Abstract
Background: Vancomycin is a glycopeptide antibiotic with a high risk of acute liver injury. Resveratrol is believed to protect the liver against toxicity.
Aim: To investigate the ability of resveratrol to attenuate vancomycin-induced liver toxicity in rats injected with vancomycin.
Method: Twenty-four adult male Wistar rats were distributed into three groups. The control group received only a vehicle, while the treated group received either vancomycin 200 (mg/kg, i. p.) only or vancomycin (200 mg/kg, i. p.) with resveratrol (20 mg/kg, oral gavage). All groups received their dose once daily for 7 days. Hepatic damage was assessed by measuring biochemical parameter levels in serum, aspartate transaminase (AST), alanine transaminase (ALT), alkaline phosphatase (ALP), and lactate dehydrogenase (LDH). Also, antioxidants and inflammation biomarkers such as Interleukin-6 (IL-6), malondialdehyde (MDA), nitric oxide (NO), and glutathione (GSH) were measured. Furthermore, the vancomycin-induced pathological changes in the liver were evaluated by histopathological studies.
Results: In the vancomycin-treated group, hepatic serum biomarkers such as AST, ALT, ALP, IL-6, and MDA were elevated, while NO and GSH were depleted. However, resveratrol co-treatment with vancomycin prevented the elevation of AST, ALT, ALP, IL-6, and MDA and it protected the liver from NO and GSH depletion. Also, regarding vancomycin-induced degeneration of hepatocytes, resveratrol co-treatment with vancomycin prevented such degeneration and improved mononuclear cells in the liver.
Conclusion: The results showed that oral administration of resveratrol has a significant hepatoprotective effect against vancomycin-induced hepatotoxicity.
Keywords: vancomycin, resveratrol, hepatotoxicity, hepatoprotection, glycopeptide
Introduction
Many drugs are known to produce liver injury, and these adverse hepatic events usually result in severe liver injury if not treated properly (Bissell et al., 2001). It has been estimated that drug-induced liver failure represents half of the cases of all forms of acute and chronic liver disease (Kaplowitz, 2001). Approximately 10% of chronic hepatitis cases occur due to drug use, and 5% from hospital admissions, while 50% of acute liver failure cases occur due to drug use (Pandit et al., 2012). Hepatotoxicity associated with antibiotics is asymptomatic and usually presents mild hepatic injury (Thiim and Friedman, 2003). Vancomycin is a glycopeptide antibiotic with known bactericidal activity, and it is considered the drug of choice for treating methicillin-resistant Staphylococcus aureus infections (David and Daum, 2010; Steinmetz et al., 2015). However, several side effects have been reported with vancomycin, such as hypotension, phlebitis, nephrotoxicity, and hepatotoxicity (Badran et al., 2011; Bamgbola, 2016).
Moreover, a few reports have shown that chronic use of glycopeptide antibiotics has the potential to elevate liver enzymes and induce hepatotoxicity (Cadle et al., 2006; Chen et al., 2011; Brunetti et al., 2020). However, data to support the influence of vancomycin on liver dysfunction are limited, and the mechanism of vancomycin-induced hepatotoxicity has not been studied effectively. Many risk factors contribute to vancomycin-induced hepatotoxicities, such as long-term treatments, high doses, obesity, patient age, and overall health (Larrey, 2002; Breedt et al., 2005; Kohno et al., 2007; Florescu et al., 2008). Moreover, the hepatic injury associated with vancomycin could also be due to sepsis, bacterial endotoxins, fever, or hemolysis (Sibai, 2004; Shah et al., 2010; Kouijzer et al., 2021). While different strategies have been suggested to reduce any potential risk of hepatotoxicity associated with vancomycin treatment (Aldaz et al., 2000; Hwang et al., 2015; Regal et al., 2019; Tsutsuura et al., 2021), the exact mechanism for this injury is not fully understood. Several studies have suggested that vancomycin-induced toxicity could be due to several factors, including the generation of free radicals, oxidative stress, and inflammation, which cause liver injury in animal studies (Sahin et al., 2006; El Bohi et al., 2021). In addition, reactive oxygen species (ROS) are usually generated within cells, leading to the initiation of oxidative stress-related intermediates, which contribute to chronic inflammation and liver fibrogenesis (Bataller and Brenner, 2005; Friedman, 2008; Novo and Parola, 2008). Therefore, herbal compounds with antioxidant and anti-inflammatory properties have been considered.
Indeed, cumulative reports have suggested that herbal compounds have a great potential to attenuate drug-induced liver toxicity due to their antioxidant and anti-inflammatory properties (Abou Seif, 2016; Parthasarathy and Evan Prince, 2021). Hence, many herbal compounds have been used as traditional medicines for liver disorders (Ali et al., 2008; Zhang et al., 2018; Philips et al., 2020; Das et al., 2022). In addition, these are potential sources of new therapeutic agents that could be used to prevent hepatic injuries. For example, resveratrol has long been known to have antioxidant and anti-inflammatory effects. Moreover, researchers have recently become more interested in resveratrol, from its ability to extend human lifespans to its effect on chemoprevention, cardiovascular diseases, and neurodegenerative disorders, as reported in several studies (Gescher and Steward, 2003; Srivastava et al., 2013; Pourhanifeh et al., 2019; Banez et al., 2020; Labban et al., 2021a; Labban et al., 2021b). The antioxidant properties of resveratrol have been demonstrated in several in vitro studies. The antioxidant property of resveratrol has been demonstrated by inhibiting nicotinamide adenine dinucleotide phosphate oxidases, which inhibit the production of reactive oxygen species (ROS) (Halliwell, 2007; Yousefian et al., 2019). As well as protecting cells from oxidative stress, resveratrol also promotes the expression of antioxidative enzymes and their substrates (Miguel et al., 2021; Santos et al., 2021). Recently, it has been suggested that resveratrol has hepatoprotection properties through its anti-inflammatory and antioxidant effects (Chupradit et al., 2022; Ma et al., 2022; Tong et al., 2022). It has also been reported that resveratrol attenuates acetaminophen toxic metabolite N-acetyl-p-benzoquinone-imine and facilitates liver regeneration by modulating the silent mating type information regulation two homolog (SIRT1), tumor protein P53, and Tumor Necrosis Factor-alpha (TNF-α) (Sener et al., 2006; Wang et al., 2015). Moreover, resveratrol has been shown to improve glutathione (GSH) levels and antioxidant enzyme activities, and to decrease ROS production in liver tissues (Bujanda et al., 2008; Rivera et al., 2008; Rubiolo and Vega, 2008; Sebai et al., 2010). Also, one study reported that the thioacetamide-induced hepatotoxic effect associated with TNF-α and iNOS elevation was inhibited by resveratrol (Ebrahim et al., 2022).
This study investigates the effect of high doses of vancomycin administered to induce liver toxicity. A few studies have investigated similar regimens and found that high doses of vancomycin were associated with elevated levels of liver enzymes, the tissue activities of catalase, superoxide dismutase activities, lipid peroxidation, and malondialdehyde (MDA) (Ahmida, 2012; Çağlayan et al., 2019; El Bohi et al., 2021). Moreover, this research investigates the ability of resveratrol to attenuate vancomycin-induced liver toxicity through several biomarkers, such as liver tissues, inflammatory mediators, liver enzymes, and antioxidant property markers.
Materials and methods
Drugs
Resveratrol (ProHealth, United States) and vancomycin (Medis, Tunisia) were used in the study. All other chemicals and reagents used were of analytical grade. Resveratrol and vancomycin were dissolved in a saline solution (0.9% NaCl) as a vehicle for both drugs.
Dose selection
The vancomycin dose was based on several recent studies using 200 mg/kg, i. p. to induce hepatotoxicity (Kucukler et al., 2020) and nephrotoxicity (Ahmida, 2012) once daily for seven consecutive days. The resveratrol dose was based on several studies using the same dose against several compounds, such as dimethylnitrosamine (Lee et al., 2010) and concanavalin (Zhou et al., 2015).
Animals
Twenty-four male adult Wistar rats (weighing 170–207 g) were used. The animals were housed in plastic cages (4 rats per cage) under a 12 h light/12 h dark schedule in a humidity-controlled room and were fed a normal diet. They had access to food and water ad libitum and were monitored daily to ensure proper animal welfare. The rats were acclimatized for 1 week before starting the experiment. Then, the rats were distributed into three groups (n = 8 in each group). The rats received only a vehicle in the first group (control). In the second group, vancomycin, the rats received vancomycin (200 mg/kg, i. p.) once daily for seven consecutive days. In the last group, vancomycin + resveratrol, the rats received vancomycin (200 mg/kg, i. p.) and resveratrol (20 mg/kg, oral gavage) once daily for seven consecutive days. All the treatments were carried out within 7 days, and the animals were euthanized using CO2 and sacrificed on the eighth day. The tissue and serum samples were collected, homogenized, centrifuged, for analysis.
Measurement of biochemical parameters
The serum samples were used for the measurement of all biochemical parameters. The usage of serum samples was based on several reportes that have useed similar methods to assess hepatic function. Aspartate transaminase (AST), Alanine transferase (ALT) as reported in (Yin et al., 2019), Alkaline phosphatase (ALP) (Ibrahim et al., 2020), Interleukin-6 (IL-6) (Xia et al., 2019), nitric oxide (NO) (Fathy et al., 2019), GSH (Ibrahim et al., 2020) and MDA (Omara et al., 2021).
Markers of liver tissue damage
The serum samples were analyzed using assay kits and ELISA for liver functions. Aspartate transaminase (AST), Alanine transferase (ALT) and Alkaline phosphatase (ALP) were assessed using ELISA kits (MyBioSource kits catalog: MBS269614, MBS264975, MBS011598, MBS726781; MyBioSource, Inc.) A centrifuge was then performed at approximately 1000× g for 15 min. Serum was collected, and the assay was immediately performed according to the manufacturer’s recommendations (MyBioSource, Inc.). A standard curve was established using a series diluent. A Microplate reader (450 nm detection wavelength filter, 570 nm or 630 nm correction wavelength filters) was used to perform all the tests.
Markers of inflammation
Interleukin-6 (IL-6) and nitric oxide (NO) levels in the serum were measured with the fully automatic ELISA DSX best 2000® microtiter plate and the ELISA kits. A centrifuge was then performed at approximately 1000× g for 15 min. Serum was collected, and the assay was immediately performed according to the manufacturer’s recommendations (MyBioSource, Inc.).
Markers of antioxidant and prooxidant
GSH and MDA levels in the serum were measured using an ELISA DSX best 2000® microtiter plate and the ELISA kits. In a serum separator tube, the serum was clotted for 2 hours at room temperature and overnight at 2°C–8°C. A centrifuge was then performed at approximately 1000× g for 15 min. Serum was collected, and the assay was immediately performed according to the manufacturer’s recommendations (MyBioSource, Inc.). A Microplate reader (450 nm detection wavelength filter) was used to perform all the tests.
Histopathology
The liver tissues were used for the histopathological assessment and prepared in 10% formalin solution for 2 days. In addition, the tissue was embedded in paraffin blocks following routine tissue tracking procedures. Finally, Hematoxylin and eosin stains were used to stain the slides. Masson’s Trichrome method was employed, which involves deparaffinizing and rehydrating the liver in descending series of alcohols before staining them with Biebrich scarlet-acid fuchsin solution. A solution of phosphomolybdic-phosphotungstic acid was then used to differentiate the sections.
Statistical analysis
Statistical analyses were performed using GraphPad Prism™ (v9.3.1). Data were expressed as mean ± standard error of the mean. A one-way ANOVA, followed by Tukey’s post hoc test, was used for comparisons. A p-value of <0.05 was considered statistically significant.
Results
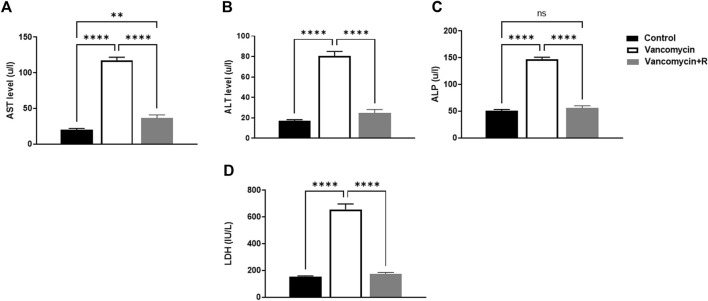
Measured levels of AST, ALT, ALP, and LDH
The effect of vancomycin on AST, ALT, ALP and LDH was observed in the rats’ serum. The one-way ANOVA test revealed a significant main effect on the AST serum levels [F (2, 21) = 216.0, p < 0.0001, Figure 1A]. Further analysis using Tukey’s multiple comparisons test revealed that rats injected with only vancomycin had significantly increased levels of AST compared to the control group (p < 0.0001). Interestingly, the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity. In addition, the vancomycin + resveratrol group of rats showed a significant increase in AST levels, p = 0.0083, compared to the control group.
FIGURE 1.
(A) Aspartate transaminase (AST) levels in u/l, (B) Alanine aminotransferase (ALT) in u/l, (C) Alkaline phosphatase (ALP) in unit/liter (u/l), and (D) lactate dehydrogenase (LDH) (IU/L), were measured in the control rats, rats injected with vancomycin only, and rats injected with vancomycin and resveratrol. Significant difference: ns = non-significant, **p < 0.001 ****p < 0.0001.
Moreover, vancomycin had a significant main effect on the ALT serum levels in the groups [F (2, 21) = 124.0, p < 0.0001, Figure 1B]. Further analysis using Tukey’s multiple comparisons test revealed that the control group rats displayed no change in ALT, p = 0.1949. However, the rats injected with only vancomycin displayed a significant increase in ALT compared to the control group (p < 0.0001). Interestingly, the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity.
Another significant main effect on ALP serum levels in the groups [F (2, 21) = 209.3, p < 0.0001, Figure 1C]. Further analysis using Tukey’s multiple comparisons test revealed that the control rats displayed no change in ALP, p = 0.5888. The rats injected with vancomycin showed a significant increase in ALP compared to the control group (p < 0.0001), and the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity.
Moreover, significant main effect on LDH serum levels in the groups [F (2, 21) = 130.9, p < 0.0001, Figure 1D]. Additional analysis using Tukey’s multiple comparisons tests indicated that the control group rats had no change in LDH, p = 0.8200. However, the rats injected with only vancomycin displayed a significant increase in LDH compared to the control group (p < 0.0001). Remarkably, resveratrol demonstrated a protective role against vancomycin-induced toxicity.
Measured levels of IL-6 and NO
The effect of vancomycin on IL-6 and NO levels was observed in the rats’ serum. The one-way ANOVA test revealed that vancomycin had a significant main effect on the IL-6 serum levels in the groups F (2, 21) = 141.8, p < 0.0001, Figure 2A. Further analysis using Tukey’s multiple comparisons test revealed that the control rats displayed no change in IL-6, p = 0.9185. However, the rats injected with only vancomycin had a significant increase in IL-6 compared to the control group (p < 0.0001). Interestingly, the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity.
FIGURE 2.
Interleukin-6 (IL-6) levels in ng/ml and (B) nitric oxide (NO) levels in parts per million (ppb) were measured in the control rats, rats injected with vancomycin only, and rats injected with vancomycin and resveratrol. Significant difference: ****p < 0.0001.
The significant main effect on NO serum levels in the groups [F (2, 21) = 118.3, p < 0.0001, Figure 2B]. Tukey’s multiple comparisons test revealed that the control group rats displayed no change in NO serum levels, p = 0.6613. However, the rats injected with only vancomycin showed a significant NO increase compared to the control group (p < 0.0001). Remarkably, the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity.
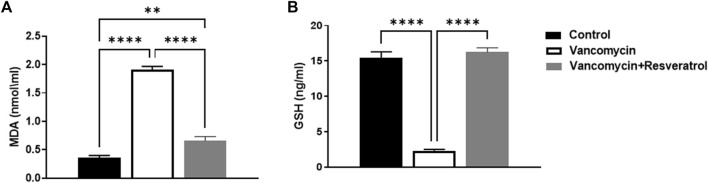
Measured levels of MDA and GSH
The effect of vancomycin on MDA was observed in the rats’ serum. A further one-way ANOVA test showed that vancomycin had a significant main effect on the MDA serum levels in the groups [F (2, 21) = 190.2, p < 0.0001, Figure 3A]. Also, Tukey’s multiple comparisons test revealed that the control group rats displayed a significant change in MDA serum levels, p < 0.0057. Again, the rats injected with only vancomycin displayed a significant increase in LDH compared to the control group (p < 0.0001), while the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity.
FIGURE 3.
(A) Malondialdehyde (MDA) (nmol/ml) and (B) Glutathione (GSH) levels in ng/ml were measured in the control rats, rats injected with vancomycin only, and rats injected with vancomycin and resveratrol. Significant difference: **p < 0.001; ****p < 0.0001.
The effect of vancomycin on GSH levels was observed in rats’ serum. The test revealed a significant main effect on GSH serum levels in the groups [F (2, 21) = 167.3 < 0.0001, Figure 3B]. Further analysis using Tukey’s multiple comparisons test revealed that the control group rats displayed no change in GSH, p = 0.5894. However, rats injected with only vancomycin displayed a significant decrease in GSH compared to the control group (p < 0.0001). Interestingly, the rats injected with resveratrol and vancomycin were protected against vancomycin-induced toxicity.
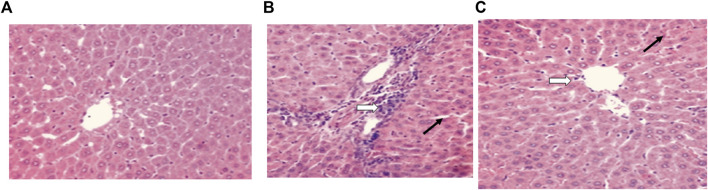
Histopathological results
For the control group, a microscopic examination of the liver revealed a normal appearance, as shown in Figure 4A. For the control + vancomycin group, liver-intralobular mononuclear inflammatory infiltrations and Mallory bodies were evident due to the degeneration of hepatocytes, as shown in Figure 4B. For the vancomycin + resveratrol group, the liver showed a marked improvement in the mononuclear cells, as shown in Figure 4C.
FIGURE 4.
Histopathological liver evaluation in (A) control rats, (B) rats injected with vancomycin only, liver-Intralobular mononuclear inflammatory infiltrations (white arrow), and Mallory bodies (black arrow) due to degeneration of hepatocytes and increased vacuolation in the cytoplasm of hepatocytes appeared as indistinct clear vacuoles (black arrow) indicate glycogen infiltration and (C) rats injected with vancomycin and resveratrol, liver-showed marked improved on a mononuclear cell, and decrease number of mononuclear inflammatory infiltrates (white arrow) and decrease of Mallory bodies (black arrow).
Discussion
Biological systems depend on the liver to detoxify xenobiotics (Apte and Krishnamurthy, 2011). Several studies have shown that hepatic damage disrupts the body’s regular metabolism (Fabbrini and Magkos, 2015; Kurland et al., 2015). There are several causes of acute liver failure, including viral hepatitis, toxic liver damage caused by poisons and drugs, and ischemia (Jalan et al., 2012; Bernal and Wendon, 2013). The liver metabolises xenobiotics as the body’s first line of defense against ingested toxins and drugs, which often cause necrosis and apoptosis (Tsochatzis et al., 2014). A growing body of research focuses on the potential toxicity of antibiotics in the liver (Acevedo, 2015; Fernández et al., 2016; Zoratti et al., 2022). Vancomycin tends to cause adverse events after prolonged use, and large doses may be toxic to the liver (Kucukler et al., 2020). This study aimed to determine whether resveratrol plays a beneficial protective role against vancomycin-induced toxicity in the livers of male Wistar rats.
This study’s findings align with several other research studies that present vancomycin’s potential toxicity (Kucukler et al., 2020). However, to our knowledge, no previous study has investigated the protective role of resveratrol. This study revealed an elevation in serum biomarkers such as AST, ALT, and ALP levels in the groups given only vancomycin or vancomycin with resveratrol, compared to the control group. The serum level of ALT is the most widely used clinical biomarker of hepatic function (Senior, 2012). Furthermore, GSH, an antioxidant, was restored to the normal level in the rats injected with vancomycin and resveratrol, indicating the antioxidant activity of the latter.
Moreover, the rats injected with vancomycin only had significantly reduced GSH levels, confirming the previous findings. Several parameters were affected by the administration of vancomycin. The levels of IL-6, LDH, MDA, and NO were highly increased in the rats injected with vancomycin. Vancomycin administration caused hepatocyte damage, leading to liver enzyme elevation. Hepatotoxic studies commonly measure liver enzyme levels such as ALT, AST, and ALP as serum hepatic biomarkers for determining liver lesions (Deshpande et al., 1998; Sadeghi et al., 2008; Mehrzadi et al., 2018). In this study, vancomycin caused a significant elevation in the serum hepatic biomarkers ALT, AST, and ALP. The concentration of ALT and AST enzymes in serum reflects the severity of liver damage as these enzymes are present in high concentrations in the liver (Adeyemi and Akanji, 2011; Adeyemi and Adewumi, 2014; Yilmaz et al., 2017). In addition, many tissues in the body contain ALP; therefore, it can be considered a non-specific enzyme (López-Posadas et al., 2011). Furthermore, hepatobiliary duct dysfunction or the destruction of hepatic cell membranes can cause a rise in serum ALP, which could indicate a problem with the excretory function (Lowe et al., 2017; Kashima et al., 2018). On the other hand, co-treatment of vancomycin with resveratrol protected against vancomycin-induced hepatic damage, evidenced by the significantly decreased levels of the hepatic serums AST, ALT, and ALP.
It is well known that vancomycin is almost completely eliminated from the body by the kidneys; however, the mechanism by which nephrotoxicity occurs is still unclear. It has been demonstrated in experimental animals that the drug may cause tubular ischemia and acute tubulointerstitial injury by inducing oxidative stress in the proximal renal tubule cells (King and Smith, 2004; Gupta et al., 2011a). Here, vancomycin increased the serum levels of IL-6 (a pro-inflammatory cytokine). The cell surface receptors of the IL-6 family of cytokines regulate cell function (Taga and Kishimoto, 1997). IL-6 consists of two structural subunits: a ligand-binding subunit called the IL-6 receptor and a signal-transducing glycoprotein called Gp130 (Yamauchi-Takihara and Kishimoto, 2000). The liver synthesizes several acute phase proteins in response to IL-6 as it is involved in the pathogenesis of many fibrogenic diseases (Choi et al., 1994). In recent studies, IL-6 has been linked to acute and chronic liver damage (Cao et al., 1998; Gewiese-Rabsch et al., 2010; Bergmann et al., 2017; Shao et al., 2020). In addition, many xenobiotics drugs can injure the liver and trigger the release of pro-inflammatory cytokines like TNF-α and IL6 into the bloodstream (Takai et al., 2016; Olaniyan et al., 2018; Wu et al., 2018). By demonstrating the changes in cytokines that occur in hepatic cells, rodent models can illustrate the molecular changes associated with human hepatic cell death. In this study, we also tested the serum level of MDA, an oxidative stress biomarker that serves as an index of oxidative damage in the liver (Bakan et al., 2002). MDA has been reported to induce collagen production by hepatic stellate cells, resulting in fibrosis (Hadizadeh et al., 2017). Also, it has been reported that vancomycin could initiate an intracellular production of peroxides that triggers the production of MDA (Oktem et al., 2005). Thus, in this study, the vancomycin-induced high serum levels of MDA could be due to vancomycin’s free radical trapping activity and oxidative stress.
GSH has several functions, including serving as an antioxidant, and playing a role in redox and cell signaling (Franco and Cidlowski, 2009; Mari et al., 2009). It acts by reducing hydrogen peroxide, scavenging ROS, and reactive nitrogen species (RNS); therefore, it protects cells against oxidative damage (Day and Suzuki, 2005; Winter et al., 2017). The build-up of an oxidized form of GSH, glutathione disulfide (GSSG), and the depletion of GSH are closely related to ROS and RNS effects on the liver and cells (Yuan and Kaplowitz, 2009; Eskandari et al., 2012). Hepatic NO and its derivatives are essential in liver physiology and pathophysiology (Laskin et al., 2001; Chen et al., 2003; Diesen and Kuo, 2010). It is also a second messenger that acts in several pathways and plays a crucial role in regulating blood pressure by relaxing the endothelium, attacking tumor cells, and stimulating the brain (Gupta et al., 2011b; Korde Choudhari et al., 2013; Picon-Pages et al., 2019). Although NO has multiple and complex roles, it has been suggested that it affects the pathogenesis and progression of liver diseases (Iwakiri and Kim, 2015; Ekhlasi et al., 2017; Wang et al., 2018). On the other hand, LDH (a non-specific tissue damage biomarker) was elevated in vancomycin-treated animals. Numerous tissues and organs in the body produce LDH, including the muscles, liver, heart, pancreas, kidneys, brain, and blood. Body tissue damage can be detected by using the LDH test, determining its location and severity (Farhana and Lappin, 2022). In this study, vancomycin administration causes liver damage, contributing to LDH elevation in the serum. This elevation could arise from vancomycin, causing damage to the kidneys. It has been reported that vancomycin can cause kidney damage (Naghibi et al., 2007), making this test a non-specific marker for liver damage.
Resveratrol is a natural compound extensively studied in preclinical studies as a nutraceutical and therapeutic agent. In addition, the antioxidant properties of resveratrol have been demonstrated in a wide range of hepatic disorders (Pan et al., 2017; Bircan et al., 2018). The antioxidant effect functions mainly by reducing ROS and eliminating direct free radicals, while improving the activity of endogenous antioxidant enzymes superoxide dismutase, catalase, and GSH (Carrizzo et al., 2013; de Oliveira et al., 2018). Furthermore, it has been reported that resveratrol is involved in several vital pathways regulating de novo fibrogenesis deposition in the liver (Hessin et al., 2017). For example, resveratrol (10 and 20 mg/kg/day) was administered to cirrhotic rats, where it reduced portal pressure, improved vasodilatory acetylcholine responsiveness, and reduced the production of thromboxane A2, resulting in liver tissue regeneration (Di Pascoli et al., 2013; Zhang et al., 2016).
Globally, liver illnesses continue to be a severe health burden. For the treatment of this category of disorders, new and secure therapeutic options are required. This study shows that resveratrol is a good alternative in this area. This approach could significantly improve potential resveratrol therapeutic applications. Understanding how resveratrol improves many liver disease conditions may lead to novel treatment possibilities. For example, resveratrol produces beneficial effects and reduces possible toxic effects when combined with other medications and substances. As a result, there is still future work to be done because there are still significant gaps in our knowledge about this chemical.
Acknowledgments
The authors extend their appreciation to the Deanship for Research and Innovation, Ministry of Education in Saudi Arabia for funding this research work through project number: IFP22UQU4310453DSR244.
Funding Statement
This project was funded by the Deanship for Research and Innovation, Ministry of Education in Saudi Arabia through project number: IFP22UQU4310453DSR244.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was conducted according to the guidelines for ethical scientific research at Umm Alqura University. The Biomedical Committee of Research Ethics at the faculty of medicine at Umm Al-Qura University approved the study (Approval No. HAPO-02-K-012-2022-06-1127).
Author contributions
FA, NA participated protocol design, data collection and in conducting the study. FA wrote the manuscript. NA analyzed the data. All authors reviewed the approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Abou Seif H. S. (2016). Physiological changes due to hepatotoxicity and the protective role of some medicinal plants. Beni-suef Univ. J. basic Appl. Sci. 5 (2), 134–146. 10.1016/j.bjbas.2016.03.004 [DOI] [Google Scholar]
- Acevedo J. (2015). Multiresistant bacterial infections in liver cirrhosis: Clinical impact and new empirical antibiotic treatment policies. World J. hepatology 7 (7), 916–921. 10.4254/wjh.v7.i7.916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeyemi O. S., Adewumi I. (2014). Biochemical evaluation of silver nanoparticles in wistar rats. Int. Sch. Res. Not. 2014, 196091. 10.1155/2014/196091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adeyemi O. S., Akanji M. A. (2011). Biochemical changes in the kidney and liver of rats following administration of ethanolic extract of Psidium guajava leaves. Hum. Exp. Toxicol. 30 (9), 1266–1274. 10.1177/0960327110388534 [DOI] [PubMed] [Google Scholar]
- Ahmida M. H. (2012). Protective role of curcumin in nephrotoxic oxidative damage induced by vancomycin in rats. Exp. Toxicol. Pathol. 64 (3), 149–153. 10.1016/j.etp.2010.07.010 [DOI] [PubMed] [Google Scholar]
- Aldaz A., Ortega A., Idoate A., Giraldez J., Brugarolas A., BrugArolAs A. (2000). Effects of hepatic function on vancomycin pharmacokinetics in patients with cancer. Ther. Drug Monit. 22 (3), 250–257. 10.1097/00007691-200006000-00004 [DOI] [PubMed] [Google Scholar]
- Ali S. S., Kasoju N., Luthra A., Singh A., Sharanabasava H., Sahu A., et al. (2008). Indian medicinal herbs as sources of antioxidants. Food Res. Int. 41 (1), 1–15. 10.1016/j.foodres.2007.10.001 [DOI] [Google Scholar]
- Apte U., Krishnamurthy P. (2011). Detoxification Functions of the Liver. Molecular pathology of liver diseases. Springer, 147–163. [Google Scholar]
- Badran E., Shamayleh A., Irshaid Y. (2011). Pharmacokinetics of vancomycin in neonates admitted to the neonatology unit at the Jordan University Hospital. Int. J. Clin. Pharmacol. Ther. 49 (4), 252–257. 10.5414/CP201456 [DOI] [PubMed] [Google Scholar]
- Bakan E., Taysi S., Polat M. F., Dalga S., Umudum Z., Bakan N., et al. (2002). Nitric oxide levels and lipid peroxidation in plasma of patients with gastric cancer. Jpn. J. Clin. Oncol. 32 (5), 162–166. 10.1093/jjco/hyf035 [DOI] [PubMed] [Google Scholar]
- Bamgbola O. (2016). Review of vancomycin-induced renal toxicity: An update. Ther. Adv. Endocrinol. Metab. 7 (3), 136–147. 10.1177/2042018816638223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banez M. J., Geluz M. I., Chandra A., Hamdan T., Biswas O. S., Bryan N. S., et al. (2020). A systemic review on the antioxidant and anti-inflammatory effects of resveratrol, curcumin, and dietary nitric oxide supplementation on human cardiovascular health. Nutr. Res. 78, 11–26. 10.1016/j.nutres.2020.03.002 [DOI] [PubMed] [Google Scholar]
- Bataller R., Brenner D. A. (2005). Liver fibrosis. J. Clin. investigation 115 (2), 209–218. 10.1172/JCI24282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann J., Müller M., Baumann N., Reichert M., Heneweer C., Bolik J., et al. (2017). IL‐6 trans‐signaling is essential for the development of hepatocellular carcinoma in mice. Hepatology 65 (1), 89–103. 10.1002/hep.28874 [DOI] [PubMed] [Google Scholar]
- Bernal W., Wendon J. (2013). Acute liver failure. N. Engl. J. Med. 369 (26), 2525–2534. 10.1056/NEJMra1208937 [DOI] [PubMed] [Google Scholar]
- Bircan F., Pasaoglu O., Turkozkan N. (2018). The effects of resveratrol on hepatic oxidative stress in metabolic syndrome model induced by high fructose diet. Bratisl. Lek. listy 119 (1), 36–40. 10.4149/BLL_2018_008 [DOI] [PubMed] [Google Scholar]
- Bissell D. M., Gores G. J., Laskin D. L., Hoofnagle J. H. (2001). Drug-induced liver injury: Mechanisms and test systems. Hepatology 33 (4), 1009–1013. 10.1053/jhep.2001.23505 [DOI] [PubMed] [Google Scholar]
- Breedt J., Teras J., Gardovskis J., Maritz F. J., Vaasna T., Ross D. P., et al. (2005). Safety and efficacy of tigecycline in treatment of skin and skin structure infections: Results of a double-blind phase 3 comparison study with vancomycin-aztreonam. Antimicrob. Agents Chemother. 49 (11), 4658–4666. 10.1128/AAC.49.11.4658-4666.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunetti L., Song J. H., Suh D., Kim H. J., Seong Y. H., Lee D. S., et al. (2020). The risk of vancomycin toxicity in patients with liver impairment. Ann. Clin. Microbiol. Antimicrob. 19 (1), 13. 10.1186/s12941-020-00354-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujanda L., Hijona E., Larzabal M., Beraza M., Aldazabal P., Garcia-Urkia N., et al. (2008). Resveratrol inhibits nonalcoholic fatty liver disease in rats. BMC Gastroenterol. 8 (1), 40. 10.1186/1471-230X-8-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadle R. M., Mansouri M. D., Darouiche R. O. (2006). Vancomycin-induced elevation of liver enzyme levels. Ann. Pharmacother. 40 (6), 1186–1189. 10.1345/aph.1G668 [DOI] [PubMed] [Google Scholar]
- Çağlayan C., Taslimi P., Demir Y., Küçükler S., Kandemir F. M., Gulcin I. (2019). The effects of zingerone against vancomycin‐induced lung, liver, kidney and testis toxicity in rats: The behavior of some metabolic enzymes. J. Biochem. Mol. Toxicol. 33 (10), e22381. 10.1002/jbt.22381 [DOI] [PubMed] [Google Scholar]
- Cao Q., Batey R., Pang G., Russell A., Clancy R. (1998). IL-6, IFN-gamma and TNF-alpha production by liver-associated T cells and acute liver injury in rats administered concanavalin A. Immunol. Cell Biol. 76 (6), 542–549. 10.1046/j.1440-1711.1998.00779.x [DOI] [PubMed] [Google Scholar]
- Carrizzo A., Forte M., Damato A., Trimarco V., Salzano F., Bartolo M., et al. (2013). Antioxidant effects of resveratrol in cardiovascular, cerebral and metabolic diseases. Food Chem. Toxicol. 61, 215–226. 10.1016/j.fct.2013.07.021 [DOI] [PubMed] [Google Scholar]
- Chen T., Zamora R., Zuckerbraun B., Billiar T. R. (2003). Role of nitric oxide in liver injury. Curr. Mol. Med. 3 (6), 519–526. 10.2174/1566524033479582 [DOI] [PubMed] [Google Scholar]
- Chen Y., Yang X. Y., Zeckel M., Killian C., Hornbuckle K., Regev A., et al. (2011). Risk of hepatic events in patients treated with vancomycin in clinical studies: A systematic review and meta-analysis. Drug Saf. 34 (1), 73–82. 10.2165/11539560-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Choi I., Kang H. S., Yang Y., Pyun K. H. (1994). IL-6 induces hepatic inflammation and collagen synthesis in vivo . Clin. Exp. Immunol. 95 (3), 530–535. 10.1111/j.1365-2249.1994.tb07031.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chupradit S., Bokov D., Zamanian M. Y., Heidari M., Hakimizadeh E. (2022). Hepatoprotective and therapeutic effects of resveratrol: A focus on anti-inflammatory and antioxidative activities. Fundam. Clin. Pharmacol. 36 (3), 468–485. 10.1111/fcp.12746 [DOI] [PubMed] [Google Scholar]
- Das R., Mitra S., Tareq A. M., Emran T. B., Hossain M. J., Alqahtani A. M., et al. (2022). Medicinal plants used against hepatic disorders in Bangladesh: A comprehensive review. J. Ethnopharmacol. 282, 114588. 10.1016/j.jep.2021.114588 [DOI] [PubMed] [Google Scholar]
- David M. Z., Daum R. S. (2010). Community-associated methicillin-resistant Staphylococcus aureus: Epidemiology and clinical consequences of an emerging epidemic. Clin. Microbiol. Rev. 23 (3), 616–687. 10.1128/CMR.00081-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Day R. M., Suzuki Y. J. (2005). Cell proliferation, reactive oxygen and cellular glutathione. Dose-response 3 (3), 425–442. dose-response. 10.2203/dose-response.003.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira M. R., Chenet A. L., Duarte A. R., Scaini G., Quevedo J. (2018). Molecular mechanisms underlying the anti-depressant effects of resveratrol: A review. Mol. Neurobiol. 55 (6), 4543–4559. 10.1007/s12035-017-0680-6 [DOI] [PubMed] [Google Scholar]
- Deshpande U. R., Gadre S. G., Raste A. S., Pillai D., Bhide S. V., Samuel A. M. (1998). Protective effect of turmeric (Curcuma longa L.) extract on carbon tetrachloride-induced liver damage in rats. Indian J. Exp. Biol. 36 (6), 573–577. [PubMed] [Google Scholar]
- Di Pascoli M., Divi M., Rodriguez-Vilarrupla A., Rosado E., Gracia-Sancho J., Vilaseca M., et al. (2013). Resveratrol improves intrahepatic endothelial dysfunction and reduces hepatic fibrosis and portal pressure in cirrhotic rats. J. Hepatol. 58 (5), 904–910. 10.1016/j.jhep.2012.12.012 [DOI] [PubMed] [Google Scholar]
- Diesen D. L., Kuo P. C. (2010). Nitric oxide and redox regulation in the liver: Part I. General considerations and redox biology in hepatitis. J. Surg. Res. 162 (1), 95–109. 10.1016/j.jss.2009.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim H. A., Kamar S. S., Haidara M. A., Latif N. S. A., Ellatif M. A., ShamsEldeen A. M., et al. (2022). Association of resveratrol with the suppression of TNF-α/NF-kB/iNOS/HIF-1α axis-mediated fibrosis and systemic hypertension in thioacetamide-induced liver injury. Naunyn Schmiedeb. Arch. Pharmacol. 395 (9), 1087–1095. 10.1007/s00210-022-02264-w [DOI] [PubMed] [Google Scholar]
- Ekhlasi G., Zarrati M., Agah S., Hosseini A. F., Hosseini S., Shidfar S., et al. (2017). Effects of symbiotic and vitamin E supplementation on blood pressure, nitric oxide and inflammatory factors in non-alcoholic fatty liver disease. EXCLI J. 16, 278–290. 10.17179/excli2016-846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Bohi K. M., Abdel-Motal S. M., Khalil S. R., Abd-Elaal M. M., Metwally M. M. M., Wm E. L. (2021). The efficiency of pomegranate (Punica granatum) peel ethanolic extract in attenuating the vancomycin-triggered liver and kidney tissues injury in rats. Environ. Sci. Pollut. Res. Int. 28 (6), 7134–7150. 10.1007/s11356-020-10999-3 [DOI] [PubMed] [Google Scholar]
- Eskandari M. R., Fard J. K., Hosseini M. J., Pourahmad J. (2012). Glutathione mediated reductive activation and mitochondrial dysfunction play key roles in lithium induced oxidative stress and cytotoxicity in liver. Biometals 25 (5), 863–873. 10.1007/s10534-012-9552-8 [DOI] [PubMed] [Google Scholar]
- Fabbrini E., Magkos F. (2015). Hepatic steatosis as a marker of metabolic dysfunction. Nutrients 7 (6), 4995–5019. 10.3390/nu7064995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farhana A., Lappin S. L. (2022). Biochemistry, lactate dehydrogenase. StatPearls. Treasure island (FL). StatPearls Publishing. [PubMed] [Google Scholar]
- Fathy M., Khalifa E. M., Fawzy M. A. (2019). Modulation of inducible nitric oxide synthase pathway by eugenol and telmisartan in carbon tetrachloride-induced liver injury in rats. Life Sci. 216, 207–214. 10.1016/j.lfs.2018.11.031 [DOI] [PubMed] [Google Scholar]
- Fernández J., Tandon P., Mensa J., Garcia Tsao G. (2016). Antibiotic prophylaxis in cirrhosis: Good and bad. Hepatology 63 (6), 2019–2031. 10.1002/hep.28330 [DOI] [PubMed] [Google Scholar]
- Florescu I., Beuran M., Dimov R., Razbadauskas A., Bochan M., Fichev G., et al. (2008). Efficacy and safety of tigecycline compared with vancomycin or linezolid for treatment of serious infections with methicillin-resistant Staphylococcus aureus or vancomycin-resistant enterococci: A phase 3, multicentre, double-blind, randomized study. J. Antimicrob. Chemother. 62 (1), i17–i28. 10.1093/jac/dkn250 [DOI] [PubMed] [Google Scholar]
- Franco R., Cidlowski J. A. (2009). Apoptosis and glutathione: Beyond an antioxidant. Cell Death Differ. 16 (10), 1303–1314. 10.1038/cdd.2009.107 [DOI] [PubMed] [Google Scholar]
- Friedman S. L. (2008). Mechanisms of hepatic fibrogenesis. Gastroenterology 134 (6), 1655–1669. 10.1053/j.gastro.2008.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gescher A. J., Steward W. P. (2003). Relationship between mechanisms, bioavailibility, and preclinical chemopreventive efficacy of resveratrol: A conundrum. Cancer Epidemiol. Prev. Biomarkers 12 (10), 953–957. [PubMed] [Google Scholar]
- Gewiese-Rabsch J., Drucker C., Malchow S., Scheller J., Rose-John S. (2010). Role of IL-6 trans-signaling in CCl₄induced liver damage. Biochimica Biophysica Acta (BBA)-Molecular Basis Dis. 1802 (11), 1054–1061. 10.1016/j.bbadis.2010.07.023 [DOI] [PubMed] [Google Scholar]
- Gupta A., Biyani M., Khaira A., KhAirA A. (2011). Vancomycin nephrotoxicity: Myths and facts. Neth J. Med. 69 (9), 379–383. [PubMed] [Google Scholar]
- Gupta K. J., Fernie A. R., Kaiser W. M., van Dongen J. T. (2011). On the origins of nitric oxide. Trends Plant Sci. 16 (3), 160–168. 10.1016/j.tplants.2010.11.007 [DOI] [PubMed] [Google Scholar]
- Hadizadeh F., Faghihimani E., Adibi P. (2017). Nonalcoholic fatty liver disease: Diagnostic biomarkers. World J. Gastrointest. Pathophysiol. 8 (2), 11–26. 10.4291/wjgp.v8.i2.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliwell B. (2007). Dietary polyphenols: Good, bad, or indifferent for your health? Cardiovasc. Res. 73 (2), 341–347. 10.1016/j.cardiores.2006.10.004 [DOI] [PubMed] [Google Scholar]
- Hessin A. F., Hegazy R. R., Hassan A. A., Yassin N. Z., Kenawy S. A. (2017). Resveratrol prevents liver fibrosis via two possible pathways: Modulation of alpha fetoprotein transcriptional levels and normalization of protein kinase C responses. Indian J. Pharmacol. 49 (4), 282–289. 10.4103/ijp.IJP_299_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang J. H., Lee J. H., Hwang J. H., Chung K. M., Lee E. J., Yoon Y. J., et al. (2015). Comparison of arbekacin and vancomycin in treatment of chronic suppurative otitis media by methicillin resistant Staphylococcus aureus . J. Korean Med. Sci. 30 (6), 688–693. 10.3346/jkms.2015.30.6.688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim J., Kabiru A. Y., Abdulrasheed-Adeleke T., Lawal B., Adewuyi A. H. (2020). Antioxidant and hepatoprotective potentials of curcuminoid isolates from turmeric (Curcuma longa) rhizome on CCl4-induced hepatic damage in Wistar rats. J. Taibah Univ. Sci. 14 (1), 908–915. 10.1080/16583655.2020.1790928 [DOI] [Google Scholar]
- Iwakiri Y., Kim M. Y. (2015). Nitric oxide in liver diseases. Trends Pharmacol. Sci. 36 (8), 524–536. 10.1016/j.tips.2015.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalan R., Gines P., Olson J. C., Mookerjee R. P., Moreau R., Garcia-Tsao G., et al. (2012). Acute-on chronic liver failure. J. hepatology 57 (6), 1336–1348. 10.1016/j.jhep.2012.06.026 [DOI] [PubMed] [Google Scholar]
- Kaplowitz N. (2001). Drug-induced liver disorders: Implications for drug development and regulation. Drug Saf. 24 (7), 483–490. 10.2165/00002018-200124070-00001 [DOI] [PubMed] [Google Scholar]
- Kashima J., Okuma Y., Shimizuguchi R., Chiba K. (2018). Bile duct obstruction in a patient treated with nivolumab as second-line chemotherapy for advanced non-small-cell lung cancer: A case report. Cancer Immunol. Immunother. 67 (1), 61–65. 10.1007/s00262-017-2062-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King D. W., Smith M. A. (2004). Proliferative responses observed following vancomycin treatment in renal proximal tubule epithelial cells. Toxicol Vitro 18 (6), 797–803. 10.1016/j.tiv.2004.03.013 [DOI] [PubMed] [Google Scholar]
- Kohno S., Yamaguchi K., Aikawa N., Sumiyama Y., Odagiri S., Aoki N., et al. (2007). Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan. J. Antimicrob. Chemother. 60 (6), 1361–1369. 10.1093/jac/dkm369 [DOI] [PubMed] [Google Scholar]
- Korde Choudhari S., Chaudhary M., Bagde S., Gadbail A. R., Joshi V. (2013). Nitric oxide and cancer: A review. World J. Surg. Oncol. 11 (1), 118–211. 10.1186/1477-7819-11-118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouijzer I. J., van Leerdam E. J., Gompelman M., Tuinte R. A., Aarntzen E. H., Berrevoets M. A., et al. (2021). Intravenous to oral switch in complicated Staphylococcus aureus bacteremia without endovascular infection: A retrospective single-center cohort study. Clin. Infect. Dis. 73 (5), 895–898. 10.1093/cid/ciab156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucukler S., Darendelioğlu E., Caglayan C., Ayna A., Yıldırım S., Kandemir F. M. (2020). Zingerone attenuates vancomycin-induced hepatotoxicity in rats through regulation of oxidative stress, inflammation and apoptosis. Life Sci. 259, 118382. 10.1016/j.lfs.2020.118382 [DOI] [PubMed] [Google Scholar]
- Kurland I. J., Broin P. O., Golden A., Su G., Meng F., Liu L., et al. (2015). Integrative metabolic signatures for hepatic radiation injury. PLoS One 10 (6), e0124795. 10.1371/journal.pone.0124795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labban S., Alghamdi B. S., Alshehri F. S., Kurdi M. (2021). Effects of melatonin and resveratrol on recognition memory and passive avoidance performance in a mouse model of Alzheimer's disease. Behav. Brain Res. 402, 113100. 10.1016/j.bbr.2020.113100 [DOI] [PubMed] [Google Scholar]
- Labban S., Alshehri F. S., Kurdi M., Alatawi Y., Alghamdi B. S. (2021). Melatonin improves short-term spatial memory in a mouse model of alzheimer's disease. Degener. Neurol. Neuromuscul. Dis. 11, 15–27. 10.2147/DNND.S291172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larrey D. (Editor) (2002). “Epidemiology and individual susceptibility to adverse drug reactions affecting the liver,” Seminars in liver disease (Medical Publishers, Inc.). Copyright© 2002 by Thieme333 Seventh Avenue, New. [DOI] [PubMed] [Google Scholar]
- Laskin J. D., Heck D. E., Gardner C. R., Laskin D. L. (2001). Prooxidant and antioxidant functions of nitric oxide in liver toxicity. Antioxid. Redox Signal 3 (2), 261–271. 10.1089/152308601300185214 [DOI] [PubMed] [Google Scholar]
- Lee E. S., Shin M. O., Yoon S., Moon J. O. (2010). Resveratrol inhibits dimethylnitrosamine-induced hepatic fibrosis in rats. Arch. Pharm. Res. 33 (6), 925–932. 10.1007/s12272-010-0616-4 [DOI] [PubMed] [Google Scholar]
- López-Posadas R., Gonzalez R., Ballester I., Martínez-Moya P., Romero-Calvo I., Suárez M. D., et al. (2011). Tissue-nonspecific alkaline phosphatase is activated in enterocytes by oxidative stress via changes in glycosylation. Inflamm. bowel Dis. 17 (2), 543–556. 10.1002/ibd.21381 [DOI] [PubMed] [Google Scholar]
- Lowe D., Sanvictores T., John S. (2017). Alkaline phosphatase. [PubMed] [Google Scholar]
- Ma Z., Sheng L., Li J., Qian J., Wu G., Wang Z., et al. (2022). Resveratrol alleviates hepatic fibrosis in associated with decreased endoplasmic reticulum stress-mediated apoptosis and inflammation. Inflammation 45 (2), 812–823. 10.1007/s10753-021-01586-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mari M., Morales A., Colell A., Garcia-Ruiz C., Fernandez-Checa J. C. (2009). Mitochondrial glutathione, a key survival antioxidant. Antioxid. Redox Signal 11 (11), 2685–2700. 10.1089/ARS.2009.2695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrzadi S., Fatemi I., Esmaeilizadeh M., Ghaznavi H., Kalantar H., Goudarzi M. (2018). Hepatoprotective effect of berberine against methotrexate induced liver toxicity in rats. Biomed. Pharmacother. 97, 233–239. 10.1016/j.biopha.2017.10.113 [DOI] [PubMed] [Google Scholar]
- Miguel C., Noya-Riobó M., Mazzone G., Villar M., Coronel M. (2021). Antioxidant, anti-inflammatory and neuroprotective actions of resveratrol after experimental nervous system insults. Special focus on the molecular mechanisms involved. Neurochem. Int. 150, 105188. 10.1016/j.neuint.2021.105188 [DOI] [PubMed] [Google Scholar]
- Naghibi B., Ghafghazi T., Hajhashemi V., Talebi A. (2007). Vancomycin-induced nephrotoxicity in rats: Is enzyme elevation a consistent finding in tubular injury? J. Nephrol. 20 (4), 482–488. [PubMed] [Google Scholar]
- Novo E., Parola M. (2008). Redox mechanisms in hepatic chronic wound healing and fibrogenesis. Fibrogenes. Tissue Repair 1, 5–58. 10.1186/1755-1536-1-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oktem F., Arslan M. K., Ozguner F., Candir O., Yilmaz H. R., Ciris M., et al. (2005). In vivo evidences suggesting the role of oxidative stress in pathogenesis of vancomycin-induced nephrotoxicity: Protection by erdosteine. Toxicology 215 (3), 227–233. 10.1016/j.tox.2005.07.009 [DOI] [PubMed] [Google Scholar]
- Olaniyan M. F., Atibor R. A., Afolabi T. (2018). Evaluation of tumor necrosis factor alpha (TNFα), interleukin 4, interleukin 6, aspartate aminotransferase, and alanine aminotransferase in rabbits overdosed with ibuprofen and supplemented with guava leaf (Psidium guajava) extract. Biomed. Biotechnol. Res. J. (BBRJ) 2 (4), 254. 10.4103/bbrj.bbrj_121_18 [DOI] [Google Scholar]
- Omara F., Aziz S., El-Sheikh S., Said M. (2021). Ascorbic acid attenuated the hepatic parenchymal necrosis induced by azithromycin-etoricoxib interaction in rats. J. Anim. Health Prod. 9 (1), 42–48. 10.17582/journal.jahp/2021/9.s1.42.48 [DOI] [Google Scholar]
- Pan Y., Zhang H., Zheng Y., Zhou J., Yuan J., Yu Y., et al. (2017). Resveratrol exerts antioxidant effects by activating SIRT2 to deacetylate Prx1. Biochemistry 56 (48), 6325–6328. 10.1021/acs.biochem.7b00859 [DOI] [PubMed] [Google Scholar]
- Pandit A., Sachdeva T., Bafna P. (2012). Drug-induced hepatotoxicity: A review. J. Appl. Pharm. Sci. 2 (5), 233–243. [Google Scholar]
- Parthasarathy M., Evan Prince S. (2021). The potential effect of phytochemicals and herbal plant remedies for treating drug-induced hepatotoxicity: A review. Mol. Biol. Rep. 48 (5), 4767–4788. 10.1007/s11033-021-06444-4 [DOI] [PubMed] [Google Scholar]
- Philips C. A., Ahamed R., Rajesh S., George T., Mohanan M., Augustine P. (2020). Comprehensive review of hepatotoxicity associated with traditional Indian Ayurvedic herbs. World J. Hepatol. 12 (9), 574–595. 10.4254/wjh.v12.i9.574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Picon-Pages P., Garcia-Buendia J., Munoz F. J. (2019). Functions and dysfunctions of nitric oxide in brain. Biochim. Biophys. Acta Mol. Basis Dis. 1865 (8), 1949–1967. 10.1016/j.bbadis.2018.11.007 [DOI] [PubMed] [Google Scholar]
- Pourhanifeh M. H., Shafabakhsh R., Reiter R. J., Asemi Z. (2019). The effect of resveratrol on neurodegenerative disorders: Possible protective actions against autophagy, apoptosis, inflammation and oxidative stress. Curr. Pharm. Des. 25 (19), 2178–2191. 10.2174/1381612825666190717110932 [DOI] [PubMed] [Google Scholar]
- Regal R. E., Ren S. P., Paige G., Alaniz C. (2019). Evaluation of vancomycin dosing in patients with cirrhosis: Beginning de-liver-ations about a new nomogram. Hosp. Pharm. 54 (2), 125–129. 10.1177/0018578718772266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera H., Shibayama M., Tsutsumi V., Perez-Alvarez V., Muriel P. (2008). Resveratrol and trimethylated resveratrol protect from acute liver damage induced by CCl4 in the rat. J. Appl. Toxicol. 28 (2), 147–155. 10.1002/jat.1260 [DOI] [PubMed] [Google Scholar]
- Rubiolo J. A., Vega F. V. (2008). Resveratrol protects primary rat hepatocytes against necrosis induced by reactive oxygen species. Biomed. Pharmacother. 62 (9), 606–612. 10.1016/j.biopha.2008.06.034 [DOI] [PubMed] [Google Scholar]
- Sadeghi H., Nikbakht M. R., Izadpanah G., Sabzali S. (2008). Hepatoprotective effect of Cichorium intybus on CCl4-induced liver damage in rats. Afr. J. Biochem. Res. 2 (6), 141–144. [Google Scholar]
- Sahin M., Cam H., Olgar S., Tunc S. E., Arslan C., Uz E., et al. (2006). Protective role of erdosteine on vancomycin-induced oxidative stress in rat liver. Mol. Cell Biochem. 291 (1-2), 155–160. 10.1007/s11010-006-9209-4 [DOI] [PubMed] [Google Scholar]
- Santos M. A., Franco F. N., Caldeira C. A., de Araújo G. R., Vieira A., Chaves M. M., et al. (2021). Antioxidant effect of Resveratrol: Change in MAPK cell signaling pathway during the aging process. Archives Gerontology Geriatrics 92, 104266. 10.1016/j.archger.2020.104266 [DOI] [PubMed] [Google Scholar]
- Sebai H., Sani M., Yacoubi M. T., Aouani E., Ghanem-Boughanmi N., Ben-Attia M. (2010). Resveratrol, a red wine polyphenol, attenuates lipopolysaccharide-induced oxidative stress in rat liver. Ecotoxicol. Environ. Saf. 73 (5), 1078–1083. 10.1016/j.ecoenv.2009.12.031 [DOI] [PubMed] [Google Scholar]
- Sener G., Toklu H. Z., Sehirli A. O., Velioglu-Ogunc A., Cetinel S., Gedik N. (2006). Protective effects of resveratrol against acetaminophen-induced toxicity in mice. Hepatol. Res. 35 (1), 62–68. 10.1016/j.hepres.2006.02.005 [DOI] [PubMed] [Google Scholar]
- Senior J. R. (2012). Alanine aminotransferase: A clinical and regulatory tool for detecting liver injury-past, present, and future. Clin. Pharmacol. Ther. 92 (3), 332–339. 10.1038/clpt.2012.108 [DOI] [PubMed] [Google Scholar]
- Shah A. A., Patton M., Chishty W. H., Hussain A. (2010). Analysis of elevated liver enzymes in an acute medical setting: Jaundice may indicate increased survival in elderly patients with bacterial sepsis. Saudi J. Gastroenterol. 16 (4), 260–263. 10.4103/1319-3767.70609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao M., Xu Q., Wu Z., Chen Y., Shu Y., Cao X., et al. (2020). Exosomes derived from human umbilical cord mesenchymal stem cells ameliorate IL-6-induced acute liver injury through miR-455-3p. Stem Cell Res. Ther. 11 (1), 37–13. 10.1186/s13287-020-1550-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibai B. M. (2004). Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count. Obstet. Gynecol. 103 (5), 981–991. 10.1097/01.AOG.0000126245.35811.2a [DOI] [PubMed] [Google Scholar]
- Srivastava P., Prabhu V. V., Yadav N., Gogada R., Chandra D. (2013). Effect of dietary resveratrol in the treatment of cancer. Cancer chemoprevention and treatment by diet therapy. Springer, 1–22. [Google Scholar]
- Steinmetz T., Eliakim-Raz N., Goldberg E., Leibovici L., Yahav D. (2015). Association of vancomycin serum concentrations with efficacy in patients with MRSA infections: A systematic review and meta-analysis. Clin. Microbiol. Infect. 21 (7), 665–673. 10.1016/j.cmi.2015.04.003 [DOI] [PubMed] [Google Scholar]
- Taga T., Kishimoto T. (1997). Gp130 and the interleukin-6 family of cytokines. Annu. Rev. Immunol. 15, 797–819. 10.1146/annurev.immunol.15.1.797 [DOI] [PubMed] [Google Scholar]
- Takai S., Oda S., Tsuneyama K., Fukami T., Nakajima M., Yokoi T. (2016). Establishment of a mouse model for amiodarone-induced liver injury and analyses of its hepatotoxic mechanism. J. Appl. Toxicol. 36 (1), 35–47. 10.1002/jat.3141 [DOI] [PubMed] [Google Scholar]
- Thiim M., Friedman L. S. (2003). Hepatotoxicity of antibiotics and antifungals. Clin. Liver Dis. 7 (2), 381–399. vi-vii. 10.1016/s1089-3261(03)00021-7 [DOI] [PubMed] [Google Scholar]
- Tong Y., Yu X., Huang Y., Zhang Z., Mi L., Bao Z. (2022). Hepatic-targeted nano-enzyme with resveratrol loading for precise relief of nonalcoholic steatohepatitis. ChemMedChem. 10.1002/cmdc.202200468 [DOI] [PubMed] [Google Scholar]
- Tsochatzis E. A., Bosch J., Burroughs A. K. (2014). Liver cirrhosis. Lancet 383 (9930), 1749–1761. 10.1016/S0140-6736(14)60121-5 [DOI] [PubMed] [Google Scholar]
- Tsutsuura M., Moriyama H., Kojima N., Mizukami Y., Tashiro S., Osa S., et al. (2021). The monitoring of vancomycin: A systematic review and meta-analyses of area under the concentration-time curve-guided dosing and trough-guided dosing. BMC Infect. Dis. 21 (1), 153. 10.1186/s12879-021-05858-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Jiang Y., Fan X., Tan H., Zeng H., Wang Y., et al. (2015). Hepato-protective effect of resveratrol against acetaminophen-induced liver injury is associated with inhibition of CYP-mediated bioactivation and regulation of SIRT1–p53 signaling pathways. Toxicol. Lett. 236 (2), 82–89. 10.1016/j.toxlet.2015.05.001 [DOI] [PubMed] [Google Scholar]
- Wang Y. Y., Chen M. T., Hong H. M., Wang Y., Li Q., Liu H., et al. (2018). Role of reduced nitric oxide in liver cell apoptosis inhibition during liver damage. Arch. Med. Res. 49 (4), 219–225. 10.1016/j.arcmed.2018.09.001 [DOI] [PubMed] [Google Scholar]
- Winter A. N., Ross E. K., Daliparthi V., Sumner W. A., Kirchhof D. M., Manning E., et al. (2017). A cystine-rich whey supplement (Immunocal®) provides neuroprotection from diverse oxidative stress-inducing agents in vitro by preserving cellular glutathione. Oxid. Med. Cell Longev. 2017, 3103272. 10.1155/2017/3103272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K., Fan J., Huang X., Wu X., Guo C. (2018). Hepatoprotective effects exerted by Poria Cocos polysaccharides against acetaminophen-induced liver injury in mice. Int. J. Biol. Macromol. 114, 137–142. 10.1016/j.ijbiomac.2018.03.107 [DOI] [PubMed] [Google Scholar]
- Xia H. M., Wang J., Xie X. J., Xu L. J., Tang S. Q. (2019). Green tea polyphenols attenuate hepatic steatosis, and reduce insulin resistance and inflammation in high-fat diet-induced rats. Int. J. Mol. Med. 44 (4), 1523–1530. 10.3892/ijmm.2019.4285 [DOI] [PubMed] [Google Scholar]
- Yamauchi-Takihara K., Kishimoto T. (2000). Cytokines and their receptors in cardiovascular diseases—Role of gp130 signalling pathway in cardiac myocyte growth and maintenance. Int. J. Exp. pathology 81 (1), 1–16. 10.1046/j.1365-2613.2000.00139.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz S., Kaya E., Comakli S. (2017). Vitamin E (alpha tocopherol) attenuates toxicity and oxidative stress induced by aflatoxin in rats. Adv. Clin. Exp. Med. 26 (6), 907–917. 10.17219/acem/66347 [DOI] [PubMed] [Google Scholar]
- Yin Y., Liu H., Zheng Z., Lu R., Jiang Z. (2019). Genistein can ameliorate hepatic inflammatory reaction in nonalcoholic steatohepatitis rats. Biomed. Pharmacother. 111, 1290–1296. 10.1016/j.biopha.2019.01.004 [DOI] [PubMed] [Google Scholar]
- Yousefian M., Shakour N., Hosseinzadeh H., Hayes A. W., Hadizadeh F., Karimi G. (2019). The natural phenolic compounds as modulators of NADPH oxidases in hypertension. Phytomedicine 55, 200–213. 10.1016/j.phymed.2018.08.002 [DOI] [PubMed] [Google Scholar]
- Yuan L., Kaplowitz N. (2009). Glutathione in liver diseases and hepatotoxicity. Mol. Asp. Med. 30 (1-2), 29–41. 10.1016/j.mam.2008.08.003 [DOI] [PubMed] [Google Scholar]
- Zhang C., Wang N., Xu Y., Tan H. Y., Li S., Feng Y. (2018). Molecular mechanisms involved in oxidative stress-associated liver injury induced by Chinese herbal medicine: An experimental evidence-based literature review and network Pharmacology study. Int. J. Mol. Sci. 19 (9), 2745. 10.3390/ijms19092745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang D. Q., Sun P., Jin Q., Li X., Zhang Y., Zhang Y. J., et al. (2016). Resveratrol regulates activated hepatic stellate cells by modulating NF-κB and the PI3K/akt signaling pathway. J. Food Sci. 81 (1), H240–H245. 10.1111/1750-3841.13157 [DOI] [PubMed] [Google Scholar]
- Zhou Y., Chen K., He L., Xia Y., Dai W., Wang F., et al. (2015). The protective effect of resveratrol on concanavalin-A-induced acute hepatic injury in mice. Gastroenterol. Res. Pract. 2015, 506390. 10.1155/2015/506390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoratti C., Moretti R., Rebuzzi L., Albergati I. V., Di Somma A., Decorti G., et al. (2022). Antibiotics and liver cirrhosis: What the physicians need to know. Antibiotics 11 (1), 31. 10.3390/antibiotics11010031 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.