Abstract
Purpose:
To estimate the prevalence of diabetic retinopathy (DR), an emerging cause of sight threat and blindness from a large rural population in Pakistan.
Methods:
This was a population-based cross-sectional study. We selected a rural district of Matiari Sindh Province in Pakistan, where we selected all the health facilities and their attached Lady Health Workers (LHWs)/Lady Health Supervisors (LHSs). These female health workers were trained to identify high-risk diabetic individuals in their catchment areas using pre-defined criteria and to refer them to the nearest health facilities for screening and testing random blood sugar (BSR). Adults of 18 years or above, male or female, were included in the study for DM and DR screening. Ophthalmic examination was conducted by the optometrists on those who had BSR level >180 mg/dl for the evidence of DR. Identified DR patients were referred to a linked tertiary-level ophthalmology institute for their free DR treatment.
Results:
Of the identified and referred 24,463 participants, 23,999 were tested for BSR and 2,331 (9.74%) were found to be high-risk patients (BSR >180 mg/dl) and had ophthalmic examination conducted. Of these, 563 had clinically established DR, a prevalence of 24.2% (95% CI, 22–26%). Significantly more DR patients (228, 40.5%) were found in the age group >60 years, with more among female (327, 58.1%) with DR.
Conclusion:
DR is highly prevalent in the Pakistani rural population. The establishment of an integrated approach within the health care system could decrease the burden of DR in Pakistan.
Keywords: Cross-sectional study, diabetic retinopathy, population-based, prevalence, rural Pakistan
Diabetic retinopathy (DR) is a disease of retina affected by the long-term effect of diabetes mellitus (DM) and is the main reason of blindness and vision impairment.[1] Globally, DR is the fourth leading cause of blindness and the fifth leading cause of visual impairment.[2] Vision impairment affects several functional spheres of life including the physical, mental, social, and overall quality of life and well-being.[3,4] In the year 2019, it was estimated that as many as 30.6 million people had DR in South-East Asia.[5] A meta-analysis of the published data proposed that the worldwide prevalence of any type of DR for the period 2015–2018 was 27.0%.[6] Currently, Pakistan is ranked sixth in terms of diabetic population and will progress to fifth by 2030[7] suspecting an increase of DR burden.
Sufficient large study data are available in most of the South-East Asia countries on the prevalence of DR, and they have established their national plans to preventer burden.[8] However, in Pakistan, the burden of vision loss from DM is not clear,[9] evaluation of DR in diabetic patients is not normally carried out, and there are insufficient studies on prevalence of DR.[9,10] In a recent systematic review on the prevalence of DR in Pakistan by Mumtaz SN et al,[9] the pooled prevalence of DR was found to be 28.78% with very wide variation from 10.6% to 91.3%.[9] Reliable population-based data and particularly data from rural areas for the prevalence of DR are lacking. The complex nature of the DR diagnosis and its assessment in the community are considered as extra difficulties for obtaining reliable DR estimates.[11]
A DR care study was implemented to screen, estimate DR burden, and treat detected patients. We present here the DR prevalence estimates and the age- and gender-wise distribution in a large sample of the rural population in Pakistan.
Methods
The Integrated Model of Care for Diabetic Retinopathy (IMCDR) study was the implementation of an integrated model of care of DM and DR eye-health components into the existing primary health care system. This study was to detect and manage DR in diabetic patients in a rural-population in Sindh province, Pakistan. Here, we present the results of the first part of the study concerned to DM and DR prevalence estimation. The second part of the study is not reported in this paper.
Settings
Sindh is the second largest of the four provinces of Pakistan by population. Matiari, one of 29 districts, was chosen as the rural representative study location having non-availability of eye and diabetic care services. First, it was assumed that disease burden would be greater in such a situation. The second is the possibility of developing an IMCDR within the Government health sector. The other reason was availability of the public-sector functional tertiary-level Institute of Ophthalmology and Visual Sciences (SIOVS) at a nearby adjacent district, from where it was convenient for supervision purposes. In Pakistan, the district is the main unit of the health care delivery system organized by public health sector. Matiari was the fourth smallest district in Sindh with an estimated population of 0.6 million.[12] The district public health sector had 42 health facilities including primary (dispensaries, basic health units, and rural health centers located in the community) and secondary (Taluka hospitals at Tehsil/main town levels and district hospital at the district headquarter level) health facilities along with attached 496 Lady Health Workers (LHWs) working under the supervision of 20 Lady Health Supervisors (LHSs). The LHWs are a cader of female health workers in Pakistan for the responsibility to provide basic primary health care services in their local catchment area.
Study design, participants, and data collection
Our study design was a population-based cross-sectional study. The study participants were accessed through public health-sector primary and secondary health care facilities and selected via their attached LHWs/LHSs at the community level throughout whole district. It was a census of the population of the district in which this work force covered approximately 68.54% of the whole district’s population.[12]
The IMCDR consists of home education/awareness, client visit, blood sugar random (BSR) test, ophthalmic assessment, and then reference to a tertiary-care hospital. Hence, the model of integrated care was to address the issue of DM and DR from identification of high-risk participants by LHW/LHS, the first level of contact in the community, and then refer them to the local health facility for screening and ophthalmology examination. LHW/LHS created awareness, mobilized the community, identified high-risk DM or DR study participants, and referred them to the local health facility for screening and assessment by a health-facility physician and eye examination by a qualified and trained optometrist of the project team. After completing the assessment, if diagnosed as a DR case, then the participant is referred to SIOVS.
The LHWs/LHSs were provided an extensive and detailed training (under supervision of the project study team) by an ophthalmologist regarding DM and its complications such as DR and blindness and other eye health arising issues and risk factors. LHWs/LHSs were also trained on how to mobilize the community and how to create awareness in the community. Printing material containing figures, flow charts, and diagrams were provided and made available to LHWs at all the time during the project period.
After training, LHW was asked to visit door-to-door in her assigned catchment-area houses to teach the families and then find participants having high-risk features for DM such as the family history of diabetes, obesity, frequent urination, unintentional weight loss, slow wound healing, or any impairment of vision. The participants who were meeting the high-risk criteria were encouraged and referred by their LHW to attend a nearby health facility on a fixed scheduled date for screening. At the health facility, initially participants were screened for measuring the BSR level and recorded. The participants whose BSR level was found >180 mg/dl were assigned as DM patients who further underwent for a detailed ophthalmoscope examination by a trained optometrist for the diagnosis of any type of DR. The optometrist completed a standardized ophthalmic examination of all the DM patients, and diagnosis was confirmed if any type of DR was found on dilated eyes. DM-diagnosed patients were referred to the health-facility physician for diabetes management, and all confirmed patients with DR were referred to the linked eye-hospital (SIOVS) for clinical DR treatment and diabetes management.
At the health facility apart from the facility physician, the project team comprised an optometrist, an ophthalmic technician, a data entry operator, and a project-team leader for the purpose of project management. The optometrist was qualified to perform eye examination and well trained to distinguish between normal and abnormal retinas of a dilated eye pupil by using a direct ophthalmoscope. The team visited a health facility as per the planned and approved monthly schedule by a District Health Officer with a coordinated and well-informed way among all the stakeholders. The concerned LHWs/LHSs were asked to refer the identified high-risk participants for the screening and ophthalmic examination on the fixed dates as per the monthly schedule.
Ophthalmic examination was carried out on all the diabetic patients having a BSR level above 180 mg/dl. Diabetic patients had their eye pupils dilated with 1% tropicamide and were screened for DR by an optometrist using a direct ophthalmoscope. The main outcome measure was the presence of DR considered of any type, grade, and severity and at any stage, whether proliferative- or non-proliferative-type DR.
Data collection was performed by the project-team and health-facility staff at the time of the screening and clinical examination. A structured questionnaire was administered by face-to-face interview to collect the data on some socio-demographic characteristics including age, gender, home address, occupation, blood test recording of the BSR level, and ophthalmic examination findings. The screened patient’s history was studied and lab tests for BSR level, examination and the diagnoses, and so on were carried out and recorded by the ophthalmic technician/data entry operator.
Inclusion criteria were any adults of ≥18 years of age, male or female, who were residing in the local catchment areas and consented for DM and DR screening, DR-diseased/non-diseased, known/unknown for diabetes, referred by LHW/LHS or the health-facility physician or self-referred for the screening purpose at the local health facility. If BSR >180 mg/dl, then the case was considered for ophthalmic examination. The exclusion criteria were any adult male or female not less than the age of 18 years, mentally handicapped, not consented, and not belonging to the district locally.
Sample size
The sample size was based on the available local information regarding areas and population of administrative units from the Bureau of Statistics Pakistan[12] and estimates of DR from a study by Ahsan et al.,[13] published in the year 2015. For our study, we considered a whole Matiari district population of 670,516. The district’s covered population by LHWs was 459,603 (68.54%). We assumed about 40% of the covered population above 18 years of age to be screened in 2 years (2017–18) for DM and DR based on the DM prevalence rate at 6.8% and the DR prevalence rate at 27% in the confirmed DM cases having BSR level >180 mg/dl.[13]
Statistical analysis
Data were entered using Microsoft Excel and then cleaned and moved for analyses using SPSS Software version 20.0 (IBM Corporation, New York, USA). The rates and percentages of age and gender were calculated. The overall prevalence of DR verified/diagnosed by eye examination was estimated. DR prevalence by age categories and gender are also reported. Chi-square test was used to observe the relationship between DR status and demographic variables including age groups and gender. Univariate and multi-variable analyses were performed using the Cox proportional hazard algorithm. The results are reported in terms of crude and adjusted prevalence ratios with 95% confidence intervals. Continuous variables were also tested using the independent sample t-test. The statistical significance level was set at P < 0.05.
Results
In the district Matiari during 2017–2018, altogether, 24,463 identified high-risk participants, aged ≥18 years and above, were referred by LHWs/LHSs/MOs to health facilities for the screening purpose. Of these, 23,999 (98%) participants who meet the criteria were screened for testing BSR. A total of 2,331 (9.7%) had BSR level >180 mg/dl and were considered eligible for ophthalmoscopy examination. Therefore, the prevalence of high-risk and confirmed DM cases for the screened sample of participants was 9.74% [2331/23999; 95% confidence interval (CI): 9.36–10.11%] [see Fig. 1 study flow diagram and Table 1]. Of the 2,331 confirmed DM patients, examination confirmed any type of DR in 563 patients. Therefore, the prevalence of DR was 24.2% [563/2331; 95% CI 22–26%].
Figure 1.
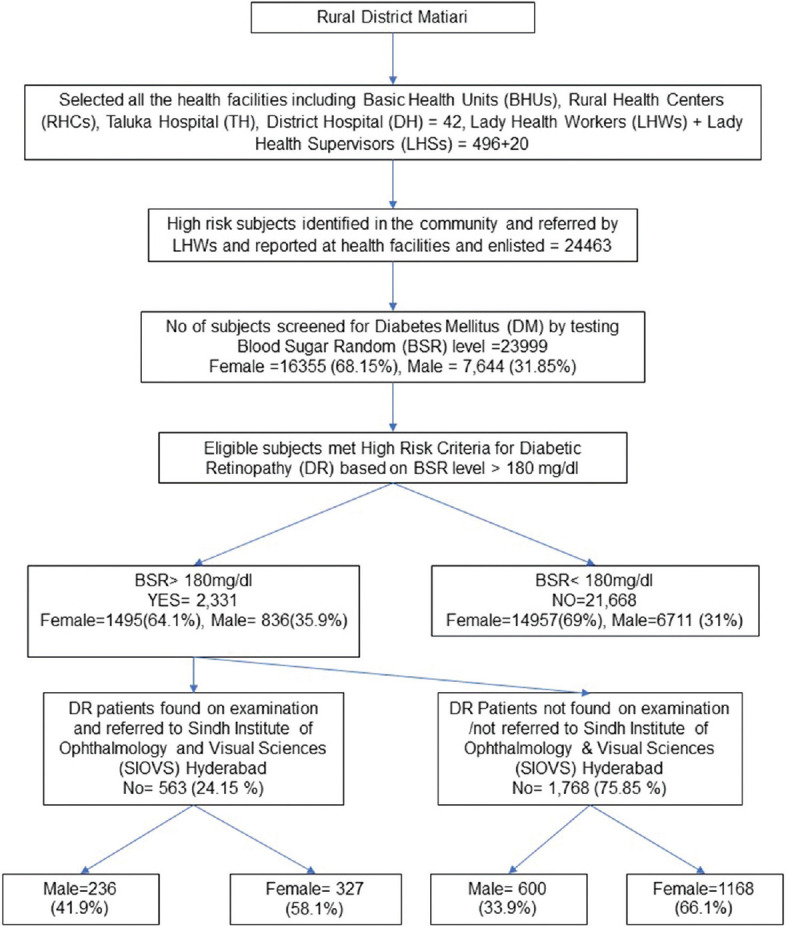
Flow Diagram showing the Screening of Objectæs and identification of DR patients through the examination of DM patients in District Matiari
Table 1.
Demographic characteristics of diabetic patients with and without DR
| Characteristics | DR cases (n=563) n (%) | No DR cases (n=1768) n (%) | Total Diabetic cases (n=2331) n (%) | P |
|---|---|---|---|---|
| Age (years) | ||||
| <30 years | 6 (1.1) | 72 (4.1) | 78 (3.3) | <0.001 |
| 30-34 years | 11 (2.0) | 44 (2.5) | 55 (2.4) | |
| 35-39 years | 30 (5.3) | 273 (15.4) | 303 (13.0) | |
| 40-44 years | 51 (9.1) | 322 (18.2) | 373 (16.0) | |
| 45-49 years | 73 (13.0) | 259 (14.6) | 332 (14.2) | |
| 50-54 years | 73 (13.0) | 238 (13.5) | 311 (13.3) | |
| 55-59 | 91 (16.2) | 241 (13.6) | 332 (14.2) | |
| >60 years | 228 (40.5) | 319 (18.0) | 547 (23.5) | |
| Gender | ||||
| Male | 236 (41.9) | 600 (33.9) | 836 (35.9) | 0.003 |
| Female | 327 (58.1) | 1168 (66.1) | 1495 (64.1) |
Some of the detailed characteristics of the patients with DR and without DR are given in Table 1.
Table 2 shows DR patients and their age and gender distribution. The mean age of the patients with DR was 54.93 ± 11.28 (range 65 years) compared with 48.06 ± 11.84 (range 67 years) in those without DR. This difference was not statistically significant, but in terms of age groups, significantly more patients with DR were aged >60 years (P < 0.001) as most of the DR patients were found in the older age group of 60 years or above in 228 (40.5%) patients. There was no gender difference either but significantly more of the females with DR than males with DR (P 0.003) as female patients with DR 327 (58.1%) were found to be more than male patients with DR 236 (41.9%) [Table 1].
Table 2.
Age distribution of DR patients by gender.
| Female n (%) | Male n (%) | Both Male and Female (563) n (%) | |
|---|---|---|---|
| Age (Years) | |||
| <30 years | 4 (0.7) | 2 (0.4) | 6 (1.1) |
| 30-34 years | 6 (1.1) | 5 (0.9) | 11 (2.0) |
| 35-39 years | 21 (3.7) | 9 (1.6) | 30 (5.3) |
| 40-44 years | 27 (4.8) | 24 (4.3) | 51 (9.1) |
| 45-49 years | 46 (8.2) | 27 (4.8) | 73 (13.0) |
| 50-54 years | 47 (8.3) | 26 (4.6 | 73 (13.0) |
| 55-59 | 50 (8.9) | 41 (17.3) | 91 (16.2) |
| >60 years | 126 (22.4) | 102 (18.1) | 228 (40.5) |
Table 3 shows that the prevalence ratio between age and gender characteristics of diabetic patients with DR. Multi-variable analysis using the Cox regression algorithm carried out for identifying the prevalence ratio showed that the prevalence of DR patients among DM cases in the age group 30–34 years was 2.45 times more as compared to DM cases in the age group <30 years, and this independently increasing association with an increased likelihood of DR patients was seen in all the age groups. In the case of gender, the prevalence of female DR patients in DM cases was 23% lower (PR = 0.77) as compared to male DM cases [Table 3].
Table 3.
DR Prevalence Ratio (95% CI) by Demographic Characteristics of Diabetic Patients
| Risk Factor | Total Diabetic Patients in the group | Number with DR | Prevalence within the group | PR | (95% CI) | P |
|---|---|---|---|---|---|---|
| DR by Age (years) | ||||||
| <30 years | 78 | 6 | 7.69 | 1.00 | - | <0.001 |
| 30-34 years | 55 | 11 | 20.0 | 2.45 | 0.91-6.655 | 0.077 |
| 35-39 years | 303 | 30 | 9.9 | 1.25 | 0.52-3.016 | 0.611 |
| 40-44 years | 373 | 51 | 13.67 | 1.75 | 0.75-4.076 | 0.195 |
| 45-49 years | 332 | 73 | 21.98 | 2.78 | 1.21-6.385 | 0.016 |
| 50-54 years | 311 | 73 | 23.47 | 3.00 | 1.31-6.902 | 0.010 |
| 55-59 | 332 | 91 | 27.40 | 3.43 | 1.50-7.837 | 0.003 |
| >60 years | 547 | 228 | 41.68 | 5.263 | 2.34-11.842 | <0.001 |
| DR by Gender | ||||||
| Male | 836 | 236 | 28.23 | 1.00 | - | <0.001 |
| Female | 1495 | 327 | 21.87 | 0.77 | 0.65-0.915 | 0.003 |
Discussion
In Pakistan, hardly any study has reliably estimated DR prevalence at the rural-population level to understand the DR disease burden in the country for an action planning strategy. In this study, suspected high-risk participants with DM were mobilized, encouraged, and referred by LHWs to the local public health care system facilities, followed by a complete assessment of DM and an eye examination for DR confirmation. This study has shown a DR prevalence of 24.2% (95% CI, 22–26%) in all DM cases aged 18 years and above, 28.2% (95% CI, 25.2–31.3%) in males and 21.9% in females (95% CI, 19.8–24.0%).
The result for prevalence of DR from our study is consistent with some of the similar types of studies seen in the literature globally, regionally, and nationally. First, globally for the period 2015–18, a meta-analysis of published data suggests that the worldwide prevalence for any type of DR was 27.0%.[1] Second, regionally, meta-analysis was performed for nine South-East Asian countries, including Nepal, Bangladesh, Bhutan, India, Indonesia, Maldives, Myanmar, Sri Lanka, and Thailand; the pooled prevalence of DR was 27.8% (varied from 12.4 to 43.1%).[1] There were only three cross-sectional studies conducted in the countries Indonesia, Sri Lanka, and Thailand with the prevalence of 43.1%, 27.4%, and 31.4%, respectively. Our study results are consistent to Sri Lankan study.[14] Third, at the national Pakistan level from a recent systematic review by Mumtaz SN et al,[9] of the included 29 nationwide studies in 27 years (1990–2017), a pooled analysis of 38,438 subjects with diabetes showed DR in 11,064 patients, with an estimated prevalence of 28.78% for any type of DR.[9] However, the prevalence found in our study is consistent with one of the prevalence studies reported by Memon et al.,[15] which found 24.7% because of some of methodological similarities of both of the studies. A study by Memon et al.,[15] conducted between March 2009 and December 2011 at the World Health Organization collaborative primary health-care center, where 10,768 registered diabetic cases were screened for retina examination by a fundus camera and retina specialist, evaluated the retinal photographs. The overall frequency of DR was found in 266 (24.7%) patients. Regardless of Type I or II diabetes, DR was found with an increased rate in females of the working age group compared to males.
In our study, distribution of DR disease was found in almost all age groups, but a higher number of cases [228 (40.5%)] was observed in the older age group above 60 years of age. The best suggestion for this could be because DM has the associated impact of long-term chronic complications and the influence of an advanced age and long duration of the disease in the development of such complication.[1] Almost the same is the finding in the study by Memon, et al.,[15] where a higher number of DR cases were seen in the older age group of 46–60 years but with Type II diabetes. However, trends with an increasing frequency of DR cases were seen with Type I diabetes in the younger and working class age group of 16–30 years. It is a general experience that the majority of diabetic patients who develop DR have no symptoms until the late stages of proliferative DR complications occur.[1] In our study, a few cases [6 (1.1%)] were seen in the younger age group below 30 years. However, this increase of DR in the younger age group reflects the alarming situation in South-East Asia regarding DM and DR.[1]
In our study, significantly more female patients with DR, 327 (58.1%), were observed compared to male patients with DR, 236 (41.9%). These results are also consistent with findings from Memon et al.[15] study that the DR was found with an increased frequency in females regardless of the kind of diabetes. However, in the study by Katulanda P et al.[14] from Sri Lanka, no significant gender difference (females 25.6%, males 30.5%; P = 0.41) was observed in the prevalence of DR.
The prevalence of DR found in our study is inconsistent from other studies found in the national or international published literature. It is because of consideration of different methodological issues including different sampling schemes, inclusion/exclusion criteria, small sample sizes, duration of study periods, different study designs conducted (hospital-based or population-based), different data collection methods, use of non-suitable detection tools for DR examination procedures, and using different examination methods or applying classification systems for assessing the types of DR. For example, since the systematic review by Mumtaz SN et al.,[9] there were only four cross-sectional studies out of 29 studies. In most of the studies, even age groups or gender variations were not taken into account. Furthermore, both DM and DR are the diseases that also get influenced by other multiple social and environmental factors such as living life style, diet, activity, obesity, and so on.[16]
Strengths and limitations
This population-based cross-sectional study has its strengths as follows: This is the first time this study is conducted in a rural area where we created an awareness and mobilized study participants for screening of DR at the community level. Therefore, there was a high response rate and a large sample of over 24,000 participants who attended the health centers for screening of DR. The data collection methods were designed in such a way to maximize the identification of high-risk DM cases from LHW-referred cases and likelihood of accurate diagnosis of DR patients at the health facility. At the planning stage, maximum attention was given to accurate diagnosis of DR despite deficiency of eye health experts in the rural area. The LHWs were given proper training and provided with printing material to create a confidence in them and in the community and explained participants that necessary treatment would be available and free.
The possible limitations of the study are as follows: Although the referral and attendance response at the health facilities was very high, it might be possible that many high-risk participants who were encouraged and asked for referral by LHWs did not attend for the screening of DR at the health facilities, and possibly, we missed some of those DR patients. Therefore, it could be possible that not all high-risk participants with DR attended the health facilities. Hence, we did not calculate non-responsive high-risk community participants. Furthermore, because our main focus of the study was estimation of the burden of DR disease at the community level, the estimation of the lifetime prevalence of DR was not taken in this study.
Conclusion
There is a very less number of rural population-based studies conducted in the country. The estimate of DR, 24.2% in Pakistan, is very high and required to be made both to prevent its occurrence via the establishment of an integrated model DM and DR care services into the health care system and to provide its complete treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Strengthening diagnosis and treatment of diabetic retinopathy in the South-East Asia Region. Global burden of diabetes and diabetic retinopathy (IAPB vision atlas) June 2020. World Health Organization South-East Asia [Google Scholar]
- 2.TADDS-WHO:Tool for assessment of DR and Diabetes Management systems. WHO. 2015 [Google Scholar]
- 3.Swenor BK, Lee MJ, Varadaraj V, Whitson HE, Ramulu PY. Aging with vision loss:A framework for assessing the impact of visual impairment on older adults. Gerontologist. 2020;60:989–95. doi: 10.1093/geront/gnz117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ICF- International classification of functional disabilities and health WHO-2001. [Last accessed on2022 Jan 07]. at https.//www.who.int/standards/classifications .
- 5.Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besancon S, et al. Global and regional estimates and projections of diabetes-related health expenditure:Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Research and Clinical Practice. 2020:162. doi: 10.1016/j.diabres.2020.108072. [DOI] [PubMed] [Google Scholar]
- 6.Thomas RL, Halim S, Gurudas S, Sivaprasad S, Owens DR. IDF Diabetes Atlas:A review of studies utilising retinal photography on the global prevalence of diabetes related retinopathy between 2015 and 2018. Diabetes Res Clin Pract. 2019;157:107840. doi: 10.1016/j.diabres.2019.107840. [DOI] [PubMed] [Google Scholar]
- 7.Sohail M. Prevalence of diabetic retinopathy among type- 2 diabetes patients in Pakistan- Vision Registry. Pak J Ophthalmol. 2014;30:204–12. [Google Scholar]
- 8.Hassan B, Ahmed R, Li B, Noor A, Hassan Zu. A comprehensive study capturing vision loss burden in Pakistan (1990-2025):Findings from the Global Burden of Disease (GBD) 2017 study. PLoS One. 2019;14:e0216492. doi: 10.1371/journal.pone.0216492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mumtaz SN, Fahim MF, Arslan M, Shaikh SA, Kazi U, Memon MS. Prevalence of diabetic retinopathy in Pakistan;A systematic review. Pak J Med Sci. 2018;34:493–500. doi: 10.12669/pjms.342.13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Afghani T, Khan SB, Mansoor H, Nisar S, Waseem S. Assessment of diabetic retinopathy and diabetes management systems in Pakistan using a WHO tool. J Pak Med Assoc. 2020;70:1619–24. doi: 10.5455/JPMA.12450. [DOI] [PubMed] [Google Scholar]
- 11.Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health:Vision beyond 2020. Lancet Glob Health. 2021;9:E489–551. doi: 10.1016/S2214-109X(20)30488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Areas and population of Administrative Units. Pakistan Bureau of Statistics. 1998. Available from: https://www.pbs.gov.pk/node/3391/?name=087 .
- 13.Ahsan S, Basit A, Ahmed KR, Ali L, Khanam R, Fawwad A, et al. Risk indicators of diabetic retinopathy in patients with type 2 diabetes screened by fundus photographs:A study from Pakistan. Int J Diabetes Dev Ctries. 2015;35:333–8. [Google Scholar]
- 14.Katulanda P, Ranasinghe P, Jayawardena R. Prevalence of retinopathy among adults with self-reported diabetes mellitus:The Sri Lanka diabetes and Cardiovascular Study. BMC Ophthalmol. 2014;14:100. doi: 10.1186/1471-2415-14-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Memon S, Ahsan S, Riaz Q, Basit A, Sheikh SA, Fawad A, et al. Frequency, severity and risk indicators of retinopathy in patients with diabetes screened by fundus photographs:A study from primary health care. Pak J Med Sci. 2014;30:366–72. [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung N, Mitchell P, Wong TY. Diabetes retinopathy. Lancet. 2010;376:124–36. doi: 10.1016/S0140-6736(09)62124-3. [DOI] [PubMed] [Google Scholar]


