Abstract
Background
Midline surgical incision used in Total Knee Arthroplasty (TKA) is associated with iatrogenic injury to the infrapatellar branch of the saphenous nerve, which leads to neuropathic dermatitis around the healed surgical scar. There are very few studies with a limited number of cases that have reported this complication. We evaluated the incidence of neuropathic dermatitis and its implication for the functional outcome in TKA patients.
Methodology
Patients who underwent primary TKA between 1 January 2010 and 31 August 2019 and presented in follow-up with sensory disturbances and skin lesions adjacent to the surgical incision were evaluated in this study.
Results
A total of 3318 patients with 4282 TKAs were included, of which 188 patients presented with the clinical picture of neuropathic dermatitis. There were 136 females and 52 males with a mean age of 67.13 years (range 37–92 years). The mean duration from surgery to the appearance of skin lesions was 4.4 months (range 2–6 months), and they resolved at a mean duration of 7.67 (range 6–12) weeks. In our study, we found an incidence of 5.52%. All these patients had a stable and well-functioning knee at the time of presentation of the lesion with a mean Knee Society Score (KSS) of 92 (range 84–96).
Conclusion
In our study, we found the incidence of neuropathic dermatitis to be 5.52%, without any long-term implication on the functional outcome of operated knees. For a self-limiting complication of midline knee incision of TKA, it either resolves on its own or requires a short duration of topical steroid application.
Keywords: Neuropathy dermatitis, Autonomic denervation dermatitis, SKINTED, Total Knee Arthroplasty, Infrapatellar branch, Saphenous nerve
Introduction
Worldwide, Total Knee Arthroplasty (TKA) is the most commonly performed elective surgery for pain relief in patients with severe knee osteoarthritis [1]. The most frequently used surgical approach to perform TKA is a midline surgical incision with medial parapatellar arthrotomy [2]. The midline surgical incision used for TKA is associated with iatrogenic injury to the infrapatellar branch of the saphenous nerve (IPBSN) [3, 4]. The reported incidence of IPBSN injury with the midline surgical incision used for knee surgeries, in literature, is up to 70% [3, 4]. IPBSN is a purely sensory nerve that arises from the saphenous nerve. After exiting the adductor canal, it becomes subcutaneous and traverses from the medial to the lateral side below the patella. It provides cutaneous sensation to the anterior knee, and the innervation can reach up to the lateral aspect of the knee [2–4]. There are several variations described in the course of IPBSN, of which the most common is the presence of 1–3 sub-branches of IPBSN that cross the knee and give terminal cutaneous sensory supply to the anterolateral aspect of the knee [2].
Iatrogenic transaction of the IPBSN following midline knee incision for TKA leads to an area of altered skin sensation lateral to the skin incision (which ranges from mild paresthesia to complete anesthesia), and pain, which can lead to knee joint stiffness and poor functional outcome [2, 5, 6]. In the area of altered skin sensation, cutaneous lesions from a simple rash to extensive eruptions, papules, or macules may appear [5, 6]. Similar skin lesions were also described after other surgeries around the knee like arthroscopic medial meniscus cyst debridement [7], arthroscopic surgery for cruciate ligament reconstruction mainly using bone-patellar tendon-bone graft, and saphenous venous graft harvest surgery for coronary artery bypass [4, 8, 9].
In literature, various terms have been used for this phenomenon by different authors, such as neuropathic dermatitis [10], autonomic denervation dermatitis (ADD) [8], and SKINTED (surgery of the knee, injury to infrapatellar branch of the saphenous nerve, traumatic eczematous dermatitis) [9]. Skin lesions usually appear 2–3 months after surgery, and if undiagnosed, they may get secondarily infected and can cause periprosthetic joint infection. The probable mechanism for this entity is the disruption of the autonomic constituents of the skin, which leads to an alteration in the microcirculation and aberrant differentiation and proliferation of keratinocytes. The inflammatory cascade following the injury can be another potential mechanism [11]. There are very few published studies, either case reports or with a limited number of patients, which described the incidence and implication of neuropathic dermatitis in relation to TKAs. The reported incidence of neuropathic dermatitis in literature is 4.4% [6] in a series of 207 cases; however, we need a study with a larger number of cases to find the exact incidence. Hence, this study aims to estimate the incidence of neuropathic dermatitis and its implication on knee function following TKA.
Materials and Methods
In a retrospective analysis of prospectively collected data, patients of either sex who underwent primary TKA for osteoarthritis between 1 January 2010 and 31 August 2019 at our institute, and presented with skin lesions adjacent to the surgical incision at the lateral aspect during the follow-up period in the out-patient department, were identified. Exclusion criteria were: Patients who underwent TKA for inflammatory arthritis (e.g., rheumatoid arthritis, psoriatic arthritis), pre-existing skin allergy, pre-existing skin disease before surgery, patients having fungal infection in the body, history of Leprosy, allergy to any metallic substance, and intake of steroids for any pre-existing disease.
All these patients had been operated on under appropriate anesthesia (175 under regional and eight patients under general anesthesia) through a midline surgical incision with medial parapatellar arthrotomy by a single senior arthroplasty surgeon. In all patients, implant used was cemented posterior stabilized fixed bearing (PFC sigma, DePuy). The femoral and tibial components were made up of cobalt-chromium, and the insert was made up of ultrahigh-molecular-weight highly cross-linked polyethylene. Patellar resurfacing was not done in any of the patients included in the study. In all patients, the cement used for implant fixation was gentamycin mixed with high-viscosity bone cement (SmartSet, DePuy Synthes). Periarticular cocktail (60 cc 0.2% ropivacaine, 0.3 cc 1:1000 adrenaline, 2 cc ketorolac, 60 mg clonidine, and fentanyl 100 µg in 2 ml) infiltration was given in all knees intraoperatively for pain control.
Subcutaneous closure was done using an absorbable suture (Ethicon absorbable surgical suture Vicryl), and metal staples were used for skin closure. Wound dressing was done with a dry cotton gage and bandage. A surgical-site inspection was done on a postoperative day one, and the subsequent dressing was done with an occlusive dressing (3 M Tegaderm HP + Film Dressing). In none of the patients, the adhesive dressing was used during the postoperative period. None of our patients have reported any allergic skin reaction to betadine used for preoperative painting and intra-operative occlusive dressing used to cover the incision site, either in the postoperative period or during follow-up.
During the follow-up period, they were evaluated for any localized dry, scaly erythematous, non-itching skin lesions, discoloration of the skin or sensory loss over the skin adjacent to the surgical incision was documented. Patients who presented with skin lesions adjacent to the surgical incision were seen by a dermatologist and followed up in OPD every 2 weeks till the complete resolution of skin lesions and after that in every 6 months to watch for any recurrence of lesions till one year after the complete resolution of the lesion. Institutional review board approval was obtained, and informed written consent was taken from all the patients included in this study.
Statistical Analysis
All data are presented as mean values with range and percentage, and no specific statistical test was applied for data analysis. The incidence was estimated by comparing the patients identified with a skin lesion and symptoms to the total number of TKA operated on during the study period.
Results
A total of 3318 patients with 4282 TKAs were included in this study. 964 patients underwent bilateral TKA, and 2354 patients underwent unilateral TKA during the study period. 188 patients (136 females and 52 males) who presented with a skin lesion or symptoms of neuropathic dermatitis were included in the study. Five patients were lost to follow-up after 8 weeks postoperatively and were excluded from the final analysis. Finally, 183 patients, 91 with bilateral and 92 with unilateral dermatitis, were included. The mean age of the patients was 67.13 years (range 37–92 years). The mean body mass index was 28.2 (range 19.4–36.3). Sixty-three patients had diabetes mellitus, of which 53 patients had optimum glycaemic control remaining 11 were optimized before surgery. The mean duration of surgery for an individual knee was 66 min (range 110–45 min). The mean duration from surgery to the appearance of skin lesions was 4.4 months (range 2–6 months) (Table 1). The minimum follow-up for all patients post-TKA was 2 years.
Table 1.
Patients and lesion details included for final analysis
| Number of patients | 183 |
| Mean age | 67.13 (range 37–92) years |
| Gender ratio (Female:Male) | 136:47 |
| Knee involvement | 91 bilateral and 92 unilateral |
| Type of implant used | CoCr (Cobalt chrome) |
| Site of skin lesion appearance | Lateral to surgical incision in all patients |
| Mean time from surgery to dermatitis | 4.4 (range 2–6) months |
| Mean time taken for healing | 7.67 (6–12) weeks |
All patients who developed skin lesions had an uneventful postoperative period until the appearance of skin lesions. None of these patients had a history of use of any new topical medication. On thorough dermatological examination, no similar skin lesion was found anywhere in the body. All patients had varying degrees of sensory loss ranging from hypoesthesia to complete sensory loss over lateral to the surgical incision. None of them had sensory loss medial to the midline surgical incision. Initially, a small, non-pruritic red, scaly rash appeared, gradually increasing in size over a few days to a week. Skin lesions varied from small erythematous scaly non-itchy plaque or patch to a sizeable well-demarcated area of hyperpigmented patch exclusively on the lateral aspect of the midline surgical incision, corresponding to the skin area supplied by IPBSN. There was no local rise in temperature, tenderness, or vasodilation over the skin involved. The lesion was pruritic in 18 (9.8%) patients (Figs. 1, 2, 3).
Fig. 1.

A scaly erythematous skin lesion, right knee limited to lateral aspect of the healed midline surgical incision
Fig. 2.

Resolving scaly erythematous skin lesion, right knee limited to lateral aspect of the healed midline surgical incision
Fig. 3.

Resolving hyperpigmented scaly skin lesion over the right knee limited to lateral aspect of the healed midline surgical incision
Complete blood counts and relevant serological evaluation of all patients were normal. Radiological assessment of the affected knee showed a well-aligned and well-cemented implant in place. Based on the clinical and hematological picture (normal values of ESR, q-CRP, total and differential leucocyte counts), absence of prosthetic joint infection, and superficial skin infection, a diagnosis of neuropathic dermatitis was made. The incidence of neuropathic dermatitis in our study was 5.52% per number of patients (183 in 3318 patients) and 6.37% per number of TKR. We did not find an increased occurrence of neuropathic dermatitis in relation to the duration of surgery or diabetes mellitus.
Topical application of mildly potent steroid ointment twice a day and an emollient were prescribed to all patients. Additionally, those with pruritic rash were given oral anti-histaminic medications for 7 days. Infection of the lesion was noted in only one patient with bilateral TKR, treated with oral antibiotics for 10 days, and complete resolution of infection was seen at 12 weeks (Fig. 4). None of the patients developed PJI. The mean time for resolution of skin lesions was 7.67 (6–12) weeks. In 7 patients, healing took a slightly longer period, up to 12 weeks. None of these patients had a recurrence till 1 year of follow-up after the complete resolution of the skin lesions. Sensory loss gradually improved in all patients over the period to near normal in 178 patients. 5 (2.7%) patients still have a significant level of hypoesthesia. All patients were doing well and had a stable and well-functioning knee at the time of the presentation of the rash, with a mean Knee Society Score (KSS) of 92 (Range 84–96). 7 patients who had delayed resolution of skin lesions had temporary deterioration of KSS till the resolution of skin lesions, which improved and comparable to other patients.
Fig. 4.
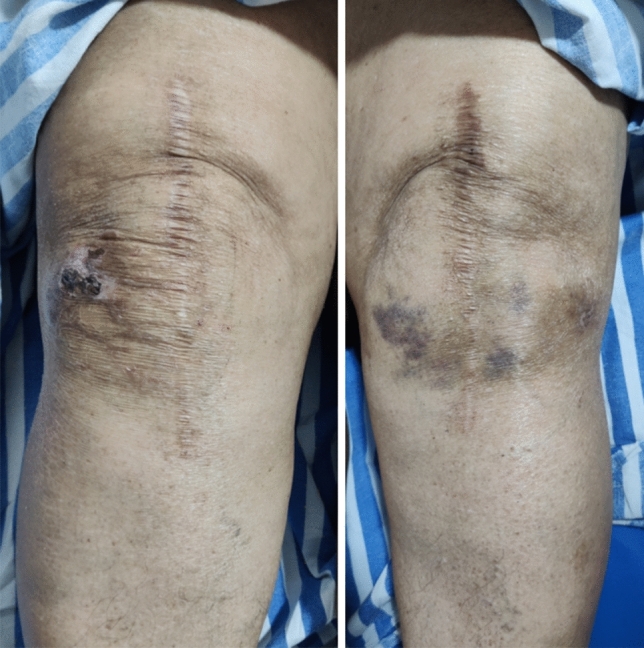
A Bilateral knee involvement, right knee shows infected resolving skin lesion. B Left knee resolved skin lesion limited to lateral aspect of healed midline surgical incision
Discussion
The reported incidence of iatrogenic IPBSN injury in literature is 22–70% following midline knee incisions [12]. The most common skin-related symptom of iatrogenic IPSBN injury after TKA is an altered skin sensation lateral to the surgical incision. In a few cases, skin lesions manifested as neuropathic dermatitis 2–3 months postoperatively, limited to the lateral side and do not cross the midline. There are various anatomical variations in the branching pattern of IPBSN, even in two different limbs of the same patient. This explains the fact that, in a bilateral case of TKA, some patients have dermatitis on one side only while others have it on both sides [2, 13].
There are few published articles with a limited number of cases that describe neuropathic dermatitis in TKA patients. Satku et al. [14] in their series of 4 TKA, first described dermatitis complicating the operative site and hypothesized loss of autonomic and sensory function as the contributory cause. Later, in the year 2009, Verma et al. [9] hypothesized that iatrogenic injury to the cutaneous innervation around the operated knee alters the barrier function of the epidermis, which results in water loss across the epidermis causing xerosis and eventually eczematous dermatitis. They proposed the term SKINTED for this entity in TKA patients. On the contrary, Sharquie et al. [10] proposed the term neuropathic dermatitis They suggested that during nerve regeneration, nerve terminals various other neuropeptides have a role in regulating the immediate and delayed types of skin hypersensitivity reaction. However, Madke et al. [8] suggested the term ADD (autonomic denervation dermatitis) for the skin lesion that appears after traumatic denervation of various autonomic organs in the skin.
Neuropathic dermatitis needs to be distinguished from the other types of skin lesions or hypersensitivity reactions that may occur in the postoperative period. The skin hypersensitivity reaction due to betadine/iodine solution wound dressing materials is usually localized to the skin contact area and can be present anywhere around the knee joint.
Allergic dermatitis presents acutely within 5–14 days of exposure to the offending agent. The lesions are intensely pruritic erythematous papules or vesicles [15]. On the other hand, metal hypersensitivity is a rare complication wherein patients present with joint swelling, inflammation, and very rarely localized or generalized dermatitis around the neck, buttocks, or extremities. A pruritic, erythematous, scaly rash appears all around the surgical site 2 months to 2 years after the surgery. A family history of metal hypersensitivity is usually present. Although skin lesions due to metal hypersensitivity respond well to topical steroids, recurrence is common after treatment stops. Metal hypersensitivity affects both the operated knees [16, 17]. Although hypersensitivity reaction to vicryl suture is infrequent, it can present as erythema, pruritus, and epidermal thickening all around the suture site. However, this usually presents on both sides of the incision [18, 19].
Neuropathic dermatitis is a self-limiting condition that requires a mild topical steroid application and resolves in a few weeks to months without recurrence. The diagnosis of neuropathic dermatitis was mainly based on the clinical characteristic of the skin lesion and its specific location.
Nazeer et al. [6] reported the incidence of neuropathic dermatitis to be 4.4% in their series of 203 patients. In contrast, we found an incidence of 5.52% in our study, which is higher than all previous studies. The higher percentage of occurrence of neuropathic dermatitis in our series may be due to a larger number of patients included in our study (3318 patients with 4282). It may be possible that neuropathic dermatitis is a relatively unrecognized, neglected, and undocumented entity.
We did not find any adverse effect of neuropathic dermatitis on knee function in any of the patients. A similar result was presented by Dhillon et al. [12] in their recent systematic review. This under-documented complication of TKA can be prevented by minimizing the iatrogenic injury to IPBSN, which triggers neuropathic dermatitis. A lateral arthrotomy for TKA in place of the usual medial parapatellar arthrotomy can be explored to avoid nerve injury. The anterolateral skin incision carries less risk of injury to the nerve than the midline skin incision [20]. However, the lateral parapatellar arthrotomy has its complications. The limitations of this study are, a retrospective, single-center study, there may be inaccuracy in calculation due to loss to follow-up, and there was no comparative group. Second, the diagnosis of neuropathic dermatitis was based on clinical examination only, and we did not perform a histopathological examination.
We also present a literature review of reported studies on neuropathic dermatitis in TKA patients, as shown in Table 2.
Table 2.
Literature review of reported cases of neuropathy dermatitis
| Sl no | Author/year | Study design | Number of patients | Number of patients developed skin lesion | Sex (M/F) (developed lesion) | Age (years) | Surgery in past | Site of skin lesion in relation to incision | Time since surgery to appearance of skin lesion | Mean Time taken for complete healing lesion | H/o any topical agent/allergen contact in pre- or postop periods | H/o metal allergy | Approach used in surgery | Knee function |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Satku et al. (1993) [7] | Case report | 4 (1patient developed bilateral) |
1. TKA-bilatteral 2. Chondromalcia patellae 3. TKA 4. TKA |
TKA-2/1 Chondromalacia patellae-M |
1.70 2.28 3.75 4.68 |
TKA-2 Patellar chondroplasty-1 |
Lateral to the incision-TKA Patellae- lateral to incision |
1.TKA-5 months 2.Chondroplasty-4 months 3.TKA-9 months 4. TKA-4 months |
1. 1 year 2. improvement after 2. years 3. 10 months 4. 8 months |
None | NR |
1. TKA-medial parapatellar 2. Lateral patellar |
NR |
| 2 | Logue et al. (1996) [8] | Case report | 1 | 1 | M | 46 |
Arthroscopic Partial medial meniscectomy, & enlargement of hiatus and meniscal cyst debridement |
Over the medial aspect of his left lower leg | 3 months | Improved in 1 month | None | NR | NR | NR |
| 3 | Verma et al. (2009) [9] | Case series | 55 | 55 (only 16 were available for regular follow-up) | Out of 16- 11/5 | TKA | Lateral in 12 and in 4 patients on both sides of incision | 3 weeks to 4 months | NR | None | NR | NR | NR | |
| 4 | Sharquie et al. (2011) [10] | Case report | 7 | 7 |
5/2 TKA-F |
Mean-58 (50–66) TKA-60 |
1-TKA 6-Saphe-nous vein grafting |
Lateral side of the incision scar |
2–3 months TKA-around 3 months |
NR | NR | NR | NR | NR |
| 5 | Madke et al. (2017) [6] | Case report | 10 | 10 |
9/1 TKA-3/2 OR-Male Sephanous -3/1 |
TKA-mean-60.8 OR-55 |
5-TKA 4 ‑Saphenous vein graft & 1-OR for fracture femur |
OR-Lateral aspect of thigh TKA- Not mentioned |
Overall-6 months-3 years TKA &OR-10 months-2 years |
NR | None | NR | NR | NR |
| 6 | Barbera et al. (2018) [11] | Case report | 1 bilateral | Bilateral knee | M | 65 | TKA | Lateral to incision | 3 months | 6 months | None | NR | NR | NR |
| 7 | Pathania et al. (2019) [12] | Case report | 1 bilateral | Bilateral knee | Female | 60 | TKA | Lateral to incision in both knees | 3 months | 2 weeks for improvement | None | NR | NR | NR |
| 8 | Mathur et al. (2019) [13] | Case report | 2 | Both bilateral knee |
1-M 2-F |
1–60 2–49 |
TKA | NR |
1–16 months 2–11 months |
NR | None | NR | NR | NR |
| 9 | Nazeer et al. (2020) [14] | Prospective cohort study | 148 (55b/l) = 203 knees | 8 (1 b/l) = 9 knees | 1/7 | Mean 64.5 (58–78) | TKA | Lateral to surgical site | Mean 4 (3–6) months | 6.33 (4–10) weeks | None | None | Medial parapatellar in all | Stable, mean KSS-90 (84–94)- in all |
| 10 | Present Study | Retrospective study | 3318 patients with 4282 knees | 183 (92 Bilateral) TKA | 47/136 | 67.13 (37–92) years | TKA | Lateral to surgical site | 4.4 (2–6) months | 7.67 (range 6–12) weeks | None | None | In all patients medial parapatellar | KSS-92 (84–96) |
TKA Total Knee Arthroplasty, KSS Knee Society Score, OR open reduction
Conclusion
The incidence of neuropathic dermatitis in our study is 5.52%, and it does not have any long-term implications on functional outcomes after TKA. Neuropathic dermatitis is an under-reported benign complication of TKA that either resolves on its own or requires topical steroid application for a short duration. Awareness regarding this benign self-limiting complication and proper counseling of patient will alleviate the patient’s undue agony and anxiety.
Author Contributions
All the above-mentioned authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Funding
None.
Declarations
Conflict of Interest
The authors declare no competing interests.
Ethical standard statement
Prior ethical approval obtained.
Informed Consent
Obtained from all the participant patients.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ravikumar Mukartihal, Email: doctorcmravi@gmail.com.
Rajesh Kumar Rajnish, Email: duktiraj@gmail.com.
Phuljit Patowary, Email: drphuljit@gmail.com.
Udit Kumar Biswal, Email: uditkumarbiswal@gmail.com.
Pradeep A. Ramesh, Email: drpradeepannur.sr@gmail.com
Sharan Shivaraj Patil, Email: drsharanpatil@sparshhospital.com.
References
- 1.Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R. Total Knee Arthroplasty: improving outcomes with a multidisciplinary approach. Journal of Multidisciplinary Healthcare. 2018;11:63–73. doi: 10.2147/JMDH.S140550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James NF, Kumar AR, Wilke BK, Shi GG. Incidence of encountering the infrapatellar nerve branch of the saphenous nerve during a midline approach for Total Knee Arthroplasty. J Am Acad Orthop Surg Glob Res Rev. 2019;3(12):e19.00160. doi: 10.5435/JAAOSGlobal-D-19-00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ackmann T, Von Düring M, Teske W, et al. Anatomy of the infrapatellar branch in relation to skin incisions and as the basis to treat neuropathic pain by cryodenervation. Pain Physician. 2014;17(3):E339–E348. doi: 10.36076/ppj.2014/17/E339. [DOI] [PubMed] [Google Scholar]
- 4.Kerver AL, Leliveld MS, den Hartog D, et al. The surgical anatomy of the infrapatellar branch of the saphenous nerve in relation to incisions for anteromedial knee surgery. Journal of Bone and Joint Surgery. American Volume. 2013;95(23):2119–2125. doi: 10.2106/JBJS.L.01297. [DOI] [PubMed] [Google Scholar]
- 5.Mistry D, O'Meeghan C. Fate of the infrapatellar branch of the saphenous nerve post Total Knee Arthroplasty. ANZ Journal of Surgery. 2005;75(9):822–824. doi: 10.1111/j.1445-2197.2005.03532.x. [DOI] [PubMed] [Google Scholar]
- 6.Nazeer M, Ravindran R, Katragadda BC, Muhammed EN, Rema DTJ, Muhammed MN. SKINTED: a rare complication after Total Knee Arthroplasty. Arthroplast Today. 2020;6(4):1028–1032. doi: 10.1016/j.artd.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Logue EJ, 3rd, Drez D., Jr Dermatitis complicating saphenous nerve injury after arthroscopic debridement of a medial meniscal cyst. Arthroscopy. 1996;12(2):228–231. doi: 10.1016/S0749-8063(96)90017-1. [DOI] [PubMed] [Google Scholar]
- 8.Madke B, Mhatre M, Kumar P, Singh AL, Patki A. Autonomic denervation dermatitis: a new type of eczematous dermatitis. Clinical Dermatology Review. 2017;1:61–64. doi: 10.4103/CDR.CDR_8_17. [DOI] [Google Scholar]
- 9.Verma SB, Mody BS. Explaining a hitherto nameless condition: 'SKINTED'. Clinical and Experimental Dermatology. 2009;34(7):e465–e466. doi: 10.1111/j.1365-2230.2009.03522.x. [DOI] [PubMed] [Google Scholar]
- 10.Sharquie KE, Noaimi AA, Alaboudi AS. Neuropathy dermatitis following surgical nerve injury. Case Reports in Dermatological Medicine. 2011;2011:234185. doi: 10.1155/2011/234185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Make B, Mhatre M, Kumar P, et al. Autonomic denervation dermatitis: a new type of eczematous dermatitis. Clinical Dermatology Review. 2017;1:61–64. doi: 10.4103/CDR.CDR_8_17. [DOI] [Google Scholar]
- 12.Dhillon MS, Jindal K, Shetty VD, et al. Autonomic denervation dermatitis: a relatively undocumented ‘ADD’itional complication of total knee replacements and other surgeries around the knee. JOIO. 2021 doi: 10.1007/s43465-021-00520-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ebraheim NA, Mekhail AO. The infrapatellar branch of the saphenous nerve: an anatomic study. Journal of Orthopaedic Trauma. 1997;11(3):195–199. doi: 10.1097/00005131-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Satku K, Fong PH, Kumar VP, Lee YS. Dermatitis complicating operatively induced anesthetic regions around the knee. A report of four cases. The Journal of Bone & Joint Surgery. 1993;75(1):116–118. doi: 10.2106/00004623-199301000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Chalmers BP, Melugin HP, Sculco PK, et al. Characterizing the diagnosis and treatment of allergic contact dermatitis to 2-Octyl cyanoacrylate used for skin closure in elective orthopedic surgery. Journal of Arthroplasty. 2017;32(12):3742–3747. doi: 10.1016/j.arth.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 16.Saccomanno MF, Sircana G, Masci G, Cazzato G, Florio M, Capasso L, Passiatore M, Autore G, Maccauro G, Pola E. Allergy in total knee replacement surgery: is it a real problem? World Journal of Orthopedics. 2019;10(2):63–70. doi: 10.5312/wjo.v10.i2.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lachiewicz PF, Watters TS, Jacobs JJ. Metal hypersensitivity and Total Knee Arthroplasty. Journal of American Academy of Orthopaedic Surgeons. 2016;24(2):106–112. doi: 10.5435/JAAOS-D-14-00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stocco C, Berton F, et al. Vicryl hypersensitivity test with histological response. Dermatitis. 2016;27(3):145–146. doi: 10.1097/DER.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 19.Ogbechie OA, Paul S, Schalock PC. A technique for identifying vicryl suture hypersensitivity. Dermatitis. 2014;25(6):370–371. doi: 10.1097/DER.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 20.Tsukada S, Kurosaka K, Nishino M, Hirasawa N. Cutaneous hypesthesia and kneeling ability after Total Knee Arthroplasty: a randomized controlled trial comparing anterolateral and anteromedial skin incision. Journal of Arthroplasty. 2018;33(10):3174–3180. doi: 10.1016/j.arth.2018.06.010. [DOI] [PubMed] [Google Scholar]


