Abstract
Background
Neck pain (NP) is common in all age groups and adversely affects the patients’ entire lifestyle. There exists inconclusive evidence relating faulty craniocervical posture with pain-related disability. This review aims to determine whether sagittal head and neck posture differs in NP and pain-free subjects, to critically appraise the correlation of posture with NP.
Methods
Of 3796 articles identified at primary search from CINAHL, PubMed, Google Scholar, EMBASE, 26 were included based on eligibility criteria. Mean pooled difference (MPD) and effect size (ES) were calculated to establish relationship among studies, to assess postural correlation with NP measures [Visual Analogue Scale (VAS), Numeric Pain Rating Scale (NPRS), neck disability index (NDI), Northwick Park NP Questionnaire (NPQ)] and for age- and gender-wise variation. Risk of bias was assessed using Newcastle–Ottawa Quality Assessment Scale.
Results
Craniovertebral angle (CVA) had a significant MPD of − 2.93(95% CI − 4.95 to − 0.91). Sagittal head angle (SHA) and forward head posture (FHP) had an insignificant MPD of 1.15 (95% CI − 1.16 to 3.46) and − 0.26 (95% CI − 1.89 to 1.36), respectively. Age- and gender-wise CVA difference was found to be 2.36° and 2.57°, respectively. ES was significant for correlation between CVA and pain intensity [NPRS: − 0.44 (95% CI − 0.61 to − 0.26); VAS: − 0.31 (95% CI − 0.46 to − 0.16)], and between CVA and disability [NDI: − 0.18 (95% CI − 0.31 to − 0.05); NPQ: − 0.47 (95% CI − 0.61 to − 0.320)].
Conclusion
CVA differs for age, gender, and pain vs pain-free subjects, and correlates negatively with NP measures. Other surrogate measures (SHA, cranial and cervical angles, FHP) warrant further research.
PROSPERO Registration
PROSPERO 2021 CRD42021275485.
Keywords: Neck pain, Posture, Head and neck posture, Craniocervical posture
Introduction
Neck pain (NP) is a common complaint among individuals of all age groups, negatively impacting their work productivity, health and economical status. It accounts for fourth leading cause of long-term disability worldwide [1]. NP prevalence varies worldwide, more in females [2], and Western countries reflecting the highest number of persons with chronic NP. The global point prevalence of NP was estimated to be 4.9% in the Global burden of disease 2010 [3]. Chronic pain patients tend to have altered craniocervical posture, relative to the matched controls [4–6]. Forward Head Posture (FHP) is the most common faulty posture associated with NP-related dysfunctions overtime [5, 7–9], where the tragus of ear is displaced anterior to the ideal reference line [10–12]. The neck extensors are in the shortened position, and thus develop adaptive shortening over time [13].
The faulty craniocervical posture often leads to altered motor control, increased load on vertebrae and surrounding muscles involved in upper quadrant stability (e.g., trapezius and pectorals), thus predisposing to early onset of degenerative changes; and decreased strength and endurance along with muscle imbalance and stiffness. The latter may in turn provoke pain due to ischemia and accumulation of waste metabolites [14].
Usually, in clinical practice, any faulty posture is subjectively rated as mild/moderate/severe [15], but this kind of grading is most certainly subject to the clinician’s visual estimate and level of expertise and is thus a potential source of error. Assessing various cervical postural measures (e.g., craniovertebral angle (CVA) [16] and sagittal head angle [5, 17]) using instruments ranging from simple to cumbersome, e.g., CROM (cervical ROM) device [18], plumb lines, photographic analysis [19], Rocabado Posture Gauge [20], vernier caliper, and radiographic imaging, are documented.
Evidence for the relationship between faulty posture and NP measures is quite equivocal, spanning from moderate–good correlation [5, 6, 21] to nil/weak correlation [22–25]. There is variable evidence linking the incidence of NP, faulty posture with age [26], probably because the sample population varies a great deal, ranging from adolescents to the elderly, among the existing studies. With the increased usage of smartphones and laptops for teenagers and young adults, frequency of NP is increasing in young age group too [27], with its consequent effects on neck and shoulder posture [28]. The advancing age has been shown to be a predisposing factor for FHP in asymptomatic persons [29]. Strong evidence has been reported linking the prevalence of NP to the female gender [30].
Silva et al. [31] have concluded insufficient evidence to compare FHP and neck ROM. Its sequential review [26] claimed the positive linkage of FHP with symptomatic adults and elderly, but none in adolescents [26, 32]. Although individual studies and reviews exist, there is no panoramic review analyzing the different craniocervical postural measures in relation to NP altogether. Therefore, among all the existing controversial conclusions from various studies and reviews, it is necessary to add to the current literature, a comprehensive review analyzing the association of NP to craniocervical posture, by assessing the methodological quality, age and gender-wise variations, and all postural outcomes of the included researches, and thus determine whether or not there exists an association between NP and sagittal head and neck posture.
Methodology
This systematic review and meta-analysis was registered on PROSPERO (PROSPERO 2021 CRD42021275485) and conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The methodological quality assessment of included studies was done through Newcastle—Ottawa Quality Assessment Scale.
Data Sources and Search Strategy
The studies were searched from the electronic databases EBSCO (via CINAHL), Medline (via Pubmed), Google Scholar, EMBASE published till April 2022, and also from hand-searching the reference lists of the available articles. The search was performed using the search keywords (including MeSH) as ‘cervical pain’, ‘chronic neck pain’, ‘faulty posture’, ‘neck pain’, and ‘forward head posture’ (Table 1). Out of 3796 studies identified at the primary search, finally 26 studies were found relevant for the review as per the eligibility criteria. The longitudinal and cross-sectional studies which studied neck pain (using standard scales to measure intensity and disability) with either or all of the postural measures for head and neck, with or without a control group for comparison. The studies assessing static/neutral/habitual head and neck posture on subjects ≥ 10 years of age were included. The included studies should have their full text available in or translatable to English. The studies were excluded if they were not done on humans or if the full text article could not be retrieved or if different aspects of same study was published in more than one article. Studies with traumatic NP subjects, any kind of intervention studies, conference proceedings, editorials, and studies assessing dynamic/work-related posture or posture involving any kind of external weight on spine were not considered to be part of this review.
Table 1.
Search strategy and number of articles found in each database
| Database | No. of articles | Search terms |
|---|---|---|
| PubMed | 1293 | “((((((((cervical pain)) OR (Neck Pain[Text Word])) OR (“Neck Pain”[Mesh])) OR (cervical pain[Text Word])) OR (Neckache)) OR (Neckaches)) OR (Neck Aches)) AND (((“Posture”[Mesh]) OR (neck posture[Text Word])) OR (forward head posture[Text Word]))” |
| EMBASE | 1889 | “((‘cervical pain’/exp OR ‘cervical pain’) OR (‘neck pain’/exp OR ‘neck pain’) OR (‘neck pain’/exp) OR (neckache)) AND ((‘posture’/exp OR posture) OR (‘neck posture’/exp OR ‘neck posture’) OR (‘forward head posture’/exp OR ‘forward head posture’))” |
| CINAHL | 579 | ((TX + cervical + pain) + OR + (MH + neck + pain) + OR + (TX + neckache)) + AND + ((MH + posture) + OR + (TX + neck + posture) + OR + (TX + forward + head + posture) |
Study Selection
After screening the titles and/or abstracts in the primary search, all the retrieved articles were imported into the software EndNote X8.2 (Clarivate Analytics) and checked for the duplicates by one of the authors (PP). All full text articles were then independently assessed by two reviewers (BR, AP) for relevance, based on inclusion and exclusion criteria. Secondary/hand-searching was done from the reference list of available articles. A comparison was drawn out of the relevant studies’ lists of the two reviewers. Any difference in opinion was resolved by consensus or by third reviewer (AC).
Data Extraction
Relevant data from all the studies were included, in the form of study design, sampling methods, blinding; demographic data; inclusion criteria for the pain group and control group; Outcome measures; Statistics; Results and conclusion. Corresponding authors of included studies were contacted via email, wherever additional data were required.
Quality Assessment
Quality assessment for all the included studies was done through Newcastle–Ottawa Quality Assessment Scale (adapted for cross-sectional studies) [33] independently by two reviewers (BR, AP). Any disagreement was resolved through a mutual consensus. The scale allows for a total score of 10, and comprises of three sub-sections: Selection (maximum five stars), Comparability (maximum two stars) and Outcome (maximum three stars). All studies included in the review were assessed for quality, regardless of their inclusion in the meta-analysis.
To avoid discrepancy in the terminology for the postural measures assessed by different authors, the following common terms have been used for denoting:
SHA (sagittal head angle): canthus–tragus–horizontal.
Cranial Angle: canthus–tragus–vertical.
CVA (craniovertebral angle): tragus–C7–horizontal.
SA (shoulder angle): C7–Acromion–horizontal.
HTA (high thoracic angle): C7–T7–Horizontal.
Cervical angle: tragus–C7–Vertical.
UTA (upper thoracic angle): C7–T5–Vertical.
Acromion protrusion—ear tragus perpendicular to horizontal plane.
RSP (rounded shoulder posture): acromion–table distance (supine).
PS (protracted shoulder): acromion–wall distance (sitting): forward shoulder posture.
Statistical Analysis
Data from the included studies were analyzed for comparative analysis using STATA 16 (STATA CORP LLC, 4905 Lakeway Drive College Station, Texas 77845-4512 USA). Meta-analysis was conducted for all comparative outcomes. Random effect model was used to calculate the pooled mean difference (MD) within 95% confidence interval (CI) for continuous data. I2 test assessed the statistical heterogeneity between studies, whereas heterogeneity across the studies was analyzed using Cochran’s Q test and then transformed into I2 percent with its p value. Subgroup analyses were performed with the studies for the age and gender in the CVA group. Age was categorized into young (10–50 years) and elderly (50 years). Correlation between the categories was performed by Fisher z transformation of Pearson correlation coefficient (r) from each study. Standard error and 95% CI were calculated for each r value before the calculation of weighted mean (weight depended on the sample size). z and χ2 values were then calculated to determine the p value of the overall effect across the studies. All z-transformed r values and their CI were reversed again for representation. Publication bias was tested for the CVA outcome.
Results
Study Selection and Characteristics
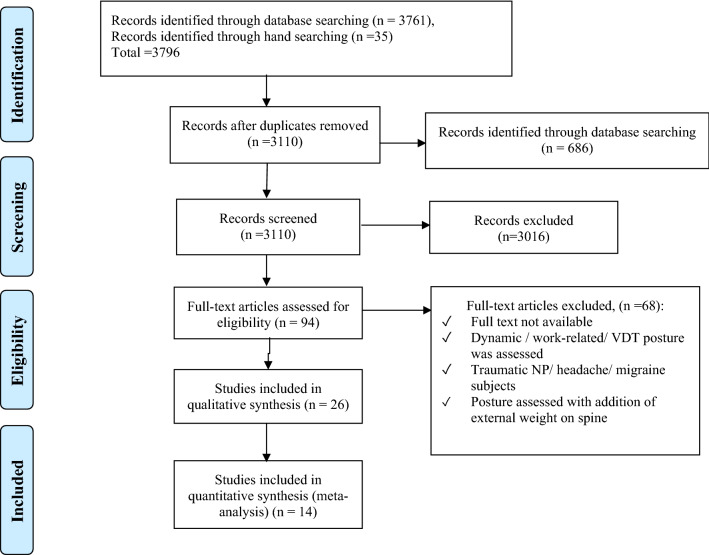
The analysis included a total of 26 studies—4 prospective cross-sectional studies without comparison, one retrospective study without comparison, 18 prospective studies which were cross-sectional and compared the neck pain/FHP subjects to the non-pain/non-FHP subjects, 2 cross-sectional cohort studies, and 1 within-subjects reliability study. Out of these, 12 studies additionally investigated the correlation of neck pain intensity and/or disability with either of the primary outcome measures for head and neck posture. PRISMA flowchart is described in Fig. 1.
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart
Demographic data and results of individual studies are described in Tables 2 and 3, respectively.
Table 2.
Demographic data
| Study ID | Setting | Study design | Population | NP group | Control group | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Age | F, M | Pain duration | N | Age | F, M | ||||
| Yip 2008 [21] | Hospital | Cross-sectional | Patients | 62 | 39.92 ± 10.80 | 40 F, 22 M | – | 52 | 42.33 ± 11.18 | 36 F, 16 M |
| Silva 2009 [6] | Hospital and general community | Cross-sectional | Patients; gen pop | 40 | 50.2 ± 7.9; (33–69) | 34 F, 6 M | > 6 months | 40 | 50.2 ± 7.9; (34–68) | 34 F, 6 M |
| Lau 2010 [38] | Hospital | – | Patients | 30 | 46.7 ± 9.5; (27–59) | 16 F, 14 M | > 3 months | – | – | – |
| Lau 2010 [39] | Hospital, clinics | Cross-sectional | Patients | 30 | 36.77 ± 9.83; (20–50) | 20 F, 10 M | – | 30 | 34.50 ± 9.95; (20–50) | 13 F, 17 M |
| Helgadottir 2011 [47] | PT clinics | – | Patients | 21 |
35.23 ± 8.41 (25–54) |
19 F, 2 M | > 6 months | 20 | 29.70 ± 7.75 (21–51) | 17 F, 3 M |
| Quek 2012 [42] | Hospital | Cross-sectional | Elderly patients | 51 |
66 ± 4.9; (60–78) |
29 F, 22 M | – | – | – | – |
| Juliana 2012 [45] | – | – | Female subjects | 11 | 31.55 ± 11.11; (20–50) | 11 F | > 3 months | 11 | 25.27 ± 2.61; (20–50) | 11 F |
| Dolphens 2012 [34] | School | Cross-sectional | Adolescent students | 1196 | 10.6 ± 0.47 | 557 F | – | – | – | – |
| 12.6 ± 0.54 | 639 M | |||||||||
| Ruivo 2014 [5] | School | Cross-sectional | 275 Adolescent students (153 F, 122 M) | 105 | 15–17 | – | – | 170 | 15–17 | – |
| Nagai 2014 [23] | Combat aviation brigade | – | Male active-duty helicopter pilots | 27 | 34.5 ± 6.4; (18–55) | 27 M | > 1 year | 27 | 34.3 ± 6.1; (18–55) | 27 M |
| Nejati 2014 [28] | University | Cross-sectional | Office workers | 55 | 39 ± 8 | 40 F, 15 M | > 3 months | 46 | – | – |
| Dunleavy 2015 [50] | – | Cross-sectional (Reliability) | – | 20 |
51.8 ± 8 (35–69) |
20 F | > 3 months | 20 |
51.7 ± 8 (35–69) |
20 F |
| Oliveira 2016 [24] | School | – | 10–12th grade students | 35 | 16.6 ± 0.7 | 25 F, 10 M | – | 35 | 16.7 ± 0.7 | 22 F, 13 M |
| Kim 2016 [17] | University | – | College students | Total 126 |
23.9 ± 1.5; (19–24) |
31 F, 95 M | – | – | – | – |
| Richards 2016 [48] | – | Cross-sectional (cohort) | Adolescents | 1108 | – | – | – | – | – | – |
| MohanKumar 2017 [4] | – | – | Young adults | 30 | 25.77 ± 2.063 (20–30) | – | > 2 months | 30 | 23.97 ± 1.974 (20–30) | – |
| Mani 2017 [40] | University teaching hospital | Cross-sectional, convenience sampling | Volunteers | 16 | 27.7 ± 16.4; (10–65 y) | – | > 6 months | 15 | 24.7 ± 6.3; 17–40 | – |
| Subbarayalu 2017 [46] | IT industry | Cross-sectional | IT professionals | Total 84 | 20–40 | 27 F, 57 M | > 3 months | – | – | – |
| DH Kim 2018 [36] | Hospital | – | Hospital employees; FHP subjects—CVA < 52 | 22 | 28.55 ± 5.15; (20–40) | 13 F, 9 M | – | 22 | 26.64 ± 4.54 | 14 F, 8 M |
| Kocur 2019 [37] | Office | – | Female office workers | 16 | 42.4 ± 9.6 (30–55) | 16 F | – | 16 | 40.4 ± 5.9 | 16 F |
| Leila Ghamkhar 2019 [22] | Outpatient clinic; university campus | Cross-sectional correlational | Patients; employees and students | 32 | 20–55 | 23 F, 9 M | > 3 months | 35 | – | 23 F, 12 M |
| Kanda 2021 [49] | – | – | Young female subjects | 21 | 20.6 ± 0.8 | 21 F | > 1 year | 18 | 20.6 ± 0.8 | 18 F |
| Elderly female subjects | 22 | 71.1 ± 4.5 | 22 F | > 1 year | 11 | 71.1 ± 4.5 | 11 F | |||
| Ertekin 2021 [35] | – | Retrospective | NSP students, RSP > 3 cm | 39 | 22.9 ± 3.8 | 39 F | – | – | – | – |
| Save 2021 [44] | College | Cross-sectional | College students | 18 | 18–25 | - | > 3 months | 18 | 18–25 | - |
| Sarig 2022 [43] | – | Cross-sectional | University staff and students | 22 | 38.1 ± 9.9 (18–65) | 14 F, 8 M | > 2 months | 20 | 33.6 ± 7.7 (18–65) | 10 F, 10 M |
| FHP Group (CVA < 50) | Control Group (CVA > 50) | |||||||||
| Patricia 2020 [41] | University | Cross-sectional | College students | 32 | 20.54 ± 2.96 | 21 F, 11 M | > 3 months | 64 | 19.48 ± 1.96 | 38 F, 26 M |
NP neck pain, N sample size, F female, M male, FHP forward head posture, CVA craniovertebral angle, NSP neck shoulder pain
Table 3.
Data from studies
| *Study design **Sampling method ***Blinding |
Sample characteristics | Inclusion criteria for NP and control group | Subjective outcome measures for neck pain | Head and neck posture measures | Other cervical measures assessed | Statistics | Results and conclusion | |
|---|---|---|---|---|---|---|---|---|
| Yip et al. 2008 [21] |
*Cross-sectional study with comparison **Convenience sampling ***Blind assessor |
NP Gp N = 62 (40 F, 22 M) Mean age = 39.92 ± 10.80 y Control Gp N = 52 (36 F, 16 M) Mean age = 42.33 ± 11.18 y |
NP Gp- diagnosed to have NP with or without referred pain, numbness or paraesthesia over the ULs Control Gp- No NP in past 3 years |
NP severity and disability (using NPQ and NPRS) | CVA (using HPSCI) | ICC, Independent Samples t test, Pearson Correlation |
Mean CVA in NP Gp: 49.93° ± 6.08°, control Gp: 55.02° ± 2.86° -CVA with NPQ (rp = − 0.3101, p = 0.015) -CVA with NPRS (rp = − 0.329; p = 0.009) - CVA with age (rp = − 0.380; p = 0.002) With age taken into account -CVA with NPQ (rp = − 0.3101; p = 0:015) -CVA with NPRS (rp = 0.1848; p = 0.154) CVA in NP Gp is significantly smaller than in control Gp -Moderate negative correlation between CVA and neck disability. Patients with small CVA have a greater FHP, and thus, greater disability |
|
| Silva et al. 2009 [6] |
*CS study with comparison ***Single blind (assessor) |
NP Gp N = 40 (34 F, 6 M) Age = 50.2 ± 7.9 (33–69) Control Gp N = 40 (34 F, 6 M) Age = 50.2 ± 7.9 (34–68) |
NP Gp NP > 6 m Control Gp No current NP and never had NP for > 3 consecutive days |
NP history during preceding week (avg NP intensity, frequency, duration, localization) |
CVA, Sagittal head angle, frontal plane head alignment (using video cameras) |
Unpaired t test, MANOVA |
- NP Gp—smaller CVA, resulting in a more FHP CVA in NP Gp: 45.4° ± 6.8°; Control Gp: 48.6° ± 7.1°; p < 0.05, CI 0.9°– 6.3° - Overall, CVA in young gp = 48.9 ± 6.9, elderly gp = 44.9 ± 6.8; p < 0.05 - CVA young NP Gp − 46.1° + 6.7° CVA young control gp -51.8° + 5.9°; p < 0.01, CI 1.8°–9.7° - No CVA difference for the older gp (NP vs control—p > 0.05) SHA for NP Gp- 21.0° ± 6.4°, Control Gp- 18.8° ± 7.7° Overall, SHA in young gp = 20.1 ± 6.9, elderly gp = 19.6 ± 7.4; p > 0.05 Younger patients with CNP were shown to have a more FHP in standing than matched Control gp |
|
| Lau et al. 2010 [38] |
N = 30 (16 F, 14 M) Mean age 46.7 ± 9.5 (27–59) |
Mechanical NP > 3 m | NPRS, NPQ |
CVA (using EHPI), AHT (using lateral cervical X-rays) |
ICC, Pearson product moment correlation coefficient, Pearson correlation |
Mean CVA: 40.8° ± 5.4° (F- 43.1° ± 5.5, M-38.1° ± 3.9) Mean AHT: 18.0 ± 12.6 mm (F- 13.3 ± 9.2, M-23.3 ± 14.2) -AHT on X-ray with CVA on EHPI (r = − 0.71, p < 0.001) -CVA with NPQ (r = − 0.67, p < 0.001) -CVA with NPRS (r = – 0.70, p < 0.001) -AHT with NPQ (r = 0.390, p = 0.033) - AHT with NPRS (r = 0.49, p = 0.006) -Negative correlation of CVA with NPQ and NPRS -Moderate positive correlation of AHT with NPQ and NPRS |
||
| Lau et al. 2010 [39] |
*CS study with comparison **Convenience sampling |
Age = 20–50 NP Gp N = 30 (20 F, 10 M) Mean age: 36.77 ± 9.83 (24–50) Control Gp N = 30 (13F, 17 M) Mean age: 34.50 ± 9.95; (20–50) |
NP Gp Minimum 3 on NPRS; > 10% on NPQ Control Gp No NP in past 6 m 0 on NPRS, < 10% on NPQ |
NP severity and disability (using NPRS, NPQ) |
High Thoracic Angle (HTA), CVA (Using Photographic measurement) |
Chi Square, ICC, Spearman Correlation, Multiple logistic and Linear Regression |
Mean CVA in NP Gp: 40.13° ± 6.68° (31.0°–52.0°); Control Gp: 48.40° + 5.52° - CVA with presence of NP (rs = -0.56, p < 0.01) HTA with presence of NP (rs = 0.63, p < 0.01), - CVA with HTA (rs = − 0.62, p < 0.01) in NP Gp - CVA with NP severity (rs = -0.36, p = 0.06) and disability (rs = -0.37, p = 0.05) HTA (OR = 1.37, p < 0.01) was a good predictor for presence of NP, even better than CVA (OR = 0.86, p = 0.04) |
|
| Helgadottir et al. 2011 [47] | **Convenience sampling |
Age 18–55 Gp1 IONP N = 21 (19 F, 2 M) Gp2 WAD N = 23 (20 F, 3 M) Gp3 Control Gp N = 20 (17 F, 3 M) |
NP Gp -a score of at least 10 on the NDI, and neck symptoms of > 6 m Control Gp: No cervical or shoulder dysfunction |
NDI, VAS (average neck pain intensity experienced over past 7 days) |
Cranial angle, Cervical angle (by a 3-space FasTrak device, Excel software program), Midthoracic curve |
Clavicle and Scapular movements | ANOVA, post hoc comparison |
- Significant difference in the cranial angle (p < .01) and a tendency in the cervical angle (p = .07), but no difference in the midthoracic curve (p = .99) - weak correlation between the dependent variables and the scores on NDI and VAS (r < .50) - significantly decreased cranial angle in IONP gp (p = .02) and WAD gp (p = .03) vs control group |
| Dolphens et al. 2012 [34] | *CS study |
N = 1196 adolescents 557 F (age 10.6 ± 0.47) 639 M (age 12.6 ± 0.54) |
Analogue questions (lifetime and 1 month Prevalence and doctor visit of NP) |
CVA (using photographic analysis), Thoracic kyphosis (using Spinal Mouse) |
ICC, Independent sample t test, logistic Regression |
A similar forward incline of the neck-head segment relative to the horizontal in both sexes CVA (F): 54.1° ± 5.2° 1 (34.4°–68.4°) CVA (M): 53.8° ± 5.8° (41°–72°) Lifetime and 1 month prevalence: Boys −25.0% and 8.9%, resp. Girls—30.2% and 10.1% resp. •In boys, CVA (OR = 0.954, p = 0.004) and trunk lean angle (OR = 1.077, p = 0.031) are significant predictors of lifetime prevalence of NP • In girls, CVA (OR = 0.905, p = 0.037) is a significant predictor of doctor visit for NP |
||
| Quek et al. 2012 [42] | * CS study |
N = 51 elderly patients (29 F, 22 M) Mean age: 66 ± 4.9 (60–78) |
NP Gp: cervical spine dysfunction (cervical pain with or without referred pain, numbness or paraesthesia) |
NDI |
CVA (using photographic analysis) Thoracic kyphosis Index (using FlexiCurve) |
Cervical ROM (using CROM device) |
Spearman and rank-biserial correlations |
Mean CVA: 45.6° ± 6.7° Women reported higher level of pain-related disability (mean NDI, 22% versus 12%; rank-biserial correlation ¼ 0.38, p < 0.01) increased age was associated with reduced cervical ROM (Spearman r = -0.41 and r = -0.51 for general and upper cervical rotation, respectively) - cervical ROM measures and CVA: positive associations between CVA and general cervical rotation (r = 0.33, p = 0.02), cervical flexion (r = 0.30, p = 0.03) and upper cervical rotation (r = 0.15, p = 0.31) - thoracic kyphosis and CVA: significantly negative association (r = -0.48, p < 0.001) FHP mediated the relationship between thoracic kyphosis and cervical ROM, specifically general cervical rotation and flexion |
|
Juliana Soares et al 2012 [45] |
Females Age 20–50 NP Gp: N = 11 Mean age: 31.55 ± 11.11; (20–50) Control Gp: N = 11 Mean age: 25.27 ± 2.61 |
NP Gp NP > 3 m Control Gp No NP |
VAS, NDI |
CVA (using photographic analysis) |
Student’s t test, spearman correlation |
CVA- lower in NP Gp vs control (p = 0.02); NP Gp: 48.55° ± 5.58°; Control Gp: 53.33° ± 3.38° CVA with VAS (r = − 0.48) CVA with NDI (r = − 0.15) NDI with VAS (r = 0.59) CVA in NP Gp was significantly less than that in control Gp, showing moderate correlation with NDI and the intensity of pain in women with complaints of NP |
||
| Nagai et al. 2014 [23] |
Male active-duty helicopter pilots Age 18–55 y NP Gp N = 27 Mean age: 34.5 ± 6.4 (18–55) Control Gp N = 27 Mean age: 34.3 ± 6.1 (18–55) |
Painfree at the time of testing, Had flown > 100 h in past 12 m |
Pain intensity (NPRS), duration, disability (NDI) | FHP (using CROM 3) |
-Conscious neck proprioception (using Vicon Nexus motion Capture system) -Isometric Cervical muscle strength and Scapular muscle (MFT, LFT) strength (using hand held dynamometer) -Prone cervical extensor strength (using a Tumble forms 2 prone pillow) -Isokinetic UFT strength (using BIODEX) -Cervical AROM (using CROM and Cross Line LASER) |
Paired T-tests or Wilcoxon Signed rank tests |
- FHP: NP Gp: 22.1 ± 1.5 cm; Control Gp: 21.7 ± 1.6 cm - Cervical ROM NP Gp: Ext: 63.7 ± 8.5°; R rot 67.7 ± 8.8°; L rot 67.4 ± 9.0° Control Gp: Ext 68.3 ± 7.4°; R rot 73.4 ± 7.4°; L rot 72.9 ± 6.8° - No significant differences were found for other variables No correlation between forward head, forward shoulder posture and NP |
|
| Ruivo et al. 2014 [5] | *CS Study |
Adolescent students N = 275 (153 F, 122 M) Age 15–17 |
ASES form, Regular NP (Y/N) |
SHA, CVA (using Photogrammetry) |
Shapiro Wilk test, Independent samples t test, chi- square test, Spearman rho Correlation |
-Mean SHA = 17.2 ± 5.7, CVA = 47.4 ± 5.2, SA = 1.4 ± 8.5° -68% subjects revealed protraction of Head -58% of subjects had protraction of shoulder -Boys showed a significantly higher mean CVA, -Adolescents with NP revealed lower mean CVA than adolescents without neck pain FHP and protracted shoulder are common postural disorders in adolescents, esp in girls. NP is prevalent in adolescents, esp girls, and it is associated with FHP |
||
| P Nejati et al. 2014 [28] | *CS Study with comparison |
Office workers N = 101 (73% F) Age: 39 ± 8 y NP Gp N = 55 (40 F, 15 M) Control Gp N = 46 |
NP Gp Chronic NP between C0 and T1, from > 3 m |
Pain location and duration, working hours, Driving hours |
High Thoracic Angle, CVA (Checked between 4th and 5th hour of work, using Photographic analysis) |
Univariate, multivariate analysis, Independent samples t test |
Mean CVA: NP Gp: 37.1° ± 7.8°; Control Gp: 37.7° ± 8.2° -statistically significant difference in CVA (p = 0.04) or HTA (p = 0.02) between NP and control Gps only during computer work (no difference during neutral position, p > 0.05) - HTA and CVA in the work position were positively correlated with NP but shoulder protrusion is not related to NP |
|
| Dunleavy et al. 2015 [50] |
*CS study with comparison **convenience sampling |
NP Gp: N = 20 F Mean age: 51.8 ± 8 (35–69) Control Gp: N = 20 F Mean age: 51.7 ± 8 (35–69) |
NP Gp: Average pain of ≥ 3/10 for more than 3 months |
Intensity (NPRS), NDI | Optotrak, FHP, Upper cervical angle (using CROM) | Independent t tests, post hoc power analysis, MDC95 |
FHP: NP Gp: 16.2 ± 2.7 cm; Control Gp: 17.5 ± 3 cm; d = 0.45; power of 0.30 No difference in CROM FHP distance between older symptomatic and asymptomatic individuals. Cervical range of motion FHP is, therefore, not recommended as a clinical outcome measure |
|
| Richards et al. 2016 [48] | *CS study with comparison |
N = 1108 adolescents (548 F, 560 M) Mean age: 17.0 ± 0.2 |
Questionnaire that included a description of NP and headache and a variety of psychosocial domains |
Postural assessment (thoracic flexion, neck flexion, cervicothoracic angle, craniocervical angle, head displacement, head flexion) in sitting | Brant test. Multivariable logistic regression |
Mean cervical angle: 47 ± 7° Four distinct clusters of sitting neck posture were identified: upright, intermediate, slumped thorax/forward head, and erect thorax/forward head. Significant associations between cluster and sex, weight, and height were found. Participants classified as having slumped thorax/forward head posture were at higher odds of mild, moderate, or severe depression. There was no significant difference in the odds of neck pain or headache across the clusters |
||
| Oliveira et al. 2016 [24] | *CS study with comparison |
10–12th grade students NP Gp N = 35 (25 F, 10 M) Mean age: 16.6 ± 0.7 Control Gp N = 35 (22 F, 13 M) Mean age: 16.7 ± 0.7 |
NP Gp: NP present at least once a week during last 3 months Control Gp No current NP; never had NP |
Intensity (VAS), frequency, duration, associated disability | CVA in standing (using goniometer and a bubble level) | Neck flexor and extensor endurance |
ICC, Mann–Whitney U test, Chi- Square test, MANOVA, Spearman Correlation |
Adolescents with NP have less FHP (CVA in NP Gp = 46.62° ± 4.92°; control Gp = 44.18° ± 3.64°, p = 0.02) and lower endurance for neck flexors (NP Gp = 24.50 ± 23.03 s; control Gp = 35.89 ± 21.53 s, p < 0.05) and extensors (NP Gp = 126.64 ± 77.94 s; Control Gp = 168.66 ± 74.77 s, p < 0.05), but No relation between FHP and NP duration, frequency and intensity |
| EK Kim et al. 2016 [17] | *CS study |
N = 126 (95 F, 31 M) College students Mean age = 23.9 ± 1.5 (19–24) N = 126 (95 F, 31 M) |
Disability (using NDI) | CVA in standing and sitting (using plumb line and digital photographic method) | Pearson Correlation |
- CVA in standing position was 61.4 ± 5.7, vs 59.7 ± 6.9 in the sitting position - RSP = 9.2 ± 1.5 - NDI = 4.9 ± 3.9 -Standing CVA with NDI (r = -0.35, p < 0.01) -Sitting CVA with NDI (r = -0.33, p < 0.01) -No significant correlation between CVA and RSP in standing and sitting positions Depending on the degree of FHP, changes were detected in the NDI. However, even an increase in the forward head tilt angle did not lead to rounded shoulder posture |
||
| Mani et al. 2017 [40] |
*CS study with comparison **Convenience Sampling |
NP Gp: N = 16, mean age: 27.7 ± 16.4 (10-65 y) Control Gp: N = 15, mean age: 24.7 ± 6.3 (17–40 y) |
NP Gp—h/o NP in past 6 m Control Gp—No h/o NP in past 6 m |
Sagittal head angle, CVA (using Photographic Analysis) |
Independent t test |
- CVA and SA were lower in NP Gp (CVA = 43.54°, SA = 49.39°) than Control Gp (CVA = 47.43°, SA = 52.28°) indicating FHP and protracted shoulder - NP Gp had high sagittal head tilt angle (SHA = 19.89° ± 5.56°) than Control Gp (SHA = 16.35° ± 8.3) indicating greater upper cervical extension, however, difference was not statistically difference |
||
| Subbarayalu et al. 2017 [46] | *CS study |
IT industry employees N = 84 (27 F, 57 M) Mean age: 20–40 |
Postural NP > 3 m, NP present at least once a week during last 3 months; NP intensity—mild (VAS 1–4) to moderate (VAS 4–6) | Pain intensity (VAS), Disability (NPQ) | CVA (using modified HPSCI) |
Deep cervical Flexor muscle performance index (using Stabilizer Pressure Biofeedback) |
Pearson correlation |
CVA in Male = 41°; Female = 42° - CVA with VAS—significant negative correlation (r = − 0.536) - CVA with NPQ—a weak negative correlation (r = − 0.389) A smaller CVA corresponded to greater NP intensity and disability No significant relationship between CVA and DCF muscle performance (r = 0.121, p = 0.275) |
| Mohankumar et al. 2017 [4] |
NP Gp N = 16, age: 25.77 ± 2.063 (20–30 y) Control Gp N = 15, age: 23.97 ± 1.974 (20–30 y) |
NP Gp NP between C0—T1 for > 2 m, NPRS 3–7 Control Gp No current NP, No h/o NP in past 1 m, Optimal posture |
NPRS (for pain in last 24 h) |
CVA, Sagittal Head Angle, Frontal plane alignment (using photographic method) |
Cervical ROM (using Goniometer) |
Independent test, Pearson correlation |
CVA—Control Gp—50.56 ± 5.47; NP Gp- 53.25 ± 3.68 t = 2.235, p = 0.029 SHA—Control Gp—22.67 ± 6.89; NP Gp- 24.91 ± 4.84 t = 2.482, p = 0.02 Cervical extension (ROM) with pain (NPRS)—fairly positive (r = 0.428) SHA (Posture) with lateral flexion and rotation (ROM) is negative (r = -0.483) FPA (Posture) with sideflexion (ROM) is positive r = 0.366 High level of significance between ROM and pain with significance level of 0.05 and between posture and ROM with significance level of 0.01 |
|
| Kim et al. 2018 [36] |
FHP subjects NP Gp: N = 22 Mean age: 28.55 ± 5.15 (20–40) Control Gp: N = 22 Mean age: 26.64 ± 4.54 (20–40) |
CVA < 52°, NP Gp: NPRS > 3 Control Gp: NPRS < 1 |
NPRS | CVA (using photogrammetry) | Active cervical ROM (using CROM equipment) | Independent sample t test, Logistic regression |
CVA in NP Gp: 44.44° ± 4.43°; Control Gp: 48.63° ± 1.9° FHP subjects in NP Gp showed a significant difference in the CVA, and the cervical ROM (flexion and extension) vs FHP subjects in Control group (p < 0.05) - Occurrence of cervical area pain was higher among subjects who had a decreased CVA (OR = 0.513, p = 0.026) and flexion motion (OR = 0.710, p = 0.038) Decreased CVA and cervical flexion range, were predictive factors for the occurrence of pain in the cervical region |
|
| P Kocur et al. 2019 [37] | *CS study |
Female office workers NP Gp: N = 16 Mean age: 42.4 ± 9.6 (30–55) Control Gp: N = 16 Mean age: 40.4 ± 5.9 |
NP Gp—diagnosed moderate work-related neck disorders (VAS 5–7, NDI: 30–48%) Control Gp: VAS 0–2 NDI ≤ 8% |
VAS, NDI |
CVA (using photographic analysis) |
Myotonometric muscle stiffness (N/m) of UFT and SCM muscles PPT of UFT, SCM (Algometer) |
Shapiro–Wilk test, Student t test/Mann–Whitney U test, Effect size (Cohen d) |
CVA in NP Gp: 43.8° ± 4.5°; control Gp: 48.3° + 5.5° NP Gp (vs Control Gp) - - significantly smaller CVA (by 8.3%; Cohen d = 0.88, p = .02) - greater stiffness of UFT myofascial tissue (by 11.3%; Cohen d = 1.05, P = .006) - No significant differences in PPT of myofascial tissue of UFT or SCM between groups NP Gp had increased anterior positioning of the head and stiffness of UFT in the sitting posture, which was not associated with changes in PPT of this muscle |
| Leila et al. 2019 [22] |
*CS study ***assessor -blind |
NP Gp N = 32 (23F, 9 M) Mean age: 36.46 ± 9.40 (20–55) Control Gp N = 35 (23 F, 12 M) Mean age: 37.31 ± 10.35 |
NP Gp—experience of pain felt dorsally between the inferior margin of the occiput and the first thoracic spine, persistent or episodic pain not associated with any trauma or known pathology for at least 3 m with a frequency no less than once a week Control Gp—no h/o NP within the year before the study |
VAS, NDI | CVA in standing (using digital photography) |
- Flexor and extensor muscle endurance - Neck muscles size was measured by a real-time ultrasonography device |
Independent t test, Mann–Whitney U test Spearman and Pearson correlation coefficients |
CVA in NP Gp: 51.39° ± 6.29°; Control Gp: 49.8° ± 7.31° NP Gp - - Significantly smaller Deep flexor (mean difference = 0.06, 95% CI = 0.02–0.11) and extensor muscles size (mean difference = 0.07, 95% CI = 0.01–0.12) - lower levels of flexor (mean difference = 14.68, 95% CI = 3.65–25.72) and global extensor endurance capacity FHP was neither different between the groups nor correlated with any of the dependent variables. Neither FHP nor endurance was correlated with pain/disability |
| Patricia et al. 2020 [41] |
*CS study **convenience sampling |
Age > 18 N = 96 FHP Gp N = 32 (21 F, 11 M) Age 20.54 ± 2.96 Control Gp N = 64 (38 F, 26 M) Age 19.48 ± 1.96 |
FHP Gp CVA < 50° Control Gp CVA > 50° |
VAS during last week, NDI | CVA (using postural assessment software) |
Cervical ROM (using CROM device) PPT (using hand held algometer) |
2*2 mixed-model ANOVA, post hoc comparison |
CVA in NP Gp: 44.63° ± 4.20°; Control Gp: 52.28° + 3.00° FHP Gp showed less PPT in all locations except for upper trapezius and scalenus medius muscles FHP Gp- less extension and right-rotation ROM No association between FHP, NP, disability, and headache |
| M Kanda et al. 2021 [49] |
- Young female subjects N = 33 (21 NSP, 18 non-NSP, mean age; 20.6 ± 0.8 years) - Elderly female subjects N = 33 (22 NSP, 11 non-NSP, mean age; 71.1 ± 4.5 years) |
NSP—symptom duration of > 1 yr |
Questionnaire for intensity, location, and duration of symptoms |
Cervical angle, Upper thoracic Angle (Using photographic method) |
Neck flexor endurance test | two-way ANOVA |
Cervical Angle in NP gp (elderly: 45.36° ± 5.14°; Young: 44.51° ± 6.22°); Control Gp (Elderly: 45.26° ± 5.22°; Young: 40.32° ± 4.81°) - No significant age-by-group interactions for any of the assessment variables - Main effect of group on the UTA was significant (p < 0.01) such that persons with NSP had larger UTA (vs without NSP) - Main effects of age on the cervical Angle (p < 0.03) and the upper thoracic angle (p < 0.01) were significant such that young persons had smaller cervical angle and UTA than elderly persons |
|
| Ertekin et al. 2021 [35] | Retrospective study | 39 NSP students who underwent SWE (Shear Wave Elastography) for upper trap and pec minor | Muscle stiffness as an alternate measure of pain | Penn shoulder scores | CVA (using Dr Goniometer) | Stiffness of b/l upper trap and pec minor (using SWE) | Multiple regression analysis |
Mean CVA: 52.2° ± 3.8° No relation between muscle stiffness (of Right UFT and b/l Pec minor), and CVA and SA, p > 0.05 Positive relation between Left UFT stiffness and SA (p = 0.003, 95% CI = 0.003–0.014) in RSP subjects There is no relationship between RSP and Neck pain |
| R Save et al. 2021 [44] | *Cross-sectional study |
Age = 18–25 NP Gp: N = 18 Control Gp: N = 18 |
NP Gp- NP > 3 m |
NRS | CVA (using Photographic analysis; ImageJ software), Protracted Shoulders |
Unpaired t- test, Mann Whitney U test, Spearman Rank Correlation test |
CVA in NP Gp: 40.213° ± 3.881°; Control Gp: 48.363° ± 2.776°; CVA with NRS (r = -0.1529; p = 0.5446) No significant correlation between CVA and protracted shoulders with severity of neck pain (p = 0.54 and p = 1.64, respectively) |
|
| Sarig Bahat H. et al. 2022 [43] |
*Cross-sectional study **Convenience Sampling |
NP Gp: N = 22 (14 F, 8 M) Mean age: 38.1 ± 9.9 (18–65) Control Gp: N = 20 (10 F, 10 M) Mean age: 33.6 ± 7.7 y (18–65) |
NP Gp- Self-reported persistent neck pain (> 2 months), with or without referral to the upper limb, and NDI > 10% (i.e., mild disability) Control Gp: No systemic diseases or spinal pain |
Pain intensity (VAS), the neck disability index (NDI) questionnaire |
CVA (using Photographic Analysis) With and without HMD |
Neck kinematics using specialized VR software |
mixed-model repeated-measures ANOVA, Studentized Maximum Modulus (SMM) post hoc adjustment, Wilcoxon Signed rank test, Spearman’s correlation |
CVA in NP Gp: 48.24° ± 7.29; Control Gp: 48.9° ± 5.89 (p > .05) NP group demonstrated a restricted range of motion and slower neck movements (p < .05) No significant correlation between FHP and VAS, NDI, and most neck kinematic measures Correlation of CVA with VAS: rs = − 0.31; CVA with NDI: rs = − 0.15 |
NP neck pain, NOS Newcastle–Ottawa scale, F female, M male, Gp group, m month, y year, NPQ Northwick Park Neck Pain Questionnaire, NPRS Numeric Pain Rating Scale, HPSCI head posture and spinal curvature instrument, UL upper limb, CS cross-sectional, EHPI electronic head posture instrument, AHT anterior head translation, IONP idiopathic neck pain, WAD Whiplash associated disorder, NDI neck disability index, VAS visual analog scale, FHP forward head posture, CVA craniovertebral angle, SHA sagittal head angle, SA shoulder angle, ASES American shoulder and Elbow Surgeons Shoulder Assessment, HTA high thoracic angle, UTA upper thoracic angle, ROM range of motion, RSP rounded shoulder posture, DCF deep cervical flexors, FPA frontal plane alignment, UFT upper fibers of trapezius, SCM sternocleidomastoid, PPT pressure pain threshold, NSP neck shoulder pain, HMD head mounted device, VR virtual reality
Neck Pain and Sagittal Head and Neck Posture
Twenty-six studies investigated for the association between NP and sagittal head and neck posture. Different measures used to assess this sagittal alignment were CVA [4–6, 17, 21, 22, 24, 28, 34–46], SHA [4–6, 40], anterior head translation (AHT) [38], cranial angle [47, 48], cervical angle [47–49], and FHP [23, 50].
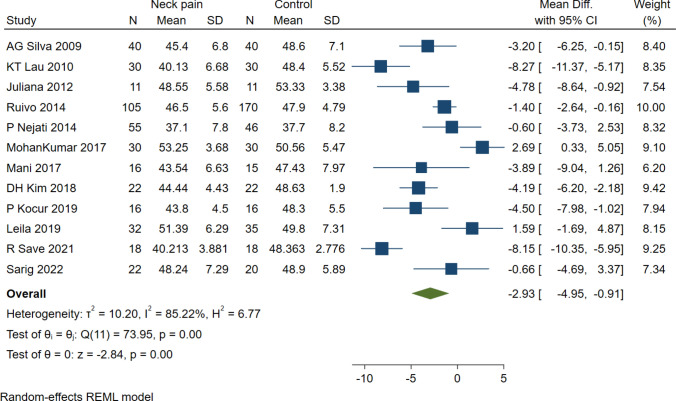
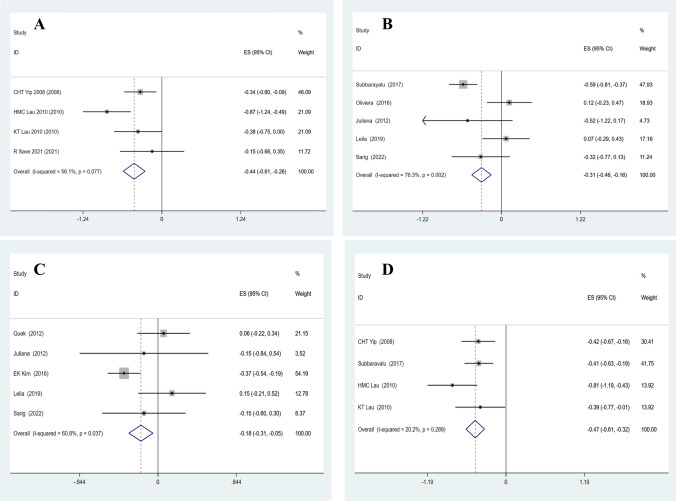
CVA and Neck Pain
Out of the total 21 studies which looked for CVA, 14 studies compared the CVA between neck pain group and control (asymptomatic) group, using different instruments. NP group characterized smaller CVA in all except three studies [4, 22, 24]. Twelve studies (N = 850 subjects) that compared CVA (photographically analyzed) [4–6, 22, 28, 36, 37, 39, 40, 43–45] had significant high statistical heterogeneity (I2 = 85.22%, H2 = 6.77), and a significant mean pool difference of − 2.93 (95% CI − 4.95 to − 0.91) between pain and pain-free groups (Fig. 2). Patricia et al. [41] compared for CVA between FHP and non-FHP groups, and reported that there were no statistically significant differences between groups in frequency, pain intensity or disability (NDI). In addition, CVA was predictive of NP occurrence in FHP group (OR = 0.513, 95% CI = 0.286–0.922, p < 0.05) [36] and lifetime NP predictor in adolescent boys (OR = 0.954, p = 0.004) or doctor visit among girls with NP (OR = 0.905, p = 0.037) [34].
Fig. 2.
Forest plot of craniovertebral angle (photographically analyzed). Comparison between Neck pain and Control (pain-free) subjects
One of the studies compared the CVA in mechanical NP patients using Electronic Head Posture Equipment, EHPI (40.8° ± 5.4°) and AHT using gold standard method of lateral cervical radiograph (18.0 ± 12.6 mm) [38]. Meta-analysis could not be performed for studies that used Head posture and spinal curvature instrument (HPSCI) [21, 46] to measure CVA in adults, owing to lack of a control group [46]. The other comparative cross-sectional study reported that the CVA of NP group was significantly smaller (p < 0.000) than control group [21].
Cervical Angle and Neck Pain
Cervical angle [47–49] has been used as the complimentary measure of CVA. Helgadottir et al. [47] found a tendency in the cervical angle (p = 0.07) among the groups, but did not mention the exact data. Kanda et al. [49] reported non-significant difference group wise (p = 0.11) and age*group wise (p = 0.13). The cross-sectional study [in the Raine Cohort study] determined four clusters of neck posture in 17-year-olds, with higher mean cervical angle in clusters 3 and 4 (N = 532) among others [48]. Out of total 1108, 219 participants (22%) reported persistent neck pain, with 141 (64%) being female. After adjusting for sex, there was no difference among the clusters and the odds of persistent neck pain (p = 0.773). Meta-analysis for cervical angle, therefore, could not be performed because of difference in methodology.
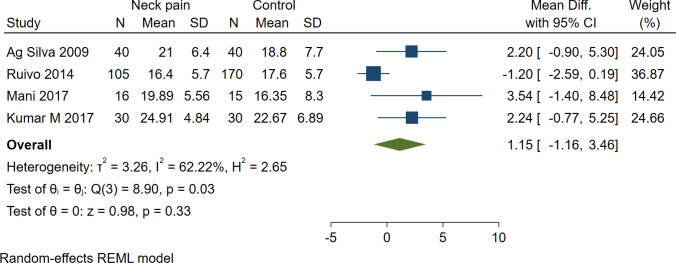
Sagittal Head Angle and Neck Pain
Another surrogate measure used for head and neck posture was SHA [4–6, 40], implying upper cervical extension commonly seen with forward head posture. NP subjects had higher SHA in all, except one study [5]. Taken together, the mean pooled difference and heterogeneity were statistically insignificant (1.15, 95% CI − 1.16 to 3.46; I2 = 62.22%, H2 = 2.65) (Fig. 3). Of four studies, only one reported significant between-group difference (p = 0.02) for SHA [4].
Fig. 3.
Forest plot of sagittal head angle. Comparison between neck pain and control (pain-free) subjects
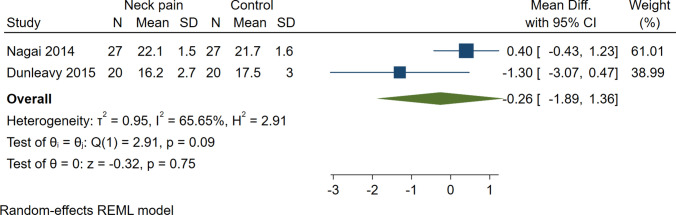
FHP and Neck Pain
Two studies [23, 50] used CROM to measure FHP; Nagai et al. [50] checked the FHP in male helicopter pilots and Dunleavy et al. [23] checked in female subjects, and both reported non-significant inter-group difference (p = 0.201, p = 0.14, respectively). The results were somewhat contradictory, where one study [23] showed higher FHP in pain group, and the other [50] showed lower FHP. The data of two studies (N = 94 subjects) revealed that the mean pooled difference [− 0.26 (95% CI − 1.89 to 1.36)] and the heterogeneity [I2 = 65.65%, H2 = 2.91] were non-significant (Fig. 4).
Fig. 4.
Forest plot of FHP. Comparison between neck pain and control (pain-free) subjects
Cranial Angle and Neck Pain
Two studies used cranial angle [47, 48] as a complementary measure of SHA to assess upper cervical posture. Helgadottir et al. [47] reported significantly decreased cranial angle in IONP group (p = 0.02) compared to control group but did not mention the exact data. Richards et al. [48] concluded the mean cranial angle to be 70 ± 8°, which was same for both the genders. The cranial angle and cervical angle were shown to have a strong negative correlation (r = − 0.73).
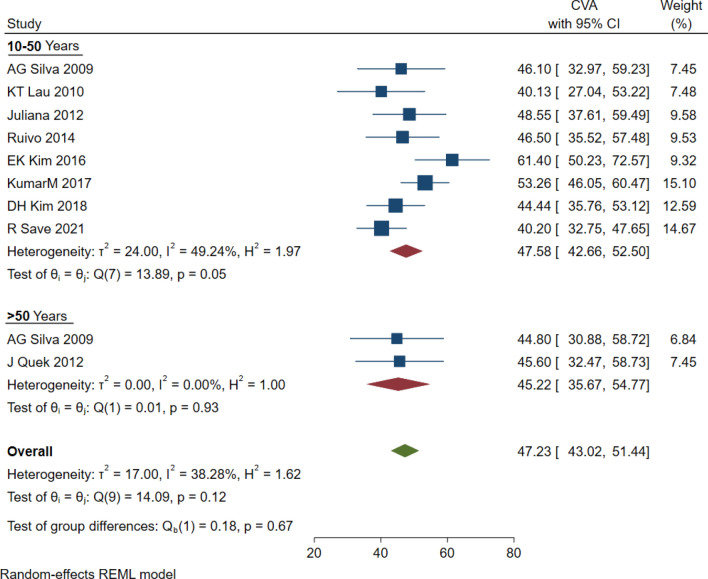
Age- and Gender-Wise Variation in Posture of Neck Pain Subjects
Nine studies were analyzed for age-wise postural (CVA) variation. Data of 433 subjects revealed a CVA difference of 2.36° among young (age 10–50) and elderly (age > 50) group (Fig. 5). Only one study [21] checked for and reported significant correlation between age and CVA (rp = − 0.380, p = 0.002), but did not mention the exact data, hence was not included in this meta-analysis.
Fig. 5.
Meta-analysis of age-wise variation in Craniovertebral Angle. Comparison between young (10–50 years) and elderly (> 50 years) subjects with neck pain
Another postural measure (cervical angle) reportedly had no significant age-wise difference (p = 0.13) [49].
Seven studies were included in the analysis for the gender-wise variation in CVA. Data of 1651 subjects revealed a difference of 2.57° (M = 44.44°, F = 47.01°) (Fig. 6). Gender-wise variation in FHP by CROM was stated by two studies [23, 50], with both studies including either males or females. Difference between the two was 5.9 cm (M = 22.1 ± 1.5 cm [23], F = 16.2 ± 2.7 cm [50]).
Fig. 6.
Meta-analysis of gender-wise variation in craniovertebral Angle. Comparison between female and male subjects with neck pain
Correlation Between Neck Pain and Craniocervical Posture
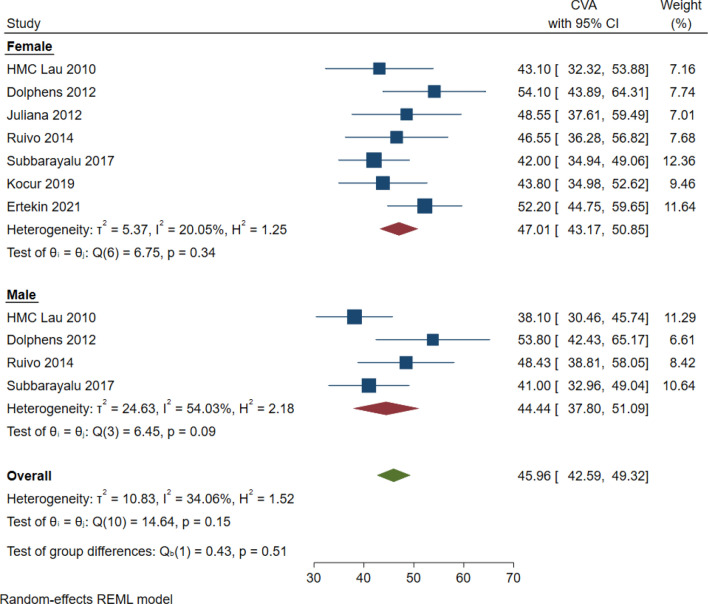
Neck Pain Intensity
Four studies (N = 140 subjects) [21, 38, 39, 44] checked for correlation between CVA and NPRS. All the studies correlated negatively (moderate-good) in adult NP subjects except one that showed a weak positive correlation [44]. The overall effect size was significant (− 0.44; 95% CI − 0.61 to − 0.26), with insignificant heterogeneity (I2 = 56.1%, p = 0.077) (Fig. 7a). Lau et al. [39] also reported significant relationship between CVA and presence of neck pain (rs = − 0.56, 95% CI − 0.71 to − 0.36, p < 0.01). The authors also conducted multiple logistic regression with the control of age and gender and concluded that CVA was a significant predictor for presence of neck pain (OR = 0.86, p = 0.04), and an insignificant predictor for NPRS (p = 0.46).
Fig. 7.
a, b Meta-analysis of correlation of craniovertebral angle with neck pain Intensity measured through a NPRS and b VAS. c, d Meta-analysis of correlation of craniovertebral angle with neck pain disability measured through c NDI and d NPQ
Five studies [22, 24, 43, 45, 46] measured the correlation between CVA and Visual Analogue Scale (VAS). Three studies [43, 45, 46] reported moderate negative correlation in young adults. On the contrary, weak positive correlation was described in adolescents [24] and adult subjects [22]. There was significant heterogeneity (I2 = 76.3%, p = 0.002) across five studies. The data from five studies (N = 206 subjects) reported a significant overall effect size at − 0.31 (95% CI − 0.46 to − 0.16) (Fig. 7b).
One study [24] suggested no correlation between FHP and NP duration, frequency and intensity, while significantly positive correlation of AHT with pain intensity (p = 0.006), disability (p = 0.033) and CVA (r = − 0.71, p < 0.001) was reported by Lau et al. [38].
Neck Pain-Related Disability
Data from five studies [17, 22, 42, 43, 45] were significantly heterogeneous (I2 = 60.8%; p = 0.037) (Fig. 7c). Studies have identified negative [17, 43, 45] to weak positive [22, 42] correlation between CVA and NDI. The overall effect size was − 0.18 (95% CI − 0.31 to − 0.05).
Across four studies (N = 206 subjects) [21, 38, 39, 46] assessing CVA and NPQ, the overall effect size for correlation and heterogeneity was − 0.47 (95% CI − 0.61 to − 0.32) and I2 = 20.2%; p = 0.289, respectively (Fig. 7d). All studies reported moderate to good negative correlation in adult subjects, though it did not reach the level of significance for one (p = 0.06) [39]. In addition, CVA was an insignificant predictor for NPQ (p = 0.67) [39].
In addition, only one of the studies [5] trivially correlated pain-related dysfunction in ADLs (ASES) with SHA in adolescents aged 15–17 (r = − 0.031 for ASES right, and r = 0.050 for ASES left).
Risk of Bias in Studies
Risk of bias in the included studies was done using the Newcastle—Ottawa Quality Assessment Scale (NOS), results of which are shown in Table 4. All the studies were assessed for quality grouped into three domains (selection, comparability and outcome). The average score for risk of bias was 5.61. Six studies were found to be of low methodological quality, scoring ≤ 4, 13 studies of moderate quality scored 5–6 on NOS, and 7 high-quality studies with score ≥ 7. The score did not affect the inclusion or exclusion of any study from the review,it instead dictated the strength of the reported results.
Table 4.
Newcastle–Ottawa quality assessment scale
| Study ID | Selection | Comparability | Outcome | Final Score |
|---|---|---|---|---|
| Yip et al. 2008 [21] | 3 | 1 | 3 | 7/10 |
| Silva et al. 2009 [6] | 3 | 1 | 3 | 7/10 |
| Lau et al. 2010 [38] | 2 | 2 | 3 | 7/10 |
| Lau et al. 2010 [39] | 3 | 1 | 2 | 6/10 |
| Helgadottir et al. 2011 [47] | 4 | 1 | 2 | 7/10 |
| Dolphens et al. 2012 [34] | 3 | 1 | 2 | 6/10 |
| Quek et al. 2012 [42] | 2 | 2 | 2 | 6/10 |
| Juliana Soares et al. 2012 [45] | 2 | 1 | 2 | 5/10 |
| Nagai et al. 2014 [23] | 3 | 1 | 2 | 6/10 |
| Ruivo et al. 2014 [5] | 4 | 1 | 3 | 8/10 |
| Nejati et al. 2014 [28] | 3 | 0 | 1 | 4/10 |
| Dunleavy et al. 2015 [50] | 3 | 1 | 2 | 6/10 |
| Richards et al. 2016 [48] | 4 | 0 | 2 | 6/10 |
| Oliveira et al. 2016 [24] | 3 | 1 | 2 | 6/10 |
| Kim et al. 2016 [17] | 1 | 1 | 1 | 3/10 |
| Mani et al. 2017 [40] | 2 | 0 | 1 | 3/10 |
| Subbarayalu et al. 2017 [46] | 3 | 1 | 1 | 5/10 |
| Mohankumar et al. 2017 [4] | 1 | 2 | 2 | 5/10 |
| Kim et al. 2018 [36] | 1 | 1 | 2 | 4/10 |
| Kocur et al. 2019 [37] | 0 | 1 | 2 | 3/10 |
| Leila et al. 2019 [22] | 5 | 1 | 3 | 9/10 |
| Patricia et al. 2020 [41] | 4 | 1 | 3 | 8/10 |
| Kanda et al. 2021 [49] | 1 | 1 | 2 | 4/10 |
| Ertekin et al. 2021 [35] | 1 | 1 | 3 | 5/10 |
| Save et al. 2021 [44] | 1 | 1 | 2 | 4/10 |
| Sarig Bahat et al. 2022 [43] | 2 | 2 | 2 | 6/10 |
Reporting Publication Bias
Publication bias for CVA is reflected in the funnel plot (Fig. 8). The craniovertebral angle measured through photographic analysis, that is, the mean difference from the individual studies on the horizontal axis was plotted against the study precision, as measured by the standard error of the mean difference on the vertical axis.
Fig. 8.
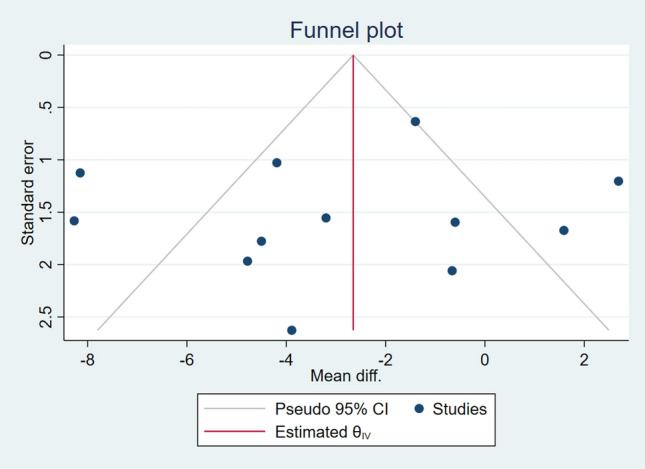
Funnel plot of craniovertebral angle (photographically analyzed)
Discussion
The aim of this review was to establish and critically appraise the existing evidence on association between sagittal head and neck posture and neck pain in individuals above 10 years of age, and to identify the association of postural measures with respect to age and gender. A total of 26 studies were included which used different instruments to measure the head and neck posture in relation to the neck pain. The common elements of neck pain included in the studies were pain intensity, frequency, duration, and pain-related disability. Few of the included studies used a self-reported questionnaire for neck pain, mostly in the form of analog data (yes–no/month and lifetime prevalence).
We found substantial heterogeneity in the included studies, in terms of sample population demographic data, instrument used to measure posture, reporting of posture- and neck pain-related parameters, etc. The variation and complexity of the measuring instruments has been talked upon in previous reviews as well [51, 52]. Thus, due to lack of consistency of the parameters and control group, and also due to variation in the type of instruments, the meta-analysis could not be performed for several of the different angular and linear postural measures, e.g., cervical angle was checked by three different studies [47–49], but only one study reported the data of neck pain and control groups.
The findings from the review indicate that the photographically analyzed CVA had statistically significant negative correlation with neck pain-related disability and a moderate negative correlation with neck pain intensity. These results are in line with the ones reported by Mahmoud et al. [26], but the latter did not analyze the different disability scales separately. Observationally, in a clinical setting, it would be interesting to test if the change in head posture ameliorate the neck pain. Quantifying cervicothoracic junction mobility hitherto remains the reliable technique to assess the chronic neck pain severity [53].
To the best of our knowledge, this is the first comprehensive review considering association of all the head and neck postural measures with neck pain characteristics, and subgrouping them with respect to instrument, age and gender. These issues have not been addressed deeply in the previous reviews. In addition, we tried grouping according to the pain duration (chronicity), but that was not feasible owing to lack of reported data. Individuals with chronic pain have a dearth of potential to modulate the pain pathway through the emotional distress. Mechanistically, this is unclear whether this holds significance in acute pain subjects [54].
Factors other than just pain should also be considered while discussing about postural alterations. For instance, occupational exposure, participation in sports, screen addiction, etc. can be equally responsible for development of faulty spinal alignment.
Similarly, a very important factor that plays role in development of neck shoulder pain and/or poor craniocervical posture is the sitting duration, though this has not been the focus in our study. Five elements of sitting relating to upper quadrant musculoskeletal pain in children and adolescents as identified in a review by Brink and Louw [55] are sitting duration, activities while sitting, activities while sitting and sitting duration, dynamism and postural angles. In another review [56], the authors reported that duration of sitting posture and other psychosocial factors may contribute to upper quadrant musculoskeletal pain in children and adolescents. Similar results were reported by Ariens et al., who concluded that sitting at work for more than 95% of the working time seems to be a risk factor for neck pain [57].
The results showed that the most commonly studied postural measure for head and neck was Craniovertebral angle, and due to the expected age-related biomechanical changes, and the fact that pain prevalence increases with age [58, 59], it could be assumed that CVA should be lower in elderly population. This was supported by the findings of this review, though the difference was very minute. Previously, Mahmoud et al. [26] described the relation of primarily CVA with neck pain, and grouped them into three for the age. The authors concluded that FHP was significantly correlated with neck pain measures in adults and elderly, but not in adolescents. Similar results were reported in the review by Andias and Silva, which found limited evidence that there is no difference in cervicothoracic posture in adolescents with and without Neck pain [32]. In adults, the conflicting results were reported in an earlier systematic review by Silva et al., which found insufficient good-quality evidence of difference in head posture between neck pain and pain-free subjects [31].
We found conflicting results for SHA and FHP in the included studies. Contradictory findings between studies could be due to difference in the age group of included population, difference in the methodological quality, e.g., SHA was found to be lower in NP subjects by Ruivo et al. [5], while it was higher for the other three studies. It is claimed that a more forward head posture is associated with an increase in head extension [60].
Considering the gender-related differences in the postural measures, meta-analysis for pooled gender variation in our review revealed higher CVA and lower FHP by CROM in female NP subjects. This needs future research consideration keeping in mind the findings of previously reported studies that there exists a gender bias with respect to incidence of neck pain (females being affected more than males) [2, 30], thus accounting for the altered biomechanical alignment, and less strength/endurance of deep cervical flexors. This warrants extensive research, so as to clearly comment on the influence of gender on different postural angles with reference to the neck pain measures.
Since most of the included studies were of cross-sectional design, the cause-and-effect relation of posture and pain could not be established [61], i.e., the question whether faulty posture is the cause for neck pain or vice versa, remains unanswered.
Limitations
This review does not take into account the factors, other than pain, that need consideration when talking about postural alterations (e.g., sitting duration, screen time, and physical activity). The position used to assess the posture was not specified in many studies, hence could not be a factor for analysis. Communication with certain authors was not successful, hence, there was lack of data from few studies. In addition, the high variability in the instrument used to measure craniovertebral angle posed difficulty in collective analysis, owing to lack of sufficient information regarding the instruments’ specifications, sensitivity/specificity and the measurable range.
Clinical Implication
The clinical implication for this review includes correction of faulty head and neck posture in sagittal plane for relief in neck pain. The techniques, for instance, may focus on correcting the biomechanical aspect by strengthening the deep cervical flexors muscles or manually releasing the overactive global neck flexors and/or suboccipital muscles [62, 63].
Conclusion
The present review found strong evidence that the craniovertebral angle as a measure of sagittal head and neck posture differs in individual with and without neck pain, with CVA being lower in subjects with neck pain. Differences in CVA exist for gender and age in neck pain subjects. Limited evidence exists with regards to sagittal head angle, and very limited evidence for other surrogate measures that there exists no difference in neck pain and asymptomatic subjects. The postural measures (CVA) correlated well with the neck pain intensity and disability, but with limited evidence from moderate to high-quality studies. To conclude, the authors can state that the craniovertebral angle differs for age, gender, and pain vs pain-free subjects, and that the other surrogate measures for sagittal craniocervical posture need to be further explored extensively to be able to comment upon.
Author Contributions
BR: conceptualization, data curation, methodology, writing—original draft preparation, and writing—reviewing and editing. AP: data curation, writing—original draft preparation. AC: formal analysis, methodology, and software. PP: software and data curation. MSD: conceptualization, methodology, and writing—reviewing and editing.
Funding
The authors did not receive support from any organization for the submitted work.
Data Availability
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Declarations
Conflict of Interest
ON behalf of all the authors, the corresponding author states that there is no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This article does not contain any original research carried out on animal or human subjects.
Informed Consent
Since this is a review article with data from already published studies, and no direct/indirect patient involvement, hence informed consent was not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
2/17/2023
An article note has been removed.
References
- 1.Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clinic Proceedings. 2015;90:284–299. doi: 10.1016/j.mayocp.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: A systematic critical review of the literature. European Spine Journal. 2006;15:834–848. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoy D, March L, Woolf A, et al. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Annals of the Rheumatic Diseases. 2014;73(7):1309–1315. doi: 10.1136/annrheumdis-2013-204431. [DOI] [PubMed] [Google Scholar]
- 4.Mohankumar P, Yie LW. Head and Neck Posture in Young Adults with Chronic Neck Pain. International Journal of Recent Advances in Multidisciplinary Research. 2017;04(11):2946–2951. [Google Scholar]
- 5.Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Brazilian Journal of Physical Therapy. 2014;18(4):364–371. doi: 10.1590/bjpt-rbf.2014.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silva AG, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI. Head posture and neck pain of chronic non-traumatic origin: A comparison between patients and pain-free persons. Archives of Physical Medicine and Rehabilitation. 2009;90:669–674. doi: 10.1016/j.apmr.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 7.Chiu TW, Ku WY, Lee MH, Sum WK, Wong CY, Yuen CK. A study on the prevalence of and risk factors for neck pain among university academic staff in Hong Kong. Journal of Occupational Rehabilitation. 2002;12(2):77–91. doi: 10.1023/a:1015008513575. [DOI] [PubMed] [Google Scholar]
- 8.Good M, Stiller C, Zauszniewski JA, Anderson GC, Stanton-Hicks M, Grass JA. Sensation and distress of pain scales: Reliability, validity, and sensitivity. Journal of Nursing Measurement. 2001;9(3):219–223. doi: 10.1891/1061-3749.9.3.219. [DOI] [PubMed] [Google Scholar]
- 9.Haughie LJ, Fiebert IM, Roach KE. Relationship of forward head posture and cervical backward bending to neck pain. The Journal of Manual & Manipulative Therapy. 1995;3(3):91–97. doi: 10.1179/jmt.1995.3.3.91. [DOI] [Google Scholar]
- 10.Harrison AL, Barry-Greb T, Wojtowicz G. Clinical measurement of head and shoulder posture variables. Journal of Orthopaedic and Sports Physical Therapy. 1996;23(6):353–361. doi: 10.2519/jospt.1996.23.6.353. [DOI] [PubMed] [Google Scholar]
- 11.McLean L. The effect of postural correction on muscle activation amplitudes recorded from the cervicobrachial region. Journal of Electromyography and Kinesiology. 2005;15(6):527–535. doi: 10.1016/j.jelekin.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Woodhull AM, Maltrud K, Mello BL. Alignment of the human body in standing. European Journal of Applied Physiology. 1985;54(1):109–115. doi: 10.1007/BF00426309. [DOI] [PubMed] [Google Scholar]
- 13.Kendall F, McCreary E, Provance P, Rodgers MM, Romani WA. Muscles testing and function, with posture and pain. 5. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 14.Visser B, Van Dieen JH. Pathophysiology of upper extremity muscle disorders. Journal of Electromyography and Kinesiology. 2006;16(1):1–16. doi: 10.1016/j.jelekin.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 15.Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Physical Therapy. 1992;72(6):425–431. doi: 10.1093/ptj/72.6.425. [DOI] [PubMed] [Google Scholar]
- 16.Watson DH. (1994). Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Grieve’s Modern Manual Therapy—The Vertebral Column. 2nd edn., p. 349–60. [DOI] [PubMed]
- 17.Kim EK, Kim JS. Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture. Journal of Physical Therapy Science. 2016;28(10):2929–2932. doi: 10.1589/jpts.28.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garrette TR, Youdas JW, Madson TJ. Reliability of measuring forward head posture in a clinical setting. Journal of Orthopaedic Sport Physical Therapy. 1993;17(3):155–160. doi: 10.2519/jospt.1993.17.3.155. [DOI] [PubMed] [Google Scholar]
- 19.Wilmarth MA, Hilliard TS. Measuring head posture via the craniovertebral angle. Orthopaedic Physical Therapy Practice. 2002;14(1):13–15. [Google Scholar]
- 20.Willford CH, Kisner C, Glenn TM, Sachs L. The interaction of wearing multifocal lenses with head posture and pain. Journal of Orthopaedic and Sports Physical Therapy. 1996;23(3):194–199. doi: 10.2519/jospt.1996.23.3.194. [DOI] [PubMed] [Google Scholar]
- 21.Yip CHT, Chiu TTW, Poon ATK. The relationship between head posture and severity and disability of patients with neck pain. Manual Therapy. 2008;13(2):148–154. doi: 10.1016/j.math.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Ghamkhar L, Kahlaee AH. Is forward head posture relevant to cervical muscles performance and neck pain? A case-control study. Brazilian Journal of Physical Therapy. 2019;23(4):346–354. doi: 10.1016/j.bjpt.2018.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagai T, Abt JP, Sell TC, et al. Neck proprioception, strength, flexibility, and posture in pilots with and without neck pain history. Aviation, Space and Environmental Medicine. 2014;85:529–535. doi: 10.3357/asem.3874.2014. [DOI] [PubMed] [Google Scholar]
- 24.Oliveira AC, Silva AG. Neck muscle endurance and head posture: A comparison between adolescents with and without neck pain. Manual Therapy. 2016;22:62–67. doi: 10.1016/j.math.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 25.Straker LM, O’Sullivan PB, Smith AJ, Perry MC, Coleman J. Sitting spinal posture in adolescents differs between genders, but is not clearly related to neck/shoulder pain: An observational study. Australian Journal of Physiotherapy. 2008;54:127–133. doi: 10.1016/s0004-9514(08)70046-1. [DOI] [PubMed] [Google Scholar]
- 26.Mahmoud NF, Hassan KA, Abdelmajee SF, Moustafa IM, Silva AG. The relationship between forward head posture and neck pain: A systematic review and meta-analysis. Current Reviews in Musculoskeletal Medicine. 2019;12:562–577. doi: 10.1007/s12178-019-09594-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gustafsson E, Thomee S, Grimby-Ekman A, Hagberg M. Texting on mobile phones and musculoskeletal disorders in young adults: A five-year cohort study. Applied Ergonomics. 2017;58:208–214. doi: 10.1016/j.apergo.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 28.Nejati P, Lotfiyan S, Moezy A, Nejati M. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Medical Journal of The Islamic Republic of Iran. 2014;28:26. [PMC free article] [PubMed] [Google Scholar]
- 29.Dalton M, Coutts A. The effect of age on cervical posture in a normal population. In: Boyling JD, Palastanga N, editors. Grieve’s modern manual therapy: The vertebral column. Churchill Livingstone; 1994. [Google Scholar]
- 30.McLean SM, May S, Klaber-Moffett J, Sharp DM, Gardiner E. Risk factors for the onset of non-specific neck pain: A systematic review. J Epidemiol Community Health England. 2010;64(7):565–572. doi: 10.1136/jech.2009.090720. [DOI] [PubMed] [Google Scholar]
- 31.Silva AG, Sharples P, Johnson MI. Studies comparing surrogate measures for head posture in individuals with and without neck pain. The Physical Therapy Review. 2010;15(1):12–22. doi: 10.1179/174328810X12647087218631. [DOI] [Google Scholar]
- 32.Andias R, Silva AG. A systematic review with meta-analysis on functional changes associated with neck pain in adolescents. Musculoskeletal Care. 2019;17:23–36. doi: 10.1002/msc.1377. [DOI] [PubMed] [Google Scholar]
- 33.Modesti PA, Reboldi G, Cappuccio FP, et al. ESH working group on CV risk in low resource settings. Panethnic differences in blood pressure in Europe: A systematic review and meta-analysis. PLoS ONE. 2016;11(1):e0147601. doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dolphens M, Cagnie B, Coorevits P, et al. Sagittal standing posture and its association with spinal pain: A school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine. 2012;37:1657–1666. doi: 10.1097/BRS.0b013e3182408053. [DOI] [PubMed] [Google Scholar]
- 35.Ertekin E, Guanydin OE. Neck pain in rounded shoulder posture: Clinico-radiologic correlation by shear wave elastography. International Journal of Clinical Practice. 2021;75(8):e14240. doi: 10.1111/ijcp.14240. [DOI] [PubMed] [Google Scholar]
- 36.Kim DH, Kim CJ, Son SM. Neck pain in adults with forward head posture: Effects of craniovertebral angle and cervical range of motion. Osong Public Health and Research Perspectives. 2018;9(6):309–313. doi: 10.24171/j.phrp.2018.9.6.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kocur P, Wilski M, Lewandowski J, Łochynski D. Female office workers with moderate neck pain have increased anterior positioning of the cervical spine and stiffness of upper trapezius myofascial tissue in sitting posture. The Journal of Injury, Function, and Rehabilitation. 2019;11:476–482. doi: 10.1016/j.pmrj.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 38.Lau HMC, Chiu TTW, Lam T-H. Measurement of craniovertebral angle with electronic head posture instrument: Criterion validity. Journal of Rehabilitation Research and Development. 2010;47(9):911–918. doi: 10.1682/JRRD.2010.01.0001. [DOI] [PubMed] [Google Scholar]
- 39.Lau KT, Cheung KY, Chan Kwok B, Chan MH, Lo KY, Wing Chiu TT. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Manual Therapy. 2010;15(5):457–462. doi: 10.1016/j.math.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 40.Mani S, Sharma S, Omar B, Ahmad K, Muniandy Y, Singh DKA. Quantitative measurements of forward head posture in a clinical settings: A technical feasibility study. European Journal of Physiotherapy. 2017;19(3):119–123. doi: 10.1080/21679169.2017.1296888. [DOI] [Google Scholar]
- 41.Martinez-Merinero P, Nuñez-Nagy S, Achalandabaso-Ochoa A, Fernandez-Matias R, Pecos-Martin D, Gallego-Izquierdo T. Relationship between forward head posture and tissue mechanosensitivity: A Cross-Sectional Study. Journal of Clinical Medicine. 2020;9:634. doi: 10.3390/jcm9030634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Manual Therapy. 2013;18:65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 43.Sarig Bahat H, Levy A, Yona T. The association between forward head posture and non-specific neck pain: A cross-sectional study. Physiotherapy Theory and Practice. 2022;23:1–10. doi: 10.1080/09593985.2022.2044420. [DOI] [PubMed] [Google Scholar]
- 44.Save R, Varghese A. Relation of neck pain, forward head position and protracted shoulders in students with chronic neck pain. International Journal of Scientific Research. 2021;10(7):28–30. doi: 10.36106/ijsr. [DOI] [Google Scholar]
- 45.Soares JC, Weber P, Trevisan ME, Trevisan CM, Rossi AG. Correlation between head posture, pain and disability index neck in women with complaints of neck pain. Fisioterapia Pesquisa. 2012;19(1):68–72. doi: 10.1590/S1809-29502012000100013. [DOI] [Google Scholar]
- 46.Subbarayalu AV, Ameer MA. Relationships among head posture, pain intensity, disability and deep cervical flexor muscle performance in subjects with postural neck pain. Journal of Taibah University Medical Sciences. 2017;12(6):541–547. doi: 10.1016/j.jtumed.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Helgadottir H, Kristjansson E, Mottram S, Karduna A, Jonsson HJ. Altered alignment of the shoulder girdle and cervical spine in patients with insidious onset neck pain and whiplash associated disorder. Journal of Applied Biomechanics. 2011;27(3):181–191. doi: 10.1123/jab.27.3.181. [DOI] [PubMed] [Google Scholar]
- 48.Richards KV, Beales DJ, Smith AJ, O’Sullivan PB, Straker LM. 2016 Neck posture clusters and their association with biopsychosocial factors and neck pain in Australian adolescents. Physical Therapy. 2016;96:1576–1587. doi: 10.2522/ptj.20150660. [DOI] [PubMed] [Google Scholar]
- 49.Kanda M, Kitamura T, Sato N. Cervicothoracic spinal alignment and neck flexor muscle endurance in young and older adult females with and without neck and shoulder pain (Katakori in Japanese) Journal of Physical Therapy Science. 2021;33:489–494. doi: 10.1589/jpts.33.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dunleavy K, Neil J, Tallon A, Adamo DE. Reliability and validity of cervical position measurements in individuals with and without chronic neck pain. The Journal of Manual & Manipulative Therapy. 2015;23(4):188–196. doi: 10.1179/2042618614Y.0000000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Vries J, Ischebeck BK, Voogt LP, et al. Joint position sense error in people with neck pain: A systematic review. Manual Therapy. 2015;20(6):736–744. doi: 10.1016/j.math.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 52.Hesby BB, Hartvigsen J, Rasmussen H, Kjaer P. Electronic measures of movement impairment, repositioning, and posture in people with and without neck pain—A systematic review. Systematic Reviews. 2019;8:220. doi: 10.1186/s13643-019-1125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee JH, Park YK, Kim JH. Chronic neck pain in young adults: Perspectives on anatomic differences. The Spine Journal. 2014;14(11):2628–2638. doi: 10.1016/j.spinee.2014.02.039. [DOI] [PubMed] [Google Scholar]
- 54.Nicholas M, Vlaeyen JWS, Rief W, et al. 2019 The IASP classification of chronic pain for ICD-11: Chronic primary pain. Pain. 2019;160:28–37. doi: 10.1097/j.pain.0000000000001390. [DOI] [PubMed] [Google Scholar]
- 55.Brink Y, Abigail LQ. A systematic review of the relationship between sitting and upper quadrant musculoskeletal pain in children and adolescents. Manual Therapy. 2013;18:281–288. doi: 10.1016/j.math.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 56.Prins Y, Crous L, Louw PQA. A systematic review of posture and psychosocial factors as contributors to upper quadrant musculoskeletal pain in children and adolescents. Physiotherapy Theory and Practice. 2008;24(4):221–242. doi: 10.1080/09593980701704089. [DOI] [PubMed] [Google Scholar]
- 57.Ariens GAM, Bongers PM, Douwes M, et al. Are neck flexion, neck rotation, and sitting at work risk factors for neck pain? Results of a prospective cohort study. Occupational and Environmental Medicine. 2001;58(3):200–207. doi: 10.1136/oem.58.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harris C, Straker L. Survey of physical ergonomics issues associated with school children’s use of laptop computers. International Journal of Industrial Ergonomics. 2000;26(3):337–346. doi: 10.1016/S0169-8141(00)00009-3. [DOI] [Google Scholar]
- 59.Ramos EMA, James CA, Bear-Lehman J. Children’s computer usage: Are they at risk of developing repetitive strain injury? Work. 2005;25:143–154. [PubMed] [Google Scholar]
- 60.Enwemeka CS, Bonet IM, Ingle JA, Prudhithumrong S, Ogbahon FE, Gbenedio NA. Postural correction in persons with neck pain. Part II: Integrated electromyography of the upper trapezius in three simulated neck positions. Journal of Orthopaedic & Sports Physical Therapy. 1986;8(5):240–242. doi: 10.2519/jospt.1986.8.5.240. [DOI] [PubMed] [Google Scholar]
- 61.Portney LG, Watkins MP. (2009). Foundations of clinical research applications of practice. 2nd edn. Prentice Hall Health, p. 277–80.
- 62.Aggarwal A, Shete SV, Palekar TJ. Efficacy of suboccipital and sternocleidomastoid release technique in forward head posture patients with neck pain: A randomized control trial. International Journal of Physiotherapy. 2018;5(4):149–155. doi: 10.15621/ijphy/2018/v5i4/175697. [DOI] [Google Scholar]
- 63.Kim B-B, Lee J-H, Jeong H-J, Cynn H-S. Effects of suboccipital release with craniocervical flexion exercise on craniocervical alignment and extrinsic cervical muscle activity in subjects with forward head posture. Journal of Electromyography and Kinesiology. 2016;30:31–37. doi: 10.1016/j.jelekin.2016.05.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.