Highlights
-
•
Penal and healthcare institutions generate and mitigate community-level health inequality, respectively.
-
•
Arkansas Counties with high prison churn and disadvantage have higher rates of HIV/AIDS.
-
•
Hospital density moderates effect of prison churn on incidence of HIV/AIDS.
1. Introduction
Beginning in the 1980s, the HIV/AIDS epidemic plagued the United States for over two decades. In addition to the alarming racial disparities in HIV/AIDS deaths and diagnoses, whereby African Americans compose over 40% of new HIV/AIDS diagnoses (Center for Disease Control and Prevention, 2020), HIV/AIDS remains a major public health crisis in this country, albeit with significant regional variation. The South suffers from more HIV/AIDS diagnoses and deaths than any other U.S. region. Southeastern rural communities, foremost the Mississippi Delta, have disproportionately high rates of HIV/AIDS (Hall et al., 2006). As the HIV/AIDS epidemic took hold, another major societal trend also swept the U.S.: mass incarceration. Counties that have high incarceration rates also have higher rates of HIV/AIDS (Henderson, 2016).
In this study, we will investigate how these trends hold across a nearly all rural Southern state, Arkansas. Arkansas, the focus of this study, has higher-than-average incidences of HIV/AIDS and high incarceration rates (Carson, 2020). Rural, southern places are understudied in research on both HIV/AIDS and mass incarceration. To this end, we explore the link between prison churn, community level factors like disadvantage/organizational density, and HIV/AIDS infection rates, based on data from a twenty-year period of mass incarceration and high HIV/AIDS rates. This important, historical data maps onto the height of both the HIV/AIDS pandemic and mass incarceration, making it particularly relevant for the study. We build specifically from Johnson and Raphael (2009), who find strong association between state level incarceration rates and the rise in state level HIV/AIDS infection rates over time. We take a place-based approach and examine the relationship between prison churn and HIV/AIDS rates across Arkansas.
2. The dynamic process of churn
The similar patterns of incarceration and HIV/AIDS lead us to the most vital concepts in exploring infectious disease and place-based inequality: carceral churn or coercive mobility. Carceral churn describes the process of removals and returns from and to communities through the criminal justice system, specifically incarceration and reentry back into communities. Churn contributes to neighborhood instability and it is linked to neighborhood concentrated disadvantage (Clear et al., 2003). Churn is also spatially concentrated, with many returning from prison to the most disadvantaged neighborhoods (Kubrin & Stewart, 2006; Visher & Farrell, 2005, pp. 1–16).
In studying churn and infectious disease pathways, it is important to examine the prison context, the lives of people returning from prison, and the communities to which people return to after prison. While reentry focuses on the process of returning home from prison, churn captures both returns and admissions. Both can be independent concepts; however, we see them as constitutive of similar social processes of punishment. For example, according to the Bureau of Justice Statistics (Durose et al., 2014), most people (67%) released from prison in 2005 were re-arrested within three years and most return to poor communities.
Many people going into prisons enter with pre-existing health problems; however, research also indicates that incarceration increases the likelihood of having additional health issues (Schnittker et al., 2011). Health problems are exacerbated by prison conditions, stress, exposure to infectious diseases, and having to live with a large number of people (Massoglia, 2008; Thompson, 2008).
The negative effects of incarceration on community integration and the resulting social, economic, and health disadvantages for people who have experienced time in prison are well-established strands of research (Morenoff & Harding, 2014; Schnittker et al., 2011; Uggen et al., 2006; Western & Pettit, 2010). People entering into and returning from prison are part of vulnerable populations even before their incarceration. They are likely to have experienced racial discrimination, mental health challenges, unemployment, poverty, and homelessness (Greenberg & Rosenheck, 2008; James & Glaze, 2006; Pager et al., 2009; Watkins-Hayes, Gay-Pittman, & Jean, 2012). Prison can put stress on familial relationships and is associated with mental health disorders, as well as increased incidences of midlife physical health problems (Christian, 2005; Massoglia, 2008; Schnittker et al., 2012; Travis et al., 2001, pp. 1–49; Turney, 2015).
Returning home from a period of incarceration is often a difficult process and it can be challenging to rebuild social ties, resume routines, and attain economic mobility. Qualitative research by Western et al. (2015) indicates the material hardship people encounter upon return from prison often goes hand in hand with experiencing anxiety and loneliness. People returning from a period of incarceration commonly grapple with intense poverty, physical pain, and substance abuse issues (Western, 2018).
Formerly incarcerated individuals often return to neighborhoods that experience residential instability, as well as lack resources, both in terms of their institutional and social network capacity, which can make people more likely to experience significant obstacles to building a life for themselves after prison (Kubrin & Stewart, 2006). Carceral churn is a form of residential instability which has long been shown to weaken the social infrastructure of neighborhoods. In turn, residential instability can impact the health of communities and their residents. Instability results in low neighborhood collective efficacy—social cohesion among neighbors coupled with residents’ propensity to intervene in matters for the good of the collective. When people intend to reside in their neighborhoods for a long period of time, own their homes, and have the economic resources to invest in their communities, they may feel more desire or responsibility to improve and maintain the health of their neighborhoods. In contrast, disadvantage spurred by race and class residential segregation, incarceration, and concentrated poverty leaves residents isolated and lacking the means to foster collective efficacy (Sampson, Raudenbush, and Earls 1997).
Some research also indicates that churn can increase neighborhood crime rates (Hipp and Yates 2009; Clear et al., 2003). When a certain percentage of residents in a neighborhood are incarcerated, additional prison admissions increase crime levels (Clear et al., 2003). Further incarceration in neighborhoods already heavily impacted by the criminal justice system may magnify social disorganization levels and impede a community’s ability to establish informal social controls (Rose & Clear, 1998).
Thus, neighborhoods significantly impacted by incarceration that also have high crime rates are already some of the most vulnerable to infectious disease transmission. High community-level rates of return from a period of incarceration creates instability and makes communities more vulnerable to HIV transmission pathways. For example, a body of research demonstrates that Black male incarceration, housing precarity, and surveillance of people returning from prison all serve to de-stabilize and dissolve relationships, resulting in HIV/AIDS risk in low-income, Black communities among both men and women (Cooper et al., 2015; Khan et al., 2018; Blankenship et al., 2021). Other challenges, including economic insecurity, also raise HIV/AIDS risk. Finally, lack of institutional support in conjunction with poverty and trauma make it difficult for people returning from prison to cope well when living with HIV/AIDS (Watkins-Hayes, Gay-Pittman, & Jean, 2012).
3. Churn and HIV/AIDS
Counties that have high incarceration rates or reentry facilities for previously incarcerated individuals also have higher rates of HIV (Henderson, 2016). These effects are not just concentrated in urban places. Previous research on prison reentry often focuses on urban neighborhoods (Miller, 2021; Visher & Farrell, 2005, pp. 1–16; Western, 2018). However, Eason, Zucker, & Wildeman (2017), drawing from Arkansas county-level data, show that high incarceration rates for both Black and white men exist across the urban-rural interface.
Communities experiencing churn are vulnerable to infectious diseases through various channels. First of all, high infection rates are seen in prison (Rosen et al., 2009). As a matter of fact, there exists an “alarming prevalence of communicable diseases like hepatitis C, TB, and HIV/AIDS among prisoners” (Restum, 2005, p. 1690). Thus, the effects of a period of incarceration on individual health outcomes has received much attention by scholars. Massoglia (2008) finds an independent negative influence of incarceration on health, especially for infectious disease, as do Schnittker and John (2007) for after prison release. Recent research has also found associations between incarceration and mortality (Daza, Palloni, and Jones 2020). A number of mechanisms explain this pattern of high HIV/AIDS infection rates inside prisons: a high baseline percentage of people diagnosed with HIV/AIDS, more risky sexual behaviors, networks containing several individuals infected with HIV/AIDS who engage in (consensual and non-consensual) sex with multiple partners, and the disruption and destabilization of relationships formed outside of prison (Johnson & Raphael, 2009).
Finally, individuals reentering their communities also face challenges with infectious diseases. Individuals with HIV/AIDS who have been previously incarcerated often experience relapsed drug use, which disrupts their medical treatment and makes the potential of re-incarceration for substance use more likely (Swan, 2015). Drawing from interviews with HIV-infected formerly incarcerated individuals in New York, Rowell-Cunsolo et al. (2020), find that study participants vary in how much antiretroviral medication they are provided by their prison upon their release—over a third received an amount that would last them less than a month. Sidibe et al. (2015) and Solomon et al. (2014) similarly find that HIV-infected individuals experience obstacles to maintaining care and antiretroviral therapy once they are released from prison. Their findings suggest that other critical reentry concerns, such as finding housing and food, compete with the task of obtaining needed health care. The authors also highlight community-level barriers to medical care such as lack of access to transportation. In addition, people infected with HIV/AIDS have trouble engaging in risk reduction strategies (Arnold et al., 2009) due to disorganization in social life post-incarceration. Blankenship, Smoyer, and Mattocks (2005) point to the de-stabilizing effect of incarceration on HIV-infected drug users in terms of disrupted networks and relationships, due to surveillance associated with being on probation and parole after incarceration and parole conditions obligating people on parole to avoid contact with former social ties.
4. HCOs as organizational resources
In this study, we hypothesize that healthcare organizations (HCOs)— specifically the presence of hospitals—may moderate the effect of churn on the incidence of HIV/AIDS. This is not to say that merely the presence of HCOs will result in access to care given transportation challenges in rural communities, lack of information about healthcare available, as well as the existence of other reentry challenges that may be a higher priority for formerly incarcerated people to tackle, such as finding housing. Surprisingly, some research shows that a presence of a HCO is related to higher rates of churn in communities in Arkansas (Wallace et al., 2015). This suggests that HCOs in of themselves may not be enough to reduce carceral churn at this point in time in some communities. However, the existence of HCOs is a crucial step towards addressing a vulnerable population’s medical needs.
Prior research indicates a significant rural disadvantage in both health outcomes and healthcare access. Poor healthcare access among rural residents is influenced by a lack of resources, such as scarcity of services and trained physicians, as well as transportation challenges (Douthit, Kiv, Dwolatzky, & Biswas, 2015). However, the presence of healthcare organizations can increase access to care and improve individuals' health outcomes in communities (Soleimanpour et al., 2010).
Distribution of resources and opportunities also influences community-level social cohesion and neighborhood health (Marwell, 2007). Hospitals and other HCOs, such as drug addiction centers and clinics, are considered neighborhood organizations: “neighborhood institutions in which the residents participate” (Small, 2006, p. 274). Proximity to organizational resources is important in facilitating their use (Allard et al., 2003; Marwell, 2007; Small, 2009). Resource utilization has been shown to improve community cohesion and ultimately promote positive individual outcomes (Sampson, 2012). For example, community-based organizations provide opportunities and connect individuals to services such as healthcare and education, which help alleviate poverty (Marwell, 2007). In the case of a HCO, having access to one not only shapes the medical care one receives but also potentially connects under-resourced individuals to opportunities and benefits through a HCO’s ties with other organizations (Marwell, 2007; Small, 2006). The presence of a HCO may also assist with advocacy on behalf of the needs of people who are using the services and bolster the services that are available to clients based on the HCO’s relationship with local governments. A HCO may provide a source of employment for residents in communities with minimal jobs opportunities (Marwell, 2007). All of these aspects can better support risk-reduction among people diagnosed with HIV/AIDS.
While we know the formally incarcerated face a multitude of challenges to successful reentry including barriers to acquire housing, educational opportunities, employment, and adequate healthcare, we lack clarity on how these receiving communities are impacted by prison churn and how healthcare organizations may moderate the impact of churn on HIV/AIDS as an intervention.
5. Research methods & data
This research project was born of an ethnographic case study of a rural Arkansas town. The project on Arkansas Reentry and Health Disparities (ARRHD) is an effort to examine the socioeconomic changes and health outcomes associated with prison reentry at the county level in the state of Arkansas. In particular, the project examines incidences of new HIV/AIDS cases in Arkansas counties as a function of both socioeconomic, demographic, and reentry conditions.
We combine these variables with admissions records to form a key independent variable: churn.
Additionally, the ARRHD project aims to assess the influence of prison reentry on socio-economic characteristics of micro-places (e.g. block groups) in the state of Arkansas. The data is a unique combination of secondary data provided in two data sets that can be merged into a multilevel format. The first data set consists of individual inmate reentry records from the Arkansas Department of Corrections (ADC) between 1990 and 2008.
The second data set consists of county-level data related to new incidents of HIV/AIDS annually between 1990 and 2011, the density of community organizations collected from annual county and zip code business pattern census data between 1990 and 2010, and structural census covariates associated with socio-economic and demographic characteristics of residents collected from the 1990, 2000, and 2010 decennial census. County-level segregation data was created using block-group census data on race and ethnicity from decennial censuses. The index of dissimilarity was included for all pairs of white individuals, Black individuals, and Latino individuals. The key outcome variables include the spatial concentration of ADC reentries across counties (n = 120,000 from 1990 to 2011), characteristics of individuals (n = 70,000 from 1990 to 2011), ADC reentries, and the county level incidence of HIV/AIDS cases from 1990 to 2011. We use a place-based (county-level) approach and ask: What is the relationship between churn and HIV/AIDS rates across counties and over time in Arkansas? And: Do HCOs moderate the association between churn and HIV/AIDS rates over time and across counties?
6. Data
To conduct the analysis, we constructed a panel dataset spanning the period 1990–2010 that measures the rate of annual new HIV/AIDS cases, annual churn rate, reentry population characteristics and the demographics of each county in Arkansas (See Table 1). The panel dataset is compiled from several data sources. We contacted the Arkansas Department of Corrections for detailed information on the incarcerated population. We also contacted the Arkansas Department of Public Health for community level HIV/AIDS incidence. Both departments provided the data without a Freedom of Information Request (FOIR). We then used R and Stata as data collection tools to clean the data and extract the variables we chose.
Table 1.
Descriptive statistics of dependent and independent variables used in regression analysis of HIV incidences, 1990–2010.
| Mean | St. Dev. | |
|---|---|---|
| Log carceral churn rate | 15.62 | 1.31 |
| HIV rate | 8.13 | 9.23 |
| Prop. non-Hispanic Black | 0.15 | 0.17 |
| Concentrated disadvantage | 0.00 | 0.93 |
| Log hosp. per 100,000 | 0.31 | 0.24 |
| Population density | 49.31 | 63.90 |
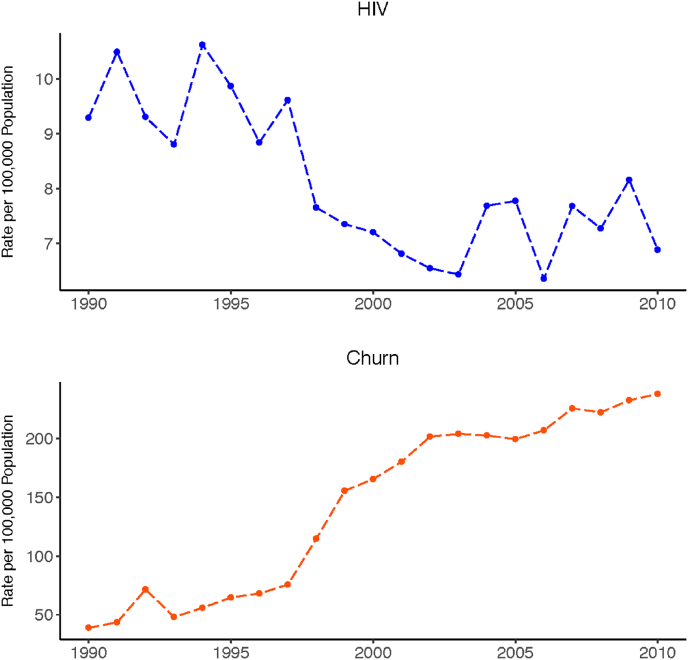
Note: The HIV rates documented here start right in the middle of the U.S. HIV/AIDS Epidemic which peaked in the mid-90s. The overall HIV rates are on a steady decline till the early 2000s and then fluctuate till the year 2010. The churn rates, on the opposite, are on a steady rise, a result of mass incarceration in the U.S.
6.1. HIV/AIDS data
De-identified data on annual new HIV/AIDS cases by county are administrative data and was obtained from the Arkansas Department of Health. The data covers new HIV/AIDS cases in 75 counties over 22 years, from 1990 to 2011. One issue with this data concerns confidentiality. In counties with few new HIV/AIDS cases, those individuals may be easily identified. To still provide data for analysis from all counties from 1990 to 2011, while also ensuring confidentiality, the Department suppressed cells that show only one or two new HIV/AIDS cases annually. Around half of the counties have suppressed counts of new HIV/AIDS cases for almost every year. For 2006, 2010, and 2011, only around 40% counties show suppressed counts. For 1996, more than 60% of the counties have suppressed counts. Three counties—Perry, Pike, and Stone—have all 22 years suppressed, meaning each year these counties recorded only one or two new HIV/AIDS cases. To use all of the cases for model estimation, we randomly assigned one or two to the suppressed values provided by the Arkansas Department of Health. Similar findings appeared from sensitivity analyses of the model with all suppressed HIV/AIDS counts assigned as one and the model with all suppressed HIV/AIDS counts assigned as two.
6.2. Reentry data
De-identified, administrative data for individual inmate reentry records from the Arkansas Department of Corrections (ADOC) between 1990 and 2008 include address data, which allowed us to geocode inmates to communities after release (we assume most formerly incarcerated individuals return to the community of prior residence).
6.3. Vera Institute of justice: In our backyard data
The Vera Institute of Justice provides county-level data on prison admissions during the study period. We merged these annual, county-level data on prison admissions with release data from ADC described earlier to construct the churn variable.
6.4. Census data
Census data includes demographic data of each county over time. We constructed a county-level disadvantage score by using factor analysis of the following socio-economic conditions: Proportion of child poverty, proportion of adults with no high school degree, percentage of unemployment, proportion of households receiving public assistance income, and proportion of female-headed households. We also considered proportion of Black individuals and population density of each county over the years. We interpolated the decennial data to construct an annual longitudinal dataset.
6.5. County business pattern data
The County Business Pattern (CBP) classifies each business with a formal payroll by the Standard Industrial Classification (SIC) code system or the North American Classification System (NAICS). These codes designate each business a code that indicates their type. Using the data between 1986 and 2008, we used the county-level count data of several business or organization types to construct two broad HCO categories: doctors’ offices and hospitals. In 1997, SIC was replaced by NAICS. While SIC and NAICS codes are not strictly comparable, and the NAICS system is updated every five years, it is possible to establish near comparability in broad classifications of industry (e.g. farming/forestry, mining, construction, retail finance, etc.). All SIC and NAICS codes have been recoded to the 2007 NAICS system, the latest system developed during the study period. The relevant codes that reflect doctors’ offices and hospitals barely changed between the two systems or over time for NAICS. The change was subtle enough to make straightforward decisions for our study.
6.6. Key independent variables
Carceral churn rate is the sum of admission and release per 100,000 residents of each county from Vera Institute of Justice Data. Using census data, we constructed the Concentrated Disadvantage Index, the county-level disadvantage score described above. HCO density is a constructed numerical variable that uses both the CBP data and the census data: the number of hospitals in a county is divided by the county’s total population. We then standardized the decimals by multiplying 100,000, which indicates the number of hospitals per 100,000 people in each county.
7. Methods
To test hypotheses relating incarceration, health care environments, socioeconomic disadvantage, racial composition, and HIV/AIDS incidences, the analysis writes county-level HIV incidences as a function of county-level prison admissions and releases (carceral churn), concentrated disadvantage, hospitals per capita, the racial composition of the county, and population density. The primary zero-inflated negative binomial equation models counts of HIV in county i in year t as follows:
Where are year fixed effects. We use a zero-inflated negative binomial regression (ZINB) because the rare event of HIV/AIDS, even at the county level. This modeling strategy is used for count data that exhibit overdispersion and excess zeros. The zero-inflated method is suitable when the distribution of zeros is high, and many cases are at reduced risk or no risk of experiencing an event. The data distribution combines the negative binomial distribution and the logit distribution, whereby the first estimates the likelihood of a zero count and the latter the expected count of the outcome variable. We use a parsimonious equation to predict zero counts that includes population density for the given county.
8. Results
Fig. 1 displays the changes in carceral churn and HIV/AIDS incidence over time. HIV/AIDS rates are somewhat steady through the 1990s and decline in the early 2000s. However, after 2004 we observe increases in HIV/AIDS incidence rivaling levels in the mid-1990s. Conversely, the rate of prison admissions and releases sharply climbs in the late 1990s, and continues to grow steadily through the 2000s.
Fig. 1.
Rates of HIV/AIDS incidences and carceral churn per 100,000 residents of Arkansas counties, 1990–2010.
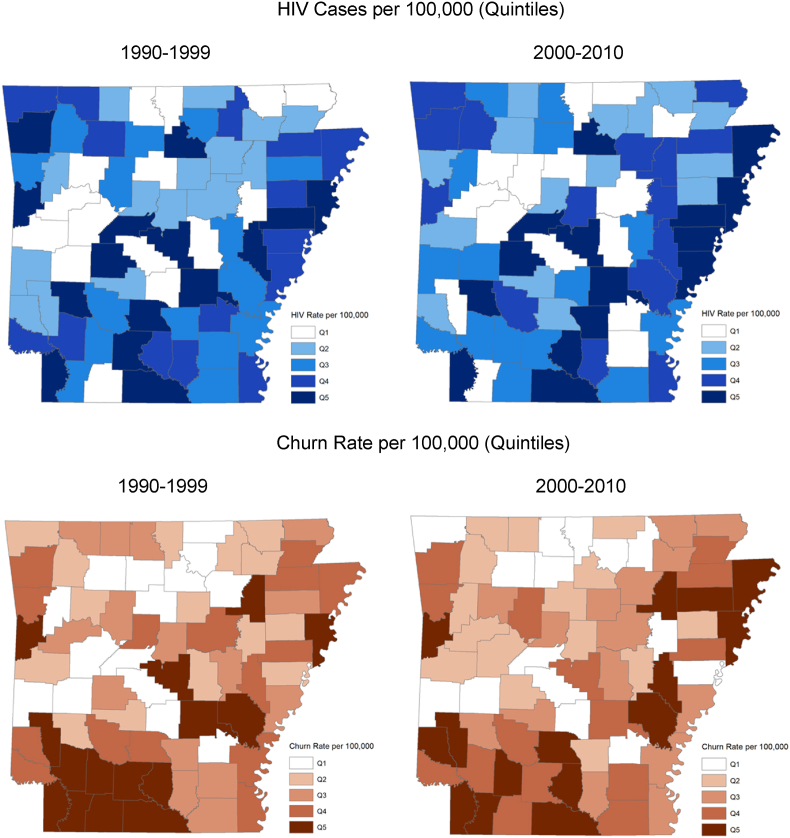
Fig. 2 displays four maps. The top panel illustrates the incidence of HIV/AIDS in Arkansas counties per 100,000 inhabitants, averaged across two time periods: 1990–1999 and 2000–2010. Rates are displayed in quintiles. Overall, the average rate for all counties in the 1990s is 9.2 per 100,000, and in the later period it is 7.2. The average churn rate is nearly three times higher in the later period—the rate climbs to 517.6 from 182 per 100,000. The bottom panel shows the average rate of carceral churn per 100,000 for the same periods. In the southwestern part of the state, HIV/AIDS is more diffuse in the earlier period and there is a higher concentration of churn. In comparison to the eastern portion of the state, which is part of the Yazoo Mississippi Delta, the southwest is more mountainous and wealthier. This could account for why churn and HIV/AIDS decline more precipitously in that region. In contrast, in the eastern portion of the state during the later period, HIV/AIDS and churn are concentrated across the highest quintiles.
Fig. 2.
Average rates of HIV/AIDS incidences and carceral churn per 100,000 inhabitants, 1990–1999 and 2000–2010. Maps display quintiles for each period.
Table 2 displays results from zero-inflated negative binomial regression results. Model 1 reports estimates for a model of carceral churn and HIV/AIDS. Model 2 introduces levels of concentrated disadvantage, and Model 3 brings in a measure of the healthcare environment. A final model introduces an interaction term between carceral churn and the rate of hospitals per 100,000 people. All models include year fixed effects and controls for log population density.
Table 2.
Zero-inflated negative binomial regression results of HIV incidences, 1990–2010.
|
Dependent variable: HIV incidences |
||||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Log carceral churn rate | 0.744*** | 0.631*** | 0.637*** | 0.685*** |
| (0.037) | (0.038) | (0.037) | (0.042) | |
| Prop. non-Hispanic Black | 0.494 | 0.517 | 0.563 | |
| (0.350) | (0.348) | (0.347) | ||
| Concentrated disadvantage | 0.197*** | 0.178*** | 0.171** | |
| (0.066) | (0.065) | (0.065) | ||
| Log hospitals per 100,000 | −0.460*** | 3.201* | ||
| (0.124) | (1.533) | |||
| Population density | 0.004*** | 0.005*** | 0.005*** | 0.006*** |
| (0.0005) | (0.001) | (0.0005) | (0.0005) | |
| Churn rate x Hospitals per 100,000 | −0.236* | |||
| (0.097) | ||||
| Constant |
−10.234*** | −8.687*** | −8.680*** | −9.467*** |
| (0.543) |
(0.554) |
(0.549) |
(0.641) |
|
| Observations | 1575 | 1575 | 1575 | |
| Log Likelihood | −2915.2 | −2859.3 | −2852.4 | −2850.0 |
Note: Models include year fixed effects. *p**p***p < 0.01.
In all models, the log rate of carceral churn is a strong predictor of HIV/AIDS incidences. In Model 3, we find a 1% change in the log rate of carceral churn is associated with an 89% increase in the expected rate of HIV/AIDS incidences [exp(0.637) = 1.89], net of the county’s concentrated disadvantage, total hospitals, population density, and year fixed effects.
Concentrated disadvantage is also strongly correlated with HIV/AIDS incidences. We find a one point increase in the county’s concentrated disadvantage score is associated with a 19% increase in the expected HIV/AIDS incidences. The healthcare environment is also predictive of HIV/AIDS incidences. A 1% increase in the rate of hospitals in the county per 100,000 residents is associated with a 0.63% decrease in the expected incidence of HIV/AIDS. Notably, the proportion of the county population that is non-Hispanic Black is not significantly related to HIV/AIDS incidences in either Model 2 or 3. Lastly, population density is positively correlated with higher HIV/AIDS incidences.
Model 4 tests the degree to which the presence of HCOs moderates the association between carceral churn and HIV/AIDS incidence. We interpret the interaction term as suggesting that the impact of carceral churn is not consistent across areas with different rates of healthcare density. The effect of churn on HIV/AIDS incidence in areas with more hospitals is lower than in areas with fewer hospitals per 100,000 residents. We find that HCOs significantly moderate the effect of carceral churn on the incidence of HIV/AIDS in Arkansas counties.
9. Discussion
Although rates of HIV/AIDS across Arkansas generally decline from 1990 to 2010, our findings demonstrate that counties with higher levels of carceral churn and disadvantage have higher rates of HIV/AIDS. However, we also find that counties with high levels of churn but more hospitals have lower rates of HIV/AIDS and, thus, that hospital density significantly moderates the effect of carceral churn on the incidence of HIV/AIDS in Arkansas counties. This important finding suggests that HCOs have a protective effect against the spread of HIV/AIDS, even in communities with higher levels of carceral churn and disadvantage.
While Arkansas is a national leader in the U.S. HIV/AIDS rate for African Americans, we do not find a significant effect specific to Black individuals at the county level after adjustment for carceral churn and other county-level factors. Finally, we conducted tests for a rural effect at the county level, but it was not significant. That said, population density was positively correlated with higher rates of HIV/AIDS in all models.
There are several potential contributing factors to help explain these findings. First, 17% of all individuals with HIV/AIDS have a history of incarceration nationally (Wakefield & Uggen, 2010). Our findings linking county-level churn across Arkansas to rates of HIV/AIDS clearly supports this national trend. In addition, while Southern states have higher rates of incarceration overall, they tend to have lower racial disparities in rates of incarceration. Furthermore, despite moves towards decarceration across the U.S. since mid 2000s (The Sentencing Project, 2019), the rate of incarceration, and therefore churn, did not significantly decline in Arkansas during our study period. Our findings of higher HIV/AIDS rates across Arkansas are consistent with Southern trends in incarceration and HIV/AIDS incidence.
While the seminal piece in this area by Johnson and Raphael (2009) is a national analysis from 1982 to 1996, our study is from 1990 to 2010. We similarly find associations between incarceration and HIV/AIDS. Furthermore, they examine incarceration, while we examine effect of churn on specific communities. While they advance our understanding of variation in HIV/AIDS rates across time, by state and individual-level characteristics, we add to this growing body of literature by measuring the importance of place-based characteristics and institutions. Specifically, we examine the importance of the political economy by looking at the county, an administrative unit, that allows us to merge census data with other administrative records. Another significant advance our study provides is finding the moderating effect of HCOs on this vital health outcome. This study affirms the importance of not only studying context but how the presence of institutions affects public health crises.
10. Limitations
While we have twenty years of data on which to base our examination of the relationship between churn and rates of HIV/AIDS, these data are limited to one Southern state. Thus, although our study provides a deep dive into one Black Belt state during a specific period, it cannot reflect the relationship overall across the country. We do know the rise in HIV/AIDS and incarceration rates are associated over the same period nationally (Johnson & Raphael, 2009). With more granular spatial data, future studies could conduct more exploratory analysis that tests how spatial proximity to HCOs before and after prison release mitigates infectious disease spread. Our county-level analysis demonstrates important population-level patterns that could be further assessed for spatial clustering and multicollinearity with more detailed data. Moreover, missing data on the prior residence and return addresses of incarcerated people, as well as HIV incidences, may bias estimates of the relationship between carceral churn and HIV. More granular data would allow researchers to assess and adjust estimates of HIV prevalence (e.g., imputation) as it relates to incarceration (Mosha et al., 2020).
Variation in type of HCO and proximity to HCO also influences the type of care that formerly incarcerated people are able to access. This is especially true in rural communities. Given that the majority of counties in Arkansas are overwhelming rural this is important for our study. This also speaks to the novelty of our study because we rarely see investigations into rural communities, especially regarding prison reentry and health outcomes. The way that space matters across rural communities is also dependent on time to travel to healthcare organizations, which speaks to the importance of future studies using spatial analyses. However, given the dearth of studies and data on rural communities, this initial investigation provides strong evidence of why we need further research on this important topic. While such questions were not in the purview of this study, future work could explore these matters to better understand how people may access medical care given variable rates of HIV/AIDS.
For future studies, we would prefer more granular data for HIV/AIDS rates at the town or neighborhood level to match the census and churn data. County level data can obscure acute inequality. U.S. Census Places or municipalities are even more accurate for examining the depth and breadth of inequality. However, the Arkansas Department of Health collects data only at the county level to anonymize the identities of vulnerable populations suffering from HIV/AIDS. Finally, the period we observe is after the initial pandemic of HIV/AIDS in the 1980s. Future studies of infectious disease should consider potentially exploring data at the neighborhood or town level and over periods when initial public health crises first appear.
11. Conclusion
Prison proliferation has severely altered the physical, social, economic, and political landscape of rural America (Lawrence & Travis, 2004), especially across southern states like Arkansas. Tomaskovic-Devey and Avent-Holt (2019) recently argued that penal institutions are inequality generators. Given the way prisons exacerbate infectious disease, we should also understand such institutions as fundamental to the production of health inequality across the U.S as well. In this study, we find evidence of prisons increasing health inequality with regards to infectious disease, and we also find that the presence of healthcare institutions in communities can help mitigate poor health outcomes. Thus, penal and healthcare institutions can generate and mitigate community-level inequality, respectively.
Of late, scholars increasingly study HIV/AIDS and health in the context of incarceration (Braithwaite et al., 1996; Gaiter & Doll, 1996; Wakefield & Uggen, 2010; Wildeman & Muller, 2012; World Health Organization, 2014); however, we suggest that HIV/AIDS and other infectious diseases are not just a health problem for prisons. We suggest it is also fruitful to look at communities to better understand how HIV/AIDS is spread and potential ways to mitigate the effects of infectious disease. Wildeman and Muller (2012) suggest the “health spillover” effects of incarceration occur through a multitude of avenues, including the relationships people in the criminal justice system have with people in the “free world.” They reveal these relationships can have a negative health impact on sexual partners, family members, and friends. These “health spillover effects” are part of the aftermath of mass incarceration that stay with the individuals and their communities as they churn through the criminal justice system.
Author statement
Chloe E. Haimson: Conceptualization; Project administration; Investigation; Supervision; Writing - original draft; Writing - review & editing. Jessica T. Simes: Conceptualization; Data curation; Formal analysis; Methodology; Project administration; Investigation; Supervision; Writing - original draft; Writing - review & editing; Methodology; Validation; Visualization. John M. Eason: Conceptualization; Data curation; Methodology; Project administration; Investigation; Supervision; Writing - original draft; Writing - review & editing. Jienian Zhang: Formal analysis; Methodology; Project administration; Validation; Writing - original draft.
Declaration of competing interest
None.
Footnotes
We would like to acknowledge Zinobia Bennefield, Verna Keith, Corey Sparks, Danielle Wallace, and Jaquelyn Jahn.
Data availability
Data will be made available on request.
References
- Allard S.W., Tolman R.M., Rosen D. Proximity to service providers and service utilization among welfare recipients: The interaction of place and race. Journal of Policy Analysis and Management. 2003;22(4):599–613. doi: 10.1002/pam.10157. [DOI] [PubMed] [Google Scholar]
- Arnold M., Hsu L., Pipkin S., McFarland W., Rutherford G.W. Race, place and AIDS: The role of socioeconomic context on racial disparities in treatment and survival in san francisco. Social Science & Medicine. 2009;69:121–129. doi: 10.1016/j.socscimed.2009.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankenship K.M., Alana Rosenberg D., Keene E., Dawson A.J., Allison K., Groves P.S. Social determination of HIV: Women’s relationship work in the context of mass incarceration and housing vulnerability. AIDS and Behavior. 2021;25(Suppl 2) doi: 10.1007/s10461-021-03238-4. S190–S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankenship K.M., Smoyer A.B., Bray S.J., Mattocks K. Black-white disparities in HIV/AIDS: The role of drug policy and the Corrections system. Journal of Health Care for the Poor and Underserved. 2005;16:140–156. doi: 10.1353/hpu.2005.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite R.L., Hammett T.M., Mayberry R.M. Jossey-Bass; San Francisco, CA: 1996. Prisons and AIDS: A public health challenge. [Google Scholar]
- Carson E.A. U.S. Department of Justice; Washington, D.C: 2020. Prisoners in 2019.” Bureau of justice statistics.https://www.bjs.gov/content/pub/pdf/p19.pdf Retrieved November 9, 2020. [Google Scholar]
- Center for Disease Control and Prevention “HIV and african Americans.”. 2020. https://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html Retrieved Dec. 15, 2020.
- Christian J. Riding the bus: Barriers to prison visitation and family management strategies. Journal of Contemporary Criminal Justice. 2005;2(1):31–48. [Google Scholar]
- Clear T.R., Rose D.R., Waring E., Scully K. Coercive mobility and crime: A preliminary examination of concentrated incarceration and social disorganization. Justice Quarterly. 2003;20(1):33–64. [Google Scholar]
- Cooper H.L.F., Caruso B., Terrika Barham, Embry V., Dauria E., Clark C.D., Comfort M.L. Partner incarceration and african-American women’s sexual relationships and risk: A longitudinal qualitative study. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2015;92(3):527–547. doi: 10.1007/s11524-015-9941-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daza S., Alberto P., Jones J. The consequences of incarceration for mortality in the United States. Demography. 2020;57:577–598. doi: 10.1007/s13524-020-00869-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douthit N., Kiv S., Dwolatzky T., Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- Durose M.R., Cooper A.D., Snyder H.N. U.S. Department of Justice; Washington, D.C: 2014. Recidivism of prisoners released in 30 states in 2005: Patterns from 2005 to 2010-update. Bureau of justice statistics.https://www.bjs.gov/index.cfm?ty=pbdetail&iid=4986 Retrieved November 9, 2020. [Google Scholar]
- Eason J.M., Zucker D., Wildeman C. Mass Imprisonment across the Rural-Urban Interface. Ann. Am. Acad. Polit. Soc. Sci. 2017;672(1):202–216. [Google Scholar]
- Gaiter J., Doll L.S. Editorial: Improving HIV/AIDS prevention in prisons is good public health policy. American Journal of Public Health. 1996;86(9):1201–1203. doi: 10.2105/ajph.86.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg G.A., Rosenheck R.A. Homelessness in the state and federal prison population. Criminal Behaviour and Mental Health. 2008;18(2):88–103. doi: 10.1002/cbm.685. [DOI] [PubMed] [Google Scholar]
- Hall H.I., Li J., McKenna M.T. HIV in predominantly rural areas of the United States. The Journal of Rural Health. 2006;21(3):245–253. doi: 10.1111/j.1748-0361.2005.tb00090.x. [DOI] [PubMed] [Google Scholar]
- Henderson L. Mass incarceration, residential segregation and racial disparities in HIV. Journal of AIDS and HIV Research. 2016;8(11):150–162. [Google Scholar]
- James D.J., Glaze L.E. Bureau of Justice Statistics; 2006. Mental health problems of prison and jail inmates.https://bjs.ojp.gov/content/pub/pdf/mhppji.pdf Washington D.C.: U.S. Department of Justice (Also available at: [Google Scholar]
- Johnson R.C., Raphael S. The effects of male incarceration dynamics on acquired immune deficiency syndrome infection rates among african American women and men. The Journal of Law and Economics. 2009;52(2):251–293. [Google Scholar]
- Khan M.R., Scheidell J.D., Golin C.E., Friedman S.R., Adimora A.A., Lejuez Hui Hu C.W., Quinn K., Wohl D.A. Dissolution of committed partnerships during incarceration and STI/HIV-related sexual risk behavior after prison release among african American men. Journal of Urban Health. 2018;95:479–487. doi: 10.1007/s11524-018-0274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubrin C.E., Stewart E.A. Predicting who reoffends: The neglected role of neighborhood context in recidivism studies. Criminology. 2006;44(1):165–197. [Google Scholar]
- Lawrence S., Travis J. The Urban Insitute; Washington, D.C.: 2004. The new landscape of imprisonment. Retrieved June 9, 2021 ( https://www.urban.org/sites/default/files/publication/57971/410994-The-New- Landscape-of-Imprisonment.PDF. [Google Scholar]
- Marwell N.P. University of Chicago Press; Chicago, IL: 2007. Bargaining for brooklyn: Community organizations in the entrepreneurial city. [Google Scholar]
- Massoglia M. Incarceration, health, and racial disparities in health. Law & Society Review. 2008;42(2):275–306. [Google Scholar]
- Miller R.J. Little, Brown and Company; New York City, New York: 2021. Halfway home: Race, punishment and the afterlife of mass incarceration. [Google Scholar]
- Morenoff J.D., Harding D.J. Incarceration, prisoner reentry, and communities. Annual Review of Sociology. 2014;40(1):411–429. doi: 10.1146/annurev-soc-071811-145511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosha N.R., Aluko O.S., Todd J., Machekano R., Young T. Analytical methods used in estimating the prevalence of HIV/AIDS from demographic and cross-sectional surveys with missing data: A systematic review. BMC Medical Research Methodology. 2020;20(65):1–10. doi: 10.1186/s12874-020-00944-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pager D., Bonikowski B., Western B. Discrimination in a low-wage labor market: A field experiment. American Sociological Review. 2009;74(5):777–799. doi: 10.1177/000312240907400505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restum Z.G. Public health implications of substandard correctional health care. American Journal of Public Health. 2005;95(10):1689–1691. doi: 10.2105/AJPH.2004.055053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose D.R., Clear T.R. Incarceration, social capital, and crime: Implications for social disorganization theory. Criminology. 1998;36(3):441–480. [Google Scholar]
- Rosen D.L., Schoenbach V.J., Wohl D.A., White B.L., Stewart P.W., Golin C.E. Characteristics and behaviors associated with HIV infection among inmates in the North Carolina prison system. American Journal of Public Health. 2009;99(6):1123–1130. doi: 10.2105/AJPH.2007.133389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowell-Cunsolo, Tawandra L., Hu G., Rahwa H. It’s like I was out there by myself”: The receipt of reentry support among HIV-infected formerly incarcerated individuals in New York city. Health & Justice. 2020;8(6):1–8. doi: 10.1186/s40352-020-00108-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson R.J. University of Chicago Press; Chicago: 2012. Great American city: Chicago and the enduring neighborhood effect. [Google Scholar]
- Schnittker J., John A. Enduring stigma: The long-term effects of incarceration on health. Journal of Health and Social Behavior. 2007;48:115–130. doi: 10.1177/002214650704800202. [DOI] [PubMed] [Google Scholar]
- Schnittker J., Massoglia M., Uggen C. Incarceration and the health of the african American community. Du Bois Review. 2011;8(1):1–9. [Google Scholar]
- Schnittker J., Massoglia M., Uggen C. Out and down: Incarceration and psychiatric disorders. Prison and Men’s Mental Health. 2012;53(4):448–464. doi: 10.1177/0022146512453928. [DOI] [PubMed] [Google Scholar]
- Sidibe T., Golin C., Turner K., Fray N., Cathie Fogel. Flynn P., Gould M., Knight K., Wohl D. Provider perspectives regarding the health care needs of a key population: HIV-infected prisoners after incarceration. Journal of the Association of Nurses in AIDS Care. 2015;26(5):556–569. doi: 10.1016/j.jana.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small M.L. Neighborhood institutions as resource brokers: Childcare centers, interorganizational ties, and resource access among the poor. Social Problems. 2006;53(2):274–292. [Google Scholar]
- Small M.L. Oxford University Press; New York, NY: 2009. Unanticipated gains: Origins of network inequality in everyday life. [Google Scholar]
- Soleimanpour S., Geierstanger S.P., Kaller S., McCarter V., Brindis C.D. The role of school health centers in health care access and client outcomes. American Journal of Public Health. 2010;100(9):1597–1603. doi: 10.2105/AJPH.2009.186833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon L., Montague B.T., Beckwith C.G., Baillargeon J., Costa M., Dumont D., Kuo I., Kurth A., Rich J.D. Survey finds that many prisons and jails have room to improve HIV testing and coordination of postrelease treatment. Health Affairs. 2014;33(3):434–442. doi: 10.1377/hlthaff.2013.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan H. Different patterns of drug use and barriers to continuous HIV care post-incarceration. Journal of Drug Issues. 2015;45(1):38–52. doi: 10.1177/0022042614542512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Sentencing Project . 2019. The U.S. Prison population trends. Retrieved June 9th, 2021 ( https://www.sentencingproject.org/publications/u-s-prison-population-trends-massive-buildup-and-modest-decline/ [Google Scholar]
- Thompson A. NYU Press; New York: 2008. Releasing prisoners, redeeming communities: Reentry, race, and politics. [Google Scholar]
- Tomaskovic-Devey D., Avent-Holt D. Oxford University Press; New York, NY: 2019. Relational inequalities: An organizational approach. [Google Scholar]
- Travis J., Solomon A.L., Waul M. The Urban Institute; Washington D.C.: 2001. From prison to home: The dimensions and consequences of prisoner reentry. [Google Scholar]
- Turney K. Liminal men: Incarceration and relationship dissolution. Social Problems. 2015;62(4):499–528. [Google Scholar]
- Uggen C., Manza J., Thompson M. Citizenship, democracy, and the civic integration of criminal offenders. The Annals of the American Academy of Political and Social Science. 2006;605(1):281–310. [Google Scholar]
- Visher C., Farrell J. Urban Institute; Washington, D.C.: 2005. Chicago communities and prison reentry. [Google Scholar]
- Wakefield S., Uggen C. Incarceration and stratification. Annual Review of Sociology. 2010;36(1):387–406. [Google Scholar]
- Wallace D., Eason J.M., Lindsey A.M. The influence of incarceration and Re-entry. on the Availability of Health Care Organizations in Arkansas. 2015;3(3):1–11. [Google Scholar]
- Watkins-Hayes C., Gay-Pittman L.S., Jean B. Dying from” to “living with” framing institutions and the coping processes of african American women living with HIV/AIDS. Social Science & Medicine. 2012;74:2028–2036. doi: 10.1016/j.socscimed.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Western B. Russell Sage Foundation; New York: 2018. Homeward: Life in the year after prison. [Google Scholar]
- Western B., Braga A.A., Davis J., Sirois C. Stress and hardship after prison. American Journal of Sociology. 2015;120(5):1512–1547. doi: 10.1086/681301. [DOI] [PubMed] [Google Scholar]
- Western B., Pettit B. Incarceration & social inequality. Dædalus. 2010;139(3):8–19. doi: 10.1162/daed_a_00019. [DOI] [PubMed] [Google Scholar]
- Wildeman C., Muller C. Mass imprisonment and inequality in health and family life. Annual Review of Law and Social Science. 2012;8(1):11–30. [Google Scholar]
- World Health Organization . 2014. Prisons and health.https://apps.who.int/iris/bitstream/handle/10665/128603/Prisons%20and%20Health.pdf Retrieved June 9, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.