Abstract
The effects of violence exposure on the risk of self-harming behaviors of youth in low- and middle-income countries is not well-understood. Using household survey data from one nationally representative sample and one sample from conflict-affected areas, we examined violence exposure and self-harm among Colombian youth aged 13-24. Survey-weighted prevalence ratios comparing self-harming behaviors by exposure to violence were estimated with Poisson log-linear models, controlling for age, sex, education, and food insecurity. Compared to unexposed youth, those exposed to violence in both home and community settings were 7.97 (95% confidence interval [CI]:2.72-23.36) times more likely in the conflict-affected sample, and 21.05 (95% CI: 8.80-50.34) times more likely in the national sample to report having attempted suicide. Among Colombian youth, exposure to violence as either witness or victim was associated with greater prevalence of self-harming behaviors. Youth suicide prevention programs can address exposures to violence as a risk factor for self-harm.
Keywords: suicide, self-harm, interpersonal violence, adolescent mental health
Introduction
Self-directed harm is a serious public health problem around the world, causing substantial morbidity and mortality.[1] Self-harming behaviors take many forms including fatal and nonfatal suicide attempts, suicidal ideation (planning or seriously thinking about suicide), and self-injury.[2] One of the strongest predictors of suicide is a prior suicide attempt or injurious self-harm.[3,4]
The risks of suicide ideation, attempt, and death are high during adolescence and early adulthood.[3,5] Globally, suicide is the 4th leading cause of death among 15-29 year-olds.[1] There are about twice as many suicides among males than females, but some evidence suggests female adolescents attempt suicide more often than males.[6,7]Adolescence (10-19 years) is a vulnerable period during which multiple social, physical, and emotional changes take place, and mental health problems emerge.[3,8] Adolescents’ exposure to interpersonal violence in their home or community, either as victims or as witnesses, may cause primary effects such as anxiety or depression symptoms, and secondary effects resulting from disruption of their psychosocial development trajectories, which may in turn affect their coping skills as adults.[8]
In addition to mental health disorders such as depression, known risk factors for suicide and self-harming behaviors include characteristics of the social environment.[2,5,9] For example, there is strong evidence linking poor socioeconomic conditions and diminished social support structures as important risk factors for suicide and self-harm.[10,11] Exposure to violence is one particularly salient feature of social environments that can contribute to trauma, psychological distress, and self-harming behaviors.[8,12]
The majority of suicides (77%) occur in low- and middle-income countries.[1] In Colombia, suicide mortality rates had been declining from 2000 to 2015, but have increased in recent years.[13-15] A 2009 analysis of the National Mental Health Study in Colombia estimated a 12.4% lifetime prevalence of suicidal ideation and 4.7% lifetime prevalence of suicide attempt among Colombian adults.[16] In 2018, Colombia’s national suicide rate was 5.9 deaths per 100,000 population, below the global average, but a 30% increase from 2009.[15] The rate of increase was highest among young people: approximately half of all suicide deaths in 2018 were among those aged 15-29 years.[11,15,17]
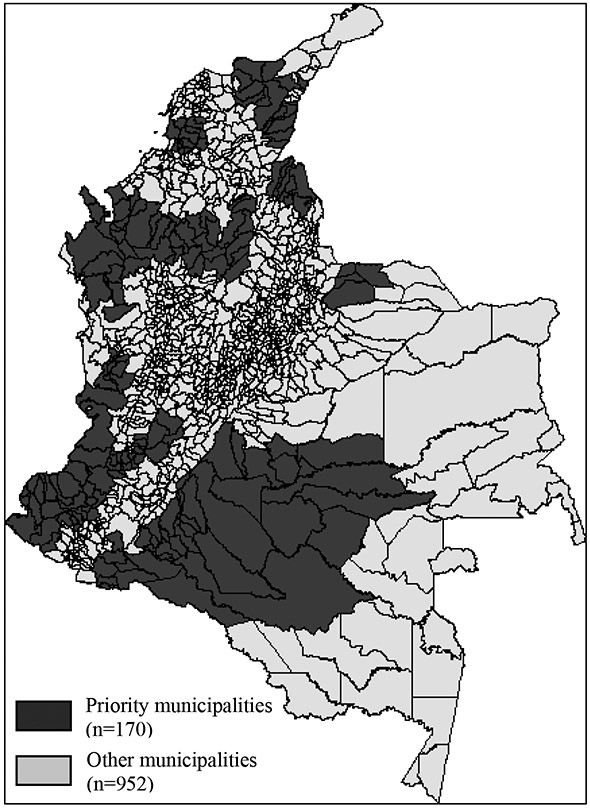
Exposure to community violence is relatively common in Colombia, where low-intensity, asymmetric armed conflict has simmered for over half a century. As a result of chronic violence and forced displacement, Colombia is home to one of the world’s largest internally-displaced persons (IDP) populations, and around 30% of the population nationally has been officially registered as victims of the armed conflict.[18] In 2013, the Colombian government announced a Territory-Focused Development Plan (PDET in Spanish) initiative which designated 170 municipalities (out of 1100 in the country) which had been most affected by the armed conflict with targeted development programs and designated as ‘priority’ municipalities.[19,20] The priority municipalities were selected because they were most affected by violence, poverty, and reduced institutional presence as a result of the armed conflict.[20] These priority municipalities disproportionately impacted by the armed conflict collectively represent 24% of the national population, and comprise 36% of the national territory.[21]
Forced displacement and exposure to the armed conflict have been found to be associated with multifaceted stressors and resulting trauma, among other negative mental and physical health outcomes.[22] Due to the intersectional and cyclical natures of violence, chronic exposure to violence in the community also increases risk of violence in other domains, such as the home.[23] Sometimes referred to as family or domestic violence, violence directed at intimate partners or children within the home environment tends to be recurrent, and has documented detrimental effects on children.[24,25]
The effects of exposure to interpersonal violence in the home and community on the risk of self-harming behaviors and psychological well-being of youth in low- and middle-income countries is not well-understood.[5,26] In settings with chronic or pervasive community violence, this relationship, as well as any mediating risk or protective factors, are even less defined.[7,27] In this cross-sectional study, we sought to examine psychological distress and self-harming behaviors among youth and young adults in relation to exposure to interpersonal violence, conceptualized in two different ways. First, we compared direct violence victimization to indirect exposure, or witnessing someone else being attacked. Second, we compared exposures (both direct and indirect) to violence in the home and community domains. We evaluate these associations in two separate, national samples of data collected by the 2018 Violence Against Children Survey (VACS) in Colombia. One of the VACS samples is nationally-representative, while the other is representative of the priority-designated municipalities disproportionately affected by the internal armed conflict.
Materials and Methods
Data
We used data from the Violence Against Children and Youth Survey (VACS) administered in Colombia in 2018. For this round of the VACS survey in Colombia, two samples were drawn and surveyed: The first is a nationally-representative sample of youth aged 13-24 in Colombia (‘National Sample’). The second sample was designed to be representative of ‘priority municipalities’ (‘Priority Sample’). One hundred and seventy municipalities (out of 1222 total) were designated as priority municipalities, as described above. The priority sample of VACS was drawn from a stratum representative of these 170 municipalities. In the national sample, a 20% oversample from specific areas of Colombia’s 4 largest cities was also drawn.[20,28]
The Colombia VACS sampling and survey methodology has been previously described.[28] Briefly, a probabilistic subsample of adolescents aged 13-24 was drawn from a nationally representative sample of households that were selected through a multistage, clustered design. A similar process was followed to be representative of adolescents living in households in the priority municipalities. Data collection for male and female respondents were conducted in separate secondary sampling units (SSUs) to protect confidentiality of selected participants. In the national sample, 43 out of 662 selected SSUs were not able to be surveyed due to the presence of community violence, inaccessibility, or inclement weather. Thirty eight of 554 selected SSUs were not surveyed in the priority sample for the same reasons. Some survey responses were missing data on outcomes, which are noted in the tables. These missing responses accounted for less than 5% of the data and were excluded from regression analyses.
Measures
Exposure to violence
Survey respondents were interviewed about their experiences with multiple forms of physical violence, including intimate partner violence, peer violence, family violence, and community violence. We chose to focus on family and community violence in this analysis, because they were most likely to apply to the general study population of youth aged 13-24. For example, situations of peer violence may be misclassified by older respondents who are likely not attending school, and there could be ambiguity between ‘peers’ and ‘adults in the community’. For both home and community violence exposures, respondents were asked about experiences wherein they were directly victimized, and about experiences when they witnessed violence perpetrated against someone else. Questions about indirectly witnessing violence (in the home or community) were restricted to events witnessed before age 18 for respondents aged 18-24, while respondents aged 13-17 were instructed to include violence witnessed at any time in their lifetime. For questions relating to direct victimization, all respondents were to include any events that occurred in their lifetime. All measures of violence exposure were originally collected in terms of frequency, but in this analysis they were dichotomized.
Direct & indirect victimization
Direct victimization by community violence was measured by positive endorsement that the respondent had ever been attacked by either (a) adults in the community, including teachers, police, community leaders, neighbors, or strangers; or (b) other people their own age, not including romantic partners. Direct victimization was measured if it occurred at any point in the respondent’s lifetime. For each form of physical violence exposure, questions about several methods of physical attacks were elicited specifically, including whether the community member slapped, pushed, punched, kicked, beat with an object, choked, smothered, burned, tried to drown, or used or threatened the respondent with a knife, gun or other weapon. Direct victimization by home violence was similarly measured by positive endorsement that the respondent had ever been attacked by a parent, adult caregiver, or adult relative. The format and listed methods of physical attack are consistent between all forms of violence.
Indirect victimization was measured by several survey questions that asked whether the respondent had witnessed someone get attacked in various contexts. For the questions regarding witnessing violence, respondents aged 13-17 were instructed to include attacks they witnessed at any age, while respondents aged 18-24 were asked about witnessing the same types of attacks before the age of 18. Witnessing community violence was measured by (dichotomized) positive endorsement to either of the following questions: “Outside of your home and family environment, how many times did you see anyone get attacked?” and “In a situation of combat within the internal conflict, how many times did you see anyone get attacked?”. Witnessing violence in the home was measured by (dichotomized) positive endorsement to either of the following: “How many times did you see or hear your mother or step-mother being punched, kicked, or beaten up by your father or step-father?” and “How many times did you see or hear a parent punch, kick, or beat your brothers or sisters?”.
Home and community violence
When comparing violence exposures in the home and community, direct and indirect victimization were combined within each realm. In other words, a respondent was considered exposed to home violence if they witnessed violence perpetrated by a father/step-father against a mother/step-mother, or against a sibling, or if the respondent themself had been violently victimized by a parent or adult relative. Similarly, respondents were recorded as exposed to community violence if they witnessed someone attacked outside their home environment, witnessed someone attacked in a situation of combat within the armed conflict, or if they themself had been physically attacked by a peer (excluding intimate partners) or by an adult in the community.
Self-harming behaviors & psychological distress
A 6-item series of screening questions known as the Kessler psychometric distress scale (K6) was included in each survey.[29,30] Respondents were asked how often in the past 30 days they felt nervous, restless, worthless, so sad that nothing could cheer them, that everything was an effort, and hopeless/anxious. Each of these scale items had 5 response options of frequency, so the possible scores ranged from 0-24. Moderate psychological distress was indicated by a K6 score of 5 or higher. This optimized threshold was found to be 75% sensitive and 75% specific in classifying individuals who needed clinical care for mental health.[31] The K6 scale has been validated in several languages and diverse settings, including Spanish-speaking populations.[29,31]
Self-harming behaviors were measured by positive response to the question, “Have you ever intentionally hurt yourself in any way?”. It is important to note that the question does not include any specification about whether there was suicidal intention. Suicidal ideation was measured by response to the question “Have you ever thought about killing yourself?” and for those answering yes to that question, they were asked about suicide attempts by the question, “Have you ever tried to kill yourself?”
Analysis
We constructed Poisson regression models with log link functions for each of the four dichotomous outcomes: suicide attempt, suicide ideation, non-suicidal self-injury, and moderate or worse psychological distress. The independent variable was categorical exposure to interpersonal violence. Prevalence ratios for each outcome were adjusted for age (in years), sex, educational status (highest level attending or completed), and a binary household-level indicator for food insecurity (past 12 months). For these inferential analyses, there were no missing responses to several variables, and very few missing responses to others. Specifically, in the national sample, n=3 (0.1% of N=2705) were missing responses about self-injury, n=7 (0.3%) were missing responses about suicidal ideation, and n=10 (0.4%) were missing responses about suicide attempt. In the priority sample, n=9 (0.4% of 2504) were missing responses about self-injury, and n=7 (0.3%) were missing responses to both suicidal ideation and attempt. As such, considering the substantially low frequency of missingness, we conducted complete-case analyses.
Sampling weights were applied to all descriptive statistics and regression analyses. Due to the separate sampling frames, analyses were conducted separately for the national and priority municipality samples. This is a secondary analysis of de-identified data; the Colombia VACS survey was approved by the Ethics and Research Methods Committee of the National Institute of Health in Colombia, and the Centers for Disease Control and Prevention (CDC) Institutional Review Board. All analyses were conducted in Stata version 14.2 (StataCorp, College Station TX).
Results
The analytical study population consisted of 2,705 respondents in the nationally-representative sample which covered all municipalities of Colombia. An additional representative sample from the 170 priority municipalities was drawn and corresponded to 2,504 respondents. A map of priority municipalities is shown in Figure 1. Overall demographics and exposures to violence were similar between the national and priority samples, as shown in Table 1. The proportion of males and females was nearly identical in both samples because respondent sex was included in the clustering scheme. Levels of educational attainment are also somewhat similar between the two samples. However, there were slightly more respondents in the priority sample who had never attended school (2.1%; 95% confidence interval [CI] 1.1, 3.9), or only attended primary school (9.8%; 95% CI 7.6, 12.7) compared to the national sample (Table 1). Those in the priority sample were more likely to have someone in the household officially registered as a victim of the armed conflict (44.1%; 95% CI 38.7, 49.6) compared to the national sample (20.1%; 95% CI 15.9, 25.1). However, the proportion of respondents who experienced food insecurity in the past year was similarly high in both the priority (75.8%; 95% CI 71.2, 79.9) and national (72.5%; 95% CI 67.5, 76.9) samples.
Figure 1.
Priority municipalities of Colombia
Table 1.
Distribution of key demographic variables in the national and the priority municipalities samples, Colombia VACS, 2018.
| National Sample N=2705 |
Priority Sample N=2504 |
|||
|---|---|---|---|---|
| n | Weighted Proportion (95% CI) |
n | Weighted Proportion (95% CI) |
|
| Age | ||||
| 13-17 | 1290 | 41.5 (38.3, 44.8) | 1243 | 43.0 (40.0, 46.1) |
| 18-24 | 1415 | 58.5 (55.2, 61.7) | 1261 | 57.0 (53.9, 60.0) |
| Female sex | 1406 | 48.9 (41.3, 56.6) | 1296 | 48.9 (41.8 (56.0) |
| Education Status | ||||
| Never attended school | 53 | 1.7 (0.9, 3.0) | 55 | 2.1 (1.1, 3.9) |
| Completed/attending primary | 159 | 4.9 (3.6, 6.7) | 252 | 9.8 (7.6, 12.7) |
| Completed/attending secondary | 1833 | 69.6 (65.7, 73.2) | 1835 | 69.3 (65.4, 72.9) |
| Higher than secondary | 656 | 23.8 (20.3, 27.7) | 359 | 18.9 (15.6, 22.6) |
| Race/Ethnicity | ||||
| Indigenous* | 465 | 9.3 (7.2, 12.0) | 277 | 9.9 (7.7, 12.7) |
| Black/Afrocolombian | 307 | 13.6 (10.5, 17.5) | 526 | 21.2 (18.1, 24.7) |
| Mestizo | 806 | 29.8 (26.3, 33.5) | 670 | 27.4 (23.1, 32.2) |
| None of the above | 828 | 33.6 (29.1, 38.3) | 678 | 26.9 (22.9, 31.2) |
| Don’t know | 297 | 13.7 (10.2, 18.1) | 352 | 14.6 (11.4, 18.5) |
| Experienced food insecurity past year | 1537 | 72.5 (67.5, 76.9) | 1686 | 75.8 (71.2, 79.9) |
| Household registered in victim’s unit | 430 | 20.1 (15.9, 25.1) | 961 | 44.1 (38.7, 49.6) |
| Victimized | ||||
| Physical violence by adult in community | 189 | 7.3 (5.3, 10.0) | 158 | 5.2 (4.0, 6.8) |
| Physical violence by peer | 673 | 27.4 (22.7, 32.7) | 589 | 23.7 (20.3, 27.6) |
| Physical violence by parent/adult relative | 528 | 19.6 (16.5, 23.1) | 515 | 22.6 (19.1, 26.5) |
| Witnessed violence | ||||
| Witnessed physical violence against mother | 561 | 20.0 (16.5, 24.1) | 526 | 19.7 (16.9, 22.9) |
| Witnessed physical violence against siblings | 564 | 25.2 (21.1, 29.8) | 465 | 20.5 (17.1, 24.3) |
| Witnessed someone attacked outside of home | 1450 | 53.0 (48.5, 57.4) | 1155 | 49.7 (45.1, 54.3) |
| Witnessed attack in conflict-related battle | 360 | 16.3 (13.2, 20.0) | 441 | 19.0 (15.7, 22.9) |
| Safety | ||||
| Stayed home for fear of threats/extortion | 228 | 11.5 (8.6, 15.3) | 303 | 11.4 (9.1, 14.2) |
| Stayed home for fear of police/military violencea | 104 | 6.0 (4.0, 9.1) | 190 | 8.9 (6.8, 11.5) |
| Carried any weapon past 30 days | 192 | 8.8 (6.2, 12.3) | 180 | 8.2 (6.3, 10.7) |
| Self-Harming Behaviors | ||||
| Harmed self | 300 | 11.6 (9.0, 14.7) | 263 | 9.7 (7.5, 12.4) |
| Suicidal ideation | 364 | 12.0 (9.1, 15.7) | 277 | 11.2 (8.7, 14.3) |
| Attempted suicide | 197 | 7.3 (5.2, 10.2) | 144 | 4.1 (3.0, 5.5) |
| Substance Use | ||||
| Drug use past 30 days | 164 | 5.6 (3.6, 8.8) | 72 | 2.7 (1.6, 4.5) |
| Binge drinking (4+ drinks)b | 844 | 36.7 (31.8, 41.8) | 764 | 34.0 (29.8, 38.3) |
| Psychological Distress | ||||
| None or low mental distress | 1504 | 56.3 (51.5, 60.9) | 1469 | 60.4 (56.0, 64.7) |
| Moderate mental distress | 1041 | 38.5 (34.0, 43.2) | 913 | 35.5 (31.4, 39.8) |
| Serious mental distress | 154 | 5.3 (3.6, 7.6) | 124 | 4.1 (3.0, 5.6) |
includes Raizal of the Archipelago and Palenquero of San Basilio
Missing n = 229 in priority sample; missing n=187 in national sample
Missing n=263 in priority sample; missing n=370 in national sample
Proportions of exposure to physical violence within the household—both in terms of violent victimization and witnessing violence directed at someone else—were somewhat similar between the two samples (Table 1). For example, in the national sample, 19.6% (95% CI 16.5, 24.1) had been violently victimized by a parent or adult relative in the past year, while 20.0% (95% CI 16.5, 24.1) witnessed physical violence against their mother and 25.2% (95% CI 21.1, 29.8) witnessed physical violence against a sibling. In the priority sample, 22.6% (95% CI 19.1, 26.5) were violently victimized by a parent or adult relative, while 19.7% (95% CI 16.9, 22.9) witnessed violence against their mother and 20.5% (95% CI 17.1, 24.3) witnessed violence against a sibling. Approximately half of respondents in both the national sample (53.0%; 95% CI 48.5, 57.4) and the priority sample (49.7%; 95% CI 45.1, 54.3) reported witnessing someone being attacked outside of their home. The proportions of respondents who had witnessed someone attacked in the context of battle related to the armed conflict were not significantly different between the two samples: 19.0% (95% CI 15.7, 22.9) of participants in the priority sample and 16.3% (95% CI 13.2, 20.0) of participants in the national sample had witnessed a battle-related attack.
Table 2 provides the prevalence of each grouping of violence exposure in the national and priority samples. Overall, the prevalence of exposures to violence were similar in the two samples. In both the national and priority sample, approximately 30% of respondents were exposed to (i.e., either witnessed or were victimized by) violence both in the home and the larger community. There were slightly more differences in violence exposure between the samples when grouping violence exposure by witnessing and direct victimization by violence. In the national sample, 28.4% (95% CI 24.6, 32.4) of respondents neither witnessed nor were victimized by violence in the home or community, compared to 32.6% (95% CI 28.5, 37.0) in the priority sample. The prevalence of having witnessed violence, but not having been personally victimized, was slightly higher in the national sample; 34.1% (95% CI 30.0, 38.4) of respondents in the national sample and 30.8% (95% CI 27.2, 34.8) of respondents in the priority sample had seen someone being attacked, but had not been attacked themselves. Approximately one-third of respondents in each sample (31.3% [95% CI 26.9, 36.1] in the national sample and 30.2% [95% CI 26.5, 34.2] in the priority sample) had both witnessed violence against someone else, and had been violently victimized themselves.
Table 2.
Distribution of population by exposures to community or home violence and witnessing versus not witnessing violence, Colombia VACS, 2018.
| National Sample, N=2705 |
Priority Sample, N=2504 |
|||
|---|---|---|---|---|
| n | w% (95% CI) | n | w% (95% CI) | |
| Exposure Grouping 1 | ||||
| Neither home nor community violence | 806 | 27.7 (24.0, 31.6) | 825 | 31.7 (27.6, 36.1) |
| Home violence, no community violence | 219 | 10.0 (7.3, 13.5) | 258 | 10.1 (8.0, 12.6) |
| Community violence, no home violence | 877 | 32.3 (28.7, 36.2) | 711 | 28.8 (25.3, 32.6) |
| Home and community violence | 803 | 30.0 (25.7, 34.8) | 710 | 29.4 (25.8, 33.2) |
| Exposure Grouping 2 | ||||
| Neither witnessed nor victimized by violence | 822 | 28.4 (24.6, 32.4) | 856 | 32.6 (28.5, 37.0) |
| Witnessed violence, not victimized by violence | 891 | 34.1 (30.0, 38.4) | 740 | 30.8 (27.2, 34.8) |
| Victimized by violence, did not witness violence | 156 | 6.3 (4.2, 9.2) | 180 | 6.4 (4.8, 8.5) |
| Witnessed and victimized by violence | 831 | 31.3 (26.9, 36.1) | 726 | 30.2 (26.5, 34.2) |
Reports of psychological distress and self-harming behaviors by exposure to violence are presented in Tables 3A & 3B. In both samples, the prevalence of psychological distress and self-harming behaviors were higher among those who were exposed to community violence, compared to those who were not exposed to community violence (Table 3A). For example, in the national sample, 10.1% (95% CI 6.9, 14.5) of those who were exposed to community violence had attempted suicide, compared to 2.6% (95% CI 1.2, 5.9) of those who were not exposed to community violence. In the priority sample, 46.5% of respondents (95% CI 41.2, 52.0) who were exposed to violence in the community reported moderate or worse psychological distress, compared to 29.7% (95% CI 24.2, 36.0) of those who were not exposed to community violence. Similar patterns were observed when looking at psychological distress and self-harming behaviors by exposure to violence in the home (Table 3B). In the national sample, 55.2% (95% 47.6, 62.5) of those who were exposed to violence at home reported moderate or worse psychological distress, compared to 36.1% (95% CI 30.3, 42.3) of those who were not exposed to violence at home; this difference was even larger in the priority sample. Similarly, 12.3% (95% CI 8.5, 17.5) of those who were exposed to home violence in the national sample reported having attempted suicide, compared to 3.9% (95% CI 2.3, 6.6) of those who had not been exposed to violence at home.
Table 3.
Psychological distress and self-harming behaviors by exposure to community violence and home violence among national and priority municipalities populations, Colombia, VACS, 2018.
| Psychological distress | Non-suicidal self-injury* |
Suicidal ideation** | Suicide attempt† | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Exposure Group | n | w% (95% CI) | n | w% (95% CI) | n | w% (95% CI) | n | w% (95% CI) |
| National Sample | ||||||||
| Exposed to community violence, N=1680 | 836 | 47.3 (42.3, 52.4) | 241 | 14.4 (11.1, 18.3) | 281 | 15.4 (11.7, 20.1) | 158 | 10.1 (6.9, 14.5) |
| Not exposed to community violence, N=1025 | 359 | 37.8 (30.9, 45.2) | 59 | 6.9 (4.3, 10.9) | 83 | 6.4 (3.9, 10.2) | 39 | 2.6 (1.2, 5.9) |
| Exposed to violence at home, N=1022 | 563 | 55.2 (47.6, 62.5) | 174 | 16.6 (12.4, 21.8) | 216 | 18.0 (13.1, 24.2) | 127 | 12.3 (8.5, 17.5) |
| Not exposed to violence at home, N=1683 | 632 | 36.1 (30.3, 42.3) | 126 | 8.2 (5.6, 11.9) | 148 | 8.0 (5.5, 11.5) | 70 | 3.9 (2.3, 6.6) |
| Priority Sample | ||||||||
| Exposed to community violence, N=1421 | 703 | 46.5 (41.2, 52.0) | 206 | 14.0 (10.7, 18.3) | 221 | 15.7 (12.0, 20.3) | 116 | 5.6 (4.1, 7.6) |
| Not exposed to community violence, N=1083 | 331 | 29.7 (24.2, 36.0) | 57 | 3.6 (2.4, 5.3) | 56 | 4.9 (2.7, 8.9) | 28 | 1.9 (1.1, 3.5) |
| Exposed to violence at home, N=968 | 501 | 55.5 (49.2, 61.6) | 157 | 15.9 (12.4, 20.3) | 186 | 21.0 (16.0, 27.0) | 97 | 6.8 (4.6, 9.8) |
| Not exposed to violence at home, N=1536 | 535 | 29.5 (25.0, 34.5) | 106 | 5.7 (3.7, 8.7) | 91 | 5.0 (3.3, 7.3) | 47 | 2.4 (1.6, 3.6) |
w%: weighted proportion; CI: confidence interval
All models adjusted for: age, sex, education level, and food insecurity
missing n=9 in priority sample, n=3 in national sample
missing n=7 in priority sample, n=7 in national sample
missing n=7 in priority sample, n=10 in national sample
Adjusted prevalence ratios for psychological distress and self-harming behaviors by exposure to home or community violence are presented in Table 4. In both samples, respondents exposed to both home and community violence were approximately twice as likely (aPR: 2.08 [95% CI 1.52, 2.85] in the nationally-representative sample, 2.45 [95% CI 1.85, 3.24] in the priority sample) to score on the K6 instrument indicating moderate or worse psychological distress, compared to their counterparts who had experienced neither form of violence. The strongest association with exposure to home and community violence was observed for suicide attempt in the nationally-representative sample (aPR 21.05 [95% CI 8.80, 50.34). In the priority sample, exposure to both home and community violence was most strongly associated with suicidal ideation, with respondents exposed to violence in both domains 9.23 (95% CI 4.84, 17.62) times as likely to report thinking about or planning suicide.
Table 4.
Adjusted prevalence ratios for psychological distress and self-harming behaviors by exposure to home or community violence
| Psychological distress | Non-suicidal self- injury |
Suicidal ideation | Suicide attempt | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Exposure Group | aPR | 95% CI p-value |
aPR | 95% CI p-value |
aPR | 95% CI p-value |
aPR | 95% CI p-value |
| National Sample | ||||||||
| Neither home nor community violence | Ref | Ref | Ref | Ref | ||||
| Home violence, no community violence | 2.09 | (1.34, 3.27) | 1.34 | (0.47, 3.81) | 5.27 | (2.14, 12.98) | 8.88 | (3.10, 25.47) |
| Community violence, no home violence | 1.66 | (1.22, 2.26) | 1.93 | (0.88, 4.25) | 5.57 | (1.49, 6.82) | 10.01 | (4.01, 25.01) |
| Home and community violence | 2.08 | (1.52, 2.85) | 3.24 | (1.50, 6.99) | 7.91 | (2.56, 12.12) | 21.05 | (8.80, 50.34) |
| Priority Sample | ||||||||
| Neither home nor community violence | Ref | Ref | Ref | Ref | ||||
| Home violence, no community violence | 1.74 | (1.21, 2.50) | 2.64 | (1.17, 5.95) | 5.05 | (2.08, 12.22) | 5.26 | (1.56, 17.79) |
| Community violence, no home violence | 1.41 | (1.03, 1.93) | 3.26 | (1.53, 6.96) | 3.18 | (1.49, 6.82) | 4.39 | (1.49, 12.91) |
| Home and community violence | 2.45 | (1.85, 3.24) | 7.38 | (4.09, 13.32) | 9.23 | (4.84, 17.62) | 7.97 | (2.72, 23.36) |
aPR: adjusted prevalence ratio; CI: confidence interval
All models adjusted for: age, sex, education level, and food insecurity
Table 5 shows adjusted prevalence ratios for psychological distress and self-harming behaviors by violence exposure type, that is, witnessing someone being attacked compared to being attacked oneself. The findings are similar to those comparing violence exposure by domain where it occurred. In the nationally-representative sample, respondents who were both directly and indirectly exposed to violence were 3.48 (95% CI 1.51, 8.02) times more likely to report non-suicidal self-injury, 10.35 (95% CI 4.92, 21.76) times more likely to report suicidal ideation and 29.05 (95% CI 12.51, 67.46) times more likely to report having attempted suicide, compared to their counterparts who were neither directly victimized by nor witnessed violence in their home or community. In the priority sample, those who had been exposed both directly and indirectly to violence were 7.25 (95% CI 4.08, 12.90) times more likely to report non-suicidal self-injury, 9.00 (95% CI 4.96, 16.31) times more likely to report suicidal ideation, and 6.56 (95% CI 2.62, 16.45) times more likely to report a suicidal attempt, compared to their counterparts who were neither directly victimized by nor witnessed violence in their home or community.
Table 5.
Adjusted prevalence ratios for psychological distress and self-harming behaviors by direct and indirect exposure to violence
| Psychological distress |
Non-suicidal self-injury |
Suicidal ideation | Suicide attempt | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Exposure Group | aPR | 95% CI p-value |
aPR | 95% CI p-value |
aPR | 95% CI p-value |
aPR | 95% CI p-value |
| National Sample | ||||||||
| Neither witnessed violence nor directly victimized | Ref | Ref | Ref | Ref | ||||
| Witnessed violence, not directly victimized | 1.78 | (1.28, 2.49) | 1.76 | (0.89, 3.46) | 4.44 | (2.04, 9.65) | 6.44 | (2.69, 15.44) |
| Violently victimized, did not witness violence | 1.81 | (1.18, 2.80) | 2.02 | (0.71, 5.79) | 9.44 | (4.63, 19.27) | 15.03 | (4.24, 53.24) |
| Witnessed and directly victimized by violence | 2.18 | (1.62, 2.94) | 3.48 | (1.51, 8.02) | 10.35 | (4.92, 21.76) | 29.05 | (12.51, 67.46) |
| Priority Sample | ||||||||
| Neither witnessed violence nor directly victimized | Ref | Ref | Ref | Ref | ||||
| Witnessed violence, not directly victimized | 1.43 | (1.07, 1.91) | 1.93 | (1.06, 3.52) | 3.38 | (1.80, 6.36) | 3.25 | (1.24, 8.51) |
| Violently victimized, did not witness violence | 1.43 | (0.93, 2.20) | 2.16 | (0.96, 4.86) | 1.09 | (0.39, 3.00) | 1.71 | (0.47, 6.24) |
| Witnessed and directly victimized by violence | 2.39 | (1.84, 3.11) | 7.25 | (4.08, 12.90) | 9.00 | (4.96, 16.31) | 6.56 | (2.62, 16.45) |
aPR: adjusted prevalence ratio; CI: confidence interval
All models adjusted for: age, sex, education level, and food insecurity
Youth who witnessed violence against someone else, but were not directly victimized, were also more likely to report negative mental health outcomes, compared to youth who were neither directly nor indirectly exposed. In the national sample, youth who witnessed violence were 4.44 (95% CI 2.04, 9.65) times more likely to report suicidal ideation and 6.55 (95% CI 2.69, 15.44) times more likely to report a suicide attempt compared to their unexposed counterparts. In the priority sample, youth who witnessed violence were 3.38 (95% CI 1.80, 6.36) times more likely to report suicidal ideation and 3.25 (95% CI 1.24, 8.51) times more likely to report having attempted suicide.
Discussion
We found significant differences in reported psychological distress and self-harming behaviors by multiple forms of exposure to violence among Colombian youth. In both the national and priority samples, those who were either directly victimized or witnessed violence more commonly reported psychological distress, non-suicidal self-injury, suicidal ideation, and suicide attempt, compared to those who experienced neither form of violence exposure. Compared to those who experienced neither form of violence exposure, those who were both directly victimized and witnessed violence were over twice as likely to report psychological distress, non-suicidal self-injury, suicidal ideation or suicide attempt, compared to those who were neither directly nor indirectly exposed to violence. In the priority sample, those who both witnessed and were victimized by violence were 9 times more likely to report suicidal ideation and nearly 7 times more likely to report suicide attempt, compared to those who experienced neither form of exposure. The magnitude of the association was even higher in the nationally-representative sample, where those who both witnessed and were victimized by violence were 10 times more likely to report suicidal ideation and 29 times more likely to report having attempted suicide, compared to their counterparts who were neither victimized by nor witnessed violence. In both samples, youth who were indirectly exposed by witnessing violence against someone else, even if they were not violently victimized themselves, were more likely to report psychological distress, suicidal ideation, and suicide attempt, compared to their peers who were neither directly or indirectly exposed.
Our findings underscore the intersectional nature of violence. Self-harming behaviors and many forms of interpersonal violence are intertwined, often co-occur, and share multiple risk factors.[23,32,33] Exposure to interpersonal violence can be particularly emotionally and psychologically traumatic to children and adolescents.[34] Interpersonal violence that occurs in a child’s home or neighborhood threaten the safety of the child’s immediate environment and induce emotional responses of fear, hopelessness, and heightened arousal, which are associated with negative mental and physical health outcomes and altered psychosocial development trajectories.[8,35] Long-term effects of violence exposure during childhood and adolescence have been linked to increased risk of poor physical and mental health into adulthood.[36] Furthermore, since home and community violence tend to be recurring, repeated exposures to violence can result in prolonged states of fear or heightened arousal, which in turn alter the child’s emotional, cognitive, and behavioral development trajectories.[12]
Among Colombian youth, exposure to multiple forms of violence was associated with greater prevalence of self-harming behaviors, with particularly strong associations with suicidal ideation and attempt. We observed modest, but significant, increases in prevalence of psychological distress and non-suicidal self-injury associated with nearly all forms of exposure to violence considered. The public health framework for primary and secondary prevention of violence considers the intersecting layers of individual, interpersonal, community, and structural risk factors for multiple forms of violence. Due to the inter-related nature of self-harming behaviors and interpersonal violence among youth, it is important for prevention programs to take a comprehensive approach to both prevent violence from occurring, and to support victims who have been exposed to interpersonal violence.[33]
There were some differential findings between the conflict-affected and nationally-representative samples that future research may seek to elucidate. Our estimated prevalence of exposure to community violence—either in the context of combat, or community violence not directly related to the internal conflict—were similar between the two samples, even though the priority sample is representative of those most historically affected by the armed conflict, with a legacy of high levels of multi-dimensional poverty.[20] A recent report by the Colombian government showed clear differences in populations’ exposures to violence between PDET and non-PDET municipalities. For example, in 2019 the homicide rate was 29 per 100,000 in non-PDET municipalities in Colombia, and nearly 59 per 100,000 population.[37] Importantly, the priority sample in this study includes a 20% oversample of specific areas from 4 major cities, which are not officially PDET-designated, so it is not a direct comparison. Nevertheless, another notable distinction between PDET and non-PDET priorities is the rate of forced displacement: in PDET communities, 1300 per 100,000 population had been forcibly displaced, compared to 222 per 100,000 in non-PDET municipalities.[37] Forced displacement was not included as a form of exposure to community violence in our study, but evidence has shown that forced displacement is a traumatic experience, and involves multiple hazards and stressors including exposures to violence.[22] In Mexico, which experiences similar levels of interpersonal violence, one study of university students who were exposed to high levels of community violence found no association with several measures of psychological distress, suggesting chronic exposure to violence may normalize it or enhance resilience.[38] The effects of chronic exposure to violence, including conflict-related displacement, on self-harming behaviors is another direction for future research.
There is mixed evidence on the potential role of poverty in the relationship between violence exposure and self-harm. Some studies have found that lower resourced communities tend to be exposed to high levels of violence and have less social cohesion and lower social capital, increasing vulnerability to psychological distress and self-harming behaviors.[39-41] In other studies, lower-income communities or those exposed to high levels of neighborhood violence have been found to have greater resilience to the traumatic effects of violence exposure, likely due to protective effects of strong familial or social support networks.[42-44] Further research is required to understand the reasons for differences observed between the national and priority samples.
This study is subject to some limitations. First, the study relies on self-reported behaviors. The instruments used in the VAC surveys have been validated and interviewers are trained to solicit responses to sensitive questions, but as in all surveys on sensitive topics, responses may be subject to social desirability bias and/or recall bias. Additionally, survey sample weights were calculated based on the 2005 Colombian Population and Household Census. Considerable population movement, including conflict-related displacement, may have resulted in inaccurately portioned population weights. Due to the predominant rural to urban migration direction, inaccurate population weights would likely result in larger analytical weight assigned to survey respondents in rural areas. Finally, those who died from suicide are not included in either survey sample. Therefore, our findings may under-estimate the burden of suicide attempts and other self-harming behaviors in the study population because it does not capture individuals who completed suicide.
In conclusion, we found that direct and indirect exposure to interpersonal violence in the home and in the community were associated with significantly increased prevalence of self-reported suicide attempts and ideation among youth and young adults in Colombia. The results underscore the significance of witnessing violence directed at another, even separate from direct violent victimization, in contributing to poor mental health outcomes. Overall, our findings highlight the importance of reducing and mitigating the effects of youth exposure to violence in the home and community as part of comprehensive suicide prevention efforts.
Footnotes
Declaration of interest statement: None
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.World Health Organization (WHO). Suicide worldwide in 2019: global health estimates. Geneva: 2021. [Google Scholar]
- 2.National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. Promoting individual, family, and community connectedness to prevent suicidal behavior; strategic direction for the prevention of suicidal behavior. Atlanta: 2013. https://stacks.cdc.gov/view/cdc/5275 (accessed 16 Jul 2021). [Google Scholar]
- 3.World Health Organization. Fact Sheet: Adolescent mental health. 2020.https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed 16 Jul 2021).
- 4.Aparicio Castillo YA, Blandón Rodríguez AM, Chaves Torres N-M. Alta prevalencia de dos o más intentos de suicidio asociados con ideación suicida y enfermedad mental en Colombia en 2016. Rev Colomb Psiquiatr (English ed) 2020;49:95–100. doi: 10.1016/J.RCPENG.2018.07.002 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Preventing suicide: A global imperative. Luxembourg: 2014. https://www.who.int/publications/i/item/9789241564779 (accessed 16 Jul 2021). [Google Scholar]
- 6.PM L, P R, JR S, et al. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry 2001;40:427–34. doi: 10.1097/00004583-200104000-00011 [DOI] [PubMed] [Google Scholar]
- 7.Lim K-S, Wong CH, McIntyre RS, et al. Global Lifetime and 12-Month Prevalence of Suicidal Behavior, Deliberate Self-Harm and Non-Suicidal Self-Injury in Children and Adolescents between 1989 and 2018: A Meta-Analysis. Int J Environ Res Public Heal 2019, Vol 16, Page 4581 2019;16:4581. doi: 10.3390/IJERPH16224581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Margolin G, Gordis EB. The effects of family and community violence on children. Annu. Rev. Psychol 2000;51:445–79. doi: 10.1146/annurev.psych.51.1.445 [DOI] [PubMed] [Google Scholar]
- 9.Durkheim É Suicide : A Study in Sociology. Suicide A Study Sociol 2005;:1–374. doi: 10.4324/9780203994320 [DOI] [Google Scholar]
- 10.Dávila-Cervantes CA, Pardo-Montaño AM. Impacto de factores socioeconómicos en la mortalidad por suicidios en Colombia, 2000-2013. Gerenc y Políticas Salud 2017;16:36–51. doi: 10.11144/JAVERIANA.RGPS16-33.IFSM [DOI] [Google Scholar]
- 11.Acevedo Navas C ¿Influye la realidad económica en el suicidio?: el caso colombiano. Rev Econ del Caribe 2010;5:143–87. doi: 10.14482/rec.v0i5.1257 [DOI] [Google Scholar]
- 12.Garrido EF, Culhane SE, Raviv T, et al. Does Community Violence Exposure Predict Trauma Symptoms in a Sample of Maltreated Youth in Foster Care? Violence Vict 2010;25. doi: 10.1891/0886-6708.25.6.755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cardona D, Segura AM, Espinosa A, et al. Homicidios y suicidios en jóvenes de 15 a 24 años, Colombia, 1998-2008. Biomédica 2013;33:574–86. doi: 10.7705/biomedica.v33i4.848 [DOI] [PubMed] [Google Scholar]
- 14.Quinlan-Davidson M, Sanhueza A, Espinosa I, et al. Suicide Among Young People in the Americas. J Adolesc Heal 2014;54:262–8. doi: 10.1016/J.JADOHEALTH.2013.07.012 [DOI] [PubMed] [Google Scholar]
- 15.Instituto Nacional de Medicina Legal y Ciencias Forenses. Forensis 2018: Datos para la vida. Bogotá: 2019. [Google Scholar]
- 16.Posada-Villa J, Camacho JC, Valenzuela JI, et al. Prevalence of Suicide Risk Factors and Suicide-Related Outcomes in the National Mental Health Study, Colombia. Suicide Life-Threatening Behav 2009;39:408–24. doi: 10.1521/SULI.2009.39.4.408 [DOI] [PubMed] [Google Scholar]
- 17.Instituto Nacional de Medicina Legal y Ciencias Forenses. Forensis 2017: Datos para la vida. Bogotá: 2018. [Google Scholar]
- 18.Franco S, Mercedes Suarez C, Naranjo CB, et al. The effects of the armed conflict on the life and health in Colombia Os efeitos do conflito armado sobre a vida e a saúde na Colômbia. Cienc e Saude Coletiva 2006;11:349–61. [Google Scholar]
- 19.Staguhn J, Yayboke E, Dalton M. Colombia at a Stabilization Crossroads. Washington, D.C.: 2020. https://csis-website-prod.s3.amazonaws.com/s3fs-public/publication/200305_StaguhnYaybokeDalton_ColombiaStabilization_FINAL.pdf (accessed 14 Jul 2021). [Google Scholar]
- 20.Agencia de Renovación del Territorio. Informe de seguimiento a la implementación de los PDET. 2020;:1–165. [Google Scholar]
- 21.Agencia de Renovación del Territorio. Abecé PDET: Los Programos de Desarrollo con Enfoque Territorial. Bogotá: 2019. https://www.renovacionterritorio.gov.co/descargar.php?idFile=29067 [Google Scholar]
- 22.Shultz JM, Rose Garfin D, Espinel Z, et al. Internally Displaced ‘Victims of Armed Conflict’ in Colombia: The Trajectory and Trauma Signature of Forced Migration. Curr Psychiatry Rep 2014;16:475. doi: 10.1007/s11920-014-0475-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Decker MR, Wilcox HC, Holliday CN, et al. An Integrated Public Health Approach to Interpersonal Violence and Suicide Prevention and Response. Public Health Rep 2018;133:65S–79S. doi: 10.1177/0033354918800019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mrug S, Windle M. Prospective effects of violence exposure across multiple contexts on early adolescents’ internalizing and externalizing problems. J Child Psychol Psychiatry 2010;51:953–61. doi: 10.1111/j.1469-7610.2010.02222.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanson RF, Self-Brown S, Fricker-Elhai AE, et al. The Relations Between Family Environment and Violence Exposure Among Youth: Findings From the National Survey of Adolescents. Child Maltreat Published Online First: 2006. doi: 10.1177/1077559505279295 [DOI] [PubMed] [Google Scholar]
- 26.Aggarwal S, Patton G, Reavley N, et al. Youth self-harm in low- and middle-income countries: Systematic review of the risk and protective factors: http://dx.doi.org/101177/0020764017700175 2017;63:359–75. doi: 10.1177/0020764017700175 [DOI] [PubMed] [Google Scholar]
- 27.Vermeiren R, Ruchkin V, Leckman PE, et al. Exposure to violence and suicide risk in adolescents: A community study. J Abnorm Child Psychol 2002;30:529–37. doi: 10.1023/A:1019825132432 [DOI] [PubMed] [Google Scholar]
- 28.Government of Colombia, Ministry of Health and Social Protection. Colombia Violence Against Children and Youth Survey, 2018. Bogotá: 2019. [Google Scholar]
- 29.Stolk Y, Kaplan I, Szwarc J. Clinical use of the Kessler psychological distress scales with culturally diverse groups. Int J Methods Psychiatr Res 2014;23:161–83. doi: 10.1002/MPR.1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Green JG, Gruber MJ, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res 2010;19:4–22. doi: 10.1002/MPR.310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prochaska JJ, Sung HY, Max W, et al. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res 2012;21:88–97. doi: 10.1002/mpr.1349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bossarte RM, Simon TR, Swahn MH. Clustering of adolescent dating violence, peer violence, and suicidal behavior. J Interpers Violence 2008;23:815–33. doi: 10.1177/0886260507313950 [DOI] [PubMed] [Google Scholar]
- 33.Wilkins N, Tsao B, Hertz M, et al. Connecting the Dots: An Overview of the Links Among Multiple Forms of Violence. Oakland, CA: 2014. [Google Scholar]
- 34.Castellví P, Miranda-Mendizábal A, Parés-Badell O, et al. Exposure to violence, a risk for suicide in youths and young adults. A meta-analysis of longitudinal studies. Acta Psychiatr Scand 2017;135:195–211. doi: 10.1111/ACPS.12679 [DOI] [PubMed] [Google Scholar]
- 35.McLaughlin K Posttraumatic stress disorder in children and adolescents: Epidemiology, pathogenesis, clinical manifestations, course, assessment, and diagnosis. UpToDate. 2019.https://www.uptodate.com/contents/14345 (accessed 15 Jul 2021). [Google Scholar]
- 36.Boynton-Jarrett R, Ryan LM, Berkman LF, et al. Cumulative violence exposure and self-rated health: longitudinal study of adolescents in the United States. Pediatrics 2008;122:961–70. doi: 10.1542/peds.2007-3063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cabal Jaramillo JA, Estupiñan Heredia JS, Guzmán Coronado CA, et al. Seguridad en los Municipios PDET. Bogotá: 2020. [Google Scholar]
- 38.Gurrola-Pena GM, Esparza-Del Villar O, Balcazar-Nava P, et al. Protective Factors for the Development of Psycho-pathological Symptoms in Young Victims of Community Violence. Int J Emerg Ment Heal Hum Resil 2018;20:1–9. [Google Scholar]
- 39.Stansfeld SA, Rothon C, Das-Munshi J, et al. Exposure to violence and mental health of adolescents: South African Health and Well-being Study. BJPsych Open 2017;3:257–64. doi: 10.1192/BJPO.BP.117.004861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harpham T, Snoxell S, Grant E, et al. Common mental disorders in a young urban population in Colombia. Br J Psychiatry 2005;187:161–7. doi: 10.1192/BJP.187.2.161 [DOI] [PubMed] [Google Scholar]
- 41.Norman R, Schneider M, Bradshaw D, et al. Interpersonal violence: an important risk factor for disease and injury in South Africa. Popul Heal Metrics 2010 81 2010;8:1–12. doi: 10.1186/1478-7954-8-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schofield TJ, Conger RD, Conger KJ, et al. Neighborhood Disorder and Children’s Antisocial Behavior: The Protective Effect of Family Support Among Mexican American and African American Families. doi: 10.1007/s10464-011-9481-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wight RG, Botticello AL, Aneshensel CS. Socioeconomic Context, Social Support, and Adolescent Mental Health: A Multilevel Investigation. J Youth Adolesc 2006 351 2006;35:109–20. doi: 10.1007/S10964-005-9009-2 [DOI] [Google Scholar]
- 44.Fagan AA, Wright EM, Pinchevsky GM. The Protective Effects of Neighborhood Collective Efficacy on Adolescent Substance Use and Violence Following Exposure to Violence. J Youth Adolesc 2014;43:1498–512. doi: 10.1007/s10964-013-0049-8 [DOI] [PMC free article] [PubMed] [Google Scholar]