Abstract
Epidural analgesia is one of the most common methods of relieving labor pain. The objective of this study was to examine the effectiveness of epidural analgesia, maternal satisfaction and relationship between the effectiveness of epidural analgesia and various factors. Data were analyzed retrospectively and collected during 2022. A total of 60 parturients participated in the study. Data were collected through a questionnaire before the parturient was discharged from the hospital. The mean assessment of pain on a 1–10 numeric rating scale before epidural analgesia was 7.7 and 3.4 after administration of epidural analgesia. The median assessment of pain before epidural analgesia was 8 (7¬¬–8), and the median assessment of pain after epidural analgesia was 3 (2–5). The average satisfaction with epidural analgesia on a 1–10 scale was 8.11, and the median satisfaction was 10 (7–10). Total of 35 (58.3%) parturients rated satisfaction with 10. Statistically significant association between the effectiveness of epidural analgesia and parity, dilution of administered levobupivacaine, fentanyl administration, and level of education was not found. Childbirth pain is significantly alleviated by the application of epidural analgesia and the satisfaction of parturients is very high.
Keywords: epidural analgesia, labor pain relief, effectiveness of epidural analgesia, maternal satisfaction
Introduction
Epidural analgesia is a central nerve block technique achieved by injection of local anesthetic close to nerves that transmit pain and is widely used as a form of pain relief in labor (1, 2). The most significant benefit of regional analgesia in childbirth during a normal pregnancy is the elimination of childbirth suffering in mothers, while in high-risk pregnancies it also ensures a safer outcome for both mother and child. It also enables the mother to be awake and actively experience childbirth and establish first contact with the newborn child. Performed technically correctly and professionally, it is not a source of complications for either the mother or the child. In case of necessity to complete the delivery by caesarean section, analgesia is very easily upgraded to regional anesthesia with application of anesthetics and analgesics via an already placed catheter, which enables relaxation of the musculature and uninterrupted work of the obstetrician (3, 4).When epidural analgesia is administered to the parturient in labor, different management choices must be made by the anesthetist: how will we initiate analgesia; how will analgesia be maintained; which local anesthetic will we use for epidural analgesia and which adjuvant drugs will we combine? (5, 6). The aim of this study is to examine the effectiveness of epidural analgesia and maternal satisfaction.
Material and Methods
Data were analyzed retrospectively and collected through a questionnaire, after delivery with epidural analgesia and before parturient was discharged from the hospital. Data were obtained from parturient and from medical records. A total of 60 parturients participated in the study. All parturients received 0.25% or 0.125% of levobupivacaine using 2 µg/ml fentanyl through intermittent bolus continuous infusion of 8-10 ml/h on epidural catheter. The pain was assessed on a 1–10 numeric rating scale (NRS) and maternal satisfaction on a 1–10 scale. Exclusion criteria were parturients with comorbidities and previous headaches (Fig. 1).
Fig. 1.
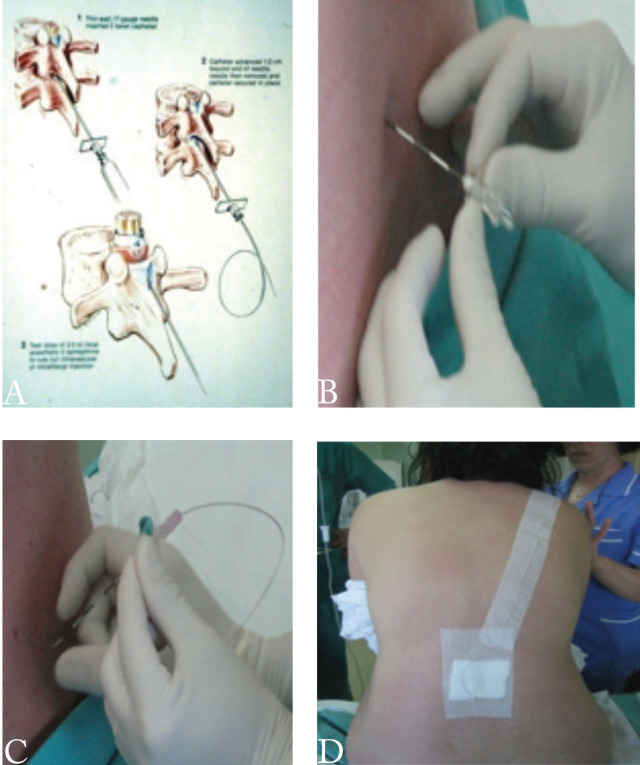
Anatomical (A) and technical application epidural needle (B) catheter (C) and fixation (D)
B initial puncture with a peridural needle and detection of peridural space by the hanging drops method; C introduction of an epidural catheter in place; D attached superficially to the skin
Ethics
This study was carried out in accordance with the Helsinki Declaration of 1975, as revised in 1983. The Ethics Committee of the University Hospital Center Osijek and the Faculty of Dental Medicine and Health Osijek approved the study. Each parturient signed informed consent to participate in the study.
Statistics
Numerical variables are age and pain assessment, described by the median, all other variables are categorical. The existence of a relationship between categorical variables was tested using the Chi-square test. For certain categorical variables, data were further grouped to perform a Chi-square test. The significance level of all tests was set to Alpha = 0.05. The statistical program used for statistical analysis was R Core Team (2020). R: A language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria; https://www.R-project.org; 2020).
Results
Basic characteristics of parturients in a single center are showed in Table 1.
Table 1. Basic characteristics of the subjects.
|
N = 60 N (%) |
|
|---|---|
| Gender | |
| Women | 60 (100.0) |
| Body mass index before pregnancy | |
| <25 | 35 (61.7) |
| >25 | 23 (38.3) |
| Weight gain during pregnancy | |
| <15 | 31 (51.7) |
| >15 | 29 (48.3) |
| Parity | |
| Primipara | 49 (81.7) |
| Secundipara | 9 (15.0) |
| Terti- and multipara | 2 (3.3) |
| Residence | |
| Village | 20 (33.3) |
| City | 40 (66.7) |
| Level of education | |
| High school level | 22 (36.7) |
| Higher and highest level | 38 (63.3) |
| Number of persons in a household | |
| Two persons | 39 (65.0) |
| Three persons | 9 (15.0) |
| Four persons | 4 (6.7) |
| More than four persons | 8 (13.3) |
The mean assessment of pain before epidural analgesia was 7.7 and 3.4 after administration of epidural analgesia (Table 2, Fig. 2).
Table 2. Assessment of pain before and after administration of epidural analgesia.
|
N = 60 N (%) |
|
|---|---|
| Assessment of pain before administration of EA* | |
| No pain (0) | 0 (0.0) |
| Mild pain (1–3) | 0 (0.0) |
| Moderate pain (4–6) | 11 (18.3) |
| Severe pain (7–10) | 49 (81.7) |
| Assessment of pain after administration of EA* | |
| No pain (0) | 8 (13.3) |
| Mild pain (1–3) | 23 (38.3) |
| Moderate pain (4–6) | 25 (41.7) |
| Severe pain (7–10) | 4 (6.7) |
*epidural analgesia
Fig. 2.
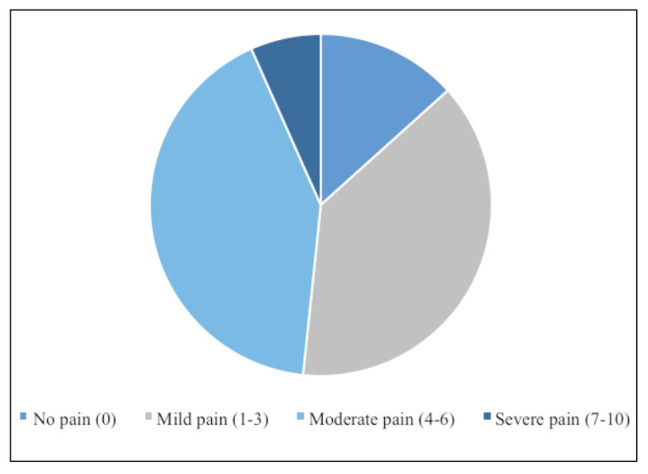
Assessment of pain after administration of epidural analgesia
The median assessment of pain before epidural analgesia was 8 (interquartile range of 7 to 8) and the median assessment of pain after epidural analgesia was 3 (interquartile range of 2 to 5). The average reduction in pain was 4.3 units on the numeric rating scale, i.e. a reduction of 55.2% (Table 3, Fig. 3).
Table 3. Reduction in pain after administration of epidural analgesia.
|
N = 60 N (%) |
|
|---|---|
| Reduction in pain after administration of EA | |
| Small or no pain reduction (0–2) | 12 (20.0) |
| Medium pain reduction (3–5) | 31 (51.7) |
| Significant pain reduction (6–8) | 17 (28.3) |
*epidural analgesia
Fig. 3.
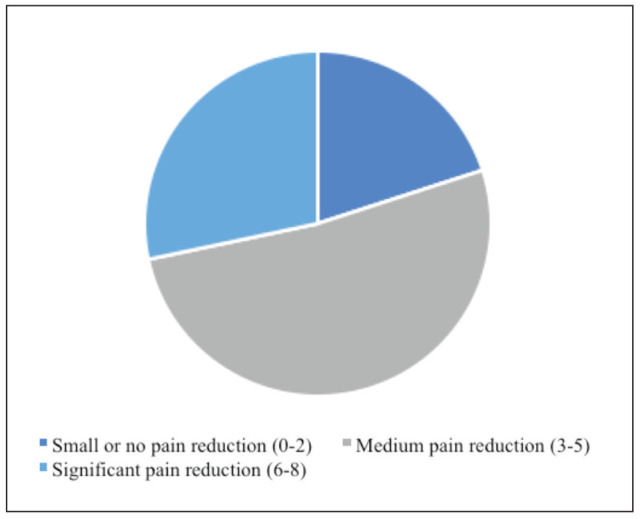
Reduction in pain after administration of epidural analgesia
The pain reduction range was between 0 and 8 units on the numeric rating scale. Lidocaine 2% was used as an epidural test dose in all subjects. Levobupivacaine was used in all subjects, in dilutions of 0.25% or 0.125%. Total of 34 parturients received one bolus, which is 56.7% of the sample. Total of 39 parturients received 0.25% levobupivacaine in at least one bolus, which is 65% of the sample. Total of 43 parturients received fentanyl in combination with levobupivacaine, which is 71.7% of the sample. Total of 36 parturients did not breastfeed in the first 60 minutes after delivery, accounting for 60% of the sample. Total of 49 mothers breastfed in the first 24 hours after delivery, accounting for 81.7% of the sample. The association between fentanyl administration and breastfeeding failure in the first 60 minutes after delivery was tested. No statistically significant association was found between fentanyl administration and breastfeeding in the first 60 minutes after delivery (Chi-squared test, P = 0.18) (Table 4)
Table 4. Breastfeeding in the first 60 minutes and 24 hours after delivery.
|
N = 60 N (%) |
|
|---|---|
| Breastfeeding in the first 60 minutes after delivery | |
| Yes | 24 (40.0) |
| No | 36 (60.0) |
| Breastfeeding in the first 24 hours after delivery | |
| Yes | 49 (81.7) |
| No | 11 (18.3) |
One parturient had a headache, which is 1.7% of the sample. Satisfaction was assessed on a scale of 1 to 10. The average satisfaction with epidural analgesia was 8.11, the median satisfaction was 10 (interquartile range of 7 to 10). Total of 35 parturients rated satisfaction with 10, which is 58.3% of the sample.
The following fears were monitored: fear of chronic pain (back pain, headache), fear of loss of feeling or movement (in legs, for example), fear of the impossibility of natural (vaginal) completion of labor due to epidural analgesia and the fear of the impact of analgesia on the newborn. Total of 25 parturients stated that they did not have any of these fears, which is 41.7% of the sample. Total of 22 parturients reported having fear of chronic pain, accounting for 36.7% of the sample. Total of 10 parturients reported having two or more fears, accounting for 16.7% of the sample showed in Table 5.
Table 5. Fears present in parturients.
|
N = 60 N (%) |
|
|---|---|
| Fears present in parturients | |
| Fear of chronic pain (back pain, headache) | 22 (36.7) |
| Fear of loss of feeling or movement | 7 (11.7) |
| Fear of the impossibility of natural (vaginal) completion of labor due to epidural analgesia | 3 (5.0) |
| Fear of the impact of analgesia on the newborn | 13 (21.7) |
| No fear | 25 (41.7) |
Parturients were categorized into those who had fear and those who did not have fear.
No statistically significant relationship was found between the level of education and fears present in parturients (Chi-squared test, P > 0.99).
Discussion
Pain relief has an important impact on women in labor. In our investigation, we confirmed the high effectiveness of epidural analgesia with levobupivacaine and fentanyl on maternal pain relief and satisfaction in relation to various factors such as complications, fear and breastfeeding. Pain intensity before epidural analgesia was 7.7 and 3.4 after administration of epidural analgesia, with a reduction of 55.2%. The need for pain relief in labor is also influenced by the type of labor onset (spontaneous or induced) and medical interventions, such as instrumental vaginal delivery and episiotomy. Several methods of relieving pain in labor and various coping strategies have been advocated, ranging from limited interventions such as breathing exercises to medical techniques like epidural analgesia. The level of pain experienced and the effectiveness of pain relief may influence a woman’s satisfaction with labor and birth and may have immediate and long‐term emotional and psychological effects (7). Women experience varying degrees of pain in labor and exhibit an equally varying range of responses to it. Our data of the presented study analyzed the average satisfaction with epidural analgesia of 8.11 (scale of 1 to 10) and 58.3% of parturients rated satisfaction with 10 points with epidural analgesia. The type of pain relief used in labor may impact breastfeeding and mother‐infant interaction (8). In our study, a total of 36 (60%) parturients did not breastfeed in the first 60 minutes after delivery, but no statistically significant association was found between fentanyl administration and breastfeeding. A total of 49 (81.7%) mothers breastfed in the first 24 hours after delivery without significant side effects and complications. Only one (1.7%) parturient had a headache.
An individual’s reaction to labor pain may be influenced by the circumstances of her labor, the environment, her cultural background, preparation for labor and the support available to her (9-11). Our parturients who had fear of chronic back pain, headache, loss of feeling or movement, natural completion of labor and fear of the impact of epidural analgesia on the newborn and those who did not have fear showed no statistically significant relationship between the middle and highest level of education and fears. Regardless of the intensity of the pain experienced and response generated, it is important that whatever method is used to ameliorate maternal discomfort, it is both effective and safe for the mother and baby.
Postpartum pain causes a number of stress responses of the organism visible in cardiovascular (hypertension, tachycardia, increased peripheral vascular resistance, total stroke volume), respiratory (hyperventilation, hypocapnia, respiratory alkalosis), neuroendocrine-adrenal stimulation adrenocorticotropic hormones, cortisol, antidiuretic hormone, renin and angiotensin II, β-endorphins, β-lipotropins, etc.), metabolic (increased need for consumption and utilization of oxygen, lactic acidosis, hyperglycemia and lipolysis), and gastrointestinal disorders, uterine (uncoordinated contractions of the uterus), uteroplacental (reduction of uteroplacental blood flow), fetal (fetal acidosis) and psychological effects (suffering, fear of the mother) (12–17). The modern obstetric analgesia in childbirth is the use of minimally invasive techniques with a selection of administered neuraxial anesthetics and analgesics, depending on the status of the pregnant woman, which will allow good analgesia without unwanted motor paralysis (18).
Conclusion
The results of our study show that childbirth pain is significantly alleviated by the application of epidural analgesia and the satisfaction of parturients very high. Although the study sample was fairly small, the incidence of complications of epidural analgesia in the form of headache is low and we can conclude that the benefit-risk balance is in favor of epidural analgesia. Categorizing the data, which was necessary due to the small sample, reduced the accuracy of the statistical tests. A larger sample is necessary in order to draw conclusions about the association of the effectiveness of epidural analgesia with various factors.
References
- 1.Wall PD, Melzack R. Wall and Melzack’s textbook of pain. 6th ed. McMahon SB, Koltzenburg M,Tracey I, Turk DC, editors. Philadelphia: Elsevier; 2013. p. 772-93 [Google Scholar]
- 2.Chestnut D. Chestnut’s Obstetric Anesthesia: Principles and Practice. 6th ed. Chestnut D, Wong C, Tsen L, Ngan Kee W, Beilin Y, Myhre J, editors. Philadelphia: Elsevier; 2019. [Google Scholar]
- 3.Bartolek D, Šakić, K. Bezboni porod// Medix,10 (2004), 54/55; 133-134
- 4.Collis RE, Plaat FS, Morgan BM. Comparison of midwife top-ups, continuous infusion and patient-controlled epidural analgesia for maintaining mobility after a low-dose combined spinal-epidural. Rev Esp Anestesiol Reanim. 1999;82(2):233–6. 10.1093/bja/82.2.233 [DOI] [PubMed] [Google Scholar]
- 5.Van de Velde M. Modern neuraxial labor analgesia: options for initiation, maintenance and drug selection. Rev Esp Anestesiol Reanim. 2009;56:546–61. [DOI] [PubMed] [Google Scholar]
- 6.Butwick AJ, Wong CA, Guo N. Maternal Body Mass Index and Use of Labor Neuraxial Analgesia: A Population-based Retrospective Cohort Study. Anesthesiology. 2018 Sep 1;129(3):448 58.doi: 10.1097/aln. 0000000000002322 [DOI] [PMC free article] [PubMed]
- 7.Christiansen P, Klostergaard KM, Terp MR, Poulsen C, Agger AO, Rasmussen KL. Long‐memory of labour pain. Ugeskr Laeger. 2002;164(42):4927–9.[ [PubMed)] [PubMed] [Google Scholar]
- 8.Walker M. Do labour medications affect breastfeeding. J Hum Lact. 1997;13(2):131–7. [PubMed] [Google Scholar] 10.1177/089033449701300214 [DOI] [PubMed] [Google Scholar]
- 9.Brownridge P. Treatment options for the relief of pain during childbirth. Drugs. 1991. January;41(1):69–80. 10.2165/00003495-199141010-00007 [DOI] [PubMed] [Google Scholar]
- 10.Wright ME, McCrea H, Stringer M, Murphy-Black T. Personal control in pain relief during labour. J Adv Nurs. 2000. November;32(5):1168–77. 10.1046/j.1365-2648.2000.01587.x [DOI] [PubMed] [Google Scholar]
- 11.Rowlands S, Permezel M. Physiology of pain in labour. Baillieres Clin Obstet Gynaecol. 1998. September;12(3):347–62. 10.1016/S0950-3552(98)80071-0 [DOI] [PubMed] [Google Scholar]
- 12.El-Boghdadly K, Pawa A, Chin KJ. Local anesthetic systemic toxicity: current perspectives. Local Reg Anesth. 2018;11:35–44. 10.2147/LRA.S154512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reynolds F, Russel R, Porter J, Smeeton N. Does the use of low dose bupivacain/opioid epidural infusion increase the normal delivery rate? Int J Obstet Anesth. 2003;12(3):156–63. 10.1016/S0959-289X(03)00008-6 [DOI] [PubMed] [Google Scholar]
- 14.Fabris Kalagac L, Belci D, Šakić K, Hrgović Z, Šakić L. Do we need cephalic spread of spinal anaesthesia for caesarean section? A different approach to CSE-EVE for reducing hypotension.// Zeitschrift fur Geburtshilfe und Neonatologie,217 (2013), 4; 130-138 doi: 10.1055/s-0033-1347214 10.1055/s-0033-1347214 [DOI] [PubMed]
- 15.Šklebar I, Bujas T and Habek D.Spinal Anaesthesia-induced Hypothensia in Obstetrics:Precvention and therapy// Acta clinica Croatica,58 (2019), 1; 90-95 doi: 10.20471/acc.2019.58.s1.13 10.20471/acc.2019.58.s1.13 [DOI] [PMC free article] [PubMed]
- 16.Bagatin D, Bagatin T, Nemrava J, Sakic K, Sakic L, Deutsch J, et al. Levobupivacaine features and linking in infiltrating analgesia // Features and Assessments of Pain, Anaesthesia, and Analgesia / Rajendram, Rajkumar; Preedy, Victor R; Patel, Vinood B; Martin, Colin R (Ed.).London: Academic Press Elsevier Inc., 2022. str. 433-442 doi: 10.1016/B978-0-12-818988-7.00033-9 10.1016/B978-0-12-818988-7.00033-9 [DOI] [Google Scholar]
- 17.Šakić L, Ujević B, Šakić K, Šklebar I, Habek D. Management of massive postpartum haemorriiage after vaginal labour in multipara with primary caesarean sbction delivery // Book of Proceeding and Abstracts / Suljević, Ismet (Ed.).Sarajevo: Association for the Development of Medical Research in Bosnia and Herzegovina, 2020. str. 52-59 [Google Scholar]
- 18.Habek D and Šklebar I.Medico-Legal responsibility in management of acute and chronic pain in Obstetric// Acta clinica Croatica,58 (2019), 1; 114-117 doi: 10.20471/acc.2019.58.s1.17 10.20471/acc.2019.58.s1.17 [DOI] [PMC free article] [PubMed]


