Abstract
Background
Despite the increasing application of tolvaptan in cardiac surgery, there is no information on the use of tolvaptan in Stanford patients with type A aortic dissection. This study aimed to evaluate the postoperative clinical effects of tolvaptan in patients with type A aortic dissection after tafter surgery.
Methods
A retrospective analysis was performed on 45 patients treated for type A aortic dissection in our hospital from 2018 to 2020. These included 21 patients who were treated with tolvaptan (Group T) and 24 patients who received traditional diuretics (Group L). The hospital's electronic health records were used to obtain perioperative data.
Results
Group T did not differ significantly from Group L in terms of the duration of mechanical ventilation, postoperative blood required, length of catecholamine use, or the amount of intravenous diuretic drugs administered (all P > 0.05). The development of postoperative atrial fibrillation was significantly less in the tolvaptan group (P = 0.023). The urine volumes and change in body weight loss were slightly higher in group T than in group L but the differences were non-significant (P > 0.05). Serum potassium, creatinine, and urea nitrogen levels did not differ between the groups in the week after surgery, At the same time, sodium was significantly higher in the Group T group on day 7 after transfer from the ICU (P = 0.001). In Group L, sodium levels were also elevated by day 7 (P = 0.001). On days 3 and 7, serum creatinine and urea nitrogen levels increased in both groups (both P < 0.05).
Conclusions
Both tolvaptan and traditional diuretics were found to be effective and safe for patients with acute Stanford type A aortic dissection. Moreover, tolvaptan may be associated with reducing the incidence of postoperative atrial fibrillation.
Keywords: Loop diuretic, Cardiopulmonary bypass, Deep hypothermic circulatory arrest, Replacement of aorta
Background
Heart failure may develop during acute type A aortic dissection (AD) due to the necessity for heart arrest during surgery [1–5]. Together with hemodilution, hypothermia, and inflammatory responses, cardiopulmonary bypass and deep hypothermic circulatory arrest (DHCA) can lead to complications such as increased vascular permeability and decreased colloidal osmotic pressure, which can result in interstitial edema [6–9]. Therefore, sufficient volume is required to avert intravascular hypovolemia soon after surgery [10]. The volume is then reduced after stabilizing of inflammation and temperature [11].
The control of excess fluid with diuretics is crucial for the postoperative management of surgery involving the great vessels [12]. Intermittent diuretic and fluid administration is often used during the early postoperative period [14]. Tolvaptan is a vasopressin-2 receptor antagonist that differs in its diuretic mechanism from traditional diuretics, such as furosemide and spironolactone. It acts on distal nephritis and can augment the urine volume without electrolyte removal [13–15]. It has been shown that, in contrast to other diuretics, tolvaptan does not adversely affect blood pressure, renal function, or electrolyte balance [16, 17]. To date, numerous reports have indicated the usefulness of tolvaptan in managing postoperative fluid volumes in patients with cardiac diseases treated with surgery [10].
However, despite the acceptance of tolvaptan for various types of cardiovascular conditions treated by surgery, there is limited information on its use after surgery for type A AD. Therefore, we retrospectively analyzed the clinical effectiveness of tolvaptan in patients after surgery for type A AD in our hospital over two-years, compared with those receiving loop diuretics during the same period.
Methods
Study design and ethics approval
There was no precise protocol because this was a retrospective study. The study primarily focused on patient data collected during hospitalization. The Dalian Municipal Central Hospital Ethics Committee approved the study with (Approval No. YN2022-010-01), and the need for informed consent was waived.
Patients
Fifty-one patients with acute Stanford type A AD were surgically treated at our hospital between January 1, 2018, and December 31, 2020. Four of these patients died after surgery, and two were excluded from the study due to incomplete clinical data.
Of the remaining 45 patients, 21 received tolvaptan after surgery (Group T), while 24 patients did not (Group L).
The normal procedure for cardiac surgery in our hospital is that that patients return to the ward from the intensive care unit (ICU) when their pain VAS score is below 5 and their blood oxygen saturation is continuously higher than 90%.
All patients started oral diuretic therapy (torasemide 20 mg/day oral) on the first day after transfer to the department of cardiac surgery from the ICU and continued for at least one week. The patients receiving tolvaptan were given oral tolvaptan in addition to oral torasemide. Tolvaptan was administered at a 15 mg/day dose for at least one week. Intravenous injection of furosemide (20 mg/potion) or torasemide (10 mg/potion) was used intermittently according to the patient's urine volume.
Data source and variables
Data were obtained from the hospital’s medical records. The general information including age, sex, body surface area (BSA), body mass index (BMI), comorbidities, and AD etiology, as well as serum levels of alanine transaminase (ALT), albumin, creatinine, and urea nitrogen, were taken at the time of hospital admission.
Intraoperative information included the operative method, operative time, extracorporeal circulation time, and the number and times of DHCAs. Postoperative information of patients included the time spent in ICU, mechanical ventilation time, duration of vasoactive drug use, postoperative blood transfusion volume, length of postoperative hospitalization, the incidence of complications, urine volume, changes of body weight loss, changes in serum sodium, changes in serum potassium, and changes in creatinine and urea nitrogen.
Complications included gastrointestinal bleeding, cerebral infarction, postoperative atrial fibrillation (POAF), and intracranial hemorrhage.
Urine volume: The cumulative urine volume of patients on days 1, 3, and 7 after transfer from the ICU to the cardiac and vascular surgery ward was recorded.
Changes in body weight loss: Patients' cumulative body weight loss on days 1, 3, and 7 after transfer from the ICU to the cardiac and vascular surgery ward were recorded.
Serum sodium, potassium, urea nitrogen, and creatinine: these were determined on days 1, 3, and 7 after transfer from the ICU to the ward.
Statistical analysis
All data was maintained in Office 365. SPSS Version 26.0 (IBM Corp., Armonk, NY, USA) was used to analyze the data. Data from all measurements are expressed as means ± standard deviation. Student’s t-test was used to assess differences in normally distributed data, while the Wilcoxon rank-sum test was applied for non-normally distributed data. Count data were expressed as the number of cases or composition ratio, and comparisons were performed using the χ2 test. Continuous correction χ2 tests were utilized if the expected frequency of a cell was greater than 1 and less than 5. Fisher's exact test was employed for measurement data where the predicted frequency of any cell was less than 1. The Wilcoxon rank-sum test was used to compare the test results of the same group of patients at different periods. All the tests were two-tailed, and P-values less than 0.05 (P < 0.05) were considered statistically significant.
Results
General information
All patients were classified as Penn class Aa. None of the patients had a history of heart failure. None of the patients had a history of long-term diuretic use, nor did any have a prior history of underlying kidney disease. Groups T and L did not differ significantly in terms of patient characteristics at the time of admission (P > 0.05) (Table 1). No patients had preoperative atrial fibrillation. No differences were seen in the general preoperative data, intraoperative conditions, duration of mechanical ventilation, length of ICU stay, the volume of blood transfused, or the length of catecholamine use between group T and the traditional diuretic group L (p > 0.05) (Table 1).
Table 1.
Comparison of characteristics between groups L and T
| Parameters | Group T (n = 21) | Group L (n = 24) | P |
|---|---|---|---|
| General | |||
| Age (years) | 60.52 ± 10.73 | 55.46 ± 14.66 | 0.199 |
| Male (cases) | 13 (61.9) | 18 (75) | 0.344 |
| BSA | 1.82 ± 0.18 | 1.84 ± 0.21 | 0.752 |
| BMI | 25.08 ± 2.65 | 25.43 ± 3.98 | 0.734 |
| Smoke (cases) | 12 (57.1) | 14 (58.3) | 0.936 |
| Comorbidities | |||
| Hypertension (cases) | 16 (76.2) | 17 (70.8) | 0.685 |
| Diabetes (cases) | 2 (9.5) | 4 (16.7) | 0.670 |
| Stroke (cases) | 1 (4.8) | 2 (8.3) | 1.000 |
| Coronary artery disease (cases) | 0 | 2 (8.3) | 0.491 |
| Preoperative cardiac condition | |||
| Acute myocardial infarction (cases) | 0 | 1 (4.2) | 1.000 |
| Pericardial effusion (cases) | 10 (47.6) | 9 (37.5) | 0.493 |
| Moderate or above aortic regurgitation (cases) | 4 (19) | 4 (16.7) | 1.000 |
| Etiology | |||
| Aortic arteriosclerosis (cases) | 21 (100) | 23 (95.2) | 1.000 |
| Marfan syndrome (cases) | 0 | 1 (4.8) | 1.000 |
| Preoperative laboratory examinations | |||
| ALT(U/L) | 118.19 ± 26.78 | 40.08 ± 20.04 | 0.495 |
| Albumin(g/L) | 36.69 ± 5.38 | 39.97 ± 9.24 | 0.203 |
| Creatinine(umol/L) | 88.81 ± 39.16 | 73.83 ± 23.80 | 0.387 |
| Urea nitrogen (mmol/L) | 7.14 ± 2.56 | 6.76 ± 2.34 | 0.562 |
Surgery information
All the patients received the intervention of the ascending aorta only or the Frozen Elephant Trunk Technique (FETT) with the concurrent intervention of the ascending aorta. Groups T and L did not differ significantly in terms of surgical methods, operative time, extracorporeal circulation time, the proportion of patients requiring DHCA, and the length of DHCA (all P > 0.05–) (see Table 2).
Table 2.
Comparison of surgery between groups L and T
| Parameters | Group T (n = 21) | Group L (n = 24) | P |
|---|---|---|---|
| Surgery information | 0.124 | ||
| Isolate ascending aorta replacement/Bentall Procedure (cases) | 16 | 13 | – |
| Ascending aorta replacement + FETT (min) | 5 | 11 | – |
| Surgery time (min) | 323.57 ± 72.99 | 371.67 ± 103.78 | 0.083 |
| Cardiopulmonary bypass time (min) | 137.38 ± 30.85 | 146.67 ± 9.03 | 0.425 |
| DHCA (cases) | 8 (38.1) | 14 (58.3) | 0.175 |
| DHCA time (min) | 16.00 ± 6.78 | 17.69 ± 6.52 | 0.576 |
Postoperative situation
Groups T and L did not differ significantly in terms of the duration of postoperative mechanical ventilation, time spent in ICU hospitalization, length of postoperative hospitalization, postoperative blood transfusion volume, time of use of catecholamines, and the amount of intravenous diuretic drugs administered (all P > 0.05).
All patients with POAF within 3–7 days after being transferred from ICU to the cardiac surgery ward, and were converted to sinus rhythm within 3 days after receiving symptomatic treatment such as amiodarone conversion.
The occurrence of POAF in group T was significantly less than that in group L (P = 0.023) (see Table 3 for details).
Table 3.
Comparison in postoperative information between groups L and T
| Parameters | Group T (n = 21) | Group L (n = 24) | P |
|---|---|---|---|
| Duration of mechanical ventilation (h) | 38.67 ± 47.11 | 33.21 ± 38.35 | 0.741 |
| Duration of ICU stay (days) | 2.90 ± 2.66 | 2.42 ± 2.02 | 0.662 |
| Catecholamine use (h) | 35.71 ± 11.99 | 32.29 ± 5.78 | 0.148 |
| Postoperative blood transfusion volume (ml) | 723.81 ± 126.46 | 695.83 ± 80.45 | 0.727 |
| Time from surgery to discharge (days) | 18.81 ± 6.31 | 16.63 ± 6.21 | 0.209 |
| Number of intravenous diuretic injections (times) | 10.38 ± 2.17 | 6.75 ± 1.49 | 0.083 |
| Complications | |||
| POAF (cases) | 3 (14.3) | 11 (45.8) | 0.023 |
| Stroke (cases) | 1 (4.8) | 1 (4.2) | 1 |
| Gastrointestinal bleeding (cases) | 1 (4.8) | 0 | 1 |
| Subarachnoid hemorrhage (cases) | 1 (4.8) | 0 | 1 |
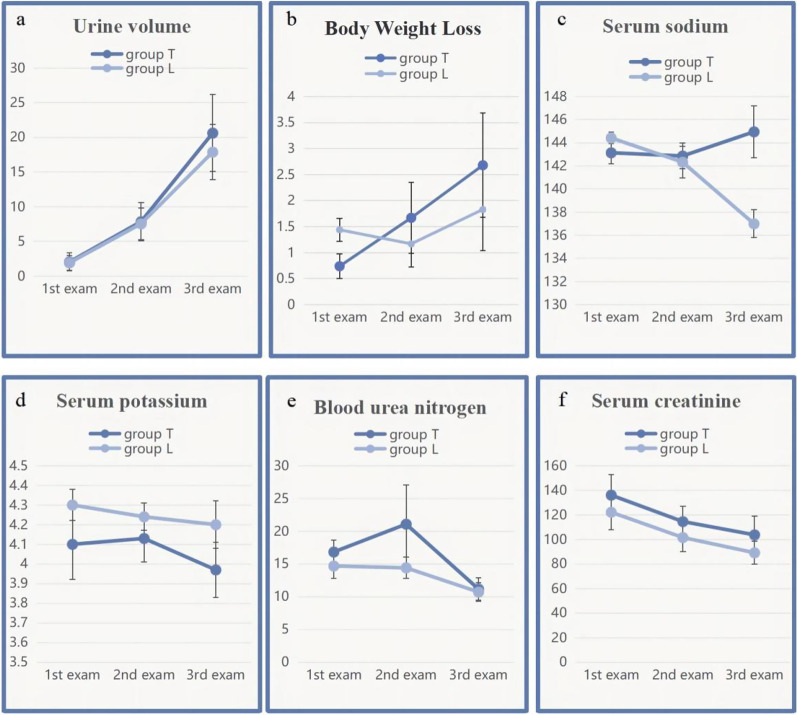
After transfer from the ICU to the cardiovascular surgery ward, the urine volumes and change in body weight were slightly greater in group T than in group L but the differences were non-significant (P > 0.05). No changes were seen in serum potassium, creatinine, and urea nitrogen between the groups at any time (all P > 0.05). Although the sodium ion level did not differ between the groups on days 1 and 3 after the transfer, it was significantly elevated in group T on day 7 (P = 0.001). See Figs. 1, 2, and Table 4 for details.
Fig. 1.
Changes in cumulative urine volume, body weight, and serum levels of sodium, potassium, creatinine, and urea nitrogen a–f: *Significant difference between groups T and L
Fig. 2.
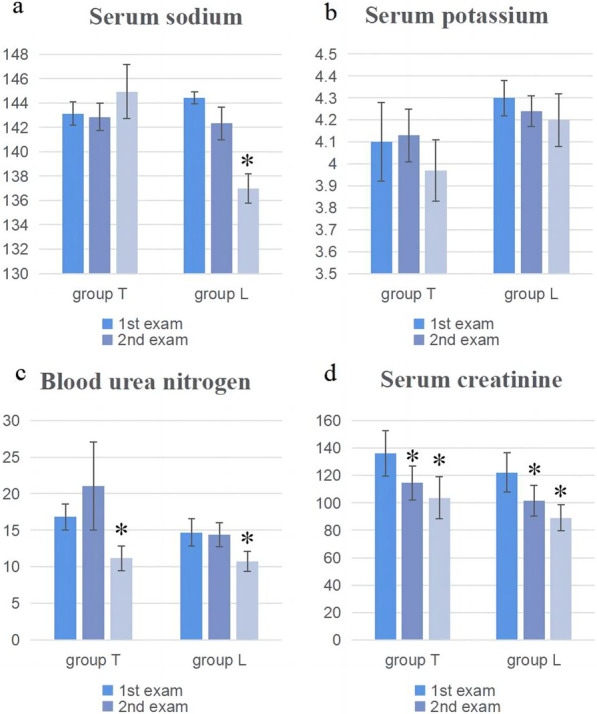
Changes in serum levels of sodium, potassium, creatinine, and urea nitrogen a–d: *Significantly different from day 1 measurement
Table 4.
Changes in cumulative urine volume and levels of serum sodium, potassium, creatinine, and urea nitrogen
| Group T (n = 21) | Group L (n = 24) | P | |
|---|---|---|---|
| Urine volume (L) | |||
| Day 1 | 2.05 ± 1.28 | 1.92 ± 1.06 | 0.820 |
| Day 3 | 7.86 ± 2.76 | 7.54 ± 2.30 | 0.613 |
| Day 7 | 20.62 ± 5.56 | 17.88 ± 3.99 | 0.154 |
| Loss of body weight (kg) | |||
| Day 1 | 0.74 ± 0.24 | 1.44 ± 0.22 | 0.061 |
| Day 3 | 1.67 ± 0.68 | 1.17 ± 0.44 | 0.554 |
| Day 7 | 2.68 ± 1.00 | 1.83 ± 0.79 | 0.524 |
| Serum sodium (mmol/L) | |||
| Day 1 | 143.14 ± 0.97 | 144.42 ± 0.50 | 0.436 |
| Day 3 | 142.86 ± 1.11 | 142.33 ± 1.36 | 0.784 |
| Day 7 | 144.95 ± 2.24 | 137.58 ± 1.21 | 0.001 |
| Serum potassium (mmol/L) | |||
| Day 1 | 4.1 ± 0.18 | 4.30 ± 0.08 | 0.453 |
| Day 3 | 4.13 ± 0.12 | 4.24 ± 0.07 | 0.250 |
| Day 7 | 3.97 ± 0.14 | 4.20 ± 0.12 | 0.246 |
| Serum creatinine (umol/L) | |||
| Day 1 | 136.05 ± 16.75 | 122.13 ± 14.32 | 0.569 |
| Day 3 | 114.52 ± 12.46 | 101.54 ± 11.37 | 0.439 |
| Day 7 | 103.71 ± 15.10 | 89.13 ± 9.32 | 1.000 |
| Blood urea nitrogen (mmol/L) | |||
| Day 1 | 16.83 ± 1.77 | 14.68 ± 1.89 | 0.265 |
| Day 3 | 21.08 ± 6.91 | 14.41 ± 1.64 | 0.682 |
| Day 7 | 11.17 ± 1.69 | 10.72 ± 1.39 | 0.585 |
The serum sodium, potassium, creatinine, and urea nitrogen levels in the groups were compared with those measured at the time of the first examination. The serum sodium levels differed between days 1 and 7 after transfer from the ICU in group L (P = 0.001). The creatinine and urea nitrogen levels in both groups also differed significantly between days 1 and 7 (all P < 0.05). See Table 5 for details.
Table 5.
Comparison of the day 3 and day 7 levels of serum sodium, potassium, creatinine, and urea nitrogen with the day 1 results
| Group T (n = 21) | Group L (n = 24) | |
|---|---|---|
| P | P | |
| Serum sodium (mmol/L) | ||
| Day 1 versus day 3 | 0.572 | 0.053 |
| Day 1 versus day 7 | 0.681 | 0.001 |
| Serum potassium (mmol/L) | ||
| Day 1 versus day 3 | 0.149 | 0.637 |
| Day 1 versus day 7 | 0.351 | 0.449 |
| Serum creatinine (umol/L) | ||
| Day 1 versus day 3 | 0.037 | 0.001 |
| Day 1 versus day 7 | 0.006 | 0.001 |
| Blood urea nitrogen (mmol/L) | ||
| Day 1 versus day 3 | 0.498 | 0.415 |
| Day 1 versus day 7 | 0.006 | 0.006 |
Discussion
The present study compared the efficacy of tolvaptan and traditional diuretics after acute Stanford type A AD.
In previous post-cardiac surgery studies, the subjects were primarily patients after cardiac surgery. Most of these patients have basic heart failure before the operation, and most need cardiotomy and other heart-damaging operations during the process [1–8]. The object of this study was acute Stanford type A AD surgery. There was no heart failure before the procedure, and no cardiotomy was required during the procedure. This may also have a certain impact on the patient's postoperative fluid management.
In previous studies of tolvaptan in cardiac surgery, patients' postoperative urine output was mainly 10-15L/7 days [10, 17–19]. But in this study, patients had significantly more urine output. The patient's postoperative fluid management and changes in urine volume depend on the patient's postoperative intake and excretion adjustment. In this study, we applied diuretics to remove fluid retention while supplementing the patient's basic daily fluid requirements. This could explain why our patient had increased urine output following surgery. We noted the patient's weight changes to more accurately reflect the patient's fluid changes. It was observed that both tolvaptan and conventional diuretics achieved satisfactory voiding volume and body weight loss after surgery, and there was no difference in the need for intravenous diuretics.
Before surgery, there were no significant changes in serum creatinine and urea nitrogen levels between the two groups. This was related to the level of preoperative ischemia. Laboratory results depend heavily on the effect of AD on the blood supply to the organs [18]. All patients in this study were Penn's type Aa patients. Although the dissection was extensive in some patients, there was no adverse organ perfusion. This also allows us to bserve diuretics' effect on these patients better.
Previous reports have shown that tolvaptan increases urine output significantly more than conventional diuretics [10, 19]. The current study observed a slight, but non-significant, elevation in urine output in the T group than in the L group. And no significant difference was observed in weight loss between the T group and the L group. The long-term use of loop diuretics may result in diuretic resistance often caused by sodium reabsorption in the distal tubules. Tolvaptan can reduce sodium loss and thus mitigate diuretic resistance [20]. However, patients undergoing surgery for type A AD do not usually have histories of long-term loop diuretic use, and none of the present study participants had a history of traditional diuretic use. These patients would not be resistant to diuretics and, consequently, would likely be highly sensitive to loop diuretics [21].
Furthermore, Nishi et al. evaluated the response to tolvaptan in patients undergoing cardiovascular surgery. The amount of urine excreted after tolvaptan administration was discovered to be dependent on the degree of fluid retention before and during surgery, even though there was no substantial difference between responders and non-responders in terms of preoperative comorbidities or blood tests [22]. Patients with type A AD do not experience significant fluid retention before surgery as there is no underlying heart disease, which may render these patients unresponsive to tolvaptan. However, the sample size was relatively small and future studies are needed for confirmation.
Hypernatremia is defined as excessive sodium levels in the blood. It usually happens when a person has a low fluid intake or excessive fluid loss. Hypernatremia is an important public health issue. In this study, blood sodium levels in the T group were considerably higher after one week than in the L group.Significantly raised sodium levels were also seen in the L group on day 7 after transfer to the cardiac surgery ward compared to day 1. Studies have found that the development of hypernatremia was not dependent on the type of protocol used [23, 24]. It was found that although sodium levels increased over time in patients receiving tolvaptan, the rise was significantly lower than in patients not receiving tolvaptan [12, 24].
The serum potassium ion level is also a concern in diuretic patients. Here, no differences were seen in the potassium levels over time in the two groups, nor between the groups simultaneously. A previous meta-analysis of serum potassium in patients on tolvaptan concluded no difference in the mean serum potassium levels in patients with or without tolvaptan [25].
Tolvaptan has been reported to maintain renal blood flow during diuresis without activating the renin–angiotensin–aldosterone system [26, 27]. It has been suggested that using tolvaptan in cardiac surgery patients may enhance renal perfusion and stimulate the elimination of urea nitrogen [23, 28]. However, in this study, the levels of blood creatinine and urea nitrogen in both T and L groups showed a significant downward trend with the prolongation of postoperative time. Neither creatinine nor urea nitrogen levels differed between the groups at similar time points. Previous results showed no significant difference in renal function indicators, such as serum creatinine, between patients receiving loop diuretics and those receiving tolvaptan. None of the patients in this study had renal disease, and serum creatinine and urea nitrogen on a postoperative day 1 were only slightly elevated. It has been reported that the protective effect of tolvaptan on the kidney increases as essential renal function decreases [29]. The question arises as to whether this protective action of tolvaptan may not be as strong as expected in patients with type A AD. Nevertheless, tolvaptan does not have serious adverse effects on kidney function, at least compared with traditional diuretics.
Risk factors for POAF after conventional cardiac surgery include age and cardiac structural changes [30, 31]. Recent studies have shown that volume overload, electrolyte imbalance, acute kidney injury, and sympathetic nervous system activation are also risk factors for POAF after cardiac surgery [32]. Based on the patient's bodily fluid change, weight change, and electrolyte status, in conjunction with the patient's surgical circumstances. Additionally, we compared the surgical procedure, operation time, postoperative pain control, oxygen saturation level, and other parameters associated with postoperative new-onset atrial fibrillation. However, there were no statistically significant differences observed.
The current study observed significantly less development of new atrial fibrillation in the T group than in the L group. In all patients with new-onset AF, AF occurred 3 days after admission from the ICU to the cardiac surgery unit. Although the weight loss rate of group L appeared to be faster than that of group T on day 1, it was not statistically significant. Previous studies have shown no significant adverse effects of the drug on the occurrence of complications after thoracotomy [30, 31]. Recent studies have suggested that tolvaptan may reduce the occurrence of atrial fibrillation after cardiac surgery by inhibiting the activation of the renin–angiotensin–aldosterone axis and sympathetic nervous system [32].
A variety of factors influenced the duration of hospitalization. No significant length of hospital stay differences was seen between the two groups.
This study has several limitations. First, this was a single-center retrospective study with a limited number of patients that could cause selection bias and residual confounding. Second, the duration of medication was defined from the time of transfer from the ICU to the cardiovascular surgery ward, thus excluding the course of treatment in the ICU. Further limitations are that several important laboratory indicators such as urine ions and urine osmotic pressure were not included.
Conclusion
In conclusion, both tolvaptan and traditional diuretics were found to be effective and safe for patients with acute Stanford type A AD. Tolvaptan may be associated with reducing the incidence of postoperative atrial fibrillation.
Acknowledgements
None.
Abbreviations
- AD
Aortic dissection
- ALT
Alanine transaminase
- BMI
Body mass index
- BSA
Body surface area
- DHCA
Deep hypothermic circulatory arres
- FETT
Frozen elephant trunk technique
- ICU
Intensive care unit
- POAF
Postoperative atrial fibrillation
Author contributions
WW and FG have made equal contributions to this research. This project was conceived by XZ, WW and FG. WW, FG, XH, YG, LS and WL participated in analysis and interpretation. WW, FG, XH, YG, LS, WL and XZ participated in the data collection. The statistical analysis was conceptualized and conducted by WW, FG, XH, YG, LS, WL and XZ. The manuscript was drafted by WW, FG, XH, YG, LS, WL and XZ, and critically revised by WW, FG, XH, YG, LS, WL and XZ. WW, FG and XZ were responsible for obtaining funding. All authors have read and approved the final version of the manuscript. All authors have agreed to be accountable. All authors read and approved the final manuscript.
Funding
No funding was received for this study.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was granted exemption from ethic review by the Ethics Committee of Dalian Municipal Center Hospital (Ref No YN2022-010-01 February 15, 2022). The Ethics Committee of Dalian Municipal Central Hospital waived informed consent. The research was a retrospective study and used only existing collections of data that contain only non-identifiable data and is of negligible risk. The Ethics Committee of Dalian Municipal Central Hospital ensures that the data used in this study does not involve any patient privacy and only provides raw data to members of the study group. Research involving human data was performed following the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gudbjartsson T, Ahlsson A, Geirsson A, Gunn J, Hjortdal V, Jeppsson A, et al. Acute type A aortic dissection—a review. Scand Cardiovasc J. 2020;54:1–13. doi: 10.1080/14017431.2019.1660401. [DOI] [PubMed] [Google Scholar]
- 2.Zhu Y, Lingala B, Baiocchi M, Tao JJ, Toro Arana V, Khoo JW, et al. Type A aortic dissection-experience over 5 decades: JACC historical breakthroughs in perspective. J Am Coll Cardiol. 2020;76:1703–1713. doi: 10.1016/j.jacc.2020.07.061. [DOI] [PubMed] [Google Scholar]
- 3.Xu S, Liu J, Li L, Wu Z, Li J, Liu Y, et al. Cardiopulmonary bypass time is an independent risk factor for acute kidney injury in emergent thoracic aortic surgery: a retrospective cohort study. J Cardiothorac Surg. 2019;14:90. doi: 10.1186/s13019-019-0907-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi Q, Mu X, Zhang C, Wang S, Hong L, Chen X. Risk Factors for postoperative delirium in type A aortic dissection patients: a retrospective study. Med Sci Monit. 2019;25:3692–3699. doi: 10.12659/MSM.913774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aass T, Stangeland L, Moen CA, Salminen PR, Dahle GO, Chambers DJ, et al. Myocardial function after polarizing versus depolarizing cardiac arrest with blood cardioplegia in a porcine model of cardiopulmonary bypass. Eur J Cardiothorac Surg. 2016;50:130–139. doi: 10.1093/ejcts/ezv488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giacinto O, Satriano U, Nenna A, Spadaccio C, Lusini M, Mastroianni C, et al. Inflammatory response and endothelial dysfunction following cardiopulmonary bypass: pathophysiology and pharmacological targets. Recent Pat Inflamm Allergy Drug Discov. 2019;13:158–173. doi: 10.2174/1872213X13666190724112644. [DOI] [PubMed] [Google Scholar]
- 7.Fang Z, Wang G, Liu Q, Zhou H, Zhou S, Lei G, et al. Moderate and deep hypothermic circulatory arrest has a comparable effect on acute kidney injury after total arch replacement with frozen elephant trunk procedure in type A aortic dissection. Interact Cardiovasc Thorac Surg. 2019;29:130–136. doi: 10.1093/icvts/ivz092. [DOI] [PubMed] [Google Scholar]
- 8.Li J, Yang L, Wang G, Wang Y, Wang C, Shi S. Severe systemic inflammatory response syndrome in patients following Total aortic arch replacement with deep hypothermic circulatory arrest. J Cardiothorac Surg. 2019;14:217. doi: 10.1186/s13019-019-1027-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kertai MD, Cheruku S, Qi W, Li YJ, Hughes GC, Mathew JP, et al. Mast cell activation and arterial hypotension during proximal aortic repair requiring hypothermic circulatory arrest. J Thorac Cardiovasc Surg. 2017;153(68–76):e2. doi: 10.1016/j.jtcvs.2016.05.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishi H. Advent of New perioperative care for fluid management after cardiovascular surgery: a review of current evidence. J Cardiol. 2020;75:606–613. doi: 10.1016/j.jjcc.2019.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Hollinger A, Bolliger D. Tolvaptan-new opportunity in fluid management after cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2019;33:2180–2182. doi: 10.1053/j.jvca.2019.01.037. [DOI] [PubMed] [Google Scholar]
- 12.Matsuyama K, Koizumi N, Nishibe T, Iwasaki T, Iwahasi T, Toguchi K, et al. Effects of short-term administration of tolvaptan after open heart surgery. Int J Cardiol. 2016;220:192–195. doi: 10.1016/j.ijcard.2016.06.156. [DOI] [PubMed] [Google Scholar]
- 13.Felker GM, Mentz RJ, Cole RT, Adams KF, Egnaczyk GF, Fiuzat M, et al. Efficacy and safety of tolvaptan in patients hospitalized with acute heart failure. J Am Coll Cardiol. 2017;69:1399–1406. doi: 10.1016/j.jacc.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 14.Lisco G, Giagulli VA, Iovino M, Zupo R, Guastamacchia E, De Pergola G, et al. Endocrine system dysfunction and chronic heart failure: a clinical perspective. Endocrine. 2022;75(2):360–376. doi: 10.1007/s12020-021-02912-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ali Y, Dohi K, Okamoto R, Katayama K, Ito M. Novel molecular mechanisms in the inhibition of adrenal aldosterone synthesis: Action of tolvaptan via vasopressin V2 receptor-independent pathway. Br J Pharmacol. 2019;176:1315–1327. doi: 10.1111/bph.14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tamaki S, Yamada T, Morita T, Furukawa Y, Kawasaki M, Kikuchi A, et al. Impact of adjunctive tolvaptan on sympathetic activity in acute heart failure with preserved ejection fraction. ESC Heart Fail. 2020;7:933–937. doi: 10.1002/ehf2.12690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kin H, Matsumura K, Yamamoto Y, Fujii K, Otagaki M, Takahashi H, et al. Renoprotective effect of tolvaptan in patients with new-onset acute heart failure. ESC Heart Fail. 2020;7:1764–1770. doi: 10.1002/ehf2.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Ghofaily L, Feinman JW, Augoustides JG. Acute aortic dissection-refining contemporary outcomes with the penn classification for this aortic emergency. J Cardiothorac Vasc Anesth. 2020;34(4):874–876. doi: 10.1053/j.jvca.2019.12.037. [DOI] [PubMed] [Google Scholar]
- 19.Kato TS, Nakamura H, Murata M, Kuroda K, Suzuki H, Yokoyama Y, et al. The effect of tolvaptan on renal excretion of electrolytes and urea nitrogen in patients undergoing coronary artery bypass surgery. BMC Cardiovasc Disord. 2016;16:181. doi: 10.1186/s12872-016-0341-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cox ZL, Hung R, Lenihan DJ, Testani JM. Diuretic strategies for loop diuretic resistance in acute heart failure: the 3T trial. JACC Heart Fail. 2020;8:157–168. doi: 10.1016/j.jchf.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bovee DM, Visser WJ, Middel I, De Mik-van EA, Greupink R, Masereeuw R, et al. A randomized trial of distal diuretics versus dietary sodium restriction for hypertension in chronic kidney disease. J Am Soc Nephrol. 2020;31:650–662. doi: 10.1681/ASN.2019090905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nishi H, Toda K, Miyagawa S, et al. Effects of tolvaptan in the early postoperative stage after heart valve surgery: results of the STAR (Study of Tolvaptan for fluid retention AfteR valve surgery) trial[J] Surg Today. 2015;45(12):1542–1551. doi: 10.1007/s00595-015-1251-y. [DOI] [PubMed] [Google Scholar]
- 23.Kishimoto Y, Nakamura Y, Harada S, Onohara T, Kishimoto S, Kurashiki T, et al. Can tolvaptan protect renal function in the early postoperative period of cardiac surgery? Results of a single-center randomized controlled study. Circ J. 2018;82:999–1007. doi: 10.1253/circj.CJ-17-0967. [DOI] [PubMed] [Google Scholar]
- 24.Ito H, Mizumoto T, Tempaku H, Fujinaga K, Sawada Y, Shimpo H. Efficacy of tolvaptan on fluid management after cardiovascular surgery using cardiopulmonary bypass. J Cardiothorac Vasc Anesth. 2016;30:1471–1478. doi: 10.1053/j.jvca.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 25.Chen H, Jiang W, Li X, Meng Z, Chen H, Li J, et al. Efficacy of tolvaptan for fluid management after cardiovascular surgery: a systematic review and meta-analysis of randomized control trials. Exp Ther Med. 2020;20:2585–2592. doi: 10.3892/etm.2020.9007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tamaki S, Sato Y, Yamada T, Morita T, Furukawa Y, Iwasaki Y, et al. Tolvaptan reduces the risk of worsening renal function in patients with acute decompensated heart failure and preserved left ventricular ejection fraction- prospective randomized controlled study. Circ J. 2017;81:740–747. doi: 10.1253/circj.CJ-16-1122. [DOI] [PubMed] [Google Scholar]
- 27.Ikeda Y, Inomata T, Kida K, Shibagaki Y, Sato N, Izumi T, et al. Different diuretic properties between tolvaptan and furosemide in congestive heart failure patients with diuretic resistance and renal impairment: a subanalysis of the K-STAR. Heart Vessels. 2019;34:442–451. doi: 10.1007/s00380-018-1270-x. [DOI] [PubMed] [Google Scholar]
- 28.Kato TS, Ono S, Kajimoto K, Kuwaki K, Yamamoto T, Amano A. Early introduction of tolvaptan after cardiac surgery: a renal sparing strategy in the light of the renal resistive index measured by ultrasound. J Cardiothorac Surg. 2015;10:143. doi: 10.1186/s13019-015-0372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamada M, Nishi H, Sekiya N, Horikawa K, Takahashi T, Sawa Y. The efficacy of tolvaptan in the perioperative management of chronic kidney disease patients undergoing open-heart surgery. Surg Today. 2017;47:498–505. doi: 10.1007/s00595-016-1406-5. [DOI] [PubMed] [Google Scholar]
- 30.Kerling A, Toka O, Ruffer A, Müller H, Habash S, Weiss C, et al. First experience with Tolvaptan for the treatment of neonates and infants with capillary leak syndrome after cardiac surgery. BMC Pediatr. 2019;19:57. doi: 10.1186/s12887-019-1418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kono T, Tayama E, Hori H, Ueda T, Yamaki Y, Tanaka H. A Safety and efficacy study of tolvaptan following open heart surgery in 109 cases. Int Heart J. 2016;57:496–502. doi: 10.1536/ihj.15-483. [DOI] [PubMed] [Google Scholar]
- 32.Nakamura Y, Kishimoto Y, Harada S, Onohara T, Otsuki Y, Horie H, et al. Tolvaptan can limit postoperative paroxysmal atrial fibrillation occurrence after open-heart surgery. Surg Today. 2020;50:841–848. doi: 10.1007/s00595-020-01962-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.