Abstract
Background:
The integrity of the acetabular labrum is critical in providing normal function and minimizing hip degeneration and is considered key for success in today’s hip preservation algorithm. Many advances have been made in labral repair and reconstruction to restore the suction seal.
Purpose/Hypothesis:
To compare the biomechanical effects of segmental labral reconstruction between the synthetic polyurethane scaffold (PS) and fascia lata autograft (FLA). Our hypothesis was that reconstruction with a macroporous polyurethane implant and autograft reconstruction of fascia lata would normalize hip joint kinetics and restore the suction seal.
Study Design:
Controlled laboratory study.
Methods:
Ten cadaveric hips from 5 fresh-frozen pelvises underwent biomechanical testing with a dynamic intra-articular pressure measurement system under 3 conditions: (1) intact labrum, (2) reconstruction with PS after a 3-cm segmental labrectomy, then (3) reconstruction with FLA. Contact area, contact pressure, and peak force were evaluated in 4 positions: 90º of flexion in neutral, 90º of flexion plus internal rotation, 90º of flexion plus external rotation, and 20º of extension. A labral seal test was performed for both reconstruction techniques. The relative change from the intact condition (value = 1) was determined for all conditions and positions.
Results:
PS restored contact area to at least 96% of intact (≥0.96; range, 0.96-0.98) in all 4 positions, and FLA restored contact area to at least 97% (≥0.97; range, 0.97-1.19). Contact pressure was restored to ≥1.08 (range, 1.08-1.11) with the PS and ≥1.08 (range, 1.08-1.10) with the FLA technique. Peak force returned to ≥1.02 (range, 1.02-1.05) with PS and ≥1.02 (range, 1.02-1.07) with FLA. No significant differences were found between the reconstruction techniques in contact area in any position (P > .06), with the exception that FLA presented greater contact area in flexion plus internal rotation as compared with PS (P = .003). Suction seal was confirmed in 80% of PSs and 70% of FLAs (P = .62).
Conclusion:
Segmental hip labral reconstruction using PS and FLA reapproximated femoroacetabular contact biomechanics close to the intact state.
Clinical Relevance:
These findings provide preclinical evidence supporting the use of a synthetic scaffold as an alternative to FLA and therefore avoiding donor site morbidity.
Keywords: hip, labrum, reconstruction, polyurethane scaffold, autograft
The acetabular labrum is critical in providing normal function and minimizing hip degeneration and is considered key for success in today’s hip preservation algorithm. Although tears were initially subject to debridement or excision, 21 surgeons have come to understand the important role of the labrum in stabilizing the hip and restoring the suction seal. Losing the seal (ie, vacuum) results in negative sealing pressure that produces an audible sound and dislocation of the hip. If the seal is not maintained, no resistance to the distracting force is perceived, nor is the sound heard. Many advances have been made in labral repair and reconstruction to restore the suction seal.
The current gold standard for a hip labral tear is to repair it when possible. There are cases, however, where the tear is not amendable to repair or a revision is required after a primary repair. In an attempt to preserve the hip joint, the concept of labral reconstruction (or replacement) has become popular 23 in recent years, with the aim of minimizing joint degenerative changes that occur after an irreparable or postlabral debridement injury (labrectomy). Arthroscopy is the preferred technique for labral reconstruction, being 86% of the total techniques used 2 and resulting in superior functional results, lower reintervention rates, 39 and faster recovery as compared with an open surgical dislocation procedure. 6
The indications for labral reconstruction are rupture of the labral seal, tears or labral lesions that are not amendable to repair (eg, insufficient labral size, degenerative labrum, damaged, surgically debrided, calcified, flattened, defibrillated, or nonviable), and failed prior surgical repair in young active patients. 3,5,16 Many autograft and allograft options now exist for labral reconstruction, including iliotibial band (fascia lata), semitendinosus, indirect head of the rectus femoris tendon, and gracilis. The most used autograft for reconstruction is fascia lata (iliotibial band). 3,5
As an alternative to using human tissue, biodegradable synthetic polyurethane scaffolds (PSs) were developed >15 years ago to restore the meniscus, with successful results clinically. 7,11,14,36 In this study, we aimed to compare the effects of labral reconstruction using a macroporous PS vs a fascia lata autograft (FLA) on the contact area, contact pressure, and peak force of the articular cartilage as well as on the hip suction seal. We hypothesized that macroporous PS reconstruction and FLA reconstruction would normalize hip joint kinetics and restore the suction seal.
Methods
Specimens
Ethics approval was obtained for the study protocol. Twenty-two adult human hip specimens (11 complete pelvises including the proximal third of the femur) were obtained from the donation program of the local university in accordance with the legal and ethical procedures of human donation programs. The specimens were admitted consecutively, with anonymity maintained and sex and age registered at the time of death.
The inclusion criteria were hips with intact acetabular labrum, in which fluoroscopy confirmed normal anatomy and no femoroacetabular impingement or impairment of the femoral head (Wiberg angle between 25° and 40° and absence of alterations in femoral head sphericity) and conservation of joint space (Tönnis grade <2). The exclusion criteria were hips with a history of fracture or surgery, osteoarthritis history (Tönnis grade ≥2), 8,10,20 or metastatic bone disease. In addition, we excluded hips where an undetectable severe osteochondral lesion was not indicated on radiology and those where the size of the acetabulum would not allow proper positioning of the sensor.
Two pelvic specimens (4 hips) presented with severe osteochondral damage on direct inspection and were therefore excluded. Another pelvis (2 hips) was too small for adequate insertion of the sensors. We used 3 pelvises (6 hips) in a pilot study to test the calibration and sensor positioning and to refine the reconstruction technique and biomechanical workflow. This left 5 pelvises (10 hips) remaining for study testing.
The pelvic specimens were handled following a previously described protocol 25,38 ; however, they were not divided into separate hips but were kept intact. The specimens were defrosted at room temperature for 12 hours; then, a systematic dissection was performed by eliminating all musculature and soft tissue and keeping the ligament capsule complex untouched. They were refrozen and thawed only on the day of biomechanical testing. At the conclusion of the testing, the specimens were frozen a third time using the same protocol in case a test needed to be repeated. None of the tests required repeating; therefore, the specimens were not thawed a third time.
Testing Procedure
The complete pelvic specimens were fixed in an anatomic position on a biomechanical test bench. This bench allows for angular control in the 3 axes of joint mobility. In the absence of servomotors for movement control, maximum mobility for each specimen can be achieved. The design and methodology have been described. 22,35
This testing protocol has also been described. 12 Testing was carried out in 3 clinical situations for each specimen: (1) with the acetabular labrum intact, (2) after a 3-cm-long labrectomy and labral reconstruction with a polyurethane implant, and (3) after labral reconstruction with a labral FLA. During the preparation of each test and when the specimen was not being tested, the labral surface and cartilage were kept lubricated with a gauze with normal saline solution. At the end of each test, both surfaces were lubricated with cadaveric fat to avoid dehydration.
Intact Condition
A wide 360° capsulotomy was performed on each specimen to 2 mm of the acetabular rim, and the round ligament was sectioned to allow for insertion of the dynamic pressure sensors in a semicircular design (model 4400 N; Tekscan). The sensors, which were designed to cover the entire chondral surface of the hip, 29 were attached to the capsule and labrum with a 3-point capsular suture (silk 2/0) to achieve a static position during testing; after each reconstruction was performed, the sensor was reinserted at the same place marked with the 3 capsular suture points to allow reproducible measurements. A dynamometer was used to ensure that stable pressure was maintained throughout the study for all specimens (Digital Force Gauge SF-500; Besland).
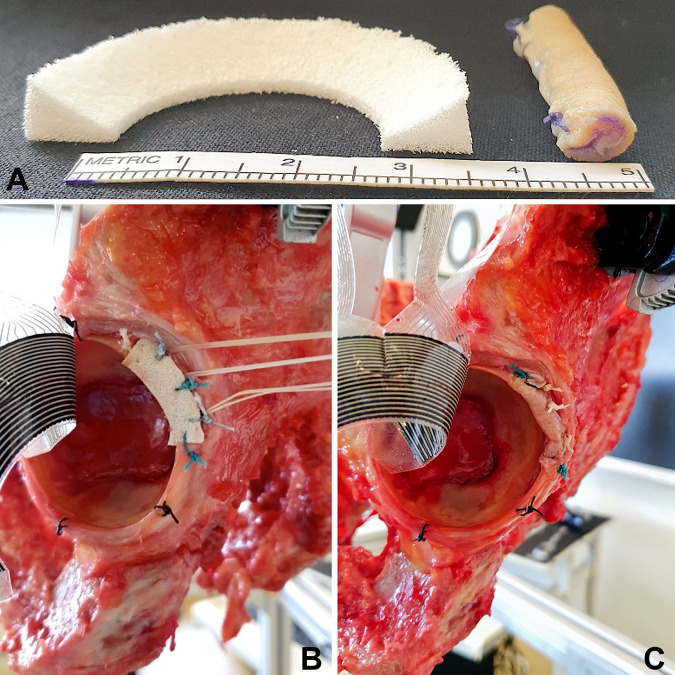
Polyurethane Scaffold
Although normally performed arthroscopically, an open procedure was used for this study. After the testing with intact native labrum was completed, the pressure sensors were detached from the capsule, which was retracted laterally. A longitudinal labral cut 3 cm long in the anterolateral zone was performed with a No. 10 scalpel, leaving a 2-mm lateral margin (labrectomy). Reconstruction was then carried out as previously described 12 with insertion of a biodegradable synthetic PS (Actifit; Orteq) (Figure 1). This implant was modified for the hip, is highly porous, and is composed of aliphatic polyurethane. The scaffold was trimmed to a thickness of 8 mm and a length of 3 cm to fit the defect; three 5-mm anchors (Wedge Anchor II, No. 2 Force Fiber; Stryker) were placed every 7 mm in the middle to secure the implant; and 1 side-to-side suture (high-resistance suture, Force Fiber; Stryker) was used to attach the labral remnant at each end. The sensor was reattached to the capsule in the same place, and the specimen was repositioned on the bench. Because of the quality of the bone for specimen 8, an extra anchor was used in the middle of the scaffold.
Figure 1.
(a) Polyurethane scaffold and fascia lata autograft. Reconstruction with (b) polyurethane scaffold and (c) fascia lata autograft. (b, c) On specimen 4 (left side), there are 3 anchors and 2 side-to-side translabral sutures.
Fascia Lata Autograft
After testing with the PS was complete, the sensors and the implant were removed. Reconstruction with the FLA was performed according to the technique of Lee et al, 22 tubularizing and trimming it to a thickness between 6 and 7 mm and a length of 3 cm (Figure 1) and securing the graft with 1 continuous Vicryl 3.0 suture (Ethicon). The sensors were then reinserted.
Suction Seal Testing
The suction seal was tested according to the methods of Suppauksorn et al, 33 which is performed with the hip in a neutral anatomic position. After the capsulotomy, a section of the round ligament of the femoral head was rearticulated, and an axial distraction force was applied and rated qualitatively if the seal was maintained. The suction seal was tested in the intact labrum on all specimens to confirm that it was present. It was performed again after reconstruction with PS and after reconstruction with FLA. All labral sealing tests were performed by the same investigator (B.C.).
Data Collection
The contact area (cm2), contact pressure (kPa/cm2), and peak force (kPa) of the acetabular cartilage were measured after the introduction of the femoral head into the acetabular cavity. The same sequence of movements was reproduced for each pelvic specimen. The dynamic study began from the anatomic position in extension, rotation, and neutral abduction, and progressive flexion was performed to 90º. The joint was then brought to maximum internal rotation (IR), followed by maximum external rotation (ER) and back to neutral, finishing with an excursion in extension of 20º. The mean of 3 consecutive examinations was used for each measurement. The movement was carried out manually, with each position timed and documented. Throughout the study, a constant force of 50 N was applied with the dynamometer, with a variation of ±5 N. Each cycle lasted 30 seconds (±10%). If greater variations in strength or duration occurred, they were discarded, and the cycle was repeated. Each test for the study was repeated 3 times, and the mean of the results was used.
The contact area, contact pressure, and peak force values were normalized as the relative change from the intact condition (value = 1). This was necessary, as hips were different sizes and adaptation of the sensor may have been influenced by that difference.
To assess the participation of each area of the acetabular surface, an analysis of the data was carried out in the following 4 positions: 90° of flexion in neutral, maximum IR at 90° of flexion, maximum ER at 90° of flexion, and extension at 20° of neutral rotation.
Statistical Analysis
The normalized contact area, contact pressure, and peak force values were compared between conditions (intact vs PS, intact vs FLA, PS vs FLA) at each of the 4 positions. Because multiple measurements were taken per specimen, normalized values were modeled using a repeated measures analysis of variance to account for potential correlation within each specimen. The least squares means and 95% confidence intervals are reported with a P value that reflects the test: H0 (mean = 1) vs H1 (mean ≠ 1). Statistical analyses were performed using SAS Version 9.4 (SAS Institute).
Results
Contact Area
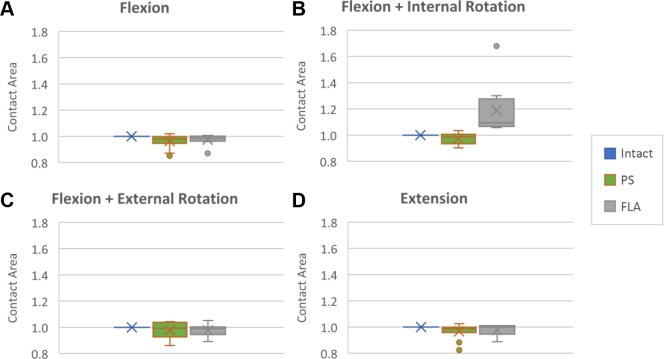
PS reconstruction restored the contact area to normal in all positions, with an overall recovery ≥96% (normalized range, 0.96-0.98) and with no statistically significant differences as compared with the intact labrum. When compared with the intact condition, the contact area was restored to 0.96 (95% CI, 0.93-1.00; P = .061) in flexion, 0.98 (95% CI, 0.94-1.01; P = .187) in flexion + IR, 0.98 (95% CI, 0.94-1.02; P = .243) in flexion + ER, and 0.97 (95% CI, 0.93-1.00; P = .076) in extension (Figure 2).
Figure 2.
Contact areas for the intact, PS, and FLA conditions: (a-d) flexion, flexion + internal rotation (FLA vs intact, P = .006), flexion + external rotation, and extension. X, mean; horizontal line, median; top and bottom of box, first and third quartiles; whiskers, range; dots, outliers. *P < .01 vs intact. FLA, fascia lata autograft; PS, polyurethane scaffold.
FLA reconstruction restored the contact area to at least 97% of intact. When compared with the intact condition, no significant difference was found in flexion (0.97; 95% CI, 0.95-0.995; P = .062), flexion + ER (0.98; 95% CI, 0.934-1.02; P = .148), or extension (0.98; 95% CI, 0.95-1.01; P = .147). The position of flexion + IR, though, was significantly different (1.19; 95% CI, 1.07-1.31; P = .006) (Figure 2).
Comparing the contact area between reconstruction with the macroporous polyurethane implant and FLA revealed no differences in any of the positions of the joint range (P > .6) except in flexion + IR, where FLA presented greater contact area than PS (P = .003).
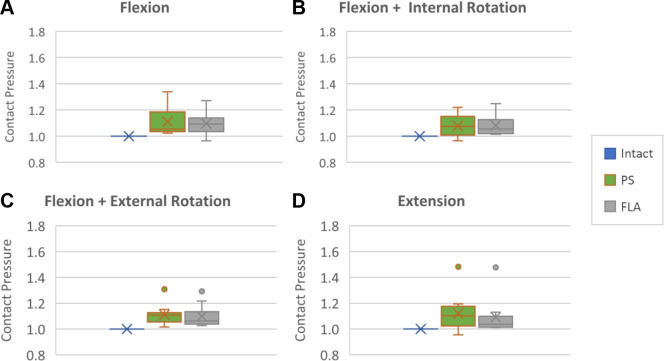
Contact Pressure
When the contact pressure was compared between the intact labrum and both reconstruction techniques (PS and FLA) after labrectomy, it was nearly restored to the intact labrum in all movements of the analyzed joint range, although some positions were significantly different. For the PS reconstruction in flexion, the contact pressure was restored to 1.11 (95% CI, 1.04-1.18; P = .003), flexion + IR to 1.08 (95% CI, 1.00-1.14; P = .008), flexion + ER to 1.11 (95% CI, 1.04-1.18; P = .0004), and extension to 1.12 (95% CI, 1.05-1.19; P = .02) (Figure 3).
Figure 3.
Contact pressure for the intact, PS, and FLA conditions: (a-d) flexion (PS vs intact, P = .003; FLA vs intact, P = .002), flexion + internal rotation (PS vs intact, P = .008; FLA vs intact, P = .005), flexion + external rotation (PS vs intact, P = .0004; FLA vs intact, P = .002), and extension (PS vs intact, P = .005; FLA vs intact, P = .05). X, mean; horizontal line, median; top and bottom of box, first and third quartiles; whiskers, range; dots, outliers. FLA, fascia lata autograft; PS, polyurethane scaffold.
For the FLA reconstruction, contact pressure was restored to 1.1 (95% CI, 1.04-1.16; P = .002) in flexion, 1.08 (95% CI, 1.03-1.13; P = .005) in flexion + IR, 1.11 (95% CI, 1.04-1.16; P = .002) in flexion + IR, and 1.11 (95% CI, 1.00-1.17; P = .05) in extension, with some values significantly different vs intact (Figure 3).
When the contact pressure was compared between PS and FLA, no significant difference was found in any position of the joint range (P > .7).
Peak Force
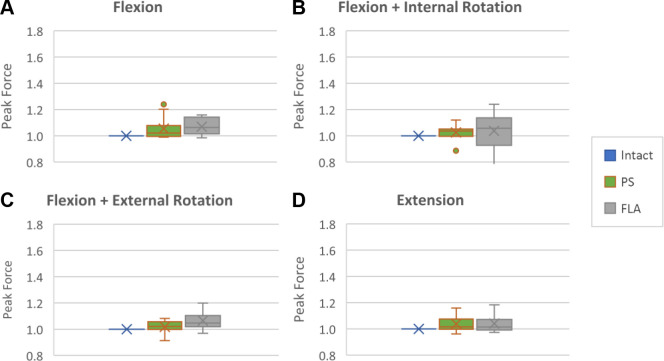
Comparing peak force between intact labrum and PS, we observed a recovery >95% of the peak force after the labrectomy, with no statistically significant differences found. In flexion, it was restored to 1.05 (95% CI, 0.99-1.11; P = .07); in flexion + IR, 1.03 (95% CI, 0.99-1.10; P = .20); in flexion + ER, 1.02 (95% CI, 0.99-1.05; P = .26); and in extension, 1.04 (95% CI, 1.00-1.08; P = .07) (Figure 4).
Figure 4.
Peak force for the intact, PS, and FLA conditions: (a-d) flexion (FLA vs intact, P = .002), flexion + internal rotation, flexion + external rotation (FLA vs intact: P = .008), and extension. X, mean; horizontal line, median; top and bottom of box, first and third quartiles; whiskers, range; dots, outliers. FLA, fascia lata autograft; PS, polyurethane scaffold.
In the comparison of peak force between intact labrum and FLA reconstruction, we observed a recovery >98.5% of peak force. No differences were found in flexion + IR (1.04; 95% CI, 0.96-1.12; P = .391) or extension (1.04; 95% CI, 0.99-1.09; P = .109); however, a significant increase was observed in flexion (1.07; 95% CI, 1.04-1.11; P = .002) and flexion + ER (1.07; 95% CI, 1.03-1.11; P = .008) (Figure 4).
Comparison of peak force between reconstruction with PS and FLA found no differences in any position in the joint range (P > .09).
Suction Seal Testing
Labral sealing was confirmed in 100% of the intact labral specimens. After reconstruction with the macroporous polyurethane implant, 80% of cases recovered labral sealing (P < .01), and after reconstruction with the fascia autograft, 70% (P < .01) were recovered. No statistically significant differences were observed in the labral sealing test between the PS and FLA (P = .06).
Discussion
The most important finding of this study is that reconstruction with the macroporous polyurethane implant and FLA restored the contact area, contact pressures, and peak force stresses to almost normal levels without differences between the types of reconstruction techniques in any joint motion analyzed (P > .05), with the exception of contact area in flexion and IR.
The results show that the PS could be considered equally efficient in terms of its ability to reestablish the joint kinetics of the hip, although FLA is one of the most used and studied in clinical practice with good clinical results. 7,11,14,36 The major advantages of autografts include the maintenance of patient biology, the lack of disease transmission, and the ready availability and lower cost. 23 Although early reconstruction techniques favored the use of autograft, it is not without its complications. Ayeni et al 3 reported that graft harvesting is not a benign procedure but comes with the disadvantages of pain and donor site morbidity. They suggested that when labral reconstruction is being considered, other options should be evaluated as they provide advantages by overcoming the associated harvesting and donor site challenges of autografts. In an early study on anterior cruciate ligament reconstruction using the FLA, Bak et al 4 reported that 8% of patients complained of swelling and pain laterally on the thigh after harvest of an FLA and 20% expressed slight dissatisfaction with the cosmetic appearance of the lateral thigh herniation.
Another limitation to the use of autografts is reduced survival time. Philippon et al 26 observed 70% survival at 5 years and only 61% at 10 years with a mean survival time of 9 years with total hip arthroplasty as the endpoint. Nine percent had a revision while 27% were revised to a total hip arthroplasty. Survival times for the PS scaffold in the knee have been reported as 89% at 5 years 36 and 80% at 10 years. 28
The first published article on labral reconstruction was in 2009 and described a technique using the ligamentum teres capitis. 31 Since then, more graft sources and reconstructive techniques have evolved. 23 Bessa et al 5 published a recent review analyzing the current state of labral reconstruction. This systematic review included 7 studies (evidence levels 3 and 4) and 402 patients. It is the best current evidence available on indications, types of grafts used, and results between 1 and 12 years of follow-up. The authors concluded that when labral insufficiency or other conditions not amenable to repair are encountered, arthroscopic acetabular labral reconstruction with autografts results in significant improvement, based on short- and midterm self-reported outcomes in young patients without moderate or advanced osteoarthritis of the hip.
The polyurethane implant used in this study is an off-the-shelf, readily available scaffold that has several advantages over autografts and allografts. It is easy to maneuver, being of a strong consistency; it also has faster operative times, no donor site morbidity, and reduced infection rates and disease transmission; finally, it retains its sutures until integrated with the surrounding tissue. 34 Because of its triangular shape, it is closer to the shape of the labrum as compared with the tubularized FLA. 34 It has been used with great success in the knee as a meniscal replacement, 29,36,37 and no inflammatory response of the implant in the knee has been reported up to 10 years. 13,28,36,37 The implant was customized to fit the hip for this study and a previously published study by Tey-Pons et al. 12,34
In our study, macroporous polyurethane implant reconstruction and the FLA managed to increase the contact area after labrectomy and normalize that parameter relative to intact labrum, reestablishing the contact area and normalizing intra-articular stress. The exception was in flexion and IR for the FLA where the increase was maintained. Since this is an impingement position, this might suggest some issues in the future.
These findings are consistent with the cadaver study by Philippon et al 27 showing that labral reconstruction produced improvements in hip joint contact area and contact pressure as compared with labral resection.
One of the main functions of the labrum is to distribute pressures in the femoroacetabular joint. 24 Biomechanical studies have shown that an intact labrum allows direct pressure to be evenly distributed within that joint. 15 In this study, intra-articular contact pressure was restored to close to normal with both reconstruction techniques, although the positions were still significant. It is unknown at this time what the effects of this finding would be. Also, when compared with reconstructed joints that show a smooth and homogeneous morphology of cartilage surfaces, postoperative implants have histological, compression, and traction characteristics similar to those of native labrum. When faced with irreparable labral injury, labral reconstruction improves the distribution of intra-articular loads. Shi et al 30 concluded that the development of osteoarthritis can be attenuated after labral reconstruction, contributing to homeostasis of the hip joint.
It is important to consider not only contact pressure but also the peak force applied to the intra-articular surface. There is a relationship between increased stress forces and damage to the chondral surface caused by an increase of these stresses, and it is considered an independent risk factor of osteoarthritis. 17 Areas of cartilage exposed to higher loads may have an increased risk of damage and reduced ability to effectively distribute loads during movement. 18 Intense and acute or chronic impact where surfaces are subjected to a continuous excessive load can lead to degradation of the joint cartilage. We showed that reconstruction with macroporous polyurethane implant and FLA managed to normalize peak force when compared with the intact labrum. This could add to the finding that labral reconstruction might not completely normalize the contact pressure to the intact state; yet, if it manages to restore the peak forces, it could consequently decrease elevated tissue deformation and shear forces that produce fibrillation and chondral delamination, 9 thereby reducing osteoarthritis progression. 30 An exception should be mentioned for peak force in FLA reconstruction in flexion plus ER and flexion where the joint capsule being the main stabilizer is likely to have more impact with the acetabular labrum playing a secondary role. 19 It is unknown at this time what the long-term consequences would be.
In our study, we performed the same labral sealing test as described by Suppauksorn et al. 33 Our results show that labral sealing after a wide capsulotomy was maintained in 100% of the intact labral specimens and was reestablished in 80% of specimens after reconstruction with the PS and 70% reconstructed with the FLA. Suppauksorn et al reported their results after a total labrectomy at 270° and reconstruction using an iliotibial band allograft. In our study, we analyzed the reconstruction of a 3-cm anterosuperior partial labrectomy, which could explain the difference between our 80% recovery of the seal and their 22.5% with reconstruction at 270°. Based on these results, it could be suggested that it is better to perform a partial reconstruction rather than a 270° reconstruction to recover the labral sealing function.
Limitations
There are several limitations to the study. Although the sample size was initially 22 specimens, 4 were used for trial cases and 2 were not large enough to accommodate the sensors. This left 10 specimens for our study. Most biomechanical cadaver studies, however, have used between 5 and 10 specimens. 1,32,33,35 The sensors in this study were designed to be used in the hip but require a wide capsulotomy to be inserted. Although it may affect the distribution of the loads, we did not consider it a major limitation since we compared 3 clinical situations all in the same scenario. Cadaver specimens do not remain in the same condition as hips in the surgical setting. We kept the specimens lubricated with saline and cadaveric fat to preserve them as much as possible, although the measured pressures may differ from those in the surgical situation. All conditions and positions were subject to this limitation. Although the polyurethane implant used in this study was developed for meniscal reconstruction, it is largely unknown how it will act in the hip. Yet, Tey-Pons et al 34 observed good clinical outcomes in their small study with no progression to osteoarthritis using the same implant as used in this study. Its triangular shape does allow for good insertion at the base of the triangle and correct apposition on the femoral head.
Future animal and clinical studies are planned to assess (1) the ability of the scaffold to integrate into the subchondral bone and (2) the degree of revascularization from the synovial membrane, thereby allowing it to generate new tissue similar to the labrum, restore the native biomechanics of the hip joint, and potentially slow the progression to osteoarthritis.
Conclusion
Reconstruction of a partial labrectomy with a synthetic macroporous PS and FLA restores the joint kinetics of the hip to similar values as the intact labrum. Of 12 assessments, 11 showed no difference between the techniques. It appears biomechanically that a synthetic scaffold is a suitable alternative to a FLA for reconstruction the hip.
Acknowledgment
The authors acknowledge the technicians Miriam Hidalgo and Marçal Asso for their invaluable work in the anatomy-biomechanical laboratory and Dr Eduard Tornero for his support in the statistical analysis.
Footnotes
Final revision submitted September 29, 2022; accepted October 21, 2022.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Hospital Universitari de Girona Doctor Josep Trueta (No. 2018/8109/I).
References
- 1. Afoke NY, Byers PD, Hutton WC. Contact pressures in the human hip joint. J Bone Joint Surg Br. 1987;69(4):536–541. [DOI] [PubMed] [Google Scholar]
- 2. Al Mana L, Coughlin RP, Desai V, et al. The hip labrum reconstruction: indications and outcomes—an updated systematic review. Curr Rev Musculoskelet Med. 2019;12(2):156–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ayeni OR, Alradwan H, de Sa D, Philippon MJ. The hip labrum reconstruction: indications and outcomes—a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):737–743. [DOI] [PubMed] [Google Scholar]
- 4. Bak K, Jorgensen U, Ekstrand J, Scavenius M. Results of reconstruction of acute ruptures of the anterior cruciate ligament with an iliotibial band autograft. Knee Surg Sports Traumatol Arthrosc. 1999;7(2):111–117. [DOI] [PubMed] [Google Scholar]
- 5. Bessa FS, Williams BT, Polce EM, et al. Indications and outcomes for arthroscopic hip labral reconstruction with autografts: a systematic review. Front Surg. 2020;7:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Botser IB, Jackson TJ, Smith TW, et al. Open surgical dislocation versus arthroscopic treatment of femoroacetabular impingement. Am J Orthop (Belle Mead NJ). 2014;43(5):209–214. [PubMed] [Google Scholar]
- 7. Bouyarmane H, Beaufils P, Pujol N, et al. Polyurethane scaffold in lateral meniscus segmental defects: clinical outcomes at 24 months follow-up. Orthop Traumatol Surg Res. 2014;100(1):153–157. [DOI] [PubMed] [Google Scholar]
- 8. Bruckl R, Hepp WR, Tonnis D. Differentiation of normal and dysplastic juvenile hip joints by means of the summarized hip factor. Article in German. Arch Orthop Unfallchir. 1972;74(1):13–32. [DOI] [PubMed] [Google Scholar]
- 9. Bsat S, Frei H, Beaule PE. The acetabular labrum: a review of its function. Bone Joint J. 2016;98B(6):730–735. [DOI] [PubMed] [Google Scholar]
- 10. Busse J, Gasteiger W, Tonnis D. A new method for roentgenologic evaluation of the hip joint—the hip factor. Article in German. Arch Orthop Unfallchir. 1972;72(1):1–9. [DOI] [PubMed] [Google Scholar]
- 11. Butt U, Vuletic F, Stenhouse G, Hudetz D, Bradbury N. Meniscal scaffold for the treatment of partial meniscal defect—clinical and radiological outcomes in a two-year follow-up. Int Orthop. 2021;45(4):977–983. [DOI] [PubMed] [Google Scholar]
- 12. Capurro B, Reina F, Carrera A, et al. Hip labral reconstruction with a polyurethane scaffold: restoration of femoro-acetabular contact biomechanics. Orthop J Sports Med. 2022;10(9):23259671221118831. doi:10.1177/23259671221118831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Caro F, Perdisa F, Dhollander A, Verdonk R, Verdonk P. Meniscus scaffolds for partial meniscus defects. Clin Sports Med. 2020;39(1):83–92. [DOI] [PubMed] [Google Scholar]
- 14. Efe T, Getgood A, Schofer MD, et al. The safety and short-term efficacy of a novel polyurethane meniscal scaffold for the treatment of segmental medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc. 2012;20(9):1822–1830. [DOI] [PubMed] [Google Scholar]
- 15. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33(8):953–960. [DOI] [PubMed] [Google Scholar]
- 16. Gursoy S, Vadhera AS, Singh H, et al. Remplissage and labral reconstruction technique correlated with dynamic hip examination using the kite technique for restoration of the suction seal in revision hip arthroscopy. Arthrosc Tech. 2021;10(8):e1995–e2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hadley NA, Brown TD, Weinstein SL. The effects of contact pressure elevations and aseptic necrosis on the long-term outcome of congenital hip dislocation. J Orthop Res. 1990;8(4):504–513. [DOI] [PubMed] [Google Scholar]
- 18. Hunt MA, Charlton JM, Esculier JF. Osteoarthritis year in review 2019: mechanics. Osteoarthritis Cartilage. 2020;28(3):267–274. [DOI] [PubMed] [Google Scholar]
- 19. Johannsen AM, Ejnisman L, Behn AW, et al. Contributions of the capsule and labrum to hip mechanics in the context of hip microinstability. Orthop J Sports Med. 2019;7(12):2325967119890846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kovalenko B, Bremjit P, Fernando N. Classifications in brief: Tonnis classification of hip osteoarthritis. Clin Orthop Relat Res. 2018;476(8):1680–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40(5):1015–1021. [DOI] [PubMed] [Google Scholar]
- 22. Lee S, Wuerz TH, Shewman E, et al. Labral reconstruction with iliotibial band autografts and semitendinosus allografts improves hip joint contact area and contact pressure: an in vitro analysis. Am J Sports Med. 2015;43(1):98–104. [DOI] [PubMed] [Google Scholar]
- 23. Lodhia P, McConkey MO, Leith JM, et al. Graft options in hip labral reconstruction. Curr Rev Musculoskelet Med. 2021;14(1):16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mavcic B, Iglic A, Kralj-Iglic V, Brand RA, Vengust R. Cumulative hip contact stress predicts osteoarthritis in DDH. Clin Orthop Relat Res. 2008;466(4):884–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Moon DK, Woo SL, Takakura Y, Gabriel MT, Abramowitch SD. The effects of refreezing on the viscoelastic and tensile properties of ligaments. J Biomech. 2006;39(6):1153–1157. [DOI] [PubMed] [Google Scholar]
- 26. Philippon MJ, Arner JW, Crawford MD, Bolia IK, Briggs KK. Acetabular labral reconstruction with iliotibial band autograft: outcome and survivorship at a minimum 10-year follow-up. J Bone Joint Surg Am. 2020;102(18):1581–1587. [DOI] [PubMed] [Google Scholar]
- 27. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal—part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722–729. [DOI] [PubMed] [Google Scholar]
- 28. Reale D, Lucidi GA, Grassi A, et al. A comparison between polyurethane and collagen meniscal scaffold for partial meniscal defects: similar positive clinical results at a mean of 10 years of follow-up. Arthroscopy. 2022;38(4):1279–1287. [DOI] [PubMed] [Google Scholar]
- 29. Schuttler KF, Haberhauer F, Gesslein M, et al. Midterm follow-up after implantation of a polyurethane meniscal scaffold for segmental medial meniscus loss: maintenance of good clinical and MRI outcome. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1478–1484. [DOI] [PubMed] [Google Scholar]
- 30. Shi Y, Chen L, Xu Y, et al. Acetabular labral reconstruction using autografts reduces osteoarthritis development compared with labral resection in a porcine model. Am J Transl Res. 2019;11(4):2484–2495. [PMC free article] [PubMed] [Google Scholar]
- 31. Sierra RJ, Trousdale RT. Labral reconstruction using the ligamentum teres capitis: report of a new technique. Clin Orthop Relat Res. 2009;467(3):753–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Smith MV, Panchal HB, Ruberte Thiele RA, Sekiya JK. Effect of acetabular labrum tears on hip stability and labral strain in a joint compression model. Am J Sports Med. 2011;39:103S–110S. [DOI] [PubMed] [Google Scholar]
- 33. Suppauksorn S, Beck EC, Chahla J, et al. Comparison of suction seal and contact pressures between 270 degrees labral reconstruction, labral repair, and the intact labrum. Arthroscopy. 2020;36(9):2433–2442. [DOI] [PubMed] [Google Scholar]
- 34. Tey-Pons M, Capurro B, Torres-Eguia R, et al. Labral reconstruction with polyurethane implant. J Hip Preserv Surg. 2021;8(suppl 1):i34–i40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tey-Pons M. Study of the Function of the Acetabular Labrum in the Biomechanics of the Hip. Doctoral dissertation. Universitat Autonoma de Barcelona; 2015. [Google Scholar]
- 36. Toanen C, Dhollander A, Bulgheroni P, et al. Polyurethane meniscal scaffold for the treatment of partial meniscal deficiency: 5-year follow-up outcomes—a European multicentric study. Am J Sports Med. 2020;48(6):1347–1355. [DOI] [PubMed] [Google Scholar]
- 37. Verdonk P, Beaufils P, Bellemans J, et al. Successful treatment of painful irreparable partial meniscal defects with a polyurethane scaffold: two-year safety and clinical outcomes. Am J Sports Med. 2012;40(4):844–853. [DOI] [PubMed] [Google Scholar]
- 38. Woo SL, Orlando CA, Camp JF, Akeson WH. Effects of postmortem storage by freezing on ligament tensile behavior. J Biomech. 1986;19(5):399–404. [DOI] [PubMed] [Google Scholar]
- 39. Zhang D, Chen L, Wang G. Hip arthroscopy versus open surgical dislocation for femoroacetabular impingement: a systematic review and meta-analysis. Medicine (Baltimore). 2016;95(41):e5122. [DOI] [PMC free article] [PubMed] [Google Scholar]