Abstract
Background
Coronary artery disease affects a significantly larger proportion of Canadians of South Asian origin than Canadians of other ethnic origins. We compared differences in presentation, risk factors and management of myocardial infarction (MI) between South Asian Canadians and matched control subjects.
Methods
We reviewed the charts of 553 South Asian patients and 553 non-South Asian matched control subjects presenting with acute MI (International Classification of Diseases code 410) to 2 hospitals in Canada from January 1994 to April 1999. We identified South Asian subjects by their surnames and first names, and by using self-reported ethnicity and country of birth when available. Patients of Southeast Asian and Middle Eastern origin were excluded. The remaining patients were classified as non-South Asian. Subjects were matched by age within 5 years, sex, discharge date within 6 months and hospital of admission. Presentation characteristics, risk factors and major complications were compared between the 2 groups.
Results
The median time from symptom onset to presentation with acute MI was significantly longer among the South Asian subjects than among the control subjects (3.92 v. 3.08 hours) (p = 0.04). The South Asians were more likely than the control subjects to have diabetes mellitus (43.4% v. 28.2%) (p < 0.001) despite having a significantly lower mean body mass index (25.7 v. 28.0) (p = 0.05) but were less likely to have hyperlipidemia (36.2% v. 42.7%, p = 0.05), to smoke (29.3% v. 67.8%) (p < 0.001) or to have pre-existing vascular disease (49.4% v. 55.0%, p = 0.04). Treatment of acute MI was similar between the South Asian and matched control groups. Also similar were the in-hospital outcomes, including mortality (9.6% and 7.8%, p = 0.27).
Interpretation
There are clear differences in the risk factor profile between Canadians of South Asian origin and those of non-South Asian origin who have acute MI. Despite the higher incidence of cardiovascular disease in the South Asian population, our results indicate that the in-hospital case-fatality rate for MI is the same for South Asian and non-South Asian Canadians.
Cardiovascular disease accounts for the largest proportion of deaths in most industrialized countries, including Canada, despite significant declines in cardiovascular disease rates in recent decades.1 In Canada, people born outside the country make up about 17% of the population.2 The 2 largest non-white ethnic groups include people of Chinese origin and those of South Asian origin (people who originated from India, Pakistan, Sri Lanka or Bangladesh).2 Substantial variations in rates of death from cardiovascular disease among different ethnic groups in Canada have been observed.3 South Asian people experience among the highest rates of coronary artery disease in Canada and the world. An analysis of Canadian data showed that the age-standardized proportional rates of death from coronary artery disease are much higher among Canadians of South Asian origin (men 42% and women 29%) than among Canadians of European origin (men 29% and women 19%).3 The reasons for the higher rates among South Asians are unclear, and the higher rates cannot be explained by an excess of conventional cardiovascular risk factors.4
Although the higher prevalence of death from coronary artery disease among South Asian Canadians is well established, the clinical course of acute myocardial infarction (MI) among patients of South Asian origin is not well characterized. Previous studies from the United Kingdom provide conflicting information on this subject,4,5,6 and given the differences between the health care systems in the United Kingdom and Canada, a country-specific analysis is necessary. In 1996, there were about 600 000 people of South Asian origin in Canada.2 Given that South Asians represent an increasing proportion of the Canadian population, we felt that a detailed study of risk factors, hospital management and outcomes of South Asian Canadians who have had an acute MI is timely.
Methods
We performed a matched comparison of Canadians of South Asian origin and those of non-South Asian origin who had had an acute MI at 1 of 2 Toronto-area hospitals: the Brampton Campus of the William Osler Health Centre or the Centenary Site of the Rouge Valley Health System. The study was approved by the Ethics Review Committee of the William Osler Health Centre and the Institutional Review Board of the Rouge Valley Health System.
We obtained a list of all patients with a discharge diagnosis of acute MI (International Classification of Diseases, ninth revision,7 code 410) between January 1994 and April 1999 from the 2 hospitals (n = 4180). We identified South Asian patients by their surnames and first names, and by using self-reported ethnicity and country of birth when available.8 Both foreign and Canadian-born South Asian patients were included. Patients of Southeast Asian and Middle Eastern origin were excluded from the analysis. The remaining patients were classified as non-South Asian. Of the 734 patients (17.6%) identified as probable South Asians, 553 were matched to non-South Asian patients by age within 5 years, sex, hospital and discharge date within 6 months. Most of the remaining 181 South Asian patients were excluded because of inability to find a matched control subject or missing charts. We used a standardized form to collect chart information, which we entered into a computerized database. Chart abstraction and data collection were performed by 4 trained students (F.R., F.M., J.K. and A.K.).
We reviewed the patients' records for presentation characteristics; conventional coronary artery disease risk factors; type, size and location of MI; medications and procedures; and in-hospital outcomes. The anatomic location of the MI was determined by the presence of ST-segment elevation or development of pathological Q waves in at least 2 contiguous leads on 12-lead electrocardiography (anterior: V1 to V4; lateral: I, aVL, V5, V6; inferior: II, III, aVF). All infarctions were confirmed by at least a 2-fold elevation of the creatine kinase (CK) level or any elevation of its MB isoenzyme (CK MB) level, or both. All electrocardiograms were read by 2 experienced clinical cardiologists (M.G. and N.S.). We measured infarct size indirectly using peak CK levels. Regional wall motion scores and ejection fraction were not measured routinely at the hospitals during the study period and therefore were not used to determine infarct location or size. Peripheral arterial disease was determined to be present if the patient had a history of intermittent claudication or prior peripheral arterial angioplasty or surgery, or prior amputation. Diabetes mellitus, hypertension and hyperlipidemia were recorded as pre-existing risk factors if they were self-reported at admission or if the patient was receiving treatment for any of these conditions at admission. We measured intra- and interobserver variation by a review of 10% of the charts on 2 occasions by 2 independent reviewers (A.K. and A.V.D.). The intraobserver kappa score (mean 0.96, range 0.83–1.00) and interobserver kappa score (mean 0.89, range 0.61–1.00) for agreement were high.
We reviewed 5 years of patient data in order to have adequate statistical power to characterize the presentation features, in-hospital management and outcomes reliably. Descriptive data are presented as means or as medians where appropriate. We used χ2 tests for comparisons of categorical variables and independent sample t-tests for comparisons of continuous variables. For comparisons of nonnormal continuous variables, we used nonparametric statistics for significance testing of medians.
Results
Patient profiles and risk factors
The mean age of the South Asian patients was similar to that of the control patients (62.6 and 63.0 years respectively), and in both groups 31% of the subjects were women. In both groups 51% of the subjects were admitted to the Centenary Site of the Rouge Valley Health System and 49% to the Brampton Campus of the William Osler Health Centre.
Pre-existing diabetes was much more common in the South Asian group than in the control group (43.4% v. 28.2%) (p < 0.001) (Table 1). The South Asians were less likely than the control subjects to be current or former smokers (29.3% v. 67.8%) (p < 0.001) and to have hyperlipidemia (36.2% v. 42.7%) (p = 0.05). They also had a significantly lower mean body mass index than the control subjects (25.7 v. 28.0, equivalent to a 5.5-kg weight difference) (p = 0.05). The rates of hypertension in the 2 groups were similar. Lipid profiles were rarely recorded during the hospital stay and thus were unavailable for comparison.
Table 1
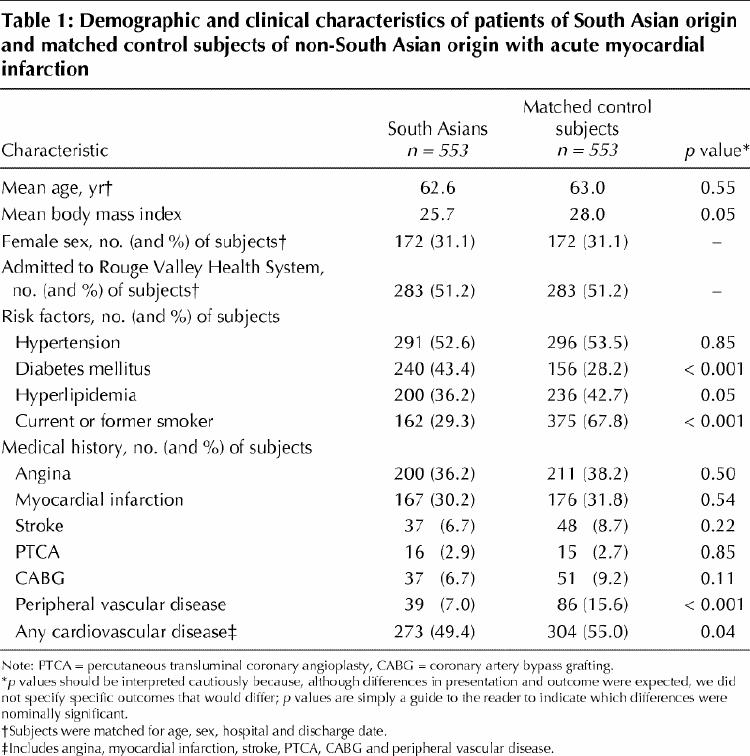
There were no significant differences between the 2 groups in rates of prior angina, MI, stroke, percutaneous transluminal coronary angioplasty or coronary artery bypass surgery (Table 1). However, fewer South Asians than control subjects had peripheral vascular disease (7.0% v. 15.6%) (p < 0.001). The South Asians were less likely than the control subjects to have a history of vascular disease when all cardiovascular conditions were combined (49.4% v. 55.0%) (p = 0.04).
Presentation characteristics and in-hospital treatment
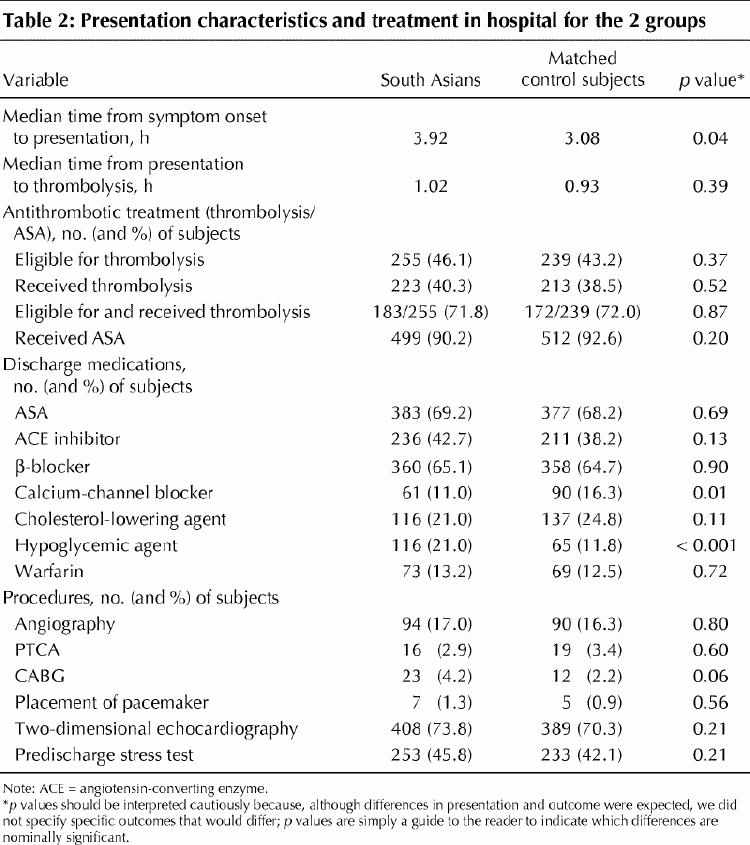
The median time from symptom onset to presentation with acute MI was significantly longer in the South Asian group than in the control group (3.92 v. 3.08 hours) (p = 0.04) (Table 2). Despite the difference, the proportions of South Asians and control subjects who received thrombolytic treatment in hospital were similar (40.3% and 38.5% respectively). According to the criteria suggested by the Canadian Consensus Conference on Coronary Thrombolysis,9 255 (46.1%) of the South Asians and 239 (43.2%) of the control subjects were eligible for thrombolysis (p = 0.37). Of these, 183 (71.8%) and 172 (72.0%), respectively, received thrombolysis; the difference was not significant. The time from hospital presentation to thrombolysis did not differ between the South Asian group and the control group (1.02 and 0.93 hours respectively). Almost all of the subjects were treated with ASA in hospital (90.2% and 92.6% respectively).
Table 2
Anterior infarctions occurred more frequently among the South Asians than among the control subjects (28.2% v. 21.3%) (p = 0.007). Infarct size did not differ significantly between the 2 groups (peak CK level 1401 IU/L v. 1272 IU/L respectively).
Discharge medications
No differences were noted between the 2 groups in the use of discharge medications, with 2 exceptions: the South Asians were more likely than the control subjects to be discharged receiving orally administered hypoglycemics or insulin (21.0% v. 11.8%) (p < 0.001), and the control subjects were more likely to be discharged receiving calcium-channel blockers (16.3% v. 11.0%) (p = 0.01) (Table 2).
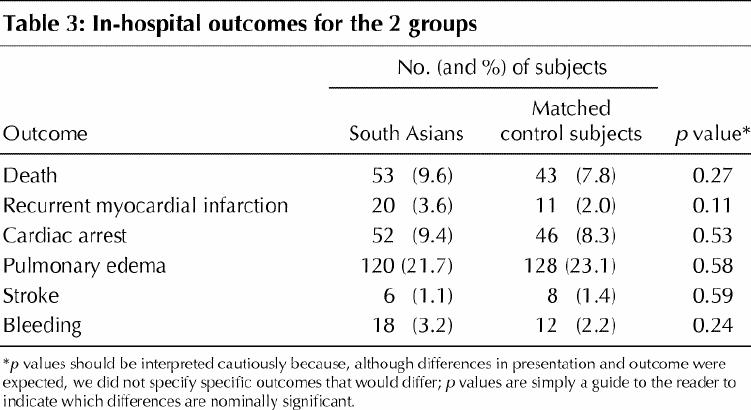
In-hospital outcomes
The median length of hospital stay was 6 days for both groups. The distribution in length of stay did not differ significantly between the groups (p = 0.18, Mann–Whitney U test). Major complications occurred with similar frequency in the 2 groups (Table 3). In general, procedures in hospital were also performed with similar frequency in the 2 groups (Table 2), although the frequency of coronary artery bypass grafting was higher in the South Asian group than in the control group (4.2% v. 2.2%), but not significantly so (p = 0.06). The death rate was 9.6% among the South Asians and 7.8% among the control subjects. We developed a logistic regression model using age, smoking status and diabetes; in this model, the risk-adjusted death rate remained similar for the 2 groups (9.1% and 7.7% respectively) (p = 0.20).
Table 3
Interpretation
Current knowledge regarding the increased risk of cardiovascular disease in South Asians stems largely from studies performed in the United Kingdom and Indian subcontinent. Limited data are available for the South Asian population in Canada, although it is encouraging to note the recent emergence of ethnicity-based research in this country.3,8,10,11
The South Asians in our study had a different cardiovascular disease risk factor profile than did the non-South Asians. Almost half of the South Asians (43%) had diabetes, despite having a significantly lower mean body mass index. Numerous studies have confirmed that insulin resistance and the metabolic syndrome are common among South Asians compared with other populations.12,13,14,15,16,17,18 The non-South Asians in our study were more likely than the South Asians to be smokers and to have hyperlipidemia, findings consistent with those in other studies.16,19,20 Although conventional risk factors remain strongly associated with the development of cardiovascular disease in South Asians, they may not completely explain the relative excess risk in this population.3,4,18
Time from symptom onset to hospital arrival was significantly longer for the South Asians than for the control subjects. This difference merits further investigation, since early presentation and treatment of acute MI may reduce death rates. Reasons for the delay in presentation among South Asians cannot be ascertained from our study but may include language barriers and decreased awareness of the significance of symptoms. If these are found to be factors causing delay, public education of this group at high risk may be necessary. On hospital arrival, however, time to treatment and type of treatment did not differ between the 2 groups.
A greater proportion of South Asians than of control subjects experienced anterior infarctions, with a trend toward higher peak CK levels. This finding suggests that South Asians may experience larger infarctions than non-South Asians. Calcium antagonists were used less often in South Asians, although one may have expected preferential use of calcium antagonists versus β-blockers in a population prone to diabetes. It is possible that calcium antagonists were used less frequently in the South Asian group to reduce the risk of precipitating congestive heart failure in patients deemed to have larger, anterior infarctions.
In-hospital coronary angiography was performed infrequently in both groups. This low rate of angiography is consistent with clinical practice in Canada during the study period. At the 2 participating hospitals, in-hospital angiography was performed largely for postinfarction ischemia or clinical instability. Patients whose condition was stable may have undergone angiography following discharge at the discretion of their cardiologist, but these data were unavailable to us. No statistically significant differences were noted between the groups in the use of percutaneous transluminal coronary angioplasty or other procedures.
Urgent coronary artery bypass grafting was performed almost twice as often in the South Asian group as in the control group. The difference approached statistical significance. Our results are consistent with those of other studies showing that South Asians have more diffuse coronary artery disease19 and are more likely to have triple-vessel disease20 than white people in Britain. As well, we recently showed that South Asian Canadians have more severe and diffuse coronary artery disease at the time of angiography than do Canadians of European origin.11 However, the results of our current study are limited since many patients may have undergone angiography and revascularization following discharge.
Studies from the United Kingdom comparing death rates after MI between South Asians and other subjects have given conflicting results. Wilkinson and colleagues21 found significantly higher 6-month death rates in South Asians with an acute MI than in indigenous control subjects. Two other studies did not demonstrate a difference up to 4 years after MI, but their samples were smaller.5,6 Our study has the largest sample, but we examined only in-hospital mortality (within the first week after MI). The fact that early death rates were similar suggests that the pathology of acute MI is similar among Canadians of South Asian and non-South Asian ancestry.
Our study had limitations. It was based on a retrospective review of charts from 2 hospital sites, and thus the results are not necessarily generalizable to the entire Canadian population. Although theoretically our data on differences in risk factors between South Asian patients and non-South Asian control patients with MI should not be extrapolated to a random sample of subjects from either group, the Study of Health Assessment and Risk in Ethnic groups,18 based on population sampling, demonstrated higher rates of diabetes among South Asians in Canada. An additional limitation was the possible contamination of case and control subjects based on surnames and given names of ambiguous ethnic origin. As well, reliance on self-reporting of some risk factors may have led to inaccuracies in reporting. Such inaccuracies are generally random and would tend to minimize differences between the groups toward the null.
Conclusion
Given the increasing numbers of Canadians of South Asian origin coupled with their higher risk of cardiovascular disease, it is important for the Canadian medical community to understand the unique characteristics of South Asians presenting with acute MI. Public health efforts should be focused on increasing the awareness of the symptoms of acute MI in South Asian communities, as has been done for Canadians of non-South Asian origin. Further studies are needed to assess longer-term outcomes and to determine whether it is appropriate to develop prevention and treatment strategies specific to South Asian patients experiencing acute MI.
Acknowledgments
Mr. Doobay is a recipient of a Heart and Stroke Foundation of Ontario John D. Schultz Science Student Scholarship. Dr. Anand is a recipient of a Medical Research Council of Canada Clinician Scientist Award. Dr. Yusuf is a recipient of a Canadian Institutes of Health Research Senior Career Scientist Award and holds a Heart and Stroke Foundation of Ontario Research Chair. This study was supported in part by an unrestricted grant from Bristol-Myers Squibb Canada.
Footnotes
This article has been peer reviewed.
Contributors: Drs. Gupta, Singh, Anand and Yusuf contributed significantly to the study design, data collection and analysis, and manuscript development. Dr. Raja, Ms. Mawji, Ms. Karavetian, Mr. Kho and Mr. Yi contributed significantly to data collection and analysis, and to manuscript review.
Competing interests: None declared.
Correspondence to: Dr. Salim Yusuf, Canadian Cardiovascular Collaboration, Hamilton General Hospital, 237 Barton St. E, Hamilton ON L8L 2X2 [Reprints will be available only to individuals in developing countries.]
References
- 1.The changing face of heart disease and stroke in Canada 2000. Ottawa: Heart and Stroke Foundation of Canada; 2000. p. 23-44.
- 2.1996 census: population by ethnic origin. Ottawa: Statistics Canada; 1997.
- 3.Sheth T, Nair C, Nargundkar M, Anand S, Yusuf S. Cardiovascular and cancer mortality among Canadians of European, south Asian and Chinese origin from 1979 to 1993: an analysis of 1.2 million deaths. CMAJ 1999;161:132-8. Available: www.cma.ca/cmaj/vol-161/issue-2/0132.htm [PMC free article] [PubMed]
- 4.Enas EA, Mehta J. Malignant coronary artery disease in young Asian Indians: thoughts on pathogenesis, prevention and therapy. Clin Cardiol 1995;18:131-5. [DOI] [PubMed]
- 5.Hughes LO, Raval U, Raftery EB. First myocardial infarction in Asian and white men. BMJ 1989;298:1345-50. [DOI] [PMC free article] [PubMed]
- 6.Mukhtar HT, Littler WA. Survival after acute myocardial infarction in Asian and white patients in Birmingham. Br Heart J 1995;73:122-4. [DOI] [PMC free article] [PubMed]
- 7.International classification of diseases. 9th revision. Geneva: World Health Organization; 1978. [PubMed]
- 8.Anand SS, Yusuf S, Vuksan V, Devanesan S, Montague P, Kelemen L, et al. The Study of Health Assessment and Risk in Ethnic groups (SHARE): rationale and design. Can J Cardiol 1998;41:1349-57. [PubMed]
- 9.Canadian Consensus Conference on Coronary Thrombolysis. Recommendations. Can J Cardiol 1993;9:559-65. [PubMed]
- 10.Jha P, Enas EA, Yusuf S. Coronary artery disease in Asian Indians: prevalence and risk factors. Asian Am Pac Isl J Health 1993;1:164-75. [PubMed]
- 11.Gupta M, Singh N, Warsi M, Reiter M, Ali K. Canadian South Asians have more severe angiographic coronary disease than European Canadians despite having fewer risk factors. Can J Cardiol 2001;17(Suppl C):226C.
- 12.Hughes LO, Cruickshank JK, Wright J, Raftery EB. Disturbances of insulin in British Asian and white men surviving myocardial infarction. BMJ 1989; 299: 537-41. [DOI] [PMC free article] [PubMed]
- 13.Bhatangar D, Anand IS, Durrington PN, Patel DJ, Wander GS, Mackness MI, et al. Coronary risk factors in people from the Indian subcontinent living in West London and their siblings in India. Lancet 1995;345:405-9. [DOI] [PubMed]
- 14.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991;337:382-6. [DOI] [PubMed]
- 15.Dhawan J, Bray CL, Warburton R, Ghambhir DS, Morris J. Insulin resistance, high prevalence of diabetes, and cardiovascular risk in immigrant Asians. Genetic or environmental effect? Br Heart J 1994;72:413-21. [DOI] [PMC free article] [PubMed]
- 16.McKeigue PM, Ferrie JE, Pierpoint T, Marmot MG. Association of early-onset coronary heart disease in South Asian men with glucose intolerance and hyperinsulinemia. Circulation 1993;87:152-61. [DOI] [PubMed]
- 17.Knight TM, Smith Z, Whittles A, Sahota P, Lockton JA, Hogg G, et al. Insulin resistance, diabetes, and risk markers for ischaemic heart disease in Asian men and non-Asian in Bradford. Br Heart J 1992;67:343-50. [DOI] [PMC free article] [PubMed]
- 18.Anand SS, Yusuf S, Vuksan V, Devanesan S, Teo KK, Montague PA, et al. Difference in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet 2000;356:279-84. [DOI] [PubMed]
- 19.McKeigue PM, Marmot MG. Mortality from coronary heart disease in Asian communities in London. BMJ 1988;297:903. [DOI] [PMC free article] [PubMed]
- 20.Dhawan J, Bray CL. Angiographic comparison of coronary artery disease between Asians and Caucasians. Postgrad Med J 1994;70:625-30. [DOI] [PMC free article] [PubMed]
- 21.Wilkinson P, Sayer J, Laji K, Grundy C, Marchant B, Kopelman P, et al. Comparison of case fatality in south Asian and white patients after acute myocardial infarction: observational study. BMJ 1996;312:1330-3. [DOI] [PMC free article] [PubMed]


