Abstract
Introduction
Heart failure is a rapidly growing public health problem and has become a major cause of hospitalization in middle-aged and older adults. Biomarkers are clinically important in managing heart failure and have attracted more attention from researchers in recent years. This study aimed to evaluate the global research of heart failure biomarkers by bibliometrics and to identify the hot spots and perspectives for further advancement.
Methods
Selection of relevant documents was from the Web of Science Core Collection. Microsoft Excel, VOSviewer, SciMA, and CiteSpace software were used for bibliometric analysis.
Results
As of October 29, 2021, 5,978 documents for heart failure biomarkers have been identified from 1989 to 2021. European Journal of Heart Failure and Circulation respectively ranked first in terms of the number of publications and the number of co-citations. A total of 5,698 institutions from 90 countries participated in these publications, with the USA leading with 2,045 documents. The most productive institution was Harvard University. Januzzi, J.L. and Maisel, A.S. were the most productive and most cited authors respectively. Natriuretic peptide, copeptin, valsartan, ferric carboxymaltose, empagliflozin, preserved ejection fraction, myocardial fibrosis, and heart transplantation were hot themes.
Conclusions
Extensive national and inter-institutional collaboration should be enhanced to bridge the gap between developed and less developed countries in heart failure biomarkers research. The research in this field seems to have reached a relatively mature stage, with a decrease in research fervor in recent years. The study of the natriuretic peptide family still has high centrality, with advances in the study of expression products and inflammatory markers. Cardiac fibrosis, cardiac remodeling, and therapies regarding heart failure have become hot spots.
Keywords: Heart failure, Biomarker, Bibliometric analysis, Science mapping, Citation analysis
1. Introduction
Heart failure (HF) is a fast-growing public health challenge, affecting about 40 million people worldwide and becoming the main cause of hospitalization among middle-aged and elderly people [1,2]. The American College of Cardiology Foundation (ACCF) and American Heart Association (AHA) define HF as " a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood” [3]. The poor prognosis of HF increases morbidity and mortality, placing a huge burden on the healthcare system. A study published in 2014 estimated global spending on HF at $108 billion in 2012, 60% of which went directly to healthcare costs [4]. Between 2012 and 2030, HF is expected to increase in prevalence by 46% in the USA, and total healthcare costs are projected to increase from $20.9 billion to $53.1 billion [5].
The diagnosis of HF is very important in the management of HF, and great progress has been made in recent years. Traditional physician clinical assessment is based on medical history and physical examination [6], yet due to the non-specific nature of HF symptoms, this diagnostic method is limited in its accuracy [7]. More advanced diagnostic methods are cardiovascular imaging or invasive hemodynamic cannulation, but there are limitations. On the one hand, the measurement level is not consistent with the real situation [8]; on the other hand, due to its expensive, time-consuming, and invasive nature, its role in routine HF diagnosis and monitoring is limited [9]. In recent years, biomarkers with their diagnostic sensitivity, specificity, and ease of implementation have played an important role in predicting future HF incidence, stratifying the risk of HF patients, and possibly serving as biological tools to guide HF treatment. As the understanding of the pathophysiology of HF has been expanded from a simple hemodynamic model to a more complex multi-system syndrome, the combination of candidate molecules has expanded as well [10]. In addition, a large number of potential biomarkers have been proposed in recent years with the formal introduction and use of the concept of biomarkers. However, a comprehensive and visualized analysis of the evolution and trends for HF biomarkers is still lacking.
Bibliometric analysis aims to evaluate the current situation and trends in specific research areas through a visible approach, thus providing research directions [11,12]. This study analyzed the research status and frontiers of HF biomarkers through bibliometric analysis of related documents and predicted the future research trend. At the same time, this research could help supporters and policymakers allocate resources and help researchers set research directions and partners.
2. Methods
2.1. Literature search
Our search experts have developed a selective and well-rounded search strategy combined with Boolean logical operators to complete the literature retrieval on Web of Science (WoS) on October 29, 2021, to avoid deviations from database updates. The search strategy was developed by the search experts around the keywords of “HF” and “biomarker”, as detailed in Table 1. There was no limitation of time and language, and the literature source was limited to Science Citation Index Expanded (SCI-EXPANDED) of Web of Science Core Collection (WoSCC) to preliminarily control the quality of documents.
Table 1.
Search strategy for heart failure biomarkers.
| Set | Search |
|---|---|
| #1 | TS= ((heart* or cardiac* or myocard*) near/2 (fail* or insuff*)) |
| #2 | TS= (heart* near/2 decomp*) |
| #3 | TS= (biomarker OR “biologic marker” OR “biological marker” OR “serum marker” OR “clinical marker” OR “biochemical marker” OR “Immune marker” OR “molecule marker” OR biomarkers OR “biologic markers” OR “biological markers” OR “serum markers” OR “clinical markers” OR “biochemical markers” OR “immune markers” OR “molecule markers") |
| #4 | #1 OR #2 |
| #5 | #3 AND #4 |
2.2. Literature selection and data collection
Retrieved records were output to EndNote X8 for further analysis. Two researchers screened the literature independently by scanning the titles and abstracts, and if necessary, reading the full text. After the primary screening, the two researchers checked each other, discussed suspicious literature, and if necessary, the third researcher involved in solving discrepancies to reach a consensus on the inclusion of the suspicious literature. So that all literature on HF biomarkers was included as much as possible. The types of publications were limited to articles and reviews, excluding other types such as meeting abstracts, letters, and editorials.
The following data were extracted for further analysis: year, country, institution, author, journal, and impact factor (IF, from Journal Citation Reports 2020 released by Clarivate Analytics), co-cited citations, co-cited authors, co-cited journals and keywords. In analyzing the data, papers from Scotland, Wales, Northern Ireland, and England were grouped together in the United Kingdom (UK), and papers from Taiwan, Macau, and Hong Kong were grouped together in China [13].
2.3. Bibliometric analysis
Before data analysis, we conducted data cleaning, which mainly manifested as the standardization of different expressions of the same scientific concept. We complemented the proposed data with different computer programs for the bibliometric analysis.
Microsoft Excel 2021 was tooled to create bar chart and analyze trends in publications. A polynomial model (of order 6) was applied to predict the increase in publications.
VOSviewer was developed by Leiden University, The Netherlands, to retrieve and analyze co-occurrence of keywords, co-authorship and co-citation information [14]. We visually analyzed the co-occurrence of authors, institutions, countries, keywords, and co-citations through the network map and hot map produced in VOSviewer 1.6.17.
CiteSpace is an application that progressively visualizes the field of knowledge, revealing the dynamics of the field of study through a visual analysis of trends and patterns [15]. Burst is defined as a character in that documents are cited regularly in a period. Version 5.8. R3 was used to detect co-occurrence items’ bursts. We also used CiteSpace to make a dual-map overlay of journals.
Science Mapping Analysis Software Tool (SciMAT), developed by the University of Granada, is an open resource scientific graphing software [16]. SciMAT 1.1.04 was used to analyze afferent and efferent keywords and to describe the thematic evolution for HF biomarkers. Publications have been divided into four consecutive periods based on the volume of literature: 1989–2005, 2006–2010, 2011–2015, and 2016–2021.
3. Results
3.1. Publications trend forecast
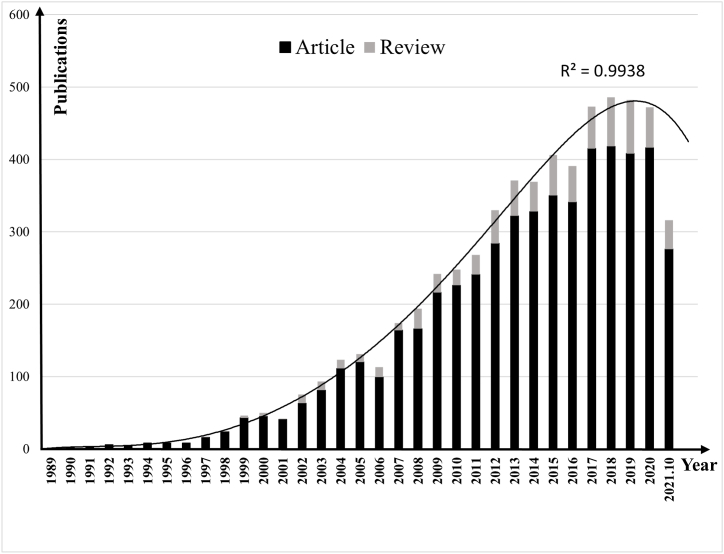
The amount of retrieved records was 10,996, and a total of 5,978 documents were screened for further analysis. Among the 5,978 publications, there were 5,255 original articles (87.91%) and 723 reviews (12.09%), indicating that original articles accounted for a large proportion. Studies on HF biomarkers began to trickle in around the 1990s, with no more than 10 documents published between 1989 and 1996 yet an increasing trend. In 1997, the number of documents published exceeded single digits, with 17. Since entering the 21st century, research in this field has been paid more and more attention, and the quantity of publications has been slowly rising. In 2004, the number of documents published exceeded 100, reaching 123. Since then, the quantity of documents published has exceeded 100 every year, and generally presented a growing trend, exceeding 200 in 2009, 300 in 2012, and 400 in 2015. With increased interest in the diagnosis of HF, the quantity of literature has increased quickly over the past decade, with 4,364 studies (73.00%) from 2011 to November 2021. However, the annual rate of growth of publications in 2021 was significantly negative, and the number of documents had a significant decline. As shown in Fig. 1, the stacked bar chart and polynomial model describe the relationship between publication years and publications. There was a significant correlation (except for 2021) between the amounts of publications and the year, with a high determination factor (R2 = 0.9938). The research in this area can foresee will either reach a peak or reach a bottleneck, and the number of publications will continue to decrease in the coming years.
Fig. 1.
Annual distribution of publications and growth forecast for heart failure biomarkers.
3.2. Analysis of source and co-authorships
829 journals contributed to these 5,978 publications. Among them, European Journal of Heart Failure (N = 311, 5.20%) published the most documents, followed by International Journal of Cardiology (N = 222, 3.71%) and Journal of Cardiac Failure (N = 210, 3.51%). A total of 5,698 institutions from 90 countries contributed to these publications. The USA made the largest contribution, publishing 2,045 documents, accounting for 34.21%, ranking first. And the top three institutions were Harvard University in the USA (N = 238, 3.98%), Duke University in the USA (N = 221, 3.70%), and the University of Groningen in the Netherlands (N = 204, 3.41%). The most influential author was Januzzi, J.L., from Massachusetts General Hospital in the USA, who published 118 documents and were cited 6,966 times, ranking first. Followed by Voors, A.A. (N = 106, 1.77%, Citation = 15,427) and Van Veldhuisen, D.J. (N = 101, 1.69%, Citation = 6,243) from University Medical Center Groningen in the Netherlands. For detailed information on this section see Appendix A.
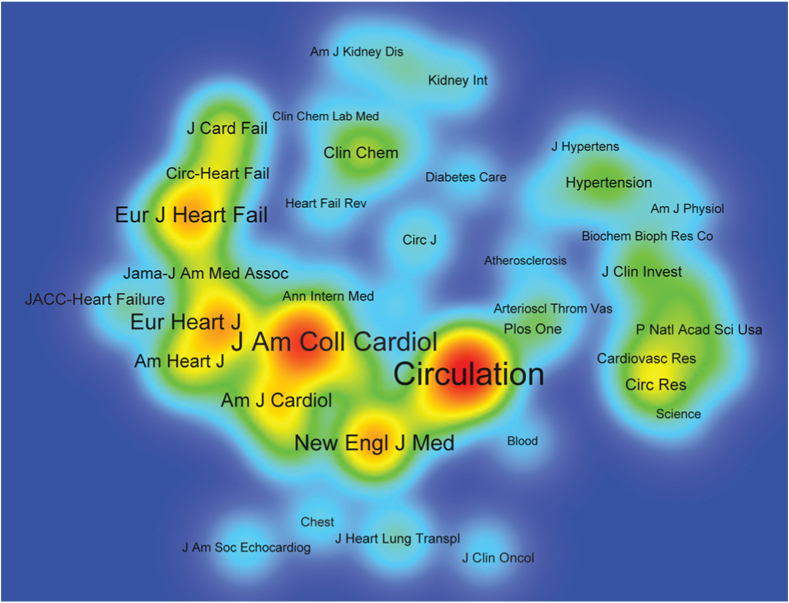
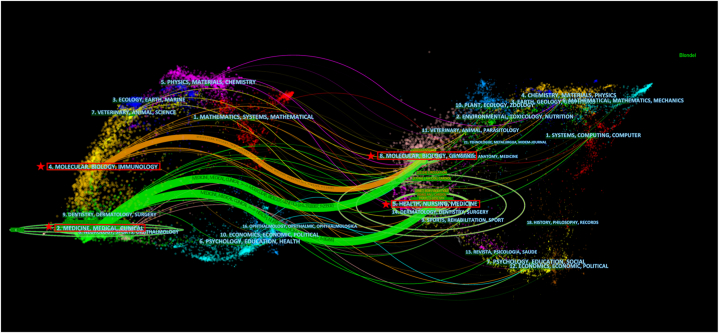
3.3. Analysis of co-citations
A total of 8,285 journals were co-cited. Table 2 lists the top co-cited 10 journals, of whom Circulation was cited 22,156 times, ranking first. Journal of the American College of Cardiology (Citations = 17,758) and New England Journal of Medicine (Citations = 9,431) followed closely behind. Fig. 2 is a hotspot map of co-cited journals, indicating the distribution of 53 highly co-cited journals with at least 600 co-citations. Fig. 3 shows a dual-map overlay of journals. The map on the left indicates cited journals and the map on the right represents co-cited journals. This label represents the subject covered by the journal [17]. The colored curves represent the referential path, starting from the cited journals maps and directing to the co-cited journals maps on the right. The map shows three major citation routes. The green route referred to documents published in health/nursing/medicine, and molecular/biology/genetics mostly cited publications in medicine/medical/clinical. And the orange route referred to documents published in molecular/biology/genetics mostly cited publications in molecular/biology/immunology.
Table 2.
Top 10 co-cited journals for heart failure biomarkers.
| Rank | Journal | Citations | Country | IF |
|---|---|---|---|---|
| 1 | Circulation | 22,156 | USA | 29.690 |
| 2 | Journal of The American College of Cardiology | 17,758 | USA | 24.093 |
| 3 | New England Journal of Medicine | 9,431 | USA | 91.253 |
| 4 | European Heart Journal | 9,195 | UK | 29.983 |
| 5 | European Journal of Heart Failure | 8,986 | Netherlands | 15.534 |
| 6 | American Journal of Cardiology | 6,346 | USA | 2.778 |
| 7 | American Heart Journal | 4,810 | USA | 4.749 |
| 8 | Lancet | 4,208 | UK | 79.323 |
| 9 | Journal of Cardiac Failure | 4,016 | USA | 5.712 |
| 10 | International Journal of Cardiology | 3,656 | Ireland | 4.164 |
Fig. 2.
Density map of co-cited journals for heart failure biomarkers.
Fig. 3.
Dual-map overlay of journals for heart failure biomarkers.
A total of 109,694 documents were cited, of which the top 10 are listed in Table 3, and each document was cited more than 200 times. A document published in European Heart Journal by Ponikowski, P. et al., in 2016 was cited 542 times, ranking first [18]. A document published by Maisel, A.S. et al. in New England Journal of Medicine in 2002 had also been cited more than 400 times [19]. Three documents were cited 300 to 400 times. Citation burst in references refer to document that is frequently referenced during a period. When the citation duration was five, 168 co-cited references were included. In Appendix B2, the blue line indicates the overall time interval, the red line indicates the duration of the burst, and the two ends of the red line indicate the beginning and end of the burst. The first document whose burst lasted for five years was published in 1990 and continued to break out from 1991 to 1995. There were seven documents lasting for six years or more. There were seven documents with an intensity of more than 40.00, among which the highest intensity was published by McMurray, J.J. et al. in European Heart Journal in 2012 [20].
Table 3.
Top 10 co-cited references for heart failure biomarkers.
| Rank | Co-cited reference | Citations |
|---|---|---|
| 1 | Ponikowski P, Voors AA, Anker SD et al., 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37(27): 2129-200. | 542 |
| 2 | Maisel AS, Krishnaswamy P, Nowak RM et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002; 347(3): 161-7. | 428 |
| 3 | Yancy CW, Jessup M, Bozkurt B et al., 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 62(16): e147-239. | 335 |
| 4 | McMurray JJ, Packer M, Desai AS et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 2014; 371(11): 993–1004. | 329 |
| 5 | McMurray JJ, Adamopoulos S, Anker SD et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012; 33(14): 1787-847. | 309 |
| 6 | Januzzi JL, Jr., Camargo CA, Anwaruddin S et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol 2005; 95(8): 948-54. | 246 |
| 7 | Braunwald E. Biomarkers in heart failure. N Engl J Med 2008; 358(20): 2148-59. | 242 |
| 8 | Troughton RW, Frampton CM, Yandle TG, Espiner EA, Nicholls MG, Richards AM. Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations. Lancet 2000; 355(9210): 1126-30. | 233 |
| 9 | Januzzi JL, van Kimmenade R, Lainchbury J et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur Heart J 2006; 27(3): 330-7. | 210 |
| 10 | Dickstein K, Cohen-Solal A, Filippatos G et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008; 29(19): 2388-442. | 200 |
The authors of the cited documents in the paper being analyzed are called co-cited authors. 63,963 authors were cited, and 810 authors were cited more than 35 times. The top 10 co-cited authors are listed in Table 4. Maisel, A.S. from University of California at San Diego (USA), was cited 1,385 times and ranked first by an absolute margin. Followed by Januzzi, J.l. from Massachusetts General Hospital (USA), was cited 1,054 times. Packer, M. (Citations = 832) from Columbia University (USA) and Yancy, C.W. (Citations = 828) from University of Texas South Medical Center (USA) had also been cited more than 800 times.
Table 4.
Top 10 co-cited authors for heart failure biomarkers.
| Rank | Author | Institution | Citations |
|---|---|---|---|
| 1 | Maisel, A.S. | University of California at San Diego (USA) | 1,385 |
| 2 | Januzzi, J.l. | Massachusetts General Hospital (USA) | 1,054 |
| 3 | Packer, M. | Columbia University (USA) | 832 |
| 4 | Yancy, C.W. | University of Texas Southwestern Medical Center (USA) | 828 |
| 5 | Ponikowski, P. | Wroclaw Medical University (Poland) | 734 |
| 6 | Felker, G.M. | Duke Clinical Research Institute (USA) | 641 |
| 7 | Damman, K. | University Medical Center Groningen (Netherlands) | 638 |
| 8 | Anand, I.S. | University of Minnesota Medical School (USA) | 616 |
| 9 | Anker, S.D. | Imperial College (UK) | 583 |
| 10 | Tsutamoto, T. | Shiga University of Medical Science (Japan) | 577 |
Keywords clusters and bursts detection; Keywords broadly reflect the research theme and primary content of the documents, and they could reasonably describe the research hot spots. A total of 12,037 keywords were extracted from a total of 5,978 publications. Table 5 lists the top 20 keywords with high frequency related to HF biomarkers. In addition to the search words heart failure, biomarker and commonly used clinical indicators such as mortality, disease, risk, outcome, etc., the incidence of keywords such as brain natriuretic peptide, natriuretic peptide, angiotensin II, nt-pro-bnp, prognosis and diagnosis were high.
Table 5.
Top 20 keywords for heart failure biomarkers.
| Rank | Keyword | Occurrences | Rank | Keyword | Occurrences |
|---|---|---|---|---|---|
| 1 | heart failure | 2,965 | 11 | myocardial infarction | 619 |
| 2 | mortality | 1,319 | 12 | dysfunction | 551 |
| 3 | brain natriuretic peptide | 1,143 | 13 | association | 544 |
| 4 | biomarker | 1,048 | 14 | outcome | 481 |
| 5 | natriuretic peptide | 965 | 15 | prognostic value | 459 |
| 6 | prognosis | 733 | 16 | nt-pro-bnp | 425 |
| 7 | disease | 727 | 17 | chronic heart failure | 411 |
| 8 | angiotensin ii | 690 | 18 | inflammation | 380 |
| 9 | diagnosis | 658 | 19 | expression | 374 |
| 10 | risk | 639 | 20 | survival | 370 |
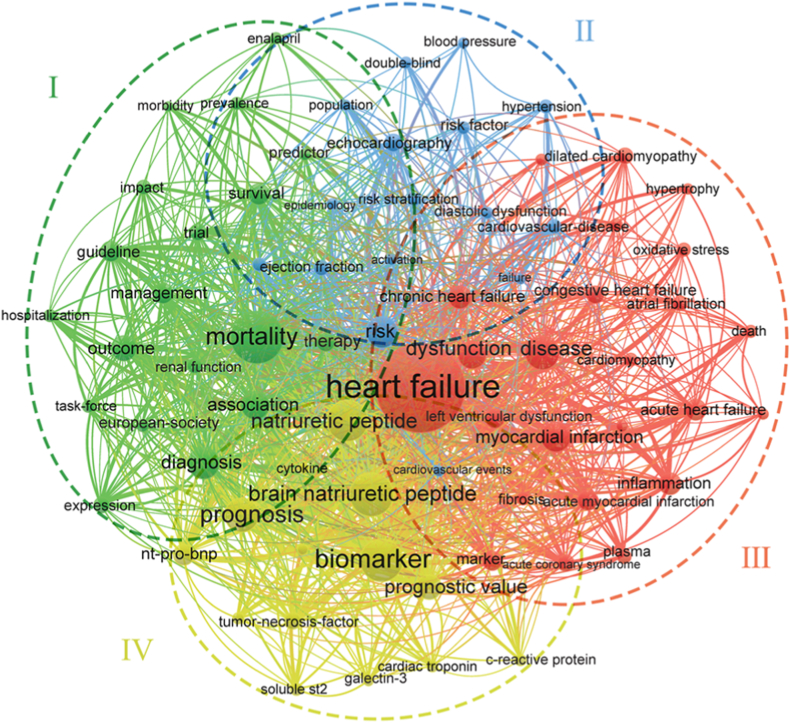
Fig. 4 shows the keywords cluster analysis of 73 keywords that appear at least 130 times, which were divided into four clusters. High-frequency keywords included in green cluster Ⅰ, mortality, survival, association, impact, outcome, management, etc. Cluster Ⅱ in blue, the high-frequency keywords contained risk, diastolic dysfunction, double-blind, failure, hypertension, etc. In the red cluster Ⅲ, heart failure, chronic heart failure, dysfunction, congestive heart failure, myocardial infarction, disease, etc. appeared frequently. Among the cluster Ⅳ in yellow, biomarker, brain natriuretic peptide, natriuretic peptide, prognostic value, and nt-pro-bnp were the main high-frequency keywords.
Fig. 4.
Network map of keywords for heart failure biomarkers.
The keywords bursts are shown in Appendix B1. For the time span of keywords from 1989 to 2021, the minimum duration was set to five, and 103 strongly cited keywords were detected. Early keywords (began from 1991 to 1995) were atrial natriuretic peptide, atrial natriuretic factor, plasma level, congestive heart failure, angiotensin II, etc. Cardiovascular magnetic resonance, enalapril, lcz696, preserved ejection fraction, and myocardial fibrosis were the main emergent keywords lasting until 2021. Those lasting more than 18 years included response, release, convergent heart failure, idiopathic written cardiology, and hemodynamics. The Burst Strength above 20.00 included convergent heart failure, tumor necrosis factor, and left ventricular dysfunction. Among them, the Burst Strength of left ventricular dysfunction was the highest, 41.57.
3.4. Theme overlapping, strategy, and evolution
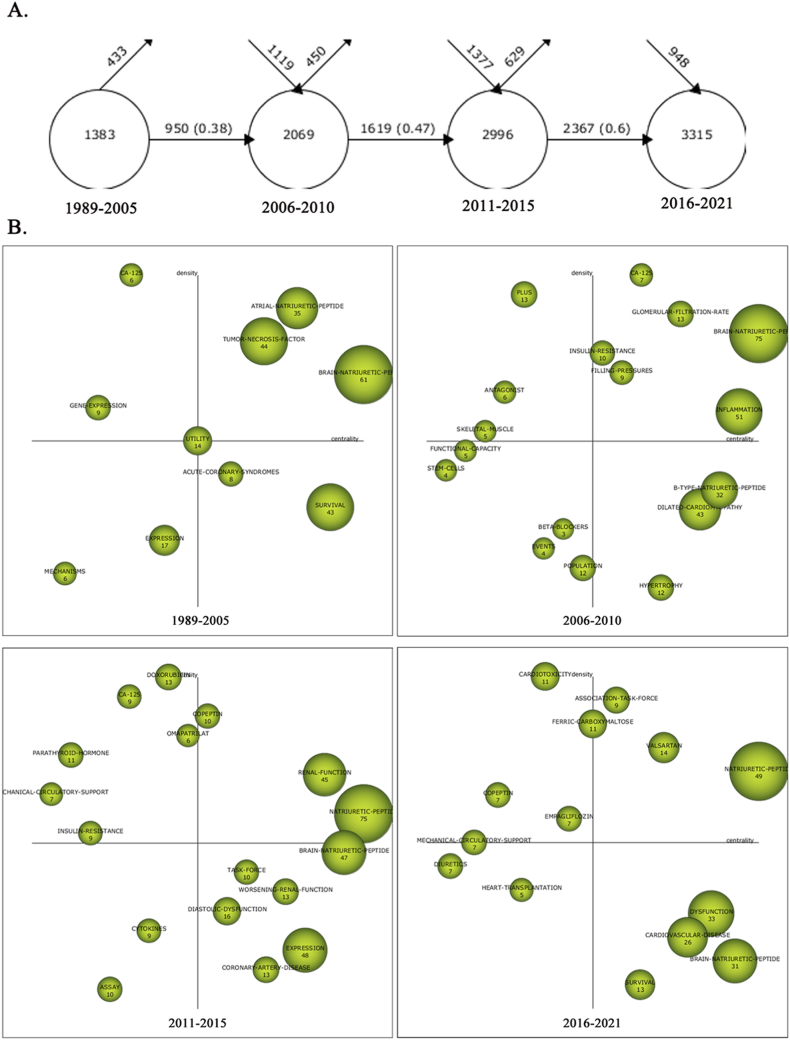
Fig. 5A shows the keyword overlapping map for the four periods, where the Similarity Index in parentheses revealed an increasing trend (0.38–0.47∼0.6) and the Similarity Index was greater than 0.5 for the third to fourth periods. New themes were greater than the declining themes in each period, and the total amount of themes was increasing while the innovation index was decreasing.
Fig. 5.
A Overlapping map of keywords for heart failure biomarkers. B Strategic diagrams for heart failure biomarkers.
The two crossed axes of the strategy map represent density and centrality, respectively, and the four quadrants distinguished represent the maturity and development potential of the themes in which they are located. Quadrant in the upper right corner of which shows strong centrality and high density, indicating that the research themes represented by the keywords in this region are the most popular. The H-index of the word represented by the node in the strategy map determines the size of the node. The strategy diagram in Fig. 5B shows the allocation of themes in four different stages. Hot themes in the first period (1989–2005) included atrial natriuretic peptide, tumor necrosis factor, and brain natriuretic peptide. The second period (2006–2010) focused on brain natriuretic peptide, inflammation, insulin resistance, CA125, filling pressures, and glomerular filtration rate. The third phase (2011–2015) focused on copeptin, renal function, and natriuretic peptide. The final phase (2016–2021) was the association task force, valsartan, ferric carboxymaltose, and natriuretic peptide.
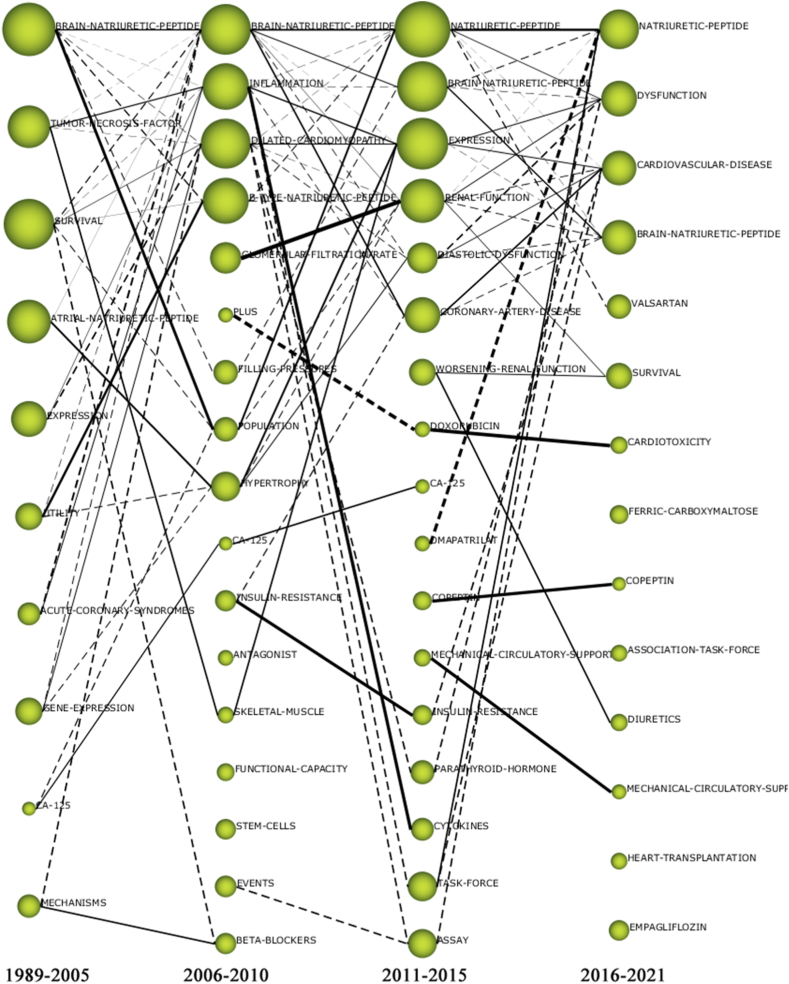
Fig. 6 shows the evolution diagram, and the H-index associated with the thematic cluster represented by the node determines the size of the node. Solid lines represent associated clustering topics that share major analysis units, indicating that the two topics are persistent and indicate the mainstream evolution orientation. The dashed lines represent the thematic shared elements that are not the primary analysis unit and represent the evolution direction of the tributaries. Isolated nodes represent themes that occur only in one period and somewhat reflect new themes. We can also use the timeline in Fig. 6 to examine the changing relationships and trends of keywords over time. As a representative marker of HF, brain natriuretic peptide has been in the mainstream of research. From the third period, the study was extended from brain natriuretic peptide to the whole natriuretic peptide family, which became a hot research theme and had high centrality. The mainstream evolutions of tumor necrosis factor and acute coronary syndromes were to inflammation to cytokines; or to expression to dysfunction and cardiovascular disease. Atrial natriuretic peptide has been studied in the first period, and its mainstream evolution was to hypertrophy and then to expression; or to diastolic dysfunction and then to cardiovascular disease. The mainstream evolution of gene expression was to dilated cardiomyopathy and then to expression. CA125 had a high density and was a hot spot for research in the first three periods. Biomarkers of interest in recent years include copeptin, in addition to the natriuretic peptide family. Other topical studies have focused on the treatment of HF, including valsartan, ferric carboxymaltose, diuretics, empagliflozin, mechanical circulatory support, and heart transplantation.
Fig. 6.
Thematic evolution map for heart failure biomarkers.
4. Discussion
Analysis of publications and trend curves of HF biomarkers showed that few papers were published before the 21st century. Before 1997, the number of publications only stayed in single digits. After 1997, although the quantity of publications broke through single digits, the annual number of publications remained below 100 from 1997 to 2003. However, since entering the 21st century, there has been a significant increase in the number of documents published in this field. The predictors of HF were proposed earlier. As early as 1956, in a small sample study of 40 patients with HF, it was found that C-reactive protein (CRP), an inflammatory immune marker, was significantly increased in patients with severe HF [21]. Subsequent studies found that hs-CRP was an independent predictor of HF prognosis [22]. With the in-depth study on the pathophysiology of HF, neurohormonal markers were also proposed in the late 1980s, including plasma norepinephrine, natriuretic peptide, vasopressin, etc. Although markers for HF were developed earlier, the formal use of biomarkers was later. As far as we can discover, “biomarker” was first used in 1973 in the title of a document [23], and the earliest clinical use began in 1977 in a publication entitled “Tumor biomarkers of value in the management of gynecologic malignancy will also be correlated for clinical course” [24]. The significant increase in interest in biomarkers began in 2005 and has been particularly dramatic since 2010 [25]. This was consistent with the significant increase in annual publications of HF biomarkers since 2005, with studies accounting for 72.63% of total publications in the decade since 2010. In addition, with the in-depth exploration of genetic, metabolic, and inflammatory mechanisms and the rapid development of omics in recent years, some new biomarkers have been continuously discovered, such as oxidative stress markers [26] and cardiomyocyte extracellular matrix remodeling markers [27], which also promoted the increase in the number of HF biomarkers. However, the annual growth rate in the past two years has gradually turned negative, especially significantly negative in 2021, which may indicate that the research on HF biomarkers has reached a relatively mature stage or reached a bottleneck. It could be predicted that the number of documents published in this field will also show a downward trend in the next few years. It suggests that researchers should change their research thinking and conduct a broader and deeper longitudinal study on the identified markers.
Among the list of journals with the top 10 co-citations were some of the top medical journals, such as Circulation, New England Journal of Medicine, and Lancet. There were also some special journals on Heart, such as European Heart Journal, European Journal of Heart Failure, American Heart Journal, etc. The average IF of these ten journals is 28.728, with six of them exceeding 10.000, showing that journals with high IF values are more easily cited. Bradford's law still holds true in such co-cited journals, with a large number of citations coming from a small number of central journals. The top 10 co-cited references were mainly guidelines and trials, including European Society of Cardiology (ESC) and ACCF/AHA guidelines on HF, and studies were mainly large multicenter studies. It was highly co-cited because of its comprehensive summary and cutting-edge exploration of various aspects of HF including HF biomarker. Burst strength of more than 50.00 was reported in three documents, one of which was a multicenter study of rapid measurement of HF by B-type Natriuretic Peptide, a classic biomarker of HF, published in 2002 [19], and two of which were ESC guidelines for the treatment and diagnosis of HF published in 2008 and 2012, respectively [20,28]. Among the authors of the top 10 co-citations, Maisel, A.S. ranked first, and the number of publications ranked third among the top 20 most prolific authors, indicating that Maisel, A.S. has made outstanding contributions in the HF biomarkers research. Januzzi, J.l. ranks first in the number of publications and has more than 1,000 citations, indicating his profound influence in this field. Among these 10 authors, six authors are among the top 20 most prolific authors, indicating a good coincidence between the most prolific authors and highly co-cited authors.
Keywords analysis showed 12,037 keywords were extracted from 1989 to 2021. There were 1,697 (14.98%) keywords that appeared more than five times, 875 (7.27%) keywords that appeared more than 10 times, and 92 keywords that appeared more than 100 times (0.76%). High-frequency keywords reflect the hot issues in a certain research field. Among the top 20 high-frequency keywords (as shown in Table 5), there were methodology keywords and commonly used clinical index search terms. When only HF biomarkers are considered, brain natriuretic peptide, natriuretic peptide, angiotensin II and nt-pro-bnp have a high incidence, indicating their core position in this field. The co-occurrence analysis of keywords provides a basis for the distribution of topics and research trends in related fields for researchers. The 73 keywords that appeared at least 130 times were clustered into four categories.
Cluster Ⅰ with green color contained 19 keywords, mainly related to the epidemiological characteristics, diagnosis, treatment, and management of HF. HF remains a rising global epidemic. In the USA, the number of patients with HF tripled from 1979 to 2004 alone [29]. It was estimated that by 2030, the prevalence of HF in the USA is expected to increase by 46% to more than eight million people (2.97%) [5]. In addition, the prevalence of HF will continue to increase in many developing countries undergoing an epidemiological transition, coupled with an expanding and aging global population [30]. In recent years, with the improvement of primary prevention of cardiovascular disease and treatment of ischemic heart disease in developed countries such as Europe and the USA, the incidence of HF in certain populations has shown signs of stabilization and possible reduction [31,32]. However, differences in race, region, and socioeconomic status lead to huge differences in disease rates [33]. The Framingham Heart Study of 1971 provided a clinical diagnostic standard [34], and in 2015, the American Society of Echocardiography published updated guidelines for the echocardiographic assessment of left ventricular function [35].
Cluster Ⅱ in blue contained 16 keywords, mainly related to some causes and risk factors of HF. Dzau.V. and Braunwald, E. in their 1991 review, proposed the “cardiovascular event chain”, which refers to a chronological sequence of cardiovascular events starting with risk factors for cardiovascular disease, leading to myocardial ischemia leading to myocardial infarction, and finally to HF and death [36]. Therefore, all risk factors leading to cardiovascular disease may be HF risk factors, such as hypertension, diabetes, obesity and so on [[37], [38], [39], [40]]. The risk of HF can be stratified based on ejection fraction or some biomarker for management [41,42]. It was worth noting that although the number of patients with HF with preserved ejection fraction (HFpEF) accounts for the majority of patients with heart failure, there are often delays in diagnosis and limited treatment options [43,44]. This diagnostic and therapeutic challenge has led to a growing interest in HFpEF in the literature.
Cluster Ⅲ in red contained the most 24 keywords, mainly related to the mechanism, etiology, and classification of HF. HF syndrome is the result of abnormalities in the structure, function, rhythm, or conduction of the heart. Ventricular dysfunction is the most common underlying problem, mainly caused by myocardial infarction, hypertension, myocardial intimal fibrosis, and many types of cardiomyopathy [45]. Myocardial hypertrophy or fibrosis resulting from ventricular “remodeling” exacerbates left ventricular systolic dysfunction and the progression of HF [[46], [47], [48]]. This remodeling may occur in two main ways, one is complicated by cardiac events (eg, myocardial infarction), and the other is due to another system process (eg, the neurohumoral pathway) that is activated by reduced systolic function [49,50]. Atrial fibrillation and HF often coexist and are closely related in pathophysiology [51]. The classification of HF varies according to different classification standards. There are acute HF and chronic HF according to the onset rate. According to ejection fraction, there are HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF) [52].
Cluster Ⅳ in yellow contained 14 keywords, which were mainly related to HF biomarkers and their clinical value. Although biomarkers were formally put forward late, they have rapidly entered the field of vision due to their advantages of minimally invasive or non-invasive clinical application, short detection time, low cost, and high sensitivity [25]. One of the early biomarkers of HF was CRP, which is associated with NYHA grading, readmission, and death [53]. Tumor necrosis factor (TNF) is another inflammatory immune marker, which was found that the increase of TNF-α concentration in blood was an important biomarker for the progression of left ventricular dysfunction from asymptomatic to symptomatic [54]. Galectin-3 is also an inflammatory immune marker and is normally only expressed in a small amount in cardiac tissue. However, in the case of myocardial injury, the concentration of Galectin-3 rapidly increases to myocardial fibrosis and ventricular remodeling, which can provide short-term or long-term independent prognostic information for HF patients [55]. Soluble growth stimulation expression gene 2 protein (sST2), a member of the IL-1 gene family, has been reported to be highly sensitive for predicting short-term adverse events in HF and can be used as a marker for one-year assessment of adverse events in HF [56,57]. Of note, ST2, along with Galectin-3, is the only novel HF biomarkers included in the ACC/AHA guidelines for HF, and together they serve as biomarkers for ventricular remodeling and fibrosis [58]. Based on the in-depth understanding of the pathophysiology of HF, neurohumoral regulation plays an important role in the progression of HF, so neurohormonal markers play an important role in the HF biomarkers. Natriuretic peptides (NP) represent the gold standard for HF biomarkers, and since their introduction, the understanding of their biological and clinical applications has grown exponentially [59]. The NP family mainly includes Atrial Natriuretic Peptide (ANP), Brain Natriuretic Peptide (BNP), C-type Natriuretic Peptide (CNP), Renal Natriuretic Peptide and Dendroaspis Natriuretic Peptide (DNP) [60]. Of these, ANP and BNP are transcribed and mainly produced in cardiac myocytes of the atrium and ventricle respectively [61]. Both are caused by stretching of the heart muscle caused by stress or volume overload [62], which is common in HF. In recent years, BNP and N-terminal pro-B-type Natriuretic Peptide (NT-proBNP) have become powerful biomarkers for the diagnosis and prognosis of HF patients, and they have been included in the latest ESC guidelines for the diagnosis of clinical HF [63]. In addition, BNP and NT-proBNP also serve as indicators for HF risk stratification [64] and assessment of patients with acute HF [65]. The levels of cardiac troponin T and I (cTnT/I) increase sharply after myocardial injury, which is widely used in acute coronary syndromes due to their good sensitivity and specificity, and have important value in the prognostic assessment of acute HF [66]. Growth differentiation factor 15 (GDF-15) is a candidate marker that can dynamically predict poor prognosis in patients with acute HF, especially in HF patients associated with diabetes mellitus [67]. In addition to the biomarkers described above, a variety of classical or novel biomarkers together constitute the biomarker network for monitoring the progression of HF.
Co-occurrence analysis of keywords may reflect hotspots in research, while keyword bursts may indicate cutting-edge and emerging themes in research. In the Burst chart, we conducted a comprehensive comparative analysis from two aspects of the beginning and end of time and burst strength to roughly grasp the research situation in this field. The earliest keywords were from the NP family (ANP), followed by angiotensin II, endothelin, cytokine, TNF, BNP, ST2, cTnI, and other keywords related to biomarker appeared in sequence according to the research focus time order. There were fewer keywords related to biomarkers in the main keywords to 2021, but more keywords about drug therapy of HF, indicating that the treatment research of enalapril, LCZ696, ferric carboxymaltose, and other drugs to improve cardiac function and prognosis of patients with HF has gradually become a research hotspot, while the research interest of HF biomarker has decreased. It is worth noting that myocardial fibrosis, which is a key pathological feature and driving factor of cardiac remodeling in HF, has been intensively studied in recent years. Further clarification of the cellular and molecular mechanisms of myocardial fibrosis may provide potential therapeutic targets for the treatment of HF [68]. Left ventricular dysfunction has the highest burst intensity, reflecting its central position in HF, so most of the treatment measures for HF are focused on restoring left ventricular function.
Although the total number of themes continued to increase over the four periods, the overlapping of themes increased further and the innovation index showed a decreasing trend. This is consistent with the conclusion drawn from the negative growth rate of annual publications: research on HF biomarkers reached a relatively mature stage. As mentioned earlier, the NP family has an important role in the research of HF biomarkers and has been a hot theme of research in this field as it has been studied more extensively and deeply in recent years [69,70]. Inflammation, as an intermediate theme in the evolution of multiple directional themes, is an important component of the pathophysiology of HF and chronic inflammation is involved in myocardial fibrosis and ventricular remodeling [71,72]. A variety of inflammatory factors can be used as HF biomarkers, such as CRP, TNF, and Galectin-3, as described previously, in addition to IL-1 and IL-6. Although CA125 is a tumor marker, several studies have shown that it can be used to predict and guide the treatment of HF, making it a research hot spot for a while [73,74]. Expression is also a theme of high H-index, which covers the whole “central law” of cell biology. Excluding the translated products of the previously listed macromolecules, the transcriptional products of some gene expressions also act as HF biomarkers. For example, microRNAs and other non-coding RNAs also play important roles in the regulation of HF [75,76]. Copeptin is a novel HF biomarker, especially for predicting the risk of acute HF and cardiovascular death, and has great potential for clinical application [77]. The theme evolution diagram and strategy map analysis of hot trends in recent years and the conclusion of keyword burst mapping are consistent: HF mechanism research and treatment have become hot, while HF biomarkers have declined in fervor. Of note are the benefit of the glucose-lowering drug empagliflozin in HFpEF patients [78,79], the effectiveness of ferric carboxymaltose in improving symptoms and quality of life in chronic HF and iron deficiency patients [80], and the heat of mechanical circulatory support and heart transplantation.
5. Strength and limitations
With the development of the Times and advances in healthcare, HF, a serious threat to people's health, is receiving more and more attention. To the best of our knowledge, this is the first global untimed bibliometric analysis of HF biomarkers research based on visual maps. The analysis addresses publication trends, co-citations, journals, co-authorships, and keywords. The cluster analysis and hotspots could allow us to analytically assess the global output of the field and generate academic rankings and reveal the current state of research in the field and predictions for future research frontiers.
Some limitations arose. 1) Only related literature contained in SCI-EXPANDED in WoSCC was evaluated, including two types of literature (article and review), and nearly all of the literature was in English. Therefore, the sources of the included literature may be biased. 2) Although the literature screening was implemented by three researchers, biases caused by personal opinions and knowledge backgrounds, etc., were unavoidable. 3) Author and institution rankings were based on data provided by WoSCC. In some cases, the name of the author or institution may be spelled differently, may be abbreviated, or the author may have more than one affiliate. This could lead to inaccurate productivity reports from these agencies or authors. 4) Although we manually standardized different expressions of the same scientific concept prior to the analysis to reduce bias, this could not be eliminated.
6. Conclusion
This study provides the first comprehensive analysis of HF biomarkers research from a visualization and bibliometric perspective. We observed that there were regional differences in research and that collaboration between underdeveloped and developed countries needs to be further strengthened to facilitate the generation of cross-cutting topics. European Journal of Heart Failure and Circulation was the most prolific and most cited journals, respectively. Januzzi, J.l. and Maisel, A.S. ranked in the top five in terms of a number of documents published and high citations in this field. In addition, the study of HF biomarkers seems to have reached a relatively mature stage, with a decrease in research fervor in recent years. The study of the NP family still has high centrality, with advances in the study of expression products and inflammatory markers. Cardiac fibrosis and cardiac remodeling have become the focus of HF research. LCZ696, ferric carboxymaltose, empagliflozin, and other therapies regarding HF have become hot spots.
Author contribution statement
Xin Dong; Yafei Xie: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Jianguo Xu: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
Yu Qin; Qingyong Zheng: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Rui Hu: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Xin Zhang; Wenxin Wang: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Jinhui Tian; Kang Yi: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
Dr. Kang Yi was supported by Natural Science Foundation of Gansu Province [22JR5RA655, 21JR1RA027].
Jinhui Tian was supported by Science and Technology Program of Gansu Province [20CX4ZA027, 20CX9ZA112].
Data availability statement
Data included in article/supp. material/referenced in article.
Declaration of interest’s statement
The authors declare no competing interests.
Acknowledgement
The authors gratefully acknowledged the financial supports from the Natural Science Foundation of Gansu Province (22JR5RA655, 21JR1RA027) and the Gansu Province Science and Technology Plan Funded Project (20CX4ZA027, 20CX9ZA112).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e13509.
Contributor Information
Jinhui Tian, Email: tjh996@163.com.
Kang Yi, Email: yikang09@126.com.
Appendix A&B. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Baman J.R., Ahmad F.S. Heart failure. JAMA. 2020;324:1015. doi: 10.1001/jama.2020.13310. [DOI] [PubMed] [Google Scholar]
- 2.Stefil M., Manzano L., Montero-PeRez-Barquero M., Coats A.J.S., Flather M. New horizons in management of heart failure in older patients. Age Ageing. 2019;49:16–19. doi: 10.1093/ageing/afz122. [DOI] [PubMed] [Google Scholar]
- 3.Writing Committee M., Yancy C.W., Jessup M., Bozkurt B., Butler J., Casey D.E., Jr., Drazner M.H., Fonarow G.C., Geraci S.A., Horwich T., et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–e327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 4.Cook C., Cole G., Asaria P., Jabbour R., Francis D.P. The annual global economic burden of heart failure. Int. J. Cardiol. 2014;171:368–376. doi: 10.1016/j.ijcard.2013.12.028. [DOI] [PubMed] [Google Scholar]
- 5.Heidenreich P.A., Albert N.M., Allen L.A., Bluemke D.A., Butler J., Fonarow G.C., Ikonomidis J.S., Khavjou O., Konstam M.A., Maddox T.M., et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ. Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swedberg K., Cleland J., Dargie H., Drexler H., Follath F., Komajda M., Tavazzi L., Smiseth O.A., Gavazzi A., Haverich A., et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): the task force for the diagnosis and treatment of chronic heart failure of the European society of cardiology. Eur. Heart J. 2005;26:1115–1140. doi: 10.1093/eurheartj/ehi204. [DOI] [PubMed] [Google Scholar]
- 7.Thomas J.T., Kelly R.F., Thomas S.J., Stamos T.D., Albasha K., Parrillo J.E., Calvin J.E. Utility of history, physical examination, electrocardiogram, and chest radiograph for differentiating normal from decreased systolic function in patients with heart failure. Am. J. Med. 2002;112:437–445. doi: 10.1016/s0002-9343(02)01048-3. [DOI] [PubMed] [Google Scholar]
- 8.McDonagh T.A., Morrison C.E., Lawrence A., Ford I., Tunstall-Pedoe H., McMurray J.J., Dargie H.J. Symptomatic and asymptomatic left-ventricular systolic dysfunction in an urban population. Lancet. 1997;350:829–833. doi: 10.1016/S0140-6736(97)03033-X. [DOI] [PubMed] [Google Scholar]
- 9.Wang T.J., Evans J.C., Benjamin E.J., Levy D., LeRoy E.C., Vasan R.S. Natural history of asymptomatic left ventricular systolic dysfunction in the community. Circulation. 2003;108:977–982. doi: 10.1161/01.CIR.0000085166.44904.79. [DOI] [PubMed] [Google Scholar]
- 10.Mann D.L., Bristow M.R. Mechanisms and models in heart failure: the biomechanical model and beyond. Circulation. 2005;111:2837–2849. doi: 10.1161/CIRCULATIONAHA.104.500546. [DOI] [PubMed] [Google Scholar]
- 11.Liao J., Wang J., Liu Y., Li J., He Q., Jiang W., Dong Y. The most cited articles in coronary heart disease: a bibliometric analysis between 1970 and 2015. Int. J. Cardiol. 2016;222:1049–1052. doi: 10.1016/j.ijcard.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Gao Y., Shi S., Ma W., Chen J., Cai Y., Ge L., Li L., Wu J., Tian J. Bibliometric analysis of global research on PD-1 and PD-L1 in the field of cancer. Int. Immunopharm. 2019;72:374–384. doi: 10.1016/j.intimp.2019.03.045. [DOI] [PubMed] [Google Scholar]
- 13.Gao Y., Ge L., Shi S., Sun Y., Liu M., Wang B., Shang Y., Wu J., Tian J. Global trends and future prospects of e-waste research: a bibliometric analysis. Environ. Sci. Pollut. Res. Int. 2019;26:17809–17820. doi: 10.1007/s11356-019-05071-8. [DOI] [PubMed] [Google Scholar]
- 14.van Eck N.J., Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523–538. doi: 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc. Natl. Acad. Sci. U. S. A. 2004;101(Suppl 1):5303–5310. doi: 10.1073/pnas.0307513100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cobo M.J., Lopez-Herrera A.G., Herrera-Viedma E., Herrera F. SciMAT: a new science mapping analysis software tool. J. Am. Soc. Inf. Sci. Technol. 2012;63:1609–1630. doi: 10.1002/asi.22688. [DOI] [Google Scholar]
- 17.de Mendonca Lima C.A., De Leo D., Ivbijaro G., Svab I. Suicide prevention in older adults. Asia Pac. Psychiatr. 2021;13 doi: 10.1111/appy.12473. [DOI] [PubMed] [Google Scholar]
- 18.Ponikowski P., Voors A.A., Anker S.D., Bueno H., Cleland J.G., Coats A.J., Falk V., Gonzalez-Juanatey J.R., Harjola V.P., Jankowska E.A., et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592. [DOI] [PubMed] [Google Scholar]
- 19.Maisel A.S., Krishnaswamy P., Nowak R.M., McCord J., Hollander J.E., Duc P., Omland T., Storrow A.B., Abraham W.T., Wu A.H., et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N. Engl. J. Med. 2002;347:161–167. doi: 10.1056/NEJMoa020233. [DOI] [PubMed] [Google Scholar]
- 20.McMurray J.J., Adamopoulos S., Anker S.D., Auricchio A., Bohm M., Dickstein K., Falk V., Filippatos G., Fonseca C., Gomez-Sanchez M.A., et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European society of cardiology. Developed in collaboration with the heart failure association (HFA) of the ESC. Eur. Heart J. 2012;33:1787–1847. doi: 10.1093/eurheartj/ehs104. [DOI] [PubMed] [Google Scholar]
- 21.Elster S.K., Braunwald E., Wood H.F. A study of C-reactive protein in the serum of patients with congestive heart failure. Am. Heart J. 1956;51:533–541. doi: 10.1016/0002-8703(56)90099-0. [DOI] [PubMed] [Google Scholar]
- 22.Adukauskiene D., Ciginskiene A., Adukauskaite A., Pentiokiniene D., Slapikas R., Ceponiene I. Clinical relevance of high sensitivity C-reactive protein in cardiology. Medicina. 2016;52:1–10. doi: 10.1016/j.medici.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Rho J.H., Bauman A.J., Boettger H.G., Yen T.F. A search for porphyrin biomarkers in Nonesuch Shale and extraterrestrial samples. Space Life Sci. 1973;4:69–77. doi: 10.1007/BF02626343. [DOI] [PubMed] [Google Scholar]
- 24.Order S.E. Beneficial and detrimental effects of therapy on immunity in breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 1977;2:377–380. doi: 10.1016/0360-3016(77)90101-8. [DOI] [PubMed] [Google Scholar]
- 25.Aronson J.K., Ferner R.E. Biomarkers-A general review. Curr. Protoc. Pharmacol. 2017;76:9. doi: 10.1002/cpph.19. 23 21-29 23 17. [DOI] [PubMed] [Google Scholar]
- 26.Ungvari Z., Gupte S.A., Recchia F.A., Batkai S., Pacher P. Role of oxidative-nitrosative stress and downstream pathways in various forms of cardiomyopathy and heart failure. Curr. Vasc. Pharmacol. 2005;3:221–229. doi: 10.2174/1570161054368607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sackner-Bernstein J.D. The myocardial matrix and the development and progression of ventricular remodeling. Curr. Cardiol. Rep. 2000;2:112–119. doi: 10.1007/s11886-000-0007-4. [DOI] [PubMed] [Google Scholar]
- 28.Dickstein K., Cohen-Solal A., Filippatos G., McMurray J.J., Ponikowski P., Poole-Wilson P.A., Stromberg A., van Veldhuisen D.J., Atar D., Hoes A.W., et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the task force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European society of cardiology. Developed in collaboration with the heart failure association of the ESC (HFA) and endorsed by the European society of intensive care medicine (ESICM) Eur. Heart J. 2008;29:2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 29.Fang J., Mensah G.A., Croft J.B., Keenan N.L. Heart failure-related hospitalization in the U.S., 1979 to 2004. J. Am. Coll. Cardiol. 2008;52:428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 30.Roth G.A., Forouzanfar M.H., Moran A.E., Barber R., Nguyen G., Feigin V.L., Naghavi M., Mensah G.A., Murray C.J. Demographic and epidemiologic drivers of global cardiovascular mortality. N. Engl. J. Med. 2015;372:1333–1341. doi: 10.1056/NEJMoa1406656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao D., Liu J., Xie W., Qi Y. Cardiovascular risk assessment: a global perspective. Nat. Rev. Cardiol. 2015;12:301–311. doi: 10.1038/nrcardio.2015.28. [DOI] [PubMed] [Google Scholar]
- 32.Djousse L., Driver J.A., Gaziano J.M. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook N.L., Lauer M.S. The socio-geography of heart failure: why it matters. Circ. Heart Fail. 2011;4:244–245. doi: 10.1161/CIRCHEARTFAILURE.111.962191. [DOI] [PubMed] [Google Scholar]
- 34.Mahmood S.S., Wang T.J. The epidemiology of congestive heart failure: the Framingham Heart Study perspective. Glob. Heart. 2013;8:77–82. doi: 10.1016/j.gheart.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lang R.M., Badano L.P., Mor-Avi V., Afilalo J., Armstrong A., Ernande L., Flachskampf F.A., Foster E., Goldstein S.A., Kuznetsova T., et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015;28:1–39. doi: 10.1016/j.echo.2014.10.003. e14. [DOI] [PubMed] [Google Scholar]
- 36.Dzau V., Braunwald E. Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshop consensus statement. Am. Heart J. 1991;121:1244–1263. doi: 10.1016/0002-8703(91)90694-d. [DOI] [PubMed] [Google Scholar]
- 37.Komanduri S., Jadhao Y., Guduru S.S., Cheriyath P., Wert Y. Prevalence and risk factors of heart failure in the USA: NHANES 2013 - 2014 epidemiological follow-up study. J. Community Hosp. Intern. Med. Perspect. 2017;7:15–20. doi: 10.1080/20009666.2016.1264696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho J.E., Enserro D., Brouwers F.P., Kizer J.R., Shah S.J., Psaty B.M., Bartz T.M., Santhanakrishnan R., Lee D.S., Chan C., et al. Predicting heart failure with preserved and reduced ejection fraction: the international collaboration on heart failure subtypes. Circ. Heart Fail. 2016;9 doi: 10.1161/CIRCHEARTFAILURE.115.003116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhambhani V., Kizer J.R., Lima J.A.C., van der Harst P., Bahrami H., Nayor M., de Filippi C.R., Enserro D., Blaha M.J., Cushman M., et al. Predictors and outcomes of heart failure with mid-range ejection fraction. Eur. J. Heart Fail. 2018;20:651–659. doi: 10.1002/ejhf.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Echouffo-Tcheugui J.B., Greene S.J., Papadimitriou L., Zannad F., Yancy C.W., Gheorghiade M., Butler J. Population risk prediction models for incident heart failure: a systematic review. Circ. Heart Fail. 2015;8:438–447. doi: 10.1161/CIRCHEARTFAILURE.114.001896. [DOI] [PubMed] [Google Scholar]
- 41.Bayes-Genis A., Ordonez-Llanos J. Multiple biomarker strategies for risk stratification in heart failure. Clin. Chim. Acta. 2015;443:120–125. doi: 10.1016/j.cca.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 42.Magri D., Gallo G., Parati G., Cicoira M., Senni M. Risk stratification in heart failure with mild reduced ejection fraction. Eur. J. Prev. Cardiol. 2020;27:59–64. doi: 10.1177/2047487320951104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brouwers F.P., de Boer R.A., van der Harst P., Voors A.A., Gansevoort R.T., Bakker S.J., Hillege H.L., van Veldhuisen D.J., van Gilst W.H. Incidence and epidemiology of new onset heart failure with preserved vs. reduced ejection fraction in a community-based cohort: 11-year follow-up of PREVEND. Eur. Heart J. 2013;34:1424–1431. doi: 10.1093/eurheartj/eht066. [DOI] [PubMed] [Google Scholar]
- 44.Borlaug B.A. Evaluation and management of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2020;17:559–573. doi: 10.1038/s41569-020-0363-2. [DOI] [PubMed] [Google Scholar]
- 45.McMurray J.J., Pfeffer M.A. Heart failure. Lancet. 2005;365:1877–1889. doi: 10.1016/S0140-6736(05)66621-4. [DOI] [PubMed] [Google Scholar]
- 46.Konstam M.A., Udelson J.E., Anand I.S., Cohn J.N. Ventricular remodeling in heart failure: a credible surrogate endpoint. J. Card. Fail. 2003;9:350–353. doi: 10.1054/j.cardfail.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 47.Feldman A.M., Li Y.Y., McTiernan C.F. Matrix metalloproteinases in pathophysiology and treatment of heart failure. Lancet. 2001;357:654–655. doi: 10.1016/s0140-6736(00)04151-9. [DOI] [PubMed] [Google Scholar]
- 48.Marshall D., Sack M.N. Apoptosis: a pivotal event or an epiphenomenon in the pathophysiology of heart failure? Heart. 2000;84:355–356. doi: 10.1136/heart.84.4.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Swedberg K. Importance of neuroendocrine activation in chronic heart failure. Impact on treatment strategies. Eur. J. Heart Fail. 2000;2:229–233. doi: 10.1016/s1388-9842(00)00102-1. [DOI] [PubMed] [Google Scholar]
- 50.Anker S.D., von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004;90:464–470. doi: 10.1136/hrt.2002.007005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sugumar H., Nanayakkara S., Prabhu S., Voskoboinik A., Kaye D.M., Ling L.H., Kistler P.M. Pathophysiology of atrial fibrillation and heart failure: dangerous interactions. Cardiol. Clin. 2019;37:131–138. doi: 10.1016/j.ccl.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 52.Lam C.S.P., Solomon S.D. Classification of heart failure according to ejection fraction: JACC review topic of the week. J. Am. Coll. Cardiol. 2021;77:3217–3225. doi: 10.1016/j.jacc.2021.04.070. [DOI] [PubMed] [Google Scholar]
- 53.Alonso-Martinez J.L., Llorente-Diez B., Echegaray-Agara M., Olaz-Preciado F., Urbieta-Echezarreta M., Gonzalez-Arencibia C. C-reactive protein as a predictor of improvement and readmission in heart failure. Eur. J. Heart Fail. 2002;4:331–336. doi: 10.1016/s1388-9842(02)00021-1. [DOI] [PubMed] [Google Scholar]
- 54.Torre-Amione G., Kapadia S., Benedict C., Oral H., Young J.B., Mann D.L. Proinflammatory cytokine levels in patients with depressed left ventricular ejection fraction: a report from the Studies of Left Ventricular Dysfunction (SOLVD) J. Am. Coll. Cardiol. 1996;27:1201–1206. doi: 10.1016/0735-1097(95)00589-7. [DOI] [PubMed] [Google Scholar]
- 55.Filipe M.D., Meijers W.C., Rogier van der Velde A., de Boer R.A. Galectin-3 and heart failure: prognosis, prediction & clinical utility. Clin. Chim. Acta. 2015;443:48–56. doi: 10.1016/j.cca.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 56.Gaggin H.K., Szymonifka J., Bhardwaj A., Belcher A., De Berardinis B., Motiwala S., Wang T.J., Januzzi J.L., Jr. Head-to-head comparison of serial soluble ST2, growth differentiation factor-15, and highly-sensitive troponin T measurements in patients with chronic heart failure. JACC Heart Fail. 2014;2:65–72. doi: 10.1016/j.jchf.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 57.Huang A., Qi X., Hou W., Qi Y., Zhao N., Liu K. Prognostic value of sST2 and NT-proBNP at admission in heart failure with preserved, mid-ranged and reduced ejection fraction. Acta Cardiol. 2018;73:41–48. doi: 10.1080/00015385.2017.1325617. [DOI] [PubMed] [Google Scholar]
- 58.Yancy C.W., Jessup M., Bozkurt B., Butler J., Casey D.E., Jr., Colvin M.M., Drazner M.H., Filippatos G.S., Fonarow G.C., Givertz M.M., et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of cardiology/American heart association task force on clinical practice guidelines and the heart failure society of America. Circulation. 2017;136:e137–e161. doi: 10.1161/CIR.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 59.Gaggin H.K., Januzzi J.L., Jr. Biomarkers and diagnostics in heart failure. Biochim. Biophys. Acta. 2013;1832:2442–2450. doi: 10.1016/j.bbadis.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 60.Nakao K., Ogawa Y., Suga S., Imura H. Molecular biology and biochemistry of the natriuretic peptide system. I: natriuretic peptides. J. Hypertens. 1992;10:907–912. [PubMed] [Google Scholar]
- 61.Mukoyama M., Nakao K., Hosoda K., Suga S., Saito Y., Ogawa Y., Shirakami G., Jougasaki M., Obata K., Yasue H., et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J. Clin. Invest. 1991;87:1402–1412. doi: 10.1172/JCI115146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mazurkiewicz L., Ruzyllo W., Chmielak Z., Opalinska-Ciszek E., Janas J., Hoffman P., Hryniewiecki T., Grzybowski J. ANP and BNP plasma levels in patients with rheumatic mitral stenosis after percutaneous balloon mitral valvuloplasty. Postepy Kardiol. Interwencyjnej. 2017;13:18–25. doi: 10.5114/aic.2017.66182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ponikowski P., Voors A.A., Anker S.D., Bueno H., Cleland J.G.F., Coats A.J.S., Falk V., Gonzalez-Juanatey J.R., Harjola V.P., Jankowska E.A., et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 64.Mueller C., Scholer A., Laule-Kilian K., Martina B., Schindler C., Buser P., Pfisterer M., Perruchoud A.P. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N. Engl. J. Med. 2004;350:647–654. doi: 10.1056/NEJMoa031681. [DOI] [PubMed] [Google Scholar]
- 65.Januzzi J.L., Jr., Rehman S., Mueller T., van Kimmenade R.R., Lloyd-Jones D.M. Importance of biomarkers for long-term mortality prediction in acutely dyspneic patients. Clin. Chem. 2010;56:1814–1821. doi: 10.1373/clinchem.2010.146506. [DOI] [PubMed] [Google Scholar]
- 66.Harrison N., Favot M., Levy P. The role of troponin for acute heart failure. Curr. Heart Fail. Rep. 2019;16:21–31. doi: 10.1007/s11897-019-0420-5. [DOI] [PubMed] [Google Scholar]
- 67.Echouffo-Tcheugui J.B., Daya N., Ndumele C.E., Matsushita K., Hoogeveen R.C., Ballantyne C.M., Coresh J., Shah A.M., Selvin E. Diabetes, GDF-15 and incident heart failure: the atherosclerosis risk in communities study. Diabetologia. 2022;65:955–963. doi: 10.1007/s00125-022-05678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gonzalez A., Schelbert E.B., Diez J., Butler J. Myocardial interstitial fibrosis in heart failure: biological and translational perspectives. J. Am. Coll. Cardiol. 2018;71:1696–1706. doi: 10.1016/j.jacc.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 69.Segar M.W., Khan M.S., Patel K.V., Vaduganathan M., Kannan V., Willett D., Peterson E., Tang W.H.W., Butler J., Everett B.M., et al. Incorporation of natriuretic peptides with clinical risk scores to predict heart failure among individuals with dysglycemia. Eur. J. Heart Fail. 2022;24:169–180. doi: 10.1002/ejhf.2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Buchan T.A., Ching C., Foroutan F., Malik A., Daza J.F., Hing N.N.F., Siemieniuk R., Evaniew N., Orchanian-Cheff A., Ross H.J., et al. Prognostic value of natriuretic peptides in heart failure: systematic review and meta-analysis. Heart Fail. Rev. 2022;27:645–654. doi: 10.1007/s10741-021-10136-3. [DOI] [PubMed] [Google Scholar]
- 71.Adamo L., Rocha-Resende C., Prabhu S.D., Mann D.L. Reappraising the role of inflammation in heart failure. Nat. Rev. Cardiol. 2020;17:269–285. doi: 10.1038/s41569-019-0315-x. [DOI] [PubMed] [Google Scholar]
- 72.Dick S.A., Epelman S. Chronic heart failure and inflammation: what do we really know? Circ. Res. 2016;119:159–176. doi: 10.1161/CIRCRESAHA.116.308030. [DOI] [PubMed] [Google Scholar]
- 73.Yilmaz M.B., Nikolaou M., Cohen Solal A. Tumour biomarkers in heart failure: is there a role for CA-125? Eur. J. Heart Fail. 2011;13:579–583. doi: 10.1093/eurjhf/hfr022. [DOI] [PubMed] [Google Scholar]
- 74.Huynh K. Heart failure: CA125-guided therapy reduces AHF rehospitalizations. Nat. Rev. Cardiol. 2016;13:634–635. doi: 10.1038/nrcardio.2016.142. [DOI] [PubMed] [Google Scholar]
- 75.Shen N.N., Wang J.L., Fu Y.P. The microRNA expression profiling in heart failure: a systematic review and meta-analysis. Front. Cardiovasc. Med. 2022;9 doi: 10.3389/fcvm.2022.856358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Garcia-Padilla C., Lozano-Velasco E., Garcia-Lopez V., Aranega A., Franco D., Garcia-Martinez V., Lopez-Sanchez C. Comparative analysis of non-coding RNA transcriptomics in heart failure. Biomedicines. 2022;10 doi: 10.3390/biomedicines10123076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alehagen U., Dahlstrom U., Rehfeld J.F., Goetze J.P. Association of copeptin and N-terminal proBNP concentrations with risk of cardiovascular death in older patients with symptoms of heart failure. JAMA. 2011;305:2088–2095. doi: 10.1001/jama.2011.666. [DOI] [PubMed] [Google Scholar]
- 78.Heerspink H.J.L., Inker L., Greene T. Empagliflozin in heart failure with a preserved ejection fraction. N. Engl. J. Med. 2022;386:e57. doi: 10.1056/NEJMc2118470. [DOI] [PubMed] [Google Scholar]
- 79.Voors A.A., Angermann C.E., Teerlink J.R., Collins S.P., Kosiborod M., Biegus J., Ferreira J.P., Nassif M.E., Psotka M.A., Tromp J., et al. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: a multinational randomized trial. Nat. Med. 2022;28:568–574. doi: 10.1038/s41591-021-01659-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ponikowski P., Kirwan B.A., Anker S.D., McDonagh T., Dorobantu M., Drozdz J., Fabien V., Filippatos G., Gohring U.M., Keren A., et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet. 2020;396:1895–1904. doi: 10.1016/S0140-6736(20)32339-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supp. material/referenced in article.