Abstract
Background
The Najuta stent-graft (Kawasumi Laboratories Inc., Tokyo, Japan) is usually easily advanced to the correct deployment position in the ascending aorta thanks to the pre-curved delivery J-sheath with all fenestrations automatically oriented towards the supra-aortic vessels. Aortic arch anatomy and delivery system stiffness could however represent limitations for proper endograft advancement, especially when the aortic arch bends sharply. The aim of this technical note is to report a series of bail-out procedures that could be useful to overcome the difficulties encountered during the Najuta stent-graft advancement up to the ascending aorta.
Main body
The insertion, positioning and deployment of a Najuta stent-graft requires a through-and-through guidewire technique using a .035″ 400 cm hydrophilic nitinol guidewire (Radifocus™ Guidewire M Non-Vascular, Terumo Corporation, Tokyo, Japan) with right brachial and both femoral accesses. When standard maneuver to put the endograft tip into the aortic arch, some bail-out procedures can be applied to obtain proper positioning. Five techniques are described into the text: positioning of a coaxial extra-stiff guidewire; positioning of a long introducer sheath down to the aortic root from the right brachial access; inflation of a balloon inside the ostia of the supra-aortic vessels; inflation of a balloon inside the aortic arch (coaxial to the device); and transapical access technique. This is a troubleshooting guide for allowing physicians to overcome various difficulties with the Najuta endograft as well as for other similar devices.
Short conclusion
Technical issues in advancing the delivery system of Najuta stent-graft could occur. Therefore, the rescue procedures described in this technical note could be useful to guarantee the correct positioning and deployment of the stent-graft.
Supplementary Information
The online version contains supplementary material available at 10.1186/s42155-023-00351-4.
Keywords: Najuta stent-graft, Aortic arch, Thoracic endovascular aortic repair (TEVAR)
Background
Among fenestrated endografts, the semi-custom made Najuta stent-graft (Kawasumi Laboratories Inc., Tokyo, Japan) is a useful tool for endovascular specialists’ armamentarium (Sato et al. 2020; Isernia et al. 2023), even in patients with bovine arch (Toya et al. 2018).
The aim of this technical note is to describe a series of bail-out procedures to overcome potential difficulties encountered during the Najuta stent-graft advancement to the ascending aorta.
Main text
The insertion, positioning and deployment of a Najuta stent-graft requires a through-and-through guidewire technique using a .035″ 400 cm hydrophilic nitinol guidewire (Radifocus™ Guidewire M Non-Vascular, Terumo Corporation, Tokyo, Japan) with right brachial and both femoral accesses. The standard technique consists of advancing the endograft over the through-and-through maintaining tension pulling the wire from cranial and distal accesses, until the endograft tip reaches the arch, then tension is released and a loop is created in the aortic root to facilitate the stent-graft tip advancement up to the desired deployment position into the ascending aorta. If this standard maneuver fails, and the endograft tip cannot be properly advanced into the aortic arch, some bail-out procedures can be applied to obtain proper positioning in the ascending aorta and aortic arch.
Coaxial extra-stiff guidewire
The first bail-out maneuver consists in positioning a super-stiff guidewire (Lunderquist .035″ extra-stiff 260 cm guidewire; Cook Inc. Bloomington, IN, USA is generally preferred) from the contralateral femoral access (through the introducer in place for the pigtail insertion). The extra-stiff guidewire should be advanced close to the aortic root using a pig-tail catheter to protect the valve. Once the extra-stiff guidewire has been positioned, the stent-graft can be pushed at the same time by using the standard loop technique, facilitating the positioning of the stent-graft tip into the ascending aorta (Fig. 1).
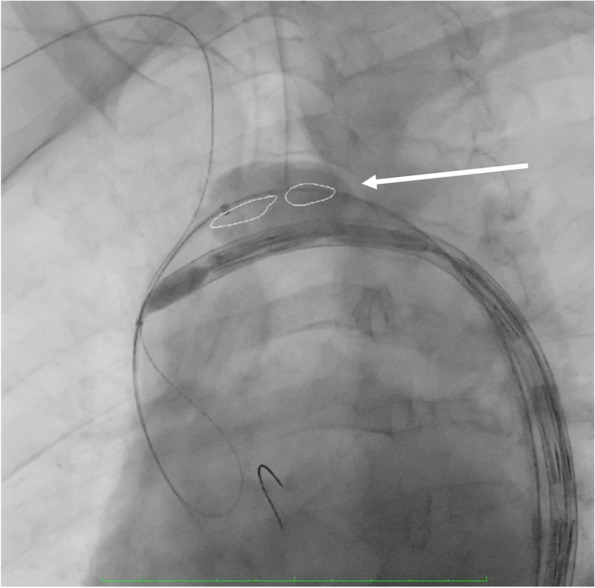
Fig. 1.
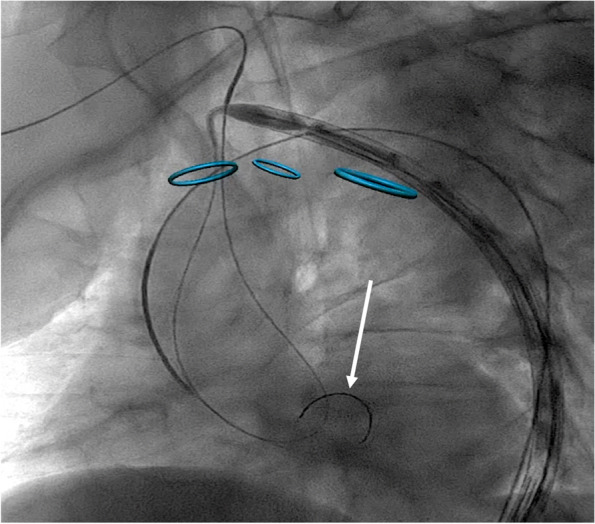
Coaxial extra-stiff guidewire put inside the ascending aorta (arrow)
Long introducer sheath down to the aortic root from the right brachial access
If the coaxial extra-stiff guidewire fails, the second bail-out procedure option is the positioning of a long introducer sheath close to the aortic root from the right brachial access.
This technique consists of exchanging the brachial introducer sheath (usually a 4Fr 11 cm is used to perform the standard through-and-through guidewire technique) with one larger and longer (7-8Fr and at least 70 cm recommended). This maneuver should allow the user to apply a force focused on the aortic root to allow the stent-graft tip advancement into the ascending aorta. Two experienced physicians are needed to perform this procedure: one pushes the introducer sheath onto the aortic root, and the other one pushes the graft forward from the femoral access. Tension on the through-and-through guidewire must be carefully adjusted according to perceived friction and opposition during graft advancement.
A sheath-anchoring rail guidewire can be used to improve the pushability of the long introducer sheath onto the aortic root.
The main disadvantage of this second approach is the need to increase the introducer sheath size of the right brachial access, increasing the risk of periprocedural complications (Fig. 2).
Fig. 2.
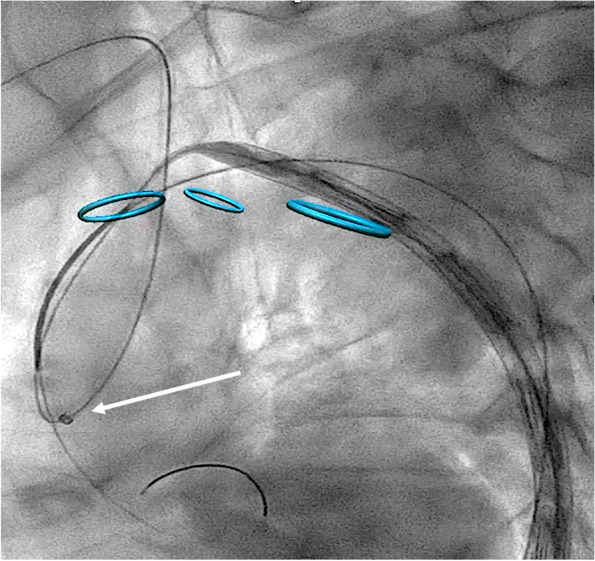
Long introducer sheath from right brachial access down to the aortic root (arrow)
Balloon inflated inside the supra-aortic vessels
If the second bail-out procedure results are also ineffective, the subsequent maneuver consists of inflating a standard angioplasty balloon inside one of the supra-aortic vessels ostia aiming to provide a smooth surface on the outer arch curvature. Thus facilitates the Najuta stent-graft advancement towards the inner curvature of the aortic arch until the ascending aorta. The diameter of the balloon should be evaluated based on a meticulous preoperative assessment.
The first ostium to be used should be the innominate artery since the right brachial access is already available. If the inflation of the ostium of the innominate trunk also fails, it is possible to inflate a balloon on the ostium of the left subclavian artery; to do that it is then necessary to perform a left brachial/axillary access with a percutaneous or surgical approach. The ostium of the left common carotid should be considered as the last option, and it could be reached with a retrograde approach (surgical or percutaneous) (Fig. 3).
Fig. 3.
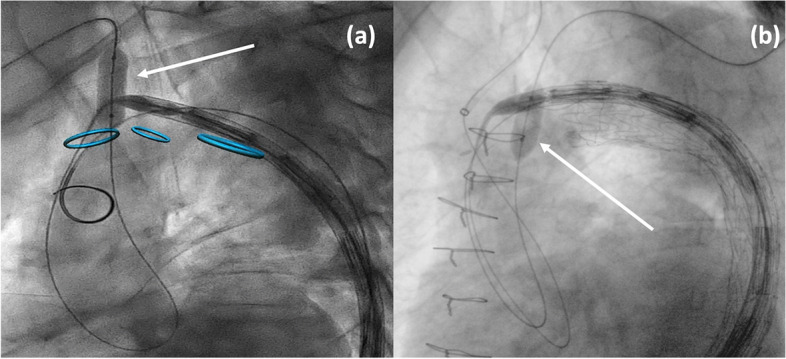
Balloon inflated inside the ostia of the supra-aortic vessels: a innominate trunk (arrow); b left subclavian artery (arrow)
Cerebral monitoring is useful to evaluate the cerebral status during the balloon inflations inside the ostia of the supra-aortic vessels.
Balloon inflated inside the aortic arch
Another technique to be performed is to inflate a large compliant balloon (usually a Coda, Cook Inc. Bloomington, IN, USA) into the aortic arch very close to the Najuta stent-graft tip. The aortic balloon should be inserted from the contralateral femoral access. This bail-out procedure also should be performed by two skilled operators, who simultaneously inflate the aortic balloon turning away the Najuta stent-graft from the aortic arch outer curvature and redirect the tip towards the ascending aorta. However, the proper balloon positioning into the outer curvature is not easy to obtain. This technique is the riskiest since it could lead to cerebral and peripheral embolizations (Fig. 4).
Fig. 4.
Balloon inflated inside the aortic arch (arrow)
Transapical access
The last option is a transapical access. A left mini-thoracotomy in the fifth intercostal space is performed exposing the apex of the heart. After transesophageal echocardiography (TEE) control the correct entry site is defined and double pledgeted U-stitch purse strings with 2/0 monofilament suture are placed in the apical-lateral portion of the ventricle as described elsewhere (Colli et al. 2014) (Additional file 1).
Under fluoroscopy or TEE guidance, the apex is punctured with a standard fluoroscopic needle and a standard 7F introducer sheath is placed and a guidewire is advanced crossing the aortic valve. A goose neck system could be advanced into the ascending aorta and the tip of the guidewire supporting the Najuta stent-graft could be exteriorized from the transapical access. As described in the long introducer sheath technique, a synchronized push and pull from two operators is required to further advance the Najuta stent-graft into the ascending aorta.
Conclusions
A recent systematic review (Blanco Amil et al. 2021) reported similar numbers of patients treated with fenestrated or branched grafts for aortic arch pathologies; no comparative study has been published in Literature.
Najuta stent-graft offers low complication rates (Sato et al. 2020; Isernia et al. 2023).
Delivery system advancement could present some technical issues, especially in sharp aortic arch anatomy. Fernandez-Alonso et al. (Fernández-Alonso et al. 2020) described a bail-out procedure during a Bolton Relay PLUS by placing a 4F pigtail with a stiff guidewire from the right brachial access in order to perform a through-and-through guidewire technique with a femoral access. Mastrorilli et al. (Mastrorilli et al. 2022) described the sheath-anchoring rail guidewire technique to advance a thoracic stent-graft into the aortic arch.
Another technical issue has been reported during the deployment of a Cook Zenith preloaded F-TEVAR: the through-and-through guidewire entanglement around the delivery sheath, resulting in a device malrotation. A total of four bail-out procedures have been already reported in order to face these situations (Prendes et al. 2021).
However, none of the bail out procedures described in literature has the Najuta as stent-graft. Endovascular repair with Najuta stent-graft is useful as a less-invasive option for high-risk patients who are unfit for open surgery of the aortic arch, even if the perioperative outcomes could be affected by the length of the proximal aortic neck into the ascending aorta.
In this paper, we report several bail-out procedures with the aim to provide a troubleshooting guide for allowing physicians to overcome various difficulties with the Najuta endograft as well as for other similar devices. Once all the endovascular bail-out procedures have been attempted, a transapical access with a through-and-through guidewire technique could be considered.
Supplementary Information
Acknowledgements
Not applicable.
Italian Najuta registry collaborators
Nicola Mangialardi, Matteo Orrico (Department of Vascular Surgery, San Camillo Forlanini Hospital, Rome, IT).
Giacomo Isernia, Gioele Simonte, Massimo Lenti, Gianbattista Parlani, Gianluigi Fino (Vascular and Endovascular Surgery Unit, Santa Maria della Misericordia Hospital, Perugia).
Roberto Silingardi, Tea Covic, Stefano Gennai (Department of Vascular Surgery, University of Modena and Reggio Emilia, Modena).
Andrea Gaggiano, Michelangelo Ferri, Emanuele Ferrero, Simone Quaglino (Vascular and Endovascular Surgery Unit, Mauriziano Umberto Hospital, Torino).
Antonio Rizza (Fondazione G. Monasterio, Ospedale del Cuore G. Pasquinucci, Massa).
Gabriele Maritati (Vascular and Endovascular Surgery Unit, Ospedale dei Castelli, Roma).
Michele Portoghese (Division of Cardiac Surgery, Ospedale Civile SS Annunziata, Sassari).
Fabio Verzini, Andrea Discalzi (Department of Surgical Sciences, Città della Salute e della Scienza, Torino).
Raffaele Pulli, Aaron Fargion (Vascular Surgery, Department of Cardiothoracic and Vascular Surgery, Careggi University Teaching Hospital, University of Florence, Firenze).
Stefano Bonvini (Department of Vascular Surgery, Santa Chiara Hospital, Trento).
Francesco Intrieri (Unit of Vascular Surgery, Annunziata Hospital, Cosenza).
Francesco Speziale, Wassim Mansour (Vascular Surgery Unit, Policlinico Umberto I Roma).
Diego Moniaci (Vascular and Endovascular Surgery Unit, San Giovanni Bosco Hospital, Torino).
Raffaella Berchiolli, Nicola Troisi, Giulia Bertagna (Vascular Surgery Unit, Department of Translational Research and New Technologies in Medicine and Surgery, University of Pisa, Pisa).
Andrea Colli, Laura Besola (Division of Cardiac Surgery, Department of Surgical, Medical and Molecular Pathology and Critical Care, University of Pisa, Pisa).
Stefano Camparini, Genadiev Genavi (Vascular Surgery Service, Cardiovascular Department, San Michele Hospital, ARNAS “G. Brotzu, Cagliari).
Giovanni Pratesi (Vascular and Endovascular Surgery Unit, Ospedale Policlinico San Martino, University of Genoa, Genova).
Francesco Massi (Department of Cardiovascular and Thoracic Surgery, Giuseppe Mazzini Hospital, Teramo).
Stefano Michelagnoli, Emiliano Chisci (Unit of Vascular and Endovascular Surgery, San Giovanni di Dio Hospital, Firenze).
Stefano Bonardelli (Unit of Vascular Surgery, Department of Surgical and Clinical Sciences, ASST Spedali Civili di Brescia, University of Brescia School of Medicine, Brescia).
Massimo Maione (Vascular Surgery Unit, Santa Croce e Carle Hospital, Cuneo).
Domenico Angiletta, Sergio Zacà (Vascular and Endovascular Surgery Unit, University of Bari Aldo Moro, Bari).
Gian Franco Veraldi, Luca Mezzetto (Department of Vascular Surgery, University Hospital and Trust of Verona, University of Verona-School of Medicine, Verona).
Abbreviations
- TEE
Transesophageal echocardiography
- F-TEVAR
fenestrated thoracic endovascular aortic repair
Authors’ contributions
RB, writing, data analysis, final revision, final approval. NT, writing, data analysis, final revision, final approval. GB, writing, data analysis, final revision, final approval. AC, writing, data analysis, final revision, final approval. LB, data analysis, final revision, final approval. RS, data analysis, final revision, final approval. GS, data analysis, final revision, final approval. GI, data analysis, final revision, final approval. INRC, data collection. All authors read and approved the final manuscript.
Funding
The present study has not been funded.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval was waived due to the retrospective nature of the study with the aim to analyze techniques adopted during the standard practice.
Consent for publication
All patients gave their consent to publish the pictures of their own procedures.
Competing interests
Giacomo Isernia is consultant for SB-Kawasumi Laboratories Inc., Kanagawa, Japan; Giacomo Isernia, Gioele Simonte, and Roberto Silingardi are consultant for Penumbra Europe GmbH, Berlin, Germany (distributor in Europe for SB-Kavasumi Laboratories Inc.). The other authors have no conflicts of interest related to the article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Raffaella Berchiolli and Nicola Troisi shared first authorship.
Contributor Information
Raffaella Berchiolli, Email: raffaella.berchiolli@unipi.it.
Nicola Troisi, Email: nicola.troisi@unipi.it.
Giulia Bertagna, Email: giuliaberty.it@hotmail.it.
Andrea Colli, Email: andrea.colli@unipi.it.
Laura Besola, Email: laura.besola@hotmail.it.
Roberto Silingardi, Email: roberto.silingardi@unimore.it.
Gioele Simonte, Email: giosimonte@gmail.com.
Giacomo Isernia, Email: iserniagiacomo1@gmail.com.
Italian Najuta registry collaborators:
Matteo Orrico, Massimo Lenti, Gianbattista Parlani, Gianluigi Fino, Tea Covic, Stefano Gennai, Michelangelo Ferri, Emanuele Ferrero, Simone Quaglino, Antonio Rizza, Gabriele Maritati, Michele Portoghese, Fabio Verzini, Andrea Discalzi, Raffaele Pulli, Aaron Fargion, Stefano Bonvini, Francesco Intrieri, Francesco Speziale, Wassim Mansour, Diego Moniaci, Nicola Troisi, Andrea Colli, Stefano Camparini, Genadiev Genavi, Giovanni Pratesi, Francesco Massi, Stefano Michelagnoli, Emiliano Chisci, Stefano Bonardelli, Massimo Maione, Domenico Angiletta, Sergio Zacà, Gian Franco Veraldi, and Luca Mezzetto
References
- Blanco Amil CL, Mestres Alomar G, Guarnaccia G, Luoni G, Yugueros Castellnou X, Vigliotti RC, et al. The initial experience on branched and fenestrated Endografts in the aortic arch. A systematic review. Ann Vasc Surg. 2021;75:29–44. doi: 10.1016/j.avsg.2021.03.024. [DOI] [PubMed] [Google Scholar]
- Colli A, Manzan E, Fabio FZ, Sarais C, Pittarello D, Speziali G, et al. TEE-guided transapical beating-heart neochord implantation in mitral regurgitation. JACC Cardiovasc Imaging. 2014;7:322–323. doi: 10.1016/j.jcmg.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Fernández-Alonso L, Fernández Alonso S, Martínez Aguilar E, Santamarta Fariña E, Alegret Solé J, Atienza Pascual M, et al. Fenestrated and scalloped endovascular grafts in zone 0 and zone 1 for aortic arch disease. Ann Vasc Surg. 2020;69:360–365. doi: 10.1016/j.avsg.2020.06.009. [DOI] [PubMed] [Google Scholar]
- Isernia G, Simonte G, Orrico M, Silingardi R, Gaggiano A, Covic T et al (2023) Preliminary results from an Italian National Registry on the outcomes of the Najuta fenestrated aortic arch endograft. J Vasc Surg 2023. 10.1016/j.jvs.2022.12.059 in press [DOI] [PubMed]
- Mastrorilli D, Mezzetto L, Scorsone L, Leone N, Gennai S, Veraldi E, et al. Sheath-anchoring for rail guidewire technique to advance and deploy thoracic endograft in hostile anatomy. Ann Vasc Surg. 2022;80:393. doi: 10.1016/j.avsg.2021.09.033. [DOI] [PubMed] [Google Scholar]
- Prendes CF, Banafsche R, Stana J, Binskin R, Konstantinou N, Kölbel T, et al. Technical aspects of fenestrated arch TEVAR with preloaded fenestration. J Endovasc Ther. 2021;28:510–518. doi: 10.1177/15266028211007469. [DOI] [PubMed] [Google Scholar]
- Sato H, Fukada J, Tamiya Y, Mikami T, Sibata T, Harada R, et al. Long-term clinical outcomes of thoracic endovascular aortic repair for arch aneurysms with the Najuta thoracic stent-graft system. Ann Vasc Dis. 2020;13:384–389. doi: 10.3400/avd.oa.20-00102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toya N, Ohki T, Fukushima S, Shukuzawa K, Ito E, Murakami Y, et al. Case series of aortic arch aneurysm in patients with bovine arch treated with proximal scalloped and fenestrated stent graft. Cardiovasc Intervent Radiol. 2018;41:1648–1653. doi: 10.1007/s00270-018-2058-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.