Abstract
Here, we report for the first time a series of compounds potentially useful for the management of oxaliplatin-induced neuropathy (OINP) able to modulate the human Carbonic Anhydrases (hCAs) as well as the Transient Receptor Potential Vanilloid 1 (TRPV1). All compounds showed effective in vitro inhibition activity toward the main hCAs involved in such a pathology, whereas selected items reported moderate agonism of TRPV1. X-ray crystallographic experiments assessed the binding modes of the two enantiomers (R)-37a and (S)-37b within the hCA II cleft. Although the tails assumed diverse orientations, no appreciable effects were observed for their hCA II affinity. Similarly, the activity of (R)-39a and (S)-39b on TRPV1 was not influenced by the stereocenters. In vivo evaluation of the most promising derivatives (R)-12a, (R)-37a, and the two enantiomers (R)-39a, (S)-39b revealed antihypersensitivity effects in a mouse model of OINP with potent and persistent effect up to 75 min after administration.
Introduction
Cancer is a major health threat worldwide and is estimated that more than half a million deaths in the United States alone by 2021 are directly correlated to such a disease.1 Nevertheless, cancer survival has improved over the last 50 years thanks to new therapeutic breakthroughs although frequent adverse effects remain.2 The platinum-based chemotherapy (i.e., cisplatin, carboplatin, and oxaliplatin) has acquired and still retains significant importance since it is widely used within the oncological field for the management of advanced metastatic cancers (i.e., colorectal, ovarian, breast, and lung as the major examples).3 However, several side effects are associated with platinum drugs, and among others, dose-limiting toxicity, nephrotoxicity, ototoxicity, myelosuppression, and neurotoxicity are those of major concern as often result in discontinuation of the therapy.4,5 For instance, peripheral neurotoxicity affects almost all patients with acute symptoms (i.e., paresthesia/dysesthesias) which over time turn into chronic sensory neurotoxicity. In addition, chronic painful pathologies are highly debilitating and heavily affect life quality.6 To date, there are no effective options for the management of oxaliplatin-induced neuropathic pain (OINP), being only the nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids able to act slightly as pain relievers although associated with important side effects.7,8 Although the pathophysiology of OINP is not fully understood, several reports agree that homeostasis dysfunctions of dorsal root ganglion (DRG) neurons take place.9−12 Such a hypothesis is consistent with the location of DRGs outside the central nervous system (CNS) and thus not protected by the blood–brain barrier.13 An important piece of evidence is that patients treated with oxaliplatin showed an interference with some members of the Transient Receptor Potential (TRP) channel family (such as TRPM8, TRPV1, and TRPA1) through the chelation of calcium ions by oxaliplatin metabolites (i.e., oxalate). In this context, we turned our attention to TRPV1 as it recently assumed importance as a potential analgesic target since it is involved in the transmission of nociceptive stimuli by triggering an important cellular influx of Ca2+ ions.14,15
Desensitization of the TRPV1 receptor through its activation16,17 represents a promising strategy for pain management. Early attempts to manipulate TRPV1 receptor did make use of agonists such as capsaicin (Figure 1A)18 or resiniferatoxin (Figure 1). The latter is better considered as “molecular scalpel” since it was reported to cause prolonged TRPV1 channel opening with cytotoxicity effects evident only to sensory neurons expressing it.19 TRPV1 partial agonists were also effective in inducing pain relief.20
Figure 1.
Structures of agonists (A) and antagonists (B) of TRPV1 receptor.
An alternative approach to modulate pain relief includes compounds endowed with TRPV1 antagonist features such as capsazepine or SB-705498 in Figure 1B. In this case, the pain reversal effects were strongly associated with risks of hyperthermia and accidental burns and that did make such a route unfeasible for further development.21 OINPs usually are associated with uncontrolled intracellular acidification of DRG neurons as a result of the formation of metal (i.e., platinum) adducts with hemoglobin.12 The same study reported that uncontrolled pH fluctuations by subtraction of the main pH buffering system may be reverted by inhibition of the Carbonic Anhydrase (CA, EC 4.2.1.1) isoforms therein present (i.e., hCA II).12 Based on the seminal study from Potenzieri et al., we sought to intervene in OINP pH imbalances by making use of compounds able to inhibit the metalloenzymes CAs and activate TRPV1 receptors.12,22−25 Besides the evident pH implications, inhibition of the highly abundant CNS-expressed CAs (i.e., II, VII, and XII) may be expected to induce a reduction of the bicarbonate-dependent depolarization of GABAA receptors when KCC2 is compromised in peripheral nerve injuries.26,27 Our interests in this field were also fostered by seminal contributions from some of us which demonstrated that CAs inhibitors (CAIs) synergistically enhanced the antitumor activity of platinum-based drugs.28,29
Results and Discussion
Design and Synthesis
We sought to make use of the potent CNS-penetrant and selective TRPV1 antagonism of SB-705498 with the aim to introduce within its chemical scaffold minimal functional groups necessary to endow the final products with activity against the hCAs of interest (Figure 2).30
Figure 2.
Design of TRPV1-CA derivatives reported in this study.
Our synthetic strategy accounted for: (i) replacement of CF3 moiety on SB-705498 with the prototypic pharmacophore for CA inhibition such as the primary sulfonamide; moreover, different substituents on phenyl ring were employed to discover the best interactions in both targets; (ii) replacement of the bromine atom within SB-705498 with the same group either in meta or para position and, in addition, other groups instead CF3 moiety was investigated (i.e., NO2 and H) (Figure 2). Finally, we investigated whether the stereocenter could affect the binding affinity against the different CA isoforms and TRPV1 receptor.
The first synthetic route was accomplished by preparing the intermediate 2 in a single-step procedure which involved the nucleophilic reaction between the commercially available sulfonyl chloride 1 and ammonia in tetrahydrofuran (THF) at 0 °C. The chloro pyrimidine derivative 2 was reacted with enantiopure-protected pyrrolidines (R)-3a and (S)-3b in N,N-dimethylformamide (DMF) at 100 °C with K2CO3 to afford 4a and 4b. Boc-deprotection by hydrolysis afforded 5a-b, which were subjected to coupling reactions with available isocyanates and isothiocyanates 6a-p to provide the sulfonamide containing urea and thiourea derivatives 7–22 (Scheme 1).
Scheme 1. General Synthesis of Derivatives 7–22.

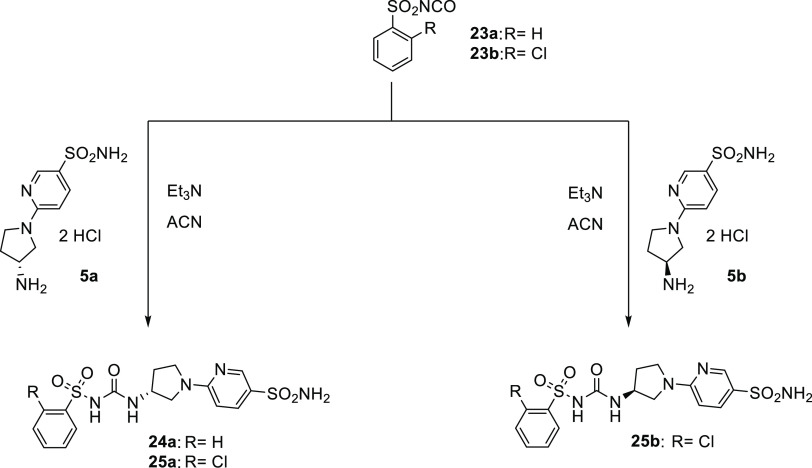
Moreover, we employed two aromatic sulfonyl isocyanates (23a-b) to obtain compounds 24 and 25 bearing the sulfonylureido moiety (Scheme 2).
Scheme 2. General Synthesis of Derivatives 24–25.
As for the second synthetic route, the chloropyridine 26a-c are reacted with the enantiopure pyrrolidines 3a-b using the same conditions previously reported for 4a-b. Subsequently, standard Boc-deprotection was carried out with trifluoroacetic acid (TFA) followed by treatment with a 1 N aqueous solution of NaOH to obtain free amines 30–32. Two different synthetic pathways were pursued for the synthesis of 35–46 (Scheme 3).
Scheme 3. General Synthesis of Derivatives 41–46.

As reported above, first we used two different sulfonamide isothiocyanates (33a-b) to give the thioureido derivatives 35–40. On the other hand, the ureido ones (i.e., 41–46) were obtained by means of carbamates 34a-b (Scheme 3).
Carbonic Anhydrase Inhibition
The inhibition profiles of all product synthesized (7a,b–22a,b, 24a, 25a-b, 35a–46a, 37b–40b, 43b–46b) against the physiologically relevant hCAs I, II, IV, VII, IX, and XII isoforms were investigated by the stopped-flow CO2 hydrase assay and compared to the reference CAI acetazolamide (AAZ)31 (Table 1).
Table 1. Inhibition Data of hCA Isoforms I, II, IV, VII, IX, and XII with Compounds 7a,b–22a,b, 24a, 25a,b, 35–46a, 37b–40b, 43b–46b, and AAZ by a Stopped-Flow CO2 Hydrase Assay.
|
KI (nM)a | ||||||
|---|---|---|---|---|---|---|
| cmp | hCA I | hCAII | hCAIV | hCAVII | hCAIX | hCAXII |
| 7a | 27.4 | 15.1 | 2656 | 6.6 | 32.2 | 59.3 |
| 7b | 260.4 | 187.3 | 8242 | 12.1 | 20.2 | 50.3 |
| 8a | 68.8 | 12.1 | 3115 | 8.6 | 30.8 | 39.5 |
| 8b | 94.5 | 55.6 | 2695 | 2.6 | 27.3 | 35.4 |
| 9a | 164.0 | 45.9 | 3732 | 8.5 | 25.5 | 59.3 |
| 9b | 321.1 | 178.9 | 9478 | 11.6 | 54.1 | 23.4 |
| 10a | 788.1 | 453.4 | 4019 | 78.6 | 737.0 | 67.6 |
| 10b | 707.3 | 478.3 | 8516 | 15.6 | 77.5 | 7.6 |
| 11a | 37.0 | 23.3 | 2516 | 187.3 | 280.9 | 73.0 |
| 11b | 475.8 | 137.5 | 4458 | 11.6 | 20.1 | 43.9 |
| 12a | 82.5 | 70.3 | 3002 | 73.5 | 316.2 | 83.6 |
| 12b | 393.0 | 95.2 | 2031 | 0.9 | 22.9 | 41.7 |
| 13a | 937.6 | 818.0 | 3079 | 76.9 | 245.0 | 406.6 |
| 13b | 871.4 | 725.5 | 5354 | 52.0 | 89.8 | 89.9 |
| 14a | 547.0 | 82.2 | 4903 | 26.5 | 1798 | 7.2 |
| 14b | 959.0 | 555.6 | 2528 | 12.1 | 74.4 | 44.6 |
| 15a | 72.2 | 50.2 | 3560 | 9.4 | 192.4 | 6.7 |
| 15b | 544.8 | 400.3 | 5725 | 29.5 | 82.0 | 62.9 |
| 16a | 903.3 | 714.9 | 5161 | 40.8 | 1438 | 37.9 |
| 16b | 625.3 | 432.3 | 2495 | 8.3 | 54.9 | 9.4 |
| 17a | 80.6 | 42.2 | 848.6 | 7.8 | 32.0 | 3.9 |
| 17b | 91.5 | 42.9 | 5217 | 14.9 | 8.6 | 27.8 |
| 18a | 73.5 | 287.4 | 5077 | 68.7 | 36.1 | 72.2 |
| 18b | 476.0 | 309.6 | 7857 | 58.8 | 61.8 | 38.5 |
| 19a | 252.3 | 436.8 | 1525 | 56.1 | 145.0 | 57.4 |
| 19b | 800.4 | 525.0 | 5716 | 8.2 | 67.5 | 8.5 |
| 20a | 154.2 | 409.2 | 4817 | 27.9 | 379.3 | 44.2 |
| 20b | 72.4 | 35.3 | 2686 | 8.6 | 5.5 | 48.7 |
| 21a | 31.3 | 14.9 | 3087 | 50.7 | 378.2 | 8.3 |
| 21b | 68.7 | 31.3 | 843.4 | 2.6 | 7.2 | 41.0 |
| 22a | 93.8 | 446.1 | 4883 | 41.1 | 35.8 | 8.1 |
| 22b | 584.3 | 481.9 | 8195 | 14.0 | 48.3 | 8.2 |
| 24a | 19.5 | 513.0 | 36.6 | 78.8 | 27.5 | 49.3 |
| 25a | 72.3 | 15.4 | 704.5 | 30.1 | 9.2 | 279.7 |
| 25b | 89.2 | 38.5 | 911.4 | 46.4 | 9.7 | 308.6 |
| 35a | 48.0 | 6.9 | 774.5 | 9.7 | 9.6 | 9.0 |
| 36a | 85.1 | 9.6 | 320.4 | 55.4 | 310.8 | 78.2 |
| 37a | 74.8 | 6.7 | 471.3 | 174.7 | 16.8 | 408.6 |
| 37b | 54.5 | 4.9 | 3203 | 7.7 | 1.3 | 8.8 |
| 38a | 78.5 | 8.6 | 238.0 | 83.6 | 162.0 | 237.7 |
| 38b | 8.7 | 3.9 | 1295 | 15.6 | 1.4 | 9.3 |
| 39a | 90.8 | 18.9 | 4969 | 73.3 | 355.0 | 62.5 |
| 39b | 93.2 | 11.5 | 9722 | 15.7 | 6.0 | 9.4 |
| 40a | 490.3 | 20.4 | 805.9 | 55.1 | 36.4 | 29.4 |
| 40b | 412.7 | 95.4 | 668.7 | 14.2 | 7.9 | 9.6 |
| 41a | 58.3 | 8.0 | 3511 | 9.5 | 29.1 | 31.6 |
| 42a | 9.6 | 1.7 | 2476 | 8.1 | 125.5 | 8.2 |
| 43a | 68.3 | 7.5 | 2293 | 163.6 | 93.6 | 83.7 |
| 43b | 76.2 | 14.9 | 8226 | 8.7 | 26.9 | 9.1 |
| 44a | 76.0 | 6.1 | 2101 | 74.8 | 971.3 | 37.9 |
| 44b | 87.2 | 6.6 | 9551 | 17.7 | 192.7 | 48.4 |
| 45a | 72.4 | 27.4 | 3900 | 8.2 | 36.7 | 6.3 |
| 45b | 68.6 | 46.3 | 9711 | 12.8 | 54.0 | 8.6 |
| 46a | 198.6 | 8.4 | 4023 | 6.9 | 247.0 | 6.6 |
| 46b | 305.5 | 8.9 | 8770 | 13.4 | 44.0 | 8.9 |
| AAZ | 250.0 | 12.1 | 74.0 | 2.5 | 25.7 | 5.7 |
Mean from three different assays, by a stopped-flow technique (errors were in the range of ±5–10% of the reported values).
Taking into account the reported data, the structure–activity relationship (SAR) based on specific isoforms is drawn below:
-
The cytosolic hCA II is inhibited by derivatives 7–22a,b with Ki’s spanning from low nanomolar range (12.1 nM 8a) up to high nanomolar values (i.e., Ki of 818 nM 13a). The affinities for hCA I are similar, thus falling within comparable inhibition ranges. Also in this case, 13a was the least effective (Ki of 937.6 nM for the hCA I). From the general point of view, the same kinetic trend for isoforms I and II were observed. Of note, all of the (R) enantiomers (i.e., 7–22a, 24a, 25a, and 35–46a) were more effective inhibitors compared to the (S) series comprising 7–22b, 25b, 37–40b, and 43–46b. Among them, compound 7a was almost 10-fold more potent than its (S) enantiomer 7b on both hCA isoforms. The derivative 11a (Ki 37.0 nM) became 13-fold more active than 11b (Ki 475.8 nM) against hCA I.
As in the case of compounds 10a-b, 16a-b, and 20a-b, an opposite inhibition trend for the two enantiomers was observed, being the (S)-10b, (S)-16b, and (S)-20b far more effective hCA I, II inhibitors compared to the (R) counterparts (i.e., (R)-10b, (R)-16b, and (R)-20b). It is reasonable to speculate that such a reversal activity between (R) and (S) may be attributed to the CF3 group.32 On the other hand, the introduction of a bulky scaffold such as in compounds 13a-b and 17a-b flattened any discrimination between the enantiomeric series. As for the hCA II, the compound series bearing the sulfonamide moiety on the phenyl ring (35–46), it is interesting to note that the position of the sulfonamide in para or meta for thioureido derivatives 37–40a-b induced an increase in the potency of the (R) enantiomers, as in the case of 40a. On the other hand, ureido derivatives showed the same trend when the sulfonamide moiety was placed in para position (i.e., 43a and 45a).
The membrane isoform hCA IV was inhibited by almost all derivatives with KI values in the micromolar range (Table 1). Of note, the replacement of the ureido moiety with sulfonylureido resulted in a drastic increase of the potency up to medium nanomolar values as for compound 24a (Ki 36.6 nM). The addition of one chlorine atom in ortho of sulfonylureido moiety (derivative 25a-b) decreased the potency about 20-fold.
The brain-associated isoform hCA VII was strongly inhibited by almost all of the series reported with KI inhibition values in the sub-nanomolar range (i.e., 12bKi 0.9 nM). For this isoform, we observed a different inhibition trend compared to hCA I and II, as most (S) enantiomers became far more effective compared to the (R) ones. An interesting feature was represented by the simple replacement of the ureido moiety with the thioureido instead (i.e., 7a-b and 8a-b). In this case, an inversion of activity for the corresponding enantiomers was observed. Indeed, the ureido derivative 7a (Ki 6.6 nM) showed 2-fold higher potency compared to the (S) enantiomer (7b, Ki 12.1 nM). In contrast, the thioureido derivative 8b (Ki 2.6 nM) showed 3 times higher selectivity than the (R) enantiomer (8a, Ki 8.6 nM). A halogen atom in ortho position would appear to be essential for selectivity toward the (S) enantiomer, as shown by derivatives 11a-b and 21a-b with over 10-fold and 80-fold more selective than compounds 12a-b. From the general point of view, the position of the sulfonamide group in 37–46 seems also to play an important role in the enantiomeric-dependent selectivity. For instance, within the meta regioisomeric series, the selectivity for (R) enantiomer over (S) increased.
The tumor-associate isoforms hCA IX and hCA XII were effectively inhibited by all compounds herein reported and showed KI values comprised between 1.3 and 971.3 nM (Table 1). In addition, a pivotal role for the enantiomeric-dependent selectivity for such isoforms was represented by the substituents placed on the phenyl rather than the pyridine ring. We observed for derivatives 9, 14, 15, 17, 18, and 21 an inverted selectivity between the hCA IX and XII (Table 1). An interesting case for the hCA IX was observed among compounds 11a-b and 21a-b as replacement of the ureido group in the former with the thioureido in the latter resulting in increased (S) selectivity (11b was 13.9-fold more active than 11a; 21b was 52.5-fold more active than 21a). On the other hand, for hCA XII, the inhibition selectivity shifted toward the enantiomer (R) such as for derivative 21a-b. Compounds 37–46 observed the (S) enantiomers as the best inhibitors against both isoforms, especially for derivatives 38a-b showing a selectivity of over 100-fold for the enantiomer (S) 38b.
TRPV1 Assay
The ability of the selected (R) enantiomers 7a, 9a–16a, 18a–22a, 24a, 35a–46a, and the (S) counterparts 39b and 45b to modulate TRPV1 receptor activity was assessed, and the data are reported in Table 2.
Table 2. EC50 Values for 7a, 9a–16a, 18a–22a, 24a, 35a–46a, and 39b on TRPV1 Receptor Activity.
| cmp | EC50 (μM) | SD |
|---|---|---|
| 7a | >100 | |
| 9a | >100 | |
| 10a | 74.5 | 2.3 |
| 11a | >100 | |
| 12a | 11.9 | 1.6 |
| 13a | >100 | |
| 14a | >100 | |
| 15a | >100 | |
| 16a | >100 | |
| 18a | >100 | |
| 19a | >100 | |
| 20a | >100 | |
| 21a | >100 | |
| 22a | >100 | |
| 24a | >100 | |
| 35a | >100 | |
| 36a | >100 | |
| 37a | 8.0 | 1.7 |
| 38a | 44.2 | 1.1 |
| 39a | 12.4 | 1.4 |
| 39b | 12.5 | 1.8 |
| 40a | 21.9 | 1.0 |
| 41a | >100 | |
| 42a | >100 | |
| 43a | >100 | |
| 44a | >100 | |
| 45a | 29.5 | 0.3 |
| 45b | 3.1 | 1.6 |
| 46a | 37.3 | 2.5 |
Although the compounds reported in this study were all derived from the TRPV1 antagonist SB-705498, the data obtained accounted for a clear agonism effect (Table 2). This is not surprising as it is well known that even small chemical modifications might lead to an agonism–antagonism switch in the modulation of TRPV1 activity.
For instance, 10a, 37a, 38a, 39a-b, 40a, 45a-b, and 46a showed moderate agonism effects with EC50 values spanning between 3.1 and 74.5 μM (Table 2). In more detail, the sulfonamide group placed into the pyridine ring became deleterious as most of such derivatives were ineffective. A slight activity (i.e., EC50 of 74.5 μM) was detected for 10a, which was remarkably restored when the chlorine atom at position 2 was introduced (EC50 of 11.9 μM) as in compound 12a. Conversely, most of the products bearing the sulfonamide moiety onto the phenyl ring showed activity with associated EC50 values in the low micromolar range such as 37a and 45b with 8.0 and 3.1 μM, respectively. Quite interestingly, the configuration of the stereocenter in some cases did not influence either the activity or the potency as clearly shown by the enantiomers 39a and 39b, which reported equal EC50 value of 12.5 μM. Isomeric-dependent discrimination in terms of potency was reported for (R)-45a and (S)-45b being the latter 9-fold more active than its counterpart 45a.
X-ray Crystal Structures
To clarify the molecular basis of CA inhibition by our derivatives, we determined the X-ray structures of hCA II in complex with the enantiomers (R)-37a and (S)-37b at 1.3 and 1.6 Å resolution, respectively (Figure 3).
Figure 3.
(A) X-ray crystal structures of hCA II bound with compound (R)-37a (green, PDB: 8BJX). (B) X-ray crystal structures of hCA II bound with compound (S)-37b (magenta, PDB: 8BOE). (C) Overlay of compounds (R)-37a and (S)-37b with hCA II. Residues involved in the binding of inhibitors are also shown; the gray sphere represents the zinc ion in the active site of the proteins.
Analysis of the electron density maps (Figure S1 in the Supporting Information (SI)) showed for the inhibitor (R)-37a a density, into the catalytic cleft, fully compatible with our ligand. As expected, the sulfonamide moiety interacted directly with the zinc ion and a hydrogen bond with the residue of Thr199, thus showing the typical binding mode of this class of inhibitors.33 Furthermore, typical hydrophobic interactions between the benzenesulfonamide moiety and side chains of Val121 and Leu198 were established and contributed to strengthen the complex within the active site. The proximal nitrogen atom of (R)-37a thioureido moiety was engaged in a water bridge with Thr200. Valuable additional hydrophobic interactions were observed between Leu198 and Pro202 and the hydrophobic sections of the main scaffold which were responsible for sticking the entire ligand within the hydrophobic region of the active site (Figure 3A).
Interesting structural features were also revealed for the second inhibitor (S)-37b bound within the hCA II (Figure 3B). First, the thioureido moiety was observed in double conformation. Moreover, interesting features were also observed for the tail of derivative (S)-37b. Indeed, the (S) stereocenter of pyrrolidine ring moved this moiety on the other side of Phe131 engaging a hydrophobic interaction with this residue. This different location of the tail of (S)-37b is also stabilized by a water bridge between the nitrogen of pyridine ring with Glu69 and the hydrophobic interaction with Ile91. The structural comparison (Figure 3C) among the two enantiomers (R)-37a and (S)-37b revealed also similar features, such as the typical benzenesulfonamide interactions with the catalytic zinc atom and Thr199; on the other hand, the stereocenter is able to influence the tail conformations of the two molecules which occupy two different hydrophobic pockets divided by Phe131 residue. Nevertheless, this structural diversity does not significantly affect the grade of inhibition of the two inhibitors for this isoform.
In Vivo Pain-Relieving Effect
Based on in vitro obtained CA and TRPV1 profiles, we selected the most appropriate compounds to subject to an in vivo mouse model of neuropathic pain induced by oxaliplatin repeated treatment.34,35 For instance, we considered derivatives: (i) (R)-36a and (R)-43a as potent CAs inhibitors devoid of TRPV1 activity; (ii) (R)-12a and (R)-37a, which are effective on both targets; and (iii) the two enantiomers (R)-39a and (S)-39b, which showed close effectiveness on CA II and TRPV1. The results are highlighted in Figure 4.
Figure 4.
Pain-relieving effect of acute administration of derivatives 12a, 36a, 37a, 39a, 39b, and 43a in a mouse model of oxaliplatin-induced neuropathic pain. Sensitivity to a non-noxious thermal stimulus was assessed by the Cold plate test. Oxaliplatin (2.4 mg/kg, i.p.) was injected on days 1–2, 5–9, and 12–14 (10 injections). On day 15, compounds were acutely per os administered in a range dose of 10–100 mg/kg. Assessment of cold allodynia was performed before and 15, 30, 45, 60, and 75 min after treatments. Results are expressed as the mean ± standard error of the mean (S.E.M.) of 10 mice analyzed in two different experimental sets. **P < 0.01 vs vehicle + vehicle; ∧P < 0.05 and ∧∧P < 0.01 vs oxaliplatin + vehicle-treated animals. Each value represents the mean ± S.E.M. of 10 mice performed in two different experimental sets.
In our experimental conditions, we evaluated the animal licking latency after oral administration of the selected compounds at increasing concentrations up to 100 mg/kg. Overall, we observed dose-dependent correlations with various outcomes as below reported:
-
(1)
Compounds (R)-36a and (R)-43a devoid of any activity on TRPV1 showed a dose-dependent effectiveness peaking at 45 min post-administration, followed by a rapid decrease of the effect which was suppressed at 75 min (Figure 4).
-
(2)
(R)-12a and (R)-37a peaked at 30 min post-administration, and were effective up to 45 min. (R)-37a was more potent and effective than (R)-12a (Figure 4). Such an effect may be reasonably attributed to the major efficacy of (R)-37a in inhibiting the CA II over (R)-12a (i.e., 10.4-fold) also in consideration DRG neurons are particularly rich in such an isoform.12
-
(3)
Quite interestingly (R)-39a and (S)-39b were significantly effective at 30 and 100 mg/kg, completely reverting oxaliplatin hypersensitive at the higher dose. Since the in vitro activity on CA II and TRPV1 were close matching (Tables 1 and 2), the slightly better profile of (S)-39a may be ascribed to differentiated metabolic processes which take place on each enantiomer after oral administration (Figure 4).
Conclusions
To the best of our knowledge, this is the first report on dual-targeting molecules able to relieve OINPs by simultaneous activation of TRPV1 and inhibition of CA enzymes. Preliminary SARs were performed by in vitro evaluation of the effects on both targets when substitutions of aromatic rings, bio-isosteric switch between ureido and thioureido linkers, as well as the introduction of stereocenters were operated. Overall, (R)- or (S)-stereocenters present within the set of compounds synthesized did not seem to have relevant effects on the activity of both targets. Particularly striking was the case of (R)-37a and (S)-37b (i.e., CA II KI’s of 6.7 and 4.9 nM, respectively) as the X-ray structures of their adducts with CA II showed the molecular tails lying onto the enzymatic hydrophobic section of the active site and occupying distinct subpockets split apart by the Phe131 residue.
Our approach to introduce the CA warhead sulfonamide moiety into the TRPV1 antagonist modulator SB-705498 resulted in the reversal of activity up to moderate agonism. The observed in vitro effects of molecular stereocenters on TRPV1 were various. For instance, (R)-39a and (S)-39b (i.e., EC50 of 12.5 μM for both compounds) did not induce any potency change, whereas for the derivatives 45, the (S)-enantiomer was 9-fold more effective than its corresponding (R)-counterpart (i.e., ECs50 of 29.5 and 3.1 μM for (R)-45 and (S)-45, respectively).
A selection among the most valuable in vitro performing compounds (i.e., (R)-12a, (R)-36a, (R)-37a, (R)-39a, (S)-39b, and (R)-43a) allowed us to explore their effects on an in vivo mouse model of OINP. All derivatives endowed with activity either on CA II or TRPV1 induced long-lasting pain-relieving effects with maximum efficacy at 30 min after administration. Conversely, compounds (R)-36a and (R)-43a endowed only with activity against the CAs reported moderate and shorter relieving outcomes, thus demonstrating the important contribution to the biological model ascribed to the TRPV1 agonist section of the molecules reported. Quite interestingly, the enantiomers (R)-39a and (S)-39b became significantly dissimilar in inducing a biochemical response in our in vivo model, with the former being far more effective and lasting compared to its (S)-counterpart.
Although this study is not exhaustive in defining the kinetic as well as biochemical features of the entire set of molecules reported to manage OINPs, it gives solid pieces of evidence that small-size molecules acting simultaneously as mild TRPV1 agonists and potent inhibitors of the CAs represent a valid and worth developing strategy useful to minimize OINP-induced symptoms such as pain.
Experimental Section
General
Anhydrous solvents and all reagents were purchased from Sigma-Aldrich, VWR, and TCI. All reactions involving air- or moisture-sensitive compounds were performed under a nitrogen atmosphere. Nuclear magnetic resonance (1H NMR, 13C NMR, 19F NMR) spectra were recorded using a Bruker Advance III 400 MHz spectrometer in DMSO-d6. Chemical shifts are reported in parts per million (ppm), and the coupling constants (J) are expressed in Hertz (Hz). Splitting patterns are designated as follows: s, singlet; d, doublet; t, triplet; m, multiplet; brs, broad singlet; dd, double of doubles. The assignment of exchangeable protons (NH) was confirmed by the addition of D2O. Analytical thin-layer chromatography (TLC) was carried out on Merck silica gel F-254 plates. Flash chromatography purifications were performed on Merck silica gel 60 (230–400 mesh ASTM) as the stationary phase, and ethyl acetate, n-hexane, acetonitrile, and methanol were used as eluents. The solvents used in MS measurements were acetone, acetonitrile (Chromasolv grade), purchased from Sigma-Aldrich (Milan, Italy), and Milli-Q water 18 MΩ, obtained from Millipore’s Simplicity system (Milan, Italy). The mass spectra were obtained using a Varian 1200L triple quadrupole system (Palo Alto, CA) equipped with electrospray source (ESI) operating in both positive and negative ions. Stock solutions of analytes were prepared in acetone at 1.0 mg mL–1 and stored at 4 °C. Working solutions of each analyte were freshly prepared by diluting stock solutions in a mixture of Milli-Q H2O/ACN 1/1 (v/v) up to a concentration of 1.0 μg mL–1. The mass spectra of each analyte were acquired by introducing, via a syringe pump at 10/L min–1, the working solution. Raw data were collected and processed by Varian Workstation, version 6.8, software. All compounds reported here are >95% of purity by NMR.
Synthesis of 6-Chloropyridine-3-sulfonamide (2)
6-Chloropyridine-3-sulfonyl chloride 1 (1 g) was dissolved at 0 °C in THF and was added to ammonia solution (28%, 4 mL). The solution was stirred at 0 °C for 4 h, quenched with H2O, extracted with EtOAc, and dried over Na2SO4 to afford compound 2 as a white solid, yield 83%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.84 (1H, d, J = 2.21 Hz), 8.26 (1H, dd, J = 8.36, 2.25 Hz), 7.81 (1H, d, J = 8.39 Hz), 7.75 (2H, bs); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 153.9, 147.9, 140.6, 138.2, 125.8; MS (ESI positive) m/z: 192.9 [M + H]+.
General Synthesis of Compounds 4a-b
To a solution of 6-chloropyridine-3-sulfonamide (2, 1 equiv) and K2CO3 (1.3 equiv) in dry DMF under inert atmosphere (N2) was added the appropriate pyrrolidine (3a,b, 1 equiv). The mixture was stirred for 4 h at 100 °C. The reaction mixture was quenched with ice-cooled, saturated NH4Cl solution and stirred for 15 min to give a precipitate, which was collected by vacuum filtration and washed with water. The obtained solid was triturated with Et2O to yield the derivatives 4a,b.
tert-Butyl (R)-(1-(5-Sulfamoylpyridin-2-yl)pyrrolidin-3-yl)carbamate (4a)
Following the general procedure, the product was a white solid 4a, yield 80%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.46 (1H, d, J = 2.17 Hz), 7.83 (1H, dd, J = 8.93, 2.25 Hz), 7.26 (1H, d, J = 5.21 Hz), 7.17 (2H, bs), 6.57 (1H, d, J = 9.00 Hz), 4.15 (1H, m), 3.68 (1H, m), 3.66 (1H, m), 3.58 (1H, m), 3.32 (1H, m), 2.17 (1H, m), 1.94 (1H, m), 1.43 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.5, 156.2, 147.2, 135.6, 128.1, 106.6, 78.8, 53.1, 50.7, 45.8, 31.4, 29.1; MS (ESI positive) m/z: 343.1 [M + H]+.
tert-Butyl (S)-(1-(5-Sulfamoylpyridin-2-yl)pyrrolidin-3-yl)carbamate (4b)
Following the general procedure, the product was a white solid 4b, yield 82%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.45 (1H, d, J = 2.21 Hz), 7.82 (1H, d, J = 8.97, 2.46 Hz), 7.28 (1H, d, J = 6.04 Hz), 7.18 (2H, bs), 6.57 (1H, d, J = 9.01 Hz), 4.16 (1H, m), 3.70–3.67 (1H, m), 3.58 (1H, m), 3.48 (1H, m), 3.31 (1H, m), 2.18–2.15 (1H, m), 1.95–1.92 (1H, m), 1.43 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 156.2, 147.2, 135.5, 128.1, 106.6, 78.8, 53.1, 50.7, 45.8, 31.4, 29.1; MS (ESI positive) m/z: 343.1 [M + H]+.
General Synthesis of Compounds 5a-b
To a solution of 1 N HCl in EtOAc was added tert-butyl (1-(5-sulfamoylpyridin-2-yl)pyrrolidin-3-yl)carbamate 4a or 4b, and the mixture was stirred overnight at room temperature. Subsequently, the solvent was removed under vacuum to obtain the HCl salt of derivatives 5a,b.
(R)-6-(3-Aminopyrrolidin-1-yl)pyridine-3-sulfonamide (5a)
Following the general procedure, the product was a light yellow solid 5a, yield 99%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.49 (1H, d, J = 1.82 Hz), 8.28 (3H, bs), 7.88 (1H, dd, J = 8.93, 1.37 Hz), 7.23 (2H, bs), 6.65 (1H, d, J = 8.84 Hz), 4.00 (1H, m), 3.79–3.74 (1H, m), 3.66–3.57 (3H, m), 2.42–2.35 (2H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 147.3, 135.5, 127.9, 106.5, 55.3, 51.3, 46.0, 34.1; MS (ESI positive) m/z: 243.1 [M + H]+.
(S)-6-(3-Aminopyrrolidin-1-yl)pyridine-3-sulfonamide (5b)
Following the general procedure, the product was a light yellow solid 5b, yield 97%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.63 (3H, m), 8.42 (1H, d, J = 1.81 Hz), 8.03 (1H, dd, J = 9.08, 1.69 Hz), 7.49 (2H, bs), 6.92 (1H, d, J = 9.12 Hz), 4.02 (1H, m), 3.88–3.76 (3H, m), 3.67 (1H, m), 2.41–2.37 (1H, m), 2.29–2.25 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 154.2, 141.0, 138.2, 129.3, 111.8, 52.7, 50.3, 47.1, 29.8; MS (ESI positive) m/z: 243.1 [M + H]+.
General Synthesis of Compounds 7–22
Compound 5a/5b (1 equiv) in acetonitrile was added to isocyanate or isothiocyanate 6a-p (1 equiv) and Et3N (3 equiv). The solution was stirred overnight at room temperature. The reaction was quenched with saturated solution of NH4Cl, extracted with EtOAc, and dried over Na2SO4. The crude material was purified by flash column chromatography (MeOH/DCM: 5:95), to yield compounds 7–22.
(R)-6-(3-(3-(4-Fluorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (7a)
Following the general procedure, the product was a white solid 7a, yield 78%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, bs), 8.39 (1H, bs), 7.85 (1H, d, J = 8.95 Hz), 7.42 (2H, m), 7.18 (2H, bs), 7.11–7.07 (2H, m), 6.62 (1H, d, J = 8.66 Hz), 6.55 (1H, d, J = 6.50 Hz), 4.36 (1H, m), 3.74–3.70 (1H, m), 3.58 (2H, m), 3.41 (1H, m), 2.28–2.23 (1H, m), 2.00–1.96 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 157.9 (d, J = 237.52 Hz), 155.9, 147.2, 137.5, 135.6, 128.4, 120.2 (d, J = 7.15 Hz), 116.0 (d, J = 22.09 Hz), 106.7, 53.5, 50.0, 45.8, 31.9; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −122.4; MS (ESI positive) m/z: 380.1 [M + H]+.
(S)-6-(3-(3-(4-Fluorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (7b)
Following the general procedure, the product was a white solid 7b, yield 47%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, bs), 8.39 (1H, bs), 7.85 (1H, d, J = 8.56 Hz), 7.42 (2H, m), 7.18 (2H, bs), 7.09 (2H, t, J = 8.61 Hz), 6.62 (1H, d, J = 8.93 Hz), 6.55 (1H, d, J = 6.35 Hz), 4.36 (1H, m), 3.74–3.70 (1H, m), 3.58 (2H, m), 3.41 (1H, m), 2.28–2.23 (1H, m), 2.03–1.98 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 157.9 (d, J = 237.00 Hz), 155.9, 147.2, 137.5, 135.6, 128.4, 120.2 (d, J = 7.48 Hz), 116.0 (d, J = 22.11 Hz), 106.7, 53.5, 50.0, 45.8, 31.9; MS (ESI positive) m/z: 380.1 [M + H]+.
(R)-6-(3-(3-(4-Fluorophenyl)thioureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (8a)
Following the general procedure, the product was a white solid 8a, yield 56%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.45 (1H, bs), 8.49 (1H, d, J = 1.96 Hz), 8.14 (1H, bs); 7.85 (1H, dd, J = 8.97, 2.07 Hz), 7.48 (2H, dd, J = 8.69, 4.95 Hz), 7.17 (3H, m), 6.63 (1H, d, J = 8.93 Hz), 4.90 (1H, m), 3.84–3.80 (1H, m), 3.60–3.49 (3H, m), 2.36–2.31 (1H, m), 2.16–2.11 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.8, 158.6, 152.0 (d, J = 192.6 Hz), 147.2, 136.7, 135.7, 128.3, 126.3 (d, J = 13.3 Hz), 115.9 (d, J = 22.57 Hz), 106.7, 54.2, 52.9, 45.9, 31.3; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −118.5; MS (ESI positive) m/z: 396.1 [M + H]+.
(S)-6-(3-(3-(4-Fluorophenyl)thioureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (8b)
Following the general procedure, the product was a white solid 8b, yield 46%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.49 (1H, bs), 8.48 (1H, s), 7.87 (1H, bs); 7.86 (1H, dd, J = 8.90, 2.13 Hz), 7.48–7.47 (2H, m), 7.18–7.15 (4H, m), 6.63 (1H, d, J = 8.99 Hz), 4.91 (1H, m), 3.83–3.80 (1H, m), 3.61–3.59 (2H, m), 3.53–3.50 (1H, m), 2.36–2.32 (1H, m), 2.16–2.10 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.8, 158.5, 151.3 (d, J = 265.18 Hz), 147.1, 136.7, 135.7, 128.3, 126.4 (d, J = 7.21 Hz), 115.9 (d, J = 22.43 Hz), 106.8, 54.2, 52.9, 45.9, 31.2; MS (ESI positive) m/z: 396.1 [M + H]+.
(R)-6-(3-(3-Phenylthioureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (9a)
Following the general procedure, the product was a white solid 9a, yield 77%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.47 (1H, bs), 8.48 (1H, s), 8.13 (1H, s), 7.86 (1H, d, J = 8.56 Hz), 7.50 (2H, d, J = 7.57 Hz), 7.34 (2H, t, J = 7.37 Hz), 7.36 (2H, bs), 7.34–7.19 (1H, m), 6.63 (1H, d, J = 8.96 Hz), 4.92 (1H, m), 3.82 (1H, m), 3.60–3.53 (3H, m), 2.33 (1H, m), 2.13 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.4, 158.6, 147.3, 140.4, 135.7, 129.4, 128.3, 125.0, 123.8, 106.8, 54.2, 52.9, 45.9, 31.3; MS (ESI positive) m/z: 378.1 [M + H]+.
(S)-6-(3-(3-Phenylthioureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (9b)
Following the general procedure, the product was a white solid 9b, yield 46%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.47 (1H, bs), 8.48 (1H, s), 8.12 (1H, d, J = 5.41 Hz); 7.85 (1H, m), 7.50 (2H, d, J = 7.78 Hz), 7.34 (2H, t, J = 7.48 Hz), 7.18 (2H, bs), 7.12 (1H, t, J = 7.20 Hz), 6.63 (1H, d, J = 8.96 Hz), 4.92 (1H, m), 3.85–3.81 (1H, m), 3.61–3.51 (3H, m), 2.37–2.32 (1H, m), 2.15 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.4, 158.6, 147.2, 140.4, 135.7, 129.3, 128.3, 124.9, 123.7, 106.7, 54.2, 52.9, 45.9, 31.2; MS (ESI positive) m/z: 378.1 [M + H]+.
(R)-6-(3-(3-(4-Chloro-3-(trifluoromethyl)phenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (10a)
Following the general procedure, the product was a white solid 10a, yield 62%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.89 (1H, bs), 8.48 (1H, s), 8.11 (1H, s), 7.85 (1H, d, J = 8.81 Hz), 7.58 (2H, s), 7.19 (2H, bs), 6.80 (1H, d, J = 5.96 Hz), 6.62 (1H, d, J = 8.91 Hz), 4.37 (1H, m), 3.75–3.71 (1H, m), 3.57 (2H, m), 3.39 (1H, m), 2.27–2.24 (1H, m), 2.02–2.01 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.5, 147.2, 140.8, 135.6, 132.7, 128.3, 127.4, 125.1, 123.4, 122.5, 117.1, 106.7, 53.4, 50.1, 45.8, 31.7; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −61.4; MS (ESI positive) m/z: 464.1 [M + H]+; [α]D22° = −10 (c = 2.7; Acetone).
(R)-6-(3-(3-(4-Chloro-3-(trifluoromethyl)phenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (10b)
Following the general procedure, the product was a white solid 10b, yield 55%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.87 (1H, bs), 8.48 (1H, d, J = 1.82 Hz), 8.11 (1H, s), 7.85 (1H, dd, J = 8.91, 2.06 Hz), 7.58 (2H, s), 7.18 (2H, bs), 6.79 (1H, d, J = 6.26 Hz), 6.62 (1H, d, J = 8.99 Hz), 4.37 (1H, m), 3.76–3.72 (1H, m), 3.59–3.57 (2H, m), 3.45–3.41 (1H, m), 2.29–2.24 (1H, m), 2.04–1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.5, 147.2, 140.8, 135.6, 132.8, 128.3, 125.1, 123.4, 122.5, 117.1 (q, J = 5.39 Hz), 106.7, 53.4, 50.1, 45.8, 31.7;MS (ESI positive) m/z: 464.1 [M + H]+; [α]D22° = +11 (c = 3.1; Acetone).
(R)-6-(3-(3-(2-Fluorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (11a)
Following the general procedure, the product was a white solid 11a, yield 52%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.49 (1H, bs), 8.20–8.15 (2H, m), 7.85 (1H, dd, J = 8.76, 1.50 Hz), 7.20–7.18 (3H, m), 7.12 (1H, t, J = 7.70 Hz), 7.04 (1H, d, J = 6.57 Hz), 6.96 (1H, dd, J = 12.46, 6.57 Hz), 6.64 (1H, d, J = 8.97 Hz), 4.37 (1H, m), 3.74–3.70 (1H, m), 3.59 (2H, m), 3.43 (1H, m), 2.29–2.15 (1H, m), 2.00–1.97 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.3, 152.4 (d, J = 240.88 Hz), 147.2, 135.6, 129.0 (d, J = 10.17 Hz), 125.2 (d, J = 3.30 Hz), 122.5 (d, J = 7.55 Hz), 115.6 (d, J = 18.97 Hz), 106.7, 53.6, 50.0, 45.7, 31.9; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −130.9; MS (ESI positive) m/z: 380.1 [M + H]+; [α]D22° = −9 (c = 3.1; Acetone).
(S)-6-(3-(3-(2-Fluorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (11b)
Following the general procedure, the product was a white solid 11b, yield 57%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, d, J = 2.24 Hz), 8.22 (1H, d, J = 1.84 Hz), 8.17 (1H, t, J = 7.76 Hz), 7.86 (1H, dd, J = 8.94, 2.39 Hz), 7.21–7.19 (3H, m), 7.12 (1H, t, J = 7.54 Hz), 7.06 (1H, d, J = 6.66 Hz), 7.00 (1H, m), 6.65 (1H, d, J = 9.00 Hz), 4.37 (1H, m), 3.75–3.71 (1H, m), 3.59 (2H, m), 3.43–3.41 (1H, m), 2.29–2.23 (1H, m), 2.00–1.95 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.5, 155.3, 152.5 (d, J = 240.66 Hz), 147.0, 135.7, 129.0 (d, J = 10.21 Hz), 125.2, 122.5 (d, J = 7.36 Hz), 115.7 (d, J = 18.85 Hz), 106.9, 53.7, 50.0, 45.8, 31.9; MS (ESI positive) m/z: 380.1 [M + H]+; [α]D22° = +10 (c = 2.7; Acetone).
(R)-6-(3-(3-(2-Chlorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (12a)
Following the general procedure, the product was a white solid 12a, yield 60%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.62 (1H, bs), 8.40 (1H, m), 8.22 (1H, s), 7.47–7.42 (3H, m), 7.29 (2H, bs), 7.11 (1H, aps), 6.98 (1H, aps), 6.66 (1H, bs), 4.37 (1H, m), 3.74 (1H, m), 3.61 (3H, m), 2.25 (1H, m), 2.00 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.1, 155.2, 149.9, 147.3, 137.4, 130.0, 128.4, 125.5, 123.4, 122.6, 121.4, 116.3, 53.7, 50.1, 45.9, 31.9; MS (ESI positive) m/z: 396.1 [M + H]+; [α]D22° = −20 (c = 1.3; Acetone); Elemental analysis: calculated: C, 48.55; H, 4.58; Cl, 8.96; N, 17.69; O, 12.12; S, 8.10; found: C, 47.42; H, 4.51; N, 17.18.
(S)-6-(3-(3-(2-Chlorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (12b)
Following the general procedure, the product was a white solid 12b, yield 66%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.49 (1H, d, J = 2.27 Hz), 8.22 (1H, dd, J = 8.23, 0.93 Hz), 7.99 (1H, s), 7.86 (1H, dd, J = 8.96, 2.40 Hz), 7.44–7.42 (2H, m), 7.28 (1H, m), 7.18 (2H, bs), 6.99 (1H, m), 6.65 (1H, d, J = 9.00 Hz), 4.39 (1H, m), 3.75–3.71 (1H, m), 3.59 (2H, m), 3.45–3.42 (1H, m), 2.29–2.25 (1H, m), 2.02–1.97 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.2, 147.2, 137.4, 135.7, 130.0, 128.4, 128.3, 123.4, 121.8, 121.3, 106.7, 53.6, 50.0, 45.8, 31.9; MS (ESI positive) m/z: 396.1 [M + H]+; [α]D22° = +18 (c = 1.0; Acetone).
(R)-6-(3-(3-(4-Phenoxyphenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (13a)
Following the general procedure, the product was a white solid 13a, yield 69%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, bs), 8.39 (1H, m), 7.85 (1H, s), 7.44–7.38 (4H, m), 7.19 (2H, bs), 7.11 (1H, d, J = 6.01 Hz), 6.97 (4H, m), 6.63 (1H, s), 6.56 (1H, s), 4.37 (1H, m), 3.73 (1H, m), 3.58 (2H, m), 3.37 (1H, m), 2.26 (1H, m), 1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.7, 158.6, 155.9, 151.0, 147.2, 137.3, 135.6, 130.8, 128.2, 123.5, 120.7, 120.3, 118.3, 106.7, 53.6, 50.0, 45.8, 31.9; MS (ESI positive) m/z: 454.1 [M + H]+; [α]D22° = −13 (c = 1.8; Acetone).
(S)-6-(3-(3-(4-Phenoxyphenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (13b)
Following the general procedure, the product was a white solid 13b, yield 55%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.49 (1H, bs), 8.37 (1H, s), 7.86 (1H, dd, J = 8.90. 1.91 Hz), 7.44 (2H, d, J = 8.76 Hz), 7.38 (2H, t, J = 7.84 Hz), 7.18 (2H, bs), 7.11 (1H, t, J = 7.32 Hz), 6.97 (4H, m), 6.63 (1H, d, J = 9.00 Hz), 6.55 (1H, d, J = 6.70 Hz), 4.38 (1H, m), 3.75–3.71 (1H, m), 3.58 (2H, m), 3.43–3.41 (1H, m), 2.29–2.24 (1H, m), 2.02–1.97 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.7, 158.6, 155.9, 151.0, 147.2, 137.3, 135.6, 130.8, 128.2, 123.5, 120.7, 120.3, 118.3, 106.7, 53.6, 50.0, 45.8, 31.9; MS (ESI positive) m/z: 454.1 [M + H]+; [α]D22° = +11 (c = 2.9; Acetone).
(R)-6-(3-(3-(3,4-Dichlorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (14a)
Following the general procedure, the product was a white solid 14a, yield 54%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.71 (1H, bs), 8.47 (1H, s), 7.87–7.84 (2H, m), 7.49 (1H, d, J = 8.78 Hz), 7.28 (1H, d, J = 8.56 Hz), 7.19 (2H, bs), 6.76 (1H, d, J = 6.41 Hz), 6.62 (1H, d, J = 8.95 Hz), 4.36 (1H, m), 3.73 (1H, m), 3.58 (2H, m), 3.43 (1H, m), 2.28–2.24 (1H, m), 2.02–1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.5, 147.2, 141.4, 135.6, 131.8, 131.3, 128.3, 123.3, 119.7, 118.7, 106.7, 53.4, 50.1, 45.8, 31.8; MS (ESI positive) m/z: 430.0 [M + H]+; [α]D22° = −10 (c = 1.9; Acetone).
(S)-6-(3-(3-(3,4-Dichlorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (14b)
Following the general procedure, the product was a white solid 14b, yield 43%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.11 (1H, bs), 8.47 (1H, s), 7.88–7.85 (2H, m), 7.48 (1H, d, J = 8.48 Hz), 7.29 (1H, d, J = 7.92 Hz), 7.20 (2H, bs), 7.06 (1H, aps), 6.64 (1H, d, J = 8.63 Hz), 4.36 (1H, m), 3.75 (1H, m), 3.58 (2H, m), 3.41 (1H, m), 2.27 (1H, m), 2.00–1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.3, 155.6, 146.8, 141.5, 135.8, 131.8, 131.3, 128.3, 123.1, 119.5, 118.6, 107.0, 53.5, 50.0, 45.9, 31.7; MS (ESI positive) m/z: 430.0 [M + H]+; [α]D22° = +12 (c = 2.2; Acetone).
(R)-6-(3-(3-(2,3-Dihydrobenzo[b][1,4]dioxin-6-yl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (15a)
Following the general procedure, the product was a white solid 15a, yield 54%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.47 (1H, d, J = 1.67 Hz), 8.16 (1H, bs), 7.84 (1H, dd, J = 8.92. 1.90 Hz), 7.19 (2H, bs), 7.07 (1H, s), 6.73 (2H, s), 6.62 (1H, d, J = 9.01 Hz), 6.46 (1H, d, J = 6.65 Hz), 4.34 (1H, m), 4.33–4.20 (4H, m), 3.71–3.69 (1H, m), 3.57 (2H, m), 3.38 (1H, m), 2.26–2.22 (1H, m), 1.99–1.96 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.8, 147.2, 143.9, 138.8, 135.6, 134.9, 128.2, 117.6, 112.0, 107.9, 106.7, 65.1, 53.6, 49.9, 45.8, 31.9; MS (ESI positive) m/z: 420.1 [M + H]+.
(S)-6-(3-(3-(2,3-Dihydrobenzo[b][1,4]dioxin-6-yl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (15b)
Following the general procedure, the product was a white solid 15b, yield 42%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.76, (1H, bs), 8.47 (1H, s), 7.85 (1H, dd, J = 8.92. 1.88 Hz),7.70–7.65 (1H, m), 7.18 (2H, bs), 7.08 (1H, s), 6.73 (2H, s), 6.62 (1H, d, J = 9.01 Hz), 4.34 (1H, m), 4.33–4.19 (4H, m), 3.74–3.69 (1H, m), 3.58 (2H, m), 3.39 (1H, m), 2.26–2.22 (1H, m), 1.99–1.96 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.5, 155.9, 147.0, 143.9, 138.8, 135.7, 128.2, 126.1, 117.6, 111.9, 107.8, 106.8, 65.1, 64.7, 53.6, 49.9, 45.9, 31.9; MS (ESI positive) m/z: 420.1 [M + H]+.
(R)-6-(3-(3-(3,5-Bis(trifluoromethyl)phenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (16a)
Following the general procedure, the product was a white solid 16a, yield 75%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.14 (1H, bs), 8.48 (1H, s), 8.12 (2H, s), 7.85 (1H, d, J = 8.72 Hz), 7.60 (1H, s), 7.19 (2H, bs), 6.98 (1H, d, J = 6.13 Hz), 6.63 (1H, d, J = 8.92 Hz), 4.39 (1H, m), 3.77–3.73 (1H, m), 3.60 (2H, m), 3.46 (1H, m), 2.28–2.25 (1H, m), 2.03 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.5, 147.2, 143.2, 135.6, 131.5 (q, J = 32.57 Hz), 128.3, 122.9 (q, J = 272.42 Hz), 118.3, 114.6, 106.7, 53.3, 50.2, 45.8, 31.7; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −61.7; MS (ESI positive) m/z: 498.1 [M + H]+; [α]D22° = −12 (c = 1.0; Acetone).
(S)-6-(3-(3-(3,5-Bis(trifluoromethyl)phenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (16b)
Following the general procedure, the product was a white solid 16a, yield 67%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.39 (1H, bs), 8.48 (1H, s), 8.12 (2H, s), 7.86 (1H, d, J = 8.29 Hz), 7.58 (1H, s), 7.19 (3H, bs), 6.64 (1H, d, J = 8.79 Hz), 4.39 (1H, m), 3.75–3.74 (3H, m), 3.46 (1H, m), 2.29–2.28 (1H, m), 2.04–2.03 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.5, 155.6, 147.1, 143.4, 135.7, 131.5 (q, J = 32.45 Hz), 128.3, 124.3 (q, J = 272.61 Hz), 114.5, 106.8, 53.4, 50.2, 45.9, 31.6; MS (ESI positive) m/z: 498.1 [M + H]+; [α]D22° = +10 (c = 1.4; Acetone).
(R)-2-(3,6-Dihydroxy-9H-xanthen-9-yl)-5-(3-(1-(5-sulfamoylpyridin-2-yl)pyrrolidin-3-yl)thioureido)benzoic Acid (17a)
Following the general procedure, the product was an orange solid 17a, yield 41%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 10.13 (1H, bs), 8.65 (1H, bs), 8.49 (1H, d, J = 2.01 Hz), 8.39 (2H, s), 7.87 (1H, dd, J = 8.95, 2.28 Hz), 7.82 (1H, J = 8.12 Hz), 7.22 (3H, m), 6.71 (2H, s), 6.66–6.59 (6H, m), 4.93 (1H, m), 3.88–3.83 (1H, m), 3.64 (3H, m), 2.44–2.36 (1H, m), 2.18–2.15 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.4, 169.5, 160.4, 158.6, 152.8, 147.2, 142.4, 135.7, 130.0, 129.2, 128.4, 127.4, 126.2, 124.9, 114.6, 113.6, 110.7, 106.8, 103.2, 56.0, 54.2, 53.1, 46.0, 31.6; MS (ESI positive) m/z: 634.1 [M + H]+; [α]D22° = −9 (c = 1.0; Acetone).
(S)-2-(3,6-Dihydroxy-9H-xanthen-9-yl)-5-(3-(1-(5-sulfamoylpyridin-2-yl)pyrrolidin-3-yl)thioureido)benzoic Acid (17b)
Following the general procedure, the product was an orange solid 17b, yield 34%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 10.16 (1H, bs), 9.94 (1H, bs), 8.54 (1H, bs), 8.50 (1H, d, J = 2.16 Hz), 8.37 (1H, s), 7.87 (1H, dd, J = 8.96, 2.33 Hz), 7.81 (1H, J = 8.01 Hz), 7.20 (2H, m), 6.71 (2H, s), 6.66–6.59 (6H, m), 4.95 (1H, m), 3.89–3.84 (1H, m), 3.64–3.56 (4H, m), 2.41–2.37 (1H, m), 2.19–2.12 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.4, 169.4, 160.5, 160.4, 158.6, 152.7, 148.2, 147.2, 142.4, 135.7, 129.9, 128.4, 127.3, 124.9, 113.5, 110.6, 106.8, 103.2, 54.2, 52.9, 45.9, 31.2; MS (ESI positive) m/z: 634.1 [M + H]+; [α]D22° = +6 (c = 4.3; Acetone).
(R)-6-(3-(3-(2-Methoxyphenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (18a)
Following the general procedure, the product was a white solid 18a, yield 41%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, s), 8.13 (1H, d, J = 7.61 Hz), 7.91 (1H, s), 7.85 (1H, dd, J = 8.93, 1.97 Hz), 7.27 (1H, J = 6.65 Hz), 7.19 (2H, bs), 6.99 (1H, d, J = 7.50 Hz), 6.92–6.85 (2H, m), 6.64 (1H, d, J = 9.0 Hz), 4.36 (1H, m), 3.85 (3H, s), 3.73–3.68 (1H, m), 3.58 (2H, m), 3.43 (1H, m), 2.27–2.22 (1H, m), 1.98–1.94 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.7, 155.7, 148.1, 147.3, 135.7, 130.2, 128.7, 122.0, 121.4, 118.7, 111.5, 106.8, 56.6, 53.8, 49.9, 45.8, 32.0; MS (ESI positive) m/z: 392.1 [M + H]+; [α]D22° = −14 (c = 1.8; Acetone).
(S)-6-(3-(3-(2-Methoxyphenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (18b)
Following the general procedure, the product was a white solid 18b, yield 41%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, s), 8.13 (1H, d, J = 7.14 Hz), 7.89 (1H, s), 7.85 (1H, d, J = 7.33 Hz), 7.29 (1H, m), 7.18 (2H, bs), 6.98 (1H, d, J = 7.23 Hz), 6.92–6.86 (2H, m), 6.63 (1H, d, J = 8.93 Hz), 4.36 (1H, m), 3.84 (3H, s), 3.73–3.69 (2H, m), 3.49–3.42 (2H, m), 2.27–2.23 (1H, m), 1.98–1.95 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.7, 155.7, 148.1, 147.2, 135.7, 130.2, 128.3, 122.0, 121.4, 118.7, 111.5, 106.7, 56.6, 53.8, 49.9, 45.8, 31.6; MS (ESI positive) m/z: 392.1 [M + H]+; [α]D22° = +12 (c = 1.0; Acetone).
(R)-6-(3-(3-(4-Nitrophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (19a)
Following the general procedure, the product was a yellow solid 19a, yield 61%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.19 (1H, bs), 8.48 (1H, d, J = 1.70 Hz), 8.18 (2H, d, J = 9.06 Hz), 7.85 (1H, dd, J = 8.91, 1.87 Hz), 7.65 (2H, d, J = 9.06 Hz), 7.19 (2H, bs), 6.92 (1H, d, J = 6.63 Hz), 6.63 (2H, d, J = 8.98 Hz), 4.40 (1H, m), 3.76–3.72 (1H, m), 3.59 (2H, m), 3.43 (1H, m), 2.30–2.27 (1H, m), 2.04–2.00 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.1, 147.8, 147.2, 141.5, 135.7, 128.3, 126.1, 117.8, 106.8, 53.4, 50.1, 45.8, 37.7; MS (ESI positive) m/z: 407.1 [M + H]+; [α]D22° = −26 (c = 3.1; Acetone).
(S)-6-(3-(3-(4-Nitrophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (19b)
Following the general procedure, the product was a yellow solid 19b, yield 58%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.15 (1H, bs), 8.49 (1H, d, J = 2.11 Hz), 8.18 (2H, d, J = 9.12 Hz), 7.85 (1H, dd, J = 8.95, 2.26 Hz), 7.65 (2H, d, J = 9.14 Hz), 7.18 (2H, bs), 6.89 (1H, d, J = 6.66 Hz), 6.63 (1H, d, J = 9.00 Hz), 4.41 (1H, m), 3.77–3.72 (1H, m), 3.59 (2H, m), 3.46 (1H, m), 2.31–2.26 (1H, m), 2.05–2.00 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.1, 147.8, 147.2, 141.5, 135.7, 128.3, 126.1, 117.8, 106.7, 53.4, 50.1, 45.8, 31.7; MS (ESI positive) m/z: 407.1 [M + H]+; [α]D22° = +29 (c = 3.2; Acetone).
(R)-6-(3-(3-(4-(Trifluoromethyl)phenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (20a)
Following the general procedure, the product was a white solid 20a, yield 72%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.81 (1H, bs), 8.48 (1H, d, J = 1.67 Hz), 7.85 (1H, dd, J = 8.91, 2.01 Hz), 7.62 (4H, aps), 7.19 (2H, bs), 6.75 (1H, d, J = 6.57 Hz), 6.63 (2H, d, J = 8.98 Hz), 4.39 (1H, m), 3.76–3.72 (1H, m), 3.59 (2H, m), 3.44 (1H, m), 2.29–2.25 (1H, m), 2.03–1.9 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.7, 155.5, 147.2, 144.9, 135.7, 129.3, 126.9, 126.8, 124.2, 122.2 (q, J = 30.81 Hz), 118.2, 106.7, 53.5, 50.0, 45.8, 31.8; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −59.9; MS (ESI positive) m/z: 430.1 [M + H]+; [α]D22° = −22 (c = 3.9; Acetone).
(S)-6-(3-(3-(4-(Trifluoromethyl)phenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (20b)
Following the general procedure, the product was a white solid 20b, yield 56%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.20 (1H, bs), 8.47 (1H, d, J = 2.04 Hz), 7.85 (1H, dd, J = 8.93, 2.16 Hz), 7.62 (4H, apq, J = 8.82 Hz), 7.19 (2H, bs), 7.18 (1H, bs), 6.63 (1H, d, J = 8.99 Hz), 4.39 (1H, m), 3.76–3.72 (1H, m), 3.60–3.58 (2H, m), 3.43–3.41 (1H, m), 2.29–2.25 (1H, m), 2.02–2.00 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.5, 155.6, 147.1, 145.1, 135.7, 128.3, 126.9, 123.2 (q, J = 212.9 Hz), 121.9 (q, J = 30.81 Hz), 118.1, 106.8, 53.5, 50.0, 45.9, 31.8; MS (ESI positive) m/z: 430.1 [M + H]+;[α]D22° = +20 (c = 6.0; Acetone).
(R)-6-(3-(3-(2-Fluorophenyl)thioureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (21a)
Following the general procedure, the product was a pale yellow solid 21a, yield 73%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.18 (1H, bs), 8.49 (1H, s), 8.37 (1H, s), 7.86 (2H, d, J = 8.71 Hz), 7.29–7.19 (4H, m), 6.64 (1H, d, J = 8.91 Hz), 4.91 (1H, m), 3.84–3.80 (1H, m), 3.60–3.54 (3H, m), 2.36–2.32 (1H, m), 2.15 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm):182.2, 158.6, 147.2, 135.7, 128.3, 128.1, 124.8 (d, J = 3.07 Hz), 116.4 (d, J = 19.9 Hz), 106.8, 54.4, 52.9, 45.9, 31.3; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −124.0; MS (ESI positive) m/z: 396.1 [M + H]+; [α]D22° = −27 (c = 3.5; Acetone).
(S)-6-(3-(3-(2-Fluorophenyl)thioureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (21b)
Following the general procedure, the product was a pale yellow solid 21b, yield 51%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.19 (1H, bs), 8.49 (1H, d, J = 1.99 Hz), 8.38 (1H, s), 7.86 (2H, dd, J = 8.77, 1.83 Hz), 7.24–7.19 (4H, m), 6.64 (1H, d, J = 9.03 Hz), 4.91 (1H, m), 3.85–3.80 (1H, m), 3.61–3.51 (3H, m), 2.37–2.32 (1H, m), 2.12 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm):182.3, 158.7, 156.7 (d, J = 381.42 Hz), 147.2, 135.9, 128.5, 128.4, 125.0 (d, J = 2.86 Hz), 116.6 (d, J = 19.92 Hz), 107.0, 54.6, 53.1, 46.1, 31.4; MS (ESI positive) m/z: 396.1 [M + H]+; [α]D22° = +30 (c = 1.1; Acetone).
(R)-6-(3-(3-(2-Bromo-4,6-difluorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (22a)
Following the general procedure, the product was a white solid 22a, yield 60%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, d, J = 2.15 Hz), 7.85 (1H, dd, J = 8.95, 2.30 Hz), 7.72 (1H, s), 7.55 (1H, m), 7.42 (1H, td, J = 9.59, 2.63 Hz), 7.18 (2H, bs), 6.88 (1H, d, J = 6.83 Hz), 6.62 (1H, d, J = 9.00 Hz), 4.34 (1H, m), 3.75–3.70 (1H, m), 3.57 (2H, m), 3.36 (1H, m), 2.27–2.23 (1H, m), 2.02–1.97 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 161.6, 160.6, 158.6, 158.1, 155.7, 147.2, 135.6, 128.2, 124.7, (d, J = 14.75 Hz), 124.1 (d, J = 15.73 Hz), 116.2 (d, J = 22.42 Hz), 106.7, 104.9 (t, J = 26.12 Hz), 53.5, 50.3, 45.8, 31.8; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −110.9, -112.1; MS (ESI positive) m/z: 476.0 [M + H]+; [α]D22° = −12 (c = 3.7; Acetone).
(S)-6-(3-(3-(2-Bromo-4,6-difluorophenyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (22b)
Following the general procedure, the product was a white solid 22b, yield 44%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.48 (1H, d, J = 2.30 Hz), 7.85 (1H, dd, J = 8.98, 2.45 Hz), 7.76 (1H, s), 7.57–7.55 (1H, m), 7.43 (1H, td, J = 9.64, 2.77 Hz), 7.19 (2H, bs), 6.91 (1H, d, J = 6.50 Hz), 6.63 (1H, d, J = 9.01 Hz), 4.34 (1H, m), 3.75–3.71 (1H, m), 3.61–3.58 (2H, m), 3.40 (1H, m), 2.27–2.22 (1H, m), 2.02–1.97 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 155.8, 147.1, 135.7, 128.2, 116.4, 116.1, 106.8, 105.4, 105.2, 53.6, 50.3, 45.9, 31.9; MS (ESI positive) m/z: 476.0 [M + H]+; [α]D22° = +14 (c = 1.7; Acetone).
General Synthesis of Compounds 24 and 25
Compound 5a/5b (1 equiv) in acetonitrile was added to benzenesulfonyl isocyanate 23a-b (1 equiv) and Et3N (3 equiv). The solution was stirred overnight at room temperature. The reaction was quenched with saturated solution of NH4Cl, extracted with EtOAc, and dried over Na2SO4. The crude material was purified by flash column chromatography (MeOH/DCM: 5:95), to yield compounds 24 or 25.
(R)-6-(3-(3-(Phenylsulfonyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (24a)
Following the general procedure, the product was a white solid 24a, yield 56%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.45 (1H, d, J = 2.21 Hz), 7.92 (2H, d, J = 7.44 Hz), 7.83 (1H, dd, J = 8.93, 2.43 Hz) 7.68 (1H, m), 7.61 (2H, t, J = 7.46 Hz), 7.50 (1H, m), 7.18 (2H, bs), 6.89 (1H, bs), 6.57 (1H, d, J = 8.99 Hz), 4.19 (1H, m), 3.63 (1H, m), 3.50 (3H, m), 2.16 (1H, m), 1.91 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 153.3, 147.2, 135.6, 129.7, 128.8, 128.3, 127.9, 127.7, 106.7, 53.0, 50.2, 45.7, 31.4; MS (ESI positive) m/z: 426.1 [M + H]+.
(R)-6-(3-(3-((2-Chlorophenyl)sulfonyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (25a)
Following the general procedure, the product was a white solid 25a, yield 36%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.46 (1H, d, J = 1.62 Hz), 8.07 (1H, d, J = 7.74 Hz), 7.85–7.83 (2H, m), 7.67 (2H, aps), 7.50 (1H, s), 7.19 (2H, bs), 6.86 (1H, aps), 6.58 (1H, d, J = 8.98 Hz), 4.18 (1H, m), 3.65–3.61 (1H, m), 3.50–3.48 (3H, m), 2.17 (1H, m), 1.95–1.88 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.6, 147.2, 135.7, 135.3, 132.6, 132.4, 131.8, 131.5, 131.4, 128.3, 127.5, 106.8, 53.1, 45.8, 31.6, 30.6; MS (ESI positive) m/z: 460.0 [M + H]+; [α]D22° = −14 (c = 1.4; Acetone).
(S)-6-(3-(3-((2-Chlorophenyl)sulfonyl)ureido)pyrrolidin-1-yl)pyridine-3-sulfonamide (25b)
Following the general procedure, the product was a white solid 25b, yield 35%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.50 (1H, s), 8.23 (1H, d, J = 8.17 Hz), 7.99 (1H, s), 7.86 (1H, dd, J = 8.91, 1.96 Hz), 7.44–7.42 (2H, m), 7.28 (2H, t,, J = 7.48 Hz), 7.19 (2H, bs), 6.99 (1H, dd,, J = 11.09, 4.11 Hz), 6.64 (1H, d, J = 9.00 Hz), 4.39 (1H, m), 3.75–3.71 (1H, m), 3.45 (2H, m), 3.43 (1H, m), 2.29–2.25 (1H, m), 2.00–1.98 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 158.7, 155.3, 147.3, 137.5, 135.7, 130.1, 128.5, 128.4, 123.4, 121.9, 121.4. 106.8, 53.7, 50.1. 45.9, 32.1; MS (ESI positive) m/z: 460.0 [M + H]+; [α]D22° = +15 (c = 1.2; Acetone).
General Synthesis of Compounds 27–29
To a solution of 2-chloropyridine (26a-c, 1 equiv) and K2CO3 (1.3 equiv) in dry DMF and inert atmosphere (N2) was added pyrrolidine (3a,b, 1 equiv). The mixture was stirred for 4 h at 100 °C. The reaction mixture was quenched with ice-cooled, saturated NH4Cl solution and stirred for 15 min to give a precipitate, which was collected by vacuum filtration and washed with water. The obtained solid was triturated with Et2O to yield the derivatives 27–29.
tert-Butyl (R)-(1-(Pyridin-2-yl)pyrrolidin-3-yl)carbamate (27a)
Following the general procedure, the product was a white solid 27a, yield 76%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.08 (1H, d, J = 3.29 Hz), 7.50 (1H, t, J = 7.13 Hz), 7.22 (1H, d, J = 4.67 Hz), 6.56 (1H, m), 6.43 (1H, d, J = 8.40 Hz), 4.14 (1H, m), 3.60 (1H, m), 3.52 (1H, m), 3.49 (1H, m), 3.23 (1H, m), 2.16 (1H, m), 1.92 (1H, m), 1.43 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 157.8, 156.2, 148.7, 137.8, 112.1, 107.1, 78.7, 52.9, 50.8, 40.4, 31.5, 29.1; MS (ESI positive) m/z: 263.2 [M + H]+.
tert-Butyl (R)-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)carbamate(28a)
Following the general procedure, the product was a yellow solid 28a, yield 79%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.43 (1H, m), 8.22 (1H, m), 7.26 (1H, d, J = 4.58 Hz), 6.84 (1H, dd, J = 7.96, 4.51 Hz), 4.10 (1H, m), 3.52–3.44 (1H, m), 3.43–3.41 (2H, m), 3.12–3.08 (1H, m), 2.12–2.09 (1H, m), 1.94–1.90 (1H, m), 1.41 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 156.1, 153.0, 150.6, 135.8, 132.3, 112.6, 78.8, 55.0, 50.6, 48.0, 30.9, 29.1; MS (ESI positive) m/z: 309.2 [M + H]+.
tert-Butyl (S)-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)carbamate(28b)
Following the general procedure, the product was a yellow solid 28b, yield 92%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.43 (1H, dd, J = 4.47, 1.53 Hz), 8.22 (1H, dd, J = 8.03, 1.52 Hz), 7.25 (1H, d, J = 4.52 Hz), 6.85 (1H, dd, J = 8.03, 4.51 Hz), 4.09 (1H, m), 3.52–3.42 (1H, m), 3.12–3.08 (2H, m), 3.10 (1H, dd, J = 11.32, 4.57 Hz), 2.14–2.09 (1H, m), 1.94–1.91 (1H, m), 1.41 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 156.1, 153.1, 150.6, 135.8, 132.3, 112.6, 78.8, 55.0, 50.7, 48.0, 30.9, 29.1; MS (ESI positive) m/z: 309.2 [M + H]+.
tert-Butyl (R)-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)carbamate (29a)
Following the general procedure, the product was a white solid 29a, yield 70%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.41 (1H, s), 7.77 (1H, dd, J = 8.94, 2.21 Hz), 7.26 (1H, d, J = 5.53 Hz), 6.58 (1H, d, J = 8.96 Hz), 4.17 (1H, m), 3.70–3.65 (1H, m), 3.60–3.58 (1H, m), 3.49–3.47 (1H, m), 3.34 (1H, m), 2.20–2.16 (1H, m), 1.96–1.91 (1H, m), 1.43 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.2, 156.2, 146.5, 146.4, 134.6, 126.1 (q, J = 270.01 Hz), 113.0 (q, J = 32.13 Hz), 106.9, 78.8, 53.1, 50.7, 45.8, 31.4, 29.1; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −59.0; MS (ESI positive) m/z: 332.2 [M + H]+.
tert-Butyl (S)-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)carbamate (29b)
Following the general procedure, the product was a white solid 29b, yield 89%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.41 (1H, s), 7.77 (1H, dd, J = 8.90, 1.98 Hz), 7.28 (1H, d, J = 5.89 Hz), 6.58 (1H, d, J = 8.95 Hz), 4.17 (1H, m), 3.69–3.67 (1H, m), 3.58 (1H, m), 3.49 (1H, m), 3.33 (1H, m), 2.20–2.15 (1H, m), 1.96–1.93 (1H, m), 1.43 (9H, s); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.2, 156.2, 146.5, 134.7, 126.1 (q, J = 269.83 Hz), 113.0 (q, J = 31.97 Hz), 107.0, 78.8, 53.1, 50.7, 45.8, 31.4, 29.1; MS (ESI positive) m/z: 332.2 [M + H]+.
General Synthesis of Compounds 30–32
To the corresponding compounds 27–29 (1 equiv) in dichloromethane (DCM) was added TFA (6 equiv), and the solution was stirred overnight at room temperature. The solvents were evaporated, and the residue was dissolved in EtOAc and washed with 1 N NaOH solution to give pure compounds 30–32.
(R)-1-(Pyridin-2-yl)pyrrolidin-3-amine (30a)
Following the general procedure, the product was a yellow oil 30a, yield 68%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.07 (1H, dd, J = 4.79, 1.01 Hz), 7.48 (1H, m), 6.53 (1H, dd, J = 6.52, 5.40 Hz), 6.40 (1H, d, J = 8.48 Hz), 3.59–3.51 (3H, m), 3.37–3.35 (1H, m), 3.07–3.03 (1H, m), 2.10–2.03 (1H, m), 1.76–1.68 (3H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 148.7, 137.7, 11.7, 106.9, 55.9, 51.7, 45.8, 35.1; MS (ESI positive) m/z: 164.1 [M + H]+.
(R)-1-(6-Nitropyridin-2-yl)pyrrolidin-3-amine (31a)
Following the general procedure, the product was a yellow oil 31a, yield 79%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.42 (1H, dd, J = 4.47, 1.58 Hz), 8.20 (1H, dd, J = 8.04. 1.57 Hz), 6.81 (1H, d, J = 8.04, 4.50 Hz), 3.61–3.55 (2H, m), 3.44–3.39 (1H, m), 3.33 (1H, dd, J = 11.19, 5.72 Hz), 2.91 (1H, dd, J = 11.17. 4.80 Hz), 2.08–2.00 (3H, m), 1.77–1.69 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 153.1, 150.7, 135.8, 132.1, 112.3, 58.2, 51.5, 48.4, 34.0; MS (ESI positive) m/z: 209.1 [M + H]+.
(S)-1-(6-Nitropyridin-2-yl)pyrrolidin-3-amine (31b)
Following the general procedure, the product was a yellow oil 31b, yield 93%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.47 (1H, dd, J = 4.47, 1.45 Hz), 8.26 (1H, dd, J = 8.03. 1.43 Hz), 8.19 (3H, bs), 6.91 (1H, d, J = 8.03, 4.54 Hz), 3.95 (1H, m), 3.62 (2H, m), 3.60 (1H, m), 3.59 (1H, m), 2.37–2.29 (1H, m), 2.12–2.03 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 153.1, 150.2, 135.9, 132.8, 113.3, 53.0, 50.0, 47.7, 29.6; MS (ESI positive) m/z: 209.1 [M + H]+.
(R)-1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-amine (32a)
Following the general procedure, the product was a white solid 32a, yield 99%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.39 (1H, s), 7.75 (1H, dd, J = 8.91, 2.06 Hz), 6.55 (1H, d, J = 8.95 Hz), 3.60–3.58 (3H, m), 3.47 (1H, m), 3.16 (1H, m), 2.12–2.03 (1H, m), 1.78–1.74 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.3, 146.5, 146.4, 134.6, 126.1 (q, J = 269.55 Hz), 112.6 (q, J = 32.17 Hz), 106.8, 55.9, 51.5, 46.0, 34.8; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −58.9; MS (ESI positive) m/z: 232.1 [M + H]+.
(S)-1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-amine (32b)
Following the general procedure, the product was a white solid 32b, yield 78%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.39 (1H, s), 7.75 (1H, dd, J = 8.77, 1.70 Hz), 6.55 (1H, d, J = 8.95 Hz), 3.60–3.58 (2H, m), 3.47 (1H, m), 3.34 (1H, m), 3.16 (1H, m), 2.10–2.06 (1H, m), 1.76–1.75 (3H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.3, 146.5, 146.4, 134.6, 128.9 (q, J = 269.89 Hz), 112.6 (q, J = 31.98 Hz), 106.8, 56.0, 51.6, 46.1, 34.8; MS (ESI positive) m/z: 232.1 [M + H]+.
General Synthesis of Compounds 35–40
The appropriate isothiocyanate (33a-b, 1 equiv) was dissolved in acetonitrile and treated with the corresponding amine 30-32 (1 equiv). The mixture was stirred overnight at r.t., quenched with H2O, and the readily formed precipitate was collected by filtration and dried on air to afford the titled thiourea 35–40.
(R)-4-(3-(1-(Pyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (35a)
Following the general procedure, the product was a white solid 35a, yield 53%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.74 (1H, bs), 8.36 (1H, s), 8.11 (1H, d, J = 4.23 Hz), 7.77–7.72 (4H, m), 7.55–7.52 (1H, m), 7.29 (2H, bs), 6.61 (1H, t, J = 5.75 Hz), 6.52 (1H, d, J = 8.40 Hz), 4.90 (1H, m), 3.77–3.73 (1H, m), 3.56–3.47 (4H, m), 2.36–2.30 (1H, m), 2.12–2.11 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm):168.1, 155.8, 145.6, 145.3, 143.5, 131.4, 128.3, 126.7, 123.9, 117.7, 67.9, 46.5, 43.3, 26.1; MS (ESI positive) m/z: 378.1 [M + H]+; [α]D22° = −20 (c = 2.5; Acetone).
(R)-3-(3-(1-(Pyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (36a)
Following the general procedure, the product was a white solid 36a, yield 52%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.66 (1H, bs), 8.26 (1H, s), 8.11 (1H, d, J = 3.68 Hz), 8.04 (1H, aps) 7.74 (1H, d, J = 7.66 Hz), 7.57–7.49 (3H, m), 7.39 (2H, bs), 6.61 (1H, m), 6.52 (1H, d. J = 8.42 Hz), 4.90 (1H, m), 3.75 (1H, m), 3.56–3.45 (3H, m), 2.33 (1H, m), 2.12 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.4, 157.8, 148.8, 145.1, 141.1, 138.0, 134.7, 129.8, 124.3, 121.7, 112.4, 107.3, 54.3, 52.7, 45.6, 31.5; MS (ESI positive) m/z: 378.1 [M + H]+; Elemental analysis: calculated: C, 50.91; H, 5.07; N, 18.55; O, 8.48; S, 16.99 found: C, 49.73; H, 5.06; N, 18.36.
(R)-4-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (37a)
Following the general procedure, the product was a yellow solid 37a, yield 56%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.79 (1H, bs), 8.47 (1H, dd, J = 4.46, 1.43 Hz), 8.40 (1H, bs), 8.26 (1H, dd, J = 8.04, 1.42 Hz), 7.76 (2H, d, J = 8.73 Hz), 7.69 (2H, d, J = 8.75 Hz), 7.31 (2H, bs), 6.88 (1H, dd, J = 8.04, 4.53 Hz), 4.85 (1H, m), 3.69–3.61 (2H, m), 3.48–3.46 (1H, m), 3.32 (1H, dd, J = 11.64, 3.94 Hz), 2.35–2.27 (1H, m), 2.17–2.11 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.3, 153.2, 150.6, 143.6, 139.5, 136.0, 132.5, 127.2, 122.4, 112.9, 54.9, 54.1, 48.1, 30.7; MS (ESI positive) m/z: 423.1 [M + H]+ Elemental analysis: calculated: C, 45.49; H, 4.29; N, 19.89; O, 15.15; S, 15.18 found: C, 45.21; H, 4.28; N, 19.82.
(S)-4-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (37b)
Following the general procedure, the product was a yellow solid 37b, yield 53%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.77 (1H, bs), 8.47 (1H, d, J = 3.35 Hz), 8.38 (1H, d, J = 3.78 Hz), 8.25 (1H, d, J = 7.04 Hz), 7.76 (2H, d, J = 8.68 Hz), 7.69 (2H, d, J = 8.66 Hz), 7.29 (2H, bs), 6.88 (1H, dd, J = 8.02, 4.52 Hz), 4.85 (1H, m), 3.69–3.60 (2H, m), 3.50–3.46 (1H, m), 3.30 (1H, m), 2.34–2.29 (1H, m), 2.16–2.14 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.4, 153.2, 150.6, 143.6, 136.4, 132.6, 127.2, 122.6, 122.5, 113.0, 55.0, 54.2, 48.2, 30.8; MS (ESI positive) m/z: 423.1 [M + H]+.
(R)-3-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (38a)
Following the general procedure, the product was a yellow solid 38a, yield 66%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.70 (1H, bs), 8.46 (1H, s), 8.25 (2H, m), 8.03 (1H, s), 7.72 (2H, m), 7.56 (2H, m), 7.39 (2H, bs), 6.88 (1H, d, J = 4.17 Hz), 4.86 (1H, m), 3.65 (2H, m), 3.49–3.46 (2H, m), 2.31 (1H, m), 2.12 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.7, 153.2, 150.6, 145.2, 141.0, 136.0, 132.5, 130.0, 129.9, 122.5, 121.5, 112.9, 54.9, 54.0, 48.1, 30.8; MS (ESI positive) m/z: 423.1 [M + H]+; [α]D22° = −13 (c = 4.1; Acetone).
(S)-3-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (38b)
Following the general procedure, the product was a yellow solid 38b, yield 65%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.70 (1H, bs), 8.46 (1H, s), 8.24 (2H, m), 8.03 (1H, s), 7.72 (1H, d, J = 7.92 Hz), 7.56–7.51 (2H, m), 7.39 (2H, bs), 6.88 (1H, dd, J = 7.98, 4.51 Hz), 4.86 (1H, m), 3.69–3.61 (2H, m), 3.51–3.47 (1H, m), 3.33–3.29 (1H, m), 2.34–2.29 (1H, m), 2.14 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.7, 153.2, 150.6, 145.2, 141.0, 136.0, 132.5, 129.8, 126.7, 121.8, 120.5, 112.9, 54.9, 54.0, 48.1, 30.8; MS (ESI positive) m/z: 423.1 [M + H]+; [α]D22° = +15 (c = 2.3; Acetone).
(R)-4-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (39a)
Following the general procedure, the product was a white solid 39a, yield 71%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.78 (1H, bs), 8.45 (2H, m), 7.82 (1H, dd, J = 8.95, 2.16 Hz), 7.76 (2H, d, J = 8.81 Hz), 7.72 (2H, d, J = 8.79 Hz), 7.31 (2H, bs), 6.65 (1H, d, J = 8.94 Hz), 4.92 (1H, m), 3.85–3.81 (1H, m), 3.61 (3H, m), 2.39–2.34 (1H, m), 2.17–2.10 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.2, 159.2, 146.5, 143.6, 139.5, 134.8, 127.1, 126.1 (q, J = 251.52 Hz), 122.4, 113.3 (q, J = 32.06 Hz), 107.1, 54.2, 52.8, 45.8, 31.2; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −59.0; MS (ESI positive) m/z: 446.1 [M + H]+; [α]D22° = −45 (c = 5.1; Acetone); Elemental analysis: calculated: C, 45.84; H, 4.07; F, 12.79; N, 15.72; O, 7.18; S, 14.39 found: C, 45.73; H, 4.06; F, 12.71; N, 15.68.
(S)-4-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (39b)
Following the general procedure, the product was a white solid 39b, yield 60%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.76 (1H, bs), 8.45 (1H, s), 8.40 (1H, d, J = 3.67 Hz), 7.81 (1H, d, J = 7.85 Hz), 7.76 (2H, d, J = 8.57 Hz), 7.72 (2H, d, J = 8.55 Hz), 7.30 (2H, bs), 6.65 (1H, d, J = 8.90 Hz), 4.92 (1H, m), 3.86–3.82 (1H, m), 3.61 (3H, m), 2.39–2.34 (1H, m), 2.17–2.14 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.2, 159.2, 146.5, 143.6, 139.4, 134.8, 127.1, 126.1 (q, J = 269.91 Hz), 122.4, 113.3 (q, J = 32.25 Hz), 107.1, 54.2, 52.8, 45.8, 31.2; MS (ESI positive) m/z: 446.1 [M + H]+; [α]D22° = +40 (c = 1.9; Acetone) Elemental analysis: calculated: C, 45.84; H, 4.07; F, 12.79; N, 15.72; O, 7.18; S, 14.39 found: C, 45.74; H, 4.06; F, 12.73; N, 15.71.
(R)-3-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (40a)
Following the general procedure, the product was a white solid 40a, yield 61%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.69 (1H, bs), 8.45 (1H, s), 8.31 (1H, s), 8.04 (1H, s), 7.82 (1H, dd, J = 8.94, 2.11 Hz), 7.73 (1H, d, J = 7.63 Hz), 7.57–7.50 (2H. m), 7.40 (2H, bs), 6.66 (1H, d, J = 8.95 Hz), 4.92 (1H, m), 3.86–3.82 (1H, m), 3.62–3.57 (2H, m), 3.45–3.38 (1H, m), 2.40–2.32 (1H, m), 2.17–2.12 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.5, 159.2, 146.5, 145.1, 141.0, 134.8, 129.8, 126.5, 126.1 (q, J = 270.0 Hz), 121.7, 120.4, 113.3 (q, J = 32.16 Hz), 107.1, 54.2, 52.8, 45.8, 31.2; 19F NMR (376 MHz, DMSO-d6) δ(ppm): −59.0; MS (ESI positive) m/z: 446.1 [M + H]+; [α]D22° = −55 (c = 5.9; Acetone).
(S)-3-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)thioureido)benzenesulfonamide (40b)
Following the general procedure, the product was a white solid 40b, yield 60%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 9.68 (1H, bs), 8.45 (1H, s), 8.30 (1H, s), 8.04 (1H, s), 7.81 (1H, dd, J = 8.94, 2.16 Hz), 7.73 (1H, d, J = 7.70 Hz), 7.57–7.50 (2H. m), 7.40 (2H, bs), 6.66 (1H, d, J = 8.95 Hz), 4.92 (1H, m), 3.86–3.82 (1H, m), 3.62–3.57 (3H, m), 2.41–2.32 (1H, m), 2.17–2.12 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 181.5, 159.2, 146.5, 145.2, 141.0, 134.9, 129.9, 127.4, 126.1 (q, J = 269.94 Hz), 121.8, 120.5, 113.3 (q, J = 33.93 Hz), 107.1, 54.2, 52.8, 45.8, 31.3; MS (ESI positive) m/z: 446.1 [M + H]+; [α]D22° = +50 (c = 6.1; Acetone).
General Synthesis of Compounds 41–46
A mixture of corresponding carbamate (34a-b, 1 equiv) and corresponding amine 30–32 (1 equiv) in acetonitrile was stirred at reflux overnight. Then, water was added and the precipitate was filtered off.
(R)-4-(3-(1-(Pyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (41a)
Following the general procedure, the product was a white solid 41a, yield 51%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.77 (1H, s), 8.11 (1H, d, J = 3.84 Hz), 7.71 (2H, d, J = 8.70 Hz), 7.56 (2H, d, J = 8.79 Hz), 7.53–7.20 (1H, m), 7.20 (2H, bs), 6.72 (1H, d, J = 6.80 Hz), 6.59 (1H, m), 6.50 (1H, d, J = 8.48 Hz), 4.37 (1H, m), 3.67–3.63 (1H, m), 3.51–3.49 (3H, m), 2.27–2.22 (1H, m), 1.99–1.95 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm):157.9, 155.4, 148.8, 144.3, 137.9, 137.1, 127.7, 117.7, 112.3, 107.2, 53.3, 50.1, 45.4, 32.1; MS (ESI positive) m/z: 362.1 [M + H]+.
(R)-3-(3-(1-(Pyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (42a)
Following the general procedure, the product was a white solid 42a, yield 51%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.71 (1H, s), 8.11 (1H, d, J = 4.47 Hz), 8.04 (1H, s), 7.52–7.50 (2H, m), 7.44–7.40 (2H, m), 7.35 (2H, bs), 6.63 (1H, d, J = 6.84 Hz), 6.59 (1H, m), 6.50 (1H, d, J = 8.46 Hz), 4.37 (1H, m), 3.66–3.64 (1H, m), 3.51–3.49 (2H, m), 3.33 (1H, m), 2.29–2.21 (1H, m), 2.01–1.94 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 155.6, 148.8, 145.5, 141.7, 137.9, 136.8, 130.2, 121.4, 119.1, 115.4, 112.3, 107.3, 53.3, 50.1, 45.5, 32.1; MS (ESI positive) m/z: 362.1 [M + H]+; [α]D22° = −49 (c = 2.3; Acetone).
(R)-4-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (43a)
Following the general procedure, the product was a yellow solid 43a, yield 63%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.79 (1H, s), 8.46 (1H, s), 8.25 (1H, m), 7.70 (2H, d, J = 8.70 Hz), 7.56 (2H, d, J = 8.79 Hz), 7.20 (2H, bs), 6.88 (1H, d, J = 4.16 Hz), 6.74 (1H, s), 4.34 (1H, m), 3.58 (2H, m), 3.46 (1H, m), 3.17 (1H, m), 2.22 (1H, m), 1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 155.5, 153.2, 150.6, 144.2, 137.2, 135.9, 132.4, 127.8, 112.8, 55.6, 49.9, 48.0, 31.3; MS (ESI positive) m/z: 407.1 [M + H]+; [α]D22° = −18 (c = 1.7; Acetone) Elemental analysis: calculated: C, 47.29; H, 4.46; N, 20.68; O, 19.68; S, 7.89; found: C, 47.21; H, 4.45; N, 20.62.
(S)-4-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (43b)
Following the general procedure, the product was a yellow solid 43b, yield 98%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.77 (1H, s), 8.46 (1H, dd, J = 4.40, 1.38 Hz), 8.25 (1H, dd, J = 8.02, 1.36 Hz), 7.70 (2H, d, J = 8.72 Hz), 7.56 (2H, d, J = 8.76 Hz), 7.16 (2H, bs), 6.87 (1H, dd, J = 8.02, 4.52 Hz), 6.72 (1H, d, J = 6.37 Hz), 4.34 (1H, m), 3.60 (2H, m), 3.55 (1H, m), 3.18 (1H, dd, J = 11.46, 4.06 Hz), 2.26–2.18 (1H, m), 2.03–1.95 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 155.5, 153.1, 150.6, 144.2, 137.2, 135.9, 127.8, 122.1, 117.8, 112.8, 55.6, 49.9, 47.9, 31.3; MS (ESI positive) m/z: 407.1 [M + H]+; [α]D22° = +16 (c = 1.9; Acetone).
(R)-3-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (44a)
Following the general procedure, the product was a yellow solid 44a, yield 52%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.74 (1H, s), 8.46 (1H, s), 8.25 (1H, m), 8.03 (1H, s), 7.50 (1H,m), 7.43–7.39 (2H, m), 7.33 (2H, bs), 6.87 (1H, s), 6.66 (1H, s), 4.33 (1H, m), 3.58 (2H, m), 3.46 (1H, m), 3.19–3.16 (1H, m), 2.22 (1H, m), 2.02 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 155.7, 153.2, 150.6, 145.5, 141.6, 136.0, 132.4, 130.2, 121.5, 119.2, 115.6, 112.9, 55.6, 50.0, 48.1, 31.3; MS (ESI positive) m/z: 407.1 [M + H]+; [α]D22° = −43 (c = 5.1; Acetone).
(S)-3-(3-(1-(6-Nitropyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (44b)
Following the general procedure, the product was a yellow solid 44b, yield 50%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.72 (1H, s), 8.46 (1H, d, J = 1.58 Hz), 8.25 (1H, d, J = 7.98 Hz), 8.03 (1H, s), 7.51 (1H,m), 7.44–7.40 (2H, m), 7.32 (2H, bs), 6.87 (1H, m), 6.64 (1H, d, J = 5.93 Hz), 4.34 (1H, m), 3.62–3.54 (2H, m), 3.46 (1H, m), 3.19–3.17 (1H, m), 2.25–2.20 (1H, m), 2.02–1.96 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 155.6, 153.1, 150.6, 145.5, 141.5, 135.9, 132.4, 130.1, 121.5, 119.2, 115.5, 112.8, 55.6, 50.0, 48.0, 31.3; MS (ESI positive) m/z: 407.1 [M + H]+; [α]D22° = +40 (c = 5.5; Acetone).
(R)-4-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (45a)
Following the general procedure, the product was a white solid 45a, yield 78%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.78 (1H, bs), 8.44 (1H, s), 7.80 (1H, dd, J = 8.96, 2.16 Hz), 7.71 (2H, d, J = 8.65 Hz), 7.57 (2H. d, J = 8.70 Hz), 7.22 (2H, bs), 6.75 (1H, d, J = 6.72 Hz), 6.64 (1H, d, J = 8.95 Hz), 4.39 (1H, m), 3.75–3.71 (1H, m), 3.59 (2H, m), 3.44 (1H, m), 2.30–2.25 (1H, m), 2.03–1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.3, 155.5, 146.5, 144.3, 137.2, 134.9, 137.2, 134.9, 127.7, 126.1 (q, J = 268.0 Hz), 117.8, 113.3 (q, J = 32.18 Hz), 107.1, 53.4, 50.1, 45.8, 31.9; MS (ESI positive) m/z: 430.1 [M + H]+; [α]D22° = −26 (c = 2.0; Acetone).
(S)-4-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (45b)
Following the general procedure, the product was a white solid 45b, yield 50%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.77 (1H, bs), 8.44 (1H, s), 7.80 (1H, d, J = 8.16 Hz), 7.72 (2H, d, J = 8.43 Hz), 7.57 (2H. d, J = 8.45 Hz), 7.20 (2H, bs), 6.74 (1H, d, J = 6.41 Hz), 6.64 (1H, d, J = 8.87 Hz), 4.39 (1H, m), 3.76–3.72 (1H, m), 3.59 (2H, m), 3.44 (1H, m), 2.30–2.25 (1H, m), 2.03–2.00 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.3, 155.4, 146.5, 144.2, 137.2, 134.8, 130.1, 127.7, 126.1 (q, J = 270.81 Hz), 117.8, 113.2 (q, J = 32.35 Hz), 107.0, 53.4, 50.0, 45.7, 31.8; MS (ESI positive) m/z: 430.1 [M + H]+; [α]D22° = +30 (c = 3.0; Acetone).
(R)-3-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (46a)
Following the general procedure, the product was a white solid 46a, yield 61%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.73 (1H, bs), 8.44 (1H, s), 8.05 (1H, s), 7.80 (1H, d, J = 8.17 Hz), 7.53–7.36 (4H, m), 6.66 (1H, t, J = 8.62 Hz), 4.38 (1H, m), 3.76 (1H, m), 3.58 (2H, m), 3.41 (1H, m), 2.28–2.25 (1H, m), 2.02–2.01 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.3, 155.7, 146.5, 145.5, 141.6, 134.9, 130.2, 126.2 (q, J = 270.01 Hz), 121.5, 119.2, 115.5, 113.3 (q, J = 32.31 Hz), 107.1, 53.4, 50.1, 45.8, 31.9; MS (ESI positive) m/z: 430.1 [M + H]+; [α]D22° = −32 (c = 4.3; Acetone).
(S)-3-(3-(1-(5-(Trifluoromethyl)pyridin-2-yl)pyrrolidin-3-yl)ureido)benzenesulfonamide (46b)
Following the general procedure, the product was a white solid 46b, yield 62%. 1H NMR (400 MHz, DMSO-d6) δ(ppm): 8.71 (1H, bs), 8.44 (1H, s), 8.04 (1H, s), 7.80 (1H, dd, J = 8.92, 2.08 Hz), 7.52 (1H, d, J = 7.93 Hz), 7.42–7.34 (2H, m), 7.34 (2H, bs), 6.66–6.64 (2H, m), 4.39 (1H, m), 3.76–3.73 (1H, m), 3.59 (2H, m), 3.41 (1H, m), 2.32–2.25 (1H, m), 2.04–1.99 (1H, m); 13C NMR (100 MHz, DMSO-d6) δ(ppm): 159.4, 155.7, 146.6, 145.6, 141.7, 134.9, 130.3, 126.2 (q, J = 269.76 Hz), 121.5, 119.2, 115.5, 113.3 (q, J = 32.00 Hz), 107.2, 53.5, 50.2, 45.9, 31.9; MS (ESI positive) m/z: 430.1 [M + H]+; [α]D22° = +37 (c = 2.3; Acetone).
Carbonic Anhydrase Inhibition
An Applied Photophysics stopped-flow instrument was used to assay the CA-catalyzed CO2 hydration activity.31 Phenol red (at a concentration of 0.2 mM) was used as an indicator, working at the absorbance maximum of 557 nm, with 20 mM Hepes (pH 7.4) as a buffer, and 20 mM Na2SO4 (to maintain constant ionic strength), following the initial rates of the CA-catalyzed CO2 hydration reaction for a period of 10–100 s. The CO2 concentrations ranged from 1.7 to 17 mM for the determination of the kinetic parameters and inhibition constants.36 Enzyme concentrations ranged between 5 and 12 nM. For each inhibitor, at least six traces of the initial 5–10% of the reaction were used to determine the initial velocity. The uncatalyzed rates were determined in the same manner and subtracted from the total observed rates. Stock solutions of the inhibitor (0.1 mM) were prepared in distilled–deionized water, and dilutions up to 0.01 nM were done thereafter with the assay buffer. Inhibitor and enzyme solutions were preincubated together for 15 min at room temperature prior to the assay, to allow for the formation of the E–I complex. The inhibition constants were obtained by nonlinear least-squares methods using PRISM 3 and the Cheng-Prusoff equation as reported earlier and represent the mean from at least three different determinations. All CA isoforms were recombinant proteins obtained in-house, as reported earlier.37−39
TRPV1 Assay
SH-SY5Y-TRPV1 cells (kindly provided by Johanna Lilja and Anna Forsby (University of Stockholm, Stockholm, Sweden))40 were cultured in 96 wells. Upon 90% confluence had been reached, the cells were loaded with 5 μM Fluo-4NW for 1 h at 37 °C. The Fluo-4NW fluorescence was measured through cycles (1.7 min each) of excitation at 485 nm and emission at 535 nm (POLARstar Omega BMG LABtech). Briefly, after measuring the basal fluorescence of the plate (four cycles), testing compounds were added to the plate, and the fluorescence was measured for additional 10 cycles; thereafter, 10 μM capsaicin was added with a microinjector and the fluorescence was monitored for an additional 10 cycles. Under these conditions, testing agonists and antagonists were exposed to the cells for 25 min.
Crystallization and X-ray Data Collection
Crystals of hCAII were obtained using the hanging drop vapor diffusion method using a 24-well Linbro plate. A 10 mg/mL solution of hCA II (2 μL) in Tris-HCl 20 mM pH 8.0 was mixed with 2 μL of a solution of 1.5 M sodium citrate and 0.1 M Tris pH 8.0 and was equilibrated against the same solution at 296 K. The complexes were prepared by soaking the hCA II native crystals in the mother liquor solution containing the inhibitors at a concentration of 10 mM for 2 days. All crystals were flash-frozen at 100 K using a solution obtained by adding 15% (v/v) glycerol to the mother liquor solution as a cryoprotectant. Data on crystals of the complexes were collected using synchrotron radiation at the XRD2 beamline at Elettra Synchrotron (Trieste, Italy) with a wavelength of 1.000 Å and a DECTRIS Pilatus 6 M detector. Data were integrated and scaled using the program energy-dispersive X-ray spectrum (XDS).41 Data processing statistics are shown in the Supporting Information.
Structure Determination
The crystal structure of hCA II (PDB accession code: 4FIK) without solvent molecules and other heteroatoms was used to obtain initial phases using Refmac5;42 5% of the unique reflections were selected randomly and excluded from the refinement data set for the purpose of Rfree calculations. The initial |Fo – Fc| difference electron density maps unambiguously showed the inhibitor molecules. The inhibitor was introduced in the model with 1.0 occupancy. Refinements proceeded using normal protocols of positional, isotropic atomic displacement parameters alternating with manual building of the models using COOT.43 The quality of the final models was assessed with COOT and RAMPAGE.44 Crystal parameters and refinement data are summarized in the Supporting Information (SI). Atomic coordinates were deposited in the Protein Data Bank (PDB) accession code: 8BJX; 8BOE. Graphical representations were generated with Chimera.45
In Vivo Experiment
Animals
Male CD-1 albino mice (Envigo, Varese, Italy) weighing approximately 22–25 g at the beginning of the experimental procedure were used. The animals were housed in Ce.S.A.L (Centro Stabulazione Animali da Laboratorio, University of Florence) and used at least 1 week after their arrival. Ten mice were housed per cage (size 26 × 41 cm). The animals were fed a standard laboratory diet and tap water ad libitum and kept at 23 ± 1 °C with a 12 h light/dark cycle, light at 7 a.m. All animal manipulations were carried out according to the Directive 2010/63/EU of the European Parliament and of the European Union council (22 September 2010) on the protection of animals used for scientific purposes. The ethical policy of the University of Florence complies with the Guide for the Care and Use of Laboratory Animals of the US National Institutes of Health (NIH Publication No. 85-23, revised 1996; University of Florence assurance number: A5278-01). Formal approval to conduct the experiments described was obtained from the Animal Subjects Review Board of the University of Florence. Experiments involving animals have been reported according to ARRIVE guideline.46 All efforts were made to minimize animal suffering and to reduce the number of animals used. Protocol number of ethical assessment 229/2020-PR.
Oxaliplatin-Induced Neuropathic Pain Model and Pharmacological Treatments
Mice treated with oxaliplatin (2.4 mg/kg) were administered intraperitoneally (i.p.) on days 1–2, 5–9, and 12–14 (10 i.p. injections) according to Cavaletti and colleagues47 with minor modifications concerning the days of oxaliplatin administration.48 Oxaliplatin was dissolved in 5% glucose solution. Control animals received an equivalent volume of vehicle. Behavioral tests were performed starting from day 15 when neuropathy was well established. Compounds 12a, 37a, 39a, and 39b were suspended in 1% carboxymethylcellulose sodium salt (CMC; Sigma-Aldrich, Milan, Italy) and per os (p.o.) acutely administered in a range dose of 10–100 mg/kg. Behavioral tests were carried out before and after (15, 30, 45, and 60 min) compound’s injection.
Cold Plate Test
Thermal allodynia was assessed using the cold plate test. With minimal animal-handler interaction, mice were taken from home cages and placed onto the surface of the cold plate (Ugo Basile, Varese, Italy) maintained at a constant temperature of 4 ± 1 °C. Ambulation was restricted by a cylindrical Plexiglas chamber (diameter: 10 cm, height: 15 cm), with open top. A timer controlled by foot peddle began timing response latency from the moment the mouse was placed onto the cold plate. Pain-related behavior (licking of the hind paw) was observed, and the time (seconds) of the first sign was recorded. The cutoff time of the latency of paw lifting or licking was set at 30 s.
Statistical Analysis
Behavioral measurements were performed on 12 mice for each treatment carried out in two different experimental sets. Results were expressed as mean ± S.E.M. The analysis of variance of behavioral data was performed by one-way ANOVA, and a Bonferroni’s significant difference procedure was used as post hoc comparison. P values of less than 0.05 or 0.01 were considered significant. Investigators were blind to all experimental procedures. Data were analyzed using the “Origin 9” software (OriginLab, Northampton).
Glossary
Abbreviations Used
- AAZ
acetazolamide
- CA
Carbonic Anhydrase
- CAI
Carbonic Anhydrase Inhibitors
- CNS
central nervous system
- DRG
dorsal root ganglion
- NSAIDs
nonsteroidal anti-inflammatory drugs
- OINP
oxaliplatin-induced neuropathy
- TLC
thin-layer chromatography
- TRPV1
Transient Receptor Potential Vanilloid 1
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acs.jmedchem.2c01911.
Author Contributions
The manuscript was written through contributions of all authors. All authors have given approval to the final version of the manuscript. The authors will release the atomic coordinates upon article publication.
The authors declare no competing financial interest.
Supplementary Material
References
- Siegel R. L.; Miller K. D.; Fuchs H. E.; Jemal A. Cancer Statistics, 2021. Ca-Cancer J. Clin. 2021, 71, 7–33. 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- Jemal A.; Ward E. M.; Johnson C. J.; Cronin K. A.; Ma J.; Ryerson B.; Mariotto A.; Lake A. J.; Wilson R.; Sherman R. L.; Anderson R. N.; Henley S. J.; Kohler B. A.; Penberthy L.; Feuer E. J.; Weir H. K. Annual Report to the Nation on the Status of Cancer, 1975-2014, Featuring Survival. J. Natl. Cancer Inst. 2017, 109, djx030 10.1093/jnci/djx030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C.; Xu C.; Gao X.; Yao Q. Platinum-based drugs for cancer therapy and anti-tumor strategies. Theranostics 2022, 12, 2115–2132. 10.7150/thno.69424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wlodarczyk M. T.; Dragulska S. A.; Camacho-Vanegas O.; Dottino P. R.; Jarzęcki A. A.; Martignetti J. A.; Mieszawska A. J. Platinum (II) complex-nuclear localization sequence peptide hybrid for overcoming platinum resistance in cancer therapy. ACS Biomater. Sci. Eng. 2018, 4, 463–467. 10.1021/acsbiomaterials.7b00921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mjos K. D.; Orvig C. Metallodrugs in medicinal inorganic chemistry. Chem. Rev. 2014, 114, 4540–4563. 10.1021/cr400460s. [DOI] [PubMed] [Google Scholar]
- Mills S. E.; Nicolson K. P.; Smith B. H. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br. J. Anaesth. 2019, 123, e273–e283. 10.1016/j.bja.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehky T. J.; Leonard G. D.; Wilson R. H.; Grem J. L.; Floeter M. K. Oxaliplatin-induced neurotoxicity: acute hyperexcitability and chronic neuropathy. Muscle Nerve 2004, 29, 387–392. 10.1002/mus.10559. [DOI] [PubMed] [Google Scholar]
- Sisignano M.; Baron R.; Scholich K.; Geisslinger G. Mechanism-based treatment for chemotherapy-induced peripheral neuropathic pain. Nat. Rev. Neurol. 2014, 10, 694–707. 10.1038/nrneurol.2014.211. [DOI] [PubMed] [Google Scholar]
- Carozzi V. A.; Canta A.; Chiorazzi A. Chemotherapy-induced peripheral neuropathy: What do we know about mechanisms?. Neurosci. Lett. 2015, 596, 90–107. 10.1016/j.neulet.2014.10.014. [DOI] [PubMed] [Google Scholar]
- Hu S.; Huang K. M.; Adams E. J.; Loprinzi C. L.; Lustberg M. B. Recent developments of novel pharmacologic therapeutics for prevention of chemotherapy-induced peripheral neuropathy. Clin. Cancer Res. 2019, 25, 6295–6301. 10.1158/1078-0432.CCR-18-2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sałat K. Chemotherapy-induced peripheral neuropathy-part 2: focus on the prevention of oxaliplatin-induced neurotoxicity. Pharmacol Rep. 2020, 72, 508–527. 10.1007/s43440-020-00106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenzieri A.; Riva B.; Rigolio R.; Chiorazzi A.; Pozzi E.; Ballarini E.; Cavaletti G.; Genazzani A. A. Oxaliplatin-induced neuropathy occurs through impairment of haemoglobin proton buffering and is reversed by carbonic anhydrase inhibitors. Pain 2020, 161, 405–415. 10.1097/j.pain.0000000000001722. [DOI] [PubMed] [Google Scholar]
- Yang Y.; Zhao B.; Gao X.; Sun J.; Ye J.; Li J.; Cao P. Targeting strategies for oxaliplatin-induced peripheral neuropathy: clinical syndrome, molecular basis, and drug development. J. Exp. Clin. Cancer Res. 2021, 40, 331 10.1186/s13046-021-02141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. The functional regulation of TRPV1 and its role in pain sensitization. Neurochem. Res. 2008, 33, 2008–2012. 10.1007/s11064-008-9750-5. [DOI] [PubMed] [Google Scholar]
- Benítez-Angeles M.; Morales-Lázaro S. L.; Juárez-González E.; Rosenbaum T. TRPV1: Structure, Endogenous Agonists, and Mechanisms. Int. J. Mol. Sci. 2020, 21, 3421. 10.3390/ijms21103421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamps D.; Vriens J.; de Hoon J.; Voets T. TRP Channel Cooperation for Nociception: Therapeutic Opportunities. Annu. Rev. Pharmacol. Toxicol. 2021, 61, 655–677. 10.1146/annurev-pharmtox-010919-023238. [DOI] [PubMed] [Google Scholar]
- Iftinca M.; Defaye M.; Altier C. TRPV1-Targeted Drugs in Development for Human Pain Conditions. Drugs 2021, 81, 7–27. 10.1007/s40265-020-01429-2. [DOI] [PubMed] [Google Scholar]
- Knotkova H.; Pappagallo M.; Szallasi A. Capsaicin (TRPV1 Agonist) therapy for pain relief: farewell or revival?. Clin. J. Pain 2008, 24, 142–154. 10.1097/AJP.0b013e318158ed9e. [DOI] [PubMed] [Google Scholar]
- Brown D. C. Resiniferatoxin: The Evolution of the ″Molecular Scalpel″ for Chronic Pain Relief. Pharmaceuticals 2016, 9, 47. 10.3390/ph9030047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ann J.; Kim H. S.; Thorat S. A.; Kim H.; Ha H. J.; Choi K.; Kim Y. H.; Kim M.; Hwang S. W.; Pearce L. V.; et al. Discovery of Nonpungent Transient Receptor Potential Vanilloid 1 (TRPV1) Agonist as Strong Topical Analgesic. J. Med. Chem. 2020, 63, 418–424. 10.1021/acs.jmedchem.9b01046. [DOI] [PubMed] [Google Scholar]
- Aghazadeh Tabrizi M.; Baraldi P. G.; Baraldi S.; Gessi S.; Merighi S.; Borea P. A. Medicinal Chemistry, Pharmacology, and Clinical Implications of TRPV1 Receptor Antagonists. Med. Res. Rev. 2017, 37, 936–983. 10.1002/med.21427. [DOI] [PubMed] [Google Scholar]
- Supuran C. T. Carbonic anhydrase inhibitors and their potential in a range of therapeutic areas. Expert Opin. Ther. Pat. 2018, 28, 709–712. 10.1080/13543776.2018.1523897. [DOI] [PubMed] [Google Scholar]
- McDonald P. C.; Winum J. Y.; Supuran C. T.; Dedhar S. Recent developments in targeting carbonic anhydrase IX for cancer therapeutics. Oncotarget 2012, 3, 84–97. 10.18632/oncotarget.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrino E.; Supuran C. T. Novel approaches for designing drugs that interfere with pH regulation. Expert Opin. Drug Discovery 2019, 14, 231–248. 10.1080/17460441.2019.1567488. [DOI] [PubMed] [Google Scholar]
- Supuran C. T.; Capasso C. Biomedical applications of prokaryotic carbonic anhydrases. Expert Opin. Ther. Pat. 2018, 28, 745–754. 10.1080/13543776.2018.1497161. [DOI] [PubMed] [Google Scholar]
- Asiedu M.; Ossipov M. H.; Kaila K.; Price T. J. Acetazolamide and midazolam act synergistically to inhibit neuropathic pain. Pain 2010, 148, 302–308. 10.1016/j.pain.2009.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asiedu M. N.; Mejia G. L.; Hübner C. A.; Kaila K.; Price T. J. Inhibition of carbonic anhydrase augments GABAA receptor-mediated analgesia via a spinal mechanism of action. J. Pain 2014, 15, 395–406. 10.1016/j.jpain.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant J. L.; Gieling R. G.; Meredith S. L.; Allen T. J.; Walker L.; Telfer B. A.; Supuran C. T.; Williams K. J.; White A. Novel carbonic anhydrase IX-targeted therapy enhances the anti-tumour effects of cisplatin in small cell lung cancer. Int. J. Cancer 2018, 142, 191–201. 10.1002/ijc.31042. [DOI] [PubMed] [Google Scholar]
- Tanini D.; Carradori S.; Capperucci A.; Lupori L.; Zara S.; Ferraroni M.; Ghelardini C.; Mannelli L.; Micheli L.; Lucarini E.; Carta F.; Angeli A.; Supuran C. T. Chalcogenides-incorporating carbonic anhydrase inhibitors concomitantly reverted oxaliplatin-induced neuropathy and enhanced antiproliferative action. Eur. J. Med. Chem. 2021, 225, 113793 10.1016/j.ejmech.2021.113793. [DOI] [PubMed] [Google Scholar]
- Gunthorpe M. J.; Hannan S. L.; Smart D.; Jerman J. C.; Arpino S.; Smith G. D.; Brough S.; Wright J.; Egerton J.; Lappin S. C.; Holland V. A.; Winborn K.; Thompson M.; Rami H. K.; Randall A.; Davis J. B. Characterization of SB-705498, a potent and selective vanilloid receptor-1 (VR1/TRPV1) antagonist that inhibits the capsaicin-, acid-, and heat-mediated activation of the receptor. J. Pharmacol. Exp. Ther. 2007, 321, 1183–1192. 10.1124/jpet.106.116657. [DOI] [PubMed] [Google Scholar]
- Khalifah R. G. The carbon dioxide hydration activity of carbonic anhydrase. I. Stop flow kinetic studies on the native human isoenzymes B and C. J. Biol. Chem. 1971, 246, 2561–2573. 10.1016/S0021-9258(18)62326-9. [DOI] [PubMed] [Google Scholar]
- Berrino E.; Michelet B.; Martin-Mingot A.; Carta F.; Supuran C. T.; Thibaudeau S. Modulating the Efficacy of Carbonic Anhydrase Inhibitors through Fluorine Substitution. Angew. Chem., Int. Ed. 2021, 60, 23068–23082. 10.1002/anie.202103211. [DOI] [PubMed] [Google Scholar]
- Alterio V.; Di Fiore A.; D’Ambrosio K.; Supuran C. T.; De Simone G. Multiple binding modes of inhibitors to carbonic anhydrases: how to design specific drugs targeting 15 different isoforms?. Chem. Rev. 2012, 112, 4421–4468. 10.1021/cr200176r. [DOI] [PubMed] [Google Scholar]
- Angeli A.; Di Cesare Mannelli L.; Ghelardini C.; Peat T. S.; Bartolucci G.; Menicatti M.; Carta F.; Supuran C. T. Benzensulfonamides bearing spyrohydantoin moieties act as potent inhibitors of human carbonic anhydrases II and VII and show neuropathic pain attenuating effects. Eur. J. Med. Chem. 2019, 177, 188–197. 10.1016/j.ejmech.2019.05.058. [DOI] [PubMed] [Google Scholar]
- Angeli A.; di Cesare Mannelli L.; Lucarini E.; Peat T. S.; Ghelardini C.; Supuran C. T. Design, synthesis and X-ray crystallography of selenides bearing benzenesulfonamide moiety with neuropathic pain modulating effects. Eur. J. Med. Chem. 2018, 154, 210–219. 10.1016/j.ejmech.2018.05.026. [DOI] [PubMed] [Google Scholar]
- Supuran C. T. Carbonic anhydrases: novel therapeutic applications for inhibitors and activators. Nat. Rev. Drug Discovery 2008, 7, 168–181. 10.1038/nrd2467. [DOI] [PubMed] [Google Scholar]
- Angeli A.; Ferraroni M.; Supuran C. T. Famotidine, an Antiulcer Agent, Strongly Inhibits Helicobacter pylori and Human Carbonic Anhydrases. ACS Med. Chem. Lett. 2018, 9, 1035–1038. 10.1021/acsmedchemlett.8b00334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angeli A.; Trallori E.; Carta F.; Di Cesare Mannelli L.; Ghelardini C.; Supuran C. T. Heterocoumarins Are Selective Carbonic Anhydrase IX and XII Inhibitors with Cytotoxic Effects against Cancer Cells Lines. ACS Med. Chem. Lett. 2018, 9, 947–951. 10.1021/acsmedchemlett.8b00362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angeli A.; Peat T. S.; Bartolucci G.; Nocentini A.; Supuran C. T.; Carta F. Intramolecular oxidative deselenization of acylselenoureas: a facile synthesis of benzoxazole amides and carbonic anhydrase inhibitors. Org. Biomol. Chem. 2016, 14, 11353–11356. 10.1039/C6OB02299E. [DOI] [PubMed] [Google Scholar]
- Lilja J.; Laulund F.; Forsby A. Insulin and insulin-like growth factor type-I up-regulate the vanilloid receptor-1 (TRPV1) in stably TRPV1-expressing SH-SY5Y neuroblastoma cells. J. Neurosci. Res. 2007, 85, 1413–1419. 10.1002/jnr.21255. [DOI] [PubMed] [Google Scholar]
- Leslie A. G. W.; Powell H. R.. Procesing diffraction data with mosflm. In Evolving Methods for Macromolecular Crystallography; Read R. J.; Sussman J. L., Eds.; NATO Science series; Springer: Dordrecht, 2007; Vol. 245, p 4151. [Google Scholar]
- Murshudov G. N.; Vagin A. A.; Dodson E. J. Refinement of macromolecular structures by the maximum-likelihood method. Acta Crystallogr., Sect. D: Biol. Crystallogr. 1997, 53, 240–255. 10.1107/S0907444996012255. [DOI] [PubMed] [Google Scholar]
- Emsley P.; Lohkamp B.; Scott W.; Cowtan K. Features and development of Coot. Acta Crystallogr., Sect. D: Biol. Crystallogr. 2010, 66, 486–501. 10.1107/S0907444910007493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovell S. C.; Davis I. W.; Arendall W. B. III; de Bakker P.I.W.; Word J. M.; Prisant M. G.; Richardson J. S.; Richardson D. C. Structure validation by Cα geometry: ϕ,ψ and Cβ deviation. Proteins 2003, 50, 437–450. 10.1002/prot.10286. [DOI] [PubMed] [Google Scholar]
- Pettersen E. F.; Goddard T. D.; Huang C. C.; Couch G. S.; Greenblatt D. M.; Meng E. C.; Ferrin T. E. UCSF Chimera—a visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]
- McGrath J. C.; Lilley E. Implementing guidelines on reporting research using animals (ARRIVE etc.): new requirements for publication in BJP. Br. J. Pharmacol. 2015, 172, 3189–3193. 10.1111/bph.12955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavaletti G.; Tredici G.; Petruccioli M. G.; Dondè E.; Tredici P.; Marmiroli P.; Minoia C.; Ronchi A.; Bayssas M.; Etienne G. G. Effects of different schedules of oxaliplatin treatment on the peripheral nervous system of the rat. Eur. J. Cancer 2001, 37, 2457–2463. 10.1016/S0959-8049(01)00300-8. [DOI] [PubMed] [Google Scholar]
- Micheli L.; Di Cesare Mannelli L.; Rizzi A.; Guerrini R.; Trapella C.; Calò G.; Ghelardini C. Intrathecal administration of nociceptin/orphanin FQ receptor agonists in rats: A strategy to relieve chemotherapy-induced neuropathic hypersensitivity. Eur. J. Pharmacol. 2015, 766, 155–162. 10.1016/j.ejphar.2015.10.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.