Abstract
Purpose of Review
To assess the current literature surrounding the treatment and rehabilitation strategies surrounding proximal hamstring rupture injuries, along with comparative return to sport and patient-reported outcomes.
Recent Findings
A high degree of variability exists in protective and rehabilitation strategies after both operative and non-operative proximal hamstring rupture management. Acceptable outcomes after both operative and non-operative management have been observed but may vary greatly with injury chronicity, severity, and surgical technique.
Summary
The high complication rates observed after surgical treatment, along with poor functional outcomes that may occur in the setting of non-operative treatment or delayed surgery, highlight the importance of early injury evaluation and careful patient selection. Further high-quality research elucidating clearer indications for early operative management and an optimized and standardized rehabilitation protocols may improve outcomes and return to sport experience and metrics for individuals sustaining proximal hamstring ruptures.
Keywords: Proximal hamstring rupture, Proximal hamstring avulsion, Hamstring, Return to sport, Rehabilitation, Outcomes
Introduction
Hamstring injuries (HSI) are one of the most common sport injuries, making up 12% to 16% of all sports injuries with a reinjury rate of 22 to 34% [1–6]. One study following professional football players over 10 years found the injury rate to be 0.78 per 1000 athlete exposure hours [7]. HSI can occur anywhere along the hamstring complex and range from a mild strain to a full rupture. Proximal hamstring rupture and avulsions at the ischial tuberosity or conjoint tendon make up 10% of all HSI [8]. Proximal hamstring avulsions result from eccentric contractions during simultaneous hip flexion and knee extension, and classically occur in common sporting activities such as sprinting, hurdling, waterskiing, and jumping [9•, 10, 11•, 12, 13]. When comparing gender, age, and activity, proximal HSI has been reported more commonly in males between 30 and 60 years of age, while participating in high-intensity sports [14]. Females who sustain HSI are usually between the ages of 45 and 60, with injuries taking place while performing activities of daily living [14].
The majority of HSI are intramuscular or located at the musculotendinous junction and are treated non-operatively [15, 16]. While proximal hamstring ruptures occur less frequently, they can result in significant disability if missed or misdiagnosed [15, 17].
Diagnosis of proximal HSI depends on physical examination and imaging. Physical exam findings upon inspection and palpation of the injured lower extremity include ecchymosis of the posterior thigh (most common in avulsions; Fig. 1), a prominence in the middle 1/3 of the posterior thigh, and tenderness with or without palpable defect along ischial tuberosity [9•, 18, 19]. Gait observation may identify an altered, “stiff-legged” gait due to the avoidance of simultaneous hip extension and knee flexion [18, 19]. Neuromuscular testing may be characterized by an increased popliteal angle, weakened hamstring strength with compensation by the gastrocnemius during knee flexion, and pain at the back of the thigh or even down the leg due to irritation of the sciatic nerve and its main branches of the peroneal and tibial nerves [9•, 18]. Additionally, neuropraxia of the peroneal nerve, which innervates the short head of the biceps femoris, can manifest in foot drop or, less commonly, weakness in foot eversion [20]. Patients with an acute injury may describe a “pop” and acute shooting pain in the posterior thigh and subsequently experience problems with walking on a decline or standing. Sitting pain is also a common complaint. There are multiple provocative tests including the Puranen-Orava test, bent knee stretch test, modified bent knee stretch test, active range of motion test, and taking-off-the-shoe-test which has been reported to have sensitivity and specificity of 100% (Fig. 2) [21]. An AP radiograph of the pelvis should be obtained to identify bony proximal avulsions such as may occur in younger patients, and to rule out other bone pathology [22]. Confirmatory imaging by ultrasound and MRI show similar sensitivity in acute HSI, but MRI has higher sensitivity for follow-up imaging (Fig. 3) [23].
Fig. 1.

Ecchymosis extending down the posterior thigh in a patient with a retracted 3-tendon proximal hamstring avulsion injury as seen at the time of surgery
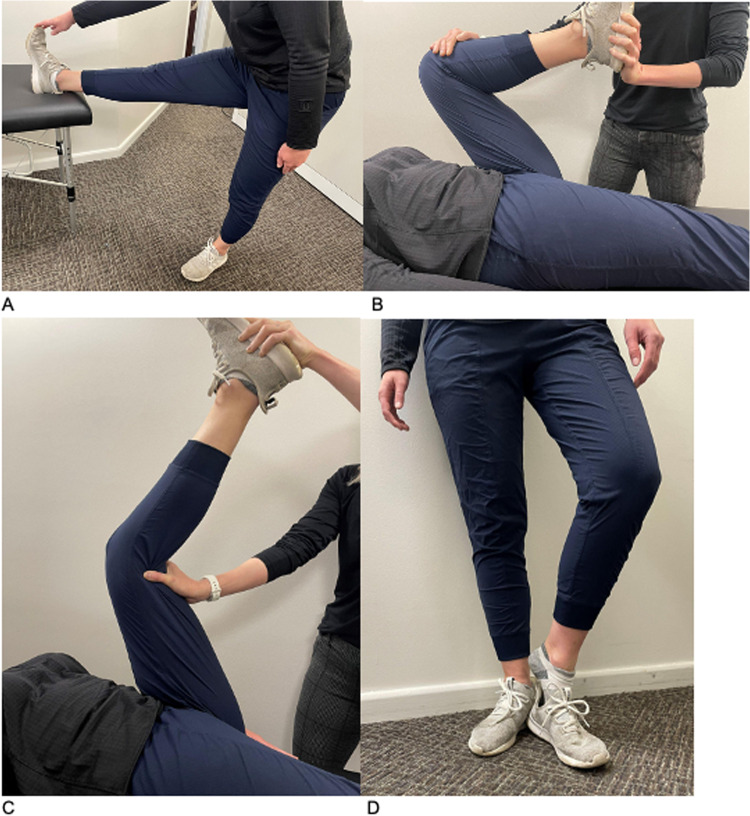
Fig. 2.
Common tests utilized in assessment of hamstring injury. A Puranen-orava. B, C Bent-knee stretch test. D Taking off the shoe. The Puranen-Orava test is performed on a low table or platform with knee fully extended and heel on platform. The patient hinges at the hips to stretch the hamstring. If pain is felt at the ischial tuberosity hamstring origination, this is a positive test. Bent-knee stretch test is performed by having the patient lay supine on the examination table. The examiner flexes both the knee and hip maximally on the patient’s affected side in line with the torso. The examiner then extends the knee. If pain is felt at the ischial tuberosity hamstring origination during knee extension, this is a positive test. Taking-off-the-shoe test is performed by having the patient stand up and capture the heel of the shoe on the affected side with the foot of their non-inured side. They are then asked to try and pull the foot of the affected leg out of the shoe while keeping the non-injured leg extended and still and hips level to the floor. This test is positive if they have difficulty completing the maneuver and/or pain in the ischial tuberosity during the attempt
Fig. 3.
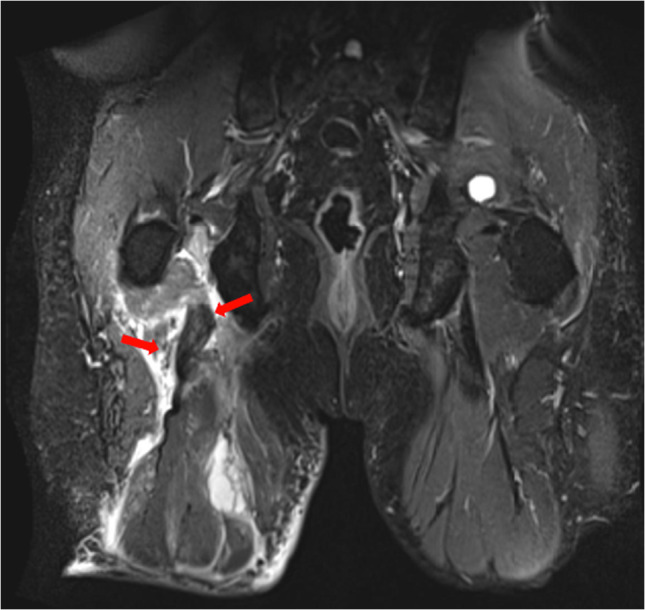
Fluid-sensitive coronal magnetic resonance imaging (MRI) of the pelvis demonstrating a right retracted 3-tendon proximal hamstring avulsion (red arrows)
Anatomy
The hamstring muscles are located in the posterior compartment of the thigh and consist of the semitendinosus, semimembranosus, and biceps femoris muscles. Each of these muscles originate at the ischial tuberosity and extend distally across the tibiofemoral joint. The semimembranosus originates from the superolateral portion of the ischial tuberosity, while the semitendinosus and biceps femoris long head originate from the superomedial portion (Fig. 4). The semitendinosus and the biceps femoris diverge approximately 10 cm distal to the origin [24]. As the semimembranosus extends distally it runs deep to the other hamstring muscles and becomes the most medial muscle as it inserts at the medial tibial condyle. The semitendinosus forms the pes anserinus along with the distal gracilis and sartorius tendons, inserting on the proximal anterolateral tibia. As the long head of the biceps femoris proceeds distally it is joined by the short head, which originates at the linea aspera along the mid-femur, forming a common muscle belly and tendon which inserts primarily at the fibular head. More complex insertional patterns have been described, involving the lateral tibia, lateral collateral ligament, joint capsule, popliteus tendon, and iliotibial tract [25–27], with one MRI-based study of 403 scans reporting an approximately 1% prevalence of complete tibial insertion of the biceps femoris [28]. Since they span the hip and knee, the hamstrings play an important role in the function of the lower extremity and pelvis. The hamstrings’ main function is extension at the hip and flexion at the knee, with secondary contributions to pelvic tilt and sacral rotation [29–31].
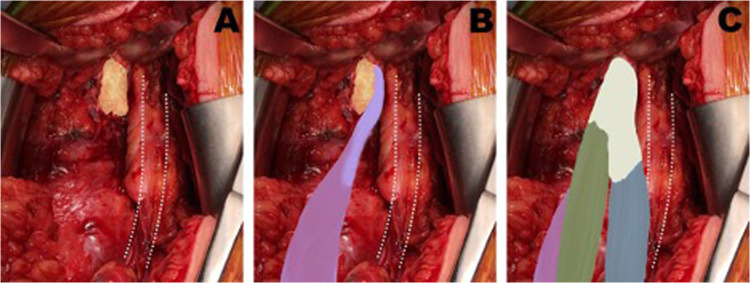
Fig. 4.
Relationships between proximal hamstring insertions and sciatic nerve (right leg). Yellow—ischial tuberosity. Purple—semimembranosus. Green—semitendinosis; blue—biceps femoris long head. White—conjoint tendon. Dotted lines—sciatic nerve. Reprinted with permission from Bertiche et al. 2020
The lumbosacral plexus gives rise to the sciatic nerve, which consists of the L4-S3 nerve roots and exits the pelvis through the greater sciatic notch, traveling 1.2 ± 0.2 cm lateral to the ischial tuberosity to continue under the biceps femoris muscle belly and eventually bifurcating into the tibial and common peroneal nerves [24]. The short head of biceps femoris is innervated by the common peroneal nerve, while the long head of biceps femoris, semimembranosus, and semitendinosus are innervated by the tibial nerve. This anatomic relationship may lead to associated nerve symptoms in some cases, and is important to recognize during surgery (Fig. 5).
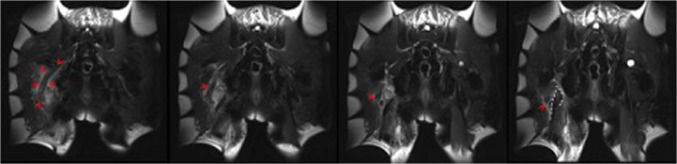
Fig. 5.
Successive coronal magnetic resonance imaging (MRI) cuts demonstrating the close relationship of the sciatic nerve (red arrows) traversing just lateral to the retracted hamstring tendons (outlined in white)
Injury Mechanism
The hamstring muscles are prone to injury because they are biarticular, crossing the hip and knee joints, allowing them to simultaneously extend the hip and flex at the knee. Rapid acceleration injuries tend to be musculotendinous or intramuscular and take place during the late swing phase just before heel strike in the running gait cycle. The late swing phase, during which the hamstrings are in eccentric contraction with the hip flexed and knee extended, is described as the common timing of this injury (Fig. 6) [32–34]. Proximal hamstring avulsions also occur during eccentric contraction, while the hip is in flexion and the knee is in extension, but in the setting of forced flexion [35–41]. These injuries, while rare overall, have been classically described in relation to high-energy forced-flexion mechanisms such as the abrupt water-skiing start in an unsafe hurdlers-type position, and in bull-riding when the hamstrings are eccentrically contracted under tension when caught in the steer’s rope [42]. They have also been shown to occur with high relative frequency in slip-and-fall accidents [43]. Additionally, one case series also described a forced flexion-abduction mechanism of proximal hamstring rupture in 2 football players and an Olympic judo competitor, who all had a similar mechanism of forced hip flexion from a fall and/or force of an opponent’s body with the knee extended and heel on the ground [44].
Fig. 6.
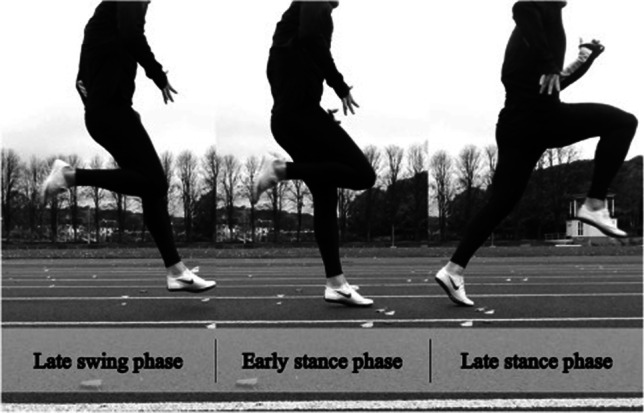
Running gait cycle, demonstrating the late swing phase that is associated with musculotendinous or intramuscular hamstring injury. Reprinted with permission from Danielsson et al.
Risk factors for hamstring injury are important to understand as they can aid in rehabilitation and preventive strategies for athletes. Non-modifiable risk factors include age, muscle composition, and previous injuries [45]. Modifiable risk factors include shortened optimal muscle length, lack of muscle flexibility, strength imbalance, insufficient warm-up, fatigue, low back injury, and increased muscle neural tension [45]. The way the hamstring heals and the quality of the new-formed scar tissue is the most important determinant of future function and risk of injury [46].
Non-operative Management
Non-operative treatment of proximal injuries is indicated for single-tendon hamstring injuries and 2-tendon tears with less than 2 cm of retraction [18, 47, 48]. Additional factors such as activity level, age, comorbidities, and ability to comply with postoperative rehabilitation may also be considered [19, 46]. However, outcomes of non-operative treatment are not as widely reported as outcomes of operative treatment, so the available evidence and algorithms may suffer from availability bias [49].
Some patients appropriately indicated for initial non-operative management may eventually elect to pursue surgical treatment. Piposar et al. found that 40% of patients in a retrospective review of 25 patients with partial thickness hamstring avulsions managed non-operatively ultimately opted for surgical treatment [50]. Appropriate patient selection for earlier operative intervention should be optimized given that scar formation and tendon retraction can increase the technical demands of delayed surgery [47, 48]. Additionally, patients treated non-operatively may be left with significant strength and functional deficits as well as an increased risk for sciatic nerve pathology due to tethering by the retracted tendons [17, 49, 51]. Incomplete tendon recovery may be expected in approximately half of patients treated non-operatively, based on the prospective study by van der Made et al. assessing outcomes of a shared decision-making model in 26 operative and 33 non-operative patients [49]. In their cohort, 100% of the operative group and 82% of the non-operative group had involvement of both the semimembranosus and conjoint tendon. At 1-year follow-up, the rate of proximal hamstring tendon discontinuity in the operative group was 5% (n = 1; MRI obtained after known reinjury), versus 48% of the non-operative group. The risks and expectations surrounding non-operative treatment of proximal hamstring avulsion injuries should be discussed as early as possible in the decision making process to allow the patient to make an informed decision. In the case of ischial tuberosity avulsion fractures in skeletally immature individuals, most are treated non-operatively, with the exception of fractures displaced more than 1.5–2 cm, where operative treatment is recommended given the risk of sciatic nerve irritation, non-union, or poor outcomes if left surgically untreated [52, 53].
Non-operative management consists of immediate initiation of phased rehabilitation that mirrors the postoperative rehabilitation protocol after the repair protection stage in the setting of operative management, described subsequently. In addition to physiotherapy and activity modification, additional non-surgical treatment strategies include the use of NSAIDs, shockwave therapy, and injection of corticosteroids or PRP serving as potentially useful adjuncts [18, 47].
Trends and Variations in Postoperative Rehabilitation
Immediate Postoperative Period
While specific rehabilitation strategies vary after proximal hamstring tendon repair, most protocols for care in the immediate postoperative period focus on protecting the repair by keeping the hamstrings in a shortened and relaxed position [20, 43]. This protective phase generally includes restricted weight bearing and hip or knee orthoses to limit knee range of motion, hip flexion, or both, depending on intraoperative and ongoing assessment of the repair and hamstring tension and range of motion [18, 43, 48, 54]. Van der Made et al. report use of cast immobilization for 2 weeks prior to bracing with a hinged knee brace [49]. Casts were applied in the operating room, with the degree of knee flexion based on intraoperative assessment of ideal tendon repair tension. Weight-bearing is progressed from 2 to 4 weeks with continuation of support with crutches until 6–8 weeks, when the orthosis is removed and specific strengthening exercises are begun. Passive hip range of motion with a physiotherapist is initiated at 2 weeks, with active hamstring exercises beginning between 4 and 6 weeks [43, 48].
Some authors have reported on less restrictive immediate postoperative protocols. Askling et al. described use of a brace only in circumstances in which the patient would be unable to keep the hamstrings in neutral position, described as knee extended and hip at 0° extension [20]. Leger-St-Jean et al. prescribed a protocol without the use of a brace and with the allowance of full weight bearing and walking with crutches as needed in their minimum 2-year outcomes study of 38 proximal hamstring repairs [54]. This protocol resulted in comparable functional outcomes and similar reinjury rates as more traditionally restrictive protocols consisting of bracing and weight-bearing restrictions, especially in the acute repair cohort [43, 55].
Rehabilitation Progression and Return to Sport
After the protective phase, physical therapy generally lasts from 4 to 6 months. The phases focus on achieving normalized and pain-free movement starting with gait and progressing to unrestricted participation in previous sport activities, using specific precautionary measures along with targeted hamstring exercises as well as hip and core strengthening and general cardiovascular conditioning. Criteria for progression may consist of parameters such as pain- and swelling-free movement at the level just below that of the next phase. However, there is no standardized postoperative protocol for rehabilitation after repair of proximal hamstring avulsion. In their observational study of online rehabilitation protocols after proximal hamstring tendon repair, Lightsey et al. found a high level of variability in the components and timing of these protocols including strengthening exercises, proprioception exercises, return to basic activity, and return to sporting activity [56]. Lunges, for example, were found to be initiated variably at timepoints ranging from 6 to 22 weeks, and were recommended in 30% of protocols (Fig. 8). Table 1 presents selected examples of the significant variability in rehabilitation protocols and their components.
Fig. 8.
Repaired hamstring before cutting sutures (right leg)
Table 1.
Selected examples of varying recommendations in rehabilitation protocols for proximal hamstring ruptures
| Rehabilitation category | Exercise or recommendation | Example | Source(s) |
|---|---|---|---|
| Immediate postoperative protection | Bracing | Hip orthosis - | [57] |
| Knee orthosis | [49, 55, 58] | ||
| Cast | [49] | ||
| No orthosis | [20, 54] | ||
| Restricted weight-bearing | Full restriction | [49] | |
| Partial restriction | [55, 58] | ||
| No restriction | [54] | ||
| Depending on use of tightness of repair and need for use of brace | [59] | ||
| Strengthening/muscle activation | Electrical muscle stimulation | [49] | |
| Pool training | [20, 43] | ||
| Proprioception/gait | Gait training | Use of anti-gravity treadmill | [49] |
| Video taping for visual feedback | [20] | ||
| Limitation of stride length | [20] |
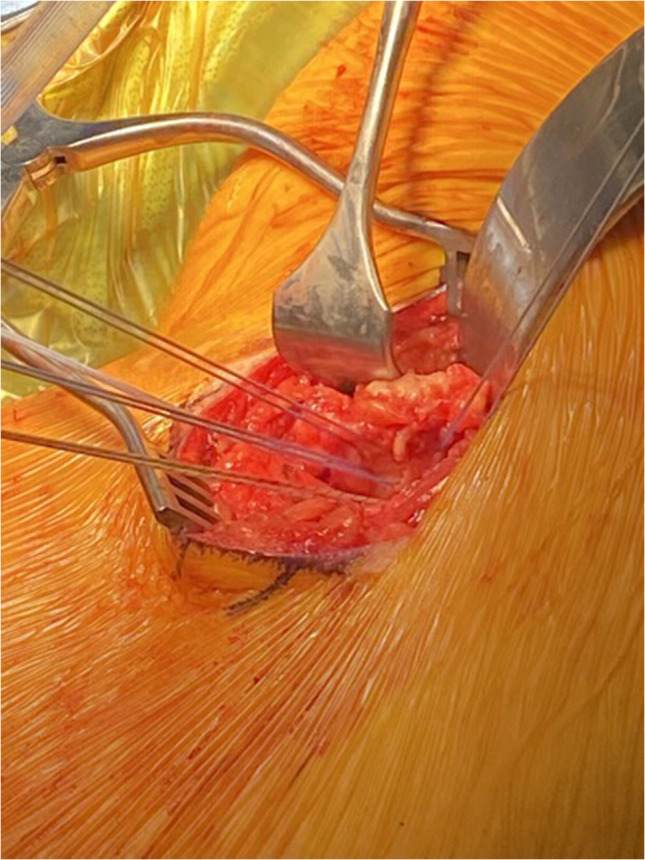
Authors’ Preferred Surgical Treatment
The patient is positioned prone on the operative table with the torso bolstered and all bony prominences padded. The entire lower extremity on the operative side is sterilely prepped and draped out. A transverse incision is created in the gluteal crease just inferior to the ischial tuberosity. Careful dissection is carried out through the underlying fat to the gluteal fascia with attention to identifying and preserving the posterior femoral cutaneous nerve deep to the gluteal musculature. Loupes may be worn to facilitate this process. The gluteal fascia is incised transversely along the inferior border of the gluteus maximus muscle which is then elevated and retracted superiorly to reveal the underlying hamstring fascia. The investing hamstring fascia is incised longitudinally exposing a second deeper “paratenon” like layer. It should be noted that some partial tears may be concealed by an intact fascial layer, and also that in some cases scar tissue in this region may create the appearance of intact tendons. It is therefore necessary to carefully review preoperative imaging to characterize the extent and location of the tear. Deep dissection is continued onto the ischial tuberosity. In more acute cases, the appropriate layer is readily identified when a large hematoma or seroma is encountered, with the ruptured tendons contained therein.
The sciatic nerve is located laterally. While dissection and mobilization of the nerve is not always necessary, especially with partial and/or less retracted tears, the surgeon should be mindful of its presence toward the lateral aspect of the dissection. A formal neurolysis is more often indicated in the setting of chronic, retracted tears, as these are more likely to scar to the nerve or in the setting of ongoing sciatic neuritis.
Once identified and mobilized (Fig. 7), the hamstring tendons are tagged with a heavy suture. The ischial footprint is debrided and abraded with periosteal elevator or curette to achieve a bleeding surface for repair. Use of a mechanical burr to prepare the tuberosity is strongly discouraged. Anchor configuration is determined by the tear pattern. For complete 3-tendon tears, 5 anchors are placed in an “X” configuration, allowing anatomic restoration of the crescent-shaped footprint of the semimembranosus and the oval-shaped footprints of the semitendinosus and biceps femoris. Knotted anchors are always used. Suture passage should aim to restore the anatomic relationship of the tendon origins with the semimembranosus laterally and the conjoint semitendinosus and biceps femoris tendon medially. Sutures are passed through the tendon in a horizontal mattress configuration and tied with the knee in at least 30° flexion (Fig. 8). The wound is then copiously irrigated and closed in layers, and the hip is placed in an orthosis limiting hip flexion to 45°.
Fig. 7.
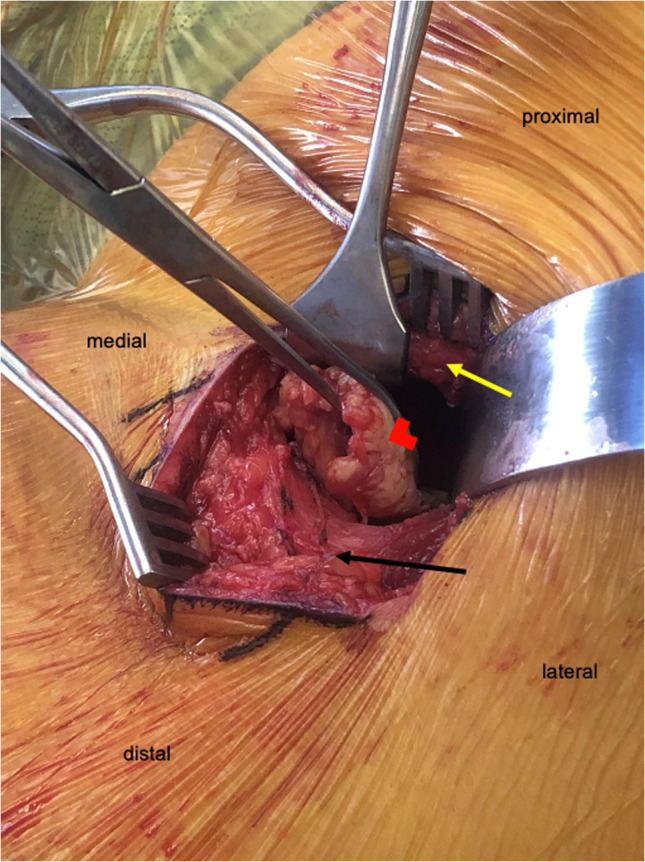
Mobilization of the avulsed hamstring tendons (right leg). Red arrowhead—hamstring tendons. Black arrow—gluteal fascia. Yellow arrow—retracted gluteus maximus
Authors’ Rehabilitation Protocol
The goal of therapy and rehabilitation is to ultimately restore motion and function while allowing the repaired tendons to heal back to the ischium. Ultimately return to athletic activities is based on isokinetic testing, and typically occurs between 6 and 10 months postoperatively.
0 to 2 Weeks Postoperatively
Patients remain toe-touch weightbearing with crutches for ambulation. The postoperative hip orthosis is maintained unlocked full-time in 45° of flexion.
3 to 5 Weeks Postoperatively
Patients progress to partial weightbearing in the brace. Passive motion of the hip and knee is initiated by the physical therapist at the beginning of the third week. Under the guidance of the therapist, patients progress to active motion at 4 weeks.
6 to 9 Weeks Postoperatively
Patients are weaned from the brace and crutches and allowed to begin full weightbearing. Therapy is directed at increasing passive and active motion. Patients may participate in aquatherapy, isometric exercises, core strengthening, and closed range exercises (Fig. 9). Isotonic strength training and dynamic exercises are initiated at 8 weeks (Fig. 10).
Fig. 9.

Isometric hamstring exercise—single leg glute bridge
Fig. 10.
Isotonic and dynamic hamstring exercises. A, B Isotonic—single leg deadlift, nordic hamstring curl. C Dynamic—alternating split squats
10 to 16 Weeks Postoperatively
An isometric strength evaluation with the knee in 60° flexion is conducted during the 10th postoperative week. If the patient exhibits appropriate strength, they may begin dry-land jogging. Therapists continue to work on improving motion, strength, and normalizing gait. An isokinetic evaluation is performed by 12 weeks, with the knee at 60°, 120°, and 180° of flexion. Results are compared with the contralateral leg, and return to sports is allowed when flexion strength of the operative leg is at least 80% of the other side.
Outcomes
Non-operative Versus Operative
Comparison of functional outcomes between non-operative and operative management of proximal hamstring ruptures is important for patient counseling and selection of the appropriate treatment option. With complication rates reported as high as 23.17% in operative cohorts, [10] the decision to proceed with operative treatment should be carefully considered, especially in an older patient population. At 1-year follow-up, van der Made et al. found operative (n = 26) and non-operative (n = 33) patients to have similar clinical outcomes and return to sport (RTS) time and rate [49]; however, post-injury MRI imaging revealed proximal continuity of the hamstring complex was restored in approximately half of non-operative patients and nearly all operative patients [60]. By contrast, Shambaugh et al. compared minimal 1-year outcomes of 11 non-operative and 14 operative patients and found non-surgical treatment of proximal hamstring ruptures to result in inferior PROs, notable hamstring weakness, and lower rates of return to sport [51]. A systematic review including 24 studies with 767 surgical patients and 28 non-surgical patients reported significantly higher patient satisfaction (90.81% vs. 52.94%), hamstring strength (85.01% vs 63.95%) Lower Extremity Functional Scale (LEFS) scores (72.77 vs 69.53), and single legged hop test results (119.1 vs 56.62 cm) (all P < 0.001) for surgical versus non-surgical treatment [10]. In terms of return to sport, there was no significant difference between the operative (79.75%) and non-operative cohorts (70.59%) (P = 0.363).
Limitations of the current literature include small sample sizes in comparative studies, large difference in cohort sizes in the systematic reviews, and lack of long-term follow-up. Such characteristics can lead to underpowered comparison studies and publication bias. Furthermore, return to sport results have been reported for heterogeneous study groups consisting of various levels of play from recreational to professional athletes. There is also a lack of consistency among outcome measurement tools reported. LEFS and mHHS are validated outcome scores while PHAT is a more recently developed score. Therefore, larger long-term prospective studies are needed to better determine if differences exist in outcomes and to what extent between non-operative and operative treatment of proximal hamstring ruptures. The proximal hamstring avulsion clinical trial (PHACT), the first randomized clinical trial on operative versus non-operative treatment of proximal hamstring avulsions, started enrollment in 2017 with 11 study sites in Europe [61••]. Sixty patients will be randomly assigned to suture anchor repair and 60 patients will undergo non-operative treatment with PROs, strength testing, and MRI imaging to be collected at 24 months. Results of this forthcoming study may help shed further light on treatment algorithms.
Acute Versus Chronic Repair
Chronicity of the proximal hamstring rupture is another important consideration when counseling patients on treatment options. The definition of acute versus chronic operative repair is variable in the literature. Shambaugh et al. compared outcomes of 93 repairs that occurred at 3 weeks (n = 47) or longer than 3 weeks (n = 46) and 6 weeks (n = 73) or longer than 6 weeks (n = 20) with no significant difference found in PROs; however, patients who underwent surgical repair more than 6 weeks from injury experienced more weakness of the operative leg compared with the contralateral side in addition to greater sitting intolerance [57]. In a systematic review, Harris et al. evaluated chronicity of repair (4 weeks vs >4 weeks) in 18 studies and found significantly better patient satisfaction and higher rate of return to pre-injury of sport in the acute repair group (91/95, 96%) versus the chronic repair group (143/191, 75%) (P < 0.001) [16]. Furthermore, acute surgery required less sciatic neurolysis (14% vs 32%, P < 0.05), less mobilization of retracted musculotendinous structures, smaller need for fractional muscle lengthening, and smaller skin incisions. Similarly, Bodendorfer et al. reported results on acute versus chronic repair, defined as (8 weeks vs more than 8 weeks), from 24 studies, which demonstrated higher satisfaction, lower pain scores and sitting pain, better strength, and higher PROs in the acute repair group [10]. Return to sport rates were not significantly different between groups. In a retrospective study, Becker et al. evaluated outcomes of 226 patients that underwent open repair with mean follow-up time of 26.2 ± 15.5 month. They found delay in surgery and female sex to be predictive factors of lower PHAT scores, while age and retraction of tendon stump on preoperative MRI did not influence PHAT scores [58].
Endoscopic Versus Open Repair
Endoscopic repair has gained traction as a minimally invasive surgical approach to address proximal hamstring avulsions; however, there is a paucity of outcomes data in the literature. Kurowicki et al. was the first retrospective study to report the outcomes of an entire cohort of endoscopic proximal hamstring repairs, including 20 patients with average follow-up of 23 months (range, 12 to 49 months). The authors found improved pain, range of motion, strength, return to sport regardless of tear severity (partial vs complete) or chronicity [62]. At mean follow-up of 44.0 ± 14.7 months, Fletcher et al. found 90% patient satisfaction, 100% return to sport and work, 73.3% complete resolution of pain, and only 3% complication and reoperation rate in 30 patients who underwent endoscopic repair [63]. For comparison of open versus endoscopic proximal hamstring repair, a multicenter comparative study was performed with 19 endoscopic repairs and 31 open repairs. The cohorts demonstrated similar PROs and satisfaction at a minimum 2-year follow-up with low rates of complications (2 open repair vs 1 endoscopic repair) [64]. Further research with larger cohorts and longer follow-up will be needed to further evaluate the efficacy and safety of the endoscopic approach. In addition, outcomes based on repair technique performed, including number of anchors and configuration, is another important area of research.
Augmentation/Reconstruction
As a relatively new technique, there is a paucity of literature reporting functional outcomes following proximal hamstring repair with augmentation of an auto- or allograft. Ebert et al. published a retrospective study including 6 patients who underwent proximal hamstring reconstruction with the ipsilateral distal hamstring tendon. At 24 months, mean knee extensor limb symmetry indices had recovered; however, a significant difference still existed between the operated and non-operated limbs in knee flexor total work [65]. Five patients (86%) were satisfied with the results of the surgery and their ability to return to activities. The remainder of available outcomes research reports mixed cohorts of repair and reconstruction or sub-analyses of the reconstruction group. Therefore, additional studies are required to validate this technique as a solution for irreparable tears or deficiencies in tissue volume.
Conclusion
Proximal hamstring ruptures are a rare but potentially debilitating injury, which, if not evaluated and treated adequately, can lead to substantial functional limitation and poor patient-reported outcomes. The dynamic biomechanics and complex anatomy of the hamstrings, along with their close spatial relationships with the sciatic nerve and its branches lead to variable presentations after proximal rupture injury functionally and on specific physical examination. While there is not a definitive consensus around the indications for operative versus non-operative management of these injuries, available data support the fact that delayed treatment, and some cases of non-operative treatment, result in functional deficits and poorer outcomes. Surgical intervention has demonstrated good functional outcomes and high return to sport rate, however, further studies examining larger patient populations with longer-term follow-up are needed to validate the efficacy of this intervention, including comparison of contrasting surgical techniques and complications. Depending on extent of injury, patient age, and activity level, non-operative treatment with appropriate rehabilitation can be considered and, in carefully selected patients, may lead to comparable outcomes. Rehabilitation protocols vary widely both in composition and timing, and patient outcomes may be improved with further research and systemization regarding the optimal rehabilitation process after proximal hamstring ruptures.
Declarations
Conflict of Interest
Austin Looney, Hannah Day, Spencer Comfort, and Stiles Donaldson declare that they have no conflict of interest. Stephen Cohen reports consulting fees from Zimmer Biomet Holdings, Inc., non-financial support from Zimmer Biomet Holdings, Inc., and Boston Scientific Corp., and educational fees from Liberty Surgical.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Sports Injuries and Rehabilitation: Getting Athletes Back to Play
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Austin M. Looney, Email: austin.looney@gmail.com
Hannah K. Day, Email: hkd14@georgetown.edu
Spencer M. Comfort, Email: smc358@georgetown.edu
Stiles T. Donaldson, Email: std24@georgetown.edu
Steven B. Cohen, Email: Steven.Cohen@rothmanortho.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Gabbe BJ, Finch CF, Bennell KL, Wajswelner H. Risk factors for hamstring injuries in community level Australian football. Br J Sports Med. British Association of Sport and Excercise Medicine. 2005;39:106–10. [DOI] [PMC free article] [PubMed]
- 2.Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A, et al. The Football Association Medical Research Programme: an audit of injuries in professional football–analysis of hamstring injuries. Br J Sports Med. 2004;38:36–41. doi: 10.1136/bjsm.2002.002352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woods C, Hawkins R, Hulse M, Hodson A. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of preseason injuries. Br J Sports Med. British Association of Sport and Excercise Medicine. 2002;36:436–41. [DOI] [PMC free article] [PubMed]
- 4.Dadebo B, White J, George KP. A survey of flexibility training protocols and hamstring strains in professional football clubs in England. Br J Sports Med. 2004;38:388–394. doi: 10.1136/bjsm.2002.000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkins RD, Hulse MA, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. Br J Sports Med. British Association of Sport and Excercise Medicine. 2001;35:43–7. [DOI] [PMC free article] [PubMed]
- 6.Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer) Am J Sports Med. 2011;39:1226–1232. doi: 10.1177/0363546510395879. [DOI] [PubMed] [Google Scholar]
- 7.Elliott MCCW, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39:843–850. doi: 10.1177/0363546510394647. [DOI] [PubMed] [Google Scholar]
- 8.Koulouris G, Connell D. Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582–589. doi: 10.1007/s00256-003-0674-5. [DOI] [PubMed] [Google Scholar]
- 9.• Bertiche P, Mohtadi N, Chan D, Hölmich P. Proximal hamstring tendon avulsion: state of the art. J ISAKOS. 2021;6:237–46. High-quality, comprehensive review. [DOI] [PubMed]
- 10.Bodendorfer BM, Curley AJ, Kotler JA, Ryan JM, Jejurikar NS, Kumar A, et al. Outcomes after operative and nonoperative treatment of proximal hamstring avulsions: a systematic review and meta-analysis. Am J Sports Med. 2018;46:2798–2808. doi: 10.1177/0363546517732526. [DOI] [PubMed] [Google Scholar]
- 11.• Coughlin RP, Kay J, Shanmugaraj A, Memon M, Naji L, Ayeni OR. Return to sport after surgical management of proximal hamstring avulsions: a systematic review and meta-analysis. Clin J Sport Med. 2020;30:598–611. Large, Comprehensive Systematic Review. [DOI] [PubMed]
- 12.Wilson TJ, Spinner RJ, Mohan R, Gibbs CM, Krych AJ. Sciatic nerve injury after proximal hamstring avulsion and repair. Orthop J Sports Med. 2017;5:2325967117713685. doi: 10.1177/2325967117713685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birmingham P, Muller M, Wickiewicz T, Cavanaugh J, Rodeo S, Warren R. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93:1819–1826. doi: 10.2106/JBJS.J.01372. [DOI] [PubMed] [Google Scholar]
- 14.Irger M, Willinger L, Lacheta L, Pogorzelski J, Imhoff AB, Feucht MJ. Proximal hamstring tendon avulsion injuries occur predominately in middle-aged patients with distinct gender differences: epidemiologic analysis of 263 surgically treated cases. Knee Surg Sports Traumatol Arthrosc. 2020;28:1221–1229. doi: 10.1007/s00167-019-05717-7. [DOI] [PubMed] [Google Scholar]
- 15.Buckwalter J, Westermann R, Amendola A. Complete proximal hamstring avulsions: is there a role for conservative management? A systematic review of acute repairs and non-operative management. J ISAKOS. 2017;2:31–35. doi: 10.1136/jisakos-2016-000105. [DOI] [Google Scholar]
- 16.Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures - a systematic review. Int J Sports Med. 2011;32:490–495. doi: 10.1055/s-0031-1273753. [DOI] [PubMed] [Google Scholar]
- 17.Hofmann KJ, Paggi A, Connors D, Miller SL. Complete avulsion of the proximal hamstring insertion: functional outcomes after nonsurgical treatment. J Bone Joint Surg Am. 2014;96:1022–1025. doi: 10.2106/JBJS.M.01074. [DOI] [PubMed] [Google Scholar]
- 18.Degen RM. Proximal hamstring injuries: management of tendinopathy and avulsion injuries. Curr Rev Musculoskelet Med. 2019;12:138–146. doi: 10.1007/s12178-019-09541-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arner JW, McClincy MP, Bradley JP. Hamstring injuries in athletes: evidence-based treatment. J Am Acad Orthop Surg. 2019;27:868–877. doi: 10.5435/JAAOS-D-18-00741. [DOI] [PubMed] [Google Scholar]
- 20.Askling CM, Koulouris G, Saartok T, Werner S, Best TM. Total proximal hamstring ruptures: clinical and MRI aspects including guidelines for postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013;21:515–533. doi: 10.1007/s00167-012-2311-0. [DOI] [PubMed] [Google Scholar]
- 21.Zeren B, Oztekin HH. A new self-diagnostic test for biceps femoris muscle strains. Clin J Sport Med. 2006;16:166–169. doi: 10.1097/00042752-200603000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Fletcher AN, Cheah JW, Nho SJ, Mather RC., 3rd Proximal hamstring injuries. Clin Sports Med. 2021;40:339–361. doi: 10.1016/j.csm.2021.01.003. [DOI] [PubMed] [Google Scholar]
- 23.Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975–984. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- 24.Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A cadaveric study. J Bone Joint Surg Am. 2007;89:44–8. [DOI] [PubMed]
- 25.Sneath RS. The insertion of the biceps femoris. J Anat. 1955;89:550–553. [PMC free article] [PubMed] [Google Scholar]
- 26.Terry GC, LaPrade RF. The biceps femoris muscle complex at the knee. Its anatomy and injury patterns associated with acute anterolateral-anteromedial rotatory instability. Am J Sports Med. 1996;24:2–8. [DOI] [PubMed]
- 27.Tubbs RS, Caycedo FJ, Oakes WJ, Salter EG. Descriptive anatomy of the insertion of the biceps femoris muscle. Clin Anat. 2006;19:517–521. doi: 10.1002/ca.20168. [DOI] [PubMed] [Google Scholar]
- 28.Malalagama GN, Solomon LB, Loftus WK. Complete tibial insertion of the biceps femoris tendon: an MRI-based study to assess the prevalence of this variant. Surg Radiol Anat. 2020;42:661–665. doi: 10.1007/s00276-019-02384-8. [DOI] [PubMed] [Google Scholar]
- 29.Schache AG, Dorn TW, Blanch PD, Brown NAT, Pandy MG. Mechanics of the human hamstring muscles during sprinting. Med Sci Sports Exerc. 2012;44:647–658. doi: 10.1249/MSS.0b013e318236a3d2. [DOI] [PubMed] [Google Scholar]
- 30.Thelen DG, Chumanov ES, Sherry MA, Heiderscheit BC. Neuromusculoskeletal models provide insights into the mechanisms and rehabilitation of hamstring strains. Exerc Sport Sci Rev. 2006;34:135–141. doi: 10.1249/00003677-200607000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Fields KB, Bloom OJ, Priebe D, Foreman B. Basic biomechanics of the lower extremity. Prim Care. 2005;32:245–251. doi: 10.1016/j.pop.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Schache AG, Kim H-J, Morgan DL, Pandy MG. Hamstring muscle forces prior to and immediately following an acute sprinting-related muscle strain injury. Gait Posture. 2010;32:136–140. doi: 10.1016/j.gaitpost.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 33.Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high-speed running. Med Sci Sports Exerc. 2011;43:525–532. doi: 10.1249/MSS.0b013e3181f23fe8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fiorentino NM, Rehorn MR, Chumanov ES, Thelen DG, Blemker SS. Computational models predict larger muscle tissue strains at faster sprinting speeds. Med Sci Sports Exerc. 2014;46:776–786. doi: 10.1249/MSS.0000000000000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ishikawa K, Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity. A report of two cases. Clin Orthop Relat Res. 1988;153–5. [PubMed]
- 36.Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6:237–248. doi: 10.5435/00124635-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Cohen S, Bradley J. Acute proximal hamstring rupture. JAAOS J Am Acad Orthop Surg. 2007;15:350. doi: 10.5435/00124635-200706000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Mann G, Shabat S, Friedman A, Morgenstern D, Constantini N, Lowe J, et al. Hamstring injuries. Orthopedics. search.proquest.com; 2007;30:536–40; quiz 541–2. [DOI] [PubMed]
- 39.Zarins B, Ciullo JV. ACute muscle and tendon injuries in athletes. Clin Sports Med. 1983;2:167–182. doi: 10.1016/S0278-5919(20)31445-9. [DOI] [PubMed] [Google Scholar]
- 40.Sarimo J, Lempainen L, Mattila K, Orava S. Complete proximal hamstring avulsions: a series of 41 patients with operative treatment. Am J Sports Med. 2008;36:1110–1115. doi: 10.1177/0363546508314427. [DOI] [PubMed] [Google Scholar]
- 41.Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996;24:130–6. [DOI] [PubMed]
- 42.Chakravarthy J, Ramisetty N, Pimpalnerkar A, Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. 2005;39:569–572. doi: 10.1136/bjsm.2004.015719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cohen SB, Rangavajjula A, Vyas D, Bradley JP. Functional results and outcomes after repair of proximal hamstring avulsions. Am J Sports Med. 2012;40:2092–2098. doi: 10.1177/0363546512456012. [DOI] [PubMed] [Google Scholar]
- 44.van der Made AD, Peters RW, Verheul C, Maas M, Kerkhoffs GM. Abduction in proximal hamstring tendon avulsion injury mechanism: a report on 3 athletes. Clin J Sport Med. 2019;29:e76–e79. doi: 10.1097/JSM.0000000000000543. [DOI] [PubMed] [Google Scholar]
- 45.Liu H, Garrett WE, Moorman CT, Yu B. Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J Sport Health Sci. 2012;1:92–101. doi: 10.1016/j.jshs.2012.07.003. [DOI] [Google Scholar]
- 46.Ahmad CS, Redler LH, Ciccotti MG, Maffulli N, Longo UG, Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med. 2013;41:2933–2947. doi: 10.1177/0363546513487063. [DOI] [PubMed] [Google Scholar]
- 47.Sheean AJ, Arner JW, Bradley JP. Proximal hamstring tendon injuries: diagnosis and management. Arthroscopy. 2021;37:435–437. doi: 10.1016/j.arthro.2020.12.201. [DOI] [PubMed] [Google Scholar]
- 48.Moatshe G, Chahla J, Vap AR, Ferrari M, Sanchez G, Mitchell JJ, et al. Repair of proximal hamstring tears: a surgical technique. Arthrosc Tech. 2017;6:e311–e317. doi: 10.1016/j.eats.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van der Made Rolf W Peters Claire Verheul Frank F Smithuis Gustaaf Reurink Maarten H Moen Johannes L Tol Gino M M J Kerkhoffs AD. Proximal hamstring tendon avulsions- comparable clinical outcomes of operative and non-operative treatment at 1-year follow-up using a shared decision-making model.pdf. Br J Sports Med [Internet]. 2022; Available from: 10.1136/bjsports-2021-104588. [DOI] [PubMed]
- 50.Piposar JR, Vinod AV, Olsen JR, Lacerte E, Miller SL. High-grade partial and retracted (<2 cm) proximal hamstring ruptures: nonsurgical treatment revisited. Orthop J Sports Med. SAGE Publications Inc; 2017;5:2325967117692507. [DOI] [PMC free article] [PubMed]
- 51.Shambaugh BC, Olsen JR, Lacerte E, Kellum E, Miller SL. A comparison of nonoperative and operative treatment of complete proximal hamstring ruptures. Orthop J Sports Med. 2017;5:2325967117738551. doi: 10.1177/2325967117738551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schuett DJ, Bomar JD, Pennock AT. Pelvic apophyseal avulsion fractures: a retrospective review of 228 cases. J Pediatr Orthop. 2015;35:617–623. doi: 10.1097/BPO.0000000000000328. [DOI] [PubMed] [Google Scholar]
- 53.Nauta HJA, van der Made AD, Tol JL, Reurink G, Kerkhoffs GM. Satisfactory clinical outcome of operative and non-operative treatment of avulsion fracture of the hamstring origin with treatment selection based on extent of displacement: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2021;29:1813–1821. doi: 10.1007/s00167-020-06222-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Léger-St-Jean B, Gorica Z, Magnussen RA, Vasileff WK, Kaeding CC. Accelerated rehabilitation results in good outcomes following acute repair of proximal hamstring ruptures. Knee Surg Sports Traumatol Arthrosc. 2019;27:3121–3124. doi: 10.1007/s00167-018-4964-9. [DOI] [PubMed] [Google Scholar]
- 55.Arner JW, Freiman H, Mauro CS, Bradley JP. Functional results and outcomes after repair of partial proximal hamstring avulsions at midterm follow-up. Am J Sports Med. 2019;47:3436–3443. doi: 10.1177/0363546519879117. [DOI] [PubMed] [Google Scholar]
- 56.Lightsey HM, Kantrowitz DE, Swindell HW, Trofa DP, Ahmad CS, Lynch TS. Variability of United States Online Rehabilitation Protocols for proximal hamstring tendon repair. Orthop J Sports Med. 2018;6:2325967118755116. doi: 10.1177/2325967118755116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shambaugh BC, Wuerz TH, Miller SL. Does time from injury to surgery affect outcomes after surgical repair of partial and complete proximal hamstring ruptures? Orthop J Sports Med. 2020;8:2325967120946317. doi: 10.1177/2325967120946317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Best R, Meister A, Meier M, Huth J, Becker U. Predictive factors influencing functional results after proximal hamstring tendon avulsion surgery: a patient-reported outcome study after 227 operations from a single center. Orthop J Sports Med. 2021;9:23259671211043097. doi: 10.1177/23259671211043097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT. A prospective evaluation of proximal hamstring tendon avulsions: improved functional outcomes following surgical repair. Knee Surg Sports Traumatol Arthrosc. 2017;25:1943–1950. doi: 10.1007/s00167-017-4475-0. [DOI] [PubMed] [Google Scholar]
- 60.van der Made AD, Smithuis FF, Buckens CF, Tol JL, Six WR, Lauf K, et al. Good interrater reliability for standardized MRI assessment of tendon discontinuity and tendon retraction in acute proximal full-thickness hamstring tendon injury. Am J Sports Med. 2021;49:2475–2481. doi: 10.1177/03635465211021612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.•• Pihl E, Kristoffersen MH, Rosenlund A-M, Laszlo S, Berglöf M, Ribom E, et al. The proximal hamstring avulsion clinical trial (PHACT)-a randomised controlled non-inferiority trial of operative versus non-operative treatment of proximal hamstrings avulsions: study protocol. BMJ Open. 2019;9:e031607. Protocol for first RCT comparing operative vs. non-operative treatment of proximal hamstring avulsions. [DOI] [PMC free article] [PubMed]
- 62.Kurowicki J, Novack TA, Mease SJ, Simone ES, Festa A, McInerney VK, et al. Short-term outcomes following endoscopic proximal hamstring repair. Arthroscopy Elsevier. 2021;37:e76–e77. doi: 10.1016/j.arthro.2020.12.158. [DOI] [PubMed] [Google Scholar]
- 63.Fletcher AN, Pereira GF, Lau BC, Mather RC., 3rd Endoscopic proximal hamstring repair is safe and efficacious with high patient satisfaction at a minimum of 2-year follow-up. Arthroscopy. 2021;37:3275–3285. doi: 10.1016/j.arthro.2021.03.067. [DOI] [PubMed] [Google Scholar]
- 64.Maldonado DR, Annin S, Lall AC, Krych AJ, Athey AG, Spinner RJ, et al. Outcomes of open and endoscopic repairs of chronic partial- and full-thickness proximal hamstring tendon tears: a multicenter study with minimum 2-year follow-up. Am J Sports Med. 2021;49:721–728. doi: 10.1177/0363546520981767. [DOI] [PubMed] [Google Scholar]
- 65.Ebert JR, Gormack N, Annear PT. Reconstruction of chronic proximal hamstring avulsion injuries using ipsilateral distal hamstring tendons results in good clinical outcomes and patient satisfaction. Knee Surg Sports Traumatol Arthrosc. 2019;27:2958–2966. doi: 10.1007/s00167-018-5310-y. [DOI] [PubMed] [Google Scholar]