Abstract
Collision tumor of the appendix is an extremely rare entity, defined as the coexistence of two independent tumors located in the same site without transitional changes. We describe in this report the case of a 75-year-old man who presented with an acute abdominal pain, nausea and vomiting. Physical examination revealed an abdominal distension with a hypogastric mass. Abdominal computed tomography showed colonic obstruction related to a sigmoid tumor. Therefore, a total colectomy was made. Macroscopic specimen examination showed a sigmoid tumor associated to a cystic dilatation of the appendix tip with mucoid content. Histological examination of the appendix showed the co-existence of two independent tumors located in the tip, without transitional changes: pTis low-grade appendiceal mucinous neoplasia and grade 1 neuroendocrine tumor. The latter was discovered incidentally during histological examination. We draw attention through our presentation to the importance of a thorough macroscopic and histological examination of the appendix.
Keywords: Appendiceal neoplasm, collision tumor, low-grade appendiceal mucinous neoplasia, neuroendocrine tumor, case report
Introduction
Primary tumors of the appendix are infrequent representing 1-2% of appendectomies [1,2]. Low-grade appendiceal mucinous neoplasia (LAMN) and well differentiated neuroendocrine tumor (NET) are the most common lesions and are incidentally found in 0.6% and 0.3-0.9% of appendectomy specimens respectively [1,3]. Collision tumors of the appendix are extremely rare, defined as the coexistence of two independent tumors located in the same site without transitional changes, giving rise to difficulties in pathologic diagnosis, therapeutic management and prediction of prognosis [4]. Therefore, we present a case of a 75-year-old man who was diagnosed with tumor of the sigmoid and in whom a collision tumor of the appendix of a low-grade mucinous neoplasm and a well differentiated neuroendocrine tumor was incidentally discovered.
Patient and observation
Patient information: a 75-year-old man without significant pathological history presented at the emergency room with a sudden onset of an acute abdominal pain, nausea and vomiting.
Clinical findings: physical examination revealed an abdominal distension with a painful hypogastric mass.
Timeline of current episode: May 2021: the patient presented at the emergency room of our institution for abdominal pain associated with nausea and vomiting. Therefore, abdominal computed tomography (CT) scan was made in urgency and the patient was referred to the operating room.
Diagnostic assessment: computed tomography scan of the abdomen showed colonic occlusion related to a sigmoid tumor. Therefore, a total colectomy was made.
Diagnosis: macroscopic specimen examination objectified a stenosing tumor of the sigmoid, measuring 6cm and located 11cm from the colonic resection margin. We also noted a cystic dilatation of the appendix tip with mucoid content, which extends over 1.5cm. Elsewhere, the appendix was of conserved morphology. Therefore, the appendix was included in its entirety. The sigmoid tumor corresponded to an invasive low-grade adenocarcinoma which invaded through the serosa. Lympho-vascular space invasion was present and there was no lymph node metastasis. Appendix examination objectified the co-existence of two independent tumors located in the tip, without transitional changes: the first tumor consisted of a LAMN classified as pTis (Figure 1). The second tumor corresponded to a well differentiated, grade 1 NET measuring 0.3cm and it was incidentally found on histological examination. Resection margins were clear. There was no regional lymph node involvement and no mesoappendiceal invasion. The NET tumor cells displayed granular cytoplasmic positivity to chromogranin A and synaptophysin (Figure 2, Figure 3). The Ki-67 was less than 1% with no mitosis.
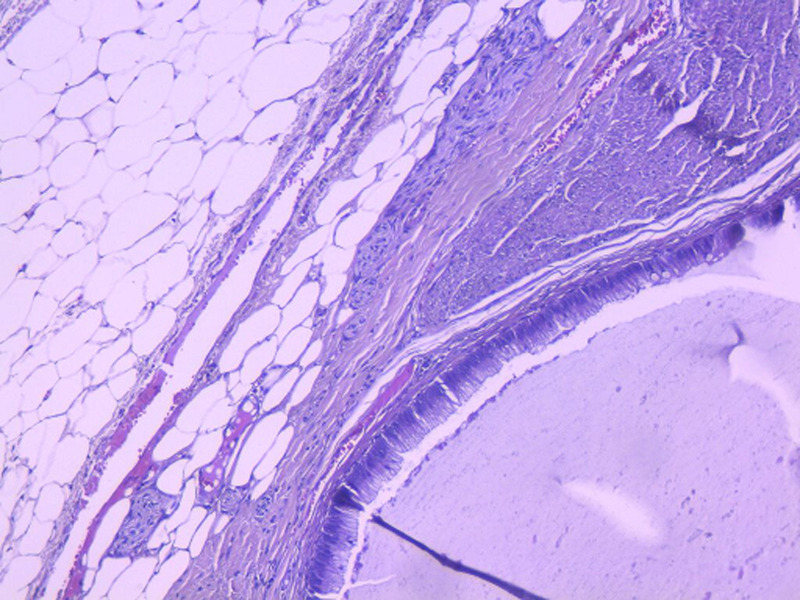
Figure 1.
low-grade appendiceal mucinous neoplasia: cystic dilatation of the appendix tip lined by a well differentiated mucinous epithelium with flat and tubulous architecture associated with atrophy of the lymphoid tissue; the muscularis propria and the subserosa tissue were not infiltrated (HEx20)
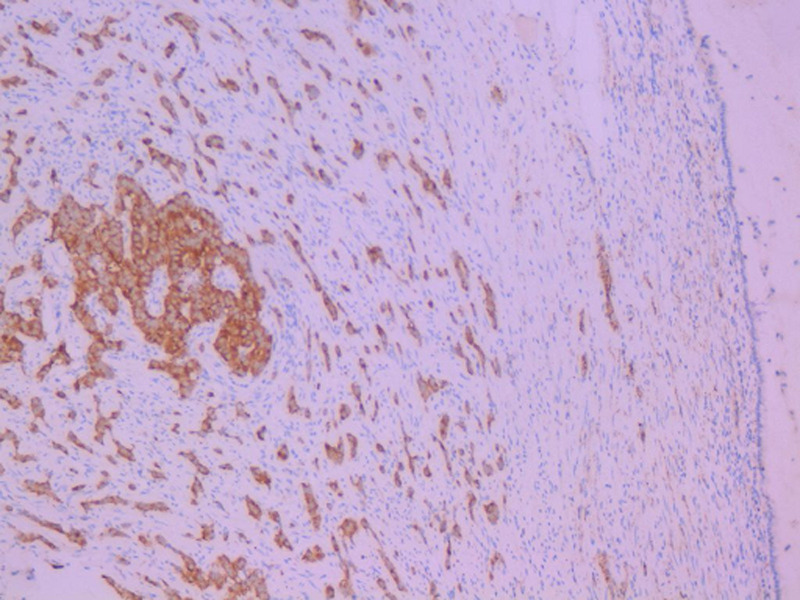
Figure 2.
neuroendocrine tumor: granular cytoplasmic positivity to chromogranin (immunohistochemistry, x20)
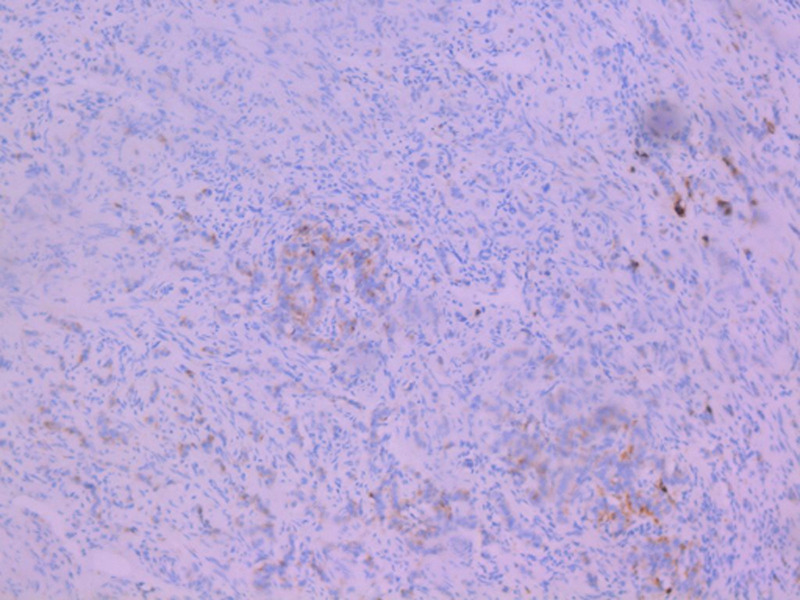
Figure 3.
neuroendocrine tumor: granular cytoplasmic positivity to synaptophysin (immunohistochemistry, x20)
Therapeutic interventions: total colectomy.
Follow-up and outcome of interventions: the postoperative course was regular and the patient was discharged in good condition on the next postoperative day. The patient was then referred to the oncology department for possible adjuvant treatment.
Patient perspective: “I will continue with the adjuvant treatment in order to cure of the cancer”.
Informed consent: the patient expressed his absolute and informed consent.
Discussion
Appendiceal tumors are uncommon entities accounting for 1-2% of all appendectomy specimens. They are usually found incidentally during appendectomy for appendicitis. Their clinical presentation is similar to acute appendicitis making the pre-operative diagnosis of appendiceal neoplasm challenging [1,2]. Collision tumor of the appendix is a rare entity defined as the coexistence of two independent neoplasms of biclonal origins, located in the same site without transitional changes [4]. Our review of the literature found a few published cases of appendiceal collision tumors involving LAMN and NET [1,4-8] summarized in Table 1.
Table 1.
cases of collision tumor low-grade appendiceal mucinous neoplasia (LAMN) and neuroendocrine tumor (NET)
| Author and year | Age (years) | Presentation | Histology | Treatment |
|---|---|---|---|---|
| Singh et al. (2011) | 52 | Abdominal discomfort + weight loss + pain and mass of the iliac fossa | Mucinous adenocarcinoma + NET | Right hemicolectomy + chemotherapy + excision of the omental deposit |
| Ekinci et al. (2018) | 60 | Abdominal discomfort + frequent pain in the right lower quadrant | LAMN + grade 1 NET | Appendectomy; NB: right hemicolectomy indicated but refused by the patient |
| Sholi et al. (2019) | 23 | Right lower quadrant pain + chronic constipation | LAMN + NET | Right hemicolectomy |
| Sugarbaker et al. (2020) | 39 | Lower quadrant and right-side pain | Ruptured LAMN + grade 1 NET | Right hemicolectomy + HIPEC |
| 32 | Mucin discovered during inguinal hernia repair | Ruptured LAMN + grade 2 NET | Right hemicolectomy + omentectomy + cholecystectomy + HIPEC | |
| Ruiz et al. (2021) | 54 | Acute appendicitis | LAMN + NET | Appendectomy |
| Villa et al. (2021) | 31 | Abdominal pain and dysuria | LAMN + grade 1 NET | Right hemicolectomy |
LAMN: low grade appendiceal mucinous neoplasia; NET: neuroendocrine tumor; HIPEC: hyperthermic intraperitoneal chemotherapy
Singh et al. reported in 2011 a case of collision tumor of the appendix composed of an aggressive mucinous adenocarcinoma, with omental deposit and metastasis to the regional lymph nodes at the time of presentation, and a well differentiated NET [4]. Another case was described by Ruiz et al. in 2021; however, in this case the mucinous adenocarcinoma was confined to the appendix [8]. In our presentation, the patient was diagnosed with adenocarcinoma of the sigmoid; collision tumor of LAMN and NET was incidentally found in the appendix tip. A comparable case to our presentation was reported by Meeks et al. in 2016 describing a case of a 95-year-old woman with synchronous quadruple primary neoplasm. She was diagnosed with adenocarcinoma of the right colon, collision tumor of NET and Schwann cell hamartoma in the appendix and sessile serrated adenoma of the appendix. The collision tumor was discovered in the histological examination [9].
LAMNs are uncommon in the appendix, accounting for 0.6% of all appendiceal lesions. They can present as appendicitis, mucocele or as pseudomyxoma peritonei. LAMNs usually have a good prognosis if confined to the appendix. NETs are the most frequent tumors of the appendix and are found in 0.3-0.9% of appendectomy specimens with small predominance in female patients. Patients mostly present with appendicitis, carcinoid syndrome is rarely observed. NET rarely metastasize and they usually have an excellent prognosis [1,3].
The management of the appendiceal collision tumors remains a matter of debate. For LAMN, the assessment depends on the grade of atypia, lymph node involvement and peritoneal extension. Simple appendectomy is a sufficient treatment for LAMN, even when ruptured. However, this condition may cause recurrence by the development of pseudomyxoma peritonei. Thus, surgical debulking or post-operative intraperitoneal chemotherapy would be necessary [1-3]. The treatment of NETs is determined by tumor size and mitotic activity. For well differentiated NET < 1cm, appendectomy is usually curative. Right hemicolectomy should be indicated in all these cases: lesions > 2cm, lymph node involvement, high mitotic activity, mesoappendix spread and positive margins [3]. Surgical approach to LAMN and NET remains controversial. In fact, a recent studies conducted by Lamberti et al. and Gonzalez et al. found that there is no improved survival rates following right hemicolectomy compared with those following appendectomy [10,11].
Conclusion
In the present case, LAMN was diagnosed during macroscopic examination of the appendix and NET was discovered incidentally on histological examination. Therefore, we conclude that appropriate preoperative and postoperative examination of the appendix is the key to the diagnosis of appendiceal tumor.
Footnotes
Cite this article: Syrine Moussa et al. Collision tumor of the appendix incidentally discovered in a patient diagnosed with an adenocarcinoma of the colon: a case report. Pan African Medical Journal. 2022;43(161). 10.11604/pamj.2022.43.161.33298
Competing interests
The authors declare no competing interests.
Authors' contributions
All authors listed have significantly contributed to the investigation, development and writing of this article. Manuscript drafting: Syrine Moussa. Data collection: Salwa Nechi and Abir Chaabane. Manuscript revision: Karim Mfarrej, Amel Dougaz and Emna Chelbi. Patient management: Slim Zribi, Mehdi Bouassida and Hassen Touinsi. All authors have read and approved the final version of the manuscript.
References
- 1.Villa M, Sforza D, Siragusa L, Guida AM, Ciancio Manuelli M, Pirozzi BM, et al. A Low-Grade Appendiceal Mucinous Neoplasia and Neuroendocrine Appendiceal Collision Tumor: A Case Report and Review of the Literature. Am J Case Rep. 2021 Feb 23;22:e927876. doi: 10.12659/AJCR.927876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baena-del-Valle J, Palau-Lázaro M, Mejía-Arango M, Otero J, Londoño-Schimmer E, Cortes N, et al. Well differentiated neuroendocrine tumor of the appendix and low-grade appendiceal mucinous neoplasm presenting as a collision tumor. Rev Esp Enferm Dig. 2015 Jun;107(6):396–8. [PubMed] [Google Scholar]
- 3.Dellaportas D, Vlahos N, Polymeneas G, Gkiokas G, Dastamani C, Carvounis E, et al. Collision tumor of the appendix: mucinous cystadenoma and carcinoid. A case report. Chirurgia (Bucur) 2014 Nov-Dec;109(6):843–5. [PubMed] [Google Scholar]
- 4.Singh NG, Mannan AA, Kahvic M, Nur AM. Mixed adenocarcinoma-carcinoid (collision tumor) of the appendix. Med Princ Pract. 2011;20(4):384–6. doi: 10.1159/000324870. [DOI] [PubMed] [Google Scholar]
- 5.Ekinci N, Gün E, Avci A, Er A. Coexistence of low-grade mucinous neoplasm and carcinoid (collision tumor) within multiple appendiceal diverticula: A case report. Turk J Surg. 2018 Aug 31;:1–3. doi: 10.5152/turkjsurg.2018.3877. [DOI] [PubMed] [Google Scholar]
- 6.Sholi AN, Gray KD, Pomp A. Pomp, Management and outcome of an appendiceal collision tumour composed of neuroendocrine and mucinous neoplasms. BMJ Case Rep. 2019 Jul 10;12(7):e229414. doi: 10.1136/bcr-2019-229414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sugarbaker PH, Ben-Yaacov A, Hazzan D, Nissan A. Synchronous primary neuroendocrine and mucinous epithelial tumors present in the same appendix. Case report of 2 patients. Int J Surg Case Rep. 2020;67:76–79. doi: 10.1016/j.ijscr.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruiz SG, Geraghty F, Padron D, Chacon D, Kahane G. The Appendix: A Rare Case of an Appendiceal Collision Tumor. Cureus. 2021;13(8):e17050. doi: 10.7759/cureus.17050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meeks MW, Grace S, Chen Y, Petterchak J, Bolesta E, Zhou Y, et al. Synchronous Quadruple Primary Neoplasms: Colon Adenocarcinoma, Collision Tumor of Neuroendocrine Tumor and Schwann Cell Hamartoma and Sessile Serrated Adenoma of the Appendix. Anticancer Res. 2016 Aug;36(8):4307–11. [PubMed] [Google Scholar]
- 10.Lamberti G, Brighi N, Campana D. Comment on. “Current Management and Predictive Factors of Lymph Node Metastasis of Appendix Neuroendocrine Tumors": A National Study From the French Group of Endocrine Tumors (GTE) Ann Surg. 2019 Aug;270(2):e43–e44. doi: 10.1097/SLA.0000000000003077. [DOI] [PubMed] [Google Scholar]
- 11.González-Moreno S, Sugarbaker PH. Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg. 2004 Mar;91(3):304–11. doi: 10.1002/bjs.4393. [DOI] [PubMed] [Google Scholar]