Abstract
The commonest sites for liposarcoma are the retroperitoneum and lower extremities. Liposarcoma of the head and neck region is a rare and potentially life-threatening malignancy. Tumors originating in the right cervical space cause special diagnostic and therapeutic difficulties. In the present report, we describe a case of differentiated liposarcoma of the right cervical region. The tumor continued to grow slowly over 3 years before a definitive diagnosis was established. Extended extirpation of the tumor was performed and proved efficacious in that no recurrence has been observed for 4 years. Recommendations for earlier and accurate diagnosis and treatment of this rare neoplasm are discussed.
Keywords: Cervical liposarcoma, Murine double minute 2, Cyclin-dependent kinase 4
Introduction
Liposarcoma accounts for approximately 15% of all soft tissue neoplasms [1]. The most common sites for liposarcoma are the retroperitoneum and lower extremities, with their prevalence in the head and neck region representing only 2–9% of all malignant mesenchymal tumors [1, 2]. The commonest symptoms of cervical liposarcoma are those of a painless enlarging mass. This type of tumor presents clinically as a firm mass relatively fixed to the surrounding tissues, showing relatively progressive growth. In general, patients do not have lymph node or distant metastases at the time of diagnosis. Most lesions are clinically diagnosed as benign [3]. We present a case of differentiated liposarcoma of the right cervical region in a 20-year-old woman. The tumor grew slowly over a 3-year period before a definitive diagnosis was established. Diagnostic and therapeutic options are discussed below.
Case Presentation
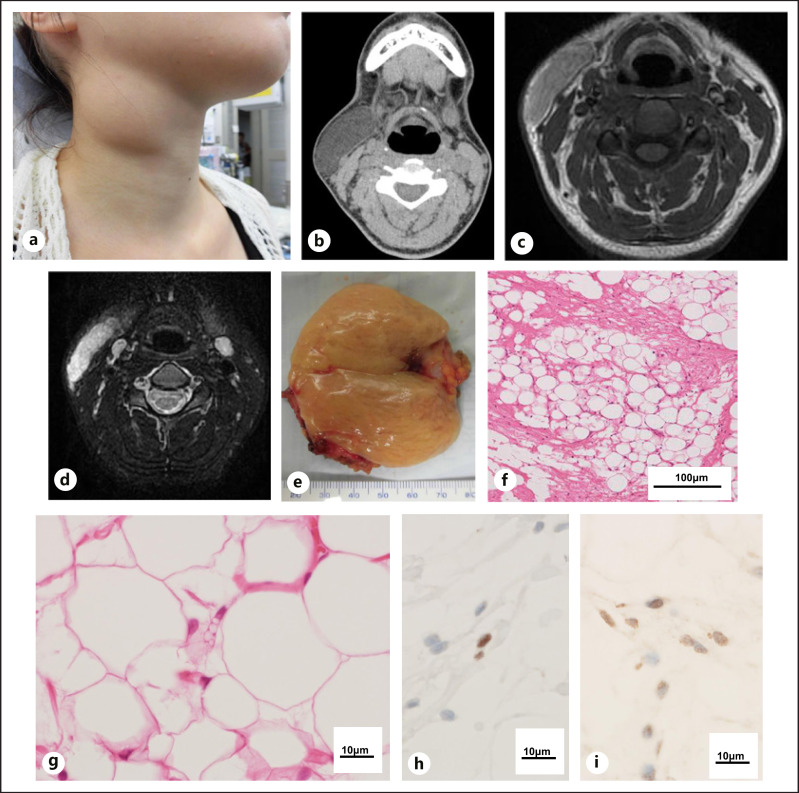
A 20-year-old woman visited our department with the chief complaint of a swelling on the right side of the cervical region, which she had noted for 3 years. The upper cervical tumor had been noticed by her family recently. On clinical examination, the patient's neck appeared asymmetric and exhibited a well-circumscribed enlargement of the right cervical region (Fig. 1a). The swelling appeared soft and was estimated to be 6 cm in diameter and to extend close to the sternocleidomastoid muscle (Fig. 1b). Preoperative magnetic resonance imaging (MRI) showed a well-circumscribed mass between the cervical skin and platysma muscle (Fig. 1c, d). The mass revealed high signal intensity, with a slightly higher signal-intensity center in T1-weighted and high signal-intensity center in T2-weighted MRI (Fig. 1c, d). There were no enlarged neck or axillary lymph nodes. General physical examination was normal. Fine needle aspiration biopsy indicated the lesion to be a lipoma. On the basis of its clinical features, the tumor was also diagnosed as a lipoma.
Fig. 1.
aPhotograph taken before surgery, demonstrating swelling of the right cervical region, with normal overlying skin (6 cm × 5.5 cm). bPreoperative axial contrast-enhanced computed tomography, showing a well-defined, slightly enhanced, nonhomogeneous soft-tissue-density mass, separate from the sternocleidomastoid muscle and located under the skin. CT revealed the center of the mass to have a different density from that of its margin. cPreoperative axial T1-weighted magnetic resonance image showing a well-circumscribed mass between the sternocleidomastoid and the cervical skin. MRI showed the center of the mass to have a different density, as shown by signal intensity, than its margin. dPreoperative axial T2-weighted, fat-suppressed MRI showing an intermediate to high signal-density mass situated laterally from the sternocleidomastoid muscle. eSurgical specimen showing a smooth, lobulated tumor mass with skin (7 × 6.2 × 4.9 cm). f, gHistologic section showing the tumor to be predominantly composed of spindle cells, many of which were large and darkly stained and exhibited pleomorphic nuclei (HE, original magnification, ×200). Immunohistochemical stating was positive for murine double minute 2 (MDM2) (h) and cyclin-dependent kinase 4 (CDK4) (i) in many atypical tumor cells.
In case of malignancy, the patient underwent extended extirpation of the tumor with overlying skin for definitive diagnosis; lipoma was suspected in the intraoperative pathological examination. The lesion was yellow-tan in color and close to the platysma muscle, but had not adhered to the muscle, and was extirpated without difficulty. Wound closure and healing were uneventful. The specimen was submitted for further histologic diagnosis.
Macroscopically, the excised specimen consisted of a nodular, apparently encapsulated mass with a lobulated surface (Fig. 1e). Microscopically, the tumor was predominantly composed of stellate (spindle) cells, many of which were large, darkly stained, and exhibited pleomorphic nuclei. Contrary to our expectations, numerous multivacuolated atypical lipoblasts were also observed in surgical specimen (Fig. 1f, g). For definitive diagnosis, immunohistochemical stating was conducted and positive for murine double minute 2 (MDM2) (Fig. 1h) and cyclin-dependent kinase 4 (CDK4) (Fig. 1i) in many atypical tumor cells. A diagnosis of differentiated liposarcoma was finally made according to the Federation Nationale des Centres de Lutte Contre le Cancer (FNCLCC) system.
The postoperative course was satisfactory, and the patient is well, with no evidence of tumor 48 months after the initial treatment. This study was approved by the Institutional Review Board (Tohoku Medical and Pharmaceutical University 2021-4-069).
Discussion/Conclusion
The biological behavior of liposarcoma of the head and neck is closely correlated to its histologic type. The histologic type of liposarcoma is divided into atypical lipomatous, tumor/well-differentiated liposarcoma, myxoid liposarcoma, pleomorphic liposarcoma, and de-differentiated liposarcoma. Well-differentiated liposarcoma is the most common entity and accounts for 30–40% of liposarcomas. The histologic classification has prognostic significance in that clinical behavior tends to be correlated with degree of cellular differentiation. Well-differentiated liposarcoma is locally aggressive and may recur if excision is not complete, but it shows a very low tendency to metastasis. It is now well established that atypical lipomatous tumor/well-differentiated liposarcoma and de-differentiated liposarcomas are characterized cytogenetically by MDM2 and CDK4 amplification [3]. The search for MDM2 and CDK4 expression by immunohistochemistry and the amplification of these two genes by FISH are thus essential tools for this diagnosis [3, 4]. In present case, the expression of MDM 2 and CDK4 was upregulated in many atypical tumor cells, and these findings might help for diagnosis of the liposarcoma.
Imaging modalities including ultrasound, CT scan, and MRI are essential for observing the size, localization, adipocytic nature, extension to the surrounding tissues, and its relationship with the neurovascular structures, as well as for the detection of metastases [4, 5]. The presence of a thickened septum of >2 mm, nodular, and/or globular areas of nonadipose tissue within the lesion or associated with the mass, and a total amount of nonadipose tissue comprising more than 25% of the lesion are characteristic features that can distinguish liposarcoma from lipoma [5, 6, 7]. These results suggest the advisability of suspecting liposarcoma if CT and MRI reveal proliferative adipose lesions that contain myxomatous tissue with increased vascularity that are not seen with benign lipoma [3].
Despite its proximity to key structures of the head and neck, the first choice of treatment is complete surgical removal. The main mass of the tumor is often surrounded by satellite nodes. For this reason, complete surgical dissection is suggested, since multiple recurrences may result from failure to remove all of the primary tumor. However, metastases from low-grade liposarcomas, including well-differentiated and myxoid types, are very rare [3, 7, 8]. Radiotherapy is not employed as a preferred treatment, but it has been used after surgery either for myxoid liposarcomas, which tend to be more radiosensitive, or for inoperable tumors. However, postoperative radiation can be useful and may prevent local recurrence. Indication of postoperative radiotherapy might be justified in cases with high-grade tumors, absence of safety margins, large tumors, aggressive extension, and complex anatomic subsites. Two cases of liposarcoma treated with carbon ion radiotherapy have been reported [8]. In suitable cases with inoperable or recurrent disease, management can be challenging and carbon ion radiotherapy might be considered. In the present case, the histopathological diagnosis was well-differentiated liposarcoma, so postoperative radiotherapy to prevent future radiation-induced cancer(s) was not performed.
Chemotherapy is used mainly in metastatic diseases, but in a few cases it has been employed as an adjunct to radiotherapy. It is still controversial as to whether or not chemotherapy for liposarcoma is effective [9, 10, 11, 12]. The chemotherapy landscape for de-differentiated liposarcoma has notably expanded in recent years. Recent clinical studies have confirmed the benefits of the CDK4 inhibitor abemaciclib and the nuclear export inhibitor selinexor, and support the continued development of anti-MDM2 therapies [9]. Investigation of synergistic combinations of novel agents such as the checkpoint inhibitors pembrolizumab and nivolumab and other therapeutic agents is ongoing for the management of liposarcoma [13, 14].
However, the usefulness of chemotherapy or radiotherapy to treat liposarcoma remains controversial. The histological grade, tumor size, localization, and metastasis to regional lymph nodes and distant organs are important prognostic factors. Prognosis also depends on the choice of treatment modality: patients receiving radiotherapy only have significantly less successful outcomes than patients who undergo surgery or surgical resection plus adjuvant radiotherapy [9, 10, 11, 12].
An extremely rare case of liposarcoma of the cervical region is presented. Liposarcoma usually exhibits very slow growth and can easily be misdiagnosed as a benign lesion. Any proliferative lesions of the adipose nature containing myxomatous tissue with increased vascularity should be carefully examined, and liposarcoma should be kept in mind when making a differential diagnosis.
Statement of Ethics
The subject of this case report has given the written informed consent to publish this case including publication of images. This study was approved by the Institutional Review Board of Tohoku Medical and Pharmaceutical University, approval number [2021-4-069].
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
The authors received no funding for this case report.
Author Contributions
Takahiro Suzuki and Nobuo Ohta, diagnosis and therapy, and composition of this case report; Shion Shirane, Naoya Noguchi, Teruyuki Sato, and Nanako Ansai, therapy; Kazue Ise, Keigo Murakami, Kazuhiro Murakami, and Yasuhiro Nakamura, pathological diagnosis and immunohistochemical examinations.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Acknowledgments
There are no other substantive contributions.
Funding Statement
The authors received no funding for this case report.
References
- 1.Gerry D, Fox NF, Spruill LS, Lentsch EJ. Liposarcoma of the head and neck: analysis of 318 cases with comparison to non-head and neck sites. Head Neck. 2014;36((3)):393–400. doi: 10.1002/hed.23311. [DOI] [PubMed] [Google Scholar]
- 2.Waters R, Horvai A, Greipp P, John I, Demicco EG, Dickson BC, et al. Atypical lipomatous tumour/well-differentiated liposarcoma and de-differentiated liposarcoma in patients aged ≤ 40 years: a study of 116 patients. Histopathology. 2019;75((6)):833–842. doi: 10.1111/his.13957. [DOI] [PubMed] [Google Scholar]
- 3.Barisella M, Giannini L, Piazza C. From head and neck lipoma to liposarcoma: a wide spectrum of differential diagnoses and their therapeutic implications. Curr Opin Otolaryngol Head Neck Surg. 2020;28((2)):136–143. doi: 10.1097/MOO.0000000000000608. [DOI] [PubMed] [Google Scholar]
- 4.Ohta N, Watanabe T, Abe Y, Onoe Y, Ishida A, Aoyagi M. Differentiated posterior cervical liposarcoma with carcinoid: report of a case. Auris Nasus Larynx. 2011;38((3)):421–425. doi: 10.1016/j.anl.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Thway K. Well-differentiated liposarcoma and dedifferentiated liposarcoma: An updated review. Semin Diagn Pathol. 2019;36((2)):112–121. doi: 10.1053/j.semdp.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Fritchie K, Ghosh T, Graham RP, Roden AC, Schembri-Wismayer D, Folpe A, et al. Well-differentiated/dedifferentiated liposarcoma arising in the upper aerodigestive tract: 8 cases mimicking non-adipocytic lesions. Head Neck Pathol. 2020;14((4)):974–981. doi: 10.1007/s12105-020-01171-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pontes FSC, de Souza LL, Vulcão ÉNC, de Abreu MC, Menezes SN, Rezende D, et al. Liposarcoma of oral cavity: systematic review of cases reported to date and analysis of prognostic factors. Head Neck. 2020;42((9)):2626–2634. doi: 10.1002/hed.26160. [DOI] [PubMed] [Google Scholar]
- 8.Vitolo V, Barcellini A, Fossati P, Fiore MR, Vischioni B, Iannalfi A, et al. Carbon ion radiotherapy in the management of unusual liposarcomas: a case report. Vivo. 2019;33((2)):529–533. doi: 10.21873/invivo.11506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gahvari Z, Parkes A. Dedifferentiated liposarcoma: systemic therapy options. Curr Treat Options Oncol. 2020;21((2)):15. doi: 10.1007/s11864-020-0705-7. [DOI] [PubMed] [Google Scholar]
- 10.Rizzo A, Pantaleo MA, Saponara M, Nannini M. Current status of the adjuvant therapy in uterine sarcoma: a literature review. World J Clin Cases. 2019;267((14)):1753–1763. doi: 10.12998/wjcc.v7.i14.1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Astolfi A, Nannini M, Indio V, Schipani A, Rizzo A, Perrone AM, et al. Genomic database analysis of uterine leiomyosarcoma mutational profile. Cancers. 2020;12((8)):2126. doi: 10.3390/cancers12082126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rizzo A, Nannini M, Astolfi A, Indio V, De Iaco P, Perrone AM, et al. Impact of chemotherapy in the adjuvant setting of early stage uterine leiomyosarcoma: a systematic review and updated meta-analysis. Cancers. 2020;12((7)):1899. doi: 10.3390/cancers12071899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou M, Bui N, Lohman M, van de Rjin M, Hwang G, Ganjoo K. Long-term remission with ipilimumab/nivolumab in two patients with different soft tissue sarcoma subtypes and no PD-L1 expression. Case Rep Oncol. 2021;14((1)):459–465. doi: 10.1159/000512828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roulleaux Dugage M, Nassif EF, Italiano A, Bahleda R. Improving immunotherapy efficacy in soft-tissue sarcomas: a biomarker driven and histotype tailored review. Front Immunol. 2021;12:775761. doi: 10.3389/fimmu.2021.775761. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.