Abstract
Purpose:
To compare the stereoacuity in patients with anisometropia, isometropia, and emmetropia.
Methods:
A cross-sectional study was conducted on 1403 subjects (range: 5–45 years) divided into anisometropes (n = 403), isometropes (n = 500), and emmetropes (n = 500). There were 258 amblyopic eyes among anisometropes and 156 amblyopic eyes among isometropes. Stereoacuity was measured using the Titmus stereo test consisting of a combination of contour targets.
Results:
There were 675 males and 728 females. A significant (P < 0.001) reduction in stereoacuity was found in anisometropes as compared to isometropes and emmetropes. The stereoacuity was even worse in amblyopes as compared to non-amblyopes. Most patients with anisometropia of <3.0 D had fair stereoacuity. However, as the degree of anisometropia increased to >3.0 D, stereoacuity deteriorated gradually. Marked reduction of stereoacuity was observed in severe degree of anisometropia (>6.0 D). Overall, an anisometropia of ≥2.12 D was associated with reduced stereoacuity. Among the anisometropes, it was found to be the poorest in myopia, followed by myopia with astigmatism, hypermetropia with astigmatism, and hypermetropia.
Conclusion:
The level of stereoacuity was worse in anisometropes as compared to isometropes and emmetropes. Amblyopes had a greater reduction in stereoacuity than non-amblyopes. Stereoacuity decreased as the degree of anisometropia increased. Among the anisometropes, myopes had worst stereoacuity than hypermetropes.
Keywords: Amblyopia, anisometropia, emmetropia, isometropia, stereoacuity
Stereopsis occurs due to the simultaneous stimulation of horizontally disparate retinal elements, the fusion of which results in a single visual impression perceived in depth.[1,2,3] Gross stereopsis is essential for orientation in space while moving, and fine stereopsis is important for fine motor tasks.[4] Surface inspection and analysis, or related tasks, may require a stereoscopic image.[5]
Most authors define anisometropia as the difference in the interocular refractive power of 1D.[6,7,8] As anisometropia disturbs binocularity, it also causes reduction in stereopsis. It has been suggested that foveal suppression in the defocused eye is the cause of decreased stereopsis.[9]
The present study was conducted to evaluate the effect of decreased stereoacuity on the quality of vision in anisometropes as compared to isometropes and emmetropes.
Methods
The cross-sectional study was conducted on 1403 patients at a tertiary eye care center between September 2019 and December 2021. Informed consent was obtained. Patients having very hazy media, lenticular opacity, ocular deviation, non-centric fixation, undergone any previous ocular surgery, any history of ocular trauma, and uncooperative patients were excluded from the study. Individuals with anisometropia >1 D, isometropia, or emmetropia between the age group of 5–45 years with clear media were included in the study.
In the present study, anisometropia was considered as an interocular difference of >1.00 D in spherical equivalent, and amblyopia was regarded as the difference in visual acuity of two or more lines on the Early Treatment Diabetic Retinopathy Study (ETDRS) chart between the eyes or visual acuity of 6/12 or worse bilaterally.
Detailed history taking and meticulous ocular examination were done. In all the cases, cycloplegic refraction and post-mydriatic test were manually carried out by a single refractionist. Assessment of distant visual acuity and refractive status was done using the ETDRS chart, with the patient seated at a distance of 4 m and recorded in logMAR units. Near vision was recorded using Jaeger chart. The patient was then subjected to cycloplegic refraction. The refractive correction was prescribed. Spherical equivalent (spherical component +½ cylinder component) was calculated for each patient.
All the patients were subjected to a meticulous slit-lamp and fundus examination by direct and indirect ophthalmoscopy and slit-lamp biomicroscopy by a 90-D lens to rule out any other ocular pathology.
Stereoacuity was assessed using the Titmus stereo test consisting of a combination of contour targets by a single orthoptist who was unaware of the refractive status of the patient. The patient was asked to wear his best refractive correction before the test, and the test was done before pupillary dilatation. The patient wore polarized glasses and was asked to see the stereo chart at a distance of 40 cm. The level of stereopsis was recorded on the basis of the last one (circle/animal) chosen correctly in seconds of arc, considering the finest (highest) stereoacuity as 40 seconds of arc and the lowest stereoacuity as 3552 seconds of arc.
The patients included in the study were divided into three major groups: anisometropic group (A), isometropic group (B), and emmetropic group (C). Based on the type of refractive error, anisometropes and isometropes were further divided into four subgroups: myopia, myopia with astigmatism, hypermetropia, and hypermetropia with astigmatism. The degree of anisometropia (difference in spherical equivalent) between the two eyes in the anisometropic group was further divided as mild (>1–3 D), moderate (>3–6 D), and severe (>6 D).
Statistical analysis was performed using SPSS 21.0 (Statistical Package for the Social Sciences version 21) for Windows software (SPSS Inc., Chicago, Illinois, USA). Values were presented as mean ± standard deviation (SD) for continuous variables and as numbers (percentage) for categorical variables. One-way analysis of variance (ANOVA) test was applied to compare data between three or more groups. Independent samples t test was used for comparison of stereoacuity between amblyopes and non-amblyopes. Bivariate correlation analysis was used for analyzing statistical significance of changes in stereoacuity with the degree of anisometropia. ROC curve was used to determine the level of anisometropia that is prone to reduced stereoacuity. P <0.05 was taken as significant.
Results
The present study was conducted on 1403 patients (age: 5–45 years) distributed into three major groups: anisometropic group (A) [>1 D, (n = 403)], isometropic group (B) [≤1 D, (n = 500)], and emmetropic group (C) [n = 500].
The anisometropic group (A) had 116 (28.8%) patients with myopia (A1), 136 (33.7%) patients with myopia with astigmatism (A2), 80 (19.9%) patients with hypermetropia (A3), and 71 (17.6%) hypermetropia with astigmatism (A4). The degree of anisometropia (difference in spherical equivalent between the two eyes) was divided as mild (>1–3 D) having 177 (43.9%) patients, moderate (>3–6 D) comprising 146 (36.2%) patients, and severe (>6 D) comprising 80 (19.9%) patients.
The isometropic group (B) had 172 (34.4%) patients with myopia (B1), 183 (36.6%) patients with myopia with astigmatism (B2), 78 (15.6%) patients with hypermetropia (B3), and 67 (13.4%) patients with hypermetropia with astigmatism (B4).
The mean age of all patients included in the study was 26.70 ± 9.40 years (range: 5–45 years). There were 675 males (48.1%) and 728 females (51.9%) in the study. There was no significant difference between any group (A, B, or C) with regard to age and gender distribution and thus were age- and gender-matched.
In the anisometropic group, the right eye was found to have more refractive error when compared to the left eye (52.4% of anisometropic subjects had a greater refractive error in the right eye, whereas 47.6% of subjects had a greater refractive error in the left eye). The eye with the higher refractive error was labeled as the “worst eye,” and the eye will less refractive error as the “fellow eye.”
In the anisometropic group, there were a total of 258 (64%) amblyopic eyes. Among the various subgroups, 55 (75.5%) worst eyes were amblyopic in the hypermetropia with astigmatism group, followed by 57 (71.3%) in the hypermetropic group, 66 (48.5%) in the myopia with astigmatism group, and 42 (36.2%) in the myopia group. The fellow eyes were amblyopic in some cases of unequal but bilateral high refractive error. In the fellow eyes, amblyopia was present in 20 (14.7%) eyes in the myopia with astigmatism group, followed by nine (11.3%) eyes in the hypermetropia group, six (5.2%) eyes in the myopia group, and three (4.2%) eyes in the hypermetropia with astigmatism group. In all four subgroups, the maximum number of worst eyes were amblyopic in the severe degree of anisometropia.
Due to equal and bilateral high refractive error, isometropic amblyopia was present in some patients of the isometropic group (B). There were a total of 156 (31%) amblyopic eyes among isometropes. Among the various subgroups, 26 (38.8%) right eyes were amblyopic in the hypermetropia with astigmatism group, followed by 32 (17.5%) in the myopia with astigmatism group, nine (11.5%) in the hypermetropic group, and 13 (7.6%) in the myopic group. In the left eyes, amblyopia was present in 26 (38.8%) eyes in the hypermetropia with astigmatism group, followed by 28 (15.3%) eyes in the myopia with astigmatism group, nine (11.5%) eyes in the hypermetropia group, and 13 (7.6%) eyes in the myopia group.
The Titmus stereo test used in the present study recorded stereoacuity ranging from 40 (best) to 3552 (worst) seconds of arc. The mean stereoacuity in the anisometropic group was 614.40 ± 1027.80 (range: 40–3552 seconds of arc). A statistically significant negative correlation was found between the degree of anisometropia and stereoacuity (Pearson’s correlation coefficient = −0.682; P < 0.001). Stereoacuity was found to be even worse in amblyopes as compared to non-amblyopes in the anisometropic group (1002.25 ± 1199.84 vs. 148.12 ± 447.88; P < 0.001).
The mean stereoacuity in the isometropic group (B) was 132.34 ± 405.432 (range: 40–3552 seconds of arc). Stereoacuity was found to be worse in amblyopes as compared to non-amblyopes in the isometropes as well [583.65 ± 889.94 vs. 46.38 ± 11.71 (95% CI: −622.26 to − 452.27); P < 0.001].
The mean stereoacuity in the emmetropic group was 40.12 ± 1.54 (range: 40–60 seconds of arc).
Stereoacuity was found to be reduced in all four subgroups of the anisometropic group (A). Stereoacuity was found to be worse in myopes (subgroups A1 and A2) as compared to hypermetropes (subgroups A3 and A4), which was statistically significant (F = 2.941; df = 3; P = 0.033) [Table 1]. In the present study, the amount of difference in spherical equivalent (severe degree of anisometropia) was found to be more in myopes as compared to hypermetropes: myopia (9.18 ± 1.77 D), myopia with astigmatism (7.54 ± 1.48 D), hypermetropia with astigmatism (6.83 ± 0.89 D), and hypermetropia (6.79 ± 0.81 D). As stereoacuity is a binocular function, this large amount of difference in spherical equivalent in myopes as compared to hypermetropes may be responsible for poorer stereoacuity in myopes than hypermetropes.
Table 1.
Stereoacuity profile in various subgroups of the anisometropic group
| Group | Mean | SD | 95% CI for mean | P | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Myopia (A1) | 518.21 | 1014.27 | 331.67 | 704.75 | 0.033 |
| Myopia with astigmatism (A2) | 783.12 | 1246.367 | 571.75 | 994.48 | |
| Hypermetropia (A3) | 676.08 | 1010.875 | 451.12 | 901.03 | |
| Hypermetropia with astigmatism (A4) | 378.87 | 310.159 | 305.46 | 452.29 | |
Bivariate correlation analysis revealed that as the degree of anisometropia increased, stereoacuity decreased. It was found to be the poorest in myopia, followed by myopia with astigmatism, hypermetropia with astigmatism, and hypermetropia [Table 2].
Table 2.
Statistical analysis of correlation of stereoacuity with the degree of anisometropia in various subgroups
| Group | Pearson’s correlation coefficient | P |
|---|---|---|
| Myopia (A1) | −0.819 | <0.001 |
| Myopia with astigmatism (A2) | −0.754 | <0.001 |
| Hypermetropia (A3) | −0.344 | 0.002 |
| Hypermetropia with astigmatism (A4) | −0.699 | <0.001 |
Most patients with anisometropia of <3.0 D had fair stereoacuity. However, as the degree of anisometropia increased to >3.0 D, stereoacuity deteriorated gradually. Marked reduction in stereoacuity was observed in severe degree of anisometropia (>6.0 D) [Fig. 1]. ROC curve was used to determine the level of anisometropia that is prone to reduced stereoacuity. Significant value for the area under the ROC (AUROC) was 0.80 (95% CI: 0.76–0.85); P < 0.001 [Fig. 2]. When the degree of anisometropia was ≥ 2.12 D, the sensitivity and specificity of the deterioration of stereoacuity were 75.5% and 70.6%, respectively. Among the various subgroups, the threshold values of anisometropia which resulted in reduced stereoacuity in myopia, myopia with astigmatism, hypermetropia, and hypermetropia with astigmatism were found to be 2.12, 2.37, 2.25, and 2.37 D, respectively.
Figure 1.

Association between the degree of anisometropia and stereoacuity
Figure 2.
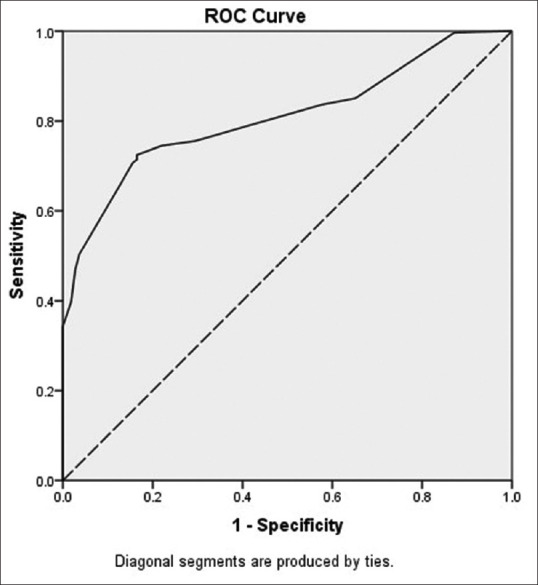
ROC curve for the level of anisometropia prone to reduced stereoacuity
Among the anisometropes, stereoacuity was found to be the worst in patients having unequal vision of more than two lines difference (amblyopes) [1039.75 ± 1245.94 (95% CI: 861.92–1217.58)], followed by patients having unequal vision of less than two lines difference [622.29 ± 1226.78 (95% CI: 200.87–1043.70)] and patients having equal vision [153.84 ± 191.36 (95% CI: 125.46–182.23)]. This difference in stereoacuity was found to be statistically significant (F = 40.901; df = 2; P < 0.001).
In the isometropic group (B), stereoacuity was reduced in hypermetropia with astigmatism and was within the normal limit in the rest of the subgroups. This could be due to the presence of more amblyopes in the hypermetropia with astigmatism group (B4), and this reduction was statistically significant (F = 17.876; df = 3; P < 0.001) [Table 3].
Table 3.
Stereoacuity profile in various subgroups of the isometropic group (B)
| Group | Mean | SD | 95% CI for mean | P | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Myopia (B1) | 81.81 | 280.66 | 39.57 | 124.06 | <0.001 |
| Myopia with astigmatism (B2) | 94.21 | 152.42 | 71.98 | 116.44 | |
| Hypermetropia (B3) | 58.21 | 48.55 | 47.26 | 69.15 | |
| Hypermetropia with astigmatism (B4) | 452.54 | 922.28 | 227.58 | 677.50 | |
Overall analysis of stereoacuity in amblyopes versus non-amblyopes combining both anisometropes as well as isometropes revealed that stereoacuity was worse in amblyopes as compared to non-amblyopes [930.25 ± 1165.85 vs. 79.27 ± 238.85 (95% CI: −942.75 to − 759.21); P < 0.001].
The stereoacuity was found to be worse among anisometropes [614.40 ± 1027.80 (95% CI: 513.75–715.05)] as compared to isometropes [132.34 ± 405.43 (95% CI: 96.72–167.97)] and emmetropes [40.12 ± 1.54 (95% CI: 39.98–40.26)], which was statistically significant (F = 113.636; df = 2; P < 0.001) [Table 4].
Table 4.
Comparison of stereoacuity profile between anisometropic group (A), isometropic group (B), and emmetropic group (C)
| Group | Mean | SD | 95% CI for mean | P | |
|---|---|---|---|---|---|
|
| |||||
| Lower | Upper | ||||
| Anisometropic group (A) | 614.40 | 1027.80 | 513.75 | 715.05 | <0.001 |
| Isometropic group (B) | 132.34 | 405.43 | 96.72 | 167.97 | |
| Emmetropic group (C) | 40.12 | 1.54 | 39.98 | 40.26 | |
Discussion
Stereopsis being the highest form of binocular cooperation adds a new quality to vision.[1,3] Surface properties such as scintillation, sheen, and luster differ in luminance and color between the right and left retinal images and cannot be viewed in single image.[5] Stereopsis is the requisite for performing fine and precise tasks and for visuo-manual coordination. The formation of high-quality foveal images in the both eyes is desirable for fine stereopsis.[1,2,3]
Anisometropia can lead to defocused retinal image in one eye, encompassing reduced retinal image size, clarity, and contrast, and the duration of the defocus spans from intermittent to permanent time periods, meaning that the signal from one anisometropic eye sent to the brain for scrutinization cannot be coordinated with that from the other anisometropic eye. It was proposed that amblyopia may occur as a result of defocused image and active suppression caused by anisometropia.[1,10]
Previous studies have shown that anisometropia is associated with reduced stereoacuity. However, the majority of these studies were conducted in fewer patients and a comparison of stereoacuity in anisometropes was not done with isometropes and emmetropes. Furthermore, there is a dearth of sufficient studies on the comparison of stereoacuity in various types of refractive errors.
Gawecki[11] conducted a study on 40 subjects to find out the threshold values of myopic anisometropia that lead to the loss of stereoacuity in majority of the patients. Various focusing lenses were placed in front of the right eye of the subject in the trial frame to evoke anisometropia. The author reported that myopic anisometropia of more than 2 D can cause a significant impairment of stereoacuity. In the present study, patients with anisometropia of ≥2.12 D were found to have reduced stereoacuity. The threshold values of anisometropia that resulted in reduced stereoacuity in myopia, myopia with astigmatism, hypermetropia, and hypermetropia with astigmatism were 2.12, 2.37, 2.25, and 2.37 D, respectively.
Jeon and Choi[12] conducted a study to assess the level of stereopsis and fusion in patients with anisometropia according to the presence of amblyopia. They divided 107 children into groups with non-amblyopic anisometropia (NA, n = 72) and amblyopic anisometropia (AA, n = 35). Normal subjects without anisometropia were included in the control group (n = 73). They observed that the levels of stereopsis and sensory fusion with anisometropic glasses were significantly worse in the amblyopic anisometropia group than in the non-amblyopic anisometropia group. Similarly, in the present study, stereoacuity was found to be even worse in amblyopes as compared to non-amblyopes.
In the present study, stereoacuity was found to be reduced in all types of refractive errors in the anisometropic group. It was observed that as the degree of anisometropia increased, stereoacuity decreased. Stereoacuity was found to be the poorest in myopia, followed by myopia with astigmatism, hypermetropia with astigmatism, and hypermetropia. In the present study, as the amount of difference in spherical equivalent (severe degree of anisometropia) was found to be more in myopes than hypermetropes, stereoacuity was worse in myopes as compared to hypermetropes.
Similarly, Nabie et al.[13] conducted a study on 60 adult participants and observed that any type of anisometropia (myopia, hypermetropia, or astigmatism) may reduce stereoacuity; which was most noticeable with myopic anisometropia. They also evaluated the effect of experimental anisometropia on stereopsis by using the Titmus, Randot, and TNO stereoacuity tests and further reported most noticeable reduced stereoacuity in the TNO test, probably due to lack of monocular cues.
Levi et al.[14] determined quantitative relationships between the degree of anisometropia and the loss of visual function in 84 anisometropic patients and observed that most of the low myopic anisometropes with reduced acuity had astigmatism. This group of astigmatic myopes contributed to the high prevalence of reduced acuities and low tolerance for defocus seen in the group of amblyopes with low myopic spherical equivalent refractive errors.
Weakley[15] conducted a study on 361 patients with anisometropia and 50 non-anisometropic controls and observed that myopic anisometropia (>2 D) and hypermetropic anisometropia (>1 D) lead to a significant increase in amblyopia and decrease in binocular function when compared with non-anisometropic controls. The patients included in Weakley’s study were much younger (aged 3–14.5 years) than our patients (aged 5–45 years). Because of the process of emmetropization, we might expect our older population to be more myopic than Weakley’s study population and possibly more myopic than they were when amblyopia developed. The present study was a hospital-based study conducted during the COVID-19 pandemic. Our tertiary care hospital was converted to a COVID-19 center, and when OPD resumed, all the eligible patients in the 5–45 years age group were included in the study. We excluded patients younger than 5 years because these children were non-cooperative for the examination and in patients older than 45 years, refractive changes can be contributed by cataractous changes and other disease conditions such as diabetic macular edema.
We also observed that among isometropes, stereoacuity was reduced in hypermetropia with astigmatism, whereas it was within normal limits in the rest of the subgroups. This could be due to the presence of more amblyopic patients in the hypermetropia with astigmatism group.
Habiba and Hussain[16] conducted a cross-sectional study on 31 patients to determine the effect on stereopsis in different degrees of myopic and hyperopic anisometropic correction and compared stereopsis between anisometropes and isometropes. Stereopsis was analyzed by Lang1, Lang2, and Frisby. They observed that stereopsis in isometropes was found to be better than anisometropes. Furthermore, they reported that stereopsis decreased with increasing degree of anisometropia, which was more critically impaired if the interocular difference increased to >6.0 D. Similarly, in the present study, it was observed that most patients with anisometropia of <3.0 D had fair stereoacuity. However, as the degree of anisometropia increased to >3.0 D, stereoacuity deteriorated gradually. Marked reduction of stereoacuity was observed in the severe degree of anisometropia (>6.0 D).
It has been suggested that worse visual acuity correlates with worse stereoacuity. Furthermore, this relationship is largely attributable to anisometropic patients.[17] In our study, among the anisometropes, stereoacuity was found to be the worst in patients having unequal vision of more than two lines difference (amblyopes), followed by patients having unequal vision of less than two lines difference and patients having equal vision. This difference in stereoacuity was found to be statistically significant.
Yang et al.[18] conducted a study on 166 school children (aged 6–18 years) to determine the correlation between stereoacuity and the severity of myopia, astigmatism, and anisometropia. Stereoacuity was analyzed by the Titmus stereo test. They found that stereoacuity was reduced in anisometropia of >1.00 D. They also observed that myopia in children was not certainly associated with reduction in stereoacuity; this may be because the performance of stereoacuity in their study was measured without spectacle correction. In the present study, stereoacuity was measured with full spectacle correction, and a significant (P < 0.001) reduction in stereoacuity was found in anisometropes as compared to isometropes and emmetropes. These findings are similar to a study conducted by Habiba and Hussain,[16] in which reduced stereoacuity was observed in anisometropes as compared to isometropes.
Similarly, Levi et al.[14] conducted a study on 84 persons with pure anisometropia (no ocular deviation, no non-centric fixation, no deprivation, and no surgical history) and compared their results with those of 27 persons with high bilateral refractive error (isoametropia) and 101 persons with both strabismus and anisometropia. They reported that in pure anisometropes, increasing interocular difference causes reduction in stereoacuity.
We observed that the level of stereoacuity was worse in anisometropes as compared to isometropes and emmetropes. The reduction in stereoacuity was greater in amblyopic patients as compared to non-amblyopic patients. As the degree of anisometropia increased, stereoacuity decreased. Among the anisometropes, myopes had worse stereoacuity than hypermetropes.
There were some limitations in our study. This was a hospital-based study rather than a large-scale community-based study. The latter would have validated these findings in the community. Moreover, the usefulness of the Titmus stereo test for clinical testing may be influenced by the possession of monocular clues in low-grade stereograms.
Conclusion
The level of stereoacuity was worse in anisometropes as compared to isometropes and emmetropes. Amblyopes had a greater reduction in stereoacuity than non-amblyopes. Stereoacuity decreased as the degree of anisometropia increased. Among the anisometropes, myopes had worst stereoacuity than hypermetropes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Von Noorden GK, Campos EC. St Louis, Mosby. Binocular Vision and Ocular Motility, Theory and Management of Strabismus. (6th ed) 2002:21–25. [Google Scholar]
- 2.Hoyt CS, Taylor D. Pediatric Ophthalmology and Strabismus, Expert Consult-Online and Print, 4:Pediatric Ophthalmology and Strabismus. Elsevier Health Sciences. 2012 [Google Scholar]
- 3.Andalib D, Nabie R, Poormohammad B. Factors affecting improvement of stereopsis following successful surgical correction of childhood strabismus in adults. Strabismus. 2015;23:80–4. doi: 10.3109/09273972.2015.1025985. [DOI] [PubMed] [Google Scholar]
- 4.Barry, S.R. Beyond the critical period:Acquiring stereopsis in adulthood. Plasticity in sensory systems. 2012:175–95. [Google Scholar]
- 5.Blanchard J, Tsuneto R. Stereoscopic viewing. Encyclopedia of Virtual Environments. 2004 [Google Scholar]
- 6.O'Donoghue L, McClelland JF, Logan NS, Rudnicka AR, Owen CG, Saunders KJ. Profile of anisometropia and aniso-astigmatism in children:Prevalence and association with age, ocular biometric measures, and refractive status. Invest Ophthalmol Vis Sci. 2013;54:602–8. doi: 10.1167/iovs.12-11066. [DOI] [PubMed] [Google Scholar]
- 7.Huynh SC, Wang XY, Ip J, Robaei D, Kifley A, Rose KA, et al. Prevalence and associations of anisometropia and aniso-astigmatism in a population based sample of 6 year old children. Br J Ophthalmol. 2006;90:597–601. doi: 10.1136/bjo.2005.083154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vincent SJ, Collins MJ, Read SA, Carney LG. Myopic anisometropia:Ocular characteristics and aetiological considerations. Clin Exp Optom. 2014;97:291–307. doi: 10.1111/cxo.12171. [DOI] [PubMed] [Google Scholar]
- 9.Fawcett SL, Birch EE. Validity of the Titmus and Randot circles tasks in children with known binocular vision disorders. J AAPOS. 2003;7:333–8. doi: 10.1016/s1091-8531(03)00170-8. [DOI] [PubMed] [Google Scholar]
- 10.Ciuffreda KJ, Levi DM, Selenow A. Amblyopia:Basic and clinical aspects. Butterworth-Heinemann. 1991 [Google Scholar]
- 11.Gawęcki M. Threshold values of myopic anisometropia causing loss of stereopsis. J Ophthalmol. 2019;2019:2654170. doi: 10.1155/2019/2654170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeon HS, Choi DG. Stereopsis and fusion in anisometropia according to the presence of amblyopia. Graefes Arch Clin Exp Ophthalmol. 2017;255:2487–92. doi: 10.1007/s00417-017-3798-3. [DOI] [PubMed] [Google Scholar]
- 13.Nabie R, Andalib D, Khojasteh H, Aslanzadeh SA. Comparison of the effect of different types of experimental anisometropia on stereopsis measured with titmus, randot and TNO stereotests. J Ophthalmic Vis Res. 2019;14:48–51. doi: 10.4103/jovr.jovr_189_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levi DM, McKee SP, Movshon JA. Visual deficits in anisometropia. Vis Res. 2011;51:48–57. doi: 10.1016/j.visres.2010.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weakley DR., Jr The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001;108:163–71. doi: 10.1016/s0161-6420(00)00425-5. [DOI] [PubMed] [Google Scholar]
- 16.Habiba UE, Hussain Z. Comparison of stereopsis and contrast sensitivity in myopic and hyperopic anisometropia. Ophthalmol Pak. 2017;7:17–21. [Google Scholar]
- 17.Levi DM, Knill DC, Bavelier D. Stereopsis and amblyopia:A mini-review. Vis Res. 2015;114:17–30. doi: 10.1016/j.visres.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang JW, Huang TY, Lee JS, Yeung L, Lin YF, Sun CC. Correlation between myopic ametropia and stereoacuity in school-aged children in Taiwan. Jpn J Ophthalmol. 2013;57:316–9. doi: 10.1007/s10384-013-0231-2. [DOI] [PubMed] [Google Scholar]


