Abstract
Objective
to map scientific evidence on the extent of tuberculosis in migrants from the international borders between Brazil and the countries of South America.
Design
Scoping review of quantitative, qualitative and mixed studies. The research was conducted between February and April 2021. The terms “migrants”, “tuberculosis”, “Brazil”, “Uruguay”, “Paraguay”, “Bolivia”, “Peru”, “British Guiana” “English Guiana”, “French Guiana”, “Suriname”, “Venezuela”, “Argentina”, “Colombia” combined with Boolean operators “AND” and “OR” to identified relevant documents. Studies addressing tuberculosis on migrants from international borders of Brazil were included. Pubmed Central (PMC), LILACS (Scientific and technical literature of Latin America and the Caribbean/BVS), Scopus (Elsevier), Scielo (Scientific Electronic Library Online) and gray literature CAPES thesis database were searched. The study was carried out in three stages where the data was selected and extracted by two independent reviewers for full reading.
Results
A total of 705 articles were extracted from the databases chosen for the search, 04 master's dissertations and 01 doctoral thesis. Of these 456 were excluded because they did not meet at least one of the eligibility criteria for this SR and 4 were further excluded because they were duplicates who had not been previously identified. A total of 58 documents were, thus, selected for assessment of the full text. Of these, 40 were further excluded for not meeting at least one of the eligibility criteria. A total of 18 studies were included for data collection: 15 articles, 2 master's dissertations and 1 doctoral thesis, produced between 2002 and 2021.
Conclusion
This scoping review mapped the existing evidence on tuberculosis at the international borders of Brazil and on access of immigrants with tuberculosis to health services in Brazil.
Descriptors
tuberculosis; immigrants; public health surveillance; epidemiological surveillance; sanitary control of borders; health services accessibility.
1. Introduction
International Migration refers to the “Movements of persons who leave their countries of origin or habitual residence to settle, permanently or temporarily, in another country. Consequently, it implies the crossing of international borders” (Organização Internacional das Migrações O. Glossário sobre Migração 2017). Migration is a constant evolving phenomenon that can have several motivations and legal frameworks. However, the main types of international migration continue to be labor migration (of legal or illegal workers), migration of refugees and displaced persons (Cierco, 2017).
Tuberculosis (TB) is an infectious disease transmitted from person to person through aerosol droplets caused by Mycobacterium tuberculosis (Silva et al., 2021). In most part of individuals who come into contact with the bacillus the primary infection is asymptomatic and when it manifests in adults the disease usually presents unspecific symptoms that include daytime fever, night sweating, weight loss, anorexia, malaise and weakness and the progression of the disease leads to the development of cough (Silva et al., 2018). Among the factors that can lead to the risk of developing the disease after the first contact, the individual's immune impairment is the main one (Santos et al., 2021).
International migrants are considered particularly vulnerable to TB (Guidance document on migration and health - PAHO/WHO | Pan American Health Organization n.d.). During the migration process, it is common for migrants to be subject to high stress situations such as food shortages, housing with poor health and crowding and lack of access to health services, which can induce the dissemination and maintenance of high loads of TB (Tavares et al., 2017, Boudville et al., 2020). Another situation that reinforces the vulnerabilities is the process of relocating these immigrants in the host country, where language barriers, documentary difficulties, costs of access to health systems, precarious housing conditions and the difficulties of access to income and essential services expose these immigrants to a higher risk of contact with tuberculosis (Moreira et al., 2020).
Brazil borders with a total of 10 countries and it is among the 22 countries with higher burden of TB with around 80,000 new cases and 5,000 deaths from the disease per year (Global Tuberculosis Report 2019 n.d.). Tuberculosis is an important and preventable cause of health lost due to premature death and disability in Brazil (Ferrer et al., 2014), a recent study calculated using the disability-adjusted life year (DALY), showed that the highest age-standardized DALY rates in 2017 were observed in States of the North and Northeast Brazilian regions, mainly in scenarios associated with social vulnerabilities (individuals in extreme poverty, precarious housing and difficulties in access to health services) (Martins-Melo et al., 2020).
Brazil is the only country in South America to have a universal, free at point-of-delivery public health system (Giovanella et al., 2007). Since the creation of the Common Market of the South (MERCOSUR), in 1991, that established the free movement of persons and goods among Member States, persons can freely circulate between the neighboring countries of Brazil - Argentina, Paraguay, Uruguay and Venezuela (Hortelan et al., 2019). As such, the border municipalities in Brazil deliver care to a population of international migrants, who enter the country in a legal or illegal way and who seek resolution for their health issues in the Unified Health System (SUS) of Brazil, including TB, a common and well described denominator to Latin-American Countries (Giovanella et al., 2007).
Previous studies carried out in municipalities in the tri-border region between Brazil, Paraguay and Bolivia showed that, between 2007 and 2010, in the 12 municipalities of South Mato Grosso (Brazil), located on the border with Paraguay and Bolivia, 2,981 new cases of TB and 218 deaths due to TB were reported, 49.1 new cases per 100,000 inhabitants and 4.0 deaths per 100,000 inhabitants, respectively, 1.6 and 1.5 times higher in border regions than in non-border regions (Marques et al., 2014, Silva et al., 2018). In these municipalities, the structural deficiencies of health services for the capture of TB patients are striking and often lead to the underreporting of new cases and hinder the mapping of the epidemiological profile of the disease in these territories (Braga et al., 2011).
The most recent wave of migration at the international borders of Brazil refers to the Venezuelan migration. The United Nations High Commissioner (UNHCR) reports that, in 2018, of the 80,000 requests for refuge applied in Brazil, about 60,000 were from Venezuelan citizens, with a distribution of requests for refuge concentrated mainly in the states of Roraima (50,770), Amazonas (10,500) and São Paulo (9,977). In 2017, Roraima had received about 16,000 requests for refuge, which represented a 3-fold increase in the number of requests for this territory in 2018 (Refugio-em-números_versão-23-de-julho-002.pdf n.d.). One of the last official epidemiological reports made by the Venezuelan government pointed to a 68% increase in the number of tuberculosis cases (7,816 new cases) in the year 2016, in Venezuela, with an incidence rate of 32.4/100,000 inhab. considered the highest in the country in 40 years (Maurera et al., 2019). Evidence seems to point-out to a regular migratory flow at the international borders of Brazil, as well as the active transmission of TB in these contexts.
In this study, we conducted a scoping review to map, in a comprehensive way, scientific evidence on the extent of tuberculosis in migrants from the international borders between Brazil and the countries of South America.
2. Material and method
We conducted a scoping review (SR) based on the recommendations of the Joanna Briggs Institute – JBI (Aromataris, n.d.) to answer to the research question “What is the scientific evidence on the extent of tuberculosis in migrants from the international borders between Brazil and the countries of South America?”. To answer to this question, we defined the Population (P) as migrants, the concept (C) as Tuberculosis and the Context (C) as international borders of Brazil (Aromataris, n.d.).
2.1. Eligibility criteria
The eligibility criteria for this SR were i) quantitative, qualitative or mixed method studies, including systematic reviews, primary and secondary studies and official manuals ii) written in Portuguese, English or Spanish; iii) addressing the epidemiology of TB in migrants from Brazil's international borders and access to health services by migrants with TB from Brazil's international borders. No time limit was defined for this SR.
2.2. Information sources
The research was conducted between February and April 2021, in Pubmed Central, LILACS, Scopus (Elsevier), Scielo (Scientific Electronic Library Online) and CAPES Theses Bank for gray literature.
The terms “migrants”, “tuberculosis”, “Brazil”, “Uruguay”, “Paraguay”, “Bolivia”, “Peru”, “British Guiana” “English Guiana”, “French Guiana”, “Suriname”, “Venezuela”, “Argentina”, “Colombia” combined with Boolean operators “AND” and “OR” to identified relevant documents. The detailed search is available from authors upon request (supplementary material).
2.3. Selection of sources of evidence and data charting
We used the basic tool form provided by the JBI Manual (supplementary material) for data search and extraction process (Peters et al., 2015) . The references of the retrieved studies were imported to ZOTERO reference management program (Roy Rosenzweig Center for History and New Media » Zotero n.d.).
The search in the databases was performed by 01 reviewer and the selection of studies, analysis and data extraction was performed by 2 independent reviewers.
The main characteristics of each study were synthetized in a table according to the population, concept and context. No critical appraisal of individual sources of evidence was conducted.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
3. Results
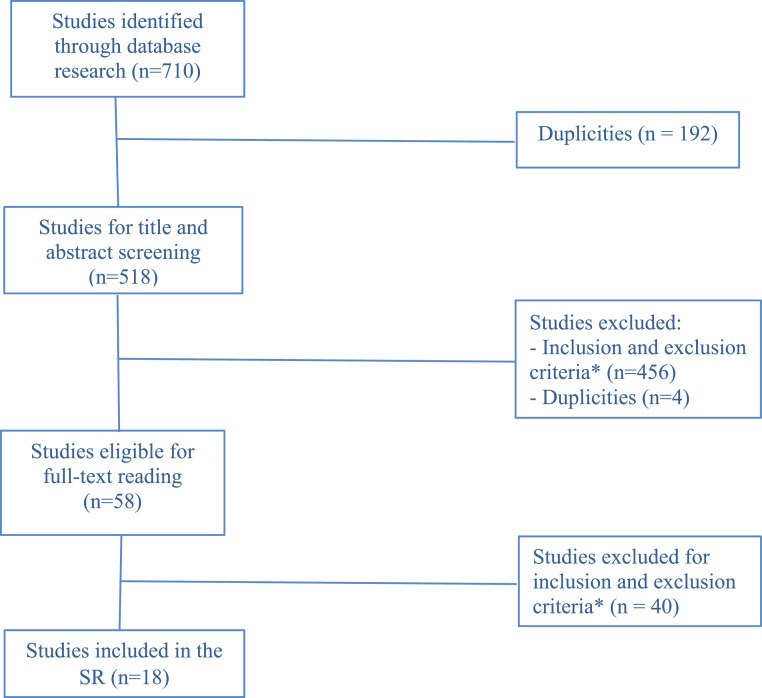
A total of 710 documents, including 705 articles, 4 master dissertations and 1 doctoral thesis were retrieved from the databases (additional studies identified through Gray Literature). A total of 187 duplicates were identified and excluded leaving 518 documents for assessment of the title and abstract. Of these 456 were excluded because they did not meet at least one of the eligibility criteria for this SR and 4 were further excluded because they were duplicates who had not been previously identified.
A total of 58 documents were, thus, selected for assessment of the full text. Of these, 40 were further excluded for not meeting at least one of the eligibility criteria.
Thus, 18 studies were finally included in this scoping review. A Flowchart is presented in Fig. 1.
Fig. 1.
Flowchart for inclusion of studies in the SR
* Eligibility criteria: population (P): studies including migrants with tuberculosis, coming from all countries of Brazil's international borders, served in the Brazilian Unified Health System; concept (C): studies addressing the descriptive and analytical epidemiology of tuberculosis in migrants from Brazil's international borders; context (C): studies including access of migrants with tuberculosis to health services at Brazil's international borders, including all entrance doors: primary care, medium and high complexity and all forms of access: diagnosis, treatment, follow-up of tuberculosis cases.
Of the 18 documents included, 15 were peer reviewed indexed articles, 2 were master's dissertations and 1 was a doctoral thesis. These had been produced between 2002 and 2021. As for the design of the studies, the majority (n=5) were qualitative studies, 4 were quantitative, 4 were molecular epidemiology studies, 3 were literature reviews and 2 were mixed methods studies. Table 1 describes the year, authors and country of the included studies.
Table 1.
Studies included in the Scoping review, by title, author, year and country of publication.
| Ref. | Author | Title of the Study | Year | Country |
|---|---|---|---|---|
| (Goldberg, 2013) | Goldberg A. | A comparative approach to the incidence of tuberculosis in Bolivian immigrants from Buenos Aires and São Paulo | 2013 | Argentina and Brazil |
| (Guerra and Bioética, 2017) | Guerra, K.; Ventura, M. | Bioethics, immigration, and health care: tensions and convergences on the human right to health in Brazil in the regional integration of countries | 2017 | Brazil |
| (Martes and Faleiros, 2013) | Martes, A. C. B.; Faleiros, S. M. | Bolivian immigrants’ access to public health services in the city of São Paulo | 2013 | Brazil |
| (Ritacco et al., 2012) | Ritacco, V., et al. | Conspicuous multidrug-resistant Mycobacterium tuberculosis cluster strains do not trespass country borders in Latin America and Spain | 2012 | Spain |
| (de Lima Junior et al., 2019) | de Lima Junior M. M., et al. | Evaluation of emerging infectious disease and the importance of SINAN for epidemiological surveillance of Venezuelans immigrants in Brazil | 2019 | Brazil |
| (Walter et al., 2021) | Walter, K.S., et al. | Local and Travel-Associated Transmission of Tuberculosis at Central Western Border of Brazil, 2014–2017 | 2021 | Brazil |
| (Pescarini et al., 2018) | Pescarini, J. M. et al. | Migration and tuberculosis transmission in a middle-income country: a cross-sectional study in a central area of São Paulo, Brazil | 2018 | Brazil |
| (Pescarini et al., 2017) | Pescarini, J. M. et al. | Migration to middle-income countries and tuberculosis -global policies for global economies | 2017 | Brazil |
| (Aguiar and Mota, 2014) | Aguiar, M.E.; Mota, A. | The Family Health Program in the neighborhood of Bom Retiro, SP, Brazil: communication between Bolivians and health workers | 2014 | Brazil |
| (Arruda-Barbosa and Sales, 2020) | Arruda-Barbosa L. de, et al. | Reflections of Venezuelan immigration in health care at the largest hospital in Roraima: qualitative analysis | 2020 | Brazil |
| (Filliol et al., 2002) | Filliol, I., et al. | Spoligotyping and IS6110-RFLP typing of Mycobacterium tuberculosis from French Guiana: a comparison of results with international databases underlines interregional transmission from neighboring countries | 2002 | French Guiana |
| (Belo et al., 2013) | Belo E. N., et al. | Tuberculosis in the municipalities of Amazonas of the Brazil-Colombia-Peru-Venezuela border: epidemiological situation and factors associated with dropout | 2013 | Brazil |
| (Pinto et al., 2018) | Pinto P.F.P.S. et al. | Tuberculosis among South American immigrants in Sao Paulo municipality: an analysis in space and time | 2017 | Brazil |
| (Page et al., 2019) | Page K.R., et al. | Venezuela's public health crisis: a regional emergency | 2019 | Venezuela |
| (Melo and Campinas L de, 2010) | Melo R.A; Campinas, L.L.S.L. | Multiculturality and morbidity reported by Bolivian immigrants in the Family Health Strategy | 2010 | Brazil |
| (Martinez, 2010) | Martinez, V.N. | Equity in health: the case of tuberculosis in the Bolivian community in the city of São Paulo - Master's dissertation | 2010 | Brazil |
| (Mello FMRVB de D e 2014) | Deus e Mello, F.M.R.V.B. | Health and Migration Process: exploratory study on access to health and tuberculosis in the Bolivian Community of the Municipality of São Paulo - Master's dissertation | 2014 | Brazil |
| (Pescarini, 2016) | Pescarini, J.M. | Transmission of Tuberculosis among South American migrants and Brazilian populations under greater vulnerability in the city of São Paulo: Implications for Tuberculosis Control - PhD thesis | 2016 | Brazil |
To facilitate the presentation and interpretation of the extracted results, after the analysis and full reading of the selected studies, the results were grouped based on the PCC strategy and are shown in Table 2.
Table 2.
Characterization and synthesis of the main results extracted for this scoping review by type of study, author, population, concept and context.
| Author | Population | Concept | Context | Results |
|---|---|---|---|---|
| Qualitative studies | ||||
| (Goldberg, 2013) |
Bolivian immigrants who work in Brazil and Buenos Aires under conditions that favor TB transmission. | TB in immigrants | Comparison of risk factors for TB transmission in Bolivian Immigration in the city of São Paulo - Brazil and Buenos Aires - Argentina | In the contexts of Brazil and Argentina the work of immigrants is carried out in overcrowded environment an several hours worked (between 15 and 18 hours per day). The characteristics of the work generally cause severe postural, respiratory and vision problems, chronic anemias and a decrease in defenses that can lead to diseases such as TB. |
| (Martes and Faleiros, 2013) |
23 Bolivian immigrants’ men and women, over the age of 20; 74% were women and 26% were men. Most interviewees (65%) are in the 20 to 30 years age group, that is, young and in productive age. | Immigrants’ accesses and qualification to the health public services | The fastest growing migratory flows in contemporary Brazil | It is possible that the occurrence of cases such as TB in Bolivian immigrants in Brazil can be explained considering the factors that impact the exit context, also because there are similar cases among Bolivian immigrants in Argentina; |
| (Aguiar and Mota, 2014) |
Three Bolivian immigrants, users of primary health care unit and six of the health professionals working there (manager, doctor, nurse, nursing technician and two community health workers, one of them Bolivian) | Migrants’ accesses to primary health services | The primary health care as immigrants gateway to meet health needs and the treatment of diseases such as TB | The relationship of the Bolivian immigrant with the Primary care unity has a fundamental meaning. Actions to improve communication are related as the creation of educational material in the Spanish language, including issues related to TB among other diseases. Usually, when a patient moves from one micro area to another, the health agents carry out a transfer of register between them. These adaptations facilitate the continuity of the treatment and the cure outcomes of Bolivian immigrants with TB. |
| (Arruda-Barbosa and Sales, 2020) |
15 nursing hospital workers: eight women and seven men. | The effects of immigration on health services and quality of care in a Public Hospital | The impact of high flow of Venezuelan migration to Brazil on hospital health services | TB is recognized by health professionals as one of the most common diseases among Venezuelan migrants seeking hospital care, especially with the most severe/advanced forms of the disease. |
| (Mello FMRVB de D e 2014) |
Health legislation in Brazil and Bolivia and secondary data on Bolivian immigration in Brazil. | Migration process of Bolivians in São Paulo | Comparison between health systems in Bolivia and Brazil and the high TB rate among Bolivian migrants | There was a deficit of epidemiological surveillance policies of TB and access to health in Bolivia, working and housing conditions that promote the spread of TB among Bolivian immigrants. Health systems in Brazil and Bolivia do not dialogue with each other for joint actions to monitor diseases such as TB. |
| Quantitative studies | ||||
| (de Lima Junior et al., 2019) |
Secondary data available in the reporting system on infectious diseases (SINAN) between 2015 and 2017 concerning Venezuelans immigrants | Infectious diseases among Venezuelan migrants | Change in the epidemiological profile of infectious diseases after de beginning of the Venezuelan migration to Brazil | Cases of TB, STI, HIV / AIDS, syphilis, hepatitis and leishmaniasis reported by Brazilian and Venezuelan migrants. More cases of TB were reported among Venezuelan immigrants (9 cases) than among Brazilians (7 cases); |
| (Belo et al., 2013) |
2157 New cases of TB reported | Factors that lead to the abandonment of TB treatment | TB treatment in Brazil's international borders in the North Arc (Amazon) | A total of 2,157 records included in the descriptive analysis, 51.9% occurred among indigenous people residents in the border region between Brazil and Colombia, Peru and Venezuela. Half of the cases came from the rural area and, among the cases of the rural area, 80% were indigenous, indicating that the villages emerged as a scenario of TB dissemination. Indigenous people have cultural and geographical difficulties in adherence to and access to Directly Observed Treatment for TB. The cases reported in the sub-regions with proximity to international borders presented greater and significant chances of treatment abandonment when compared to others sub-regions. |
| (Pinto et al., 2018) |
Immigrant population living in São Paulo and diagnosed with TB | TB in immigrants | Immigration to Brazil from South American countries | A total of 1916 new TB cases were recorded among South American immigrants residing in São Paulo, which represented 4.2% of all new TB cases in the municipality during this period. Most cases occurred in men (63.2%) and in individuals aged 15 to 29 years (72.1%). Bolivians constituted the main group of immigrants residing in high-risk TB clusters in São Paulo (79.9%). Within the low-risk spatial clusters, the largest group of the resident migrant population was composed of Argentines (26.6%), followed by Chileans (19.5%). The central area of São Paulo city showed an increasing trend in the incidence of TB in immigrants, although the trend outside the cluster was higher; |
| (Melo and Campinas L de, 2010) |
25 Bolivian immigrants, 76% of respondents were 20 to 30 years old. | TB Morbidity in immigrants | Bolivian immigrants seeking care in Primary Health Care in Brazil | About 60% of respondents reported having been affected by TB before the migration to Brazil. About 36% of respondents were in the Health Service for supervised treatment of active TB. |
| Mixed methods studies | ||||
| (Martinez, 2010) |
2.434 confirmed and reported cases of TB by bacilloscopy or culture from 1 January 1998 to 31 December 2008 in Bolivian migrants residing in the districts of Belem, Bras, Bom Retiro and Pari; 26 interviewed Bolivian immigrants in treatment for TB in Primary Health Care Unit from the selected locations. |
Epidemiological profile of TB among migrants | Bolivian migrants living in the city of São Paulo | During the study period, 2.434 cases of TB were reported, 30.4% in Bolivians. Bolivians were notified every year with a 53% increase in the number of reported cases over the period. The Bolivian TB cases were mainly in the young adult age group, average schooling, low unemployment, and sewing in the textile industry. About 85% of Bolivian immigrants in treatment at UBS were indigenous. |
| (Pescarini, 2016) |
Brazilian and South American individuals with pulmonary TB | Recent transmission of TB between Brazilians and South American migrants | South American migration to the Municipality of São Paulo | About 1764 cases of TB reported between 2013 and 2014: 79% in Brazilians and 16% in South American migrants. TB cases reported in Brazilians are characterized by an older population, predominantly male and associated with drug use, smoking, HIV and alcoholism. Fifty TB clusters were found, of which 39 were single and 11 mixed. The proportion of recent transmission of TB between Brazilians and South American immigrants, involving mixed clusters, increased from 28.1% to 41%. There was a higher proportion of mixed TB clusters among South migrants - Americans than among Brazilians. Drug users, individuals co-infected with TB/HIV, alcoholics and South American migrants suggest a greater transmission of cases resulting from recent transmission of TB. |
| Literature reviews | ||||
| (Guerra and Bioética, 2017) |
Empirical research on access to immigrant health, theoretical and ethical studies, bioethical and human rights reflections on the problem | Access to health services | Difficulties and limitations in the use of Brazilian health services by immigrants | There were 16 previous studies that presented in these results, 02 studies related to TB. It was related a high incidence of TB among the Bolivian population associated with the unhealthy conditions of sewing workshops, exhaustive work hours, treatment dropouts, and an increase in the human immunodeficiency virus (HIV) index. There were also highlighted the importance of the bond obtained by primary health care, contributing to the effectiveness of treatment. The city of São Paulo began to create specific actions for Bolivians in 2003 due to the increase in their HIV and TB rates: contract of Bolivians to act as health agents, informative on HIV prevention and TB in Spanish, and provision of Spanish courses for the professionals of the primary care units. |
| (Pescarini et al., 2017) |
Documents with strategies for TB control in migrant populations in middle-income countries | Migrants’ vulnerability and risk of contracting TB | Migrants comprise a new risk group for TB burden | Official documents describing strategies for TB control in migrant populations in middle-income countries. Income transfer programs integrated with active TB screening and strong contact tracking can have a positive impact on TB control among the poorest and most vulnerable populations, including migrant populations. Experimental provision of food baskets was associated with increased completion of TB treatment and cure rates in Brazil. There is also evidence showing a cure rate 7% higher among beneficiaries of the “Bolsa Família” program, in Brazil |
| (Page et al., 2019) |
Government and non-governmental reports and publicly available databases | Crisis in the public health system in Venezuela | Illness of the Venezuelan population | Sample: Articles published in English and Spanish until December 1, 2018. Between 2014 and 2017, TB cases increased by almost 68% (6.063 cases vs 10.185), and resistant TB (MDR) has doubled (39 against 79 cases); The incidence rate of TB in 2017 (32.4 per 100.000 inhabitants) was the highest in Venezuela in 40 years. |
| Molecular Epidemiology Studies | ||||
| (Ritacco et al., 2012) |
Epidemiological and genotyping data in all consecutive multidrug resistant TB (TB MDR) isolated in the study period with available genotypes. | Diversity of Mycobacterium tuberculosis (Mctb) genotypes that cause multidrug resistant TB | Lack of information on the transmission of TB MDR within or between Latin American countries, and between these countries and Spain | About 1000 patients with multidrug-resistant TB diagnosed from 2004 through 2008 in Argentina, Brazil, Chile, Colombia, Venezuela and Spain were compared in a database constructed ad hoc. Ten patients with Beijing genotypes were detected in the participating countries of Latin America: four in Argentina (1 Indonesian, 1 Peruvian and 2 undisclosed birth partners), three in Brazil (born in Brazil), two in Colombia (born in Colombia). |
| (Walter et al., 2021) |
Cases of pulmonary TB newly diagnosed and portrayed in 3 cities on the border of Brazil with Paraguay and Bolivia | The risk of active spread of TB in the migrant population on the borders of Brazil | Overload in the Brazilian health system in international border regions | Sample: 243 patients which were subjected to sputum culture and 215 had positive results for the culture. Twenty-seven percent of participants reported international travel in the last 5 years. Patients with a recent history of travel, defined as travel in the previous 5 years, were significantly more likely to be infected with an unassembled or single isolate (17/36) than patients with no history of travel (25/92, p = 0,03 by Fisher's exact test; odds ratio = 2,38) this is a potential evidence that they were infected outside Brazil. All four recent immigrant isolates in Brazil were unique and were out of the expected transmission clusters; again, possibly indicating that they were infected outside Brazil. |
| (Pescarini et al., 2018) |
Cases of pulmonary TB patients in the central area of São Paulo, Brazil, diagnosed between 2013 and 2014. | Migration contributes to maintenance and increase of TB loads | Presence of transmission of cross TB between South American and Brazilian migrants in the central region neighborhoods of the city of São Paulo | From 1764 cases of people with pulmonary TB, approximately 79% were Brazilians, and 19% were from other South American countries. South American migrants were younger than Brazilians (mean age 27.0 vs 38.0, p <0.001), and a higher proportion of them were female (34.6% vs 25.9%, p = 0.191). Mycobacterium tuberculosis isolates of 347 cases of 631 (55%) with positive culture were genotyped. The results had suggested that tuberculous disease after recent transmission in central areas of São Paulo is more common among Brazilians. In addition, that cross transmission between migrants and Brazilians is present, however, it is limited in both directions, from migrants to Brazilians and vice versa. |
| (Filliol et al., 2002) |
Clinical isolates of Mycobacterium tuberculosis | Phylogenetic structure of TB bacillus circulating in French Guiana | Two-thirds of TB cases in French Guiana are found among foreign patients originating essentially from Suriname and Brazil and Haiti | A total of 94 representatives of 94 patients were isolated from clinical samples at the Pasteur Institute of French Guiana between 1996 and 1998. There were founded clusters contained most isolates of relatively young Brazilian immigrants (including one isolated from a patient living in an ethnic village within the Amazon rainforest, mean age 28 years). The comparison of spoligotyping with international genotyping databases pointed to the highly diverse nature of the Mycobacterium tuberculosis population in French Guiana, with possible links to neighboring countries such as Guadeloupe, Martinique, Barbados, Haiti, Cuba, Brazil, Venezuela, Suriname and Guyana, as well as others countries of the Americas, such as Argentina, Ecuador, Honduras, Bolivia, Peru and the United States. |
3.1. Summary of the results extracted for the Scoping Review
-
•
Qualitative studies: results showed studies that compared the implementation of health policies for tuberculosis control in Brazil and countries from his international borders, and studies related to the factors that influence the process of tuberculosis illness and health access of immigrant populations in the Brazilian territory, mainly from the international borders of Argentina, Bolivia and Venezuela.
-
•
Quantitative studies: results showed studies to characterize the epidemiological profile of tuberculosis, based on statistical data, focusing on the incidence of the disease in regions of international borders of Brazil (Colombia, Peru, Venezuela, Bolivia) territories, both in rural and urban areas.
-
•
Mixed studies: results related to the sociodemographic and epidemiological profile of tuberculosis in populations of Bolivian immigrants living in urban areas of Brazil were found and about the presence of clusters of tuberculosis among vulnerable populations both national and international immigrants living together in urban territories of São Paulo in Brazil.
-
•
Literature Review: the results showed the factors that lead to tuberculosis illness in Bolivian migrants living in Brazil and the health actions implemented for access to TB treatment by these individuals, social policies that can influence the reduction of tuberculosis rates in migrant and non-migrant populations in developing countries (such as South American countries) and social factors related to the high rates of tuberculosis found in the Venezuelan population.
-
•
Molecular epidemiology studies: the results showed the circulation of Mycobacterium tuberculosis, including resistant forms of the disease, among immigrant populations actively transiting the urban and rural territories of Brazil and international border countries (Venezuela, Guyana, Argentina, Peru, Paraguay, Bolivia and Colombia).
4. Discussion
This scoping review allowed the general mapping of the available scientific production related to TB in migrants at the international borders of Brazil. Increasingly active and complex migration flows have become a challenge for international organizations due to the difficulty of guaranteeing fundamental rights to migrants in these contexts (Cierco, 2017). Immigrants move with a social, genetic and cultural background that may be directly associated with increased vulnerability of these individuals to tuberculosis infection (Gomes et al., 2017).
Qualitative, quantitative, mixed, literature review and molecular epidemiology studies were found. The qualitative studies presented relevant aspects on the relationship between the social aspects involved in the migration situation and the influence of these aspects on tuberculosis illness. The quantitative studies presented an epidemiological mapping of the distribution of disease burden in territories of international borders and in Brazilian territory, this epidemiological characterization can be an important tool for strategic decision making in the implementation of tuberculosis control actions in places of higher incidence.
The mixed studies presented a view on disease burden in international migrants in certain Brazilian national territories and on actions implemented to control tuberculosis to cover in care the peculiarities of this specific population. These studies are fundamental for the development of strategies to control tuberculosis based on experiences of the individuals themselves affected by the disease.
The review studies of Literature presented a synthesis of other studies already carried out on the theme of the illness of immigrants by tuberculosis and on legislation that guide relevant policies to combat the disease. Such studies can be used as a theoretical basis and foundation for new studies to be carried out in this theme. Molecular epidemiology studies showed results that show the active transmission of tuberculosis among migrants at international borders of Brazil, these studies are important to support the need for implementation of epidemiological surveillance of tuberculosis in Brazil's international border territories.
The results indicated a recurrent number of studies conducted in Brazil that focused mainly on the Bolivian (specifically in the State of São Paulo) and Venezuelan immigrant communities entering this country. However, studies related to the French Guiana, Argentina and to the triple borders of Brazil with Colombia and Peru and of Brazil with Paraguay and Bolivia were also found.
Data from the Epidemiological Situation of the States Parties and Associates of Mercosur showed that, until 2013, the tuberculosis incidence rate in Bolivia was 70.6 new cases per 100.000 inhabitants (Brasil, 2012). This SR revealed that Bolivians constituted the main group of immigrants residing in high-risk TB clusters in São Paulo (79.9%).
Between 1998 and 2008, one of the studies showed that 2,434 cases of TB were reported, 67.5% in Brazilians and 30.4% in Bolivians living in São Paulo - Brazil. Bolivians were notified every year with a 53% increase in the number of reported cases over the period. The incidence rate of tuberculosis in São Paulo ranged from 179.3 per100.000 inhab in 1998 to a peak of 249, 9 per 100.000 inhab in 2002 and a decline to 186, 8 per100.000 inhab in 2008. Between 2006 and 2008, the average incidence rate of tuberculosis in the city of São Paulo was 53 per 100.000 inhab. In Belém (201.2 per 100.000 inhab), Pari (157.5 per 100.000 inhab), São Brás (212.8 per 100.000 inhab) and Bom Retiro (197.0 per 100.000 inhab) (Martinez, 2010).
Currently, on the borders of South America, the largest migrations occur between Colombia, Venezuela, Chile and Brazil and are usually motivated by socioeconomic vulnerability conditions and violence that influence the social well-being and health of the population (Arenas-Suarez et al., 2021). The political and socioeconomic situation in Venezuela aggravated a crisis in the health system and increased the resurgence and proliferation of various infectious diseases that may become a major public health problem in countries with which Venezuela has borders international.
Between the years of 2014 and 2017, tuberculosis cases increased by almost 68% (6.063 cases vs 10.185), and resistant tuberculosis (MDR) has doubled (39 cases against 79 cases). The incidence rate of tuberculosis in 2017 (32.4 per 100.000 inhabitants) was the highest in Venezuela in 40 years (Page et al., 2019). The results also showed that tuberculosis is one of the most common diseases among Venezuelan migrants seeking hospital care in the border between Brazil and Venezuela, especially with the most severe/advanced forms of the disease. Between 2015 and 2017 there were more cases of tuberculosis reported among Venezuelan immigrants than among Brazilians (de Lima Junior et al., 2019, Arruda-Barbosa and Sales, 2020).
Among the results found were evidence of circulation of similar genotypes of Mycobacterium tuberculosis, (including multi-drug strains) in sputum samples of patients from Brazil and their common international borders: Argentina, Bolivia, Colombia, French Guiana, Peru and Venezuela (Filliol et al., 2002, Ritacco et al., 2012, Pescarini et al., 2018). While tuberculosis incidence declined nationally in Brazil, tuberculosis notifications have increased in Central West region border cities (Brazil, Paraguay and Bolivia). The research found genetic evidence that both local transmission and travel-associated introductions by migration contributes to incident cases even in populations deprived of liberty in these territories (Walter et al., 2021).
In the results related to the triple border between Brazil, Colombia and Peru in a total of 2.157 records included in the descriptive analysis, half of the TB cases reported came from the rural area and, among the cases of the rural area, 80% were indigenous, indicating that the villages emerged as a scenario of TB dissemination and, in this contexts, indigenous people have cultural and geographical difficulties in adherence to and access to Directly Observed Treatment for Tuberculosis (DOT) (Belo et al., 2013).
Although TB treatment is offered free of charge by the Brazilian Unified Health System, Brazil's international borders present peculiarities related to the large territorial distances between populations living in the Amazon forest areas (mostly indigenous populations with different nationalities and cultures) and the primary health service provision units, which may hinder the access and continuity of the DOT for these populations, negatively compromising the possibility of healing outcomes for these patients (Rios et al., 2013).
A theme addressed among the included studies was the access of immigrants to health services, both through the vision of patients and through the vision of health professionals. Previous evidence has been presented that the illness of immigrants with TB may be directly related to cultural issues prior to the migration process, as well as the social and health conditions experienced by immigrants both in the country of origin and in the new country (Organização Internacional das Migrações O. Glossário sobre Migração 2017). The high rates of tuberculosis in immigrant populations in Portugal - Europe are considered a reflection of the high prevalence and incidence of the disease in the immigrants' countries of origin, especially those coming from Portuguese-speaking countries (Gomes et al., 2017).
The results showed that the Bolivian population notified with TB were young adults, with average schooling, low unemployment, and most frequently seamstress employed in the textile industry. In a sample of 25 Bolivian immigrants diagnosed in a Primary Care Unit, around 60% had been affected by tuberculosis before migrating to Brazil (Martinez, 2010). However, another study showed that about 83% of Bolivian patients diagnosed in Brazil's health services did not have prior access to TB diagnosis in their country of origin (Melo and Campinas L de, 2010).
Based on the results found, we could verify that TB control actions in Bolivia are considered insufficient to combat the disease (Mello FMRVB de D e 2014) and that combined with the poverty of the population and the migratory process can be a trigger for chains of transmission of the disease among immigrants. It is possible that the occurrence of cases such as tuberculosis in Bolivian immigrants in Brazil can be explained considering the factors that impact the exit context, also because there are similar cases among Bolivian immigrants in Argentina (Martes and Faleiros, 2013).
Migrants and refugees are the most likely to submit to unhealthy jobs, low wages and precarious housing (Ventura D de and Yujra, 2019). In this review, the studies showed that the relationship between TB and Bolivian migration still suffers the influence of the environment to which they are subjected in the host countries – overcrowded work environment in rooms without ventilation, air renovation or windows (poor lighting), with accumulation of dust, damp walls, floors and ceilings, among others. The number of hours worked (between 15 and 18 hours per day) and the characteristics of the work generally increase the risk of disease including TB (Hortelan et al., 2019).
Other challenges stressed out in the included studies are difficulties in accessing TB diagnosis and early treatment, in host countries. Factors that explain these difficulties include: difference in language, lack of health literacy about access rights to the health service, document irregularity and bureaucracy to access the health system (Melo and Campinas L de, 2010, Goldberg, 2013, Martes and Faleiros, 2013, Pescarini, 2016). The lack or insufficient documents, difficulties in accessing public health care and social stigma, increase the vulnerability of immigrants and the risks of being infected and developing TB (Gomes et al., 2017, Ventura D de and Yujra, 2019).
In 2017, only 38% of Venezuelan immigrants residing in Roraima claimed to have access to the health system, 10% to the educational system and 2% to social services. About 48% had no access to any kind of public service, although universal and free coverage of these systems is guaranteed by law. There seems to be a considerable number of Venezuelan immigrants without legal authorization for residence and/or exercise of rights such as access to essential basic goods and services in the Brazilian territory in Roraima (Oliveira, 2019).
The results have shown that in Mercosur, documented migrants (who have documents such as identity card, passport, personal registration, residence permit or refugee status) have the same rights as nationals and legal residents in Brazil and can access income access programs (Bolsa Familia program) if the poverty criteria are met, however illegal migrants are not included, remaining poor and neglected. Income transfer programs integrated with active TB screening and strong contact tracing can have a positive impact on tuberculosis control among the poorest and most vulnerable populations, including migrant populations (Pescarini, 2016). Experimental provision of food baskets was associated with increased completion of TB treatment and cure rates in Brazil. There is also evidence showing a cure rate 7% higher among beneficiaries of the “Bolsa Família” program, in Brazil (Pescarini et al., 2017).
The results also highlighted the importance of the relationship between health services providers at primary health care services with immigrants in terms of TB treatment outcomes. For this purpose the city of São Paulo began to created specific actions for Bolivians in 2003 due to the increase in their HIV and TB rates: hiring of Bolivians to act as health agents, information on HIV prevention and TB in Spanish, and provision of Spanish courses for the professionals of the units (Guerra and Bioética, 2017).
It has been shown that the relationship Bolivian immigrants with primary health care services in São Paulo - Brazil is fundamental for inclusion, since the SUS card becomes a kind of identification - often the first one received in Brazil (Aguiar and Mota, 2014). Policies granting universal and free of charge access to health services for migrants have been a determining factor for the promotion of equity in health among migrants in large urban centers in Brazil and to reduce TB rates among these (Pescarini et al., 2018).
Limitations
The quality of the studies or the risk of biases of the studies was not thoroughly evaluated, thus, all studies were included in this Scoping Review, regardless of their methodological value.
5. Conclusion
Health protection measures for international migrants are a global concern. The discussion about immigration and access to health involves all the principles inherent to the Brazilian Unified Health System and mainly universality, equity, and integrality. It is necessary to maintain a permanent dialogue between health surveillance and access to health services in Brazil and with neighboring countries, given the constant dynamics of the migratory processes.
This study mapped the evidence on TB at the international borders of Brazil and on the access of immigrants to TB health services in Brazil. The main limitation of this study is related to the limited number of publications related to the thematic in relation to the territorial dimension of Brazil and the diversity of its international borders.
The results show a greater concentration of studies aimed at the immigrant Bolivian population, which can serve as a methodological and scientific basis for future research on the subject. Nevertheless, the studies analyzed still point for an existing gap of knowledge on the matter: studies on health surveillance at Brazil's international borders, health care policies for the prevention, diagnosis and treatment of tuberculosis in migrant populations at Brazil's international borders, studies on the role of primary health care for tuberculosis detection in international border areas of Brazil, studies on the impact of migration on the epidemiological profile of tuberculosis in international border areas of Brazil, among other emerging topics. Further evidence is thus needed to strengthen and inform the TB policies specially in border regions of Brazil.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmh.2023.100167.
Contributor Information
Débora de Almeida Soares, Email: dhebhorhalmeida@hotmail.com.
Aline Placeres, Email: alineplaceres@yahoo.com.br.
Ricardo A. Arcêncio, Email: ricardo@eerp.usp.br.
Inês Fronteira, Email: ifronteira@ihmt.unl.pt.
Appendix. Supplementary materials
References
- Aguiar ME de, Mota A. O Programa Saúde da Família no bairro do Bom Retiro, SP, Brasil: a comunicação entre bolivianos e trabalhadores de saúde. Interface - Comunicação, Saúde, Educação. 2014;18:493–506. doi: 10.1590/1807-57622013.0040. [DOI] [Google Scholar]
- Arenas-Suarez NE, Cuervo LI, Avila EF, Duitama-Leal A, Pineda-Peña AC. The impact of immigration on tuberculosis and HIV burden between Colombia and Venezuela and across frontier regions. Cad Saúde Pública. 2021;37 doi: 10.1590/0102-311x00078820. e00078820. [DOI] [PubMed] [Google Scholar]
- Aromataris E M Z. JBI Manual for Evidence Synthesis - JBI Global Wiki n.d. https://jbi-global-wiki.refined.site/space/MANUAL/3283910770/Chapter+11%3A+Scoping+reviews ? (accessed October 7, 2021).
- Arruda-Barbosa L de, Sales AFG, Souza ILL de. Reflexos da imigração venezuelana na assistência em saúde no maior hospital de Roraima: análise qualitativa. Saúde e Sociedade. 2020;29 doi: 10.1590/s0104-12902020190730. [DOI] [Google Scholar]
- Belo EN, Orellana JDY, Levino A, Basta PC. Tuberculosis in Amazonian municipalities of the Brazil-Colombia-Peru-Venezuela border: epidemiological situation and risk factors associated with treatment default. Rev. Panam. Salud Publica. 2013;34:321–329. [PubMed] [Google Scholar]
- Boudville DA, Joshi R, Rijkers GT. Migration and tuberculosis in Europe. J Clin Tuberc Other Mycobact Dis. 2020;18 doi: 10.1016/j.jctube.2020.100143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braga JU, Herrero MB, de Cuellar CM. Transmissão da tuberculose na tríplice fronteira entre Brasil, Paraguai e Argentina. Cad Saúde Pública. 2011;27:1271–1280. doi: 10.1590/S0102-311X2011000700003. [DOI] [PubMed] [Google Scholar]
- Brasil M da S. Ministério da Saúde; 2012. Situação epidemiológica da tuberculose nos estados partes e associados do Mercosul 2009 a 2013. [Google Scholar]
- Cierco T. Konrad Adenauer Stiftung; Rio de Janeiro: 2017. Fluxos migratórios e refugiados na atualidade. [Google Scholar]
- de Lima Junior MM, Rodrigues GA, de Lima MR. Evaluation of emerging infectious disease and the importance of SINAN for epidemiological surveillance of Venezuelans immigrants in Brazil. Braz. J. Infect. Dis. 2019;23:307–312. doi: 10.1016/j.bjid.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer GCN, Silva RM da, Ferrer KT, Traebert J. The burden of disease due to tuberculosis in the state of Santa Catarina, Brazil. J Bras Pneumol. 2014;40:61–68. doi: 10.1590/S1806-37132014000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filliol I, Ferdinand S, Sola C, Thonnon J, Rastogi N. Spoligotyping and IS6110-RFLP typing of Mycobacterium tuberculosis from French Guiana: a comparison of results with international databases underlines interregional transmission from neighboring countries. Res. Microbiol. 2002;153:81–88. doi: 10.1016/s0923-2508(01)01292-x. [DOI] [PubMed] [Google Scholar]
- Giovanella L, Guimarães L, Nogueira VMR, Lobato L de VC, Damacena GN. Saúde nas fronteiras: acesso e demandas de estrangeiros e brasileiros não residentes ao SUS nas cidades de fronteira com países do MERCOSUL na perspectiva dos secretários municipais de saúde. Cad Saúde Pública. 2007;23:S251–S266. doi: 10.1590/S0102-311X2007001400014. [DOI] [PubMed] [Google Scholar]
- Global Tuberculosis Report 2019 n.d. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-report-2019 (accessed October 6, 2021).
- Goldberg A. Un abordaje comparativo en torno a la incidencia de la tuberculosis en inmigrantes bolivianos de Buenos Aires y São Paulo. REMHU: Revista Interdisciplinar da Mobilidade Humana. 2013;21:93–106. [Google Scholar]
- Gomes R, Dias S, Nunes C. Tuberculose e Imigração em Portugal: Características Sociodemográficas. Clínicas e Fatores de Risco. Rev Migraçoes. 2017:9–23. [Google Scholar]
- Guerra K, Bioética Ventura M. imigração e assistência à saúde: tensões e convergências sobre o direito humano à saúde no Brasil na integração regional dos países. Cadernos Saúde Coletiva. 2017;25:123–129. doi: 10.1590/1414-462x201700010185. [DOI] [Google Scholar]
- Guidance document on migration and health - PAHO/WHO | Pan American Health Organization n.d. https://www.paho.org/en/documents/guidance-document-migration-and-health (accessed May 25, 2022).
- Hortelan M dos S, Almeida M de L de, Fumincelli L, Zilly A, Nihei OK, Peres AM, et al. Papel do gestor de saúde pública em região de fronteira: scoping review. Acta Paulista de Enfermagem. 2019;32:229–236. doi: 10.1590/1982-0194201900031. [DOI] [Google Scholar]
- Marques M, Ruffino-Netto A, Marques AMC, de Andrade SMO, Silva BAK da, Pontes ERJC. Magnitude da tuberculose pulmonar na população fronteiriça de Mato Grosso do Sul (Brasil), Paraguai e Bolívia. Cad Saúde Pública. 2014;30:2631–2642. doi: 10.1590/0102-311x00191513. [DOI] [PubMed] [Google Scholar]
- Martes ACB, Faleiros SM. Acesso dos imigrantes bolivianos aos serviços públicos de saúde na cidade de São Paulo. Saúde e Sociedade. 2013;22:351–364. [Google Scholar]
- Martinez VN. Equidade em saúde: o caso da tuberculose na comunidade de bolivianos no município de São Paulo 2010:[91]-[91].
- Martins-Melo FR, Bezerra JMT, Barbosa DS, Carneiro M, Andrade KB, Ribeiro ALP, et al. The burden of tuberculosis and attributable risk factors in Brazil, 1990–2017: results from the Global Burden of Disease Study 2017. Population Health Metrics. 2020;18:10. doi: 10.1186/s12963-020-00203-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurera D, Bastidas G, Maurera D, Bastidas G. Características clínicas y epidemiológicas de pacientes con tuberculosis en el estado Carabobo, Venezuela. Revista Médica del Uruguay. 2019;35:32–57. doi: 10.29193/rmu.35.2.2. [DOI] [Google Scholar]
- Mello FMRVB de D e . Universidade de São Paulo; 2014. Saúde e processo migratório: estudo exploratório sobre o acesso à saúde e tuberculose na comunidade boliviana do Município de São Paulo. text. [DOI] [Google Scholar]
- Melo RA, Campinas L de LSL. Multiculturalidade e morbidade referida por imigrantes bolivianos na Estratégia Saúde da Família. Mundo Saúde. 2010;35:25–35. doi: 10.15343/0104-7809.201012535. [DOI] [Google Scholar]
- Moreira A da SR, Kritski AL, Carvalho ACC. Determinantes sociais da saúde e custos catastróficos associados ao diagnóstico e tratamento da tuberculose 2020;46:e20200015–e20200015.
- Oliveira ATR de. A Migração Venezuelana no Brasil: crise humanitária, desinformação e os aspectos normativos. Revista de Estudos e Pesquisas sobre as Américas 2019;13:219–44. doi: 10.21057/10.21057/repamv13n1.2019.24297. [DOI]
- Organização Internacional das Migrações O. Glossário sobre Migração. vol. 22. Organização Internacional para as Migrações; 2017.
- Page KR, Doocy S, Reyna Ganteaume F, Castro JS, Spiegel P, Beyrer C. Venezuela's public health crisis: a regional emergency. Lancet. 2019;393:1254–1260. doi: 10.1016/S0140-6736(19)30344-7. [DOI] [PubMed] [Google Scholar]
- Pescarini JM, Rodrigues LC, Gomes MGM, Waldman EA. Migration to middle-income countries and tuberculosis-global policies for global economies. Global Health. 2017;13:15. doi: 10.1186/s12992-017-0236-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescarini JM, Simonsen V, Ferrazoli L, Rodrigues LC, Oliveira RS, Waldman EA, et al. Migration and tuberculosis transmission in a middle-income country: a cross-sectional study in a central area of São Paulo, Brazil. BMC Med. 2018;16 doi: 10.1186/s12916-018-1055-1. 62–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pescarini JM. Transmissão da tuberculose entre migrantes sul-americanos e populações brasileiras sob maior vulnerabilidade no município de São Paulo: implicações para o controle da TB 2016:119–119.
- Peters MDJ, Godfrey CM, McInerney P, Soares CB, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: methodology for JBI scoping reviews. 2015.
- Pinto PFPS, Neto FC, de Almeida Ribeiro MCS. Tuberculosis among South American immigrants in São Paulo municipality: an analysis in space and time. Int. J. Tuberc. Lung Dis. 2018;22:80–85. doi: 10.5588/ijtld.17.0320. [DOI] [PubMed] [Google Scholar]
- Refugio-em-números_versão-23-de-julho-002.pdf n.d.
- Rios DPG, Malacarne J, Alves LCC, Sant'Anna CC, Camacho LAB, Basta PC. Tuberculose em indígenas da Amazônia brasileira: estudo epidemiológico na região do Alto Rio Negro. Rev. Panam. Salud Publica. 2013;33:22–29. doi: 10.1590/S1020-49892013000100004. [DOI] [PubMed] [Google Scholar]
- Ritacco V, Iglesias M-J, Ferrazoli L, Monteserin J, Dalla Costa ER, Cebollada A, et al. Conspicuous multidrug-resistant Mycobacterium tuberculosis cluster strains do not trespass country borders in Latin America and Spain. Infect. Genet. Evol. 2012;12:711–717. doi: 10.1016/j.meegid.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Roy Rosenzweig Center for History and New Media » Zotero n.d. https://chnm.gmu.edu/zotero/ (accessed December 13, 2021).
- Santos ACE dos, Brunfentrinker C, Pena L da S, Saraiva S dos S, Boing AF. Análise e comparação dos desfechos do tratamento de tuberculose na população em situação de rua e na população geral do Brasil. J Bras Pneumol. 2021;47 doi: 10.36416/1806-3756/e20200178. [DOI] [Google Scholar]
- Silva MEN da, Lima DS de, Santos JE dos, Monteiro ACF, Torquato CMM, Freire VA, et al. Aspectos gerais da tuberculose: uma atualização sobre o agente etiológico e o tratamento. Rev Bras Anal Clin. 2018:228–232. [Google Scholar]
- Silva IV, Campos RB, Silva-Sobrinho RA, Nihei OK. Tuberculose em Áreas de Fronteira: Óbitos e Doenças Associadas. Revista Pleiade. 2018;12:14–22. [Google Scholar]
- Silva DR, Rabahi MF, Sant'Anna CC, Silva-Junior JLR da, Capone D, Bombarda S, et al. Consenso sobre o diagnóstico da tuberculose da Sociedade Brasileira de Pneumologia e Tisiologia. J Bras Pneumol. 2021;47 doi: 10.36416/1806-3756/e20210054. [DOI] [Google Scholar]
- Tavares AM, Fronteira I, Couto I, Machado D, Viveiros M, Abecasis AB, et al. HIV and tuberculosis co-infection among migrants in Europe: A systematic review on the prevalence, incidence and mortality. PLoS One. 2017;12 doi: 10.1371/journal.pone.0185526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura D de FL, Yujra VQ. Saúde de migrantes e refugiados. SciELO - Editora FIOCRUZ; 2019 [Google Scholar]
- Walter KS, Tatara MB, Esther da Silva K, Moreira FMF, Dos Santos PCP, de Melo Ferrari DD, et al. Local and Travel-Associated Transmission of Tuberculosis at Central Western Border of Brazil, 2014-2017. Emerg. Infect. Dis. 2021;27:905–914. doi: 10.3201/eid2703.203839. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.