Abstract
Self-care may help prevent pregnancy complications and mortality by informing parents. Mobile health applications (apps) can help individuals to improve the quality of self-care. Although it has been claimed that mobile apps have various benefits, their functionalities in pregnancy self-care are still unclear. A clear understanding of current apps can help researchers, practitioners, and app developers to identify appropriate functionalities for new development and future refinement of current apps. This review endeavored to identify appropriate functions for pregnancy self-care mobile apps and user interface (UI) features. The scope of this review integrates self-care for pregnancy apps published in Google Play and Cafe Bazaar (an Iranian Android marketplace), popular Android app stores, from July to October 2019 by sing the systematic search technique. All 4196 downloaded apps were installed, and it was found that 76 of them met the inclusion criteria. This way, their features were extracted and categorized by the conventional content analysis. Three main themes and 69 subthemes in terms of apps functionalities and their UI features were extracted as follows: 1) Training materials (maternal and paternal) with 27 subthemes; 2) self-care functionalities (consultations, fetus tracking, clinical examination, supportive assistance, and reminders) with 26 subthemes; and UI features with 16 subtheme. The findings underlined the mHealth solutions for pregnancy self-care and the need for development of the apps regarding the extracted functionalities and UI features; however, controlled trials are needed. It is recommended that transparent reporting of mHealth interventions needs to be prioritized to enable effective interpretation of the extracted data.
Keywords: Mobile applications, pregnancy, self-care, telemedicine
Introduction
According to World Health Organization, approximately 830 women die from preventable grounds during pregnancy and delivery every day.[1] More than 60 million women who survive death suffer from pregnancy and delivery complications.[2] Pregnancy care seems to be a useful strategy toward reducing pregnancy risks, elevating maternal healthy lifestyle, and promoting readiness for delivery.[3] It seems that a great majority of pregnant women do not know the dose and don’ts of pregnancy.[4]
Benefits of maternal care for developing countries vary between different social classes. Some factors such as place of residence, socioeconomic status, ethnicity, education, religion, culture, need for clinical care, and decision-making ability may lead to inequalities in maternal care coverage. The costs and quality of maternal care services vary as well.[5] The cost-effective way to reduce maternal mortality and complications before/after delivery seems to break through all of the prenatal care barriers.[6] Accordingly, improving maternal health and empowering them to take care of themselves and their fetus is the prerequisite for community development.[7]
Constant self-care for pregnancy can enhance maternal health.[8] “Self-care” apps can help parents self-manage to improve their health through awareness.[9] They have the potential for promoting the potential of self-care for pregnancy.[10] Today, telemedicine, including mobile health (mHealth), supports health services and information. It has expanded as ubiquitous health care to increase universal health coverage and has led to easy access to health care, improved decision making, long-term situation management, and providing appropriate health care in emergencies.[11]
The rapid growth of mHealth apps can play an important role in the prevention and treatment of the diseases. Today, most communication and activities are done through smartphones, and in the same vein, up to 96% of physicians provide their services and track them via smartphones.[12] Such growth has also increased the use of mobile health services.[12] Across low- and middle-income countries, 83% of women own a mobile phone and 58% use mobile internet.[13] Therefore, the healthcare industry should also make efforts to employ mobile technology in this area;[14] thus, it is now increasing access to health services via mobile health apps.
Regarding pregnancy care importance and mHealth apps efficiency in lifestyle modification and health services quality improvement, it seems that the employing self-care apps during pregnancy can help improve maternal and child health. On the contrary, women's widespread access to smartphones and their desire for using mHealth apps raise the issue of how much self-care mobile apps for pregnancy have paid attention to their needs.
Objective
This study was conducted to review the current pregnancy self-care mobile apps and provided recommendations for future apps development and current apps refinement.
Materials and Methods
In this review, functionalities of pregnancy self-care mobile apps was extracted through the conventional content analysis of the apps.[15] Google Play and Cafe Bazaar, popular Android app stores, were the starting point for the search from July to October 2019 with the keywords “Prenatal”, “Gestation”, “Anticipant”, “Expectant”, “Maternity”, “Pregnancy”, “Obstetrics”, and “Gravidity”, in English and their equivalent Persian words. Seeing as app marketers do not follow the rules of search strategy, general terms in a non-hybrid way was employed for getting a comprehensive result. Limitation on the publication date was excluded from the search criteria.
Inclusion criteria
Smartphones running the Android operating system hold an 86.2% share of the global market in 2022;[16] Thus, we focused on pregnancy self-care-related apps on Android. Besides, the markets were monitored to download updates of the under-review apps, during the three months of content analysis, and three updated apps were replaced. The inclusion criteria were apps in English and Persian that were published for public access without release-time limitation to support self-care for pregnant women to avoid unnecessary obstetrical complications.
The English keywords “Prenatal”, “Gestation”, “Anticipant”, “Expectant”, “Maternity”, “Pregnancy”, “Obstetrics” and “Gravidity” and their Persian equivalent keywords were searched.
Exclusion criteria
Because the purpose of this study was to review pregnancy self-care applications, non-self-care applications were excluded. In addition, non-English and non-Persian apps were excluded. Furthermore, 25 apps got out of reach during the review, and textual training and single-task apps were excluded.
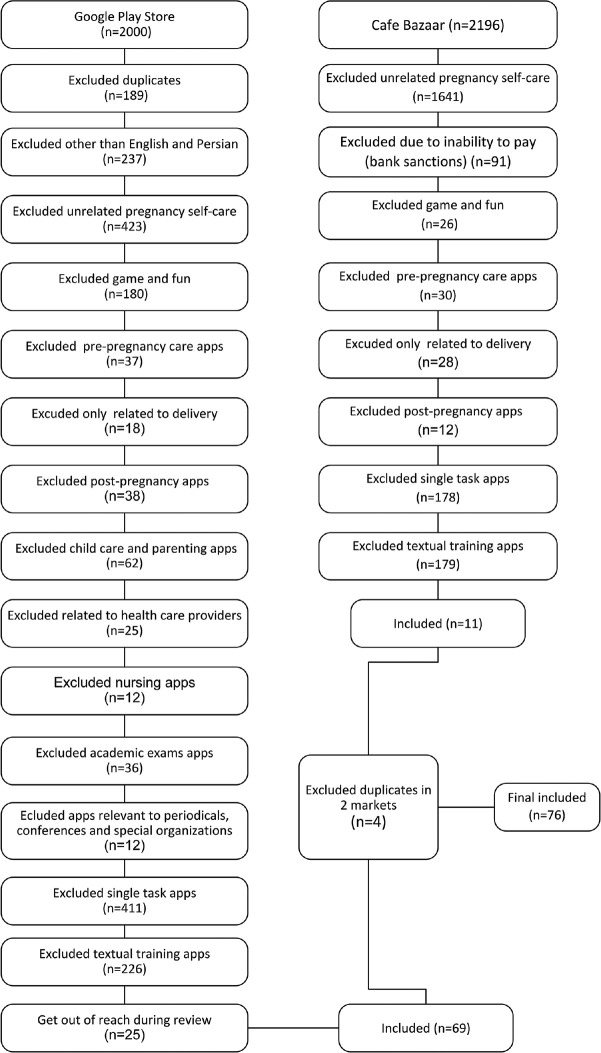
The criteria are shown in Figure 1.
Figure 1.
The trial profile for inclusion and exclusion of apps
Apps screening
During the search, 2000 and 2196 apps were found in Google Play and Cafe Bazaar, respectively, and the inclusion and exclusion criteria of the apps were reviewed according to steps shown in Figure 1. This way, the included 76 apps were divided into 66 English and 10 Persian apps [Table 1].
Table 1.
Reviewed apps related to pregnancy self-care
| Row | App name | Row | App name |
|---|---|---|---|
| 1 | Healthy Living lifestyle a Pregnancy Care | 39 | Pregnancy Tracker Week By Week |
| 2 | Pregnancy Due Date Calculator and Calendar | 40 | Pregnancy Calculators Pro |
| 3 | Pregnancy Week By Week | 41 | Best Pregnancy Videos App |
| 4 | Your Pregnancy Companion | 42 | Pregnancy app: what to expect week by week |
| 5 | BabyNet Pregnancy Tracker & Chat App | 43 | Pregnancy calculator, symptoms, signs, calendar |
| 6 | Pregnancy Calculator | 44 | Expecting: positive pregnancy with affirmations |
| 7 | Pregnancy Calculator | 45 | Pregnancy Week By Week |
| 8 | Monogram Maternity | 46 | Preggo - Antenatal, Pregnancy, Specialist Consult |
| 9 | Pregnancy Tracker + Countdown to Baby Due Date | 47 | Pregnancy Calculator |
| 10 | Pregnancy Parenting Tips: BabyCare, Moms Community | 48 | Mediclinic Baby - Baby |
| 11 | Pregnancy Mentor | 49 | My Pregnancy |
| 12 | Pregnancy Assistant | 50 | Pregnancy Tracker: Baby Due Date Calculator |
| 13 | NSH Baby Bump | 51 | Pregnancy Assistant. Pregnancy Calendar. |
| 14 | SMART PREGNANCY PLANNING GUIDES | 52 | Pregnancy Care |
| 15 | Pregnancy Garbhasanskar | 53 | Pregnancy Friend App |
| 16 | Pregnancy Tracker | 54 | Indian Pregnancy, Baby Care Tips & Conception App |
| 17 | American Pregnancy | 55 | Motherhood, Parenting & Baby Guide |
| 18 | Pregnancy Tracker. | 56 | Best of the Bump Personalized Pregnancy Tracker |
| 19 | Indian Women, Pregnancy & Childcare Community | 57 | Ovia Pregnancy Tracker: Baby Due Date Countdown |
| 20 | HMom|Pregnancy App & Due Date Calculator | 58 | Pregnancy Advice, Parenting Tips & Baby Care App |
| 21 | Pregnancy Week By Week Guide | 59 | Expecting |
| 22 | Hello Belly: Pregnancy Tracker and Baby Tips | 60 | Pregnancy Calendar and Tracker |
| 23 | Pregnancy Week by week | 61 | Pregnancy due date tracker with contraction timer |
| 24 | Pregnancy Tracker | 62 | Pregnancy and Babies |
| 25 | Pregnant2Parenting | 63 | pregnancy calendar |
| 26 | Woman Log Pregnancy Calendar | 64 | Pregnancy Tracker |
| 27 | Mother care - Pregnancy Week by Week | 65 | Pregnancy Tracker (Free) |
| 28 | Pregnancy Tracker week by week-due date calculator | 66 | Garbh Sanskar Guru - Best companion 4 pregnancy |
| 29 | Lincus Maternity | 67 | Preg/Bardari/Mamaye-Hamrahe-Shomaa |
| 30 | UNC REX Pregnancy & Baby | 68 | Niniban |
| 31 | Healthy pregnancy | 69 | Nini plus |
| 32 | Infano: Period, Fertility, Ovulation & Pregnancy App | 70 | Nini center |
| 33 | Week by Week Pregnancy App. Contraction timer | 71 | Bardari (Nahal) |
| 34 | Pocket Gynecologist | 72 | Madar sho |
| 35 | Pregnancy Week By Week pics with guide | 73 | Farzande Nikoo |
| 36 | Woman’s Pregnancy | 74 | Mamana plus |
| 37 | Pregnancy tracker and chat support for new moms | 75 | Man, nini va bardari |
| 38 | Pregnancy Tracker | 76 | Noko |
aApps in rows 67-76 are in Persian
Data extraction and classification
Each app description was reviewed to be installed and examined to extract its functionalities and features through a conventional content analysis approach. Initially, extracted functionalities were extracted and a decision was made regarding their titles. In the second step, the functionalities and features were categorized and decided on the titles of each group. In the third step, titles, categorizations, and their relations were refined, verified, and updated. We tried to resolve any disagreement of researchers by discussing, reviewing, and reconciling the data; this way, an agreement was reached.
Ethical code and ethical considerations
Ethical issues (plagiarism, misconduct, data fabrication and falsification, double publication and submission, redundancy, etc.) have been completely observed. Moreover, this study received the required ethics approval from Isfahan University of Medical Sciences Research Ethics Committee, Isfahan, Iran with ethical code number: IR.MUI.RESEARCH.REC.1398.681.
Results
Mobile apps for pregnancy care have been developed according to the needs of three categories of users: (a) medical, nursing, and midwifery students; (b) pregnant women; and (c) pregnancy care providers. In terms of content, they are divided into five categories: (a) pre-pregnancy issues, (b) pregnancy care, (c) maternity, (d) postpartum care, and (e) parenting. Their training content may also be developed taking into account two approaches: non-interactive or interactive.
As tabulated in Tables 2-4, three themes and 69 subthemes were identified from existing apps.
Table 2.
The extracted training functionalities of pregnancy self-care mobile apps
| Training Function | Function Description |
|---|---|
| Maternal | |
| Health care | Such as complete vaccination, dental and gum hygiene, skin and hair care, bathing, proper maternity clothes, and use of cosmetics |
| Physical activity | Travel: Tips for travel and entertainment during pregnancy Working conditions: Tips for adapting to the work environment during pregnancy Sleep: Including changes in sleep patterns in pregnancy Exercise in pregnancy: Suggestions about the type of exercise, its duration, and intensity (in photos or videos format) during pregnancy |
| Nutrition | Weight tracking: Tips for gaining weight during pregnancy, and investigating the relationship between overall weight gain and gestational age Proper and varied nutrition: Proper and varied nutrition Cooking recipe: Cooking the right foods for pregnant women Medications and supplements: Introducing how to take medications and supplements such as iron, folic acid, and the like |
| Common complications | Changes in the mother’s body: Hormonal changes during pregnancy and following that, common changes in blood oxygen level, temperature, skin, hair and nails, heart rate, breasts, cervix, and lumbar spine curvature |
| High-risk complications | Pregnancy risk factors: Including visual disorders, dyspnea, vaginal bleeding, fever, edema, preterm delivery, gestational diabetes, thyroid disorders, urinary tract infection, and strangury as well as tips on significant problems in pregnancy, including back pain, abdominal pain, and leg pain Other dangerous signs: Including BMI<18.5 or>35, cancer, epilepsy, age >35 or <17, twin or multiple pregnancies, history of more than 3 abortions, personal or family history of birth with congenital anomalies, history of preterm labor, infectious diseases such as HIV or hepatitis C, and itching all over the body |
| Common diseases of pregnant women | Hypertension: Tips on gestational hypertension and chronic pre-pregnancy hypertension and its timely control Pregnancy loss: Abortion, molar pregnancy, fetal death, and re-attempt to conceive Diabetes screening: Tips for gestational diabetes screening Other diseases: Including relatively common pregnancy-related diseases such as heart and liver disease, varicose veins, and hemorrhoids |
| Screening and tests | Including a description of blood and urine tests, genetic screening and anomalies, and deadline of each test |
| Preventive care | Fetal growth: Descriptions of fetal growth, development, and changes Complications and their solutions: Introducing pregnancy complications and ways to reduce them Lifestyle: Materials such as intercourse, sleeping positions, keeping pets, and other tips of coexistence in the family during pregnancy Vaccination: Time and method of vaccination |
| Mental Health | Feelings and emotions changes: Including changes in thoughts, feelings, and psyche during pregnancy Religious advice: Consists of religious memoirs, surahs, and prayers for pregnancy and the time of reciting them Music: Listening to quiet and simple music to stimulate fetal heart rate and to increase endorphin |
| Paternal | |
| Fathers training | Tips on accompanying the spouse to receive pregnancy care, participating in home affairs, providing health advice to pregnant women, empowering her to promote reproductive-sexual health to reduce mortality, improving her health, and reducing inequalities |
Table 4.
The extracted UI features of pregnancy self-care mobile apps
| UI Feature | Feature Description |
|---|---|
| Input Controls | Feedback: Sending feedback on all sections of the app to the developer |
| Navigational Components | Search: Searching all content for easier access to the intended one |
| Informational Components | About: Consist of the purpose of the app, its developers, and user contact with them Notifications: Send training or motivational announcements Messaging: Ability to send content related to each week for pregnant women Birthday widget: Counting of days left to birth and providing information about fetal imaging Q&A capability: forum with specialists and mothers |
| Setting | Units setting: Such as selecting weight and height units Appearance setting: Such as font, color, and others Input setting: Such as language and keyboard Account setting: Assigning a user account and setting up a personal profile Offline running: Running the app continuously without an internet connection Setting personal archives: Ability to create personal archives of mothers favorite content |
| Support | Backup: Data backup Update: App update and upgrade |
| Share | Sharing data with specialists and caregivers |
Table 3.
The extracted Self-care functionalities of pregnancy self-care mobile apps
| Self-care Function | Function Description |
|---|---|
| Constant consultations | Breath exercises: Doing the right breathing exercises Mental health: Asking questions about the mother’s mood and sending the right motivational message to her Signs and symptoms: Entering daily signs and symptoms and managing common or high-risk pregnancy conditions Daily care: Includes evaluation of high-risk behaviors, common complaints and danger signs, trauma, general maternal condition, physical examination, and personal hygiene Blood sugar & gestational diabetes: Pregnancy blood sugar checking Sleep hours: Tracking mother’s daily sleep hours Weight and diet: Tracking mother’s weight based on calories consumed on a daily basis Physical activity: Tracking amount of pregnancy exercise, yoga, or walking on a daily basis Medications: Mothers’ medications and supplements data entry to consult Abdomen size: Recording abdominal circumference and fetal growth rate according to gestational age Temperament: Basal body temperature increasing Heart rate: Checking the mother’s daily heart rate Blood pressure: Blood pressure screening for hypertensive care |
| Track the fetus’s condition | Blood group prediction: Fetus blood group prediction based on the parents’ blood group Kicks counting and checking fetal movement: Monitoring fetus health by paying attention to its movements, continuous recording of fetal movements attributes such as its duration and intervals Illustrating fetal size with various objects: Showing fetal size based on its resemblance to fruits, vegetables, or objects tangible to parents for easier understanding Calculating fetal age and its weekly growth: Calculating gestational age, fetal size, and weight, in weeks, millimeters, and grams, respectively, based on the date of the last menstrual period. Uterine contraction timer: Controlling uterine contractions and alert delivery date |
| Reminders | Appointment: Doctors and midwives visit reminding Medications administration: Medications reminding Tests: Clinical tests reminding Note writing: Daily notes writing and documenting previous and current pregnancies records Sonography: Sonography reminding |
| Clinical examination | Examining mother’s medical conditions |
| Supportive assistance | Helping to choose a proper clinician Emergency call |
Discussion
The study endeavored to explore the proper functionalities and features of mobile apps for pregnancy self-care. In effect, self-care for pregnancy requires women's active participation in identifying and managing their conditions. Although many studied apps play an important role in pregnancy self-care, they cannot fully meet women's needs in a comprehensive way. According to Daly et al.,[17] women are looking for apps to access information and monitor maternal and fetal health; 75% of them have downloaded at least a pregnancy app and most of them utilize at least one app every week.
Iyawa et al. conducted a systematic review to provide a narrative synthesis of the literature on the evaluation of mobile apps for self-management during pregnancy by using four databases (PubMed, CINAHL, Scopus, and EMBASE) and concluded that mobile apps for self-management have been developed with different functionalities addressing various areas of complications during pregnancy, including gestational diabetes, preeclampsia, and high blood pressure.[3]
This review has some implications and outcomes that can greatly contribute to pregnancy care providers in developing new apps or updating the current apps to achieve their real benefits. Some highlighted findings are discussed as follows:
Pregnancy care includes an integrated approach to medical and psychosocial care; therefore, these apps should also cover their comprehensive self-care needs in aspects of pregnancy such as family, social, psychological, religious, and conventional medicine. Most apps teach day-to-day care, while the psychological and emotional dimensions such as parental and emotional support are deficient.
User training is one of the pregnancy self-care apps functionalities in maternal, fetal, and child health care; postpartum care; and paternal training. According to Leiferman et al.,[18] online training can facilitate prenatal depression management through patient-provider dialogue improvement. Moreover, according to Alio et al.,[19] paternal engagement may affect infant mortality through the mother's access to resources, support, and her well-being.
Maternal perception of fetal growth and bonding with it, is another functionality of self-care apps. In the words of Warrander et al.,[20] it may help decrease the risk of stillbirth and fetal growth restriction.
Daily care consultation is one of the pregnancy apps functionalities. Alam et al's[21] findings reveal that mobile consultation provides pregnant women with valued medical advice and support.
Medication and medical non-adherence are one of the major concerns of pregnant women that can disproportionately undermine their status quo.[22,23] Pregnancy self-care apps can provide reminders about medical appointments, medication administration, tests, and note writing.
Wulff et al.[24] believe that stress and impaired mother-fetus bonding can lead to maternal and fetal adverse effects. Music in prenatal term can facilitate maternal mood and health and support maternal-fetal bonding. Self-care apps for pregnancy can work to stimulate the fetal heart rate as well as mother endorphin secretion by playing music during pregnancy.
According to Dawod et al.,[25] maternal care history documentation can decrease some risk factors and increase parental bonding. Therefore, it seems to be an important functionality of self-care apps for pregnancy.
Like any other user-friendly self-care app for pregnancy, there are UI features in pregnancy self-care apps. Zargarzadeh's findings revealed that some UI features are important, such as setting, feedback, rating, data sharing and backup, running without Internet connection, updating, sending daily and weekly emails, and a search option.[10]
Conclusion
In conclusion, three main themes and 69 subthemes were presented for pregnancy self-care-related app functionality and their UI features, with huge heterogeneity of functions in different apps. This can be due to the various development approaches. mHealth solutions can improve pregnancy self-care services, but due to the weak current literature, RCTs with economic, clinical, and long-term patient-centered outcomes are suggested. Moreover, it seems that if transparent reporting of mHealth pregnancy self-care interventions is a priority, effective interpretation of the extracted data Moreover to be provided. With the growing penetration of smartphones, new generations of mobile apps are emerging that require user-friendly and evidence-based methods to build their safety, performance, and social impact.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This article was a part of M.Sc. thesis supported by Isfahan University of Medical Sciences (IUMS). Grant no. 298188.
References
- 1.Khanum S, de Souza MdL, Sayyed A, Naz N. Designing a pregnancy care network for pregnant women. Technologies. 2017;5:80. [Google Scholar]
- 2.Dehkordi ZR, Kohan S, Rassouli M, Zarean E. Developing a perinatal palliative care service package for women with fetal anomaly diagnosis: Protocol for mixed methods study. Reprod Health. 2020;17:1–6. doi: 10.1186/s12978-020-0881-8. doi: 10.1186/s12978-020-0881-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iyawa GE, Dansharif AR, Khan A. Mobile apps for self-management in pregnancy: A systematic review. Health Technol. 2021;11:283–94. [Google Scholar]
- 4.Nkamba DM, Wembodinga G, Bernard P, Ditekemena J, Robert A. Awareness of obstetric danger signs among pregnant women in the Democratic Republic of Congo: Evidence from a nationwide cross-sectional study. BMC Women Health. 2021;21:1–12. doi: 10.1186/s12905-021-01234-3. doi: 10.1186/s12905-021-01234-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doyle K, Kazimbaya S, Levtov R, Banerjee J, Betron M, Sethi R, et al. The relationship between inequitable gender norms and provider attitudes and quality of care in maternal health services in Rwanda: A mixed methods study. BMC Pregnancy Childbirth. 2021;21:1–15. doi: 10.1186/s12884-021-03592-0. doi: 10.1186/s12884-021-03592-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Soubeiga D, Gauvin L, Hatem MA, Johri M. Birth preparedness and complication readiness (BPCR) interventions to reduce maternal and neonatal mortality in developing countries: Systematic review and meta-analysis. BMC Pregnancy Childbirth. 2014;14:1–11. doi: 10.1186/1471-2393-14-129. doi: 10.1186/1471-2393-14-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tibandebage P, Kida T, Mackintosh M, Ikingura J. Can managers empower nurse-midwives to improve maternal health care? A comparison of two resource-poor hospitals in Tanzania. Int J Health Plan Manag. 2016;31:379–95. doi: 10.1002/hpm.2279. [DOI] [PubMed] [Google Scholar]
- 8.Gülmezoglu AM, Ammerdorffer A, Narasimhan M, Wilson AN, Vogel JP, Say L, et al. Self-care and remote care during pregnancy: A new paradigm? Health Res Policy Syst. 2020;18:1–3. doi: 10.1186/s12961-020-00627-4. doi: 10.1186/s12961-020-00627-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong AKC, Wong FKY, Chang KKP. A proactive mobile health application program for promoting self-care health management among older adults in the community: Study protocol of a three-arm randomized controlled trial. Gerontology. 2020;66:506–13. doi: 10.1159/000509129. [DOI] [PubMed] [Google Scholar]
- 10.Zargarzadeh P, Ehteshami A, Mohammadi-Sichani M. A contribution into developing a model for prostate cancer self-care mobile application. Med Arch. 2018;72:344–7. doi: 10.5455/medarh.2018.72.344-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Varshney U. Mobile health: Four emerging themes of research. Decis Support Syst. 2014;66:20–35. [Google Scholar]
- 12.Patoz M-C, Hidalgo-Mazzei D, Blanc O, Verdolini N, Pacchiarotti I, Murru A, et al. Patient and physician perspectives of a smartphone application for depression: A qualitative study. BMC Psychiatry. 2021;21:1–12. doi: 10.1186/s12888-021-03064-x. doi: 10.1186/s12888-021-03064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carboni I, Jeffrie N, Lindsey D, Shanahan M, Sibthorpe C, Butler C, et al. Vol. 7. UK: GSMA Intelligence; 2021. Connected Women-The Mobile Gender Gap Report 2021. [Google Scholar]
- 14.Feroz A, Perveen S, Aftab W. Role of mHealth applications for improving antenatal and postnatal care in low and middle income countries: A systematic review. BMC Health Serv Res. 2017;17:1–11. doi: 10.1186/s12913-017-2664-7. doi: 10.1186/s12913-017-2664-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 16.Share of global smartphone shipments by operating system from 2014 to 2023. 2022. Available from: https://www.statista.com/statistics/272307/market-share-forecast-for-smartphone-operating-systems/
- 17.Daly LM, Horey D, Middleton PF, Boyle FM, Flenady V. The effect of mobile application interventions on influencing healthy maternal behaviour and improving perinatal health outcomes: A systematic review protocol. Syst Rev. 2017;6:1–8. doi: 10.1186/s13643-017-0424-8. doi: 10.1186/s13643-017-0424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leiferman JA, Farewell CV, Lee-Winn AE, Jewell J, Ulrickson C, Huberty J, et al. Management of prenatal depression: Effectiveness of an online training module across health care disciplines. J Contin Educ Health Prof. 2019;39:178–84. doi: 10.1097/CEH.0000000000000263. [DOI] [PubMed] [Google Scholar]
- 19.Alio AP, Bond MJ, Padilla YC, Heidelbaugh JJ, Lu M, Parker WJ. Addressing policy barriers to paternal involvement during pregnancy. Matern Child Health J. 2011;15:425–30. doi: 10.1007/s10995-011-0781-1. [DOI] [PubMed] [Google Scholar]
- 20.Warrander LK, Batra G, Bernatavicius G, Greenwood SL, Dutton P, Jones RL, et al. Maternal perception of reduced fetal movements is associated with altered placental structure and function. PloS One. 2012;7:e34851. doi: 10.1371/journal.pone.0034851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alam M, Banwell C, Olsen A, Lokuge K. Patients’ and doctors’ perceptions of a mobile phone–based consultation service for maternal, neonatal, and infant health care in Bangladesh: A mixed-methods study. JMIR Mhealth Uhealth. 2019;7:e11842. doi: 10.2196/11842. doi: 10.2196/11842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saghaeiannejad-Isfahani S, Sharifi-Rad J, Raeisi A, Ehteshami A, Mirzaeian R. An evaluation of adherence to society of pharmacists’ standards care in pharmacy information systems in Iran. Indian J Pharmacol. 2015;47:190–4. doi: 10.4103/0253-7613.153428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saghaeiannejad-Isfahani S, Ehteshami A, Savari E, Samimi A. Developing the medication reminder mobile application “Seeb”. Acta Inform Med. 2017;25:108–11. doi: 10.5455/aim.2017.25.108-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wulff V, Hepp P, Wolf OT, Balan P, Hagenbeck C, Fehm T, et al. The effects of a music and singing intervention during pregnancy on maternal well-being and mother–infant bonding: A randomised, controlled study. Arch Gynecol Obstet. 2021;303:69–83. doi: 10.1007/s00404-020-05727-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dawod SB, Ali RM, Bahaaldeen EF. Effectiveness of an educational program concerning nurse-midwives knowledge concerning SBAR (situation, background, assessment, recommendation) tool communication on maternal health documentation. EXECUTIVE EDITOR. 2018;9:237. [Google Scholar]