Abstract
Background
Long-term sequelae are frequent and often disabling after epidermal necrolysis (Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN)). However, consensus on the modalities of management of these sequelae is lacking.
Objectives
We conducted an international multicentric DELPHI exercise to establish a multidisciplinary expert consensus to standardize recommendations regarding management of SJS/TEN sequelae.
Methods
Participants were sent a survey via the online tool “Survey Monkey” consisting of 54 statements organized into 8 topics: general recommendations, professionals involved, skin, oral mucosa and teeth, eyes, genital area, mental health, and allergy workup. Participants evaluated the level of appropriateness of each statement on a scale of 1 (extremely inappropriate) to 9 (extremely appropriate). Results were analyzed according to the RAND/UCLA Appropriateness Method.
Results
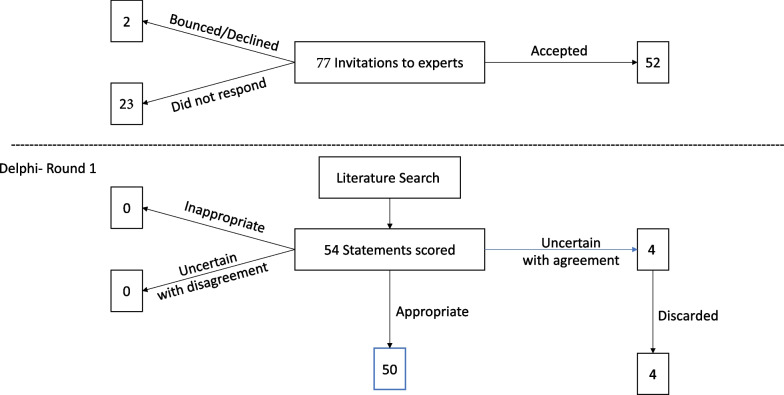
Fifty-two healthcare professionals participated. After the first round, a consensus was obtained for 100% of 54 initially proposed statements (disagreement index < 1). Among them, 50 statements were agreed upon as ‘appropriate’; four statements were considered ‘uncertain’, and ultimately finally discarded.
Conclusions
Our DELPHI-based expert consensus should help guide physicians in conducting a prolonged multidisciplinary follow-up of sequelae in SJS-TEN.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13023-023-02631-7.
Keywords: Epidermal necrolysis, Stevens-Johnson syndrome, Toxic epidermal necrolysis, Sequelae, Quality of life, Delphi, Consensus
Introduction
Epidermal necrolysis (EN), including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN, or Lyell syndrome) is a rare but severe delayed hypersensitivity reaction characterized clinically by purpuric macules, a variable extent of epidermal detachment (SJS, < 10% detached-detachable body surface area, overlap syndrome 10–29%, TEN, ≥ 30%) and mucous membrane (MM) involvement [1]. EN is induced by drugs in 85% of cases, but some cases remain “idiopathic” [2, 3]. Pathophysiology leading to epidermis and epithelia apoptosis and necrolysis is complex [4, 5]. The incidence ranges from 1–2 to 6 cases per million inhabitants per year [6]. Overall mortality, which can be predicted on an individual scale by the SCORTEN in the acute phase, is approximately 15% [7–9]. The cornerstones of management during the acute phase are the quick cessation of the culprit drug, and optimized supportive care in reference centers [10, 11]. International guidelines, including a recent DELPHI exercise, summarized the key points of this management [12–15].
After the acute phase, long-term sequelae have been described, with significant impact on the quality of life. The main ones are cutaneous (e.g. pigmentation issues, hypertrophic scars), ocular (from minor dryness to severe conjunctival inflammation, synechiae and corneal defects that may lead to blindness), and psychological distress [16–21]. Consequently, a prolonged multidisciplinary follow-up is warranted, but there is no consensus about the practical modalities of this follow-up.
Our aim in this multicenter DELPHI exercise was to harmonize modalities of follow-up of patients after the acute phase of EN.
Methods
Panel selection
The project was initiated by the SJS/TEN subgroup (ToxiTEN group) of the skin European Reference Network (ERN-skin), which is composed of dermatologists. An international multidisciplinary panel of experts in the field of EN was subsequently established. Participants were identified from academic centers that provide inpatient dermatology or intensive care services specialized in EN patient care. In total, 77 experts were identified and invited via email to participate in the DELPHI exercise. Of them, there were 39 dermatologists, 14 allergologists, 12 ophthalmologists, 3 psychologists/psychiatrists, 3 gynecologists, 3 nurses specifically involved in EN, 2 burn surgeons and 1 dentist. All participants were solicited to assess only the statements in their field of expertise.
Of the 77 identified experts, 23 did not respond to the invitation to participate, 2 declined, and the remaining 52 agreed to participate (Fig. 1).
Fig. 1.
Top: Flow chart of the experts. Bottom: Flow chart of the statements
Statements
Participants were sent an online survey consisting of 54 statements regarding EN after-care follow-up. Statements were established by the steering committee of the study (four experts of epidermal necrolysis [MCB, LF, SW, SIHO], and one dermatology resident [VS]). The statements were based on previously published studies and reviews on the topic as well as our routine practice experience and assessment of SJS/TEN patient management [13]. We screened Pubmed for literature on SJS/TEN aftercare in the past 15 years (2006–2021, papers in English; search keywords: toxic epidermal necrolysis, Stevens-Johnson syndrome, AND sequelae, quality of life, follow-up). Different types of articles were included: general/review articles about EN and original articles on the main physical (eyes, skin, genital, dental) and psychological sequelae and health-related quality of life in this disease. For the topic of allergological work-up, we screened Pubmed literature without time limitation using the following key words: toxic epidermal necrolysis, Stevens-Johnson syndrome, AND allergological work-up, skin testing, in vitro tests, patch tests, lymphocyte transformation test. Statements were organized into 8 categories: general recommendations, professionals involved, skin, oral mucosa and teeth, eyes, genital area, mental health, and allergy workup (in vivo and in vitro tests).
An online tool, “Survey Monkey”, was used to distribute surveys. Participants were asked to evaluate the level of appropriateness of statements on a scale of 1 (extremely inappropriate) to 9 (extremely appropriate). Participants were given the option of selecting “N/A” (not applicable) if they felt they did not have the necessary expertise to rank a particular statement. Participants also had the opportunity to submit comments to be incorporated into subsequent DELPHI rounds. Members of the steering committee (MCB, LF, SW, SIHO) did not respond to the survey.
Statistics
Results were analyzed according to the RAND/UCLA Appropriateness Method. The median rating for appropriateness, interpercentile range (IPR), interpercentile range adjusted for symmetry (IPRAS), and disagreement index (DI) were calculated (DI = IPR/IPRAS) for each statement [22]. Median appropriateness values were assessed as follows: 1.0 to 3.4 was considered “inappropriate”, 3.5 to 6.9 as “uncertain” and 7.0 to 9.0 as “appropriate.” A disagreement index (DI) < 1 indicated a consensus obtained among the participants in terms of a statements’ appropriateness.
Results
Participants and DELPHI exercise
Fifty-two of the 77 participants (Fig. 1 Top) who agreed to participate in the DELPHI exercise responded (67.5% response rate). Participants (women n = 26) were from 8 specialties (dermatologists n = 24, allergologists n = 11, participants from 6 other specialties n = 17), and 18 different countries on 4 continents. There were no significant differences in terms of sex and specialties among responders and non-responders (data not shown).
The statements on which the panel ‘agreed’ were ‘appropriate’ were used for the consensus.
First round
A consensus was reached for all of the 54 statements (100%). Four statements were labelled as ‘uncertain’ in the section “Eyes“, “Mental health“ and “Allergological workup“. Statements were discarded based on the discussion and reassessment by the steering committee (Fig. 1 Bottom). The statements that were discarded addressed the (non-)recommendation of corneal transplantation, additional measures such as hypnosis to reduce symptoms of anxiety or depression and the type and timing of allergological testing after re-epithelialization.
All statements with the respective DIs and medians are displayed in Table 1. All statements were agreed upon, with a DI < 1 (i.e. reached the necessary level of agreement). IPR and IPRAS values are displayed in Additional file 1: Table S1.
Table 1.
Items of the DELPHI-based exercise for the management of sequelae in epidermal necrolysis
| Disagreement index (DI)* | Median | |
|---|---|---|
| Items the panel agreed were ‘appropriate’ | ||
| General recommendations | ||
| A follow-up control SHOULD be performed 1–2 months after discharge from the hospital and regularly thereafter as needed | 0 | 9 |
| Professionals involved | ||
| Patients SHOULD be managed by a multidisciplinary team | 0 | 9 |
| The DERMATOLOGIST SHOULD lead in the management of follow-up | 0.531 | 8 |
| An OPHTHALMOLOGIST SHOULD be involved in case of ocular involvement | 0 | 9 |
| Support by a PSYCHIATRIST and/or PSYCHOLOGIST SHOULD be offered | 0.132 | 9 |
| A DENTIST and/or a STOMATOLOGIST SHOULD be involved in case of chronic oral mucosal involvement | 0.132 | 9 |
| An ENT specialist SHOULD be involved after discharge if there was nasopharyngeal and/or laryngeal involvement in the acute phase | 0.132 | 9 |
| A UROLOGIST SHOULD be involved in cases of severe genital involvement, where a risk of urethral synechiae/strictures exists | 0 | 9 |
| A GYNECOLOGIST SHOULD be involved in case of severe genital involvement, where a risk of vaginal synechiae/strictures exists | 0 | 9 |
| A PULMONOLOGIST SHOULD be involved after discharge if there was pulmonary involvement in the acute phase | 0.132 | 9 |
| A SOCIAL WORKER SHOULD be involved if needed | 0 | 9 |
| A DIETICIAN SHOULD be involved if needed | 0.292 | 9 |
| Skin | ||
| Patients SHOULD practise careful sun protection post-discharge | 0 | 9 |
| Patients SHOULD apply emollients daily | 0.262 | 9 |
| Laser treatment MAY be considered for hypertrophic scars | 0.374 | 7 |
| Residual skin pain SHOULD be further investigated | 0.292 | 8 |
| A NEUROLOGIST or a PAIN SPECIALIST SHOULD be involved in patients with chronic skin pain | 0.132 | 9 |
| Oral mucosa and teeth | ||
| Patients SHOULD receive specific instructions for dental health | 0.262 | 9 |
| Patients who had oral mucosa involvement SHOULD have regular dental check-ups | 0.132 | 9 |
| Specific therapy SHOULD be implemented in patients with xerostomia | 0.019 | 9 |
| Saliva substitutes SHOULD be used in patients with xerostomia | 0.132 | 9 |
| Topical sialagogues MAY be considered in patients with xerostomia | 0.292 | 8 |
| Eyes | ||
| Patients SHOULD undergo a complete ophthalmological examination as often as needed | 0 | 9 |
| An OPHTHALMOLOGIST SHOULD guide the medical treatment of ocular symptoms | 0 | 9 |
| A combination of artificial tears without preservatives and topical vitamin A SHOULD be used in patients with xerophthalmia | 0.319 | 8 |
| The use of topical cyclosporine or other immunosuppressive agent MAY be proposed in patients with severe xerophthalmia | 0.374 | 7 |
| The use of scleral lenses SHOULD be considered in patients with severe xerophthalmia and/or scarring | 0.292 | 8 |
| Surgical ocular surface reconstruction SHOULD be considered as a last resort in patients with extensive scarring | 0.724 | 7 |
| Genital area | ||
| Sequelae such as vulvodynia, vulvar and vaginal synechiae SHOULD be assessed after epithelialization | 0.018 | 9 |
| Topical corticosteroids SHOULD be considered in patients with vulvar and/or vaginal synechiae to reduce extensive scarring | 0.292 | 8 |
| Surgical correction SHOULD be considered in cases of extensive vulvar and/or vaginal scarring | 0.132 | 9 |
| Emollients SHOULD be used to avoid vulvar and vaginal dryness | 0.132 | 9 |
| Mental health | ||
| Every follow-up control SHOULD include a screening for psychological well-being | 0.132 | 9 |
| This screening SHOULD include questions on the quality of sleep, mood status, anxiety, nightmares, and symptoms of depression | 0 | 9 |
| A standardized tool such as hospital anxiety and depression score (HADS) MAY be helpful in the screening for psychological well-being | 0.132 | 9 |
| Psychological support SHOULD be actively offered to patients with chronic disabling sequelae | 0 | 9 |
| A psychological and/or psychiatric follow-up CAN help to reduce issues like post-traumatic stress disorder | 0 | 9 |
| Iatrogenic psychiatric symptoms SHOULD be excluded | 0.292 | 8 |
| Psychotropic drugs MAY be considered according to the psychiatrist’s evaluation | 0.292 | 9 |
| Allergy workup | ||
| A preliminary allergy card prohibiting the use of ALL suspect drugs MUST be given to the patient upon release from the hospital | 0 | 9 |
| The patient MUST be clearly informed during the hospital stay about the suspect drug(s), their avoidance and cross-reactivity | 0 | 9 |
| The patient’s companion/family MUST be clearly informed during the hospital stay about the suspect drug(s), their avoidance and cross-reactivity | 0 | 9 |
| Prick tests SHOULD NOT be routinely performed | 0.132 | 9 |
| Intradermal tests SHOULD NOT be routinely performed | 0.292 | 9 |
| If available, a lymphocytic transformation test (LTT) CAN be useful in the diagnostic work-up | 0.492 | 8 |
| If available, an Elispot test CAN be useful in the diagnostic work-up | 0.748 | 7 |
| A drug CANNOT be excluded as culprit agent solely based on negative results of any of the allergological tests | 0 | 9 |
| A definitive allergy card MUST be given to the patient after the allergy work-up | 0 | 9 |
| The patient MUST be clearly informed about the drug(s) on the allergy card, their avoidance and cross-reactivity after the allergy work-up | 0 | 9 |
| The general practitioner and all physicians involved in the management of the patient MUST be informed about the drug(s) on the allergy card, their avoidance and cross-reactivity after the allergy work-up | 0 | 9 |
| Items the panel agreed were ‘uncertain’ | ||
| Eyes | ||
| Corneal transplantation SHOULD NOT be recommended due to the risk of clinical exacerbation | 0.652 | 5 |
| Mental health | ||
| Additional measures such as hypnosis MAY help reducing symptoms of anxiety or depression | 0.652 | 5 |
| Allergy workup | ||
| Allergological testing SHOULD be performed at least 6–8 weeks after complete re-epithelization | 0.652 | 6 |
| Patch-tests SHOULD be performed for the diagnostic work-up | 0.519 | 5 |
| Items the panel agreed were ‘inappropriate’ | ||
| None | ||
| Items the panel disagreed | ||
| None | ||
*A disagreement index value greater than 1 indicates a lack of consensus; below 1 indicates a consensus
Discussion
Thanks to this DELPHI exercise, we obtained for the first time an international consensus for the main objectives of an optimal and standardized multidisciplinary follow-up of patients after the acute phase of SJS/TEN. Based on previous literature, we questioned multidisciplinary experts with the RAND/UCLA appropriateness method, developed by RAND corporation with clinicians at the University of California at Los Angeles (UCLA) and widely used for DELPHI exercises [22], and reached formal agreement for the cornerstones of the patients’ long-term follow-up.
Consensus was obtained after one round in key fields of patient management: general recommendations, professionals involved, follow-up care for skin, oral mucosa and teeth, eyes, genital area, and mental health and allergological workup. Only 4 statements remained ‘uncertain’. All other 50 statements resulted in an ‘appropriate’ consensus.
Regular follow-up within the first year after the acute phase must be organized and driven by a dermatologist, then after, tailored accordingly to the needs of each patient. The vast spectrum of potential sequelae requires a collaborating panel of medical specialists organized by the dermatologist for optimal care: ophthalmologist, psychiatrist/psychologist, ENT specialist, gynecologist/urologist, odontologist/dentist, pulmonologist, neurologist, and others according to the patient’s need. Furthermore, the intervention of a dietician may be mandatory within initial few weeks or months due to the frequent loss of weight during the acute phase. If required, based on the patient’s social situation and the local setup, a social worker may facilitate rehabilitation through helping to obtain financial support, especially in case of disability (e.g. visual impairment), and sometimes financial compensation for medical (iatrogenic) accident [23].
Skin sequelae are very frequent and include pigmentation disorders, hypertrophic scars, polymorphic nail changes and occasionally chronic skin pain [16, 17, 24, 25]. All of these issues can have a major impact on the patient’s quality of life. Consensus was obtained for prolonged sun protection and daily use of emollients. However, it is not possible to provide guidelines for the duration of these measures, which should be individualised for each patient, depending on his/her phototype and quality of healing. Consensus was also obtained for a consideration of laser procedures for disabling hypertrophic scars, and involvement of a neurologist in the exploration and management of chronic pain. The latter was shown to result from sensitization of both small-diameter (burning and itching sensations) and large-diameter nerve fibers (allodynia), and major affective and emotional components [26]. In our study, we did not provide statements about nail sequelae. The latter are frequent and polymorphic and often disabling for the patient, but best management guidelines are still missing [24].
Dental sequelae and xerostomia are frequent [27]. Consensus was obtained for a regular dental follow-up, for the necessary duration for each individual patient after the acute phase, and prescription of saliva substitutes or systemic or topical sialogogues such as pilocarpine or cevimeline, as have been described as effective in other xerostomia and hyposalivation syndromes [28].
Ocular sequelae are the main disabling sequela. Ocular changes of variable severity affect up to 75% of survivors with an impact on daily personal and professional life. Risk factors are the severity of the disease at the acute phase, including the severity of ocular involvement [18, 29]. Ocular change include dryness, ectropion, entropion, trichiasis, meibomian gland dysfunction, corneal erosions, ulcerations, neovascularization, stromal scarring, and conjunctivalization of the corneal surface with loss of visual acuity [16]. Consensus was obtained for the regular use of artificial tears without preservatives and topical vitamin A in xerophthalmia, together with a trial of an adjunctive topical immunosuppressant such as cyclosporine, the latter was demonstrated to be efficacious in a small study in EN as well as in other causes of dry eye, although may be poorly tolerated (pain, redness, and eyelid swelling) [30, 31]. Topical tacrolimus is an alternative, with interesting results on ocular surface persistent inflammation [32]. Scleral lens or tear-exchangeable, limbal, rigid contact lenses are used in the most disabling ocular surface sequelae, with good results in term of dryness improvement, visual rehabilitation, and global ocular comfort [33–35]. In contrast, the statement that corneal transplantation should not be recommended due to the risk of clinical exacerbation led to an ‘uncertain’ consensus result. Few studies were published on this topic, but outcome of keratoplasty in cicatrizing conjunctival diseases is poor, causing a further deterioration of vision and morbidity due to persistence of epithelial defects, stromal ulceration, perforation, and graft rejection [36].
In women, genital sequelae are not uncommon (about 20%) and include labial agglutination, introital stenosis, vaginal synechiae and stenosis, vaginal and vulval adenosis, hematocolpos, and hematometra, leading to dryness, dyspareunia and bleeding [37]. Although genitourinary sequelae are rare in children, caution is needed in this population [38, 39]. In our DELPHI exercise, consensus was obtained for the use of emollients to reduce vulvar or vaginal dryness, topical corticosteroids in case of synechiae to reduce the risk of more extensive scarring, and surgical correction in case of extensive synechiae, which require trained surgeons [40].
Psychological sequelae are frequent. Medicine avoidance is common, given that the disease is drug induced in the majority of cases. Other conditions include anxiety, depression, and nightmares. Of note, within the 6 months after the acute phase, 25% of patients develop post-traumatic stress disorder, especially in case of previous psychological fragility [19, 20]. Consensus was obtained for screening for psychological well-being at each follow-up appointment. This screening may be first conducted by the dermatologist, using standardized tools, such as the hospital anxiety and depression scale (HADS). HADS is reliable and easy to use self-assessment instrument developed 40 years ago for detecting states of depression (7 questions) and anxiety (7 questions) to guide the need for specialized intervention [41]. Intervention involves care from both a psychologist and a psychiatrist to prescribe psychotropic drugs according to each patient’s needs. Additional measures such as hypnosis to reduce symptoms of anxiety or depression remained of ‘uncertain’ appropriateness. Indeed, whereas the efficacy of hypnosis and other techniques such as relaxation was suggested in burns [42, 43], literature still lacks in psychological sequelae of EN.
Pulmonary sequelae are rare. A pulmonologist should be involved in case of severe initial lung involvement. The most frequent sequela is diffusion impairment, most often asymptomatic and this may be screened for by pulmonary function tests [44]. Other sequelae, especially bronchiolitis obliterans, are very rare and mostly described in children [45]. Due to this rarity, no statement was proposed to experts about pulmonary sequelae.
Prevention of relapse of EN is essential. Consensus was obtained for provision of an allergy card to the patient from the hospital discharge, giving clear information about the culprit drug(s) and all related contraindications (drugs of the same biochemical family / cross-reactivity). The patients, their family, the pharmacist and the primary care provider must be clearly informed of the suspected drugs, the need for avoidance and the drugs that may cross-react with the suspected agent(s).
Allergy workup may help for both the identification of the culprit drug(s) and identification of an alternative medication that may be used in the future. Performing the allergy work-up at a suggested time point of 6–8 weeks was rated as “uncertain” by the group. This statement was initially designed for cutaneous tests, but was maybe not precise enough, and it is possible that some experts understood the phrasing for in vitro tests also. Given the lack of precise literature on the topic, we decided to not suggest an alternative statement. The best time to perform tests remains to be further studied. Patch-tests to explore EN have been described in several small series, showing a positivity rate lower than in other drug reactions, but varied upon the drug tested (9 to 62%) [46–48]. Surprisingly, the statement that patch-tests should be performed for the diagnostic work-up remained ‘uncertain’ among experts. This is probably explained by the low rate of positivity, especially for high-risk drugs such as sulfasalazine and allopurinol which give always negative results [49], and by the fact that some teams would prefer performing in vitro tests very soon after the onset of the reaction [50]. To date, data about the usefulness and the safety of prick and intradermal tests are too scarce to recommend their use in EN. Consequently, to date, only patch-tests, which are safe in EN, are recommended in guidelines [47, 51, 52]. Even in case of negative results, provocation tests with the most highly suspected culprit drug(s) must not be performed in EN patients [53]. Lymphocyte transformation test, eventually combined with cytokine detection assays, may be useful if performed shortly after the acute phase, showing a positivity rate correlated to the ALDEN [50, 54, 55]. Other in vitro tests such as IFN-γ release Enzyme-Linked Immunosorbent Spot (ELISpot) assay may be useful, combined with in vivo skin testing [56]. However, these in vitro tests are often not available routinely available, and large series to assess their usefulness in EN are lacking. After allergy workup, a definitive allergy card must be given to the patients, with all information about the drug(s) contraindicated for the rest of their life and the list of cross-reactivities.
Conclusion
SJS and TEN are delayed-type severe hypersensitivity reactions associated with a high risk of long-term mucocutaneous disabling sequelae. Here, through a multidisciplinary consensus based on a DELPHI exercise, we propose for the first time a harmonization of practices emphasizing on the key points of a multidisciplinary long-term follow-up. The best timing of follow-up visits and the duration of the latter considerably vary among patients and depend on the severity of sequelae. The current expert consensus provides general recommendations that need to be case-to-case adapted (Table 2) and highlights the need to further determine details of follow-up care and to investigate the best management for rare but disabling sequelae in SJS/TEN patients.
Table 2.
Proposition for the follow-up multidisciplinary calendar after the acute phase
| 1–2 months after discharge |
Dermatologist (skin sequelae and coordination of the follow-up) Ophthalmologist Psychiatrist and/or psychologist ENT Pneumologist if needed (± pulmonary function tests) Gynecologist/urologist if needed (scarring) Dietetician if needed (loss of weight) Social worker if needed |
| 6 months* after the acute phase |
Same specialties according the needs of the patient Stomatologist/dentist Allergy work-up |
| 1 year* after the acute phase |
Same specialties according the needs of the patient Prolonged follow-up by the dermatologist to screen the needs of the patient and coordinate the multidisciplinary follow-up |
*Timing recommendations not part of the current DELPHI consensus
Supplementary Information
Additional file 1. Table S1. Disagreement index (DI), interpercentile range (IPR) and interpercentile range adjusted for symmetry (IPRAS) for all statements.
Acknowledgements
Not applicable.
Abbreviations
- EN
Epidermal necrolysis
- SJS
Stevens-Johnson syndrome
- TEN
Toxic epidermal necrolysis
- MM
Mucous membranes
- ERN
European Reference Network
- IPR
Interpercentile range
- IPRAS
Interpercentile range adjusted for symmetry
- DI
Disagreement index
- ENT
Ear nose throat
- ALDEN
Algorithm of drug causality for epidermal necrolysis
Author contributions
SIHO, SW, LEF and MCB designed the study; VS and MMA were associated to the organization of the DELPHI and analyzed the experts’ answers; STL and EM helped for the methodology of the DELPHI; RA, AB, AM, ASP, AR, BD, BHK, BBS, BYHT, BR, EB, BM, CGM, CYC, CS, JG, DGF, SMD, DT, GDP, EG, EJP, FL, CS, BH, JD, JS, JN, JTS, AD, KB, LSV, LJ, MPW, MG, ML, MT, MHN, NH, NHS, POR, PW, PR, RPDG, RGM, GST, RS, SR, SA, SLC, THF, WP responded as experts to the DELPHI statements; SIHO and MCB wrote the manuscript; SW and LEF added important contribution to the manuscript; all other authors read and approved the final manuscript.
Funding
The work was funded by ERN skin.
Availability of data and materials
The dataset(s) supporting the conclusions of this article is(are) included within the article (and its additional file(s)).
Declarations
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
S. Ingen-Housz-Oro and V. Schmidt contributed equally
L. E. French and M. C. Brüggen contributed equally
Contributor Information
S. Ingen-Housz-Oro, Email: saskia.oro@aphp.fr
M. M. Ameri, Email: saskia.oro@aphp.fr
References
- 1.Duong TA, Valeyrie-Allanore L, Wolkenstein P, Chosidow O. Severe cutaneous adverse reactions to drugs. Lancet. 2017;390:1996–2011. doi: 10.1016/S0140-6736(16)30378-6. [DOI] [PubMed] [Google Scholar]
- 2.Mockenhaupt M, Viboud C, Dunant A, Naldi L, Halevy S, Bouwes Bavinck JN, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: assessment of medication risks with emphasis on recently marketed drugs. The EuroSCAR-study. J Invest Dermatol. 2008;128:35–44. doi: 10.1038/sj.jid.5701033. [DOI] [PubMed] [Google Scholar]
- 3.Monnet P, Rodriguez C, Gaudin O, Cirotteau P, Papouin B, Dereure O, et al. Towards a better understanding of adult idiopathic epidermal necrolysis: a retrospective study of 19 cases. J Eur Acad Dermatol Venereol. 2021;35:1569–1576. doi: 10.1111/jdv.17274. [DOI] [PubMed] [Google Scholar]
- 4.Kuijper EC, French LE, Tensen CP, Vermeer MH, Bouwes Bavinck JN. Clinical and pathogenic aspects of the severe cutaneous adverse reaction epidermal necrolysis (EN) J Eur Acad Dermatol Venereol. 2020;34(9):1957–1971. doi: 10.1111/jdv.16339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lalevée S, Contassot E, Ortonne N, Gaudin O, Ben Said B, Vocanson M, et al. Advances in understanding of the pathophysiology of epidermal necrolysis (Stevens-Johnson syndrome and toxic epidermal necrolysis) Ann Dermatol Venereol. 2020;147:475–81. doi: 10.1016/j.annder.2020.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Chaby G, Maldini C, Haddad C, Lebrun-Vignes B, Hemery F, Ingen-Housz-Oro S, et al. Incidence of and mortality from epidermal necrolysis (Stevens-Johnson syndrome/toxic epidermal necrolysis) in France during 2003–16: a four-source capture-recapture estimate. Br J Dermatol. 2020;182:618–624. doi: 10.1111/bjd.18424. [DOI] [PubMed] [Google Scholar]
- 7.Bettuzzi T, Penso L, de Prost N, Hemery F, Hua C, Colin A, et al. Trends in mortality rates for Stevens-Johnson syndrome and toxic epidermal necrolysis: experience of a single centre in France between 1997 and 2017. Br J Dermatol. 2020;182:247–248. doi: 10.1111/bjd.18360. [DOI] [PubMed] [Google Scholar]
- 8.Bastuji-Garin S, Fouchard N, Bertocchi M, Roujeau JC, Revuz J, Wolkenstein P. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis. J Invest Dermatol. 2000;115:149–153. doi: 10.1046/j.1523-1747.2000.00061.x. [DOI] [PubMed] [Google Scholar]
- 9.Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, et al. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013;133:1197–1204. doi: 10.1038/jid.2012.510. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Doval I, LeCleach L, Bocquet H, Otero XL, Roujeau JC. Toxic epidermal necrolysis and Stevens-Johnson syndrome: does early withdrawal of causative drugs decrease the risk of death? Arch Dermatol. 2000;136:323–327. doi: 10.1001/archderm.136.3.323. [DOI] [PubMed] [Google Scholar]
- 11.Traikia C, Hua C, Le Cleach L, de Prost N, Hemery F, Bettuzzi T, et al. Individual- and hospital-level factors associated with epidermal necrolysis mortality: a nationwide multilevel study, France, 2012–2016. Br J Dermatol. 2020;182:900–906. doi: 10.1111/bjd.18294. [DOI] [PubMed] [Google Scholar]
- 12.Creamer D, Walsh SA, Dziewulski P, Exton LS, Lee HY, Dart JKG, et al. U.K. guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults 2016. Br J Dermatol. 2016;174:1194–227. doi: 10.1111/bjd.14530. [DOI] [PubMed] [Google Scholar]
- 13.Ingen-Housz-Oro S, Duong TA, Bensaid B, Bellon N, de Prost N, Lu D, et al. Epidermal necrolysis French national diagnosis and care protocol (PNDS; protocole national de diagnostic et de soins) Orphanet J Rare Dis. 2018;13:56. doi: 10.1186/s13023-018-0793-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seminario-Vidal L, Kroshinsky D, Malachowski SJ, Sun J, Markova A, Beachkofsky TM, et al. Society of Dermatology Hospitalists supportive care guidelines for the management of Stevens-Johnson syndrome/toxic epidermal necrolysis in adults. J Am Acad Dermatol. 2020;82:1553–1567. doi: 10.1016/j.jaad.2020.02.066. [DOI] [PubMed] [Google Scholar]
- 15.Brüggen MC, Le ST, Walsh S, Toussi A, de Prost N, Ranki A, et al. Supportive care in the acute phase of Stevens-Johnson syndrome and toxic epidermal necrolysis: an international, multidisciplinary Delphi-based consensus. Br J Dermatol. 2021;185:616–626. doi: 10.1111/bjd.19893. [DOI] [PubMed] [Google Scholar]
- 16.Lee HY, Walsh SA, Creamer D. Long-term complications of Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN): the spectrum of chronic problems in patients who survive an episode of SJS/TEN necessitates multidisciplinary follow-up. Br J Dermatol. 2017;177:924–935. doi: 10.1111/bjd.15360. [DOI] [PubMed] [Google Scholar]
- 17.Ingen-Housz-Oro S, Alves A, Colin A, Ouedraogo R, Layese R, Canoui-Poitrine F, et al. Health-related quality of life and long-term sequelae in survivors of epidermal necrolysis: an observational study of 57 patients. Br J Dermatol. 2020;182:916–926. doi: 10.1111/bjd.18387. [DOI] [PubMed] [Google Scholar]
- 18.Hajj C, Ezzedine K, Thorel D, Delcampe A, Royer G, Hua C, et al. Disabling ocular sequelae of epidermal necrolysis: risk factors during the acute phase and associated sequelae. Br J Dermatol. 2019;181:421–422. doi: 10.1111/bjd.18023. [DOI] [PubMed] [Google Scholar]
- 19.Hefez L, Zaghbib K, Sbidian E, Valeyrie-Allanore L, Allain M, Duong TA, et al. Post-traumatic stress disorder in Stevens-Johnson syndrome and toxic epidermal necrolysis: prevalence and risk factors. A prospective study of 31 patients. Br J Dermatol. 2019;180:1206–13. doi: 10.1111/bjd.17267. [DOI] [PubMed] [Google Scholar]
- 20.Dodiuk-Gad RP, Olteanu C, Feinstein A, Hashimoto R, Alhusayen R, Whyte-Croasdaile S, et al. Major psychological complications and decreased health-related quality of life among survivors of Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2016;175:422–424. doi: 10.1111/bjd.14799. [DOI] [PubMed] [Google Scholar]
- 21.Yang CW, Cho YT, Chen KL, Chen YC, Song HL, Chu CY. Long-term sequelae of Stevens-Johnson syndrome/toxic epidermal necrolysis. Acta Derm Venereol. 2016;96:525–529. doi: 10.2340/00015555-2295. [DOI] [PubMed] [Google Scholar]
- 22.Fitch K, Bernstein S, Aguilar MD, Burnand B, LaCalle JR, Lazaro P, van het Loo M, McDonnell J, Vader JP, Kahan JP. The RAND/UCLA appropriateness method user's manual. Santa Monica: RAND Corporation; 2001. [Google Scholar]
- 23.Isvy-Joubert A, Ingen-Housz-Oro S, Vincent R, Haddad C, Valeyrie-Allanore L, Chosidow O, et al. Severe cutaneous adverse reactions to drugs: from patients to the national office for compensation of medical accidents. Dermatology (Basel) 2014;228:338–343. doi: 10.1159/000358295. [DOI] [PubMed] [Google Scholar]
- 24.Lian SB, Oh CC, Yeo YW, Lee HY. Spectrum of nail sequelae in Stevens-Johnson syndrome and toxic epidermal necrolysis. JAMA Dermatol. 2021;157:117–119. doi: 10.1001/jamadermatol.2020.4664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Habre M, Ortonne N, Colin A, Meningaud JP, Chosidow O, Wolkenstein P, et al. Facial scars following toxic epidermal necrolysis: role of adnexal involvement? Dermatology (Basel) 2016;232:220–223. doi: 10.1159/000443164. [DOI] [PubMed] [Google Scholar]
- 26.Lefaucheur JP, Valeyrie-Allanore L, Ng Wing Tin S, Abgrall G, Colin A, Hajj C, et al. Chronic pain: a long-term sequela of epidermal necrolysis (Stevens-Johnson syndrome/toxic epidermal necrolysis) - prevalence, clinical characteristics and risk factors. J Eur Acad Dermatol Venereol. 2021;35:188–94. doi: 10.1111/jdv.16891. [DOI] [PubMed] [Google Scholar]
- 27.Gaultier F, Rochefort J, Landru MM, Allanore L, Naveau A, Roujeau JC, et al. Severe and unrecognized dental abnormalities after drug-induced epidermal necrolysis. Arch Dermatol. 2009;145:1332–1333. doi: 10.1001/archdermatol.2009.233. [DOI] [PubMed] [Google Scholar]
- 28.Villa A, Connell CL, Abati S. Diagnosis and management of xerostomia and hyposalivation. Ther Clin Risk Manag. 2015;11:45–51. doi: 10.2147/TCRM.S76282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gueudry J, Roujeau JC, Binaghi M, Soubrane G, Muraine M. Risk factors for the development of ocular complications of Stevens-Johnson syndrome and toxic epidermal necrolysis. Arch Dermatol. 2009;145:157–162. doi: 10.1001/archdermatol.2009.540. [DOI] [PubMed] [Google Scholar]
- 30.Prabhasawat P, Tesavibul N, Karnchanachetanee C, Kasemson S. Efficacy of cyclosporine 0.05% eye drops in Stevens Johnson syndrome with chronic dry eye. J Ocul Pharmacol Ther. 2013;29:372–7. doi: 10.1089/jop.2012.0009. [DOI] [PubMed] [Google Scholar]
- 31.Wan KH, Chen LJ, Young AL. Efficacy and safety of topical 0.05% cyclosporine eye drops in the treatment of dry eye syndrome: a systematic review and meta-analysis. Ocul Surf. 2015;13:213–25. doi: 10.1016/j.jtos.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 32.Lee YJ, Kim SW, Seo KY. Application for tacrolimus ointment in treating refractory inflammatory ocular surface diseases. Am J Ophthalmol. 2013;155:804–813. doi: 10.1016/j.ajo.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 33.Sotozono C, Ueta M, Yokoi N. Severe dry eye with combined mechanisms is involved in the ocular sequelae of SJS/TEN at the chronic stage. Invest Ophthalmol Vis Sci. 2018;59:DES80–6. doi: 10.1167/iovs.18-24019. [DOI] [PubMed] [Google Scholar]
- 34.Tougeron-Brousseau B, Delcampe A, Gueudry J, Vera L, Doan S, Hoang-Xuan T, et al. Vision-related function after scleral lens fitting in ocular complications of Stevens-Johnson syndrome and toxic epidermal necrolysis. Am J Ophthalmol. 2009;148:852–859.e2. doi: 10.1016/j.ajo.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Sotozono C, Yamauchi N, Maeda S, Kinoshita S. Tear exchangeable limbal rigid contact lens for ocular sequelae resulting from Stevens-Johnson syndrome or toxic epidermal necrolysis. Am J Ophthalmol. 2014;158:983–993. doi: 10.1016/j.ajo.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 36.Tugal-Tutkun I, Akova YA, Foster CS. Penetrating keratoplasty in cicatrizing conjunctival diseases. Ophthalmology. 1995;102:576–585. doi: 10.1016/S0161-6420(95)30980-3. [DOI] [PubMed] [Google Scholar]
- 37.Kaser DJ, Reichman DE, Laufer MR. Prevention of vulvovaginal sequelae in stevens-johnson syndrome and toxic epidermal necrolysis. Rev Obstet Gynecol. 2011;4:81–85. [PMC free article] [PubMed] [Google Scholar]
- 38.Holtz M, Grimstad F, Higgins J, Denny G, Strickland J, Dowlut-McElroy T. Vulvovaginal involvement in pediatric Stevens-Johnson syndrome: a case series. J Pediatr Adolesc Gynecol. 2021;34:745–748. doi: 10.1016/j.jpag.2021.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van Batavia JP, Chu DI, Long CJ, Jen M, Canning DA, Weiss DA. Genitourinary involvement and management in children with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Pediatr Urol. 2017;13:490.e1–490.e7. doi: 10.1016/j.jpurol.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 40.Boyraz G, Basaran D, Salman MC, Ozgul N, Yuce K. Vaginal reconstruction for vaginal obliteration secondary to stevens johnson syndrome: a case report and review of literature. Oman Med J. 2017;32:436–439. doi: 10.5001/omj.2017.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 42.Harorani M, Davodabady F, Masmouei B, Barati N. The effect of progressive muscle relaxation on anxiety and sleep quality in burn patients: a randomized clinical trial. Burns. 2020;46:1107–1113. doi: 10.1016/j.burns.2019.11.021. [DOI] [PubMed] [Google Scholar]
- 43.Hornsby N, Blom L, Sengoelge M. Psychosocial interventions targeting recovery in child and adolescent burns: a systematic review. J Pediatr Psychol. 2020;45:15–33. doi: 10.1093/jpepsy/jsz087. [DOI] [PubMed] [Google Scholar]
- 44.Duong TA, de Prost N, Ingen-Housz-Oro S, Carrié AS, Zerah F, Valeyrie-Allanore L, et al. Stevens-Johnson syndrome and toxic epidermal necrolysis: follow-up of pulmonary function after remission. Br J Dermatol. 2015;172:400–405. doi: 10.1111/bjd.13505. [DOI] [PubMed] [Google Scholar]
- 45.Seccombe EL, Ardern-Jones M, Walker W, Austin S, Taibjee S, Williams S, et al. Bronchiolitis obliterans as a long-term sequela of Stevens-Johnson syndrome and toxic epidermal necrolysis in children. Clin Exp Dermatol. 2019;44:897–902. doi: 10.1111/ced.13969. [DOI] [PubMed] [Google Scholar]
- 46.Wolkenstein P, Chosidow O, Fléchet ML, Robbiola O, Paul M, Dumé L, et al. Patch testing in severe cutaneous adverse drug reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. Contact Derm. 1996;35:234–236. doi: 10.1111/j.1600-0536.1996.tb02364.x. [DOI] [PubMed] [Google Scholar]
- 47.Barbaud A, Collet E, Milpied B, Assier H, Staumont D, Avenel-Audran M, et al. A multicentre study to determine the value and safety of drug patch tests for the three main classes of severe cutaneous adverse drug reactions. Br J Dermatol. 2013;168:555–562. doi: 10.1111/bjd.12125. [DOI] [PubMed] [Google Scholar]
- 48.Lin YT, Chang YC, Hui RCY, Yang CH, Ho HC, Hung SI, et al. A patch testing and cross-sensitivity study of carbamazepine-induced severe cutaneous adverse drug reactions. J Eur Acad Dermatol Venereol. 2013;27:356–364. doi: 10.1111/j.1468-3083.2011.04418.x. [DOI] [PubMed] [Google Scholar]
- 49.Barbaud A, Collet E, Milpied B, Assier H, Staumont D, Avenel-Audran M, et al. A multicentre study to determine the value and safety of drug patch tests for the three main classes of severe cutaneous adverse drug reactions. Br J Dermatol. 2013;168:555–562. doi: 10.1111/bjd.12125. [DOI] [PubMed] [Google Scholar]
- 50.Kano Y, Hirahara K, Mitsuyama Y, Takahashi R, Shiohara T. Utility of the lymphocyte transformation test in the diagnosis of drug sensitivity: dependence on its timing and the type of drug eruption. Allergy. 2007;62:1439–1444. doi: 10.1111/j.1398-9995.2007.01553.x. [DOI] [PubMed] [Google Scholar]
- 51.Phillips EJ, Bigliardi P, Bircher AJ, Broyles A, Chang YS, Chung WH, et al. Controversies in drug allergy: testing for delayed reactions. J Allergy Clin Immunol. 2019;143:66–73. doi: 10.1016/j.jaci.2018.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barbaud A, Castagna J, Soria A. Skin tests in the work-up of cutaneous adverse drug reactions: a review and update. Contact Dermat. 2022;86:344–356. doi: 10.1111/cod.14063. [DOI] [PubMed] [Google Scholar]
- 53.Bergmann MM, Caubet JC. Role of in vivo and in vitro tests in the Diagnosis of severe cutaneous adverse reactions (SCAR) to drug. Curr Pharm Des. 2019;25:3872–3880. doi: 10.2174/1381612825666191107104126. [DOI] [PubMed] [Google Scholar]
- 54.Bellón T, Rodríguez-Martín S, Cabañas R, Ramírez E, Lerma V, González-Herrada C, et al. Assessment of drug causality in Stevens-Johnson syndrome/toxic epidermal necrolysis: concordance between lymphocyte transformation test and ALDEN. Allergy. 2020;75:956–959. doi: 10.1111/all.14062. [DOI] [PubMed] [Google Scholar]
- 55.Kumkamthornkul P, Udnaen S, Tansit T, Tuchinda P, Srinoulprasert Y. Evaluation of a lymphocyte transformation test and cytokine detection assay to identify phenytoin and carbamazepine provoked DRESS or SJS/TEN in epilepsy patients. Int Immunopharmacol. 2018;63:204–210. doi: 10.1016/j.intimp.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 56.Trubiano JA, Strautins K, Redwood AJ, Pavlos R, Konvinse KC, Aung AK, et al. The combined utility of ex vivo IFN-γ release enzyme-linked immunospot assay and in vivo skin testing in patients with antibiotic-associated severe cutaneous adverse reactions. J Allergy Clin Immunol Pract. 2018;6:1287–1296.e1. doi: 10.1016/j.jaip.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Table S1. Disagreement index (DI), interpercentile range (IPR) and interpercentile range adjusted for symmetry (IPRAS) for all statements.
Data Availability Statement
The dataset(s) supporting the conclusions of this article is(are) included within the article (and its additional file(s)).