Abstract
BACKGROUND:
Modern competency-based medical education emphasizes student-centered teaching-learning strategies where students take responsibility of their own learning. Student-centered approaches facilitate multifaceted learning such as observation, critical evaluation, analysis, deeper understanding, and application of knowledge. The current study aims at assessing the students’ perception on utilization of clinical case problem-solving approach (CCPS) to promote their lifelong learning.
MATERIALS AND METHODS:
The present cross-sectional study was conducted at College of Medicine and Health Sciences (CoMHS) during the year 2021-2022. MD3 students of the academic year 2021-2022 were the study participants. The study was approved by institutional Ethic and Review Committee. Students’ performances were assessed through pre-test and post-test performances. Students’ feedback was collected through a predesigned questionnaire on a 3-point Likert scale. Cronbach's alpha coefficient test was used to assess the reliability of the questionnaire. The data was entered to Microsoft Excel and analyzed using SPSS software version 22. Paired t-test was used to compare pre-test and post-test scores and the data was expressed as numbers and percentages.
RESULTS:
In total, 103 participants were included in the study. Post-test scores were significantly higher compared to pre-test scores (p < 0.05). Questionnaire results showed that CCPS approach was accepted as an effective learning strategy. Majority (>90%) of the students expressed CCPS approach was interesting, motivated to learn, encouraged peer discussion, enhanced knowledge, and clarified their topic-related doubts. More than 80% students opined that CCPS enhanced their critical thinking, problem-solving ability, deep learning, and lifelong learning skills. Nearly 90% of the students suggested for including such sessions for more topics in immunology course in future.
CONCLUSION:
From our study results, it can be concluded that CCPS is an effective learning strategy to encourage students’ engagement and promote their deep learning skills.
Keywords: Active learning, critical thinking, immunology, medical education
Introduction
Modern highly competency-based medical education necessitates undergraduates to be introspective to practice medicine in future.[1] Traditional didactic delivery of medical curriculum is less appealing to encourage students’ active participation and tend to promote rote memorization.[2] To emanate as better lifelong learners, medical undergraduates must incorporate essential qualities such as critical thinking, clinical reasoning, deep understanding of the concept, and ability to utilize gained knowledge effectively to solve patient-related problems during clinical years and clerkships.[3,4,5,6] Recent advances in technology and innovations in medical education have focused on learning environment that promote students’ engagement and interactive discussion and thus boost their performance. This has led to the transformation of medical education from teacher-centered to student-centered strategies that foster lifelong learning skills.[7,8] Student-centered active teaching-learning methods are broadly defined as instructional strategies that encourage students’ participation and interactive peer discussion.[9,10] Consequently, it enhances their critical thinking, problem-solving ability, clinical reasoning, thus fabricates them better learners with enhanced knowledge retentiveness. Active learning strategies such as problem-based learning, team-based learning, online quizzes, flipped classroom, concept mapping, and others are more frequently used in the 21st century in higher education to facilitate lifelong learning among learners.[11,12,13,14]
Immunology is a captivating and complex course taught in a basic science medical curriculum in pre-clinical years. Teaching immunology therefore is interesting and challenging.[15] Students face significant challenges in vocabulary, identifying key areas, and understanding pathogenesis of immunological diseases, clinical reasoning, critical thinking, and correlating clinical findings in arriving at the diagnosis. Furthermore, they need to have a basic knowledge about key laboratory tests and how they are applied in diagnosis, and management of a clinical condition.[16] Accumulating an insightful knowledge during their immunology course therefore is crucial and this allows them to apply gained knowledge confidently to solve clinical problems of a patient when they progress to clinical years. Therefore, basic medical science teachers must identify and utilize teaching-learning strategies that foster learners’ lifelong learning skills. Clinical case problem-solving (CCPS) sessions are found to be encouraging techniques that help in achieving these goals. On through literature research, authors could not find any studies related to this in Oman, especially in Immunology course. Hence, the present study was aimed at assessing the effectiveness of CCPS sessions as a module in promoting students’ learning in Immunology.
Materials and Methods
Study participants and sampling
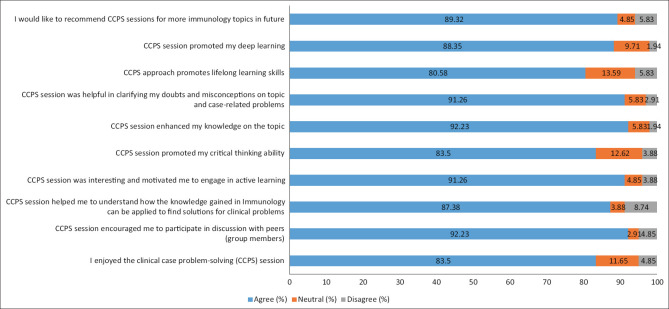
The present cross-sectional single-cohort study was conducted in the Department of Microbiology and Immunology, College of Medicine and Health Sciences (CoMHS), during 2021-2022. The CoMHS follows six-year MD program from MD1 to MD6. In MD3, students undergo training in Microbiology and Immunology along with other major courses, namely, Pathology and Pharmacology. MD3 medical students of the academic year 2021-2022 were the eligible participants, and the participation was entirely voluntary in nature. The participants were sensitized about the conduct of the study and included after obtaining an informed consent. Confidentiality and anonymity of the participants was maintained. Figure 1 depicts the flowchart of the study design.
Figure 1.
Flow chart of study design
Study design and data collection tools
A clinical case on anaphylaxis was designed, pre-validated by Microbiology and Internal Medicine experts for reliability and suitability for the use. All participants were sensitized about the CCPS session. The topic and the learning resources for the session were notified two weeks prior to the activity, and all participants were instructed to prepare before attending the session. The session was for 2 hours duration and was conducted offline in the Microbiology laboratory. The activity included administration of pre-test through Google form and collection of responses, followed by grouping of all participants with 7-8 members in each group. Each group was given pre-test-questions to discuss within the group and critically evaluate each option to arrive at the correct answers with justification. Following this, each group was given a clinical case with set of learning objectives to discuss and find the solution for case-related problems. Once all groups completed the task, each group was asked randomly to present their answers to case-related learning objectives with explanation and justification. Facilitators gave feedback and cleared all doubts and misconception of the participants. Finally, students were assessed by administering post-test through Google form and responses were collected.
Feedback
After completion of the CCPS session, students were asked to give their feedback on the session. The self-administered questionnaire, pre-validated by Immunology and Internal Medicine faculty for the reliability was administered through Google form. Before sharing the feedback, all participants were briefed about the importance of their honest and critical feedback. The questionnaire included Questions with 3-point Likert scale (agree, neutral, and disagree). The responses were collected, cleaned, entered to Microsoft Excel, and analyzed using SPSS software version 22. The results obtained were tabulated in the form of numbers and percentages.
Statistical analysis
Paired t-test was used to compare the pre-test and post-test scores. The 3-point 10-item questionnaire was analyzed to represent the perception of the participants regarding the effectiveness of CCPS as a module in encouraging their lifelong learning process. Cronbach's alpha coefficient test was used to assess the reliability of the questionnaire. The result of Cronbach's alpha test done with the SPSS version 22 for all items was calculated as 0.863, thereby representing the reliability of the questionnaire. The data was tabulated as frequencies and proportions as Agree (%), Neutral (%), and Disagree (%). Opinions regarding the teaching method were analyzed qualitatively for representative quotations until saturation of ideas was achieved.
Ethical consideration
The present study was approved by the Institutional Research and Ethic Committee [Approval no: NU/COMHS/EBC0014/2022].
Results
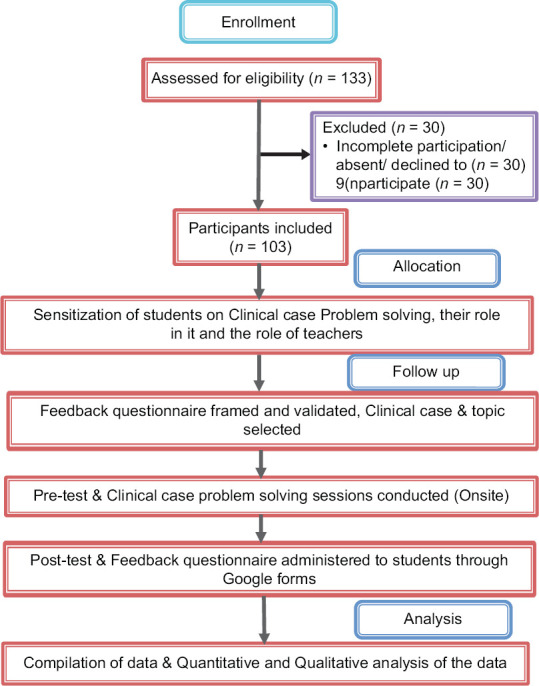
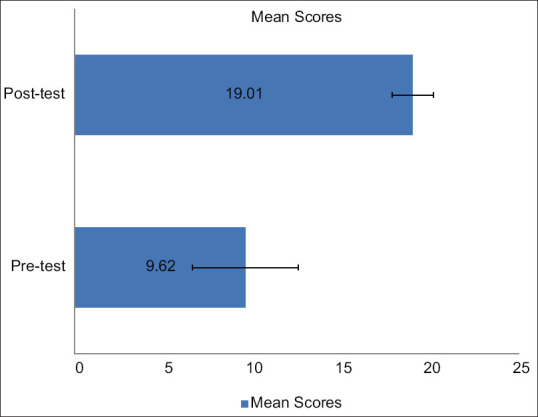
In total, 103 MD3 year students of the academic year 2021-2022 participated in the study. Figure 2 shows significant increase in post-test scores (19.01 ± 1.17) compared to pre-test scores (9.62 ± 2.98) indicating CCPS session was effective in improving students’ knowledge about the topic. Students’ perception on the effectiveness of CCPS as a teaching-learning strategy in immunology is depicted in Figure 3. Majority of students (>90%) expressed that CCPS session was interesting and motivated them to engage in active learning. Nearly 92% of students said CCPS encouraged peer discussion and enhanced their knowledge on the topic. About 83.5% students said the session was enjoyable and it enhanced their critical thinking and problem-solving ability. More than 85% of students expressed that the session helped them to understand how the gained knowledge can be confidently applied to solve the clinical-related problems. Also, majority (88%) of them felt the session benefitted them in clearing their topic-related misconceptions. Nearly 80% of the students indicated that session facilitated their lifelong learning, 88% opined CCPS promoted deep learning, while 89% of them suggested for including such sessions for more clinical immunology topics in future.
Figure 2.
Pre-test and post-test scores
Figure 3.
Students’ feedback on utilization of CCPS as a learning module in immunology
Discussion
Modern medical education is rapidly changing from teacher-centered to student-centered.[17] Medical educators have realized the importance of mixing of basic and clinical sciences as vertical integration.[18] Some educators have introduced teaching-learning strategies that illustrate teaching points with simulated or clinical case scenarios early in basic science courses. CCPS approach has received much attention in medical education worldwide as it is student-centered and exposes students to real-world clinical case scenarios which are required to be solved by deep understanding of concepts, thinking critically, linking theory to practice, interrelating, and justifying answers, and applying gained knowledge to diagnose.[10] Thus, enhances their interpretative, diagnostic, and treatment artistry. The current study was aimed at utilization of interactive CCPS approach in immunology course and to evaluate students’ perception on effectiveness of CCPS in promoting their lifelong learning skills. In our study, students’ post-test scores were significantly higher compared to pre-test scores indicating noteworthy refinement in their learning [p < 0.05]. This suggests CCPS approach is an effective method that facilitates students to build on prior knowledge and integrate the acquired knowledge to solve the clinical problem. This finding is coherent with the reports of similar studies conducted elsewhere.[19,20]
A CCPS approach involves a clinical case, set of questions or problem to be solved, and a defined set of session learning objectives with a measured outcome.[18] In this approach, some information is provided prior to the session, some presented during the learning intervention, and some information is unearthed during students’ active peer interaction and question answering session. This would encourage students to self-identify their learning needs, promotes their interest, and motivates them to get actively involved in peer discussion. This in turn, facilitates students’ arguments and expression of their views on points that they can rely on and those which should be mistrustful. This endeavor lays the foundation for students’ progression in right direction. Previous studies have demonstrated that students emerge as better lifelong learners when self-identify their learning needs, discuss with peers, and build on existing knowledge.[11,21] In our study, majority of the students opined that the CCPS stimulated interest, promoted peer discussion, and enhanced their knowledge on the topic.
Measurement of critical thinking among the medical students is considered as one of the criteria for the accreditation of medical schools by World Federation for Medical Education.[22,23] Critical thinking skills facilitate recognizing and addressing situation, processing, and organizing the facts, and linking the facts to define a problem and develop effective solutions. Clinical case-based teaching-learning approach provides an opportunity to students to critically evaluate their ideas, bridge theory and practice, acquire greater knowledge, and apply gained knowledge to find solution to clinical-related problems.[11,18,21] The current study results support these facts as most of the students expressed that CCPS improved their critical thinking ability, problem-solving skills, and knowledge on the topic.
Medical professionals must have diversified multifarious knowledge to face the various situations during their clinical practice. Hence, deeper learning that drives beyond simple rote learning and identification of correct answers is crucial during their medical training right from the beginning of the medical course. Deep learning is more aligned with impactful skills such as observation, communication, assessing the credibility of sources of information, clarification of concepts, distinguishing facts, justifying, and concluding facts, and evaluating and bridging previous information with new information resulted from reasoning and problem-solving.[11,18,21,24] Thus, focusing on deep learning approach in basic medical sciences is crucial to train medical students to face real patient-related challenges as they progress to clinical years and, prepare them as a confident future clinical practitioner. In the current study, most of the students agreed that CCPS facilitated their deep learning.
Finally, 9 out of 10 participants opined that CCPS approach should be incorporated to more topics in immunology, indicating it had a positive impact on promoting lifelong learning skills. This can be ascribed to students’ active participation in the learning process during the session. Scientific literature reveals that students engagement in discussion with peers enhances communication skills, ability to think critically, and analyze, justify, and deduce facts, and thus enhances attainment of higher level of cognition, enhancement of problem-solving ability, and understanding of disease concepts rather than just memorization.[18,24]
This study has several limitations. First, the sample size was small that has involved only MD3 cohort. Second, the study was performed using a single-case scenario. Although, the case scenario was carefully created by experts, the possibility of bias cannot be ruled out completely and therefore, validity of the study results remains limited. Third, clinical case scenarios differ from real patients. Hence, follow-up studies need to be conducted in the future to assess long-term benefits of case scenario-based learning approach in pre-clinical years on students’ clinical decision-making and their ability on performance on real cases during clinical years and future clinical practice. Finally, this study was single centered and hence, results of the study cannot be generalized; and hence, multi-centered study involving medical students at different medical universities in Oman is recommended.
Conclusion
From the findings of our study, it can be reasoned that CCPS is an effective teaching-learning strategy to encourage students’ engagement and promote their learning. It provides an opportunity to involve in active peer discussion, think critically, clarify doubts and misconceptions, deeper understanding of concepts, acquire deeper knowledge, and apply gained knowledge confidently to resolve clinical-related problems. Thus, promotes better lifelong learning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Authors would like to thank all the MD3 year students of the academic year 2021-2022 for their voluntary participation and helping us to complete the study.
References
- 1.Dankner R, Gabbay U, Leibovici L, Sadeh M, Sadetzki S. Implementation of a competency-based medical education approach in public health and epidemiology training of medical students. Isr J Health Policy Res. 2018;7:13. doi: 10.1186/s13584-017-0194-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hopper MK, Brake DA. Student engagement and higher order skill proficiency: A comparison of traditional didactic and renewed integrated active learning curricula. Adv Physiol Educ. 2018;42:685–92. doi: 10.1152/advan.00149.2018. [DOI] [PubMed] [Google Scholar]
- 3.Sakai DH, Fong SF, Shimamoto RT, Omori JS, Tam LM. Medical school hotline: Transition to clerkship week at the John A. Burns School of Medicine. Hawaii J Med Public Health. 2012;71:81–3. [PMC free article] [PubMed] [Google Scholar]
- 4.Altalhia F, Altalhia A, Magliaha Z, Abushala Z, Althaqafia A, Falemban A, et al. Development and evaluation of clinical reasoning using ‘think aloud’ approach in pharmacy undergraduates – A mixed-methods study. Saudi Pharm J. 2021;29:1250–7. doi: 10.1016/j.jsps.2021.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sannathimmappa MB, Nambiar V, Aravindakshan R. Learning out of the box: Fostering intellectual curiosity and learning skills among the medical students through gamification. J Edu Health Promot. 2022;11:79. doi: 10.4103/jehp.jehp_683_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahajan R, Badyal DK, Gupta P, Singh T. Cultivating lifelong learning skills during graduate medical training. Indian Pediatr. 2016;53:797–804. doi: 10.1007/s13312-016-0934-9. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee Y, Tuffnell C, Alkhadragy R. Mento's change model in teaching competency-based medical education. BMC Med Educ. 2019;19:472. doi: 10.1186/s12909-019-1896-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gul A, Khan RA, Yasmeen R, Ahsan NU. How case based learning promotes deep learning in preclinical years of medical students. J Ayub Med Coll Abbottabad. 2020;32:228–33. [PubMed] [Google Scholar]
- 9.Das S, Das A, Rai P, Kumar N. Case-based learning: Modern teaching tool meant for present curriculum: A behavioral analysis from faculties’ perspective. J Edu Health Promot. 2021;10:372. doi: 10.4103/jehp.jehp_1265_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ali M, Han SC, Bilal HSM, Lee S, Kang MJY, Kang BH, et al. iCBLS: An interactive case-based learning system for medical education. Int J Med Inform. 2018;109:55–69. doi: 10.1016/j.ijmedinf.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim ME, Al-Shahrani AM, Abdalla ME, Abubaker IM, Mohamed ME. The effectiveness of problem-based learning in acquisition of knowledge, soft skills during basic and preclinical sciences: Medical students’ points of view. Acta Inform Med. 2018;26:119–24. doi: 10.5455/aim.2018.26.119-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burgess A, Haq I, Bleasel J, Roberts C, Garsia R, Randalet N, et al. Team-based learning (TBL): A community of practice. BMC Med Educ. 2019;19:369. doi: 10.1186/s12909-019-1795-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sannathimmappa MB, Nambiar V, Aravindakshan R, Kumar A. Are online synchronous team-based-learning (TBL) pedagogy effective.: Perspectives from a study on medical students in Oman. J Adv Med Educ Prof. 2022;10:12–21. doi: 10.30476/JAMP.2021.92361.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sannathimmappa MB, Nambiar V, Aravindakshan R. Concept maps in immunology: A metacognitive tool to promote collaborative and meaningful learning among undergraduate medical students. J Adv Med Educ Prof. 2022;10(3):172–178. doi: 10.30476/JAMP.2022.94275.1576. doi: 10.30476/JAMP. 2022.94275.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haidaris CG, Frelinger JG. Inoculating a new generation: Immunology in medical education. Front Immunol. 2019;10:2548. doi: 10.3389/fimmu.2019.02548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Novack JP. Designing cases for case-based immunology teaching in large medical school classes. Front Immunol. 2020;11:995. doi: 10.3389/fimmu.2020.00995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sannathimmappa MB, Nambiar V, Gowda S, Aravindakshan S. Crossword puzzle: A tool for enhancing medical students’ learning in microbiology and immunology. Int J Res Med Sci. 2018;6:756–9. [Google Scholar]
- 18.McLean SF. Case-based learning and its application in medical and health-care fields: A review of worldwide literature. J Med Educ Curric Dev. 2016;3 doi: 10.4137/JMECD.S20377. JMECD.S20377. doi: 10.4137/JMECD.S20377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sangam M, Praveen K, Vinay G, Bokan RR, Deka R, Kauret A. Efficacy of case-based learning in anatomy. Cureus. 2021;13:e20472. doi: 10.7759/cureus.20472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nair SK, Rai N. Comparing the effectiveness of case based learning with conventional teaching in anatomy. Acad Anat Int. 2019;2:34–6. [Google Scholar]
- 21.Al-Drees AA, Khalil MS, Irshad M, Abdulghani HM. Students’ perception towards the problem based learning tutorial session in a system-based hybrid curriculum. Saudi Med J. 2015;36:341–8. doi: 10.15537/smj.2015.3.10216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hanse K. Basic Medical Education, WFME Global Standards for Quality Improvement. University of Copenhagen (Denmark): WFME office; 2012. THE WFME GLOBAL STANDARDS. pp. 1–46. Available from: www.wfme.org/standards .
- 23.Ghazivakili Z, Norouzi Nia R, Panahi F, Karimi M, Gholsorkhi H, Ahmadi Z. The role of critical thinking skills and learning styles of university students in their academic performance. J Adv Med Educ Prof. 2014;2:95–102. [PMC free article] [PubMed] [Google Scholar]
- 24.Jhala M, Mathur J. The association between deep learning approach and case based learning. BMC Med Educ. 2019;19:106. doi: 10.1186/s12909-019-1516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]