Abstract
The governments have been facing the challenges to develop tailored strategies to decrease COVID vaccine hesitancy (CVH) and refusal and increase the acceptability and uptake to ensure the protection of public health. In Pakistan, it has been a great challenge for the government to increase the acceptability of the COVID vaccine. CVH has been a great hurdle to achieving this objective. The authors found it imperative to identify and evaluate the factors of CVH in Pakistan. For this purpose, the authors used an integrated multicriteria decision analysis method (MCDM) by combining Delphi and DEMATEL methods. The factors of CVH have been identified and finalized using the Delphi method. The experts’ opinions were obtained to evaluate the factors. The DEMATEL method was used to find out the most critical factor(s) of CVH. Moreover, the cause/effect relationship was also developed to have a better understating of factors and their relationships. The analysis revealed “ineffective public awareness strategies” as the most critical factor of CVH followed by “misinformation and disinformation, conspiracy theories”, and “acquired knowledge”. The study also examined the cause-and-effect relationship between the prioritized factors. The government in Pakistan introduced successful efforts to deal with the COVID-19 pandemic, yet the government could do more to increase vaccine acceptance. For this purpose to serve effective scientific and evidence-based public awareness strategies are needed to increase the acquired knowledge and deal with misinformation, disinformation, and conspiracy theories to increase vaccine acceptance. The government could sue the media, especially social media to increase vaccination. The findings of the study provide a detailed understanding of the CVH in Pakistan and develop a comprehensive public health strategy to deal with any health-related potential issues in the future.
Keywords: COVID vaccine hesitancy; Socioeconomic factors; Public health; DEMATEL, COVID prevention strategy; Pakistan
Introduction
COVID-19 outbreak, with the dawn of the year 2020, nosed every critical issue on the globe out of the headlines. Socioeconomic experimentation and public health innovations sparked due COVID-19 pandemic. The strategies and frameworks have been developed and implemented to rheostat the pandemic and limit its socioeconomic costs and public health tolls (Ali et al., 2021a, b). The resources were diverted to research and development (R&D) to roll out vaccines to prevent COVID-19 infections. However, the governments and pandemic control agencies have come across a new challenge of COVID vaccine hesitancy (CVH) and uptake refusal despite the steady supplies of COVID vaccine(s) (Adhikari & Cheah, 2021; Razai et al., 2021a, b) along with the new public health challenges posed by COVID-19 and its variants. The wide acceptance and uptake of the vaccines have been challenging objectives to achieve due to multiple socioeconomic factors (Troiano & Nardi, 2021). Vaccine hesitancy is one of the major threats to global health (WHO, 2021). Health experts, health policy strategists, and governments have been endeavoring to understand the sources/causing factors of COVID vaccine hesitancy (CVH).
Bertoncello et al. (2020) explored the socioeconomic determining factor of hesitancy and refusal of vaccines for infectious diseases in Italy, but the study did not focus on the CVH. However, the study provided strong reasons to believe that socioeconomic factors influence vaccine hesitancy. Most of the previous studies concentrated on the analysis of CVH and its factor in developed countries. For instance, Okubo et al. (2021) examined CVH and its factors in Japan. CVH is higher in women compared to men, and it is higher in younger age groups than the old ones. Moreover, CVH is also higher in people with lower education levels compared to degree qualified. While considering the ethnicity in the analysis, CVH was higher in Blacks compared to Pakistani/Bangladeshi ethnic groups (Robertson et al., 2021).
Solís Arce et al. (2021) analyzed the COVID-19 vaccine hesitancy and acceptance in low- and middle-income countries (LMICs). The authors asserted the need for an examination of vaccination attitudes to achieve sufficient immunization to end the pandemic. The findings of the study find out that vaccine acceptance is driven by personal protection motivation against the COVID-19 pandemic. However, concerns about the side effects of the vaccine have been found the source of CVH in LMICs. Sung et al. (2021) focused on attitudes and factors associated with CVH among patients with breast cancer. The study stressed the need to develop a sustainable infrastructure for the effective and efficient dissemination of cancer prevention measures and provision of cancer care in the economies for cancer control. In another study, Moola et al. (2021) examined the determinants and strategies for COVID vaccine acceptance and hesitancy in LMICs. While considering the demographic determinacies, the author found that vaccine acceptance was higher in males who have higher education, higher socio-economic status, and are unmarried and employed as healthcare workers. However, misinformation about COVID-19 vaccines and public concerns over the safety of vaccines were major factors in low vaccine acceptance rates.
Some studies addressed CVH in developing countries. For instance, AL-Mohaithef et al. (2021) explored the socio-demographic correlates of CVH in the 2nd wave of COVID-19 in Saudi Arabia and found that higher risk perception and higher trust in healthcare were the main reasons to determine participants’ intentions to be vaccinated. Chaudhary et al. (2021) compared the factors related to the COVID-19 vaccine in Pakistan with a special focus on perceived beliefs, knowledge, concerns, risks, and safety perception related to COVID vaccine. However, the review of existing studies related to the COVID-19 vaccine and its acceptability reveals that there is no study on the identification, evaluation, and prioritization factors of CVH, especially in Pakistan. Nevertheless, the current study is an effort to fill this gap, and the authors find it imperious to identify, evaluate, prioritize, and trace out a cause/effect relationship among the factors of CVH for better understating and formulation of productive COVID-19 vaccine acceptance strategy.
The objective of this study is to identify, evaluate, and explore the cause-and-effect relationship between the factors of CVH in Pakistan. For this purpose, the study identifies the socioeconomic factors of CVH through a wide-ranging literature review. The most relevant factors were finalized through the DELPHI method. Further, it evaluates these factors using the decision-making trial and evaluation laboratory (DEMATEL). An efficient multicriteria decision analysis method (MCDM) serves two purposes. This study is novel in the sense that it is the first study related to CVH in Pakistan. Moreover, it contributes to the understanding of the factors of CVH using an integrated MCDM method by combining the Delphi and DEMATEL methods. The proposed methodology provides the rankings of the identified and finalized CVH factors. The DEMATEL method is useful in the sense that it not only provides the ranking of the CVH factors but also provides information about the cause-and-effect relationship among these CVH factors. This study would help understand the factors behind CVH in Pakistan. Moreover, it would also provide guidelines to develop a profound policy framework to increase the acceptability of the vaccines not only for COVID-19 but also for other diseases including polio. Furthermore, conclusions drawn from this analysis provide a deeper understanding of the factors of CVH in Pakistan and provide a comprehensive understanding to strategize the COVID-19 vaccination process in the 5th largest populous country.
Methodology
Study Design
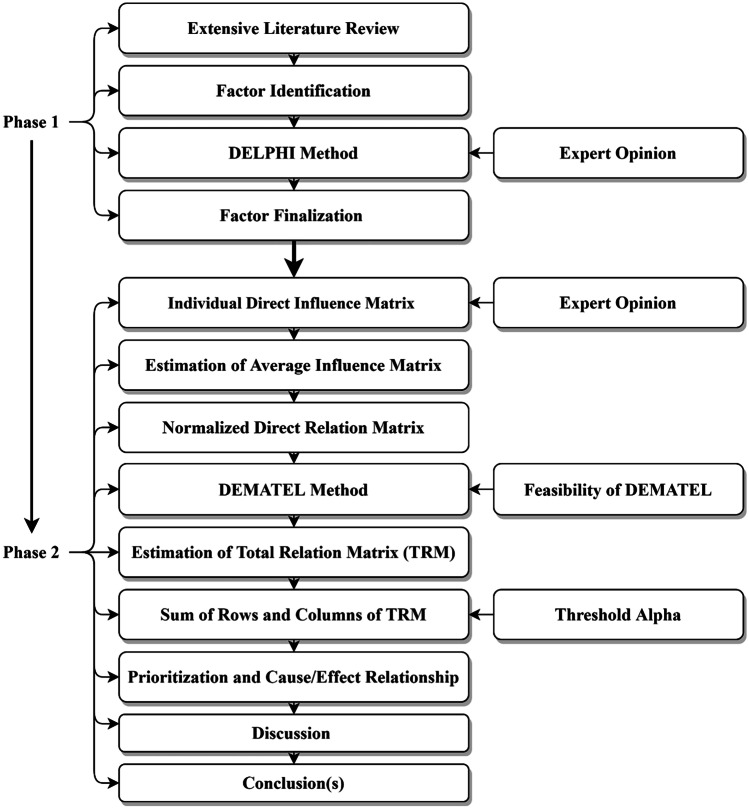
The research design of this current study consists of two parts. The first part consists of the identification and finalization of the factors of CVH (see Fig. 1). The authors used a systematic literature review (Maqbool & Khan, 2020a, b) linked to COVID-19 vaccine hesitancy. The Delphi method was used to finalize the factors based on the weights given by the experts in the perspectives of the prevalence of CVH in Pakistan. The second part contains the prioritization and creation of the cause-and-effect relationship between the factors of CVH using the DEMATEL approach. DEMATEL is a suitable technique to analyze complicated decision problems in practice (Gabus & Fontela, 1972). It helps in prioritizing and finding out the cause-and-effect relationship among the identified factors. Moreover, it also provides a deeper understanding of the distinctive sensible measures for a specific decision problem or entwined problems (Si et al., 2018). It is a widely used approach with its applications in areas related to public healthcare and management. For instance, it has been used in analyzing polio prevention (Kumar et al., 2018), identification and assessment of success factors of hospital service quality (Shieh et al., 2010), in modeling lockdown relaxation protocols in retort to COVID-19 (Ocampo & Yamagishi, 2020), and examining the putting into practice public health and social measures to avoid COVID-19 spread (Maqbool & Khan, 2020b).
Fig. 1.
Framework of the study
Identification of Factors of COVID Vaccine Hesitancy
The objective of the study is to identify and evaluate the socioeconomic factors of CVH using DEMATEL—an impressive MCDA approach. Following Kafadar et al. (2022), a comprehensive literature review serves the purpose to identify the CVH factors. The keywords “vaccine hesitancy”, “COVID vaccine hesitancy”, “factors of vaccine hesitancy”, and “determinants of COVID vaccine hesitancy” were used to search the relevant studies using Google, PubMed, Scopus, and Web of Science. The most relevant studies mentioned in column 3 of Table 1 are selected to trace out the CVH factors. The factors were identified and finalized based on the expert opinions of the experts working in the COVID-19 control and prevention programs in Pakistan. The study identifies 11 socioeconomic factors of COVID vaccine hesitancy through an extensive literature review following Maqbool and Khan (2020a, b). A detailed description of the identified factors is summarized in Table 1. Factor F1 symbolizes the demographic factor(s), F2–F9 designate the social factors, F10–F11 represent economic factors, and F12 shows the political factors in Table 1.
Table 1.
Socioeconomic factors of COVID vaccine hesitancy in Pakistan
| Factors | Symbols | Description |
|---|---|---|
| Demographic factors | F1 | Demographic factors such as gender (Dabla-Norris et al., 2021; Kabamba Nzaji et al., 2020; Kadoya et al., 2021; Troiano & Nardi, 2021; Wake, 2021; Wang et al., 2020), age (Dabla-Norris et al., 2021; Kuter et al., 2021; Malik et al., 2020; Troiano & Nardi, 2021), education levels (Kadoya et al., 2021; Malik et al., 2020; Troiano & Nardi, 2021), and marital status (Kadoya et al., 2021; Wang et al., 2020) influence the vaccine acceptance/hesitancy behavior. Education level is a critical factor and is one of the important correlates of vaccine acceptance (Ehde et al., 2021). |
| Lack of vaccine literacy | F2 | The lack of vaccine literacy (Sung et al., 2021) and poor access to accurate and reliable information (Jarrett et al., 2015; Mills et al., 2020; Razai et al., 2021a, b). |
| Lack of confidence vaccine and healthcare system | F3 | Lack of confidence in COVID vaccine (Chen et al., 2021) and the healthcare system contributes to COVID-19 vaccine hesitancy (Sung et al., 2021). |
| Misinformation, disinformation, and conspiracy theories (MDCTs) | F4 | Misinformation, disinformation, rumors, and conspiracy theories, especially social media (Jarrett et al., 2015; Mills et al., 2020; Mo et al., 2021; Razai et al., 2021a, b). |
| Acquired knowledge | F5 | Knowledge of the public about the epidemic/pandemic and its vaccination for prevention is important, but it is not enough to change behavior (Chaudhary et al., 2021; Goldstein et al., 2015). |
| Perceived severity, risk, and concerns associated with COVID-19 and its variants | F6 | Perceived severity (Mo et al., 2021), concerns and risks (Ehde et al., 2021), source of information perceive side effects (Chaudhary et al., 2021; Troiano & Nardi, 2021), and lack of confidence in vaccine and their effectiveness (Solís Arce et al., 2021), coupled with the deficient healthcare system (Bono et al., 2021). Moreover, the risk perception of the risks due to COVID-19 and the health security after vaccination is important in vaccine acceptance or vaccine hesitancy behavior (Ehde et al., 2021). |
| Poor health quality service (PHQS) and poor communication | F7 | Poor communication unfavorably affects vaccine acceptance and adds to vaccine hesitancy (MacDonald et al., 2015), discusses scarce communiqué resources, hampers the capability to deal with the destructive information about vaccines, and undermines the achievements of community support for vaccine programs. PHQS undermines acceptance in any given conditions. Even with well-resourced vaccination programs in high-income countries, PHQS is more likely to surge vaccine hesitancy and even utter refusal. Poorly communicated. |
| Ineffective public awareness strategies | F8 | Insufficient and ineffective public health messages and targeted campaigns (Jarrett et al., 2015; Mills et al., 2020; Razai et al., 2021a, b). |
| Socio-religious beliefs and biases and subjective norms and attitudes towards vaccine | F9 | The social-religious beliefs (Chaudhary et al., 2021) and biases make the public hesitant to believe in the need and necessity of vaccination. Subjective norms play important role in participants’ attitudes toward vaccines and COVID vaccine acceptance/hesitancy (Winter et al., 2021). |
| Socioeconomic and healthcare inequalities | F10 | Socioeconomic and healthcare inequalities intensify health-related issues (Jarrett et al., 2015; Laurencin, 2021; Mills et al., 2020; Razai et al., 2021a, b). |
| Economic factors | F11 | Economic factors such as household income and assets have an impact on behaviors toward vaccine acceptance/hesitancy (Kadoya et al., 2021; Laurencin, 2021). |
| Political factor(s) | F12 | Political views are one of the critical factors in vaccine hesitancy (Albrecht, 2022). |
Finalization of Factors
DELPHI method was used to identify factors to finalize the most relevant factors. A questionnaire (Kumar et al., 2018; Ali et al., 2021a, b) was used to collect opinion from 7 experts about the relevance of the factors. Snowball sampling with a scale 1–5 (i.e., 5 = extremely important, 1 = extremely unimportant) was used. Eleven out of 12 factors fulfilled the threshold level of 3.5 (Gumus, 2009; Kumar et al., 2018). The F12 was excluded from the finalized factors, as it did not fulfill the threshold. This may be due to the fact that political beliefs or views may be irrelevant to CVH in Pakistan. The results of the DELPHI analysis are summarized in Table 2.
Table 2.
Finalization of factors
| Factors | Importance | Result |
|---|---|---|
| F1 | 3.89 | Accepted |
| F2 | 4.06 | |
| F3 | 4.44 | |
| F4 | 4.17 | |
| F5 | 4.67 | |
| F6 | 3.83 | |
| F7 | 3.72 | |
| F8 | 3.56 | |
| F9 | 4.11 | |
| F10 | 3.83 | |
| F11 | 3.61 | |
| F12 | 2.83 | Rejected |
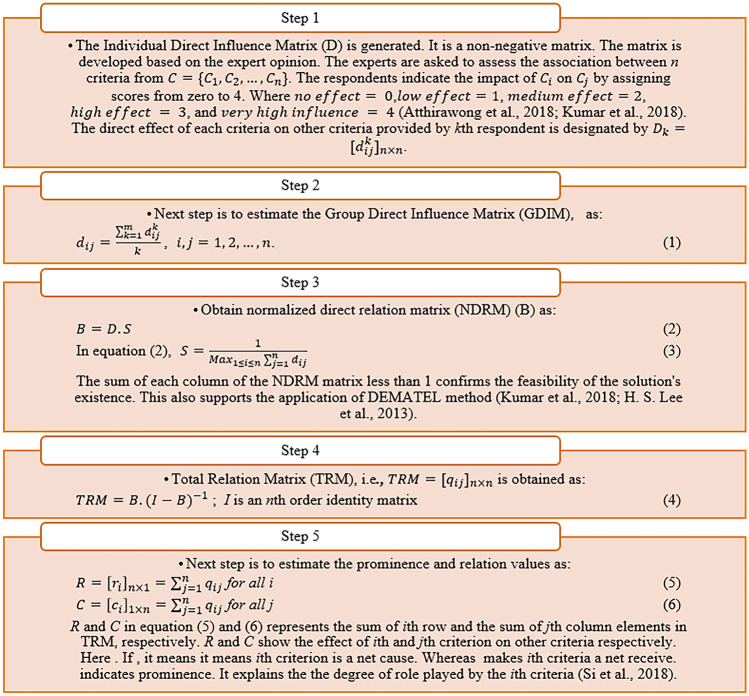
Evaluation of Factors of COVID Vaccine Hesitancy Through the DEMATEL Method
In the next step, the experts were asked to evaluate the relationships among the finalized factors (i,j = 1, …n) (Ali et al., 2021a, b; Kumar et al., 2018; Shieh et al., 2010). The study employs an MCDM method of DEMATEL to study the factors of CVH, summarized in Table 1 except F12. It is a superior method as it explains the connections between the factors and ranks the factors and also highlights the influential strength of factors (Maqbool & Khan, 2020a; Maqbool et al., 2020; Si et al., 2018). Various studies have used the DEMATEL method in examining the decision-making process related to health issues. For instance, Kumar et al. (2018) used DEMATEL to examine the role of social media in polio prevention. Further, Ali et al. (2021a, b) utilized it to analyze the barriers to implementing public health measures to control the COVID-19 pandemic. The steps of the DEMATEL method are summarized in Fig. 2.
Fig. 2.
The steps in DEMATEL method
Results and Discussion
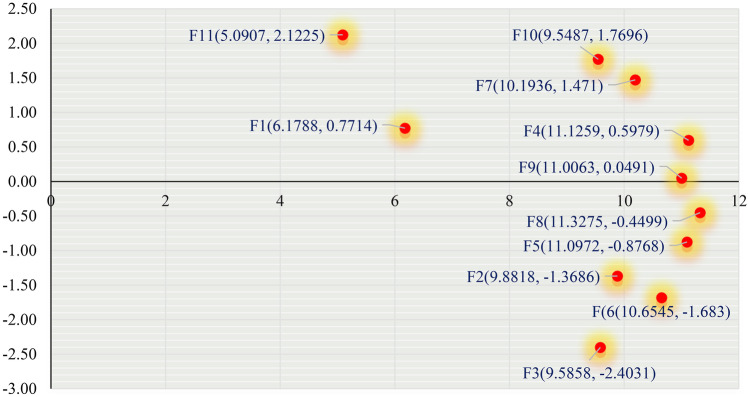
The results of the analysis summarized in Table 2 reveal ineffective public awareness strategies (F8), a pivotal factor with the highest value of 11.3275, whereas the economic factors (F11) are the least important critical factor with R + C value (5.0907). The prioritization of the factors, based on R + C, is F8 > F4 > F5 > F9 > F6 > F7 > F2 > F3 > F10 > F1 > F11. The R – C values divide the factors into two groups, i.e., causes and effects. All factors with positive R – C values are included in the cause group, and the factors with negative R – C values are found to be effects. F1, F4, F7, F9, F10, and F11 are cause factors. It implies that these factors affect the rest of the factors, which include F2, F3, F5, F6, and F8. Lack of confidence vaccine and healthcare system (F3), with the highest R – C value, turns out to be the most affected factor (Table 3).
Table 3.
Ranking of factors
| Factors | Ri | Ci | Ri + Ci | Ri – Ci | Rank | Cause/effect |
|---|---|---|---|---|---|---|
| F1 | 3.4751 | 2.7037 | 6.1788 | 0.7714 | 10 | Cause |
| F2 | 4.2566 | 5.6252 | 9.8818 | − 1.3686 | 7 | Effect |
| F3 | 3.5913 | 5.9944 | 9.5858 | − 2.4031 | 8 | Effect |
| F4 | 5.8619 | 5.2640 | 11.1259 | 0.5979 | 2 | Cause |
| F5 | 5.1102 | 5.9870 | 11.0972 | − 0.8768 | 3 | Effect |
| F6 | 4.4857 | 6.1688 | 10.6545 | − 1.6830 | 5 | Effect |
| F7 | 5.8323 | 4.3613 | 10.1936 | 1.4710 | 6 | Cause |
| F8 | 5.4388 | 5.8887 | 11.3275 | − 0.4499 | 1 | Effect |
| F9 | 5.5277 | 5.4786 | 11.0063 | 0.0491 | 4 | Cause |
| F10 | 5.6591 | 3.8896 | 9.5487 | 1.7696 | 9 | Cause |
| F11 | 3.6066 | 1.4841 | 5.0907 | 2.1225 | 11 | Cause |
Fi(R + C, R – C) are shown in Fig. 3 in which the horizontal vector (R + C) shows the degree of the important role that each factor plays in the entire system. It implies that R + C represents Fi’s impact on the system and other factors in the system. For instance, ineffective public awareness strategies (F8) (with R + C = 11.3275) show the most important factor in the system factors, whereas the vertical vector (R – C) in Fig. 1 shows the degree e of a factor's influence on the system. demonstrates a causal variable and a indicates the effect.
Fig. 3.
Cause/effect diagram
The analysis uncovers that ineffective public awareness strategies are the most critical factor of CVH in Pakistan. Though the Pakistani government put forth comparatively successful strategies and efforts to control COVID-19 transmission despite the 4 waves hit by COVID-19 and its variants, the government has got to do more to increase vaccination acceptance and uptake. It would be possible with the device of a comprehensive COVID vaccine strategy and its strict implementation. However, other factors such as MDCTs and acquired knowledge of the public are also the leading factors. Misinformation, disinformation, and conspiracy theory are great sources of concern and include the causing factors of the CVH in the country in the present analysis. Jarrett et al. (2015) show that social media is a major source of unreliable, invalid information and rumors.
Misinformation, disinformation, rumors, and conspiracy theories, especially social media have been the major factors of vaccine hesitancy (Mills et al., 2020; Mo et al., 2021; Razai et al., 2021a, b). Lack of acquired knowledge and awareness regarding the perceived severity, risk, and concerns associated with COVID-19 and its variants in the Pakistani public may have contributed to CVH in Pakistan. In addition, the lack of acquired knowledge and the inability of the public to realize the severity of situations coupled with anti-vaccines conspiracy beliefs exacerbated the CVH in Pakistan. Our findings are supported by the findings of Jolley and Douglas (2014), who reveal that people exposed to material on anti-vaccine conspiracy theories show less intention to get vaccinated. The study provides strong reasons to believe that anti-vaccine conspiracy theories potentially play role in determining health-related behaviors of the public. The low levels of vaccine acceptance may also be due to poor health quality service and poor communication between health institutions, health ministries from national to provincial levels, and related government agencies. These findings are supported by the findings of Lee and Huang (2022) that regional inequalities in healthcare services are characterized by under-vaccinated.
Conclusion
Since the outbreak of COVID-19, government all over the globe has been facing multiple challenges regarding the control of the spread and transmission of the pandemic. Inventions of multiple COVID vaccines gave hope to the pandemic-stricken world that it would help to control COVID-19 and its covariants and the world would return quicker than it occurred in previous pandemics. The governments have been facing new challenges regarding making the public vaccinated. Like other countries, in Pakistan, CVH has been a challenge as the public has been hesitant to accept the vaccines. An overall CVH has been observed in Pakistan. Owing to such issues related to COVID-19 vaccine acceptability in the masses, there is a dire need to identify, evaluate, and prioritize the factors that drive CVH behavior. For this purpose, the authors proposed an integrated MCDM approach by combining Delphi and DEMATEL methods. The present study focused on the identification, evaluation, prioritization, and cause-effect relationships between the socioeconomic factors driving CVH behavior. The socioeconomic factors were recognized and finalized through comprehensive literature and the DELPHI method, respectively. The DEMATEL method was used to prioritize and establish a cause-effect relationship between the finalized factors. The DELPHI-DEMATEL-based analysis revealed ineffective public awareness strategies as the most pivotal factor of CVH in Pakistan followed by misinformation and disinformation, conspiracy theories, and acquired knowledge. The findings of the study imply that the government in developing countries like Pakistan should formulate and strictly implement comprehensive health policies from national to provincial to local levels. Other socioeconomic policies such as education and public awareness policies should be integrated with the health policies. It is not only the development of a productive healthcare system but also creating public awareness and a sense of social responsibility in the public. The government should allocate more financial resources to education. Extended education and awareness of the public would help to reduce cognitive biases, remove conspiracy theories, and enhance understanding, and belief in evidence-based scientific findings. In addition, the government should use the sources of media to enhance public awareness. The promulgation of rules and regulations especially for social media to control the rumors and promulgation of conspiracies that are mainly sourced from social media platforms.
Data Availability
Data are available on request due to privacy or other restrictions.
Declarations
Ethical Approval
Note applicable.
Consent to Participate
Not applicable.
Consent for Publication
All authors provided consent to submit to the journal.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Waqas Ahmed, Email: wahmed@wiut.uz.
Sharafat Ali, Email: sharafat.ali.rana@gmail.com.
Hamid Waqas, Email: hwaqas@wiut.uz.
Muhammad Asghar, Email: masghar@gudgk.edu.pk.
Naila Erum, Email: nailairam786@gmail.com.
References
- Adhikari B, Cheah PY. Vaccine hesitancy in the COVID-19 era. The Lancet Infectious Diseases. 2021;3099(21):3099. doi: 10.1016/S1473-3099(21)00390-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AL-Mohaithef, M., Padhi, B. K., & Ennaceur, S. Socio-demographics correlate of COVID-19 vaccine hesitancy during the second wave of COVID-19 pandemic: A cross-sectional web-based survey in Saudi Arabia. Frontiers in Public Health. 2021;9(June):1–7. doi: 10.3389/fpubh.2021.698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrecht D. Vaccination, politics and COVID-19 impacts. BMC Public Health. 2022;22(1):1–12. doi: 10.1186/S12889-021-12432-X/FIGURES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali, S., Faizi, B., Waqas, H., Ahmed, W., & Shah, S. A. A. (2021a). Analysis of the socioeconomic barriers in implementing public health measures to contain COVID-19 transmission in Pakistan: A DELPHI–DEMATEL-based approach. Kybernetes, ahead-of-p(ahead-of-print). 10.1108/K-08-2021-0706
- Ali S, Solangi YA, Ahmad N, Gill AS, Faizi B, Waqas H. Overview of disaster preparedness and response strategies regarding COVID-19 crisis control for public safety and health protection. Empirical Economic Review. 2021;4(2):1–30. [Google Scholar]
- Bertoncello C, Ferro A, Fonzo M, Zanovello S, Napoletano G, Russo F, Baldo V, Cocchio S. Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccines. 2020;8(2):1–9. doi: 10.3390/vaccines8020276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bono SA, de Villela EF, M., Siau, C. S., Chen, W. S., Pengpid, S., Hasan, M. T., Sessou, P., Ditekemena, J. D., Amodan, B. O., Hosseinipour, M. C., Dolo, H., Fodjo, J. N. S., Low, W. Y., & Colebunders, R. Factors affecting COVID-19 vaccine acceptance: An international survey among low-and middle-income countries. Vaccines. 2021;9(5):1–19. doi: 10.3390/vaccines9050515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhary FA, Ahmad B, Khalid MD, Fazal A, Javaid MM, Butt DQ. Factors influencing COVID-19 vaccine hesitancy and acceptance among the Pakistani population. Human Vaccines and Immunotherapeutics. 2021 doi: 10.1080/21645515.2021.1944743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M, Li Y, Chen J, Wen Z, Feng F, Zou H, Fu C, Chen L, Shu Y, Sun C. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Human Vaccines and Immunotherapeutics. 2021;17(7):2279–2288. doi: 10.1080/21645515.2020.1853449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabla-Norris, E., Khan, H., Lima, F., & Sollaci, A. (2021). Who doesn’t want to be vaccinated? determinants of vaccine hesitancy during COVID-19, WP/21/130, May 2021 (WP/21/130; IMF Working Paper Series).
- Ehde, D. M., Roberts, M. K., Herring, T. E., & Alschuler, K. N. (2021). Willingness to obtain COVID-19 vaccination in adults with multiple sclerosis in the United States. Multiple Sclerosis and Related Disorders, 49. 10.1016/j.msard.2021.102788 [DOI] [PMC free article] [PubMed]
- Gabus, A., & Fontela, E. (1972). World problems, an invitation to further thought within the framework of DEMATEL. Battelle Geneva Research Center, Geneva, Switzerland, 1–8.
- Goldstein S, MacDonald NE, Guirguis S, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, Larson H, Manzo ML, Reingold A, Tshering K, Zhou Y, Duclos P, Hickler B, Schuster M. Health communication and vaccine hesitancy. Vaccine. 2015;33(34):4212–4214. doi: 10.1016/j.vaccine.2015.04.042. [DOI] [PubMed] [Google Scholar]
- Gumus, A. T. (2009). Evaluation of hazardous waste transportation firms by using a two step fuzzy-AHP and TOPSIS methodology. Expert Systems with Applications, 36(2 PART 2), 4067–4074. 10.1016/j.eswa.2008.03.013
- Jarrett, C., Wilson, R., O’Leary, M., Eckersberger, E., Larson, H. J., Eskola, J., Liang, X., Chaudhuri, M., Dube, E., Gellin, B., Goldstein, S., Larson, H., MacDonald, N., Manzo, M. L., Reingold, A., Tshering, K., Zhou, Y., Duclos, P., Guirguis, S., & Schuster, M. (2015). Strategies for addressing vaccine hesitancy - A systematic review. Vaccine, 33(34), 4180–4190. 10.1016/j.vaccine.2015.04.040 [DOI] [PubMed]
- Jolley, D., & Douglas, K. M. (2014). The effects of anti-vaccine conspiracy theories on vaccination intentions. PloS One, 9(2). 10.1371/JOURNAL.PONE.0089177 [DOI] [PMC free article] [PubMed]
- Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, Lora Mwimba B, Bene CM, A., & Mukamba Musenga, E. <p>Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo</p>. Pragmatic and Observational Research. 2020;11:103–109. doi: 10.2147/por.s271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadoya, Y., Watanapongvanich, S., Yuktadatta, P., Putthinun, P., Lartey, S. T., & Khan, M. S. R. (2021). Willing or hesitant? A socioeconomic study on the potential acceptance of COVID-19 vaccine in Japan. International Journal of Environmental Research and Public Health, 18(9). 10.3390/ijerph18094864 [DOI] [PMC free article] [PubMed]
- Kafadar, A. H., Tekeli, G. G., Jones, K. A., Stephan, B., & Dening, T. (2022). Determinants for COVID-19 vaccine hesitancy in the general population: a systematic review of reviews. Journal of Public Health (Germany), 1. 10.1007/s10389-022-01753-9 [DOI] [PMC free article] [PubMed]
- Kumar A, Kaviani MA, Bottani E, Dash MK, Zavadskas EK. Investigating the role of social media in polio prevention in India: A Delphi-DEMATEL approach. Kybernetes. 2018;47(5):1053–1072. doi: 10.1108/K-06-2017-0210. [DOI] [Google Scholar]
- Kuter BJ, Browne S, Momplaisir FM, Feemster KA, Shen AK, Green-McKenzie J, Faig W, Offit PA. Perspectives on the receipt of a COVID-19 vaccine: A survey of employees in two large hospitals in Philadelphia. Vaccine. 2021;39(12):1693–1700. doi: 10.1016/j.vaccine.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurencin CT. Addressing justified vaccine hesitancy in the Black Community. Journal of Racial and Ethnic Health Disparities. 2021;8(3):543–546. doi: 10.1007/s40615-021-01025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J., & Huang, Y. (2022). COVID-19 vaccine hesitancy: The role of socioeconomic factors and spatial effects. Vaccines, 10(3), 352. 10.3390/VACCINES10030352 [DOI] [PMC free article] [PubMed]
- MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, Goldstein S, Larson H, Manzo ML, Reingold A, Tshering K, Zhou Y, Duclos P, Guirguis S, Hickler B, Schuster M. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Malik, A. A., McFadden, S. A. M., Elharake, J., & Omer, S. B. (2020). Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine, 26. 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed]
- Maqbool A, Khan NZ. Analyzing barriers for implementation of public health and social measures to prevent the transmission of COVID-19 disease using DEMATEL method. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(5):887–892. doi: 10.1016/j.dsx.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maqbool A, Khan NZ. Analyzing barriers for implementation of public health and social measures to prevent the transmission of COVID-19 disease using DEMATEL method. Diabetes and Metabolic Syndrome: Clinical Research and Reviews. 2020;14(5):887–892. doi: 10.1016/j.dsx.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maqbool, A., Khan, S., Haleem, A., & Khan, M. I. (2020). Investigation of Drivers towards adoption of circular economy: A DEMATEL approach. Lecture Notes in Mechanical Engineering, 147–160. 10.1007/978-981-15-1071-7_14
- Mills, M. C., Rahal, C., Brazel, D., Yan, J., & Gieysztor, S. (2020). COVID-19 vaccine deployment: Behaviour, ethics, misinformation and policy strategies. The British Academy, October, 1–35. https://royalsociety.org/-/media/policy/projects/set-c/set-c-vaccine-deployment.pdf
- Mo PKH, Luo S, Wang S, Zhao J, Zhang G, Li L, Li L, Xie L, Lau JTF. Intention to receive the covid-19 vaccination in china: Application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines. 2021;9(2):1–15. doi: 10.3390/vaccines9020129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moola, S., Gudi, N., Nambiar, D., Dumka, N., Ahmed, T., Sonawane, I. R., & Kotwal, A. (2021). A rapid review of evidence on the determinants of and strategies for COVID-19 vaccine acceptance in low- and middle-income countries. Journal of Global Health, 11. 10.7189/JOGH.11.05027 [DOI] [PMC free article] [PubMed]
- Ocampo, L., & Yamagishi, K. (2020). Modeling the lockdown relaxation protocols of the Philippine government in response to the COVID-19 pandemic: An intuitionistic fuzzy DEMATEL analysis. Socio-Economic Planning Sciences, 72. 10.1016/j.seps.2020.100911 [DOI] [PMC free article] [PubMed]
- Okubo R, Yoshioka T, Ohfuji S, Matsuo T, Tabuchi T. COVID-19 vaccine hesitancy and its associated factors in Japan. Vaccines. 2021;9(6):662. doi: 10.3390/vaccines9060662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razai MS, Chaudhry UAR, Doerholt K, Bauld L, Majeed A. Covid-19 vaccination hesitancy. The BMJ. 2021;373:1136–1139. doi: 10.1136/bmj.n1138. [DOI] [PubMed] [Google Scholar]
- Razai MS, Oakeshott P, Esmail A, Wiysonge CS, Viswanath K, Mills MC. COVID-19 vaccine hesitancy: The five Cs to tackle behavioural and sociodemographic factors. Journal of the Royal Society of Medicine. 2021;114(6):295–298. doi: 10.1177/01410768211018951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, Katikireddi SV, Benzeval MJ. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain, Behavior, and Immunity. 2021;94(March):41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shieh JI, Wu HH, Huang KK. A DEMATEL method in identifying key success factors of hospital service quality. Knowledge-Based Systems. 2010;23(3):277–282. doi: 10.1016/j.knosys.2010.01.013. [DOI] [Google Scholar]
- Si, S. L., You, X. Y., Liu, H. C., & Zhang, P. (2018). DEMATEL technique: A systematic review of the state-of-the-art literature on methodologies and applications. In Mathematical Problems in Engineering (Vol. 2018). Hindawi Limited. 10.1155/2018/3696457
- Solís Arce, J. S., Warren, S. S., Meriggi, N. F., Scacco, A., McMurry, N., Voors, M., Syunyaev, G., Malik, A. A., Aboutajdine, S., Adeojo, O., Anigo, D., Armand, A., Asad, S., Atyera, M., Augsburg, B., Awasthi, M., Ayesiga, G. E., Bancalari, A., Björkman Nyqvist, M., & Omer, S. B. (2021). COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nature Medicine, 27(August). 10.1038/s41591-021-01454-y [DOI] [PMC free article] [PubMed]
- Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. 10.3322/caac.21660 [DOI] [PubMed]
- Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wake AD. The willingness to receive covid-19 vaccine and its associated factors: “Vaccination refusal could prolong the war of this pandemic” –A systematic review. Risk Management and Healthcare Policy. 2021;14(June):2609–2623. doi: 10.2147/RMHP.S311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of covid-19 vaccination during the covid-19 pandemic in china. Vaccines. 2020;8(3):1–14. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2021). Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- Winter, K., Pummerer, L., Hornsey, M. J., & Sassenberg, K. (2021). Pro-vaccination subjective norms moderate the relationship between conspiracy mentality and vaccination intentions. British Journal of Health Psychology, 1–16. 10.1111/bjhp.12550 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on request due to privacy or other restrictions.