Abstract
Purpose:
To evaluate the incidence of severe ocular injury requiring emergent ophthalmic evaluation in visually asymptomatic patients presenting with orbital fractures.
Methods:
We performed a retrospective chart review of all adult and pediatric orbital fractures between 2012–2022 at a level 1 trauma center. Ocular injuries were categorized into severe, moderate, and mild. We evaluated symptoms, mechanism of injury, visual acuity (VA), and severity of injuries using the Cochran-Armitage and linear-by-linear tests.
Results:
Of the 2,495 cases, 1,534 had ophthalmology evaluation. The mean ± standard deviation age was 40.4 ± 20.4 years. Most patients were male (73.1%) and Caucasian (75.9%). The mean time to evaluation was 0.6 ± 2.5 days. 486 (31.7%) were visually symptomatic, 760 (49.5%) were asymptomatic, and 288 (18.8%) were unknown. Of the symptomatic, 135 (27.8%) had severe injuries, 108 (22.2%) had moderate injuries, 216 (44.4%) had mild injuries, and 27 (5.6%) had no injuries. Of the asymptomatic, 67 (8.8%) had severe injuries, 183 (24.1%) had moderate injuries, 468 (61.6%) had mild injuries, and 42 (5.5%) had no injuries. Symptoms correlated with injury severity (p-value <0.001). The most common mechanism of injury were falls (24.0%), assaults (22.2%), and motor vehicle accidents (14.8%).
Conclusions:
Visually asymptomatic orbital fractures were less likely to have severe ocular injuries; however, many patients were unable to express symptoms. Emergent ophthalmology evaluation should be considered in all patients presenting with orbital fractures, especially patients with visual symptoms or are unable to report symptoms.
Keywords: Orbital fracture, ophthalmology, adult, pediatric, trauma, ocular injury
Introduction
Orbital fractures due to trauma may cause ocular and periocular injuries that range in severity from eyelid abrasions to globe rupture.1 Studies have assessed the incidence of ocular injury associated with orbital fractures,2–4 and some have attempted to correlate the type of fracture with clinical findings such as visual acuity (VA). The appropriate timing for ophthalmology referral of orbital fractures is under debate. Although early surgical intervention may lead to improved cosmetic outcomes,5 most Oculoplastic surgeons prefer to perform orbital fracture repair after swelling has improved. The exception to a delayed orbit repair is extraocular muscle entrapment or optic nerve compression. Emergency department and trauma physicians may utilize patient symptoms to determine if an emergent ophthalmic evaluation is clinically necessary; however, given the accessibility of on-call ophthalmologists, the default practice pattern tends towards immediate referral.6–8 This places a significant burden on ophthalmologists and is not cost-effective. Data suggests that emergent evaluation by an ophthalmologist is unnecessary in visually asymptomatic patients with orbital fractures.6 Therefore, in this retrospective study, we aim to evaluate the incidence of severe ocular injury requiring emergent ophthalmic evaluation in visually asymptomatic patients presenting with orbital fractures at a level 1 trauma center. Although prior studies have investigated similar questions,9 we hope to add to the growing body of literature with a larger data set and unique patient population to further guide clinical decision-making.
Methods
We performed a retrospective chart review of all adult and pediatric patients with orbital fractures between August 2012 and August 2022, presenting to the University of Utah Hospital and Primary Children’s Hospital. Both hospitals are level 1 trauma centers in Salt Lake City that serve as a major regional referral center for Utah and the surrounding states of Idaho, Nevada, Wyoming, Montana, and New Mexico. The study was approved by the University of Utah Institutional Review Board and adheres to the Declaration of Helsinki. Data collection and handling was in accordance with the Health Insurance Portability and Accountability Act (HIPAA).
We recorded patient demographic information, including age, gender, race, and ethnicity. We also identified the mechanism of injury, type of fracture, presenting symptoms, VA, and associated injuries. International Classification of Disease (ICD) codes, both ICD-9 and ICD-10, were utilized to determine fracture location. Additional information was noted, including hospital admission, length of stay, death during the index hospitalization, and incidental ophthalmic findings.
We classified ocular injuries into one of three categories following the original classification by Mellema et al.,6 including severe injuries that may require emergent intervention, moderate injuries that may require urgent intervention, and mild injuries that may not require any intervention. We placed each patient into the highest level of injury severity based on their ocular findings. Severe injuries included ruptured globe, retinal tear/hole/detachment, vitreous hemorrhage, hyphema, traumatic optic neuropathy, extraocular muscle damage or entrapment, retrobulbar hemorrhage, orbital compartment syndrome, and conjunctival laceration. Moderate injuries included traumatic iritis, traumatic mydriasis, choroidal rupture, microhyphema or traumatic pigment dispersion, corneal abrasion, posterior vitreous detachment, and eyelid or brow laceration. Mild injuries included subconjunctival hemorrhage, conjunctival ecchymosis or chemosis, periorbital ecchymosis or edema, retinal hemorrhage, commotio retinae/Berlin edema, and cranial nerve V2 hypoesthesia.
We divided patients into two groups based on their presenting symptoms, including visually asymptomatic and symptomatic. Symptoms recorded included blurry vision, change in color, a dark curtain in vision, dark spots in vision, distorted vision, double vision, photopsia, floaters, halos, photophobia, reduced vision, shadow or dark curtain in vision, tunnel vision, and vision loss. We classified patients who reported any symptoms as symptomatic; otherwise, we classified the patient as unknown. We performed statistical analysis to assess evidence of a linear association between severity and various factors, including the presence of symptoms, the mechanism of injury, and VA using the Cochran-Armitage test and linear-by-linear test of association. We performed data analysis with R-4.13 using a p-value of 0.05 for statistical significance.
Results
We identified 2,495 patients with an orbital fracture. We included 1,534 in the study who received ophthalmology evaluation during their hospitalization. Table 1 reports the demographic data of our population. The mean ± standard deviation age was 40.4 ± 20.4 years. The most common age groups were 21–30 years (22.1%) and 31–40 years (18.1%). There were 1,121 males (73.1%) and 412 females (26.9%). The gender of one patient was unknown. Much of our population was white or Caucasian (75.9%) and not Hispanic/Latino (84.7%).
Table 1.
Baseline population data.
| N = 1,534 | |
|---|---|
| Age (years), mean ± SD | 40.4 ± 20.4 |
| Age (years), number (%) | |
| 0–10 | 79 (5.2) |
| 11–20 | 156 (10.2) |
| 21–30 | 339 (22.1) |
| 31–40 | 278 (18.1) |
| 41–50 | 215 (14.0) |
| 51–60 | 188 (12.3) |
| 61–70 | 133 (8.7) |
| 71–80 | 92 (6.0) |
| >80 | 54 (3.5) |
| Gender, number (%) | |
| Female | 412 (26.9) |
| Male | 1,121 (73.1) |
| Unknown | 1 (0.001) |
| Race, number (%) | |
| American Indian and Alaska Native | 58 (3.8) |
| Asian | 33 (2.2) |
| Black or African American | 38 (2.5) |
| Native Hawaiian and Other Pacific Islander | 30 (1.9) |
| Other | 165 (10.8) |
| Unknown | 45 (2.9) |
| White or Caucasian | 1,165 (75.9) |
| Ethnicity, number (%) | |
| Hispanic/Latino | 181 (11.8) |
| Not Hispanic/Latino | 1,300 (84.7) |
| Unknown | 53 (3.5) |
| Mechanism of injury, number (%) | |
| Assault | 341 (22.2) |
| ATV | 48 (3.1) |
| Automobile versus pedestrian | 72 (4.7) |
| Bicycle accident | 84 (5.5) |
| Fall | 368 (24.0) |
| Gunshot wound | 33 (2.2) |
| Motor vehicle accident | 227 (14.8) |
| Motorcycle accident | 64 (4.2) |
| Other (scooter, ski accident, snowmobile, etc.) | 297 (19.4) |
| Fracture laterality, number (%) | |
| Right | 657 (42.8) |
| Left | 668 (43.6) |
| Bilateral | 209 (13.6) |
| Fracture location, number (%)* | |
| Roof | 124 (8.1) |
| Lateral wall | 165 (10.8) |
| Floor | 1,462 (95.3) |
| Medial wall | 183 (11.9) |
| Unspecified | 722 (47.1) |
| Time between diagnosis and evaluation, mean ± SD | 0.6 ± 2.5 |
| Hospitalized, number (%) | 722 (47.1) |
| Length of stay (days), mean ± SD | 4.2 ± 7.9 |
| Death in hospital, number (%) | 30 (1.9) |
Abbreviations: standard deviation, SD.
Based on International Classification of Disease Codes (ICD-9 and ICD-10). 713 (46.5%) fractures contained >1 ICD code.
Fractures were on the right side in 42.8% of cases, the left side in 43.6% of cases, and bilateral in 13.6% of cases. Over 95% of fractures included the orbital floor. Seven hundred and thirteen (46.5%) cases contained fractures in more than one location. The mean time between diagnosis and ophthalmology evaluation was 0.6 ± 2.5 days. Seven hundred and twenty-two (47.1%) patients required hospital admission with a mean length of stay of 4.2 ± 7.9 days. Thirty (2.0%) patients died during their hospitalization.
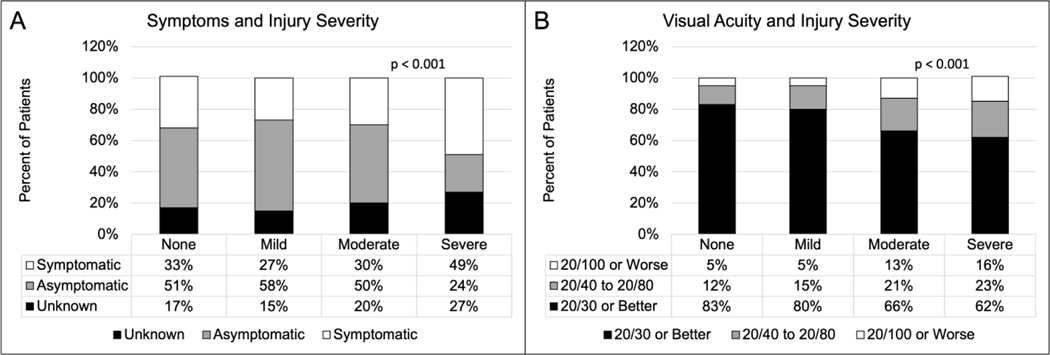
Of the 1,534 patients included, we classified 468 (31.7%) as visually symptomatic, 760 (49.5%) as asymptomatic, and 288 (18.8%) as unknown. The most common reason for symptoms being unknown was because the patient was intubated and sedated. Of the visually symptomatic, 135 (27.8%) had severe injuries, 108 (22.2%) had moderate injuries, 216 (44.4%) had mild injuries, and 27 (5.6%) had severe injuries. Of the visually asymptomatic, 67 (8.8%) had severe injuries, 183 (24.1%) had moderate injuries, 468 (61.6%) had mild injuries, and 42 (5.5%) had no injuries. Of those who had unknown symptoms, 76 (26.4%) had severe injuries, 74 (25.7%) had moderate injuries, 124 (43.1%) had mild injuries, and 14 (4.9%) had no injuries. We used the Cochran-Armitage test for trends to assess whether the proportion of patients with symptoms increased as the severity of injury increased. We excluded patients with unknown symptoms. As demonstrated in Figure 1A, the proportion of patients with symptoms increases linearly with injury severity (p <0.001).
Figure 1.
(A) Distribution of asymptomatic and symptomatic patients based on severity of ocular injury. The proportion of patients with symptoms varies linearly with injury severity (p-value <0.001). (B) Distribution of visual acuity (VA) based on severity of ocular injury. VA was linearly correlated with injury severity (p-value <0.001).
Of the 779 patients with a VA of 20/30 or better, 87 (11.2%) had a severe injury, 174 (22.3%) had a moderate injury, 465 (59.7%) had a mild injury, and 53 (6.8%) had no injury (Figure 1B). Of the 184 patients with a VA of 20/40 to 20/80, 32 (17.4%) had a severe injury, 55 (29.9%) had a moderate injury, 89 (48.4%) had a mild injury, and 8 (4.3%) had no injury. Of the 90 patients with VA of 20/100 or worse, 22 (24.4%) had a severe injury, 35 (38.9%) had a moderate injury, 30 (33.3%) had a mild injury, and 3 (3.3%) had no injury. We used the linear-by-linear association test to examine the associations between ordered variables to assess whether the VA correlated linearly with injury severity. As demonstrated in Figure 1B, a worsening VA linearly correlated with injury severity (p-value <0.001).
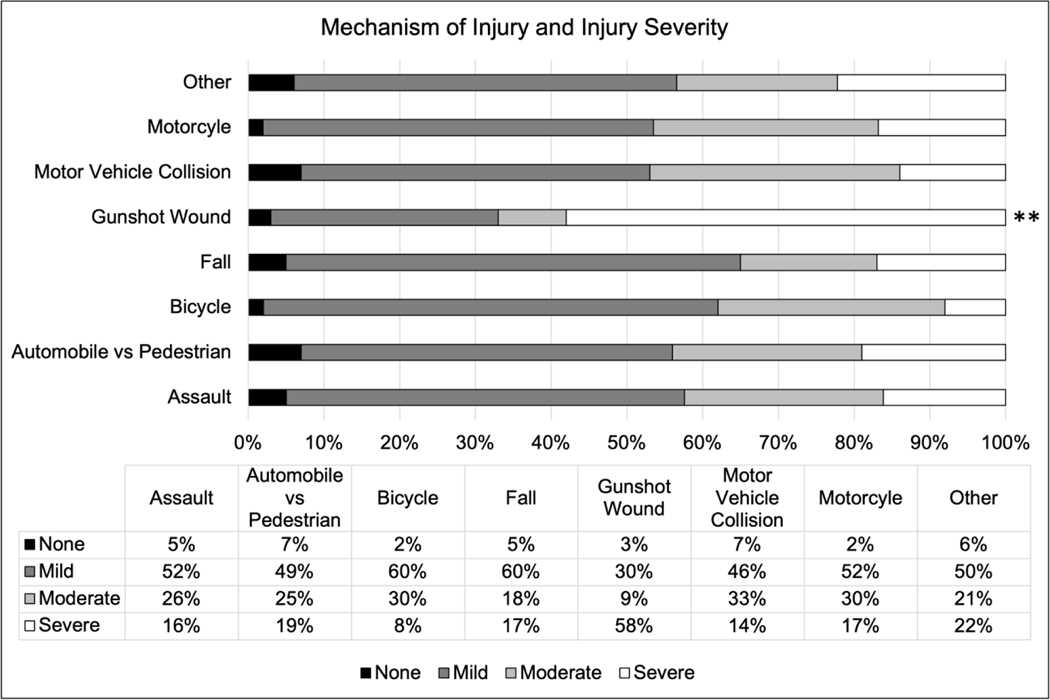
The most common mechanism of injury were falls (24.0%), assault (22.2%), and motor vehicle accidents (14.8%). Two hundred and ninety-seven (19.4%) patients had another mechanism of injury, with scooter accident (n = 16), skiing accident (n = 13), and sports-related injury (n = 11) being the most common (Supplemental Table 1). We used the Cochran-Armitage test for trend to assess for changing proportion of patients, not necessarily increasing, with each mechanism of injury versus the others across the levels of injury severity. As demonstrated in Figure 1C, the severity of injury increased with gunshot wounds (p-value <0.001). We noted a trend toward decreased injury severity with falls, but this did not reach statistical significance (p-value = 0.06).
Of the 1,534 patients evaluated, 163 (10.6%) had incidental findings. These included visually significant findings such as age-related macular degeneration (n = 8), pisciform flecks in the retina (n = 1), proliferative diabetic retinopathy (n = 1), and retinoschisis (n = 1). They also included potentially life-threatening findings such as choroidal tumor (n = 1).
Discussion
The necessity and appropriate timing of ophthalmology evaluation in the setting of orbital fractures is under debate. The mean time from diagnosis to an evaluation in our study was less than one day, highlighting the most common practice pattern in the United States of immediate ophthalmology referral.6–8 Mellema et al. performed a retrospective study evaluating the incidence of severe ocular injury in visually asymptomatic patients with an orbital fracture.6 Of the 126 patients included in the study, 46 were visually asymptomatic. Of those asymptomatic patients, zero had a severe ocular injury requiring immediate evaluation and treatment. The authors concluded that visually asymptomatic patients with an orbital fracture do not have severe ocular injuries. A retrospective study by Ross et al. included 65 patients with a routine orbital fracture and found that five had any ocular injury and zero had a severe injury.8 The authors concluded that routine orbital fractures are less likely to have ocular injuries requiring emergent ophthalmology evaluation without suspicion of severe ocular injury. Rockafellow et al. performed a combined retrospective and prospective study to determine the appropriate timing of ophthalmology consultation in the setting of orbital fractures that required surgical repair.10 Of the 84 patients included in the retrospective arm, 82 had normal post-operative exams. The remaining two patients had post-operative diplopia. Of the 39 patients included in the prospective arm, 29 did not require a preoperative ophthalmology evaluation according to their protocol. Of those 29 patients, 26 had normal post-operative exams, and the remaining three patients had diplopia. The authors concluded that routine ophthalmology consultation is not necessary for visually asymptomatic patients with orbital fractures who require surgical repair. The major limitation of these studies is the small sample size. In addition, the inclusion of only routine orbital fractures may limit the generalizability of their results.
Studies have attempted to predict the likelihood of severe ocular injury requiring emergent ophthalmology evaluation using characteristics such as fracture type and mechanism of injury.2–4 VA was considered the most sensitive predictor of severe injury;4 however, the level of clinical evidence supporting VA may be lacking.11 Therefore, Mellema et al. attempted to evaluate the presence of visual symptoms as a predictor of ocular injury severity.6 We used Mellema et al.’s ocular injury classification in our study by grouping patients into those with severe injuries that may require emergent intervention, moderate injuries that may require urgent intervention, and mild injuries that may not require any intervention. Similar to Mellema et al., most ocular injuries in our study were mild to moderate in severity. Specifically, 76.5% had mild to moderate injuries, with an additional 5.4% having no injuries. Although we found the proportion of patients with symptoms increased as the severity of injury increased, 18.8% of patients in our study were unable to report the presence of symptoms, most commonly because they were intubated and sedated. We also found that of those visually asymptomatic, 8.8% had a severe ocular injury. The discrepancy between our results and prior studies may be due to the variability in symptoms used to classify a patient as symptomatic, variability in sample sizes, inclusion criteria, and the retrospective nature of chart review not fully and accurately capturing visual symptoms. Our population also had a mortality rate of approximately 2%, suggesting a sicker population and a need for attention to life-threatening injuries – not merely vision-threatening. Future studies will evaluate the characteristics of this potentially unique population.
The reported incidence of vision loss due to orbital fractures varies widely.11 This may be due to variability in the mechanism of injury, the timing between injury and evaluation, the type of fracture, and institutional reporting practices. A systematic review by Magarakis et al. evaluating the incidence of vision loss due to facial fractures found conflicting data on fracture patterns and vision loss.11 The authors suggest that these conflicting data may be due to a lower level of evidence studies in the literature. Our study found VA to was linearly correlated with the injury severity category. However, approximately 31% of our population did not have a recorded VA due to patients being intubated and sedated, having an altered mental status, and being unable to perform the subjective exam, most commonly because of age and understanding. Surprisingly, of those patients with a visual acuity of 20/30 or better, 11.2% had a severe ocular injury. These patients may have sustained injuries that affect VA measurements to a lesser degree, such as extraocular muscle entrapment. Future studies will further characterize this group of patients.
We assess multiple mechanisms of injury, with falls, assault, and motor vehicle accidents being the most common. In addition, we saw a constellation of other mechanisms, from trampoline accidents to skiing-related injuries to plane crashes. The only mechanism of injury that was associated with severe ocular injury was gunshot wounds. Interestingly, falls were associated with lower injury severity, although the relationship did not reach statistical significance. Previous studies have demonstrated a higher likelihood of severe ocular injury with motor vehicle accidents and assault.4 Again, the discrepancy between results may be due to our increased sample size and the inherent limitations of retrospective studies. In addition, approximately 15% of our population were pediatric patients. The mechanisms of injury of pediatric orbital fractures may be different than in adult populations.12,13
Unique to our study, we collected data on incidental findings unrelated to the patient’s orbital fracture. Approximately 10% of our population had incidental findings, including vision-threatening findings such as proliferative diabetic retinopathy and potentially life-threatening conditions, such as a choroidal tumor. The question arises, how did these incidental findings influence our patient’s ophthalmic care? In addition, what percentage of our patients had their only dilated eye exam due to their orbital fracture? Further research to identify the impact of incidental findings and the likelihood that a person receives their only eye exam due to a traumatic orbital fracture is needed. Approximately 47% of our patients required hospital admission with a mean length of four days. Unfortunately, approximately two percent of our population died during their hospitalization. We did not collect data on mortality rates outside of the index hospitalization. The mortality rate seemingly demonstrates the severity of injuries often associated with high-velocity traumas resulting in orbital fractures and life-threatening injuries, such as intracranial bleeding.
Our study has limitations. First, it is a retrospective review with its inherent limitations. Our study was performed at a single institution and may not be generalizable. However, our institution does draw from numerous surrounding states and uniquely captures the population of the mountain west. In addition, we included all orbital fractures, routine and non-routine, evaluated by ophthalmology. We also included data on our pediatric population. We selected the ocular injury classification established by Mellema et al., which is not validated. However, we chose this scheme because it was the original classification for evaluating the likelihood of severe ocular injury in visually asymptomatic orbital fractures. We did not evaluate those orbital fractures not seen by ophthalmology, which may have introduced selection bias. Although we collected extensive data on the initial evaluation by ophthalmology, we did not follow our population longitudinally. A prospective analysis would be required to assess long-term outcomes in this population. Lastly, a reasonably large percentage of our patients could not express visual symptoms or provide a VA, which may have biased our results.
In conclusion, patients presenting with orbital fractures to a single institution, level 1 trauma center, were more likely to have a severe ocular injury if they were visually symptomatic, suffered a gunshot wound, or had poor VA. However, a significant percentage of patients with severe ocular injury were asymptomatic or unable to express the presence of symptoms. In addition, a substantial number of patients had incidental findings that may be vision and life-threatening. Therefore, emergent ophthalmology evaluation should be considered in all patients presenting with orbital fractures, especially those with visual symptoms and patients unable to report the presence of symptoms. However, prospective studies evaluating the necessity and timing of ophthalmology evaluation in adult and pediatric orbital fractures are needed.
Supplementary Material
Figure 2.
Distribution of mechanisms of injury based on the severity of ocular injury. Only gunshot wounds were correlated with injury severity. **, p-value <0.001.
Financial Support:
Supported in part by an Unrestricted Grant from Research to Prevent Blindness, New York, NY, to the Department of Ophthalmology & Visual Sciences, University of Utah. This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8UL1TR000105 (formerly UL1RR025764).
Footnotes
Disclosure of Interest: The authors have no financial interests to disclose.
References
- 1.Green RP, Peters DR, Shore JW, Fanton JW, Davis H. Force necessary to fracture the orbital floor. Ophthal Plast Reconstr Surg. 1990;6(3):211–217. doi: 10.1097/00002341-199009000-00012 [DOI] [PubMed] [Google Scholar]
- 2.Kreidl KO, Kim DY, Mansour SE. Prevalence of significant intraocular sequelae in blunt orbital trauma. Am J Emerg Med. 2003;21(7):525–528. doi: 10.1016/j.ajem.2003.08.009 [DOI] [PubMed] [Google Scholar]
- 3.Ocular Cook T. and periocular injuries from orbital fractures. J Am Coll Surg. 2002;195(6):831–834. doi: 10.1016/s1072-7515(02)01479-5 [DOI] [PubMed] [Google Scholar]
- 4.al-Qurainy IA, Titterington DM, Dutton GN, Stassen LF, Moos KF, el-Attar A. Midfacial fractures and the eye: the development of a system for detecting patients at risk of eye injury. Br J Oral Maxillofac Surg. 1991;29(6):363–367. doi: 10.1016/0266-4356(91)90001-l [DOI] [PubMed] [Google Scholar]
- 5.Arts HA, Eisele DW, Duckert LG. Intraocular pressure as an index of ocular injury in orbital fractures. Arch Otolaryngol Head Neck Surg. 1989;115(2):213–216. doi: 10.1001/archotol.1989.01860260087020 [DOI] [PubMed] [Google Scholar]
- 6.Mellema PA, Dewan MA, Lee MS, Smith SD, Harrison AR. Incidence of ocular injury in visually asymptomatic orbital fractures. Ophthal Plast Reconstr Surg. 2009;25(4):306–308. doi: 10.1097/IOP.0b013e3181aa9a73 [DOI] [PubMed] [Google Scholar]
- 7.Roth FS, Koshy JC, Goldberg JS, Soparkar CNS. Pearls of orbital trauma management. Semin Plast Surg. 2010;24(4):398–410. doi: 10.1055/s-0030-1269769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross M, El-Haddad C, Deschênes J. Ocular injury in orbital fractures at a level I trauma center. Can J Ophthalmol J Can Ophtalmol. 2017;52(5):499–502. doi: 10.1016/j.jcjo.2017.01.013 [DOI] [PubMed] [Google Scholar]
- 9.Akkina SR, Saurey TG, Middleton NA, et al. Factors Associated with Ocular Injury in Orbital Fracture Patients: Who Requires Urgent Ophthalmic Evaluation? Facial Plast Surg Aesthetic Med. Published online September 27, 2021. doi: 10.1089/fpsam.2021.0045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rockafellow A, Busby E, WuDunn D, Grover S, Salman SO. Evidence-Based Protocol for Ophthalmology Consult for Orbital Fractures. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2021;79(7):1507–1513. doi: 10.1016/j.joms.2021.02.026 [DOI] [PubMed] [Google Scholar]
- 11.Magarakis M, Mundinger GS, Kelamis JA, Dorafshar AH, Bojovic B, Rodriguez ED. Ocular injury, visual impairment, and blindness associated with facial fractures: a systematic literature review. Plast Reconstr Surg. 2012;129(1):227–233. doi: 10.1097/PRS.0b013e3182362a6d [DOI] [PubMed] [Google Scholar]
- 12.Imahara SD, Hopper RA, Wang J, Rivara FP, Klein MB. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207(5):710–716. doi: 10.1016/j.jamcollsurg.2008.06.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hink EM, Wei LA, Durairaj VD. Clinical features and treatment of pediatric orbit fractures. Ophthal Plast Reconstr Surg. 2014;30(2):124–131. doi: 10.1097/IOP.0000000000000026 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.