Abstract
Neuroretinitis is an inflammatory condition with rapid unilateral vision loss, optic disc edema, and macular star formation. While neuroretinitis is commonly due to infectious causes such as Bartonella henselae, neuroretinitis due to toxoplasmosis is uncommon. A 29-year-old male presents to our neuro-ophthalmology clinic on December 7, 2021, at the University of Arkansas for Medical Sciences with symptoms of left eye pain and blurred vision. Subsequent workup led to the diagnosis and treatment of toxoplasma neuroretinitis. The fundus exam eventually demonstrated a notable macular star. Treatment was well tolerated, and the patient regained total visual acuity in the affected eye. Toxoplasma neuroretinitis is known for a characteristic appearance of optic disc edema prior to appearance of stellate maculopathy with vitreous inflammation and peripheral chorioretinal scars. Although loss of vision due to toxoplasmosis is rare, it should be included as part of the differential diagnosis with pertinent history.
Keywords: Toxoplasma neuroretinitis, Toxoplasma gondii, Optic nerve/neurophthalmology, Ocular toxoplasmosis, Neuro-ophthalmology
Introduction
Neuroretinitis is an inflammatory condition that usually affects young adults causing rapid unilateral loss of vision, possible retrobulbar pain, and an afferent pupillary defect [1, 2]. Common fundoscopic findings of neuroretinitis include optic disc edema, vitreous cells in 90% of cases, occasional anterior uveitis, macular edema, and macular star formation [1, 2]. Most cases are self-limited without recurrence, and visual acuity often returns to premorbid conditions [2].
Etiologies of neuroretinitis include infectious, inflammatory, and idiopathic causes. The most common cause of infectious neuroretinitis is cat scratch disease from Bartonella henselae. Other causes include Rocky Mountain spotted fever, tuberculosis, syphilis, lyme disease, leptospirosis, toxocara canis, fungal infection, viral infections, sarcoidosis, and polyarteritis nodosa [3].
While toxoplasmosis from Toxoplasma gondii, an obligate intracellular protozoan, commonly causes chorioretinitis, it rarely presents as neuroretinitis, with or without chorioretinal scars of previous toxoplasmosis infection [2]. We report a case of a patient with unilateral toxoplasma neuroretinitis.
Case Report/Case Presentation
A 29-year-old male presented to our neuro-ophthalmology clinic with symptoms of blurred vision associated with eye pain. The patient had acquired a new kitten 3 months ago. Two months ago, he had gone deer hunting and was bitten by ticks after which he developed a rash which resolved a few days later. He did not have any symptoms of fever, muscle or joint pain, headache, or nausea. At the same time, the patient was also started on an antibiotic to treat chlamydia.
Two weeks prior to presentation, the patient began to develop symptoms of fever, pain with extraocular movement, and visual deficits of seeing a “dark spot” in his left eye which prompted him to go to urgent care. Visual acuity was 20/20 in the right eye and 20/70 in the left eye. Visual field showed a deficit in the superior temporal aspect of the left eye. The external exam was normal for both eyes. Slit-lamp exam was normal in the right eye, while there were significant 2+ vitreous cells in the left eye. The fundus exam was normal in the right eye, and the left eye showed 2+ optic disc edema with telangiectatic dilated vessels and macular edema. The workup included normal labs for Bartonella (IgM and IgG), syphilis T.ab, T-spot, tick-borne disease panel PCR, angiotensin-converting enzyme, and Rocky Mountain spotted fever IgM. Positive lab values included Rocky Mountain spotted fever with an IgG 1:64 (0–1:64), Toxoplasma antibody IgM was higher than 160 IU/mL (≤7.9 AU/mL), and Toxoplasma antibody IgG was 57.9 IU/mL (≤7.1 IU/mL). Optical coherence topography showed a normal right eye, while the left eye showed optic disc and macular edema. The diagnosis of toxoplasma neuroretinitis was made, and the patient was started on double-strength sulfamethoxazole/trimethoprim (SMX-TMP) 800-160 mg 1 tablet twice a day for 1 month.
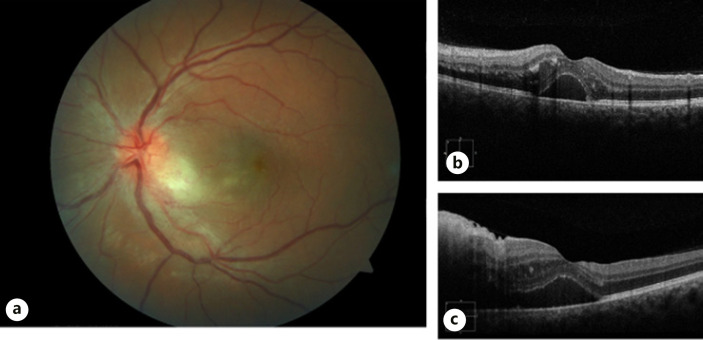
The patient followed up in retina clinic 1 week after initial visit with no changes in his visual acuity. The fundus exam was consistent with 2+ optic disc edema with telangiectatic vessels and macular edema including a small patch of retinitis just inferotemporal to the optic nerve and dilated venules (shown in Fig. 1a). OCT left eye showed subretinal fluid and macular edema (shown in Fig. 1b, c). He was started on PO prednisone 40 mg daily initially for 1 week.
Fig. 1.
a Color fundus photo of the left eye: optic nerve swelling with an adjacent area of chorioretinal whitening. b, c Horizontal and vertical OCT showing subretinal fluid, intraretinal deposits, and localized area of retinitis close to the nerve.
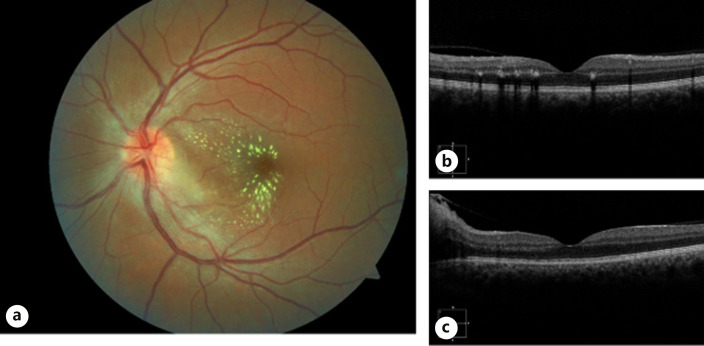
Although the patient was started on prednisone, he denied any visual improvement on follow-up visit 1 week later. While visual acuity improved to 20/30 left eye, the visual field showed a scotoma across the central temporal field. The fundus exam also revealed a new appearance of a macular star (shown in Fig. 2a). Prednisone course was tapered to 20 mg for 1 week while the patient continued current antibiotics. Due to persistent chorioretinitis shown on OCT, the patient was given a 1 mg clindamycin intravitreal injection that day.
Fig. 2.
a Follow-up color fundus photo of the left eye: resolution of the chorioretinal lesion with appearance of a macular star. b, c Horizontal and vertical OCT: resolution of the subretinal fluid with increased deposits in the outer plexiform and Henle's fiber layer.
Over the course of 1 month, patient's visual acuity in the left eye recovered to 20/20, and OCT showed improved retinal anatomy (shown in Fig. 2b, c). All medications were stopped.
Discussion/Conclusion
Toxoplasma neuroretinitis is known for a characteristic appearance of optic disc edema prior to appearance of stellate maculopathy with vitreous inflammation and peripheral chorioretinal scars [2, 4]. The first sign of neuroretinitis was described as idiopathic stellate maculopathy with optic nerve edema with a previous onset of a viral like illness [1, 3, 5]. Although loss of vision due to toxoplasmosis commonly involves chorioretinitis, neuroretinitis is relatively rare, and toxoplasmosis should be included as part of the differential diagnosis with pertinent history and retinal signs of optic disc edema and possible later development of the macular star formation [2, 6].
Our patient showed these risk factors, and therefore, initial investigation included toxoplasmosis, and positive IgM serology was detected resulting in timely treatment. Subsequently, he developed a macular star after 2 weeks from his initial visit. Toxoplasma neuroretinitis should be distinguished from idiopathic neuroretinitis as idiopathic neuroretinitis is self-limited while the former requires timely treatment for resolution [2]. Although there is a lack of randomized control studies for treatment of toxoplasma neuroretinitis, it is suggested that oral antibiotics and corticosteroids may prevent permanent damage to the optic nerve [1, 2, 4, 6–9].
Our patient was initially started on an empiric treatment involving, double-strength SMX-TMP and prednisone. Standard treatments of ocular toxoplasmosis include pyrimethamine and sulfadiazine or SMX-TMP. SMX-TMP has been shown to have less adverse effects and easier compliance with no significant difference in time of recovery when compared to pyrimethamine and sulfadiazine [9]. The patient did not initially show prompt clinical improvement despite being on the empiric regimen and was therefore provided with intravitreal clindamycin. Intravitreal injection of clindamycin is well-tolerated with high bioavailability, avoids systemic side effects, and can be given for persistent cases [8, 9]. This additive treatment resulted in a positive outcome with a complete resolution of ocular pathology and return of vision.
Overall, toxoplasma neuroretinitis has a favorable prognosis with most cases regaining good visual acuity [2, 5]. In our case, enough suspicion from history and fundus exam which included a patch of adjacent chorioretinitis resulted in timely workup and diagnosis. This interesting case demonstrates how Toxoplasma gondii may be a cause of neuroretinitis although rare and should be included in the differential diagnosis of neuroretinitis.
Statement of Ethics
This retrospective review of patient data did not require ethical approval in accordance with national guidelines. Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
Authors have no funding to declare.
Author Contributions
Christine Hsu reviewed medical record, wrote original draft of case report, and revised intellectual content. Dr. Sami Uwaydat and Dr. Joseph Chacko critically revised the manuscript and intellectual content.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and supporting images. Further inquiries can be directed to the corresponding author.
Funding Statement
Authors have no funding to declare.
References
- 1.Moreno RJ, Weisman J, Waller S. Neuroretinitis: an unusual presentation of ocular toxoplasmosis. Ann Ophthalmol. 1992;24((2)):68–70. [PubMed] [Google Scholar]
- 2.Fish RH, Hoskins JC, Kline LB. Toxoplasmosis neuroretinitis. Ophthalmol. 1993 Aug;100((8)):1177–1182. doi: 10.1016/s0161-6420(13)31511-5. [DOI] [PubMed] [Google Scholar]
- 3.Purvin V, Sundaram S, Kawasaki A. Neuroretinitis: review of the literature and new observations. J Neuroophthalmol. 2011 Mar;31((1)):58–68. doi: 10.1097/WNO.0b013e31820cf78a. [DOI] [PubMed] [Google Scholar]
- 4.Ray S, Gragoudas E. Neuroretinitis. Int Ophthalmol Clin. 2001;41((1)):83–102. doi: 10.1097/00004397-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Shoeibi N, Hosseini SM, Bayani R. Toxoplasmosis neuroretinitis: a case report. Iranian Red Crescent Med J. 2016 Apr;18((4)):e33115. doi: 10.5812/ircmj.33115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mac Grory B, Cheng D, Fisayo A. Toxoplasma neuroretinitis. R I Med J. 2019 Mar 1;102((2)):39–40. [PubMed] [Google Scholar]
- 7.Engstrom RE, Jr, Holland GN, Nussenblatt RB, Jabs DA. Current practices in the management of ocular toxoplasmosis. Am J Ophthalmol. 1991 May 15;111((5)):601–610. doi: 10.1016/s0002-9394(14)73706-7. [DOI] [PubMed] [Google Scholar]
- 8.Gerges TK. Infectious eye diseases: recent advances in diagnosis and treatment. London: IntechOpen; 2021. [Google Scholar]
- 9.Soheilian M, Sadoughi MM, Ghajarnia M, Dehghan MH, Yazdani S, Behboudi H, et al. Prospective randomized trial of trimethoprim/sulfamethoxazole versus pyrimethamine and sulfadiazine in the treatment of ocular toxoplasmosis. Ophthalmology. 2005;112((11)):1876–1882. doi: 10.1016/j.ophtha.2005.05.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and supporting images. Further inquiries can be directed to the corresponding author.