Abstract
Background
Considering various factors that influence meniscal repairability, Ortho One PROMT score (OPS) was proposed in 2019. With an increased understanding of factors influencing meniscal repair and by analysis of OPS predictions and repair results, a modified PROMT score (MPS) has been formulated. The objective of this study is to assess the superiority of MPS over OPS.
Methods
Age, chronicity, and pattern of tears were found to be important contributors to false-negative results of OPS. Considering these factors, MPS was designed. A prospective, double-blinded study was conducted between November 2020 and May 2021. Sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value, negative predictive value, and accuracy of both scores were calculated. Receiver Operating Characteristic (ROC) curve was plotted.
Results
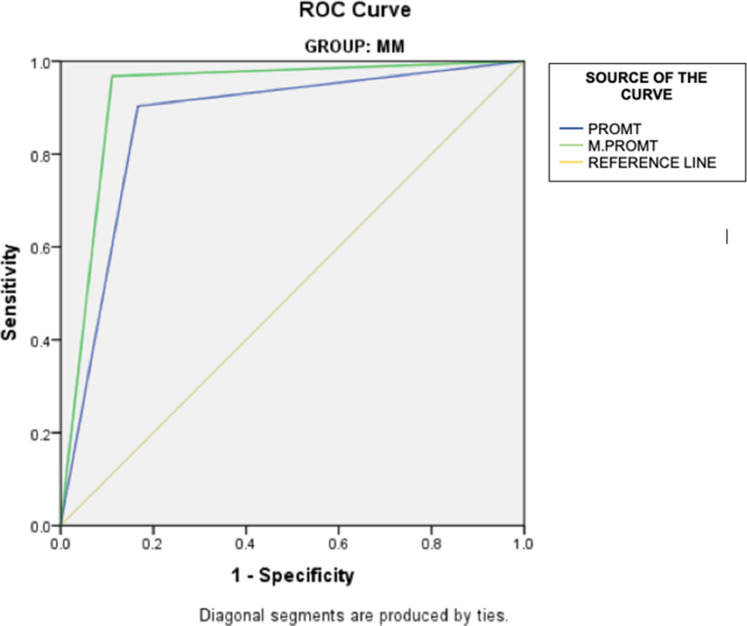
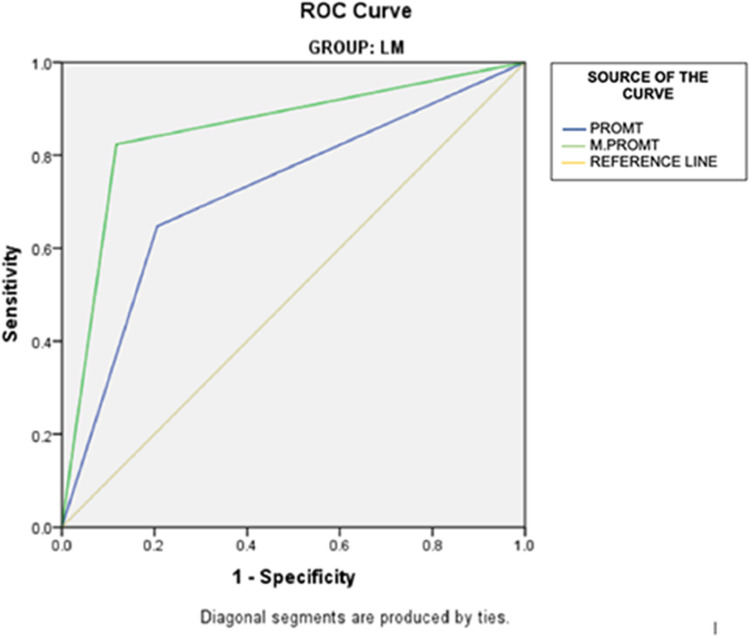
Of 133 meniscal tears, 100 met the inclusion criteria. In predicting meniscal repairability, OPS demonstrated sensitivity and specificity of 90.32% and 83.33% medially and 64.71% and 79.41% laterally. MPS had sensitivity and specificity of 96.77% and 88.89% medially and 82.35% and 88.24% laterally. Both scores showed good statistical significance (p < 0.05) in predicting meniscal reparability. For medial meniscus repairability, area under the ROC curve was 0.868 for OPS and 0.928 for MPS. For lateral repairability, the area under the curve was 0.721 for OPS and 0.853 for MPS.
Conclusion
MPS will serve as a simple and more effective tool for surgeons to predict meniscal repairability, thus enhancing their pre-surgical preparedness. This tool will also help surgeons to realistically counsel their patients and to achieve optimal patient.
Keywords: PROMT score, Meniscus, Meniscus repair, Repairability
Introduction
The menisci are the most injured structures in the knee. These fibrocartilaginous wedges play a pivotal role as joint fillers helping in load transmission and improving anteroposterior stability [1]. The meniscal tear can be traumatic or degenerative. Traumatic meniscal tears are commonly caused by twisting and pivoting maneuvers, especially during sporting activities. The ESSKA (European Society for Sports Traumatology, Knee Surgery, and Arthroscopy) recently came up with a definition for “traumatic meniscal injury” as a meniscal tear that is associated with a sufficient knee injury and sudden onset knee pain [2].
With clarity on the anatomical and functional role of menisci in recent years, meniscal preservation by repair has become the accepted treatment modality wherever possible [3, 4]. Meniscal repair is expensive, technically challenging, and requires tear pattern-specific inventory when compared to less expensive technically simple meniscal excision [5, 6]. Conventional Magnetic Resonance Imaging (MRI) although the gold standard of diagnosis, is less effective in predicting the reparability of meniscal tears [7]. Van Dyck et al. in their study concluded that the 3 Tesla MRI offers little advantage in terms of improving sensitivity and specificity in predicting meniscal tears[8]. A meniscal repairability prediction tool will thus help the surgeon to be prepared for repair and explain to the patient the prognosis of surgery. Repairability of the meniscal tear, apart from the morphology of the tear, depends on several other factors like age, degenerative changes in the joint, and duration of the tear [2]. Considering all these factors, we proposed the Ortho One PROMT (Predictability of Repair Of Meniscal Tears) score in 2019 [9].
The Ortho One PROMT score predicts medial meniscus repair with a sensitivity of 90.9% and a specificity of 93.2%. It predicts lateral meniscus repair with a sensitivity of 69.2% and specificity of 78.8%. With an increased understanding of factors influencing meniscal repair and by analysis of the previous repair results, we have formulated the modified PROMT score. The objective of this study is to assess the accuracy of the modified PROMT score in predicting meniscus repair and its superiority over the previous PROMT score. We hypothesized that the Modified PROMT Score (MPS) has improved sensitivity and specificity in predicting the reparability of meniscal tear when compared to the Ortho One PROMT Score (OPS).
Materials and Methods
Modified PROMT Score
Between 2018 and 2019, we analyzed meniscal surgeries retrospectively to improve the specificity and sensitivity of the PROMT score. We performed 320 meniscal surgeries of which 232 were repairs and 88 were excision surgeries. The PROMT score predicted medial meniscus repair with a sensitivity of 91% and a specificity of 92.3%. It predicts lateral meniscus repair with a sensitivity of 66% and specificity of 75%. We found that age and chronicity were important contributors to false-negative results during this period. We had 32 patients with a meniscal tears in the age group of 40 to 50 years and 15 patients in the age group of more than 50 years. We noticed that 24 patients of the 40–50 years age group had undergone successful meniscal repairs. 5 of the remaining 8 patients had irreparable tears because of tear pattern, zone of tear, and chronicity of the tear. A degenerative component was seen in only the rest 3 patients. The reparability was significantly reduced beyond 50 years of age (P = 0.03). The meniscal repairs were done in only 2 of the 15 patients. This decrease in repairability was due to the degenerative component present in the meniscal tears. As opposed to the previous proposal that tears of more than 1 year were less repairable, we had successfully repaired quite a good number of tears that were over 1 year of duration. We had 34 tears of more than one-year duration of which 27 were repaired. However, we did find that repairing chronic tears over 2 years of duration was difficult. Only 2 out of 12 tears of more than 2 years duration were repaired. This was due to the increased association of complex pattern tears (P = 0.024) when the duration of the tears is more than 2 years. Regarding the pattern of tears, we noticed that the complex tears were less amenable to repair than bucket-handle tears.
Incorporating these changes, we designed the MPS. The MPS and OPS are elaborated on in Tables 1 and 2 respectively. To validate the superiority of this score over the OPS, we conducted a prospective, double-blinded study was conducted between November 2020 and May 2021. Consecutive traumatic meniscal tears presenting to the hospital during this period were assessed preoperatively with the OPS and MPS to predict their reparability. 1.5 T MRI was used for imaging and the proton density fat-saturated, T1-weighted, and T2-weighted images were used in sagittal, coronal, and axial sequences to study the meniscus injuries. The inclusion criteria were isolated traumatic meniscal tears, cruciate ligament tears, or multi-ligamentous injuries along with meniscal tears in the age group of 10–60 years. The exclusion criteria were meniscal root tears, degenerative meniscal tears, revision meniscal procedures, and Kellgren–Lawrence grade 4 osteoarthritic knees. The cut-off for meniscectomy and meniscal repair was the same for MPS and OPS [21]:
Maximum score: 14
Minimum score: 1
Scores ≤ 6 (six or less): Meniscus repair
Scores ≥ 7 (seven or more): Meniscectomy
Table 1.
Ortho one PROMT score (prediction of reparability of meniscal tears)
| Criteria | Characteristics | Score |
|---|---|---|
| Age | < 20 years | 0 |
| 20–30 years | 1 | |
| 30–40 years | 2 | |
| > 40 years | 3 | |
| Chronicity | < 1 year | 0 |
| > 1 year | 1 | |
| Kellgren–Lawrence Grade | 0,1 | 0 |
| 2,3,4 | 3 | |
| Zone of tear | Red–Red | 0 |
| Red–White | 1 | |
| White–White | 3 | |
| Pattern of tear | Longitudinal, horizontal | 1 |
| Radial, oblique, flap | 2 | |
| Complex | 3 | |
| displaced bucket handle | 4 |
Maximum score: 14 (meniscectomy)
Minimum score: 1 (meniscal repair)
≤ 6: Meniscus repair (six or less)
≥ 7: Meniscectomy (seven or more)
Table 2.
Modified PROMT score (Modifications have been made bold)
| Criteria | Characteristics | Score |
|---|---|---|
| Age | < 20 years | 0 |
| 20–40 years | 1 | |
| 40–50 years | 2 | |
| > 50 years | 3 | |
| Chronicity | < 2 year | 0 |
| > 2 year | 1 | |
| Kellgren–Lawrence grade | 0,1 | 0 |
| > 1 | 3 | |
| Zone of tear | Red–Red | 0 |
| Red–White | 1 | |
| White–White | 3 | |
| Pattern of tear | Longitudinal, horizontal | 1 |
| Radial, oblique, flap | 2 | |
| Displaced bucket handle | 3 | |
| Complex | 4 |
Maximum score: 14 (meniscectomy)
Minimum score: 1 (meniscal repair)
≤ 6: Meniscus repair (six or less)
≥ 7: Meniscectomy (seven or more)
Preoperatively, the clinical examination and the analysis of imaging studies were done independently by two fellowship-trained knee surgeons and their results were tabulated. The reporting of MRI by a musculoskeletal radiologist was considered. The decision to do a meniscectomy or meniscus repair intraoperatively was made using the standard meniscus repair indications [5] and under the operating surgeon's influence who was kept blinded to OPS and MPS. 3 fellowship-trained surgeons who were blinded from the scores performed the surgeries. The operated patients after surgery were followed for 1 year and the functional outcomes were evaluated using International Knee Documentation Committee Score (IKDC) and Lysholm Knee Score (LKS).
Statistical Analysis
All data were compiled into Microsoft Excel (Microsoft 365, Microsoft Corp., Redmond, WA, USA). A socio-demographic analysis of our cohort was done to analyze the distribution, normality, and homogeneity of the data. The sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value, negative predictive value, and accuracy of the scoring systems were calculated. A Receiver Operating Characteristic (ROC) curve was plotted to compare the scoring systems. For statistical analysis, meniscal repairs were considered positive results, and meniscal excisions were considered negative results. Inter-observer agreement between the two surgeons and the Kappa score was calculated. SPSS 26 (IBM) was used to calculate the statistical results.
Results
A total of 133 meniscal tears presented to the hospital during the given period. However, only 100 patients met the inclusion criteria. Of these, 86 were males and 14 were females with 49 medial meniscus and 51 lateral meniscus injuries. The mean age of the patients was 37.6 ± 7.8 years. 44 were left knee injuries and 56 were right knee injuries. The mechanism of injury in 59 tears was road traffic accidents, 32 were due to sports injuries and 9 were due to domestic injuries. 26 patients had isolated meniscal tears, 72 had associated ACL insufficiency and 2 had PCL insufficiency. 17 patients (65.4%) had isolated lateral meniscus tears of which meniscal repair was done in 9 cases (52.9%) and excision was done in 8 cases (47.1%). 9 patients (34.6%) had isolated medial meniscus tears of which 6 (66.7%) were repaired and 3 (33.4%) were excised. Of the 74 meniscal tears associated with ACL or PCL insufficiency, 34 patients (45.9%) had lateral meniscus tears and 40 (54.1%) had medial meniscus tears. Of these, 15 (44.1%) lateral meniscus repairs and 19 (55.9%) lateral meniscus excisions were done along with 24 (60.0%) medial meniscus repairs and 16 (40.0%) medial meniscus excisions. The patient characteristics are summarized in Table 3.
Table 3.
Patient characteristics
| Patient Characteristics | Values |
|---|---|
| Age (mean ± SD) | 37.6 ± 7.8 years |
| Gender | |
| Male | 86 |
| Female | 14 |
| Site of injury | |
| Medial meniscus | 49 |
| Lateral meniscus | 51 |
| Side of injury | |
| Left knee | 44 |
| Right knee | 56 |
| Mechanism of injury | |
| RTA | 59 |
| Sports injuries | 32 |
| Domestic injuries | 9 |
| Associated injuries | |
| None | 26 |
| ACL | 72 |
| PCL | 2 |
The predictions of OPS and MPS are tabulated, and good inter-observer agreement was noted (κ = 0.7). (Tables 4 and 5).
Table 4.
Predictions of ortho one PROMT score vs actual procedure executed
| PROMT | Total predictions | Repairs done | Excisions done | P value |
|---|---|---|---|---|
| Lateral meniscus | ||||
| Procedure predicted | ||||
| Repair | 18 | 11 | 7 | P = 0.002 |
| 61.1% | 38.9% | |||
| Excision | 33 | 6 | 27 | |
| 18.2% | 81.8% | |||
| Total | 51 | 17 | 34 | |
| 100.0% | 33.3% | 66.7% | ||
| Medial meniscus | ||||
| Procedure predicted | ||||
| Repair | 31 | 28 | 3 | P < 0.001 |
| 90.3% | 9.7% | |||
| Excision | 18 | 3 | 15 | |
| 16.7% | 83.3% | |||
| Total | 49 | 31 | 18 | |
| 100.0% | 63.3% | 36.7% | ||
Table 5.
Predictions of modified PROMT score vs actual procedure executed
| MODIFIED PROMT | Total predictions | Repairs done | Excisions done | P value | ||
|---|---|---|---|---|---|---|
| Lateral meniscus | Procedure predicted | Repair | 18 | 14 | 4 | P = 0.002 |
| 77.8% | 22.2% | |||||
| Excision | 33 | 3 | 30 | |||
| 9.1% | 90.9% | |||||
| Total | 51 | 17 | 34 | |||
| 100.0% | 33.3% | 66.7% | ||||
| Medial Meniscus | Procedure predicted | Repair | 32 | 30 | 2 | P < 0.001 |
| 93.8% | 6.3% | |||||
| Excision | 17 | 1 | 16 | |||
| 5.9% | 94.1% | |||||
| Total | 49 | 31 | 18 | |||
| 100.0% | 63.3% | 36.7% | ||||
OPS demonstrated 90.32% (95% CI 74.25–97.96%) sensitivity and 83.33% (CI 58.58–96.42%) specificity in predicting medial meniscus tear reparability. Lateral meniscal repairs were predicted with a sensitivity and specificity of 64.71% (CI 38.33–85.79%) and 79.41% (62.10–91.30%) respectively. With improved sensitivity and specificity of 96.77% (CI 83.30–99.92%) and 88.89% (CI 65.29–98.62%), MPS predicted medial meniscus reparability with better accuracy. The newer score also showed better sensitivity and specificity in predicting lateral meniscus repairs at 82.35% (CI 56.57–96.20%) and 88.24% (CI 72.55–96.70%). The OPS’s positive likelihood ratio for medial meniscus and lateral meniscus was 5.42 (CI 1.92–15.32) and 3.14 (CI 1.49–6.64) respectively. The negative likelihood ratio for medial and lateral meniscus was 0.12 (CI 0.04–0.35) and 0.44 (CI 0.23–0.87). MPS’ positive likelihood ratio for medial meniscus and lateral meniscus was 8.71 (CI 2.35–32.22) and 7.00 (CI 2.72–18.04). Its negative likelihood ratio for medial and lateral meniscus was 0.04 (CI 0.01–0.25) and 0.20 (CI 0.07–0.56). The MPS showed a better accuracy rate (93.88% for medial meniscus, 86.27% for lateral meniscus) than OPS (87.76% for medial meniscus, 74.51% for lateral meniscus). Both the scores showed good statistical significance (p < 0.05) in predicting meniscal reparability (Tables 6 and 7).
Table 6.
Results of prospective prediction of outcome of meniscus surgery using ortho one PROMT score
| Ortho One PROMT SCORE | Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio | Positive predictive value | Negative predictive value | Accuracy | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| Lateral meniscus | 64.71% | 38.33% to 85.79% | 79.41% | 62.10% to 91.30% | 3.14 | 1.49 to 6.64 | 0.44 | 0.23 to 0.87 | 61.11% | 42.66% to 76.85% | 81.82% | 69.81% to 89.75% | 74.51% | 60.37% to 85.67% |
| Medial meniscus | 90.32% | 74.25% to 97.96% | 83.33% | 58.58% to 96.42% | 5.42 | 1.92 to 15.32 | 0.12 | 0.04 to 0.35 | 90.32% | 76.75% to 96.35% | 83.33% | 62.58% to 93.73% | 87.76% | 75.23% to 95.37% |
Table 7.
Results of prospective prediction of outcome of meniscus surgery using modified PROMT score
| MODIFIED PROMT | Sensitivity | Specificity | Positive likelihood ratio | Negative likelihood ratio | Positive predictive value | Negative predictive value | Accuracy | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| Lateral meniscus | 82.35% | 56.57% to 96.20% | 88.24% | 72.55% to 96.70% | 7.00 | 2.72 to 18.04 | 0.20 | 0.07 to 0.56 | 77.78% | 57.60% to 90.02% | 90.91% | 78.05% to 96.57% | 86.27% | 73.74% to 94.30% |
| Medial meniscus | 96.77% | 83.30% to 99.92% | 88.89% | 65.29% to 98.62% | 8.71 | 2.35 to 32.22 | 0.04 | 0.01 to 0.25 | 93.75% | 80.22% to 98.23% | 94.12% | 69.80% to 99.11% | 93.88% | 83.13% to 98.72% |
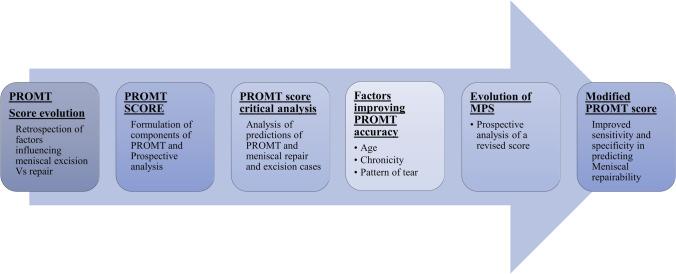
The ROC curve plotted for medial meniscus repairability showed the area under the curve was 0.868 for OPS and 0.928 for MPS (Fig. 1). For the lateral meniscus predictions, the area under the curve was 0.721 for OPS and 0.853 for MPS (Fig. 2)—demonstrating the superiority of the MPS over OPS in predicting meniscal reparability (Table 8). The outline of the development of PROMT and Modified PROMT score is shown in Fig. 3.
Fig. 1.
ROC curve plotted for medial meniscus repair predictions given by OPS and MPS (MM- lateral meniscus, PROMPT-OPS, M.PROMT-MPS)
Fig. 2.
ROC curve plotted for lateral meniscus repair predictions given by OPS and MPS (LM- lateral meniscus, PROMPT-OPS, M.PROMT-MPS)
Table 8.
Area under the curve table obtained using ROC curve comparing ortho one promt and modified promt scores
| Area Under the Curve | |||||
|---|---|---|---|---|---|
| GROUP | Test Result Variable(s) | Area | P value | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||||
| LM | OPS | 0.721 | 0.011 | 0.564 | 0.877 |
| MPS | 0.853 | < 0.001 | 0.730 | 0.976 | |
| MM | OPS | 0.868 | < 0.001 | 0.750 | 0.986 |
| MPS | 0.928 | < 0.001 | 0.835 | 1.000 | |
Fig. 3.
Development of PROMT and Modified PROMT score
Regarding the functional outcomes of the operated patients, the mean IKDC score and LKS pre-operatively were 32.5 (SD–9.6) and 48.1 (SD–8.3) respectively. This improved significantly postoperatively (P < 0.001). The mean scores were 84.6 (SD–12.5) and 91.8 (SD–7.2) respectively post-operatively.
Discussion
The most important finding in our study is the improved sensitivity and specificity of the MPS in predicting meniscal repairability. The menisci being vital biological entities play an important role in load distribution, lubrication, joint congruence, and nutrition [10, 11]. With mounting evidence, preservation of the meniscus should be the ideal treatment choice for traumatic meniscal tears. The repairability of meniscal tears depends on various factors like the age of the patient, chronicity of the tear, pattern, and location of the tear. There is a considerable difference in surgery cost, the need for equipment and implants, rehabilitation, work time loss, and long-term outcomes in terms of return to pre-injury activity level and development of osteoarthritis. Hence, it is of utmost importance to counsel patients preoperatively about the type of surgery and prognosis. The surgeon should also have a clear plan preoperatively to have the appropriate equipment and implants ready especially in low-resource settings.
Previous attempts at devising a method to predict meniscal surgery (meniscectomy or meniscal repair) were unsuccessful [7, 12–14]. Misir et al. reported that MRI alone has only moderate value in predicting meniscal repairability and emphasized the role of multiple factors in predicting meniscal repair [15]. OPS provided a simple reproducible method to predict meniscal repairability. This scoring system unlike the previously attempted scores took into consideration clinical features, plain X-ray findings along with MRI features. However, it had low sensitivity and specificity in predicting lateral meniscal tears. MPS has improved specificity and sensitivity in predicting both lateral and medial meniscal tears when compared to OPS. It is important to note that the OPS and MPS are preoperative scores that help the surgeon decide whether to repair or excise the meniscus. They help the surgeon prepare for meniscal repair with the necessary armamentarium and expertise in case repair is required according to these scores. These scores do not affect the intraoperative decision of the surgeon on whether to repair or excise the meniscus. Hence, these scores are not associated with functional outcomes such as successful repair or failure.
We have revised the criteria for age, tear pattern, and chronicity of meniscal injury. The revisions are supported by recent scientific developments. Eggli et al. in their study reported unfavorable outcomes in elderly patients undergoing meniscal repair [16]. With increasing age, a degenerative component of the involved meniscus along with wear and tear of the involved joint increases considerably making repairs difficult. However, studies by Rothermel et al. and Everhart et al. showed that there is no difference in failure rates of meniscal repair performed between patients aged above or below 40 years [17, 18]. Barrett et al. found the results of arthroscopic meniscal repairs done for traumatic tears in elderly patients were comparable to those performed in the younger age group [19]. This made them go ahead and conclude that the location of the tear is a more important predictive factor for successful repair than the age of the patient. Also, histological studies suggest a decrease in vascularity with advancing age. After 50 years of age, only the lateral quarter of the meniscal base is vascularized [20, 21].
The PROMT scoring system had a higher score for complex tear patterns when compared to bucket handle tears. Bucket handle tears are reported to account for 10% of all meniscal tears [22]. Partial meniscectomy has been the go-to method of treatment historically. Shelbourne and Carr in their review of 155 patients with isolated bucket handle tears or associated anterior cruciate ligament tears concluded that there was no difference in outcomes between the repair and partial meniscectomy group [23]. However, Bucket handle tears are increasingly identified to be repairable fully even in chronic cases. Alejandro et al. [24] reported outcomes in 24 repairs of chronic bucket handle tears as old as 60 months. Of these, only 4 cases needed revision. Quite a good number of technical notes explaining the reduction and repair of bucket-handle tears have been published in recent years [25–28]. Moatshe et al. reported comparable outcomes between repaired bucket handle and vertical tears at 2 years of follow-ups [29].
Previously, meniscal repair was favored only for acute tears. Multiple studies [16, 30] had reported better outcomes for repairs done in acute tears when compared to chronic tears. With increased emphasis on meniscal preservation, the development of good repair devices and repair techniques, and the efforts to successfully repair chronic meniscal tears have now become practical and feasible. A study on repair in chronic meniscal tears ranging from 6 to 80 months showed good functional outcomes at an average of 20-month follow-up [31].
The availability of a good preoperative prediction tool is a luxury that assuages the complex process of planning a meniscal repair. MRI reporting particularly in musculoskeletal radiology is subjective and interpretation varies with the experience of the surgeon. Even with experience and expertise, MRI shows only moderate value in identifying meniscal repairability [15]. The uniqueness of MPS is the distribution of appropriate weightage for the prediction of repairability among all the important factors that contribute to repair. This score like its predecessor is easy to understand and reproduce making it an effective clinical tool.
The main limitation of this study is that it is a single-center study. The sample size is limited and is more like a cross-sectional study. Assessment of healing of meniscus using MRI at 1-year follow-up is needed to see the success of repairs predicted by the score. Another important point to emphasize is that, though the change from the original PROMT score to MPS is based on factors that favored meniscal repairs and subsequently improved the functional outcomes in literature as well as in our experience, MPS is designed to only guide the surgeons decide pre-operatively on whether to repair or excise the meniscus. The score, if at all, would only have a very little effect on the intra-operative decision-making of the surgeon and thus would not influence the functional outcomes of meniscus surgery. The aim of the score is only to improve the preoperative preparedness of surgeons for meniscus surgery.
Conclusion
The prediction of meniscus reparability has been a diagnostic conundrum. The MPS with increased sensitivity and specificity will serve as a simple and effective tool for surgeons to predict meniscal repairability, thus enhancing their pre-surgical preparedness. This tool will also help surgeons to realistically counsel their patients and achieve optimal patient satisfaction.
Authors' contributions
SS, PP—conceptualization, data curation, formal analysis, investigations, methodology, administration, resources, supervision, validation, visualization, writing original drafts and reviewing drafts. GC, PC—conceptualization, data curation, formal analysis, investigations, methodology, supervision, validation, visualization, writing original drafts and reviewing drafts. VK, SS, DVR—conceptualization, data curation, formal analysis, investigations, methodology, administration, resources, supervision, validation, and visualization.
Funding
No external funding was received for study.
Availability of data and material
Available upon request.
Compliance with Ethical Standards
Ethics approval
Obtained from institutional ethics committee.
Consent for participation
Obtained.
Consent for publication
Obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shyam Sundar, Email: drshyam.msortho@gmail.com.
Prashanth Pandian, Email: drprashanth.sayee@gmail.com.
Girinivasan Chellamuthu, Email: giri.c.nivasan@gmail.com.
Prashanth Chalasani, Email: prashanth.chalasani@gmail.com.
Vinay Kumaraswamy, Email: maildrvinay@gmail.com.
Santosh Sahanand, Email: sahanand@gmail.com.
David V. Rajan, Email: davidvrajan@gmail.com
References
- 1.Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: Structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011;32:7411–7431. doi: 10.1016/j.biomaterials.2011.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopf S, Beaufils P, Hirschmann MT, Rotigliano N, Ollivier M, Pereira H, et al. Management of traumatic meniscus tears: The 2019 ESSKA meniscus consensus. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28:1177–1194. doi: 10.1007/s00167-020-05847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: A systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27:1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 4.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. American Journal of Sports Medicine. 2010;38:1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 5.Rogers M, Dart S, Odum S, Fleischli J. A cost-effectiveness analysis of isolated meniscal repair versus partial meniscectomy for red-red zone, vertical meniscal tears in the young adult. Arthroscopy. 2019;35:3280–3286. doi: 10.1016/j.arthro.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 6.Svantesson E, Cristiani R, HamrinSenorski E, Forssblad M, Samuelsson K, Stålman A. Meniscal repair results in inferior short-term outcomes compared with meniscal resection: A cohort study of 6398 patients with primary anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26:2251–2258. doi: 10.1007/s00167-017-4793-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matava MJ, Eck K, Totty W, Wright RW, Shively RA. Magnetic resonance imaging as a tool to predict meniscal reparability. American Journal of Sports Medicine. 1999;27:436–443. doi: 10.1177/03635465990270040601. [DOI] [PubMed] [Google Scholar]
- 8.Van Dyck P, Vanhoenacker FM, Lambrecht V, Wouters K, Gielen JL, Dossche L, et al. Prospective comparison of 1.5 and 3.0-T MRI for evaluating the knee menisci and ACL. Journal of Bone and Joint Surgery. 2013;95:916–924. doi: 10.2106/JBJS.L.01195. [DOI] [PubMed] [Google Scholar]
- 9.Kumaraswamy V, Ramaswamy AG, Sundar S, Rajan DV, Selvaraj K, Sahanand S, et al. A new scoring system for prediction of meniscal repair in traumatic meniscal tears. Knee Surgery, Sports Traumatology, Arthroscopy. 2019;27:3454–3460. doi: 10.1007/s00167-019-05377-7. [DOI] [PubMed] [Google Scholar]
- 10.Cristiani R, Rönnblad E, Engström B, Forssblad M, Stålman A. Medial meniscus resection increases and medial meniscus repair preserves anterior knee laxity: a cohort study of 4497 patients with primary anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2018;46:357–362. doi: 10.1177/0363546517737054. [DOI] [PubMed] [Google Scholar]
- 11.Becker R, Awiszus F. Physiological alterations of maximal voluntary quadriceps activation by changes of knee joint angle. Muscle and Nerve. 2001;24:667–672. doi: 10.1002/mus.1053. [DOI] [PubMed] [Google Scholar]
- 12.Bernthal NM, Seeger LL, Motamedi K, Stavrakis AI, Kremen TJ, McAllister DR, et al. Can the reparability of meniscal tears be predicted with magnetic resonance imaging? American Journal of Sports Medicine. 2011;39:506–510. doi: 10.1177/0363546510387507. [DOI] [PubMed] [Google Scholar]
- 13.Pujol N, Tardy N, Boisrenoult P, Beaufils P. Magnetic Resonance Imaging is not suitable for interpretation of meniscal status ten years after arthroscopic repair. International Orthopaedics. 2013;37:2371–2376. doi: 10.1007/s00264-013-2039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orlando Júnior N, de Souza Leão MG, de Oliveira NHC. Diagnosis of knee injuries: Comparison of the physical examination and magnetic resonance imaging with the findings from arthroscopy. Rev Bras Ortop. 2015;50:712–719. doi: 10.1016/j.rboe.2015.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Misir A, Kizkapan TB, Yildiz KI, Arikan Y, Ozcafer R, Cetinkaya E. Using only MRI is moderately reliable in the prediction of meniscal tear reparability. Knee Surgery, Sports Traumatology, Arthroscopy. 2019;27:898–904. doi: 10.1007/s00167-018-5187-9. [DOI] [PubMed] [Google Scholar]
- 16.Eggli S, Wegmüller H, Kosina J, Huckell C, Jakob RP. Long-term results of arthroscopic meniscal repair. An analysis of isolated tears. American Journal of Sports Medicine. 1995;23:715–720. doi: 10.1177/036354659502300614. [DOI] [PubMed] [Google Scholar]
- 17.Rothermel SD, Smuin D, Dhawan A. Are outcomes after meniscal repair age dependent? A Systematic Review. Arthroscopy. 2018;34:979–987. doi: 10.1016/j.arthro.2017.08.287. [DOI] [PubMed] [Google Scholar]
- 18.Everhart JS, Higgins JD, Poland SG, Abouljoud MM, Flanigan DC. Meniscal repair in patients age 40 years and older: A systematic review of 11 studies and 148 patients. The Knee. 2018;25:1142–1150. doi: 10.1016/j.knee.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy. 1998;14:824–829. doi: 10.1016/s0749-8063(98)70018-0. [DOI] [PubMed] [Google Scholar]
- 20.Michel PA, Domnick CJ, Raschke MJ, Hoffmann A, Kittl C, Herbst E, et al. Age-related changes in the microvascular density of the human meniscus. American Journal of Sports Medicine. 2021;49:3544–3550. doi: 10.1177/03635465211039865. [DOI] [PubMed] [Google Scholar]
- 21.Petersen W, Tillmann B. Age-related blood and lymph supply of the knee menisci. A cadaver study. Acta Orthopaedica Scandinavica. 1995;66:308–312. doi: 10.3109/17453679508995550. [DOI] [PubMed] [Google Scholar]
- 22.Metcalf MH, Barrett GR. Prospective evaluation of 1485 meniscal tear patterns in patients with stable knees. American Journal of Sports Medicine. 2004;32:675–680. doi: 10.1177/0095399703258743. [DOI] [PubMed] [Google Scholar]
- 23.Shelbourne KD, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. American Journal of Sports Medicine. 2003;31:718–723. doi: 10.1177/03635465030310051401. [DOI] [PubMed] [Google Scholar]
- 24.Espejo-Reina A, Serrano-Fernández JM, Martín-Castilla B, Estades-Rubio FJ, Briggs KK, Espejo-Baena A. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy. 2014;30:492–496. doi: 10.1016/j.arthro.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 25.Cetinkaya E, Gursu S, Gul M, Aykut US, Ozcafer R. Surgical repair of neglected bucket-handle meniscal tears displaced into the intercondylar notch: Clinical and radiological results. The Journal of Knee Surgery. 2018;31:514–519. doi: 10.1055/s-0037-1604146. [DOI] [PubMed] [Google Scholar]
- 26.Beatrice Tan J-N, James Loh S-Y. An approach to chronic and displaced bucket handle meniscal tear—assessment, repair (push-and-pull technique), or salvage. Arthroscopy Techniques. 2021;10:e1853–e1857. doi: 10.1016/j.eats.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yik JH, Koh BTH, Wang W. A novel technique for modified all-inside repair of bucket-handle meniscus tears using standard arthroscopic portals. Journal of Orthopaedic Surgery and Research. 2017;12:188. doi: 10.1186/s13018-017-0692-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yuen WLP, Kuo CL, Goh KMJ, Lee YHD. Technique for all-inside repair of bucket-handle meniscus tears. Arthroscopy Techniques. 2021;10:e743–e750. doi: 10.1016/j.eats.2020.10.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moatshe G, Cinque ME, Godin JA, Vap AR, Chahla J, LaPrade RF. Comparable outcomes after bucket-handle meniscal repair and vertical meniscal repair can be achieved at a minimum 2 years’ follow-up. American Journal of Sports Medicine. 2017;45:3104–3110. doi: 10.1177/0363546517719244. [DOI] [PubMed] [Google Scholar]
- 30.Tengrootenhuysen M, Meermans G, Pittoors K, van Riet R, Victor J. Long-term outcome after meniscal repair. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19:236–241. doi: 10.1007/s00167-010-1286-y. [DOI] [PubMed] [Google Scholar]
- 31.Popescu D, Sastre S, Caballero M, Lee JWK, Claret I, Nuñez M, et al. Meniscal repair using the FasT-Fix device in patients with chronic meniscal lesions. Knee Surgery, Sports Traumatology, Arthroscopy. 2010;18:546–550. doi: 10.1007/s00167-009-0926-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Available upon request.