Abstract
Background
The purpose of our study was to compare the knee implant SIGMA to the ATTUNE knee implant in a cruciate-retaining (CR) fixed-bearing (FB) total knee replacement (TKR) surgery, with no patellar resurfacing.
Methods
We examined 40 patients (19 SIGMA; 21 ATTUNE) who underwent a TKR FB CR surgery, without patellar resurfacing, due to osteoarthritis, between August 2013 and July 2017. All surgeries were performed by a single surgeon. We performed a cross-sectional analytical study based on preoperative patient data and data collected in follow-up sessions. All patients were asked to fill a quality-of-life (QOL) questionnaire, SF-36 translated to the Hebrew language. All patients were clinically evaluated using the Knee Society Score (KSS) and the Knee Function Score (KFS).
Results
Patients from the SIGMA cohort reported fewer postoperative physical function limitations in the SF-36 (p = 0.01) and the KFS (p = 0.04). Patients who underwent surgery using the SIGMA implant reported increased vitality when compared to the ATTUNE (p = 0.02). No significant differences were found between the groups in other measures of quality of life, ranges of motion, valgus, and postoperative knee stability. The average follow-up period was significantly longer for the SIGMA (p < 0.00001).
Conclusion
Significant differences were found in postoperative physical function and vitality scores between SIGMA and ATTUNE knee implants. SIGMA cohort presented superior results. Presumably, these findings are due to the differences in follow-up times.
Keywords: ATTUNE, SIGMA, Total knee replacement, Physical function, Vitality
Background
Knee arthroplasty is a surgery in which the weight-bearing surface in the knee joint is replaced in order to provide the patient with pain relief and improved function. The most common disorders treated with knee arthroplasty are osteoarthritis (OA), rheumatoid arthritis (RA) and psoriatic arthritis (PA). The main indication for a total knee replacement (TKR) is OA with debilitating pain, which is unresponsive to conservative treatment [1].
Studies have shown that between 10 and 20% of patients who have undergone TKR are dissatisfied with the joint replacement [2]. Early failure of the knee replacement is usually due to wear and tear of the polyethylene, loosening, and instability which lead to the need for a reoperation [3]. In addition, anterior knee pain (AKP) is one of the common causes of persistent complications after TKR. About 28% of patients experience knee pain, most often with moderate to severe pain levels [4].
Pain after knee replacement surgery, especially AKP, is a common condition which affects up to 50% of patients [5–7]. Improper patellofemoral tracking and patellar tilt were identified as causative agents of anterior knee pain [8]. Therefore, mechanical properties of the knee implants such as the trochlear groove and patella (anatomical or reconstructed) may affect the knee movement following TKR [9]. Despite good long-term survival rates [10], the SIGMA implant is associated with high dissatisfaction and AKP rates [11]. As a result, DePuy Synthes, designed the ATTUNE implant in a more anatomical way aiming of improving patient satisfaction.
The ATTUNE knee implant was developed to improve stability, movement, and reduce AKP [12]. The ATTUNE knee implant addresses these issues using a number of DePuy Synthes Joint technologies unique to the cruciate-retaining (CR) fixed-bearing (FB) implant: ATTUNE GRADIUS ™ Curve, LOGICLOCK ™ Tibial Base, and GLIDERIGHT ™ Articulation. In addition, the ATTUNE implant is available in 14 different sizes, compared to the SIGMA implant which is an available in eight sizes. A wider range of sizes allows for a more precise adjustment for each patient. A mismatch between the femoral and tibial surfaces can lead to a structural kinematic damage.
ATTUNE GRADIUS ™ Curve
Anterior/posterior (A/P) stability of the knee is determined in part by the geometry of the femoral component and it is fit to the joint surface of the implant. The ATTUNE GRADIUS ™ Curve is the gradual reduction of the femoral radius which produces a smooth transition during the gait cycle [13, 14]. The gradual reduction mimics the natural shape of the knee which provides stability, through a large radius, when the knee is straight and rotational freedom, through a small radius, when the knee is bent. The gradual reduction in radius minimizes forward knee movement compared to other implants, such as the SIGMA [15], which are based on multiple radii without gradual transition. The ATTUNE GRADIUS ™ Curve prevents the sharp transition between the radii.
LOGICLOCK ™ Tibial Base
In order to improve the kinematics in the FB implant, the femoral geometry and the surface of the tibial joint must match. This adjustment is achieved when the surface of the tibial joint is adjusted to the size of the femoral component in each patient. The LOGICLOCK ™ Tibial Base allows the connection and locking of different tibial joint surface sizes to the base of the tibial implant. The femoral component and the surface of the tibial joint can be adjusted size to size, thus improving the tibial–femoral mechanics, the stability, and the rotational freedom along the range of motion. This technology is designed to address the fear of wear and tear, as a result of micro-movements, which may lead to osteolysis. The unique shape and locking mechanism reduce the micro-movements in the knee joint [12].
GLIDERIGHT ™ Articulation
The patellofemoral interaction is one of the more challenging aspects in TKR surgery [16]. The soft tissue in the knee plays a significant role in stabilizing the patella at the beginning of flexion [16–19]. The ATTUNE trochlear groove is designed, anatomically, to work with the soft tissue and adapt anatomical changes in the patient by combining a funnel shape at angles 0–45°, compared to the single radius found in the SIGMA implant. This innovation allows the patient's soft tissue to lead the patellar position during knee extension and provides a smooth transition to the center of the trochlear groove. The femoral groove in the ATTUNE is characterized by a variable angle in each size range and funnel shape which maintains the patella in the center to provide proper alignment and contact area throughout the extension. Unlike the SIGMA implant which is designed to work with a reconstructed patella, the ATTUNE implant is designed to provide articular support to either the patient’s or a reconstructed patella. One of the major changes made in the ATTUNE was a minimization of the width and thickness of the trochlear margins in attempt to provide optimal fit and thus reduce the bony bulge that may lead to soft tissue irritation [12].
Following the innovations introduced to the ATTUNE, we examined the results of TKR surgeries with the use of an ATTUNE implant compared to surgeries using of the SIGMA implant. We examined differences in (1) pain, (2) range of motion (ROM) (3) stability, (4) knee alignment, (5) function, and (6) patient satisfaction.
Materials and Methods
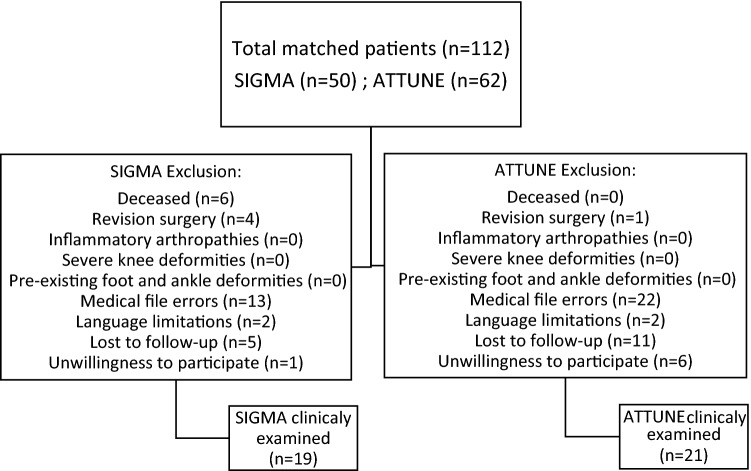
We conducted an analytical cross-sectional study based on preoperative patient data (age, sex, diagnosis, ROM, date of surgery, and implant type) taken from patient files and data collected at postoperative follow-up examinations (ROM, pain, satisfaction, stability, knee alignment, and function). One-hundred-and-twelve cases of patients who underwent TKR surgery in the orthopedic department using the FB CR method without patellar replacement as a result of OA between August 2013 and July 2017, were reviewed by a single surgeon to prevent selection bias. Exclusion criteria were death, revision surgery, inflammatory arthropathies, severe knee deformities, pre-existing foot and ankle deformities, medical file errors, language limitations, lost to follow-up examinations, or unwillingness to participate in the trial. Seventy-two patients were not included in the clinical trial (see Fig. 1).
Fig. 1.
Flowchart of patient inclusion and exclusion
Of the 40 patients included in the study, 21 had an ATTUNE implant and 19 a SIGMA implant. All patients were operated on using the same technique with a FB CR TKR method, without patella replacement. Thirteen (32.5%) patients were men, and 27 (67.5%) were women. The average age was 67.5. Patients were clinically evaluated by a senior physician at least 6 months after the surgery. At the follow-up examination, patients were asked to complete a SF-36 quality-of-life questionnaire translated into Hebrew [20], for the purpose of assessing postoperative satisfaction and function levels. Clinical assessment of the degree of pain (without pain, mild pain, and moderate to severe pain), stability and knee alignment, and ROM was based on the Knee Society score (KSS) [21]. Clinical evaluation of function was based on the knee function score (KFS), which is included in the KSS.
Ethical approval for this study was obtained from the institutional ethics committee.
Statistical Analysis
The statistical analysis was performed using SPSS Statistical Software Version 23 (IBM, Chicago, IL), with statistical significance of p < 0.05 and 1-β statistical power of 0.8. Continuous variables were assessed by the Mann–Whitney test and categorical variables were assessed using Chi-squared. Descriptive statistics are presented as a mean with standard deviation, or a range for continuous variables.
Results
No statistical difference was found regarding age (p = 0.322) and sex (men—p = 0.11, women—p = 0.22), between the two groups. The time period between surgery and follow-up shows a significant difference between the follow-up point of the two groups (p < 0.00001) (Table 1). The mean follow-up period in the SIGMA group was 45.14 ± 5.06 with a range of 37–56 months vs. a mean follow-up period of 23.87 ± 6.48 with a range of 9–33 month in the ATTUNE group.
Table 1.
Comparison of demographic characteristics of the two groups
| Variables | SIGMA | ATTUNE | p value |
|---|---|---|---|
| Mean age, years | 66.58 ± 4.8 | 68.33 ± 7.38 | 0.32 |
| Gender | |||
| Male | 8 (42%) | 5 (24%) | 0.11 |
| Female | 11 (58%) | 16 (76%) | 0.22 |
| Mean follow-up, months | 45.14 ± 5.06 | 23.87 ± 6.48 | < 0.00001 |
| Range of follow-up, months | 37–56 | 9–33 | – |
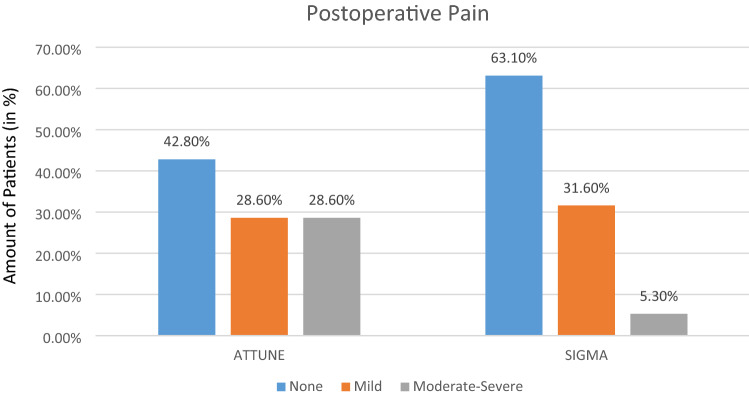
Clinical evaluation: no significant statistical differences were found in the comparison of presurgical knee extension (p = 0.17) or knee flexion (p = 0.32) ranges. In addition, no postoperative significant differences were found between the groups in regard to ROM (extension: p = 0.15, flexion: p = 0.44), change in ROM (extension: p = 0.36, flexion: p = 0.42), knee alignment (p = 0.41) and in the KSS score (p = 0.09). However, a significant difference was found in the KFS score (p = 0.04) with the SIGMA group showing a higher level of functioning (Table 2). No significant difference was found between the groups regarding the postoperative pain level (no pain: p = 0.2, mild pain: p = 0.83, moderate to severe pain: p = 0.053) (Fig. 2).
Table 2.
Differences between the clinical evaluation of the two groups
| Variables | SIGMA | ATTUNE | p value |
|---|---|---|---|
| Preoperative ROM (°) | |||
| Extension | 6.67 (8.16) | 3.95 (4.8) | 0.17 |
| Flexion | 113.33 (13.18) | 114.29 (12.17) | 0.32 |
| Postoperative ROM (°) | |||
| Extension | 0.89 (2.51) | 2.43 (5) | 0.15 |
| Flexion | 122.89 (6.94) | 122.52 (12.76) | 0.44 |
| Improvement in ROM (°) | |||
| Extension | 6.07 (7.65) | 3.19 (3.67) | 0.36 |
| Flexion | 12 (9.27) | 10.14 (11.73) | 0.42 |
| Postoperative valgus (°) | 7.79 (2.3) | 7.95 (1.99) | 0.41 |
| KSS | 85.53 (14.34) | 74.95 (21.51) | 0.09 |
| KFS | 91.32 (13.32) | 81.9 (19.4) | 0.04 |
Fig. 2.
Difference between the groups regarding the postoperative pain level
Quality of life questionnaire: In the SF-36 quality-of-life questionnaire, which the patients filled out during the follow-up examination, no significant differences were found in general health perception (p = 0.39), mental health (p = 0.36), pain (p = 0.14), physical role functioning (p = 0.08), emotional role functioning (p = 0.94), social role functioning (p = 0.42), and change in health status (p = 0.14) measures. Significant statistical differences were found with respect to patients’ sense of vitality (p = 0.02) and physical functioning (p = 0.01), in which the SIGMA group was advantageous in both cases (Table 3).
Table 3.
Differences between the quality of life of the two groups
| Variables | SIGMA | ATTUNE | p value |
|---|---|---|---|
| Physical functioning | 0.91 (0.17) | 0.72 (0.31) | 0.01 |
| Role limitation due to physical health | 0.92 (0.24) | 0.75 (0.4) | 0.08 |
| Role limitation due to emotional health | 0.72 (0.42) | 0.67 (0.48) | 0.94 |
| Vitality | 0.68 (0.21) | 0.48 (0.31) | 0.02 |
| Emotional well-being | 0.69 (0.28) | 0.7 (0.27) | 0.36 |
| Social functioning | 0.78 (0.31) | 0.77 (0.29) | 0.42 |
| Pain | 0.78 (0.28) | 0.63 (0.39) | 0.14 |
| General health | 0.66 (0.16) | 0.62 (0.23) | 0.39 |
| Health change | 0.76 (0.31) | 0.87 (0.25) | 0.14 |
Discussion
Nowadays, rightfully, most of the attention is focused on patient needs. Although knee replacement surgery can be a very successful procedure, studies show that about 20% of patients report dissatisfaction [2]. Using a knee implant which improves ROM and stability and reduces postoperative knee pain leads to an improvement in the patient’s daily functioning. DePuy Synthes developed the ATTUNE knee implant in order to provide a solution to the patients’ needs for stability and freedom of movement using an implant that is adapted to the patient’s anatomy. These improvements will enable proper lifestyle management, with an increase in patient satisfaction with the surgical procedure and a reduction in the need for revisions. The aim of our study was to compare the SIGMA knee implant with the ATTUNE knee implant, with an emphasis on the mechanical changes that DePuy Synthes introduced in the new implant (ATTUNE) and their impact on patients. To the best of our knowledge, only a few studies compared functional outcomes of the two types of implants (SIGMA vs. ATTUNE), and even fewer compared the two implants using the CR FB method without the patellar resurfacing technique. Moreover, little is known regarding quality of life as reported by patients.
In the present study, more patients in the ATTUNE group reported some degree of pain, than in the SIGMA group (57.2% vs. 36.9%). In addition, much fewer patients in the SIGMA group reported moderate to severe pain, compared to the ATTUNE group (5.3% vs. 28.6%), although this difference was not statistically significant. Similarly, Vanitcharoenkul and Unnanuntana [22] found no significant differences in AKP, between the ATTUNE and the SIGMA groups at any time point during a 5-year follow-up. These findings are similar to Maniar et al. [23], who also found no significant differences between the two groups. Nevertheless, Maniar et al. [23] found that at 1-year follow-up, AKP was present in 11% of knees in the ATTUNE group, while only in 9% of knees in the Sigma group. In contrast, our findings are not consistent with those of Ranawat et al. [24], which investigated TKR surgeries using a posterior-stabilizing (PS) implant with patellar replacement, and found that at a 2-year follow-up, more patients in the SIGMA group reported pain, than in the ATTUNE group (28.5% vs. 12.5%).
Notably, in our cross-sectional study, the follow-up period ranged from 37 to 56 months in the SIGMA group, but only from 9 to 33 months in the ATTUNE group. This difference in follow-up duration may potentially lead to bias regarding pain reports, a limitation also observed in the study by Martin et al. [25].
In the present study, no significant differences were found between the research groups in any of the objective KSS measures (ROM, valgus, knee stability) examined during the follow-up period. These findings are consistent with studies by Martin et al. [25], Ranawat et al. [24], and Bateman et al. [26], who found no clinically significant differences in ROM and other KSS measures between the Sigma and the ATTUNE groups. Of note, in the study by Bateman et al. [26] subgroup analyses revealed that mobile bearing Sigma implant resulted in higher PCC (patellar crepitus and clunk). In contrast, our findings are not consistent with several studies that found that it was precisely the ATTUNE implant that showed superior results in terms of objective postoperative ROM measures [24]. However, it seems that this difference in ROM is not clinically significant. Thus, Maniar et al. [23] found that at 3-month follow-up, the ATTUNE group achieved a significantly greater ROM compared to the SIGMA group. However, at 2-year follow-up, both implants had comparable clinical and functional results. Similarly, in the study by Vanitcharoenkul and Unnanuntana [22], the mean ROM at 5-year postoperative was significantly higher in the ATTUNE group than in the Sigma group; however, the difference was small. Of note, no significant differences were found in their study in any of the other outcome measurements at any time point during the 5-year follow-up.
The lack of difference in any of the objective KSS measures in the present study may indicate similar surgical results, since all the surgeries were performed by a single surgeon. It should be noted that it was not possible to accurately estimate the postoperative degree of improvement in ROM since the preoperative measurements were taken by different physicians, with no surveillance of the data collection process. In addition, for some of the patients in the SIGMA group (4 cases that constitute about 21% of the patient group), there was no preoperative data at all.
In the present study, the SIGMA group had an advantage in terms of patients’ sense of vitality, as revealed by the QOL questionnaire. Namely, patients from the SIGMA group reported less fatigue and more energy, compared to the ATTUNE group. The reasons for these differences are not clear, in light of the fact that no statistically significant differences were found in any of the objective KSS measures, although the Sigma group did have some advantages in terms of pain. It is possible that the difference between the groups was due to the differences in the follow-up duration. Therefore, these findings require further investigation.
In the present study, the ATTUNE group reported a more (though not statistically) significant change in postoperative health. It is possible that the timing of questionnaire completion in relation to time that passed since the surgery may have affected the results. Thus, patients in the ATTUNE group may have had better recollection of their presurgical condition, and therefore their sense of change in quality of life might be stronger.
It is acknowledged that mental health and well-being greatly influence the degree of satisfaction following a TKR surgery [7]. In order to rule out biases arising from these factors, patients were asked to assess their mental health using the SF-36 questionnaire. In this study, we found no differences between the groups in QOL variables related to general mental health, emotional or social role functioning, and general health perceptions. Therefore, we believe that the differences between the groups in our study were not due to the influence of mental factors.
Our study has several limitations. First, the population sample was small. Although our study included a single surgeon, a fact that indicates that the same surgical technique was used across all surgeries, examining patients who were operated by a number of surgeons will increase the research population and help reach significance in places where a trend has been observed without significant statistical difference. Second, the preoperative data were collected by different physicians with no control of the data collection technique. In addition, none of the postoperative rehabilitation procedures was monitored. The main limitation in our study is the fact that the postoperative clinical examination was not performed at identical time intervals between the groups. In order to complete our study, further follow-up of patients from the ATTUNE group should be performed after a period of time identical to that in the SIGMA group. In subsequent studies, a prospective study should be performed, and the postoperative follow-up times should be pre-defined.
In conclusion, in this study, we found that FB CR TKR surgery using the SIGMA implant had superior results in postoperative physical function and patients with this implant reported a sense of more vitality and less fatigue in the postoperative clinical follow-ups. We are aware of the possibility that different follow-up periods may have led to differences between the research groups. In our study, a number of trends (not statistically significant) were observed, which point to the superiority of the SIGMA in comparison to the ATTUNE implant, and it is possible that a larger research population will confirm these findings. Despite the mechanical changes and anatomical design of the ATTUNE, we found no advantage regarding ROM, knee stability and alignment, and pain, over the SIGMA implant.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yaron Berkovich and Eden Wiestov equally contributed.
References
- 1.Mahomed NN, Barrett J, Katz JN, Baron JA, Wright J, Losina E. Epidemiology of total knee replacement in the United States Medicare population. Journal of Bone and Joint Surgery American. 2005;87(6):1222–1228. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 2.Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient satisfaction after total knee replacement: a systematic review. HSS Journal. 2018;14(2):192–201. doi: 10.1007/s11420-018-9614-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clinical Orthopaedics and Related Research. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa M, Tone S, Naito Y, Wakabayashi H, Sudo A. Prevalence of persistent pain after total knee arthroplasty, and the impact of neuropathic pain. The Journal of Knee Surgery. 2019;32(10):1020–1023. doi: 10.1055/s-0038-1675415. [DOI] [PubMed] [Google Scholar]
- 5.Arthur CHC, Wood AM, Keenan ACM, Clayton RAE, Walmsley P, Brenkel I. Ten-year results of the Press Fit Condylar Sigma total knee replacement. Bone Joint J. 2013 doi: 10.1302/0301-620X.95B2.29695. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs CA, Christensen CP. Factors influencing patient satisfaction two to five years after primary total knee arthroplasty. Journal of Arthroplasty. 2014;29(6):1189–1191. doi: 10.1016/j.arth.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Clement ND, Burnett R. Patient satisfaction after total knee arthroplasty is affected by their general physical well-being. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21(11):2638–2646. doi: 10.1007/s00167-013-2523-y. [DOI] [PubMed] [Google Scholar]
- 8.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clinical Orthopaedics and Related Research. 1989;248:13–14. doi: 10.1097/00003086-198911000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Kulkarni S, Freeman MA, Poal-Manresa J, Asencio J, Rodriguez J. The patellofemoral joint in total knee arthroplasty: Is the design of the trochlea the critical factor? Journal of Arthroplasty. 2000;15(4):424–429. doi: 10.1054/arth.2000.4342. [DOI] [PubMed] [Google Scholar]
- 10.Keenan ACM, Wood AM, Arthur CA, Jenkins PJ, Brenkel IJ, Walmsley PJ. Ten-year survival of cemented total knee replacement in patients aged less than 55 years. Bone Joint J. 2012;94–B(7):928–931. doi: 10.1302/0301-620X.94B7.27031. [DOI] [PubMed] [Google Scholar]
- 11.Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J. 2014;96–B:96–100. doi: 10.1302/0301-620X.96B11.34152. [DOI] [PubMed] [Google Scholar]
- 12.Jin QH, Lee WG, Song EK, Kim WJ, Jin C, Seon JK. No difference in the anteroposterior stability between the GRADIUS and multi-radius designs in total knee arthroplasty. Knee. 2020;27(4):1197–1204. doi: 10.1016/j.knee.2020.05.019. [DOI] [PubMed] [Google Scholar]
- 13.Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ. The influence of total knee arthroplasty geometry on mid-flexion stability: An experimental and finite element study. Journal of Biomechanics. 2013;46(7):1351–1357. doi: 10.1016/j.jbiomech.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Fitzpatrick CK, Clary CW, Laz PJ, Rullkoetter PJ. Relative contributions of design, alignment, and loading variability in knee replacement mechanics. Journal of Orthopaedic Research. 2012;30(12):2015–2024. doi: 10.1002/jor.22169. [DOI] [PubMed] [Google Scholar]
- 15.Clary, C. W., Fitzpatrick, C. K., Maletsky, L. P., & Rullkoetter, P. J. (2012). Improving dynamic mid-stance stability: An experimental and finite element study. ORS 2012 Annual Meeting [DOI] [PubMed]
- 16.Senavongse W, Amis AA. The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: A biomechanical study in vitro. Journal of Bone and Joint Surgery British. 2005;87(4):577–582. doi: 10.1302/0301-620X.87B4.14768. [DOI] [PubMed] [Google Scholar]
- 17.Conlan T, Garth WP, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. Journal of Bone and Joint Surgery American. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. American Journal of Sports Medicine. 1998;26(1):59–65. doi: 10.1177/03635465980260012701. [DOI] [PubMed] [Google Scholar]
- 19.Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surgery, Sports Traumatology, Arthroscopy. 2012;20(2):331–336. doi: 10.1007/s00167-011-1598-6. [DOI] [PubMed] [Google Scholar]
- 20.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Knee society score - orthopaedic scores. http://www.orthopaedicscore.com/scorepages/knee_society_score.html. Accessed 6 May 2017
- 22.Vanitcharoenkul E, Unnanuntana A. Midterm functional recovery of Total knee arthroplasty patients compared between the ATTUNE knee system and the press fit condylar (PFC) SIGMA knee system. BMC Musculoskelet Disorders. 2021;22(1):620. doi: 10.1186/s12891-021-04464-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maniar RN, Bhatnagar N, Bidwai R, Dhiman A, Chanda D, Sanghavi N. Comparison of patellofemoral outcomes between attune and PFC sigma designs: A prospective matched-pair analysis. Clinics in Orthopedic Surgery. 2022;14(1):96–104. doi: 10.4055/cios20130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ranawat CS, White PB, West S, Ranawat AS. clinical and radiographic results of attune and PFC sigma knee designs at 2-year follow-up: A prospective matched-pair analysis. Journal of Arthroplasty. 2017;32(2):431–436. doi: 10.1016/j.arth.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 25.Martin JR, Jennings JM, Watters TS, Levy DL, McNabb DC, Dennis DA. Femoral implant design modification decreases the incidence of patellar crepitus in total knee arthroplasty. Journal of Arthroplasty. 2017;32(4):1310–1313. doi: 10.1016/j.arth.2016.11.025. [DOI] [PubMed] [Google Scholar]
- 26.Bateman DK, Preston JS, Mennona S, Gui E, Kayiaros S. Comparison between the attune and pfc sigma in total knee arthroplasty: No difference in patellar clunk and crepitus or anterior knee pain. Orthopedics. 2020;43(6):e508–e514. doi: 10.3928/01477447-20200812-05. [DOI] [PubMed] [Google Scholar]