Abstract
BACKGROUND:
Due to the role of education in improving anxiety and essential skills of mothers for caring for their infants, this study aimed to investigate the effect of education based on the health belief model (HBM) on anxiety among mothers of infants with retinopathy of prematurity (ROP).
MATERIALS AND METHODS:
This randomized controlled clinical trial was performed on 67 mothers with premature infants admitted to the ROP unit of Khatam Al Anbia Eye Hospital in Mashhad, Iran from 2019 to 2020. Participants were randomly allocated to intervention and control groups. Intervention was designed based on HBM during six sessions, each of 45–60 minutes duration. The control group received routine educations according to the hospital policies. The maternal anxiety, adherence with follow-up examinations and the rate of neonatal retinal vascularization were evaluated using an HBM- based questionnaire and State-Trait Anxiety Inventory questionnaire and checklists, respectively. Data was analyzed by using SPSS software, version 16, using Chi-squared test, Fisher's exact test, independent t test, and Mann–Whitney U test.
RESULTS:
Based on our findings, no significant difference was observed between the two groups before the intervention regarding the mean score of maternal anxiety (P = 0.141). However, after intervention, the mean score of maternal anxiety decreased significantly from 67.0 ± 6.3 to 38.5 ± 6.6 in the intervention group and increased from 69.8 ± 3.1 to 68.3 ± 3.4 in the control group (P < 0.001). In the intervention group, the mean scores of model constructs (perceived susceptibility and severity, perceived benefits, barriers, self-efficacy and cue to action) increased significantly after intervention (P < 0.001).
CONCLUSIONS:
Education based on HBM appear to be an efficient method to improve maternal anxiety among mothers of infants with retinopathy of prematurity. Accordingly, nurses and treatment staff can provide interventions in the NICU based on the HBM to the parents of hospitalized and premature infants.
Keywords: Anxiety, education, health belief model, mother-infant relations, premature infant
Introduction
Retinopathy of prematurity (ROP) is a serious problem among premature low birth weight infants.[1] ROP is a retinal vascular disorder that severely affects premature infants and is caused by abnormal blood vessel growth in the retina followed by abnormal vascular proliferation at birth.[2] ROP sometimes progresses very quickly, and delays in examinations, even for a few days, can lead to vision loss. For these reasons, timely diagnosis and treatment play a very important role in the rehabilitation of sight and vision of infants, and the emphasis on periodic examinations is especially necessary for parents. Visual impairment and blindness in infants impose a heavy psychological and physical burden on the child and it's a great tragedy for the family and society.[3]
The prevalence of ROP in newborns weighing less than 1,251 grams is reported to be 68% in the United States.[4] According to some studies, the prevalence of ROP in different regions of Iran varies from 1% to 70%.[5,6,7,8] The negative feeling of parents of premature infants, such as that their infant is vulnerable to any illness, may cause the sense of powerlessness and impairment resulting in a change in the parental role, and it could also increase anxiety and depression.[9,10,11] This attitude leads parents to inappropriate interaction with infants. It has been found that feelings of stress are associated with a decrease in maternal love and responsibilities, and can spread to babies.[12,13] Nurses play a critical role in assisting parents with premature infants; it is because during hospitalization of the infants, they are in connection with parents more than any other person, and also, they are more aware of the infant's status.[14] Studies show that mothers who have been supervised by communication and learning programs in the nursing system have less stress than mothers who have not learned these skills.[15] Considering that health education based on patterns can be effective in adoption of health behaviors, choosing a health education model is the first step in the process of designing a health education research program.[16]
One of the patterns is the health belief model (HBM) that can be used to design appropriate educational interventions for determining the relationship between health beliefs and behavior.[17] HBM is the most important model implemented in the development and design of prevention programs and is one of the patterns of education and behavior change of people at risk which is widely used by health educators.[18] The HBM has six constructs including: perceived sensitivity (a person's subjective perception of a risk of getting illness), perceived severity (a person's feelings on the seriousness of a disease), perceived benefits (a person's perception of the effectiveness of various methods for reducing the risk or severity of disease), perceived barriers (a person's feelings on the barriers such as costs to performing a health action), cue to action (a stimulus that makes one feel the need to do something), self-efficacy (a person's confidence in his or her ability to perform a behavior).[9] Many studies have been performed in different communities including patients, pregnant mothers, etc., which has shown the positive effect of HBM in reducing anxiety.[19,20,21,22]
Considering the 10-year history of working in Khatam Al Anbia Eye Hospital in Mashhad, we realized that most parents are not aware of the complications of anxiety and delayed the follow-up examination; so the researcher intends to create appropriate care behavior by creating perceived sensitivity and threat in parents. Therefore, the HBM is a suitable method in designing the intervention.
As far as we know, there is no written program for parents of infants with ROP in the country, and no research has been done on training parents in this regard. The aim of the present study was that parents with regular visits for follow-up examinations, in addition to reducing the complications of ROP, also reduce their anxiety and are able to care for their infants.
Material and Methods
Study design and setting
This study was a double-blind, randomized, controlled trial with a pre-test and post-test design. The study population consisted of mothers who had their infants admitted to the ROP unit of Khatam Al Anbia Eye Hospital in Mashhad, Iran from 2019 to 2020.
The inclusion criteria for mothers included: written consent to participate in the study, being able to read and write, no depression or anxiety disorder confirmed by a specialist doctor during the study, women who never had a pre-term infant, and lack of moderate or high level of hidden anxiety. Exclusion criteria included reluctance to continue cooperation, more than one absence in training sessions, severe stressful events such as the death of first-degree relatives, divorce, or severe family disputes.
The inclusion criteria for infants included newborns with a gestational age of 34 weeks (33 weeks and 6 days), infants who had zone II and stage 2 involvement in the first retinal screening examination, no severe asphyxia and major congenital anomalies. The exclusion criteria included infant death, hospitalization in NICU, respiratory distress syndrome, and the need for mechanical ventilation.
Study participants and sampling
Screening examination for all infants referred to the ROP unit was performed by a retinal specialist, and infants with ROP stage 2 were introduced to the researcher. The first-time retinal examination was performed based on gestational age at birth.[23] The specialist was blinded about the groups until the end of the study.
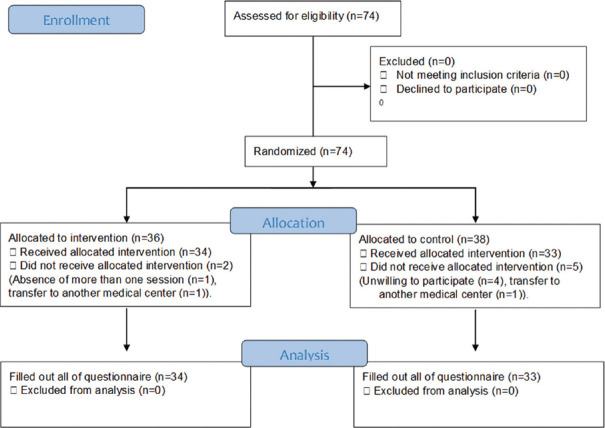
The researcher consulted in person with the parents of newborns who were referred to the premature neonatal clinic for screening for ROP. Of the 74 mothers who's own and their infant met the inclusion criteria, 67 participants (34 infants and their mothers in the intervention group and 33 infants and their mothers in the control group) were enrolled, using simple sampling method [see Figure 1]. By lot, even days were assigned to the intervention group and odd days to the control group.
Figure 1.
Flow of participants through each stage of the program
Data collection tools
A demographic characteristics form that included age, education, occupation, economic status, weight, number of children, insurance status was used.
A researcher-made HBM-based questionnaire in Persian: This questionnaire comprised of 34 questions based on six HBM constructs including six questions on perceived susceptibility, perceived severity (six questions), perceived benefits (four questions), perceived barriers (nine questions), cues to action (four questions), and self-efficacy (five questions). Likert scoring method was used to assess the answers as follows: (certainly agree = 4, agree = 3, no idea = 2, disagree = 1, and certainly disagree = 0) with a score range of 23–115.
The validity of this tool was examined by seven academic expert members of Mashhad School of Nursing and Midwifery. Some modification was made based on their opinions until it became acceptable.
The internal consistency method (Cronbach's alpha coefficient) was used by conducting a pilot study on 10 parents in one test. Cronbach's alpha for the whole questionnaire was calculated to be 89%, which was acceptable.
State-Trait Anxiety Inventory (STAI): This questionnaire was designed by Spielberger in 1970 and revised in 1983.[24] It consists of 40 questions with Likert score, of which 20 are related to the state anxiety subscale and another 20 to the trait anxiety subscale. Scoring is reversed for expressions that indicate no anxiety. Anxiety scores ranged from 20–73 with different rangers indicating different levels: 20–31 for mild anxiety; 32–42 for moderate-to-low anxiety; 43–53 for moderate-to-high anxiety; 53–62 for relatively severe anxiety; 63–72 for severe anxiety; and ≥73 for very severe anxiety. Parents whose latent anxiety levels were not moderate to high (<42) were included in the study.
Content validity and reliability were assessed as mentioned about HBM-based questionnaire; a Cronbach's alpha of 0.91 was obtained which was acceptable.
Regular check-up checklist: This checklist was prepared in accordance with the national executive regulations of retinopathy care in premature infants for the next examination of the newborn. The parents’ adherence to the mentioned schedule was evaluated by the opinion of the retinal specialist in the intervention and control group. After the first examination, based on the zone (maximum area with normal blood vessels) and stage of the disease, the examination intervals were determined. It was performed 5 days a week and in the morning shift. Evaluation of attendance for follow-up examinations included referral exactly on the day of examination, referral with telephone reminder with 1–2 days delay, with 3 days to one week delay, with more than one week delay, and non-referral despite the phone reminder.
Checklist for evaluation of retinal vascularization status in preterm infants: The rate of retinal vascularization from the first examination was monitored (by the retina specialist) until the complete retinal vascularization, according to the time interval determined by the retinal specialist (based on the zone and stage of the disease). Data analysis was based on the number of weeks that vascularization was completed.
Ethical consideration
This study was conducted after the approval and permission of Mashhad University of Medical Sciences Research Committee IR.MUMS.NURSE.REC.1398.089 and was conducted with consideration of Helsinki Declaration in all phases of the study. Confidential data treatment was guaranteed.
Implementation
The researcher visited the parents and explained the purpose of the study for the participants. Informed consent and demographic information form were given to the mothers. Then the HBM and anxiety questionnaires were completed by participants.
The control group was given routine education provided by the hospital including education and answering the questions of parents by a nurse working in the pre-term infant clinic.
In the intervention group, 6 sessions of 45–60 minutes each were performed in the form of lectures, group discussions, questions and answers, videos and slides. The content of the training included empowering mothers to comply with treatment, attendance for follow-up examinations, care needs of premature infants, controlling infant pain during eye exams, infant sleep and feeding patterns, and managing stress and anxiety in parents.
According to the results of the HBM questionnaire in the pre-test stage, the constructs of perceived barriers and perceived sensitivity were considered more than other constructs. The designed intervention in the form of a health belief model are shown in Table 1.
Table 1.
The designed intervention in the form of a health belief model
| Steps | Objectives | Educational method | Details |
|---|---|---|---|
| First | Increased perceived susceptibility | Group discussion, lecture, questions and answers, PowerPoint, educational pamphlet | Introduction to ROP and its symptoms, complications and diagnosis |
| Second | Increased perceived severity | Posters, movies | Showing videos of babies who have become blind |
| Third | Promotion of perceived benefits | Group discussion, sharing positive results, video playback | Follow-up examinations reduce your baby’s odds of developing eye complications and make you experience less anxiety. Also significantly reduce treatment costs. |
| Forth | eliminate perceived barriers | Questions and answers about perceived barriers and overview of practical solutions | Adherence to the baby’s eye examination schedule takes a little time. These examinations are simple and without side effects. |
| Fifth | Introducing cues to action | Posters, pamphlets, cyberspace, telephone consultation | Giving a pamphlet to the parents and asking the mother to encourage her husband to come in time, create a telegram group and send a message in it |
| Sixth | Promotion of self-efficacy | Practical demonstration, repetition and practice | Showing an educational video on how to take care of the baby |
Data analysis
In this study, descriptive analysis was performed using mean score and standard deviation (SD). Data was analyzed using Chi-squared test, Fisher's exact test, independent t test, and Mann–Whitney U test in SPSS version 16 (SPSS, Inc., USA). A P value lower than 0.05 was considered statistically significant.
Results
The study results showed that there was no significant difference between the two groups in terms of demographic variables before intervention (P > 0.05). The mean age of the mothers were 29.85 ± 7.17 years. The majority had elementary education (n = 24, 35.8%), were housewife (n = 52, 77.6%), poor in terms of economic conditions (n = 19, 28.3%), had one child (n = 24, 35.8%) and were without insurance coverage (n = 36, 53.7%).
A majority of neonates were boys (n = 36, 53.7%), with a mean birth weight of 1877.16 ± 296.88 grams. The infant's age and weight in the first screening of retinal disease of pre-term infant were 38.53 ± 0.5 weeks and 2522.16 ± 498.68 grams, respectively. The average hospitalization in NICU for the intervention group was 2.49 ± 2.47 days. Moreover, 95.5% of neonates did not have ventilation. The infant's age was reported to be 34 weeks of pregnancy in both groups. More details are shown in Table 2.
Table 2.
Demographic variables of infants and mothers in two groups before training
| Variables | Intervention n=34 | Control n=33 | Total n=67 | P |
|---|---|---|---|---|
| Mother’s factors | ||||
| Mother’s age (mean±SD) | 31.8±7.6 | 27.8±6.2 | 29.85±7.17 | 0.081* |
| Mother’s education, n (%) | ||||
| Elementary | 10 (29.4) | 14 (42.4) | 24 (35.8) | 0.517† |
| High school | 5 (14.7) | 4 (12.1) | 9 (13.4) | |
| Diploma | 7 (20.6) | 6 (18.2) | 13 (19.4) | |
| College degree | 12 (35.3) | 9 (27.3) | 21 (31.4) | |
| Mother’s occupation, n (%) | ||||
| Housewife | 28 (82.4) | 24 (72.7) | 52 (77.6) | 0.611†† |
| Employee | 4 (11.8) | 6 (18.2) | 10 (14.9) | |
| Others | 2 (5.9) | 3 (9.11) | 5 (7.5) | |
| Economic status, n (%) | ||||
| Excellent | 10 (29.4) | 7 (21.2) | 17 (25.4) | 0.964† |
| Good | 7 (20.6) | 9 (27.3) | 16 (23.9) | |
| Moderate | 6 (17.6) | 9 (27.3) | 15 (22.4) | |
| Poor | 11 (32.4) | 8 (24.2) | 19 (28.3) | |
| Numbers of children, n (%) | ||||
| One | 10 (29.4) | 14 (42.4) | 24 (35.8) | 0.078† |
| Two | 10 (29.4) | 13 (39.4) | 23 (34.4) | |
| Three | 7 (20.6) | 3 (9.1) | 10 (14.9) | |
| Four and more | 7 (20.6) | 3 (9.1) | 10 (14.9) | |
| Insurance status, n (%) | ||||
| With insurance | 15 (44.1) | 16 (48.5) | 31 (46.3) | 0.720†† |
| Without insurance | 19 (55.9) | 17 (51.5) | 36 (53.7) | |
| Infant’s factor | ||||
| Sex of infants, n (%) | ||||
| Female | 17 (50.00) | 14 (42.4) | 31 (46.3) | 0.534†† |
| Male | 17 (50.00) | 19 (57.6) | 36 (53.7) | |
| Birth weight (gram), (mean±SD) | 1893.2±275.0 | 1860.6±321.4 | 1877.16±296.88 | 0.656* |
| Infant’s age in first screening (week) | 38.6±0.5 | 38.5±0.5 | 38.53±0.5 | 0.400† |
| Infant’s weight in first screening (grams), (mean±SD) | 2518.2±387.5 | 2526.2±598.4 | 2522.16±498.68 | 0.725† |
| Duration of ventilation (day), n (%) | ||||
| 0 | 33 (97.1) | 31 (93.9) | 64 (95.5) | 0.742†† |
| 2 | 0 (1) | 1 (3.0) | 1 (1.5) | |
| 3 | 1 (2.9) | 1 (3.0) | 2 (3) | |
| Days in NICU, (mean±SD) | 3.6±1.7 | 3.5±2.8 | 2.49±2.47 | 0.111† |
| Mode of delivery, n (%) | ||||
| Cesarean delivery | 16 (47.1) | 17 (51.5) | 33 (49.3) | 0.440†† |
| Normal delivery | 18 (52.9) | 16 (48.5) | 34 (50.7) |
*Independent t-test, †Mann-Whitney U test, ††Chi-squared test
In the intervention group, the mean scores of maternal anxieties before and after the intervention were 67.0 ± 6.3 and 38.5 ± 6.6, respectively. In the control group, the mean scores of maternal anxieties before and after the intervention were 69.8 ± 3.1 and 68.3 ± 3.4, respectively. No significant difference was observed between the two groups before the intervention regarding the mean score of maternal anxiety (P > 0.05). However, the difference between the two groups regarding the premature infants’ maternal anxiety was significant after the intervention [Table 3].
Table 3.
The mean of maternal anxiety and the HBM constructs before and after intervention in both groups
| Variables | Group | Before intervention (mean±SD) | After intervention (mean±SD) | P |
|---|---|---|---|---|
| Maternal anxiety score | Intervention | 67.0±6.3 | 38.5±6.6 | <0.001† |
| Control | 69.8±3.1 | 68.3±3.4 | 0.89** | |
| Intra group test results | 0.141†† | <0.001†† | ||
| Health Belief Model Constructs | ||||
| Perceived susceptibility | Intervention | 17.4±2.6 | 25.3±0.9 | <0.001* |
| Control | 17.2±2.3 | 18.0±2.2 | 0.206† | |
| Intra group test results | 0.815 | <0.001 | ||
| Perceived severity | Intervention | 21.0±4.0 | 27.6±1.1 | <0.001† |
| Control | 20.6±4.1 | 20.3±2.3 | 0.461† | |
| Intra group test results | 0.552 | <0.001 | ||
| Perceived benefits | Intervention | 15.5±0.6 | 19.6±0.8 | <0.001† |
| Control | 15.5±2.5 | 15.6±1.5 | 0.644† | |
| Intra group test results | 0.155 | <0.001 | ||
| Perceived barriers | Intervention | 24.9±3.1 | 40.6±2.3 | <0.001† |
| Control | 26.0±7.7 | 24.9±4.6 | 0.576† | |
| Intra group test results | 0.905 | <0.001 | ||
| Cues to action | Intervention | 13.4±0.9 | 19.2±0.9 | <0.001† |
| Control | 13.3±2.7 | 14.2±0.9 | 0.073† | |
| Intra group test results | 0.702 | <0.001 | ||
| Self-efficacy | Intervention | 14.6±1.5 | 22.0±0.9 | <0.001† |
| Control | 13.8±3.4 | 14.2±5.4 | 0.857† | |
| Intra group test results | 0.372 | <0.001 | ||
| Total score of HBM of mothers | Intervention | 106.7±4.6 | 154.2±3.6 | <0.001† |
| Control | 106.5±6.0 | 107.2±4.3 | 0.517† | |
| Intra group test results | 0.294 | <0.001 |
Data are presented as mean±standard deviation, *Paired t-test, †Wilcoxon test, **independent t-test, ††Mann-Whitney U test, P<0.001 considered to be significant
Results showed no significant difference between the intervention and control groups in terms of perceived susceptibility, severity, benefits, barriers, cues to action, and self-efficacy before the intervention (P > 0.05). However, after the intervention, the intervention group showed a significant increase in each of these areas compared to the control group (P < 0.001) [Table 3].
The mean of timely referral score was 95.0 ± 10.9 in the intervention group and 65.2 ± 31.1 in the control group after the intervention. Based on Mann–Whitney U test, this difference was significant (P < 0.001) [Table 4].
Table 4.
Comparison of timely referrals score and duration of complete vascularization in the intervention and control groups before and after intervention
| Variables | Intervention group (mean±SD) | Control group (mean±SD) | P* |
|---|---|---|---|
| Timely referrals score | 95.0±10.9 | 65.2±31.1 | <0.001 |
| Duration of complete vascularization (week) | 9.5±1.7 | 11.3±1.5 | <0.001 |
*Mann-Whitney U test, P<0.001 considered significant
The mean duration of complete vascularization was 9.5 ± 1.7 weeks in the intervention group and 11.3 ± 1.5 weeks in the control group. Based on Mann–Whitney U test, this difference was significant (P < 0.001) [Table 4].
Discussion
The results of this study showed that HBM-based intervention could reduce the level of anxiety in mothers of infants with ROP. In line with the present study results, Fakhri et al.[25] showed that education based on the HBM had reduced the anxiety of nulliparous women. In this regard, Shahnazi et al.[22] concluded that education based on the pattern of HBM reduces anxiety of pregnancy by increasing knowledge and changing beliefs and behaviors.
These studies have been performed on pregnant women, the elderly, respiratory patients, and ocular and orthopedic patients. Despite the substantial differences between the study groups, the HBM was able to reduce the anxiety of the intervention group in all of these studies. The HBM model protects clients against health risks by highlighting the complications and consequences of the disease and improving self-efficacy. Step-by-step training of individuals based on the HBM gives the client a fundamental understanding of the current situation, potential and actual risks, and supporting resources.
The results showed that education based on the HBM was able to improve caring performance of mothers and increase follow-up treatment by highlighting the perceived threat structure. In this regard, Zhang had emphasized the perceived threat structure to reduce anxiety and depression caused by bone fractures in the elderly.[26] Contrary to this approach, Langley et al.,[27] in their study on 243 psychology students, reported that the structure of perceived benefits is the strongest predictor of intent to seek help in anxiety disorders. The difference in age, gender, education, and the level of awareness of the study groups may be the reasons for these contradictions. The HBM model emphasizes the perceived threat structure in the face of illiterate clients and focuses more on the self-efficacy construct in front of informed and highly educated clients.[28,29,30,31]
In the present study, the structure of perceived barriers for mothers regarding the need for follow-up examinations in the pre-intervention stage was almost identical in both groups. Still, a significant difference after the intervention between the two groups of mothers in this area indicates the effect of education based on the HBM on removing the perceived barriers in the intervention group. One of the main reasons for not performing hygienic behaviors is the obstacles people feel they will face while performing sanitary practices. In the present study, through group discussions and participation of all mothers, the existing barriers were identified by mothers. Mothers were then asked to describe their experiences dealing with these barriers. In the next step, mothers were asked to express in the form of brainstorming solutions that came to their minds to overcome the perceived obstacles. As the issue became clearer, mothers gradually came to believe that they could solve the problem and manage the situation in many cases. These findings were in line with a study by Diddana et al.,[32] who used group discussions and brainstorming methods to reduce the perceived barriers of pregnant women to nutritional performance. On the other hand, Sadeghi et al.[33] mainly used the lecture method to improve KAP in diabetes screening based on the HBM. Their study contained two training sessions, so it may not be possible to use methods such as brainstorming and training participation that require more time in this study.
Based on our results, before the intervention, the mothers’ self-efficacy was almost the same in both groups, whereas after the intervention, there was a significant difference between the two groups in this regard, which shows that HBM-based education can improve anxiety management, adherence to follow-up examinations, and increase maternal self-efficacy, resulting in increasing vascularity and preventing eye disorders. Guilford et al.[34] showed that one of the main factors in performing breast cancer in women with high perceived self-efficacy are more committed to activities in the face of adversity and spend more time and effort doing things.
In the present study, the cue to action of mothers in managing anxiety showed a significant difference between the two groups after the intervention. These results were consistent with the study of Hazavehi et al.[35] This structure is divided into two categories of internal and external cue to action. In the present study, external cue to action was used to motivate mothers to pursue treatment and ultimately reduce anxiety. Most HBM-based studies also use external cue to action.[26,32,34] Contrary to this approach, Keshani et al.,[36] in their study to improve the quality of adolescent diet, used more internal cue to action. The probable cause of this problem goes back to the subject of the study. Adolescents are usually very interested in fitness, and this is an intrinsic motivation that can lead to dieting and sports activities in adolescents.
The limitation of this study was that parents used other sources such as media, cyberspace, newspapers, magazine, etc., to obtain information about their baby's illness, which was beyond the control of the researcher. It is recommended that a study be conducted using the HBM with a larger sample size and scope in other ophthalmological centers of the country.
Conclusion
The implementation of education based on the health benefit model had a positive and statistically significant effect on maternal anxiety, follow-up examinations, and retinal vascularization in infants with retinopathy of prematurity. With relying on the results of the present study, nurses and treatment staff can provide interventions and training in the NICU based on the health benefit model to the parents of hospitalized and premature infants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors appreciate all the parents and staff of Khatam al-Anbia Hospital in Mashhad who assisted us in this study.
References
- 1.Huo DM, Dong FT. Recent advances in retinopathy of prematurity. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2004;26:83–7. (Original work published in Chinees) [PubMed] [Google Scholar]
- 2.Babaei H, Ansari MR, Alipour AA, Ahmadipour S, Safari-Faramani R, Vakili J. Incidence and risk factors for retinopathy of prematurity in very low birth weight infants in Kermanshah, Iran. World Appl Sci J. 2012;18:600–4. [Google Scholar]
- 3.Roohipoor R, Karkhaneh R, Farahani A, Ebrahimiadib N, Modjtahedi B, Fotouhi A, et al. Retinopathy of prematurity screening criteria in Iran: New screening guidelines. Arch Dis Child Fetal Neonatal Ed. 2016;101:F288–93. doi: 10.1136/archdischild-2015-309137. [DOI] [PubMed] [Google Scholar]
- 4.Kim SJ, Port AD, Swan R, Campbell JP, Chan RVP, Chiang MF. Retinopathy of prematurity: A review of risk factors and their clinical significance. Surv Ophthalmol. 2018;63:618–37. doi: 10.1016/j.survophthal.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naderian G, Iranpour R, Mohammadizadeh M, Najafabadi FF, Badiei Z, Naseri F, et al. The frequency of retinopathy of prematurity in premature infants referred to an ophthalmology clinic in Isfahan. JIMS. 2011;29:1–5. [Google Scholar]
- 6.Gharebagh M, Sadeghi K, Zarghami N, Mostafidi H. Evaluation of vascular endothelial growth factor, leptin and insulin-like growth factor in precocious retinopathy. Urmia Med J. 2012;23:183–90. [Google Scholar]
- 7.Gharehbaghi MM, Peirovifar A, Sadeghi K. Plasma leptin concentrations in preterm infants with retinopathy of prematurity (ROP) Iran J Neonatol. 2012;3:12–6. [Google Scholar]
- 8.Nakhshab M, Ahmadzadeh Amiri A, Dargahi S, Farhadi R, Yazdani J. The incidence rate of retinopathy of prematurity and related risk factors: A study on premature neonates hospitalized in two hospitals in sari, Iran, 2014-2015. JKUM. 2016;23:296–307. [Google Scholar]
- 9.Anthony KK, Gil KM, Schanberg LE. Brief report: Parental perceptions of child vulnerability in children with chronic illness. J Pediatr Psychol. 2003;28:185–90. doi: 10.1093/jpepsy/jsg005. [DOI] [PubMed] [Google Scholar]
- 10.Müller Nix C, Ansermet F. Prematurity, risk factors, and protective factors. Handbook of infant mental health. 2009:180–96. [Google Scholar]
- 11.Zelkowitz P, Papageorgiou A, Bardin C, Wang T. Persistent maternal anxiety affects the interaction between mothers and their very low birthweight children at 24 months. Early Hum Dev. 2009;85:51–8. doi: 10.1016/j.earlhumdev.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Hwang HS, Kim HS, Yoo IY, Shin HS. Parenting stress in mothers of premature infants. Child Health Nurs Res. 2013;19:39–48. doi: 10.5468/CHNR.2013.19.1.39 (Original work published in Korean) [Google Scholar]
- 13.Glasser S, Lerner-Geva L, Levitski O, Reichman B. Parent support activities in neonatal intensive care units: A national survey in Israel. Harefuah. 2009;148:238–42. 277, 276 (Original work published in Hebrew) [PubMed] [Google Scholar]
- 14.Davis E, Shelly A, Waters E, Boyd R, Cook K, Davern M. The impact of caring for a child with cerebral palsy: Quality of life for mothers and fathers. Child Care Health Dev. 2010;36:63–73. doi: 10.1111/j.1365-2214.2009.00989.x. [DOI] [PubMed] [Google Scholar]
- 15.Lv B, Gao XR, Sun J, Li TT, Liu ZY, Zhu LH, et al. Family-centered care improves clinical outcomes of very-low-birth-weight infants: A quasi-experimental study. Front Pediatr. 2019;7:138. doi: 10.3389/fped.2019.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebadi Fard Azar F, Solhi M, Zohoor AR, Ali Hosseini M. The effect of health belief model on promoting preventive behaviors of osteoporosis among rural women of Malayer. J Inflamm Dis. 2012;16:58–64. (Original work published in Persian) [Google Scholar]
- 17.Vahidi S. The effect of an educational program based on the health belief model on self-efficacy among patients with type 2 diabetes referred to the Iranian Diabetes Association in 2014. J Diabetes Mellitus. 2015;5:181. [Google Scholar]
- 18.Chatripour R, Shojaeizadeh D, Tol A, Sayehmiri K, Asfeia A, Kia F. The impact of teacher education on promoting knowledge, attitude and performance of students in prevention of cardiovascular diseases: Application of the HBM model. RJMS (Journal of Iran University of Medical Sciences) 2016;23:26–35. (Original work published in Persian) [Google Scholar]
- 19.Allen LB, Taylor FH, Kauwe AI, Larsen T, Hippen AA, Allen M, et al. Using the Health Belief Model to evaluate Samoan caregiver perceptions for rheumatic heart disease follow-up care. Int J Health Promot Educ. 2017;55:148–57. [Google Scholar]
- 20.Fu A. Clinical study on the improvement of anxiety and depressive state of orthopedic patients after operation through application of health belief model.”. Attend to Practice and Research. 2009 (Original work published in Chinees) [Google Scholar]
- 21.Nong CH, Liu JH, Qiu JZ. Clinical study on the improvement of anxiety and depressive state of patients after digital replantation through application of health belief model. Nurs Pract Res. 2010;14 (Original work published in Chinees) [Google Scholar]
- 22.Shahnazi H, Sabooteh S, Sharifirad G, Mirkarimi K, Hassanzadeh A. The impact of education intervention on the Health Belief Model constructs regarding anxiety of nulliparous pregnant women. J Educ Health Promot. 2015;4:1–18. doi: 10.4103/2277-9531.154120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilkinson AR, Haines L, Head K, Fielder AR. UK retinopathy of prematurity guideline. Early Hum Dev. 2008;84:71–4. doi: 10.1016/j.earlhumdev.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Spielberger CD, Rickman RL. Assessment of state and trait anxiety. Anxiety: Psychobiological and clinical perspectives. 1990:69–83. [Google Scholar]
- 25.Fakhri A, Morshedi H, Mohammadi Zeidi I. Effect of education based on health belief model with relaxation on anxiety of nulliparouse women. Scientific Journal of Kurdistan University of Medical Sciences. 2017;22:32–47. (Original work published in persian) [Google Scholar]
- 26.Zhang M. Effect of HBM rehabilitation exercises on depression, anxiety and health belief in elderly patients with osteoporotic fracture. Psychiatr Danub. 2017;29:466–72. doi: 10.24869/psyd.2017.466. [DOI] [PubMed] [Google Scholar]
- 27.Langley EL, Wootton BM, Grieve R. The utility of the health belief model variables in predicting help-seeking intention for anxiety disorders. Aust Psychol. 2018;53:291–301. [Google Scholar]
- 28.Kampouroglou G, Velonaki VS, Pavlopoulou I, Drakou E, Kosmopoulos M, Kouvas N, et al. Parental anxiety in pediatric surgery consultations: The role of health literacy and need for information. J Pediatr Surg. 2020;55:590–6. doi: 10.1016/j.jpedsurg.2019.07.016. [DOI] [PubMed] [Google Scholar]
- 29.Yong LI, Cheng-Ye JI, Jiong QI, Zhang ZX. Parental anxiety and quality of life of epileptic children. Biomed Environ Sci. 2008;21:228–32. doi: 10.1016/S0895-3988(08)60034-3. [DOI] [PubMed] [Google Scholar]
- 30.Ravarian A, Vameghi R, Heidarzadeh M, Nariman S, Sagheb S, Nori F, et al. Factors influencing the attendance of preterm infants to neonatal follow up and early intervention services following discharge from neonatal intensive care unit during first year of life in Iran. Iran J Child Neurol. 2018;12:67–76. [PMC free article] [PubMed] [Google Scholar]
- 31.Nagae M, Nakane H, Honda S, Ozawa H, Hanada H. Factors affecting medication adherence in children receiving outpatient pharmacotherapy and parental adherence. J Child Adolesc Psychiatr Nurs. 2015;28:109–17. doi: 10.1111/jcap.12113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diddana TZ, Kelkay GN, Dola AN, Sadore AA. Effect of nutrition education based on health belief model on nutritional knowledge and dietary practice of pregnant women in Dessie Town, Northeast Ethiopia: A cluster randomized control trial. J Nutr Metab 2018. 2018 doi: 10.1155/2018/6731815. 6731815. doi: 10.1155/2018/6731815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sadeghi R, Rezaeian M, Khanjani N, Iranpour A. The applied of health belief model in knowledge, attitude and practice in people referred for diabetes screening program: An educational trial. JRUMS. 2015;13:1061–72. [Google Scholar]
- 34.Guilford K, McKinley E, Turner L. Breast cancer knowledge, beliefs, and screening behaviors of college women: Application of the health belief model. Am J Health Educ. 2017;48:256–63. [Google Scholar]
- 35.Hazavehi M, Moeini B, Roshanaei G. Investigating causes of the infants’ growth disorder (6-12 months) in Hamadan health centers based on Health Belief Model. Sci J Hamadan Nurs Midwifery Fac. 2013;21:68–76. (Original work published in Persian) [Google Scholar]
- 36.Keshani P, Hossein Kaveh M, Faghih S, Salehi M. Improving diet quality among adolescents, using health belief model in a collaborative learning context: A randomized field trial study. Health Educ Res. 2019;34:279–88. doi: 10.1093/her/cyz009. [DOI] [PubMed] [Google Scholar]