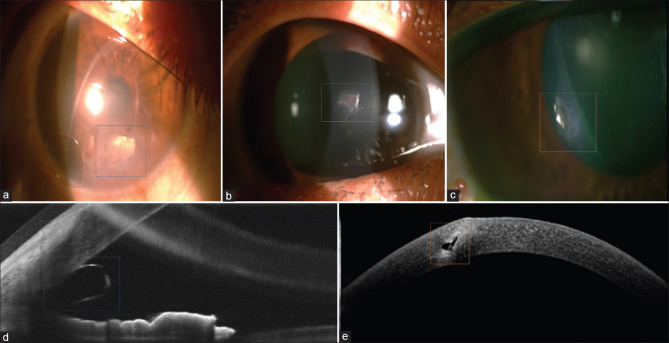
Figure 1.
Slit lamp and ASOCT characteristics of inert FBs. (a) Slit-lamp photograph of a refractive FB (glass) in the AC (blue box), (b) slit-lamp photograph of the refractive FB (plastic) in cornea (white box), (c) slit-lamp photograph of refractive FB (glass) in the cornea (orange box), (d) ASOCT image of the FB in (a) showing a hypo-reflective center with hyper-reflective borders, and (e) ASOCT image of the FB in (c) showing a hypo-reflective center with hyper-reflective borders, mid-stromal location, and an intact DM
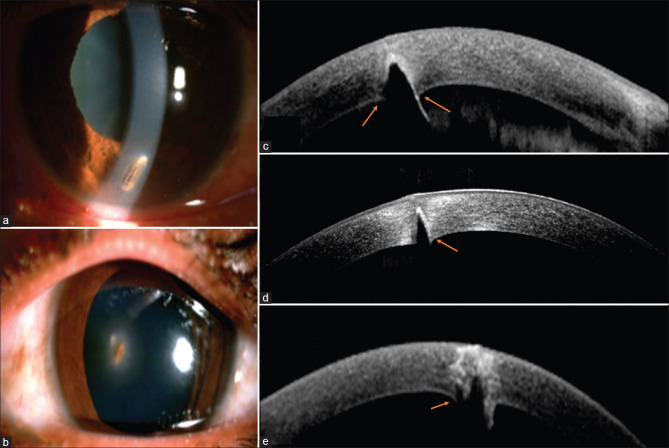
Figure 2.
Slit lamp and ASOCT characteristics of metallic, stone chip, and gun pellet corneal FBs. (a) Slit-lamp photograph of an iron and (b) of stone chip corneal FB, (c) ASOCT image of the FB in (a) showing a hyper-reflective border in the AC (blue asterisk), inward curling of the DM at the site of the DM breach (orange arrows), (d) ASOCT image of the FB in (b) showing a hyper-reflective anterior border with total posterior shadowing and inward curling of the DM at the site of the DM breach (orange arrows), (e) ASOCT image of a gun-pellet FB showing a hyper-reflective border with total posterior shadowing and inward curling of the DM at the site of the DM breach (orange arrows)
To know the type of FB based on the ASOCT characteristics
Removal of the FB depends on its composition. Different materials have demonstrated various specific ASOCT characteristics which may help to distinguish their composition.[9] Inert substances such as glass and plastic are better tolerated and do not necessarily require urgent removal.[8] Metals (gold and iron) and graphite have a hyper-reflective anterior border with no signal penetration, casting complete (total) posterior shadowing.[7,9] The posterior border is often poorly delineated due to total shadowing [Fig. 2]. ASOCT characteristics of stone chips, which are rarely described, appeared to be similar to that of metals. Materials such as glass and plastic are identified as an area of hypo-reflective content with well-defined hyper-reflective borders. Signal penetration is complete, and no shadowing effect is seen [Fig. 1d and e].[7,9] Wood appears as a hyper-reflective mass with a variable spectrum of penetrability depending on the degree of the density with a variable shadowing effect behind it.[7,9] The intrastromal silicone scleral buckle appeared as an internal area of hypo- to isoechoic intensity with hyper-reflective, well-defined borders and complete signal penetration [Fig. 3d]. On ASOCT, caterpillar setae appear as fine lineiform hyper-reflective striae with no posterior shadowing, corresponding to the location, orientation, and depth of setae in the cornea [Fig. 4c and d]. Most patients have more than one hair, all of which may not be amenable for removal at the first sitting and thus must be followed up closely.[29,30] Depending on their depth, superficial setae can be removed under a slit lamp, whereas deeper ones are difficult to remove.[31] In such circumstances, the patient can be managed conservatively with topical steroids and monitored for deeper migration of setae.[29,30,31] In case-7, setae were superficial and all could be removed under a slit lamp. In case-8, one seta was deep just anchored to the DM. On ASOCT, one end was found to just protrude in AC, which on serial ASOCT was found to migrate deep into the AC [Fig. 4c and d]. As it was not associated with any symptoms, it was best left in place.[30] ASOCT of a human hair (eyelash) revealed well-defined linear hyper-reflective structures in the AC corresponding to the hair shaft with a hypo-echoic area suggestive of a clear space between the DM and hair shaft [Fig. 4e]. ASOCT can also easily differentiate and identify the type of hair depending on thickness and density, which was thick and taut in case of the human eyelash and fine striae in a caterpillar seta. Embedded firecracker debris showed hyper-reflective clump echoes corresponding to intrastromal FB with partial posterior shadowing [Fig. 3c]. Fireworks contain gunpowder and small blobs of explosive materials called stars. The stars contain metal salts which give fireworks their color when they explode.[32] On ASOCT, they cause hyper-reflective shadows. However, as opposed to metals causing tissue reaction, these shiny particles were inert for 5 years and so were not removed.
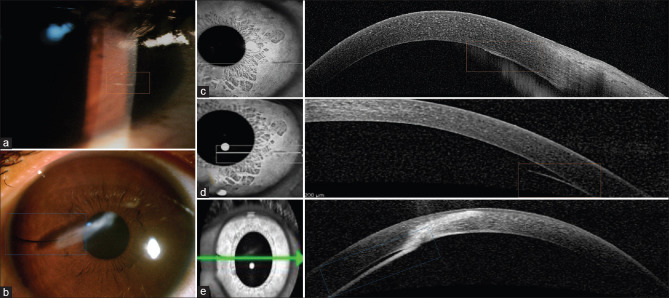
Figure 3.
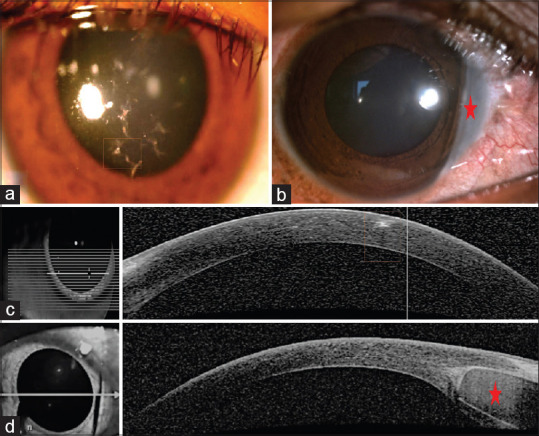
Slit lamp and ASOCT characteristics of firecracker debris and a scleral buckle. (a) Slit-lamp photograph showing multiple shiny powdery firecracker debris (orange box), (b) slit-lamp photograph showing scleral buckle in the nasal corneoscleral limbus (red asterisk), (c) ASOCT image of FB in (a) showing hyper-reflective clump echoes (orange box) in the anterior stroma with partial posterior shadowing, and (d) ASOCT image of the FB in (b) showing hypo- to isoechoic reflectivity in the center with well-defined hyper-reflective borders (red asterisk)
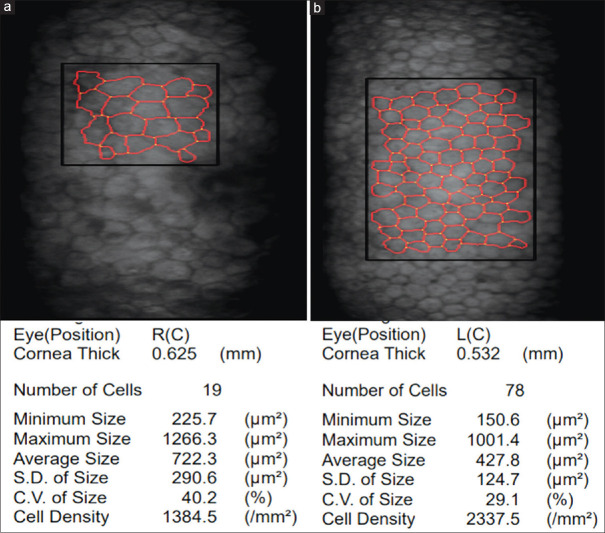
Figure 4.
Slit lamp and ASOCT characteristics of caterpillar hair and human eyelash cilia. (a) Slit-lamp photograph of a fine caterpillar hair (orange box), (b) slit-lamp photograph of human eyelash cilia (blue box), (c) ASOCT image of the FB in (a) on the first visit showing hyper-reflective caterpillar hair just anchored to the DM (blue box), (d) ASOCT image of the FB in (a) on follow-up visit showing migration of hair into the AC with the small end anchored to the DM (orange box), and (e) ASOCT image of the FB in (b) showing a thick hyper-reflective human hair in the AC with the central impacted end into the posterior stroma (blue box)
To locate a FB otherwise concealed within a corneal opacity or corneal edema
A non-inert FB-like metal, organic vegetable matter, and wood are poorly tolerated and usually incite a reaction, making it hard to miss.[8] Inert CFBs usually do not incite any reaction, and if transparent like glass or plastic, embedded in the corneal edema or opacity, they can be easily missed on routine clinical examination.[9] ASOCT is a good tool for confirming FBs when in suspicion.[8,9] In case-1, a small glass FB in the AC was missed in the initial visit due to overlying corneal edema, which could have been easily picked up in ASOCT on the first visit [Fig. 1a]. Glass being inert can be retained intraocularly for years without causing any symptoms.[33,34,35] However, in cases of endothelial cell loss, indentation of the endothelium, or posterior corneal astigmatism, it can be removed.[36,37] Glass FBs in case-1 caused chronic endothelial insult due to mechanical irritation, causing sectoral corneal edema and decreased BCVA, which reversed on FB removal. Archer et al.,[37] in their series, have described corneal edema due to endothelial damage following glass FBs in AC. We agree and further validate the same by showing endothelial cell loss with polymorphism and polymegathism on specular microscopy, which is probably not documented before [Fig. 5]. In case-4 (Fig 1c), an intrastromal glass FB caused a decrease in BCVA, leading to patient dissatisfaction. The FB was successfully removed after a precise evaluation of the depth and exact location in ASOCT. BCVA improved from 6/9 to 6/6. Modern tools such as ASOCT have allowed physicians to take calculated risks and deliver successful outcomes in a predicted manner.
Figure 5.
Specular microscopy images of the AC glass FB. (a) Specular microscopy image of the right eye of the patient in case-1 with an AC glass FB showing pleomorphism and polymegathism with decreased cell density suggestive of endothelial cell loss and decrease in cell count; increase in minimum, maximum, and average cell size; increase in corneal thickness suggestive of endothelial compromise. (b) Specular microscopy image of the normal left eye of the patient in case-1 showing normal cell size, shape, and density for age
To determine the integrity of DM in cases of deep CFBs and thus to decide an approach for removal
The management plan of any CFB removal changes once the FB has penetrated through the DM into the AC. As described before, when the DM is breached, the FB always should be removed via an internal or combined approach in OT. Removing penetrating FBs under a slit lamp can cause inadvertent slippage into the AC or full thickness leaking wound. ASOCT delineates details very beautifully about any breach in DM. In cases where DM breach is seen clinically, ASOCT acts as a confirmatory tool. Details regarding the exact depth of AC penetration, path, and orientation of FBs can be made out clearly. In cases where there is doubt regarding a DM breach, ASOCT acts as a diagnostic tool. In case-2 and case-6, a deep metal FB was suspected to breach the DM, which was confirmed via ASOCT later [Fig. 2]. In case-3, the FB was deep but did not appear to intrude on the AC clinically, but routine ASOCT showed it to breach the DM and penetrate the AC, changing the course of management [Fig. 2b and d]. Similarly, ASOCT was performed routinely to document the location and monitor the progression of deep setae in case-8. ASOCT showed one end of the seta to be protruding in the AC.
Armanik et al. have described that for the determination of penetration of an opaque material on ASOCT, one should look for the anterior border of the FB in the AC itself (mirror effect) and not the chain of signals in the posterior shadow zone.[9] In our cases, we did not find any mirror effect. Rather, inward curling of the DM at the site of the breach was a consistent finding in all cases of FBs protruding into the AC. This can be taken as one of the ASOCT characteristics of CFBs breaching the DM [Fig. 2c-e].
To detect and monitor any migration of the FB
Serial ASOCT scans go a long way in documenting and recording even subtle changes of migration in some cases of FB. Migration and extrusion of an encircling buckle are known complications of scleral buckling surgery.[38] However, anterior migration through one or more of the rectus muscles and positioning in the corneoscleral junction is an atypical complication.[39,40] In case-5, the intrastromal buckle was inert and did not cause any complication. ASOCT showed it to be intrastromal without any impingement on the endothelium or AC intrusion. Therefore, it was not removed and the patient was kept under close follow-ups for detecting any further migration. ASOCT is useful for picking up any early subtle changes that may be missed clinically. ASOCT also was helpful to monitor the migration of seta in case-8 as described above. Migration of intracorneal setae can occur anteriorly, leading to resurfacing or posteriorly into deep corneal layers or the AC, both of which can be monitored by serial ASOCT scans.[41]
I-ASOCT can be a very useful tool to guide FB removal at every step and to evaluate any tissue loss or residual corneal bed thinning after FB removal.
Intraoperative optical computed tomography (OCT) is gaining popularity in the treatment of retinal diseases and cataract removal. Intraoperative OCT provides the surgeon with real-time cross-sectional imaging, which is helpful in intraoperative management from the incision to the wound closure.[42] In some cases, after FB removal, corneal thinning might occur due to tissue loss or poor wound healing. I-ASOCT and ASOCT are extremely useful in such cases as they facilitate the quantitative assessment of remnant corneal thickness and indicate the risk of impending perforation.[8] In case-4 and case-6, cyano-acrylate glue and a bandage contact lens were used intra-operatively for thinning and tissue loss, respectively.
Conclusion
ASOCT is thus an imperative adjunct tool for the diagnosis and management of deep corneal and AC FBs. ASOCT facilitates the non-invasive rapid imaging of ocular tissues at various depths. It aids in exact localization, recognizing any breach in the integrity of the Descemet membrane, AC penetration, defining the type of FB, and the need for its removal. We highlight an additional ASOCT finding in the form of inward curling of the DM at the site of the breach in all cases of FB protruding into the AC. Management of various corneal and AC FBs differ depending on the depth (superficial vs deep vs AC) and nature (inert vs non-inert). ASOCT is a useful tool to decide not only the urgency of FB removal but also the best approach. It also helps to assess intraoperative tissue loss and the need for additional tectonic measures. This series collates ASOCT characteristics and management modalities of a unique compilation of FBs such as glass, metal, gun pellets, plastic, caterpillar hair, silicon buckle, firecracker debris, stone chip particle, and human hair, which is quite nonpareil and is under-reported. ASOCT is therefore an indispensable and invaluable tool.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nash EA, Margo CE. Patterns of emergency department visits for disorders of the eye and ocular adnexa. Arch Ophthalmol. 1998;116:1222–6. doi: 10.1001/archopht.116.9.1222. [DOI] [PubMed] [Google Scholar]
- 2.Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–69. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- 3.McGwin G, Jr, Owsley C. Incidence of emergency department-treated eye injury in the United States. Arch Ophthalmol. 2005;123:662–6. doi: 10.1001/archopht.123.5.662. [DOI] [PubMed] [Google Scholar]
- 4.Girgis R, Verma S. Unusual corneal foreign body. Eye (Lond) 2009;23:1609. doi: 10.1038/eye.2008.248. doi:10.1038/eye. 2008.248. [DOI] [PubMed] [Google Scholar]
- 5.Al-Ghadeer HA, Al-Assiri A. Identification and localization of multiple intrastromal foreign bodies with anterior segment optical coherence tomography and ocular Pentacam. Int Ophthalmol. 2014;34:355–8. doi: 10.1007/s10792-013-9800-0. [DOI] [PubMed] [Google Scholar]
- 6.Portero A, Carreño E, Galarreta D, Herreras JM. Corneal inflammation from pine processionary caterpillar hairs. Cornea. 2013;32:161–4. doi: 10.1097/ICO.0b013e318254234b. [DOI] [PubMed] [Google Scholar]
- 7.Wang T, Zhong L, Yin S, Bao T, Yang J, Wang T, et al. Comparison of different types of corneal foreign bodies using anterior segment optical coherence tomography:A prospective observational study. J Ophthalmol. 2020;2020:9108317. doi: 10.1155/2020/9108317. doi:10.1155/2020/9108317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Celebi AR, Kilavuzoglu AE, Altiparmak UE, Cosar CB, Ozkiris A. The role of anterior segment optical coherence tomography in the management of an intra-corneal foreign body. Springerplus. 2016;5:1559. doi: 10.1186/s40064-016-3242-x. doi:10.1186/s40064-016-3242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Armarnik S, Mimouni M, Goldenberg D, Segev F, Meshi A, Segal O, et al. Characterization of deeply embedded corneal foreign bodies with anterior segment optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2019;257:1247–52. doi: 10.1007/s00417-019-04309-y. [DOI] [PubMed] [Google Scholar]
- 10.Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, et al. Optical coherence tomography. Science. 1991;254:1178–81. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Izatt JA, Hee MR, Swanson EA, Lin CP, Huang D, Schuman JS, et al. Micrometer-scale resolution imaging of the anterior eye in vivo with optical coherence tomography. Arch Ophthalmol. 1994;112:1584–9. doi: 10.1001/archopht.1994.01090240090031. [DOI] [PubMed] [Google Scholar]
- 12.Doors M, Berendschot TT, de Brabander J, Webers CA, Nuijts RM. Value of optical coherence tomography for anterior segment surgery. J Cataract Refract Surg. 2010;36:1213–29. doi: 10.1016/j.jcrs.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Leung CK, Chan WM, Ko CY, Chui SI, Woo J, Tsang MK, et al. Visualization of AC angle dynamics using optical coherence tomography. Ophthalmology. 2005;112:980–4. doi: 10.1016/j.ophtha.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 14.Dorairaj S, Liebmann JM, Ritch R. Quantitative evaluation of anterior segment parameters in the era of imaging. Trans Am Ophthalmol Soc. 2007;105:99–108. discussion 108-10. [PMC free article] [PubMed] [Google Scholar]
- 15.Li H, Jhanji V, Dorairaj S, Chua J, Schmidl D, Aranha Dos Santos V, et al. Anterior segment optical coherence tomography and its clinical applications in glaucoma. J Curr Glaucoma Pract. 2012;6:68–74. doi: 10.5005/jp-journals-10008-1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nolan WP, See JL, Chew PT, Friedman DS, Smith SD, Radhakrishnan S, et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology. 2007;114:33–9. doi: 10.1016/j.ophtha.2006.05.073. [DOI] [PubMed] [Google Scholar]
- 17.Sridhar MS, Martin R. Anterior segment optical coherence tomography for evaluation of cornea and ocular surface. Indian J Ophthalmol. 2018;66:367–72. doi: 10.4103/ijo.IJO_823_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicaeus T, Erb C, Rohrbach M, Thiel HJ. Eine Analyse von 148 ambulant behandelten, berufsgenossenschaftlichen Unfällen [An analysis of 148 outpatient treated occupational accidents] Klin Monbl Augenheilkd. 1996;209:A7–11. [PubMed] [Google Scholar]
- 19.Gumus K, Karakucuk S, Mirza E. Corneal injury from a metallic foreign body:An occupational hazard. Eye Contact Lens. 2007;33:259–60. doi: 10.1097/ICL.0b013e31802c140c. [DOI] [PubMed] [Google Scholar]
- 20.Reesal MR, Dufresne RM, Suggett D, Alleyne BC. Welder eye injuries. J Occup Med. 1989;31:1003–6. doi: 10.1097/00043764-198912000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Dass RI, Gohel DJ. Ocular surface foreign body:Its incidence and correlation with specific occupations. GCSMC J Med Science. 2012;2:42–5. [Google Scholar]
- 22.Jahangir T, Butt NH, Hamza U, Tayyab H, Jahangir S. Pattern of presentation and factors leading to ocular trauma. Pak J Ophthalmol. 2011;27:96–102. [Google Scholar]
- 23.Guerra García RA, García DP, Martínez FE, ColumbiéGarbey YE, Martínez RR. The cuban ocular trauma registry. J Clin Exp Ophthalmol. 2013;4:276. doi:10.4172/2155-9570.1000276. [Google Scholar]
- 24.Reddy P, Nirmala K, Radhika S, Ravi S, Paul C. Incidence of ocular surface foreign body and its correlation with specific occupation and preventive measures. Glob J Res Anal. 2016;5:56–8. [Google Scholar]
- 25.Smolin G, Thoft RA. 1st ed. New York: Little, Brown and Company; 1994. The Cornea Scientific Foundation and Clinical Practice; pp. 605–33. [Google Scholar]
- 26.Arora T, Arora S, Sinha R. Management of intrastromal glass foreign body based on anterior segment optical coherence tomography and pentacam analysis. Int Ophthalmol. 2015;35:1. doi: 10.1007/s10792-014-0009-7. doi:10.1007/s10792-014-0009-7. [DOI] [PubMed] [Google Scholar]
- 27.Agrawal S, Raj S, Modaboyina S, Bafna R, Gupta S, Das D. Management of impacted corneal foreign bodies:A review. IP Int J Ocular Oncol Oculoplasty. 2021 doi:10.18231/J.IJOOO.2021.028. [Google Scholar]
- 28.Au YK, Libby C, Patel JS. Removal of a corneal foreign body through a lamellar corneal pocket. Ophthalmic Surg Lasers. 1996;27:471–2. [PubMed] [Google Scholar]
- 29.Sengupta S, Reddy PR, Gyatsho J, Ravindran RD, Thiruvengadakrishnan K, Vaidee V. Risk factors for intraocular penetration of caterpillar hair in Ophthalmia Nodosa:A retrospective analysis. Indian J Ophthalmol. 2010;58:540–3. doi: 10.4103/0301-4738.71711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horng CT, Chou PI, Liang JB. Caterpillar setae in the deep cornea and anterior chamber. Am J Ophthalmol. 2000;129:384–5. doi: 10.1016/s0002-9394(99)00403-1. [DOI] [PubMed] [Google Scholar]
- 31.Singh R, Tripathy K, Chawla R, Khokhar S. Caterpillar hair in the eye. BMJ Case Rep 2017. 2017 doi: 10.1136/bcr-2017-219392. bcr2017219392. doi:10.1136/bcr-2017-219392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manikandan R, Rajesh S, Rajajeyaganthan R. Influence of aluminum in firecracker chemical composition on workplace hazards. Mater Today Proc. 2021 ISSN 2214-7853. doi:10.1016/j.matpr. 2021.01.054. [Google Scholar]
- 33.Saar I, Raniel J, Neumann E. Recurrent corneal oedema following late migration of intraocular glass. Br J Ophthalmol. 1991;75:188–9. doi: 10.1136/bjo.75.3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Ghadeer HA, Al-Assiri A. Identification and localization of multiple intrastromal foreign bodies with anterior segment optical coherence tomography and ocular Pentacam. Int Ophthalmol. 2014;34:355–8. doi: 10.1007/s10792-013-9800-0. [DOI] [PubMed] [Google Scholar]
- 35.Peretz D, Vanden Hoven C, Mireskandari K. Retained intrastromal corneal glass foreign body in an infant. Can J Ophthalmol. 2019;54:e232–3. doi: 10.1016/j.jcjo.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 36.Arora T, Arora S, Sinha R. Management of intrastromal glass foreign body based on anterior segment optical coherence tomography and Pentacam analysis. Int Ophthalmol. 2015;35:1. doi: 10.1007/s10792-014-0009-7. doi:10.1007/s10792-014-0009-7. [DOI] [PubMed] [Google Scholar]
- 37.Archer DB, Davies MS, Kanski JJ. Non-metallic foreign bodies in the anterior chamber. Br J Ophthalmol. 1969;53:453–6. doi: 10.1136/bjo.53.7.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nguyen QD, Lashkari K, Hirose T, Pruett RC, McMeel JW, Schepens CL. Erosion and intrusion of silicone rubber scleral buckle. Presentation and management. Retina. 2001;21:214–20. doi: 10.1097/00006982-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Lopez MA, Mateo C, Corcóstegui I, Corcóstegui B. Transmuscular migration and straddling of the cornea by an encircling buckle. Ophthalmic Surg Lasers Imaging. 2007;38:402–3. doi: 10.3928/15428877-20070901-08. [DOI] [PubMed] [Google Scholar]
- 40.Özdek Ş, Hasanreisoğlu M, Adıgüzel U, Aktaş Z. Secondary glaucoma associated with encircling scleral buckle migration into the cornea. Turk J Ophthalmol. 2016;46:44–6. doi: 10.4274/tjo.02679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sridhar MS, Ramakrishnan M. Ocular lesions caused by caterpillar hairs. Eye (Lond) 2004;18:540–3. doi: 10.1038/sj.eye.6700692. [DOI] [PubMed] [Google Scholar]
- 42.Bondalapati S, Ambati B. Intraocular foreign body removal:A novel technique using intraoperative imaging. Int Ophthalmol. 2017;37:749–52. doi: 10.1007/s10792-016-0304-6. [DOI] [PMC free article] [PubMed] [Google Scholar]