Governments grapple with the difficult question of how to efficiently ration healthcare goods and services in public health insurance programs. Many programs use demand-side cost-sharing mechanisms to limit overuse due to moral hazard. However, such mechanisms have the undesirable property that in order to limit moral hazard, consumers must necessarily be exposed to greater financial risk (Zeckhauser, 1970). Furthermore, cost-sharing not only reduces use of low-value services but also high-value services, implying that consumers self-ration inefficiently when faced with cost-sharing (Baicker, Mullainathan and Schwartzstein, 2015; Brot-Goldberg et al., 2017). Finally, cost-sharing is typically deemed inappropriate in programs targeted to low-income households who may not have sufficient cash to pay copayments or deductibles (Gross, Layton and Prinz, 2021).
The problems with demand-side cost-sharing have led policymakers to employ alternative methods for rationing healthcare goods and services. This is especially true across the U.S. Medicaid program, which provides health insurance coverage to low-income and disabled Americans. Because Medicaid beneficiaries lack the financial means to pay even a small share of their healthcare costs, state Medicaid programs have sought other ways of rationing healthcare services. In this paper, we study two mechanisms that are popular among state Medicaid programs: caps on prescription drug use and the contracting out of medical services to private managed care plans.
Quantity limits on prescription drugs are ubiquitous in Medicaid (Council of State Governments Midwest, 2013). The number of states imposing some form of prescription drug quantity limit in their Medicaid programs increased from 12 in 2001 to 20 in 2010 (Lieberman et al., 2016). The caps vary in terms of which beneficiaries and which drugs they apply to, but they are often quite strict, with the most restrictive caps limiting beneficiaries to three prescription fills per month. Despite states’ heavy reliance on drug limits, we know little about their effects, including the extent to which they are binding, the types of drugs beneficiaries forego in response to the cap, and the extent to which the marginal drugs would “offset” spending on other types of care (Chandra, Gruber and McKnight, 2010).
The use of managed care plans is also commonplace in Medicaid, with over 80% of Medicaid beneficiaries receiving some or all of their benefits through a private managed care plan as of 2012 (Congressional Budget Office, 2018). These plans receive fixed monthly payments and bear (almost) full responsibility for healthcare costs incurred by their enrollees. They are thus incentivized to ration access to care using the tools allowed by the state, including limited provider networks, gate-keeping, prior authorization requirements, and aggressive case management, while maintaining quality in order to attract enrollees and ensure they receive future contracts from the state Medicaid program. While managed care in Medicaid has been studied previously (Lewin Group, 2004; Aizer, Currie and Moretti, 2007; Duggan and Hayford, 2013; Van Parys, 2015; Vabson, 2017; Kuziemko, Meckel and Rossin-Slater, 2018), findings have been mixed, most work has focused on largely healthy populations, and there has typically been little ability to investigate the mechanisms behind any observed effects.
To study these two rationing devices, we leverage a large reform to the Medicaid program in Texas. In February 2007, the state transitioned adults with disabilities—most of whom qualified for Medicaid due to their enrollment in the federal Supplemental Security Income (SSI) program—from the state-run public insurance plan to a program called STAR+Plus. Under the program, disabled Medicaid beneficiaries were enrolled in private Medicaid managed care (MMC) plans which were responsible for all non-inpatient, non-drug spending for these beneficiaries. Additionally, beneficiaries enrolled in the STAR+Plus program were exempted from a highly restrictive drug cap enforced in the public fee-for-service Medicaid program. Outside of the STAR+Plus program, beneficiaries could fill only three prescriptions per month. This limit applied to all adult Medicaid beneficiaries, including adults with disabilities, and included all drugs except for contraceptives. When these beneficiaries moved to STAR+Plus, they were no longer subject to any limit on the number of prescription drug fills. The transition to STAR+Plus was mandatory and abrupt; enrollment among adults with disabilities rose from around 10% to almost 80% instantaneously. Moreover, Texas implemented this coverage change in only a subset of counties, providing a clean natural experiment that we exploit in a difference-in-differences design.
We use this reform to estimate the effects of these two rationing devices (managed care and drug caps) on healthcare utilization, surrogate health outcomes (e.g., avoidable hospitalizations), and state fiscal spending. We first quantify the overall effects of the reform, and then we attempt to unpack and separate the effects of the drug cap’s removal and the transition to managed care. Overall, we find the reform significantly relaxed rationing of healthcare goods and services in Texas’s Medicaid program. Specifically, prescription drug spending increased by 30% and outpatient spending increased by almost 32% in the four years following the reform. We then show that the weakened rationing of drugs and non-inpatient services led to a significant reduction (i.e. an “offset”) in inpatient utilization. Specifically, inpatient spending decreased by 11%. On net, total fiscal spending increased by 26%. Complementary analyses of the effects of the reform on other outcomes such as mortality, employment, and exit from the SSI program are suggestive of corresponding improvements in health and functional capacity, although these effects are not statistically significant.
We then focus attention on the component of the reform related to the relaxation of the drug cap. We first provide evidence that it was the relaxation of the drug cap that led to the increase in drug utilization, and not the shift to managed care. Specifically, we show that nearly all of the increase in drug utilization was due to an increase in the probability of filling four or more prescriptions in a month, with little effect on the probability of filling one, two, or three prescriptions in a month. Thus, the drug cap was binding for many beneficiaries affected by the reform. Second, we show that the cap did not merely ration access to low-value drugs but instead it prevented disabled Medicaid beneficiaries from taking high-value drugs used to treat common chronic conditions. For example, we find strong extensive margin responses to the removal of the drug cap for anti-diabetic drugs, anti-psychotics, anti-depressants, and statins, as well as drugs used to treat asthma and pain. Third, we provide suggestive evidence that the increase in drug utilization induced by the relaxation of the cap was responsible for the decrease in inpatient spending under the reform. To do this, we first show that the groups that experienced the largest increases in drug utilization also had the largest reductions in inpatient spending. We then show that the drugs with the largest increases in utilization tended to treat the conditions with the largest concurrent decreases in inpatient admissions (i.e. mental illness and diabetes). Furthermore, because the subcategories of inpatient spending accounting for the overall reduction in inpatient spending are typically considered “avoidable” with appropriate treatment, we argue that the relaxation of the drug cap led to improvements in the health and quality of life of Medicaid beneficiaries. Lastly, we show that only around 16% of the total increase in fiscal spending can be attributed to the relaxation of the drug cap.
We then shift attention to the component of the reform that mandated enrollment in private managed care plans, which were responsible for non-inpatient, non-drug medical benefits. We find the reform led not only to an increase in spending on non-inpatient services but also to an increase in the quantity of services. In addition, managed care plans paid higher prices to providers for a given service. Together, these results suggest the supply curve for non-inpatient services in Medicaid is upward-sloping, consistent with previous evidence from Medicaid (Chen, 2017; Alexander and Schnell, 2019) and Medicare (Clemens and Gottlieb, 2014), and that private plans relax rationing of access to care by paying providers higher rates for the same services. Lastly, we show that the shifting of non-inpatient services to managed care was responsible for much (84%) of the fiscal cost of the reform. Specifically, capitation payments to managed care plans exceeded counterfactual fee-for-service spending on non-inpatient services by 39%. That said, we find that the marginal dollars mostly went to patients and/or providers in the form of higher spending on non-inpatient services, not to managed care plan profits.
In summary, our results suggest that (1) the relaxation of the drug cap led to an increase in drug utilization, a reduction in inpatient stays, and improvements in patient health, while on net accounting for only a small increase in fiscal costs, while (2) the shifting of non-inpatient services to managed care generated increased access to outpatient services but also accounted for much of the cost of the reform. This suggests that relaxing quantity-based limits on prescription drug consumption can provide large benefits for beneficiaries at limited fiscal cost while shifting non-inpatient services to managed care plans can also provide beneficiaries with benefits, though at a high fiscal cost.
Our findings make an important contribution to the literature on rationing in healthcare. This literature has largely focused on the demand side (e.g., Chandra, Gruber and McKnight, 2010; Brot-Goldberg et al., 2017), with much less work examining supply side tools. This is an important gap in the literature: when covering low-income populations, including Medicaid beneficiaries, insurers need to largely rely on supply-side tools. We show that rationing prescription drugs via arbitrary quantity limits is an effective way to restrain spending. However, the spending reduction comes at a cost: worse health for beneficiaries and increased inpatient stays, though the corresponding spending increases are not enough to fully offset the decrease in spending on drugs. Our results thus suggest that these types of quantity limits are characterized by the standard trade-off between cost and quality.
Our findings also contribute to the literature on private vs. public provision of social health insurance benefits. Previous work on Medicaid privatization (Lewin Group, 2004; Aizer, Currie and Moretti, 2007; Sparer, 2012; Duggan and Hayford, 2013; Van Parys, 2015; Vabson, 2017; Kuziemko, Meckel and Rossin-Slater, 2018) has reached mixed and inconclusive findings on private provision’s effects, largely focusing on generally healthy populations. The broader literature on private provision is equally mixed: Some papers find increased efficiency under privatization (Newhouse and McGuire, 2014; Einav, Finkelstein and Polyakova, 2018; Curto et al., 2019; Dranove, Ody and Starc, 2021), while others find limited pass-through of efficiency gains to the government and beneficiaries because of incomplete contracting and imperfect competition (Duggan, Starc and Vabson, 2016; Cabral, Geruso and Mahoney, 2018; Starc and Town, 2020; Curto et al., 2021). Our results, along with contemporaneous work by Duggan, Garthwaite and Wang (2021), provide new evidence of the consequences of private provision for a population with severe health problems (adults with disabilities), with the results suggesting a more nuanced view of the consequences of private provision. Our results do not suggest that private provision is obviously welfare-improving or welfare-decreasing. Instead, we find that private provision of non-inpatient medical benefits in Texas weakened rationing of medical services while leading to increased spending, again implying the classic trade-off between cost and quality. We are also able to unpack the mechanisms behind these results, with suggestive evidence that higher provider prices under private plans are a driving factor. Finally, our paper illustrates that transitions to private provision differ on many dimensions, including in terms of the constraints they relax and the types of services that are included or excluded in the private contracts. As highlighted by our paper and by Duggan, Garthwaite and Wang (2021), variation across these dimensions can account for differences in the estimated effects of private provision and must be understood to fully characterize the mechanisms behind those effects.
I. Background
Rationing in Public and Private Medicaid. —
Unlike most health insurance programs, Medicaid does not employ demand-side cost sharing as a tool for reducing healthcare utilization. There is no deductible, no coinsurance, and typically no copayments for services or drugs.1 Despite this, Medicaid is widely perceived to be a relatively low-cost form of health insurance coverage (Kaiser Family Foundation, 2016). How can this be?
Medicaid instead employs non-cost-sharing tools for rationing access to healthcare. With respect to medical services, Medicaid’s primary rationing tool is the level of the fees it pays to providers of healthcare services. Most state Medicaid programs pay notoriously low fees to providers, with only two states (Alaska and Montana) paying more than Medicare and over 30 states paying less than 80% of Medicare fees (Kaiser Family Foundation, 2018). Low prices directly reduce Medicaid spending. They also indirectly reduce spending by lowering the supply of care—fewer providers are willing to treat Medicaid patients compared to those with other forms of coverage, and even participating Medicaid providers may treat Medicaid patients less intensively than others (Medicaid and CHIP Payment and Access Commission, 2019). A simple economic model would suggest that, conditional on consumers facing zero prices, lower provider prices would lead to supply “shortages” in places where consumers demand more care than what is available at the price paid by the Medicaid program. As a consequence, state Medicaid programs effectively outsource the rationing of healthcare services to providers, who must choose which (if any) of the many Medicaid enrollees demanding their services they will treat. Providers appear to be responsive to Medicaid payments on various margins, including appointment availability (Polsky et al., 2015), waiting times (Oostrom, Einav and Finkelstein, 2017), and other measures of access (Chen, 2017; Alexander and Schnell, 2019). Low fees may also cause providers to offer lower-quality care (Hackmann, 2019). Texas pays particularly low fees, ranked 37th among states in terms of how their Medicaid fees compare to Medicare fees (Kaiser Family Foundation, 2018).
With respect to prescription drugs, Medicaid has even fewer rationing tools available. The prices paid by Medicaid programs for drugs are generally determined by external formulas (see Alpert, Duggan and Hellerstein, 2013, for a comprehensive review). Thus, in order to limit utilization of prescription drugs, states have opted for a more draconian and ad hoc (but legal) tool: quantity limits. The number of states imposing some form of prescription drug cap in their Medicaid programs increased from 12 in 2001 to 20 in 2010 (Lieberman et al., 2016). The caps vary in their scope, from general ones that apply to nearly all drugs and nearly all populations to highly targeted caps that do not apply to sicker populations, to generic drugs, or to drugs used to treat chronic conditions such as AIDS or diabetes (Council of State Governments Midwest, 2013). They also vary in their stringency, from strict caps of as low as 3 prescription fills up to relatively generous caps of as many as 8 fills, with the modal cap being 4 fills. Texas imposes a particularly restrictive cap of 3 drug fills per person per month, which applies to nearly all Medicaid enrollees, including enrollees with multiple chronic conditions.
An alternative cost-containment method for state Medicaid programs is to outsource rationing of healthcare services to private health plans. Under private provision (also known as Medicaid managed care, or MMC), states pay private health plans fixed per-person, per-month fees to provide all or some of the healthcare services covered by the Medicaid program. Private plans can then impose their own rationing tools, some of which are not available to the public program. On the medical side, private plans can construct customized provider networks that can include providers participating in the public program as well as providers not accepting public Medicaid. Private plans can independently negotiate payment rates with these providers and sometimes impose additional prior authorization requirements on certain services or on certain higher-cost doctors. In addition, private plans often use care managers to ensure that patients get needed treatment in order to prevent potentially costly complications or hospitalizations. For both medical services and prescription drugs, private plans are able to pass financial risk on to providers, rewarding providers who limit spending (via fewer referrals to specialists and lower utilization of tests, labs, etc.) and penalizing providers whose patients’ spending levels are unreasonably high. The greater availability of these tools to private plans, combined with the sharper incentives private plans have for applying them, can potentially allow the plans to provide higher-quality care than the public program or to provide care of similar quality at a lower price, though whether they do so in practice is an empirical question.
STAR+Plus Program. —
Texas simultaneously (1) transitioned a subset of adults with disabilities out of their publicly managed fee-for-service Medicaid program and into private Medicaid managed care plans and (2) relaxed a strict prescription drug cap during the mid-to late-2000s. Texas’s Medicaid program is divided into ten service areas, shown in the top panel of Online Appendix Figure A1. Nine service areas are marked by colors, while the 10th service area comprises much of the state and is shown in white. Starting in February 2007, four of those service areas (Bexar, Harris, Nueces, and Travis), all large urban areas of the state, required that all disabled Medicaid beneficiaries over the age of 21 and not dually enrolled in Medicare enroll in a private Medicaid managed care plan as part of the STAR+Plus program.2,3 Nearly all of these individuals were SSI beneficiaries. We refer to this group of individuals as “adults with disabilities” for the remainder of the paper. Online Appendix B provides further background on Medicaid and the SSI program.
Prior to February 2007, the vast majority of adults with disabilities in Texas were enrolled in the traditional fee-for-service public Medicaid program, under which the state directly reimbursed physicians for healthcare services using the state’s fee-for-service price schedule.4 Starting in February 2007, enrollment in STAR+Plus became mandatory for all adults with disabilities in the four affected service areas. Adults with disabilities outside these service areas remained in the public Medicaid program. Enrollment in STAR+Plus consisted of two key changes for beneficiaries. First, beneficiaries were enrolled in private MMC plans. Like many state Medicaid managed care programs at the time, Texas excluded (“carved out”) some services from its contracts with private MMC plans. Specifically, Texas carved out prescription drug and inpatient services, continuing to pay for these services on a fee-for-service basis through the public program even for beneficiaries enrolled in a private plan. These plans were paid a fixed monthly premium or capitation payment for each individual they enrolled and were financially responsible for the non-inpatient, non-drug healthcare spending of their enrollees, keeping any savings and absorbing any losses generated by healthcare spending exceeding their payments from the state.5 The state, rather than the private plan, served as the residual claimant on all drug and inpatient spending, and private plans had limited incentive to restrain spending on these services. Second, Texas lifted a restrictive three prescription per-person, per-month cap for all beneficiaries enrolled in the STAR+Plus program,6 allowing unrestricted filling of prescriptions for beneficiaries enrolled in STAR+Plus (leaving the cap in place for anyone not enrolled in the program).7,8
II. Data and Sample
We use several administrative datasets from the Centers for Medicare and Medicaid Services (CMS) for the state of Texas for 2004–2010. These datasets contain information on Medicaid enrollment status as well as healthcare utilization in the inpatient, emergency department, outpatient, and prescription drug settings. Uniquely, the data allow for construction of an individual-level panel of utilization, which covers everyone in public as well as private Medicaid plans, including those switching between the two. Importantly, inclusion in these data is not conditional on utilization of healthcare.
Using these data, we can precisely identify the cohorts of interest in our analyses. Specifically, we restrict our analysis samples to Texas residents who were enrolled in Medicaid in a given month during 2004–2010, who qualified for the program on the basis of disability, and who were not simultaneously enrolled in Medicare. Finally, we restrict our main analyses to individuals over 21, because private Medicaid plan enrollment always remained optional in Texas for those under 21. We also drop beneficiaries who ever moved between counties (5.2% of the sample).
Beneficiary Characteristics and Enrollment Information. —
We obtain information on beneficiary characteristics and enrollment status from the CMS Medicaid Analytic eXtract (MAX) Personal Summary (PS) files, which contain person-month-level enrollment status in Medicaid. For individuals enrolled in Medicaid, these files identify whether their Medicaid coverage in a given month comes through public or private Medicaid plans. These files also identify the basis for each beneficiary’s eligibility for Medicaid, such as through qualification for SSI, Temporary Assistance for Needy Families, or other eligibility pathways. Finally, the data also track specific plan of enrollment, for those in private plans.
Inpatient, Outpatient, and Prescription Drug Utilization Data. —
We track inpatient, outpatient, and prescription drug utilization using claims-level information from the MAX Inpatient (IP), Other Therapy (OT), and Prescription Drug (Rx) files. These data track claims paid by the public Medicaid program as well as those paid by private Medicaid managed care (MMC) plans. Previous work comparing outcomes under private and public plans has suffered from data quality issues arising from differential reporting of service use under the public and private programs. Our work does not face these issues for some categories of services, but does potentially suffer from reporting issues for other categories. We therefore describe data quality for each broad category of healthcare services (prescription drugs, inpatient care, non-inpatient medical services) in turn.
As discussed in Section I, prescription drugs and inpatient services in Texas are “carved-out” of private MMC plan contracts. This means that they are always paid by the public program both for beneficiaries enrolled in the public program and for beneficiaries enrolled in a private plan for their medical benefits. There is thus no change in the source of the prescription drug and inpatient claims data as beneficiaries shift from public to private plans, which means there is no concern about differential reporting affecting our estimates of the effects of the Texas reform with respect to prescription drugs and inpatient services. The prescription drug data include the prescription cost, the dates on which the prescription was written as well as filled, the days supply associated with the fill, and the drug identifier (NDC code), which we link to external data in order to group drugs by therapeutic class. Based on a drug’s therapeutic class, we are able to identify the types of conditions that it could be meant to treat. The inpatient utilization data record the date of each hospital visit, as well as the type of hospitalization, length of hospital stay, set of procedures performed, and total visit costs. Using this information, it is possible to classify hospitalizations into various relevant categories, including elective, emergency, and surgical admissions.
Unlike for inpatient services and prescription drugs, for outpatient services differential reporting could potentially be a concern. While outpatient data for Medicaid beneficiaries enrolled in public plans comes from fee-for-service claims paid directly by the state, outpatient data for private Medicaid beneficiaries comes from claims paid by the private plans themselves, which the plans then report to the state. A specific concern is under-reporting of visits by private plans (Lewin Group, 2012). This concern is less applicable to our setting because private plans had already provided coverage to other Medicaid populations for many years, allowing time for issues with data reporting to have been worked out. Concerns are also mitigated by our finding of generally higher outpatient utilization under private Medicaid plans, since under-counting of private plan visits would bias against a finding of a positive effect. This suggests that if there is a reporting issue, our estimates of outpatient utilization increases are a lower bound for the true effect of private provision. However, the possibility for differential reporting does make it difficult to differentiate between short-term (negative) disruption effects of the shift to private plans and changes in reporting. That said, while the outpatient claims data appear to be of sufficiently high-quality to allow for analyses of changes in aggregate outpatient utilization (spending and number of days with an outpatient claim), inconsistencies appear as outpatient utilization is broken down into finer categories of services. Specifically, it appears that private plans and public plans code specific outpatient services differently, making disaggregation of the effects of the Texas reform on outpatient utilization infeasible. Dissaggregation of the effects of private provision on inpatient and prescription drug utilization, however, is completely feasible due to the consistent source of the data across the public vs. private divide.
The outpatient data includes information on actual cost amounts for both the public and the private programs. Specifically, the data contains the negotiated amounts actually paid to providers by the public or private plans at the claim-line level. These actual provider payment amounts are available for all public Medicaid claims, as well as for about 80% of all private Medicaid plan claims. For the 20% of private plan claims missing cost information, we are able to impute this information, based on median observed private Medicaid rates for a given procedure. After imputation, we observe payments for 99.6% of private Medicaid claims.9
In addition to measuring each type of healthcare spending on its own, we also construct a measure of total healthcare spending. This measure is equal to the sum of outpatient, inpatient, and prescription drug spending.10
Government Expenditure Metrics. —
We construct beneficiary-level measures of government (state + federal) Medicaid expenditures using information contained in the CMS MAX files. We define government fiscal spending as the sum of any spending on healthcare services paid directly by the government and any premium payments paid by the government to private Medicaid plans. Spending on healthcare services paid directly by the government consists of spending on all services for beneficiaries enrolled in the public Medicaid plan and carved-out services for beneficiaries enrolled in private Medicaid plans. This spending is observed directly in the fee-for-service claims appearing in the inpatient, outpatient, and prescription drug files. Monthly premium payments paid by the government to private Medicaid plans are also directly observed in the MAX files for beneficiaries enrolled in private plans. We measure total government spending as the sum of these two forms of spending.11
III. Empirical Framework
Control and Treatment Counties. —
To study the effects of the STAR+Plus program (relaxation of drug cap + private provision of non-inpatient/non-drug services) for adults with disabilities, we leverage the introduction of the program to four of the ten Medicaid service areas in Texas (Bexar, Harris, Nueces, and Travis) starting in February 2007. Disabled beneficiaries residing in other service areas saw no change to the design of the program throughout the study period. We thus use a difference-in-differences strategy to estimate the effects of the reform.
Treatment (red) and control (blue) counties are shown in Panel (a) of Figure 1. The set of treatment counties is defined as any county in the affected service areas that is contiguous to at least one county in an unaffected service area. The set of control counties is similarly defined as any county in the unaffected service areas that is contiguous to at least one county in an affected service area. Table 1 shows summary statistics for the contiguous control counties and the treatment counties, as well as the full set of non-treatment counties in the state. The summary statistics reveal that for many variables all three groups of counties look similar. For most variables, however, contiguous control counties are more similar to treatment counties than the full set of non-treatment counties. These differences are likely due to the fact that STAR+Plus was implemented in urban areas of the state, while the vast majority of Texas is sparsely populated and rural. By implementing the contiguity requirement, we restrict to relatively populated control counties, making the treatment and control groups more comparable.12 To further ensure comparable treatment and control groups, in Online Appendix D we provide additional results where we zoom in on zip codes on the service area borders, requiring that treatment and control zip codes be within 25 miles of each other.
Figure 1. : Counties and First Stage.
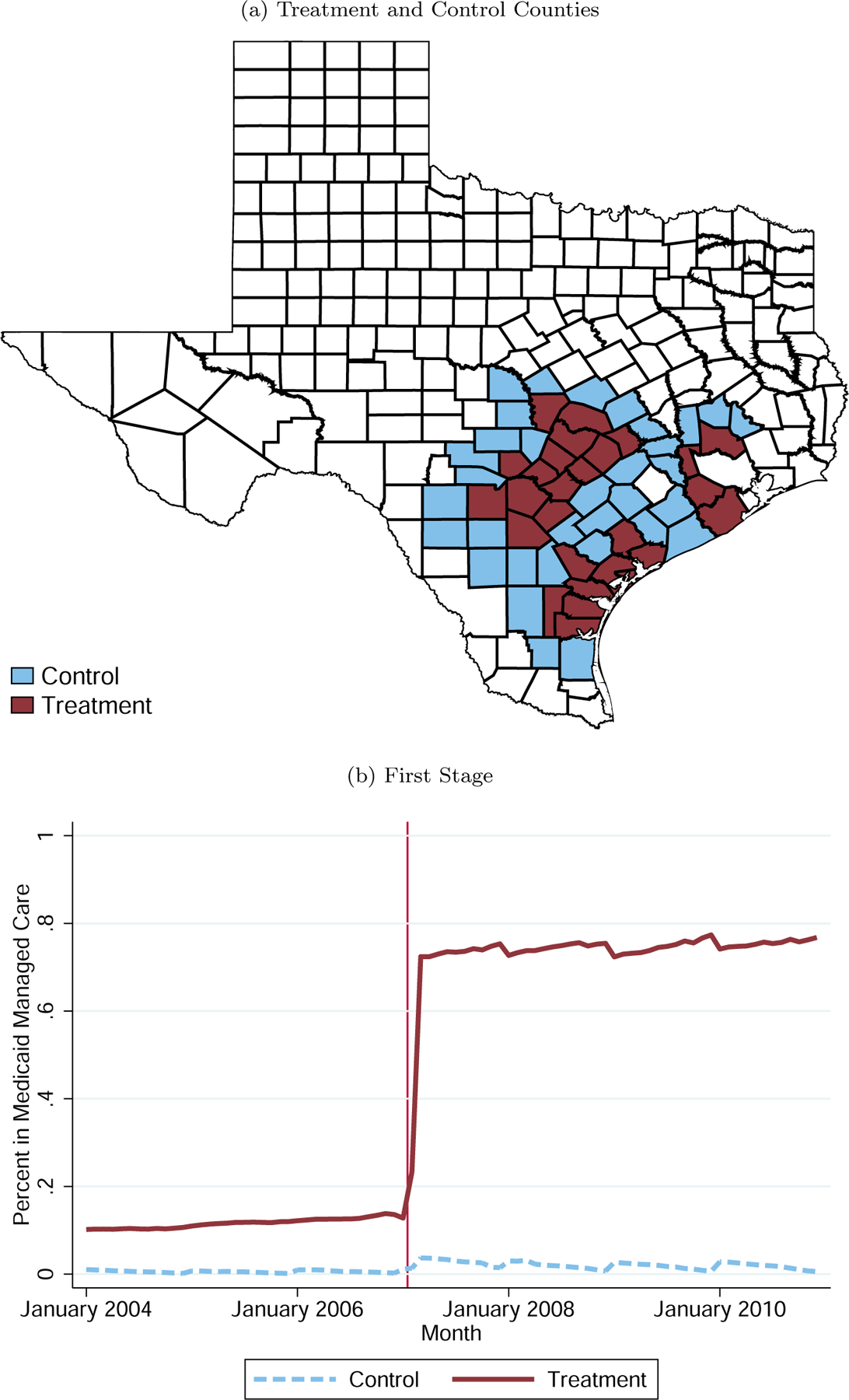
Note: Figure shows the counties that we include in our sample as treatment and control counties and Medicaid managed care enrollment in the two groups of counties. In both panels, control counties are in light blue and treatment counties are in dark red. In Panel (b), the red vertical line between January and February 2007 corresponds to the date of the introduction of the STAR+Plus Medicaid managed care program in the treatment counties. For more details, see Section III.
Table 1—:
Summary Statistics
| Contiguous Control | Treatment | Non-Contiguous Control | |
|---|---|---|---|
| Average quarterly healthcare spending 2004 | 2,683 | 2,851 | 2,906 |
| Average quarterly inpatient spending 2004 | 732 | 762 | 703 |
| Average quarterly outpatient spending 2004 | 1,375 | 1,467 | 1,592 |
| Average quarterly Rx spending 2004 | 576 | 622 | 611 |
| Age 20 to 24 | .091 | .104 | .096 |
| Age 25 to 29 | .077 | .085 | .077∗∗ |
| Age 30 to 34 | .078 | .081 | .073∗∗∗ |
| Age 35 to 39 | .082 | .088 | .079∗∗∗ |
| Age 40 to 44 | .101∗∗ | .111 | .103∗ |
| Age 45 to 49 | .129 | .128 | .121 |
| Age 50 to 54 | .142 | .136 | .140 |
| Age 55 to 59 | .164 | .146 | .164∗∗ |
| Age 60 to 64 | .137∗ | .121 | .148∗∗∗ |
| Female | .578 | .556 | .574 |
| Male | .422 | .444 | .426 |
| Heart Disease | .348∗ | .313 | .356∗∗ |
| Diabetes | .214∗∗ | .209 | .222 |
| HIV/AIDS | .009 | .015 | .011∗ |
| Cancer | .052 | .046 | .047 |
| Rheumatoid Arthritis | .036 | .034 | .042 |
| Obesity | .028 | .031 | .028 |
| Substance Use | .051∗∗∗ | .062 | .047∗∗∗ |
| Mental Illness | .210 | .235 | .197∗∗∗ |
| N recipients Jan 2004 | 7,401 | 30,510 | 76,210 |
| N recipients Dec 2010 | 9,206 | 42,210 | 106,562 |
| N pre-period recipient months | 289,353 | 1,202,845 | 2,976,227 |
| N post-period recipient months | 405,188 | 1,824,141 | 4,594,026 |
Note: Table shows summary statistics for control and treatment counties. In our analysis, control counties are counties where Medicaid managed care was not expanded that are contiguous with at least one county where Medicaid managed care was expanded. However, here we also show summary statistics for all counties in Texas where Medicaid managed care was not expanded. The significance stars show whether the control-treatment difference is statistically significant: ∗ p < 0.1, ∗∗ p < 0.05, ∗∗∗ p < 0.01. For more details, see Section III.
In addition to the contiguity restriction, we divide control counties into four groups, matching the four service areas where STAR+Plus was implemented. These groups are illustrated in the bottom panel of Online Appendix Figure A1. We use these groups to construct a set of indicators we refer to as “service area grouping”-by-quarter fixed effects. For each service area, the indicator is equal to one if the individual resides in either a treatment county or a control county assigned to that service area grouping, as illustrated in the bottom panel of Online Appendix Figure A1. We include these fixed effects in all regressions to control for any local shocks in healthcare utilization. The inclusion of these fixed effects effectively ensures that a particular treatment county is compared only to control counties that are contiguous to counties in the treatment county’s service area.
Panel (b) of Figure 1 shows the portion of disabled Medicaid beneficiaries in our sample who enrolled in a private managed care plan for the non-inpatient, non-drug portion of their Medicaid benefits in treatment and control counties in Texas for each month between January 2004 and December 2010. STAR+Plus was introduced in the treatment counties in February 2007. It is clear that the switch from the public program to private plans was swift and sharp. Recall that the relaxation of the drug cap was linked to enrollment in a private plan, implying that this relaxation was also swift and sharp. Effectively overnight, the portion of disabled Medicaid beneficiaries enrolled in a private Medicaid plan (and no longer subject to the drug cap) in treatment counties went from around 10% to almost 80%.13 This sharp variation in enrollment in private managed care plans is the variation we exploit to identify the effects of the program.14
Regression Framework. —
Because take-up is incomplete, we present reduced form estimates as well as instrumental variable (IV) estimates. Our reduced form specification is a difference-in-differences specification in event-study form:
| (1) |
where Yit is the outcome of interest, Treatit is an indicator equal to one if person i is living in a treatment county in quarter t and zero otherwise, αst represents the full set of service area-by-quarter fixed effects illustrated in the bottom panel of Online Appendix Figure A1, and ϵit represents a random error term. We also include a full set of individual fixed effects, γi to ensure that our estimates are not driven by differential changes in the composition of Medicaid enrollees over time in treatment vs. control counties. For our primary outcomes, we also include estimates from regressions without individual fixed effects. We also estimate reduced form results pooled over the pre-period (2004–2006) and post-period (2007–2010) using a modified version of the regression described in Equation (1) where we replace the quarter-by-quarter interactions between quarter dummies and Treatit with a single indicator equal to 1 for any quarter during the post period, Postt. In this regression the coefficient on Postt represents the differential change in the outcome in treatment vs. control counties averaged across the entire post-period.
Our IV specification uses the county-level mandates as an instrument for enrollment in the STAR+Plus program.15 The IV estimates are local average treatment effects (LATEs) specific to the population of disabled beneficiaries who complied with the STAR+Plus enrollment mandate (68% of the population).
Identification. —
In order for the IV estimates to represent the causal effect of the STAR+Plus program (i.e. the combination of enrollment in a private managed care plan and the relaxation of the drug cap), it must be the case that there was no other change in the treatment counties between the pre- and post-STAR+Plus periods that did not also occur in the control counties. Because there was no other contemporaneous change in Texas’s Medicaid program that only affected treatment counties and not the controls, the main potential threat to identification is spurious differential trends in outcomes across the treatment and control counties. To ensure that differential trends do not explain our results, we first include service area grouping-by-quarter fixed effects to account for any local shocks affecting healthcare utilization patterns. Second, for all outcomes, we present event study graphs showing how the difference in the outcome between the treatment and control counties changes over time. This offers a visual test of whether differential pretrends exist over the time period preceding the shift to managed care. Finally, in Online Appendix D we replicate all analyses restricting to border zip codes within 25 miles of each other to further ensure that the control group represents a valid counterfactual for the treatment group.
A more subtle threat to identification is the potential for private provision to impact the underlying composition of Medicaid enrollees. Private Medicaid plans benefit financially from increasing take-up among Medicaid eligible individuals and from decreasing the rate at which their enrollees disenroll from the program. Not all individuals are profitable, however, implying that private plans may be incentivized to increase enrollment among some (healthier) groups while decreasing enrollment among other (sicker) groups. While there is some evidence of plans engaging in this type of selection behavior for the mainstream Medicaid population (Currie and Fahr, 2005), such behavior is unlikely when it comes to the disabled population, as Medicaid eligibility for SSI beneficiaries is typically determined indirectly by the Social Security Administration rather than by state Medicaid programs.
The possibility of differential shifts in the composition of disabled Medicaid beneficiaries in treatment vs. control counties motivates our inclusion of individual fixed effects. For similar reasons, in the online appendix we also provide an alternative version of our main results restricting to a balanced panel of Medicaid beneficiaries. Including individual fixed effects ameliorates any problems stemming from composition changes, though it also causes our estimates to reflect the effects of within-person changes in enrollment in managed care and the drug cap rather than the more general consequences of these changes. The balanced panel goes even further by eliminating the possibility that any treatment effect dynamics we estimate reflect changes in the composition of beneficiaries over the course of the post-period. Overall effects of the reform combine the effects on individuals forced to actually switch from public to private plans with the effects on individuals newly enrolling in Medicaid after the switch to managed care. These two effects may be different, as the first may entail potential disruption to a beneficiary’s care while the second may not entail any such disruption. Because of this, we include results with and without individual fixed effects for all of our primary outcomes, always with the caveat that the results from regressions excluding individual fixed effects are potentially vulnerable to differential shifts in the composition of enrollees in treatment vs. control counties. Because of this potential for bias in the specifications omitting individual fixed effects, we refer to the regressions with individual fixed effects as our “preferred specification,” include individual fixed effects in all event studies, and highlight results from these specifications throughout.
Finally, as evidence that these types of compositional shifts do not explain our results, Online Appendix Table A1 suggests that there is no change in the number of adults with disabilities exiting Medicaid after the introduction of private provision. There is a small but statistically significant change in the number of beneficiaries entering Medicaid, though Online Appendix Figure A2 suggests it is consistent with prior trends. Online Appendix Figure A2 shows that there is also no significant effect on sample composition as measured by percent white, and percent female among beneficiaries and a small positive change in mean age. Alongside our use of individual fixed effects, these results provide evidence that our main estimates are not driven by differential shifts in the composition of Medicaid enrollment.
IV. Main Results: Overall Effects of the Reform
We start by reporting the overall effects of the STAR+Plus program (the combination of the shift to private managed care plans and the relaxation of the drug cap) on healthcare spending and utilization, beginning with overall healthcare spending and then drilling down on utilization by type. Next, we proceed to assess effects on fiscal/program spending. We then focus on marginal inpatient admissions and drugs in Section V and make conclusions about the effects of the reform on quality of care and quality of life for our study sample. Finally, in Section VI we attempt to separate the effects of the two pieces of the reform, the shifting of the provision of non-inpatient, non-drug Medicaid benefits to private managed care plans and the relaxation of the drug cap, and make broader statements about the costs and benefits of these two rationing devices.
Healthcare Spending. —
Main results are reported in Table 2. For each primary outcome, we report coefficients from four regressions. The first two regressions include individual fixed effects while the second two regressions do not. The first and third regressions include an interaction between an indicator for residing in a treatment county (“Treatment”) and an indicator for the quarter being after February 2007 (“Post”), the month in which mandated enrollment in private managed care plans began in Texas. The second and fourth columns break the “post” period into two periods, an “early-post” period (2007–2008) and a “late-post” period (2009–2010). For each regression specification we report both reduced form and IV coefficients. For all primary outcomes, we also present event study figures (Figure 2) showing the evolution of the reduced form difference in the outcome between the treatment and control counties over time. Event study figures present coefficients from regressions including individual fixed effects, our preferred specification. In the event study figures, event study coefficients are divided by the baseline mean so that they can be interpreted as percent changes relative to that baseline.
Table 2—:
Main Outcomes
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
|---|---|---|---|---|---|---|---|---|
| Healthcare Spending | Rx Spending | |||||||
|
| ||||||||
| Treatment × Post | 454 (67) |
423 (59) |
140 (19) |
136 (19) |
||||
| Treatment × Post (2007–2008) | 244 (52) |
273 (52) |
80 (15) |
81 (14) |
||||
| Treatment × Post (2009–2010) | 661 (90) |
512 (82) |
210 (25) |
174 (26) |
||||
|
| ||||||||
| IV Coefficient | 607 (79) |
622 (75) |
667 (92) |
646 (96) |
187 (22) |
199 (22) |
215 (30) |
212 (30) |
|
| ||||||||
| Baseline Mean | 2,818 | 2,818 | 2,818 | 2,818 | 623 | 623 | 623 | 623 |
| Percent Change | .215 (.028) |
.221 .027) |
.237 (.033) |
.229 (.034) |
.301 (.035) |
.320 (.036) |
.345 (.048) |
.340 (.048) |
| Individual Fixed Effects | X | X | X | X | ||||
|
| ||||||||
| (9) | (10) | (11) | (12) | (13) | (14) | (15) | (16) | |
| Outpatient Spending | Inpatient Spending | |||||||
|
| ||||||||
| Treatment × Post | 366 (45) |
312 (41) |
−53** (25) |
−25 (25) |
||||
| Treatment × Post (2007–2008) | 200 (37) |
201 (32) |
−35 (28) |
−9 200 |
||||
| Treatment × Post (2009–2010) | 501 (63) |
367 (60) |
−51 (31) |
−29 (31) |
||||
|
| ||||||||
| IV Coefficient | 489 (54) |
480 (58) |
492 (61) |
467 (64) |
−70** (32) |
−57** (29) |
−40 (39) |
−32 (40) |
|
| ||||||||
| Baseline Mean | 1,551 | 1,551 | 1,551 | 1,551 | 644 | 644 | 644 | 644 |
| Percent Change | .316 (.035) |
.309 (.037) |
.317 (.04) |
.301 (.041) |
−.109 (.05) |
−.089 (.045) |
−.062 (.061) |
−.05 (.062) |
| Individual Fixed Effects | X | X | X | X | ||||
Note: Table shows reduced form and instrumental variable estimates for the main outcomes. For each outcome, the first and third columns show estimates of control-treatment differences from estimating the pooled version of the reduced form specification in Equation (1) and estimates of the impact of Medicaid managed care from estimating our instrumental variable specification, pooling over the entire post-period. The second and fourth columns show reduced form and instrumental variable estimates, when the post-period is broken into two separate periods, 2007–2008 and 2009–2010. In the second and fourth columns we estimate the IV coefficient using the two separate treatment post interaction terms as instruments. We control for service area by quarter fixed effects. Standard errors are clustered at the county level. For more details, see Section III. (N = 643, 751 beneficiary-quarters.)
Figure 2. : Main Outcomes.
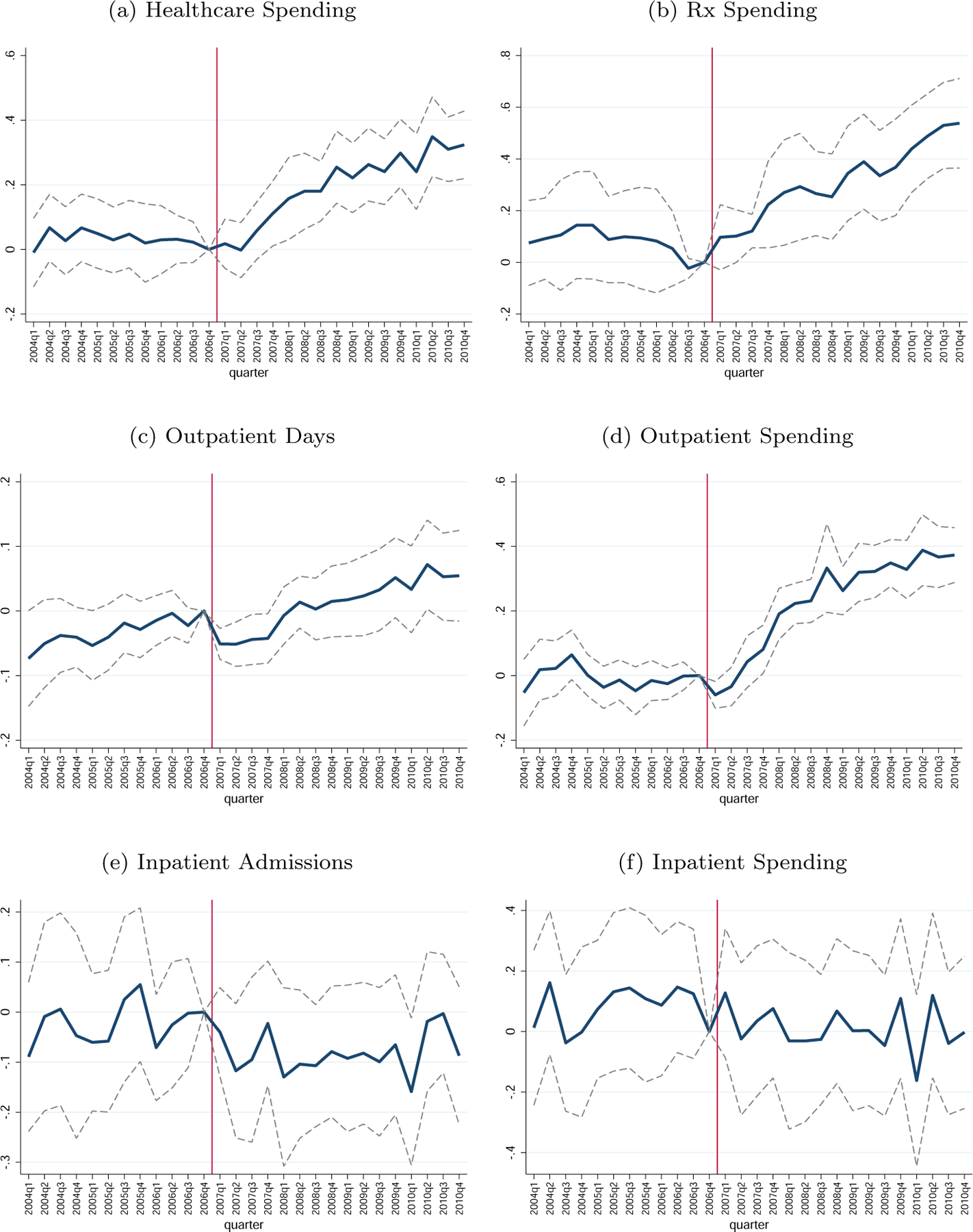
Note: Figure shows control-treatment differences in the main outcomes in percent terms relative to the treatment mean in the pre-period. These coefficients are from estimating the event study difference-in-differences specification in Equation (1), including individual fixed effects. For more details, see Section III. (N = 643; 751 beneficiary-quarters.)
The first outcome we investigate is total healthcare spending. This is not a measure of total fiscal or program spending, but instead the sum of total payments made by either the public or private plans to providers or drug manufacturers for actual healthcare services or drugs. Panel (a) of Figure 2 presents graphical evidence for the effects of the shift to STAR+Plus on this outcome, reporting event study regression coefficients describing how the difference in total spending between treatment and control counties changed over time relative to the difference in the last quarter of 2006 (the quarter prior to the introduction of STAR+Plus). The difference is relatively stable prior to the introduction of the program, providing graphical evidence that the treatment and control counties had parallel trends for the outcome and faced similar shocks during the pre-treatment period. After the introduction of STAR+Plus, the spending differential between control and treatment counties increases gradually, reaching an increase of around 30% by the fourth quarter of 2010, the end of our sample period. Regression results in Table 2 confirm the results presented in Figure 2. When post-period quarters are pooled, the average effect of the program on quarterly healthcare spending across the entire post-period is $607 (21.5%).
Prescription Drugs. —
Panel (b) of Figure 2 shows the effects of the program on drug spending. Again, the difference in drug spending between treatment and control counties is stable prior to the introduction of the program. Immediately following the introduction, however, drug spending begins to increase in treatment counties relative to control counties. By the end of our sample period, the effect of the program reaches 50% of the baseline mean, representing an enormous increase in drug spending. Table 2 shows that averaged across the full post period, the increase was $187 (30.1%).
Online Appendix Table A2 presents regression results for additional prescription drug outcomes. Specifically, we show that the program induced beneficiaries to increase days supply of drugs by 79.7 days (42.7% of the baseline mean) driven by increases of both generic (58.3%) and branded (27.1%) drugs, suggesting that the spending increase is driven by increased drug use rather than shifts to higher-priced drugs. Although the spending increases appear to come from quantity increases, we find no accompanying extensive margin effects on drug utilization. The program appears to have affected the quantity of drugs an individual consumes, but not whether she consumes any drugs in a given quarter. This result rules out the story that private plans increase drug consumption by getting people who are disconnected from the healthcare system in to see a doctor for the first time. This is not surprising, given high baseline levels of drug utilization for this population (68% of beneficiaries taking any drug). We do, however, find strong extensive margin effects at the level of the therapeutic category. Panel (b) of Online Appendix Table A3 presents results from regressions where the outcome is any spending in a particular therapeutic class. These results indicate significant increases in every category except for Immunosuppressants. These results suggest that, while the program did not affect whether beneficiaries took any drugs, it clearly caused beneficiaries to start taking new drugs that they were not previously taking. In Online Appendix Table A2 we also present effects on spending and days supply for a set of drugs typically viewed as clearly ‘high-value’ and important to patient health. We find large and statistically significant increases in both spending and days supply of these drugs, indicating that the overall increases are not solely driven by drugs of potentially marginal value to patient health.16
Outpatient Services. —
Panels (c) and (d) of Figure 2 plot event study coefficients describing effects on the number of outpatient days (Panel c) and outpatient spending (Panel d).17 For both outcomes, the difference between treatment and control counties is relatively stable throughout the pre-period, again indicating parallel pre-trends. Immediately following the introduction of the STAR+Plus program, both spending and days drop slightly. After the initial quarters, however, the effect switches from negative to positive. By the end of our sample period, outpatient spending in treatment counties has increased by almost 40% of the baseline mean relative to control counties. These results are confirmed by the regression estimates presented in Table 2, where we estimate an increase in quarterly spending of just under $500 (approximately 32%) over the post period. Online Appendix Table A4 shows that the effects on “any use” of outpatient care and the number of outpatient days are less clear, with the effect on outpatient days being around 5% but statistically insignificant and the effect on “any use” being statistically significant but very small and slightly negative, largely due to the initial drop in reported utilization (by the late-post period, the effect is statistically insignificant at close to zero).
The slight initial drop followed by a long-run increase in outpatient spending could be due to immediate “disruption” to beneficiaries’ healthcare (caused by the shift to private managed care plans) followed by long-run higher levels of outpatient spending under private plans. However, it could also be due to differential reporting (see Section II). Importantly, however, under both interpretations, these results indicate long-run higher levels of outpatient spending under STAR+Plus, and, in the case of under-reporting of outpatient claims by private MMC plans, our estimates represent a lower bound of the size of those long-run increases.18
Inpatient Services. —
Panels (e) and (f) of Figure 2 plot the event study coefficients describing effects on inpatient admissions and spending, respectively. These outcomes are noisier than other outcomes. Post-treatment, however, inpatient admissions in treatment counties seem to fall relative to control counties. The inpatient spending event studies are noisier; however, IV regression coefficients in Table 2 indicate a statistically significant spending decrease of $70, 11% of the baseline mean when including individual fixed effects. Without individual fixed effects, the effect is only about 6% and not statistically significant.
Table 3 provides regression estimates for additional inpatient outcomes. Unlike with other outcomes, there is a strong and statistically significant extensive margin (“any admissions”) effect, where the reform decreased the probability of having any inpatient admission in a quarter by 0.6 percentage points or 8% of the baseline probability. Table 3 also reveals that there is no detectable effect on inpatient admissions related to surgery, suggesting that the reduction in inpatient admissions was not driven by simply shifting beneficiaries from inpatient to outpatient surgeries. Instead, the entire effect comes through non-surgery admissions which are less likely to be viewed as “discretionary” but more likely to be deemed responsive to preventive measures (i.e., signals of low-quality care). Overall, all of these pieces of evidence combine to indicate that the reform decreased inpatient admissions and spending.
Table 3—:
Inpatient Outcomes
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Spending | Any Admissions | Admissions | ||||
|
| ||||||
| Treatment × Post | −53 (25) |
−.005 (.002) |
−.006 (.003) |
|||
| Treatment × Post (2007–2008) | −35 (28) |
−.005 (.002) |
−.006 (.003) |
|||
| Treatment × Post | −51 (31) |
−.005 (.002) |
−.005 (.003) |
|||
| IV Coefficient | −70 | −57 | −.006 | −.006 | −.008 | −.007 |
|
| ||||||
| (32) | (29) | (.003) | (.002) | (.004) | (.004) | |
| Baseline Mean | 644 | 644 | .075 | .075 | .096 | .096 |
|
| ||||||
| Percent Change | −.109 (.05) |
−.089 (.045) |
−.082 (.038) |
−.083 (.033) |
−.084 (.043) |
−.077 (.038) |
| Individual Fixed Effects | X | X | X | X | X | X |
|
| ||||||
| (7) | (8) | (9) | (10) | (11) | (12) | |
| Surgery Admissions | Non-Surgery Admissions | Length of Stay | ||||
|
| ||||||
| Treatment × Post | .001 (.001) |
−.007 (.003) |
−.054 (.032) |
|||
| Treatment × Post (2007–2008) | −.001 (.002) |
−.005 (.002) |
−.014 (.038) |
|||
| Treatment × Post | .003 (.002) |
−.008 (.003) |
−.032 (.032) |
|||
| IV Coefficient | .001 | .001 | −.009 | −.009 | −.072 | −.031 |
|
| ||||||
| (.002) | (.002) | (.003) | (.003) | (.041) | (.039) | |
| Baseline Mean | .039 | .039 | .057 | .057 | .698 | .698 |
|
| ||||||
| Percent Change | .021 (.043) |
.037 (.043) |
−.156 (.061) |
−.155 (.055) |
−.102 (.058) |
−.045 (.056) |
| Individual Fixed Effects | X | X | X | X | X | X |
Note: Table shows reduced form and instrumental variable estimates for inpatient outcomes. For each outcome, the first column shows estimates of control-treatment differences from estimating the pooled version of the reduced form specification in Equation (1) and estimates of the impact of Medicaid managed care from estimating our instrumental variable specification, pooling over the entire post-period. The second column shows reduced form and instrumental variable estimates, when the post-period is broken into two separate periods, 2007–2008 and 2009–2010. In the second and fourth columns we estimate the IV coefficient using the two separate treatment post interaction terms as instruments. We control for service area by quarter fixed effects. Standard errors are clustered at the county level. For more details, see Section III. (N = 643, 751 beneficiary-quarters.)
Heterogeneity. —
In Figure 3 and Online Appendix Table A5 we explore heterogeneity by age and health status in the effects of the program. For this analysis, we divide the population into three groups based on their pre-period Elixhauser comorbidities: the top group has no comorbidities (31% of beneficiaries), the middle group has 1–3 comorbidities (50% of beneficiaries), and the bottom group (the sickest) has 4+ comorbidities (19% of beneficiaries).19 We also divide the population into three age groups: age 20–34 (26% of beneficiaries), age 35–49 (30% of beneficiaries), and age 50–64 (44% of beneficiaries). We estimate the effects of the reform for each of the nine health-by-age groups. Figure 3 shows IV coefficients from our primary regression specification for our three primary outcomes: inpatient spending, outpatient spending, and drug spending. The figure shows that the reduction in inpatient spending and the increase in drug spending appear to be driven largely by the sickest beneficiaries in the 35–49 and 50–64 age groups. In particular, the sickest beneficiaries in the 35–49 age group experience both the largest increase in drug spending and the largest decrease in the probability of an inpatient admission.20
Figure 3. : Heterogeneity by Age and Health Status (Number of Comorbidities).
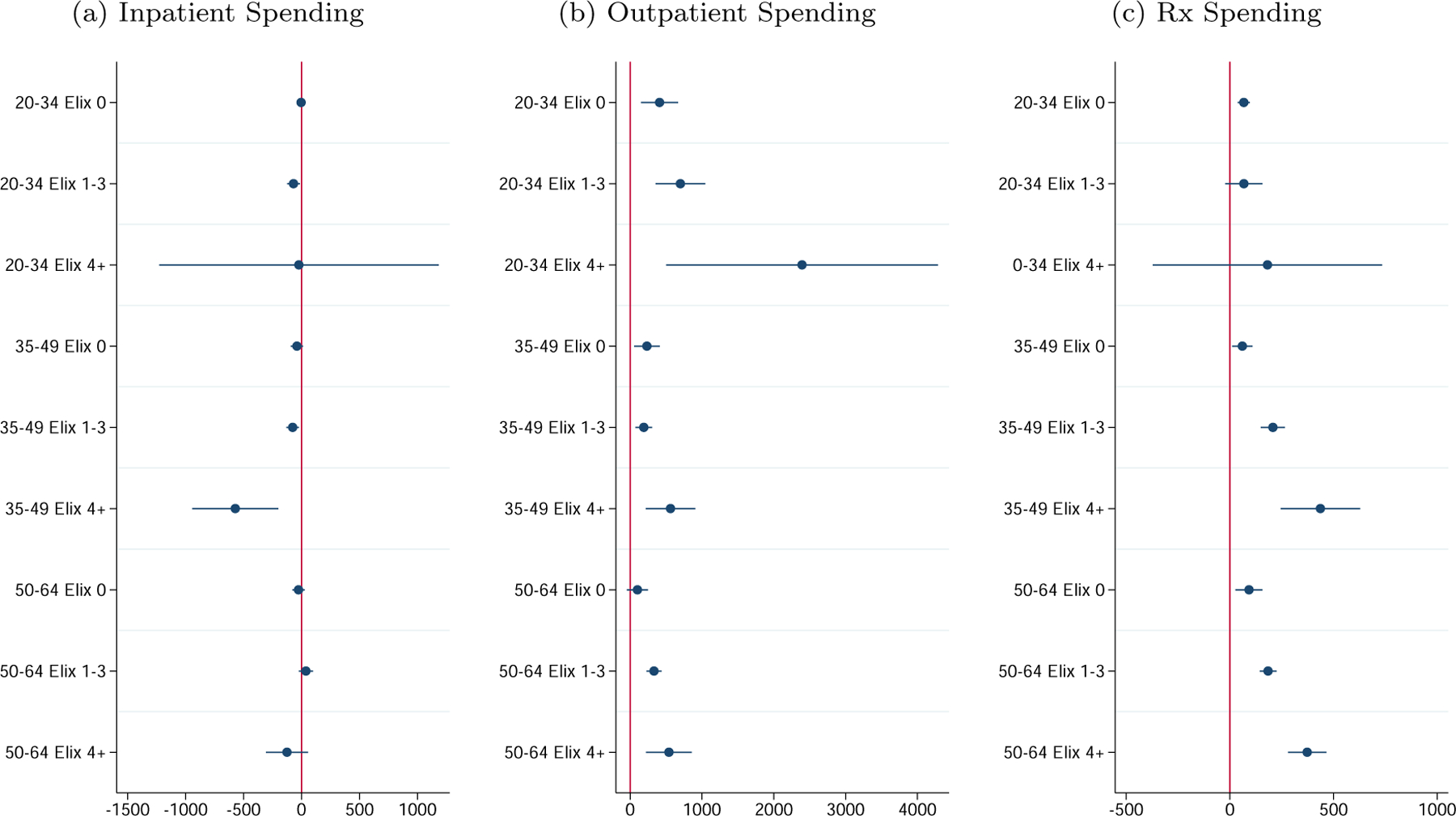
Note: Figure shows the impact of Medicaid managed care on inpatient spending, outpatient spending, and prescription drug spending by age and health status. Health status is measured as the average number of comorbidities during the pre-period, limiting our sample to beneficiaries for whom this measure can be generated. These coefficients are from estimating our instrumental variable specification separately for each age (20–34, 35–49, 50–64) by comorbidity group (no comorbidities, 1 to 3 comorbidities, at least 4 comorbidities). For more details, see Section III (N = 478, 938 beneficiary-quarters.)
We note that the inpatient effects are much larger for the 35–49 age group than the 50–64 age group. This may seem counter-intuitive, but Duggan, Kearney and Rennane (2015) show that the younger and older SSI beneficiaries are likely to be quite different. They show that over 70% of younger SSI beneficiaries (ages 18–40) qualified for SSI due to a mental disability compared to fewer than 50% of older SSI beneficiaries (ages 50–64). In Online Appendix Figure B1, we present the prevalence of a variety of clinical conditions by age. (Online Appendix B provides further details on the SSI program.) The vast majority of conditions appear to be monotonically increasing in age. However, there is one set of conditions that instead peaks at middle age: mental health conditions. In Section V below, we show that the decrease in inpatient use is largely driven by inpatient stays related to mental health conditions. Thus, the larger decrease in inpatient stays among the middle-age group is consistent with the idea that inpatient stays related to mental health conditions are more likely to be “marginal” to improvements in care (especially increased use of prescription drugs, which we show are also concentrated among drugs used to treat mental health conditions), and these types of inpatient stays are likely to be concentrated among this middle-age group. The older group, on the other hand, is afflicted by a different set of conditions, for which improvements in care are less likely to translate to lower use of inpatient care.
The treatment effect heterogeneity we document raises the possibility that the changing effects over the post-period are due to changes in the composition of the sample over time. To address this possibility, in Online Appendix Table A7 we present our main results using a balanced panel of Medicaid beneficiaries. Panel (a) uses a short panel (2005–2008) while Panel (b) requires enrollment for the entire study period (2004–2010). While the balanced panel restriction clearly hurts statistical power, our key results are robust to the use of this balanced sample.
Fiscal Costs of Medicaid and Pass-Through. —
We now turn to the fiscal costs of the program (i.e., the shift to private managed care plans and the relaxation of the drug cap). Thus far, all spending outcomes have been based on payments from Medicaid insurers (either private plans or the government) to healthcare providers. We now ask how the program affected the total fiscal cost of Medicaid for the government (state and federal). As discussed in Section II, fiscal spending consists of two components: (1) fee-for-service healthcare spending paid directly by the government to healthcare providers and (2) premium payments from the government to private MMC plans. We report regression estimates for fiscal spending outcomes in Table 4.21 The results provide clear evidence that the program led to an increase in Medicaid spending, with fiscal costs increasing by 25.9% in treatment counties relative to control counties. This spending increase appears to come both from services that are carved-out of the private plan contracts (“not covered spending”), i.e. drugs and inpatient services, and from the shift of services from FFS to MMC plans (“covered spending”). The coefficients from these regressions indicate that about 16% ($117) of the spending increase comes from increases in spending on carvedout services while the other 84% ($615) comes from premium payments to private plans being set higher than counterfactual public plan spending for covered services (standard error: 8.7%). These results suggest that the bulk of the cost of the reform came not from the relaxation of the drug cap but instead from the shift to managed care for non-drug, non-inpatient services. We discuss this more in Section VI.
Table 4—:
Medicaid Spending
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Medicaid Spending | Covered Spending | Not Covered Spending | Healthcare Spending | |
| Treatment ×Post | 548 (71) |
460 (53) |
88 (34) |
454 (67) |
|
| ||||
| IV Coefficient | 732 (82) |
615 (64) |
117 (41) |
607 (79) |
|
| ||||
| Baseline Mean | 2,828 | 1,560 | 1,268 | 2,818 |
| Percent Change | .259 (.029) |
.394 (.041) |
.092 (.032) |
.215 (.028) |
| Individual Fixed Effects | X | X | X | X |
Note: Table shows reduced form and instrumental variable estimates for Medicaid spending outcomes. For each outcome, the table shows estimates of control-treatment differences from estimating the pooled version of the reduced form specification in Equation (1) and estimates of the impact of Medicaid managed care from estimating our instrumental variable specification, pooling over the entire post-period. We control for service area by quarter fixed effects. Standard errors are clustered at the county level. For more details, see Section III. (N = 643, 751 beneficiary-quarters.)
The extent to which increases in fiscal spending under private managed care plans translate into increases in healthcare spending indicates the degree of marginal spending “pass-through” to providers and patients (vs. private insurers). The coefficients in Columns 1 and 4 of Table 4 indicate that increases in healthcare spending were slightly smaller than increases in fiscal spending. Specifically, the results indicate that the increase in healthcare spending ($607) was about 83% (standard error: 10.7%) of the increase in fiscal spending ($732), providing suggestive evidence that the vast majority of additional Medicaid spending went to providers and patients rather than to private insurers.
Robustness. —
As described above, graphical evidence from analyses of program effects indicates that all outcomes were trending similarly in treatment and control counties prior to the roll-out of STAR+Plus. This suggests that post-period trends of outcomes in control counties are likely to be good counterfactuals for post-period trends in treatment counties in the absence of the STAR+Plus program. However, parallel pre-trends need not necessitate parallel post-trends in the absence of the treatment. If treatment and control counties are hit with a shock that affects these counties differently, the effects of this shock, despite occurring in both treatment and control counties, could confound the effects of the STAR+Plus program.
Border Zip Code AnalysisConcerns about the validity of our empirical approach could include potential confounding differences between treatment and control counties, given (1) treatment counties are more urban than control counties and (2) the treatment occurred in early 2007, not long before the start of the Great Recession. If the recession affected more-urban vs. less-urban counties in different ways, this might confound program effects. To test whether this is a problem, in Online Appendix D we present results where we only include beneficiaries in treatment zip codes within 25 miles of a control zip code and beneficiaries in control zip codes within 25 miles of a treatment zip code. Online Appendix Figure D1 shows the included and excluded zip codes. This restriction effectively excludes urban centers and rural outlying areas, leading to greater similarity between treatment and control groups on some measures relative to the case where we use all zip codes in treatment and control counties.22 With these restrictions, our results are virtually identical to the baseline results. Regression estimates in Online Appendix Table D2 indicate that the reform caused a 22% increase in total healthcare spending, a 31% increase in spending on prescription drugs, and a 34% increase in outpatient spending. Again, we also find a 12% decrease in inpatient spending.
Potential SpilloversAnother potential concern might be that there are spillovers between treatment and control counties. For example, if all beneficiaries living in control counties see doctors practicing in treatment counties, and these doctors also treat a substantial number of beneficiaries living in treatment counties, the control beneficiaries may be impacted by the treatment.23 In the presence of this type of spillover, our estimates would represent a lower bound of the overall effect of the reform. This type of spillover is of particular concern when we focus on county borders as in the analysis in Online Appendix D.
To explore the extent to which spillovers may occur in our setting, we determine the extent to which control county beneficiaries see doctors with high numbers of treatment county patients. Online Appendix Figure A5 is a histogram showing the percent of claims from treatment county patients for each provider in the data. Most providers either treat only control-county beneficiaries or treatment-county beneficiaries and few providers treat patients from both treatment and control counties.24 This suggests that spillovers of the treatment onto control county patients is unlikely.
Analysis By Service AreaTo further gauge the robustness of our findings, in Online Appendix Tables A8-A11 we break down our difference-in-difference estimates by service area, finding that our key results hold in each service area in the state (though with some loss of statistical power). This shows that our results are not driven by one particular service area. Taken together, these results provide additional confidence that we are capturing the overall program effects, rather than some other confounding factor.
V. Quality and Beneficiary Health
Thus far, we have assessed the effects of the STAR+Plus program on healthcare spending and utilization patterns. We now turn to the question of how these shifts in utilization patterns affected the quality of care received by and, ultimately, the health of SSI beneficiaries. Throughout this section we continue to focus on the overall effects of the program. In Section VI, we attempt to assess which effects are attributable to the two components of the reform, the shift to managed care vs. the relaxation of the drug cap.
To assess effects on quality and health, we first focus our attention on the marginal drugs and marginal inpatient admissions. For drugs, we assess whether the marginal drugs are “high value” and have a high likelihood of positively impacting the lives of chronically ill beneficiaries. For inpatient admissions, we assess whether the marginal admissions fall into categories that are typically deemed potentially “avoidable” given appropriate management of chronic diseases.25 We then turn to measures of beneficiary health and functional capacity. Specifically, we analyze effects on mortality, employment, and exit from the SSI program using administrative data from the Social Security Administration.
Drug OutcomesPanel (a) of Figure 4 and Online Appendix Table A3 present effects on spending and “any spending” by therapeutic category for the ten largest categories. The large increase in overall drug spending we observe is driven by six categories: anti-infective agents, autonomic drugs, cardiovascular agents, central nervous system, hormones and synthetic substitutes, and gastrointestinal drugs. The central nervous system class is the largest class in this population, and further results using narrower classes within the central nervous system category (Online Appendix Table A12) reveal that the largest effects are observed for anti-depressants, anti-psychotics, and drugs used to treat pain. These drugs, especially the anti-psychotics, are critical for this population given its high rate of mental illness (see Online Appendix B). The large increase in utilization of these drugs suggests severe undertreatment of these conditions prior to the shift to managed care and relaxation of the drug cap.
Figure 4. : Prescription Drug and Inpatient Spending by Category.
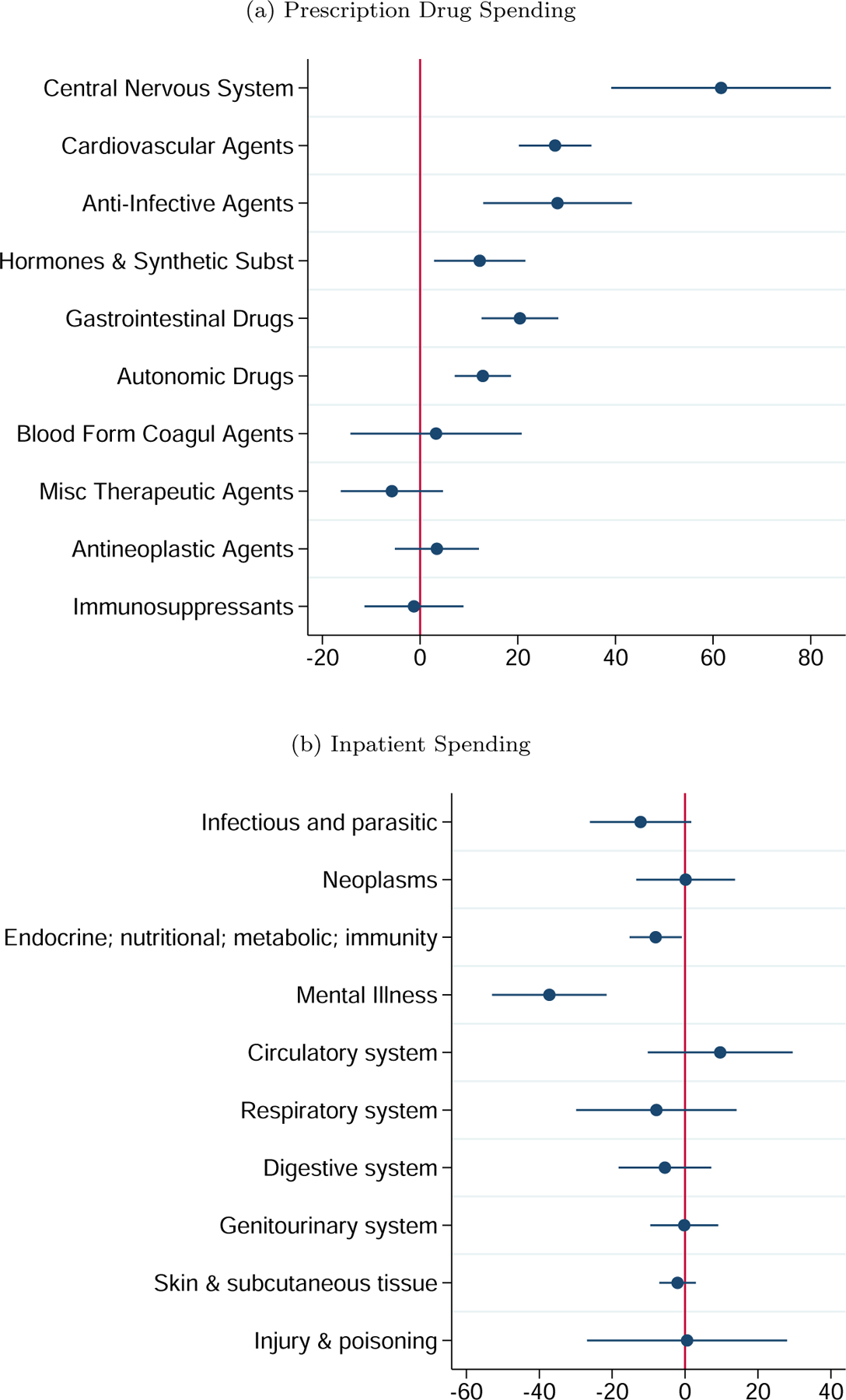
Note: Figure shows the impact of Medicaid managed care on prescription drug spending and inpatient spending. Panel (a) shows estimates for prescription drug spending by Redbook therapeutic category. Panel (b) shows estimates for inpatient spending by CCS category. These coefficients are from estimating our instrumental variable specification in separately for each of the categories. For more details, see Section III. (N = 643, 751 beneficiary-quarters.)
The detailed results for cardiovascular agents, the second largest class in this population, are reported in Online Appendix Table A13. Here, the effects are driven by ACE Inhibitors, Beta Blockers, and anti-hyperlipidemic Drugs (i.e. statins). All of these medications are considered “high value” drugs that are highly effective at treating heart disease, a common condition in this population (see Table 1), again suggesting potential improvements to health and quality of life.
The detailed results for the hormones and synthetic substitutes class, the third largest class in this population, are reported in Online Appendix Table A14. Here, the effects are driven by Adrenals and anti-diabetic agents. Adrenal drugs are used to treat asthma and COPD, two common ailments in this population.
Thus, a large portion of the large positive effect of the STAR+Plus program on prescription drug utilization comes from drugs that are used to treat chronic conditions highly prevalent in this population. Unlike some drugs, the value of these drugs for patients is well-established. These drugs are also highly unlikely to be prescribed to patients who would not benefit from them. All of these factors combine to provide suggestive evidence that the combination of the shift to managed care and the relaxation of the drug cap led to important improvements in quality of care, and likely quality of life, for this population.
Inpatient OutcomesAs with prescription drugs, our data on inpatient utilization is detailed and consistently reported pre- and post-mandate, allowing us to perform a “deep dive” into the effects of the STAR+Plus program on inpatient outcomes. Specifically, we can assess whether these policy changes led to reductions in potentially avoidable inpatient admissions. Panel (b) of Figure 4 and Online Appendix Table A15 break down the effects on inpatient spending by the Clinical Classifications Software (CCS) category of the principal diagnosis for the admission.26 The strongest effect is observed for inpatient admissions related to mental illness, for which the shift decreased the probability of an admission by 0.6 percentage points, or 64% of the baseline quarterly probability of admission. The other category that saw a clinically significant decrease in the probability of admission was Endocrine, nutritional, and metabolic diseases and immunity disorders (where the most common disease is diabetes), where the probability of admission decreased by 0.2 percentage points, or 40% of the baseline quarterly probability of admission.
Inpatient stays across these categories are often considered avoidable via appropriate management of underlying chronic conditions such as bipolar disorder, schizophrenia, depression, and diabetes. The conditions associated with these categories are also highly prevalent in this population. Reductions in inpatient spending in these areas thus provide suggestive evidence of important improvements in quality of care, and, potentially, quality of life. An alternative explanation for these results is that private managed care plans were stinting on access to necessary inpatient care in these categories. We think that there are three pieces of evidence that decreases in inpatient admissions in these categories reflect improvements in care rather than stinting by private managed care plans. First, there is a close link between the conditions associated with the CCS categories with the largest decreases in inpatient admissions and the conditions associated with the therapeutic classes of drugs with the largest increases in utilization, suggesting the drug utilization increase as a clear mechanism for the avoided inpatient admissions (discussed further in Section VI). Second, as discussed in Section I, inpatient care was carved out of private plan contracts so that private plans do not benefit financially from limiting inpatient admissions.27 Third, we see decreases in inpatient admissions in categories that are avoidable if the underlying causes are treated properly but not in other categories of inpatient care, such as inpatient admissions for surgery (see Table 3). These pieces of evidence combine to cause us to conclude that the effects on inpatient utilization are more consistent with improvements in the quality of care received by and health of disabled Medicaid beneficiaries than with stinting by managed care plans.
Mortality and Employment OutcomesWe also examine indicators of beneficiary health and functional capacity, including mortality, employment, and the suspension of SSI benefits using the SSA’s Disability Analysis File (DAF). We find decreases in mortality and increases in employment and benefit suspensions, consistent with improvements in health and functional capacity, although none of the results are statistically significant. Further details of the data used and the analysis are provided in Online Appendix F.
VI. Mechanisms
In Section IV we presented results on the effects of the introduction of the STAR+Plus program, i.e. the combined effects of the shifting of disabled Medicaid beneficiaries to managed care and the relaxation of the three prescription per person per month limit. We found that the program (1) increased prescription drug utilization and spending, (2) increased outpatient utilization and spending, (3) decreased inpatient utilization, (4) increased overall spending on healthcare, and (5) increased fiscal spending. In this section, we attempt to assess which effects were caused by the shift to managed care versus the relaxation of the drug cap by exploring the mechanisms behind the changes in each outcome.
Prescription Drug Mechanisms. —
There are three features of the STAR+Plus program in Texas that could explain the increase in drug utilization we estimated in Section IV: (1) the relaxation of the drug cap when beneficiaries entered Medicaid managed care, (2) the “carve-out” of prescription drugs from the managed care plan contracts, and (3) the shift of the provision of non-drug, non-inpatient medical benefits to managed care. In this section, we provide evidence that (1) is largely responsible for the increases in drug utilization we observe. In Online Appendix G we provide evidence, including an additional difference-in-differences analysis of a later policy that carved drugs into MMC plan contracts, that (2) and (3) are not the driving factors behind the drug result.
Drugs are strictly rationed for Texas Medicaid beneficiaries not enrolled in a private managed care plan. Individuals enrolled in the public program can only fill three prescriptions per month. There are few exceptions to this rule, making it likely to be highly binding for adults with disabilities. To underscore the stringency of this rule, given typical levels of drug utilization, 35% of adults with disabilities enrolled in both Medicaid and Medicare (a population that is similar to but not our sample, and who is not subject to the drug cap) exceeded this cap in a typical month during the 2006–2010 period. As a consequence, the relaxation of this cap for those enrolling in a private managed care plan is likely to explain much of the private vs. public difference in drug utilization.
To understand how much of the increase in drug use under private provision comes from the relaxation of the drug cap, we extend the regressions used as part of our primary analyses. In these new regressions, the outcomes are indicators for the number of months in the quarter in which the individual filled more than 0 prescriptions, more than 1 prescription, more than 2 prescriptions, etc. up to more than 6 prescriptions. If we see small or no effects for “more than 0”, “more than 1”, and “more than 2” but large effects for “more than 3”, “more than 4”, “more than 5”, etc. this will provide strong evidence that much of the effect on drug utilization is coming from the relaxation of the drug cap as opposed to the drug carve-out or the shifting of the provision of medical services to managed care because both of those features would be expected to shift all parts of the distribution of drug utilization rather than only shifting people to take more than 3 drugs.
The event study coefficients from each of these regressions are plotted in Figure 5. The dotted lines show effects for changes in drug utilization below the 3-drug cap, while the solid lines show effects for drug utilization above the 3-drug cap. There is essentially no effect for “more than 0” or “more than 1”. There is a small effect for “more than 2”. The largest effect, however, is for “more than 3”. There are also large effects for “more than 4”, “more than 5”, and “more than 6”. This, combined with the absence of any effect of the shift to managed care on drug utilization in New York (where there was no drug cap) from our prior work (Layton et al., 2019), suggests that much of the effect of private provision on drug utilization in Texas was from beneficiaries starting to fill more than 3 prescriptions in a month. This provides suggestive evidence that the relaxation of the drug cap was responsible for much of the overall drug effect.
Figure 5. : Number of Months With More Than a Given Number of Unique Drugs.
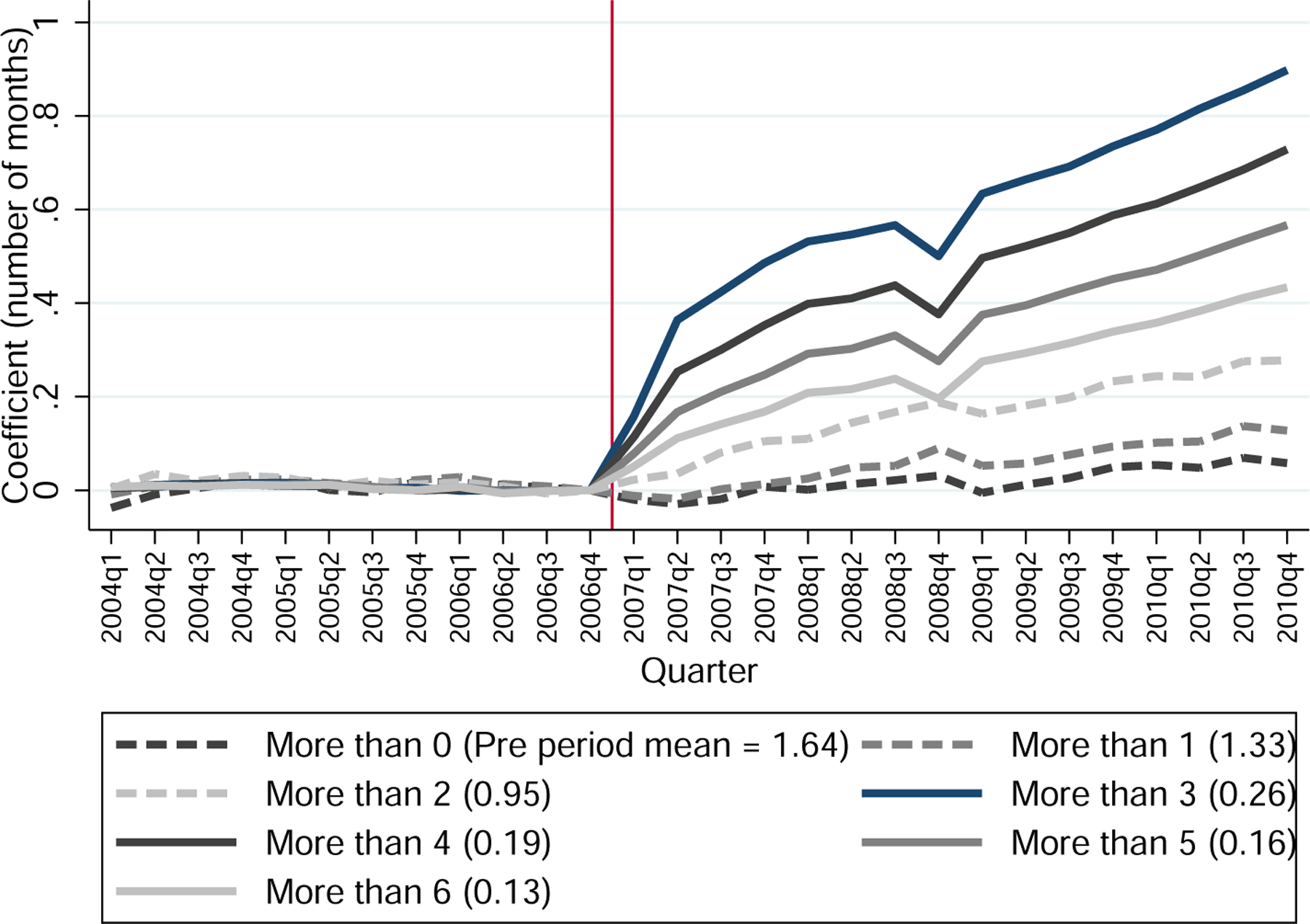
Note: Figure shows control-treatment differences in the number of months during which more than a given number of unique drugs was prescribed. These coefficients are from estimating the event study difference-in-differences specification in Equation (1), including individual fixed effects. For more details, see Section III. (N = 643, 751 beneficiary-quarters.)
Based on this evidence and the evidence presented in Online Appendix G, we argue that the relaxation of the drug cap serves as the primary mechanism through which the Texas reform produced the observed increase in drug utilization. This provides evidence that rationing drugs via quantity limits is an effective way to reduce drug spending. However, the evidence we present in Section V suggests that the spending reductions achieved using these quantity limits are not well-targeted: Much of the reduction comes via reduced utilization of high-value drugs used to treat chronic diseases that are common in this population.
Outpatient Utilization Mechanisms. —
To unpack the increase in outpatient spending in Texas, we start by decomposing the spending increase into changes in price and quantity. Recall that outpatient spending shifted from public provision to private managed care plans, so changes in spending could be due to either changes in quantities or to differences between the rates paid to providers for a given service by public versus private plans.
We start by providing descriptive comparisons of prices in Texas’s public program vs. prices paid by Texas’s private managed care plans. These descriptive analyses are found in Online Appendix H. For all analyses, we classify outpatient claims according to the procedure code listed on the claim. We then compare public and private payments for each procedure code. Online Appendix Figure H1 provides scatterplots and histograms comparing public and private prices. All figures suggest that there is some variation in prices between the public and private plans, but that overall prices appear fairly similar.
Next, we use a regression to estimate price differences between public and private plans. Specifically, we estimate a regression of the following form:
| (2) |
The unit of analysis is the claim line c, and we regress the log payment on a full set of procedure fixed effects (γp) and an indicator for whether the claim is a private plan claim vs. a public plan claim. β represents the average difference in payment for private vs. public plans, conditional on procedure, which we interpret as the public vs. private price difference. We estimate this difference to be 8.5%, as indicated in Online Appendix Table H1. We also perform a version of this regression where we allow the price difference to vary by procedure. The distribution of public vs. private price differences estimated by this regression is presented in Online Appendix Figure H2. The median price difference is 4%. Taken together, these analyses suggest that private prices are slightly higher than public prices.
This raises the question of whether the increase in outpatient spending reflects more money being transferred to providers for providing the same set of outpatient services or instead represents a combination of higher prices and increased access and utilization achieved via those higher prices. To answer this question, we first point to Panel (c) of Figure 2 and Online Appendix Table A4 where, as discussed in Section IV, we show that the quantity of outpatient care (as measured by “any use” and the number of days with an outpatient claim) increases slightly under managed care, though the increases are often not statistically significant. This result suggests that managed care resulted in higher prices and slightly higher quantities.
Next, we use the estimates from Equation (2) to “re-price” private plan claims to be based on public plan prices, by removing the estimated private plan price effect. We use these re-priced claims to build measures of price-equivalent “plan outpatient spending” for each individual, which only reflects differences in utilization and not in prices. We then run our primary regression specification using these outcomes. Results from these regressions are found in Online Appendix Table H2. This table suggests that differences between public and private prices account for 28% (standard error: 1.4%) of the $489 increase in outpatient spending under private provision. These results indicate that the overall spending increase is largely driven by increases in actual utilization rather than different public and private prices for the same services.
Finally, we consider the possibility that the increase in outpatient utilization we estimate is driven by the relaxation of the drug cap rather than the shift to managed care. It could be the case that the relaxation of the drug cap led Medicaid beneficiaries to visit the doctor more often in order to get additional prescriptions. If this is the case, some portion of the increase in outpatient utilization may have occurred even without the roll out of managed care. To explore this possibility, in Online Appendix Table A16 we divide price-standardized outpatient spending by whether a prescription was written on the same day that the outpatient spending occurred or not. We find that only 35–37% (standard error: 14.7–16.3%) of the increase in price-standardized outpatient spending occurs on days when a prescription was written, while the other 63–65% (standard error: 14.7–16.3%) occurs on days when a prescription was not written. We note that even though 35% of the marginal spending is associated with a prescription being written, this does not imply that that 35% of the increase in utilization was due to the relaxation of the drug cap: Without the relaxation of the drug cap, the utilization associated with prescriptions may still have occurred and just not been associated with any prescription. Managed care may have still led to more utilization, and possibly even more prescriptions being written, but under the drug cap many of those prescriptions may just not have been ultimately filled. Instead, we think of this analysis as providing an upper bound to the portion of the increase in outpatient utilization potentially attributable to the relaxation of the drug cap. Even with this upper bound, these results suggest that the roll out of managed care still independently led to a significant increase in outpatient utilization.
We interpret these results as suggestive evidence that in Texas (1) private plans pay higher prices to healthcare providers than public plans and (2) utilization of outpatient care increases under managed care. These results are consistent with an upward-sloping supply curve for Medicaid services, with private plans paying higher prices for healthcare services and providers responding by increasing their supply of those services to Medicaid beneficiaries. This is consistent with results from Chen (2017) and Alexander and Schnell (2019). Thus, a key characteristic of the provision of Medicaid benefits via private managed care plans in Texas seems to be improved access to care via higher prices.
Inpatient Utilization Mechanisms. —
We showed in Section IV that the combination of the relaxation of the drug cap and the shift to managed care led to a decrease in inpatient admissions in Texas. In Section V we showed that the decrease in admissions is concentrated in admissions related to mental illness, with additional effects on admissions related to diabetes. In Section V we also showed that the increase in drug utilization we observe under private provision is largely driven by drugs used to treat mental illness, with important effects also observed for drugs used to treat diabetes. This raises the question as to whether the increase in drug utilization caused the decrease in inpatient admissions.
In our setting, it is not possible to fully disentangle how much of the reduction in inpatient admissions comes from increased drug utilization (which we argued above was due to the relaxation of the drug cap) versus the shift to managed care. In other settings, managed care plans have been shown to decrease inpatient utilization (Duggan, Gruber and Vabson, 2018). However, our setting differs from those settings in that in Texas, the managed care plans did not bear financial responsibility for inpatient spending and thus had little incentive to keep beneficiaries out of the hospital. Nevertheless, it is still possible that the managed care plans engaged in actions that might have indirectly led to decreases in inpatient use.
We present two pieces of suggestive evidence that any such actions were not the driving factor behind the reduction in inpatient spending, and that this reduction was instead largely driven by the increase in drug utilization stemming from the relaxation of the drug cap. To start, we find that the groups seeing the largest increases in drug utilization (the sickest beneficiaries in the middle-age and older-age groups) also experience the largest decreases in inpatient utilization under STAR+Plus. Indeed, in Online Appendix Table A5 where we stratify our main results by age-by-health status cells, the same cell that has the largest increase in drug spending also has the largest decrease in inpatient admissions: Disabled adults aged 35–49 with 4+ Elixhauser comorbidities saw an increase in drug spending of $549 (49% of baseline) and a decrease in the probability of an inpatient admission of 5 percentage points (19% of baseline).28 Second, in Figure 4 we showed that the conditions associated with large and statistically significant inpatient admission reductions under the reform (mental illness, diabetes) also happen to be associated with large increases in drug utilization. Further, the age-by-health status cell we highlighted above with the largest drug and inpatient effects is also the group where mental health conditions such as depression and psychoses are most prevalent. These pieces of evidence combine to provide suggestive evidence that the increase in drug utilization is likely to have been at least partially responsible for the reduction in inpatient spending.
Mechanisms Behind Increases in Fiscal Spending. —
We now turn to our results establishing that the combination of the relaxation of the drug cap and the roll out of managed care led to an increase in fiscal/program spending. In this section, we attempt to unpack this overall effect and provide evidence as to whether the relaxation of the drug cap or the roll out of managed care was the driving factor behind the spending changes.
To accomplish this goal, we start by dividing fiscal spending into two components. The first component is “not covered spending,” which is spending on services that are carved out of private managed care plan contracts and always paid directly by the state, even for individuals enrolled in private plans. We start by noting that “not covered spending” consists of inpatient and drug spending. The evidence we provided above suggests that the increase in drug spending and the decrease in inpatient spending are attributable to the relaxation of the drug cap, implying that any change in “not covered spending” should be attributed to the relaxation of the drug cap. In Table 4, in column (3) we estimate the effects of the reform on “not covered spending”. The positive and significant coefficient estimates clearly imply that the increases in drug spending were not fully offset by decreases in inpatient spending. Indeed, “not covered spending” increased by around $117 per quarter or 9%.
The second component of fiscal spending is “covered spending”. “Covered spending” is equal to fee-for-service payments for non-inpatient, non-drug services (i.e. services covered by managed care plans) for individuals not in managed care and equal to the capitation payment paid to the managed care plan for individuals enrolled in managed care. The coefficient in column (2) reveals that the reform increased covered spending by $615 per quarter, or 39%. The increase in covered spending can only come from one source: capitation payments to managed care plans being set higher than counterfactual fee-for-service payments. In other words, the increase in “covered spending” is fully attributable to the shift to managed care. Importantly, comparing columns (1) and (2) shows that the increase in spending attributable to the increase in covered spending makes up 84% (standard error: 8.7%) of the overall increase in fiscal spending. This implies that the bulk of the fiscal cost of the reform is attributable to the shift to managed care, even though much of the benefit seems to be attributable to the relaxation of the drug cap.
VII. Conclusion
There are many tools for rationing healthcare services. Some, like cost-sharing, are widely used in middle- and high-income settings but may be less appropriate for low-income households. This has led state Medicaid programs, which cater exclusively to low-income households, to adopt other types of rationing mechanisms. Two of the most common are quantity limits for prescription drugs and the provision of Medicaid benefits via private managed care plans that receive capitated payments for each of their enrollees and are then responsible for all care received by those enrollees.
The results we present in this paper provide evidence of the trade-offs involved with these two commonly used tools. Our results suggest that drug caps can be effective at reducing drug spending, but that spending reduction seems not to be well-targeted: The marginal drugs are often high-value and the rationing of these drugs seems to increase the likelihood of inpatient hospital stays related to the conditions treated by the drugs. Given that inpatient hospital stays are often a sign of severe health problems, it also seems likely that these drug caps cause Medicaid beneficiaries to be in worse health than they would be without them. These results imply that the spending reductions induced by drug caps come with heavy trade-offs.
Our results also suggest that conventional wisdom about managed care may be wrong. Supporters of managed care often say that it saves money for states that adopt it. Our results reject this hypothesis in the case of Texas, showing large increases in fiscal spending. Opponents of managed care, on the other hand, often say that managed care leads to access problems for Medicaid beneficiaries. Our results also reject this hypothesis in the case of Texas, showing modest increases in utilization of non-inpatient medical care. Our results suggest a more nuanced view of managed care: Managed care seems to increase spending, but much of that increase in spending goes to patients and physicians in the form of higher prices paid to doctors and increased utilization of medical services. Thus, there is again a trade-off, this time between spending and access.
Supplementary Material
Acknowledgments
We study two mechanisms used by public health insurance programs for rationing healthcare: outsourcing to private managed care plans and quantity limits for prescription drugs. Leveraging a natural experiment in Texas’s Medicaid program, we find that the shift to managed care and the relaxation of a strict drug cap increased access to high-value drugs and outpatient services and reduced avoidable hospitalizations. Program costs increased significantly, indicating a trade-off between cost and quality. We provide suggestive evidence attributing the reduction in hospitalizations to the relaxation of the drug cap and much of the spending increase to the shift to managed care.
We thank Kate Bundorf, Heinrich Kögel, Jessica Van Parys, and Matt Rutledge for serving as discussants for the paper as well as seminar participants at Harvard Medical School, the Leonard Davis Institute of Health Economics at the University of Pennsylvania, the NBER Spring Aging Meeting, ASHEcon, the American-European Health Economics Study Group, the Disability Research Consortium Annual Meeting, the University of Minnesota, the Schaeffer Center at the University of Southern California, the Institute on Health Economics, Health Behaviors, and Disparities at Cornell University, Harvard University, the APPAM Annual Fall Research Conference, Yale School of Public Health, and RAND for useful comments. We thank Mike Geruso, Jon Kolstad, Jenn Kowalski, Chris Ody, Bastian Ravesteijn, Mark Shepard, Amanda Starc, and Jacob Wallace for helpful conversations about earlier drafts of this paper. Special thanks to Francoise Becker at the Social Security Administration (SSA) for data analysis support with the Disability Analysis File. Julia Yates provided excellent research assistance. We gratefully acknowledge financial support from the Laura and John Arnold Foundation, the Social Security Administration through grant #5 DRC12000002–06 to the National Bureau of Economic Research as part of the SSA Disability Research Consortium, the National Institute on Aging (P30-AG012810), and the Agency for Healthcare Research and Quality (K01-HS25786–01). The findings and conclusions expressed are solely those of the authors and do not represent the opinions or policy of SSA, any agency of the Federal Government, or the National Bureau of Economic Research.
Footnotes
Nominal cost-sharing is permitted for some services and drugs, with cost-sharing limits varying by income category. For those below 100% of FPL, the maximum copay ranges between $4 to $8 for most medical and drug services (Kaiser Family Foundation, 2017).
Adults with disabilities in institutional long-term care were not subject to the MMC enrollment mandate.
MMC is more likely to be introduced earlier to urban counties than to rural counties not just in Texas, but across the U.S. MMC is generally harder to launch and maintain in rural areas, as construction of adequate provider networks is more challenging due to these areas’ lower population densities, combined with their lower supply of practicing physicians (Silberman et al., 2002). Thus, states have typically expanded Medicaid managed care to rural areas only after getting experience operating managed care in less challenging urban settings, as occurred in Texas after our data ends.
Harris County is the only exception to this, as this service area transitioned adults with disabilities to STAR+Plus at an earlier date. Because of this, we omit Harris County from our sample, though we include the other counties in the Harris service area, all of which transitioned to MMC in 2007.
Base payments were set at the county level by independent actuaries based on prior spending in the region. Plan payments were then set equal to the base rate multiplied by a budget-neutral risk adjustment factor that accounts for differences in enrollee health status (as recorded in diagnoses on claims) across plans participating in a given service area. Plans then used these payments to pay providers for all healthcare services received by their enrollees, with the exception of any “carved-out” services. Carved-in services represent 55% of healthcare services received by enrollees in the treatment counties in the pre-period, while carved-out services represent 45%.
In Texas, “[a]dults enrolled in traditional fee-for-service (FFS) Medicaid are limited to three prescriptions per month. All other Medicaid-eligible individuals are allowed an unlimited amount of prescriptions.” (Texas Health and Human Services Commission, 2017) Those exempted from the Medicaid three-prescription limit are children under the age of 21, people enrolled in private Medicaid plans, and people enrolled in eligibility waiver programs. “Drugs and products that are not counted towards the three-prescription limit include family planning drugs, diabetic supplies, smoking cessation products, home health supplies, and mosquito repellent.” (Texas Health and Human Services Commission, 2018)
A number of states besides Texas have had a drug cap applying only to beneficiaries in public fee-for-service Medicaid and not to those in private Medicaid managed care. These states include Alabama, California, Kentucky, and Louisiana.
Medicaid also covers various forms of behavioral health, including a comprehensive set of mental health services. Some of these services were provided via MMC plans under STAR+Plus, though the extent of these benefits did not change. Unfortunately, our data do not allow us to analyze the effects of the reform on behavioral health independently (though it is included in our total spending estimates).
In Online Appendix C we provide some evidence that the private plan payment amounts reflect actual payments rather than fee-for-service fees from the public program. Specifically, we document cross-carrier variation in prices. There are four carriers (EverCare, Amerigroup, Molina, and Superior HealthPlan) contracted by Texas Medicaid. We estimate their impact on the negotiated price after accounting for provider, procedure, and time fixed effects. The distribution of the estimated carrier fixed effects appears plausible, suggesting that the observed negotiated rate information is high-quality and reflects actual payments. If the payment amounts were just fee-for-service amounts or charges, we would not expect to observe the amount of cross-carrier variation in prices within a provider that we estimate.
Our ability to analyze long-term care spending is limited because our long-term care data is of lower quality than the data for other types of spending and is also only available in the form of summary measures at the annual level from the Personal Summary file. Because of this, and because adults with disabilities in institutional long-term care were not subject to the MMC enrollment mandate, we do not include long-term care spending as part of total healthcare spending. For completeness, in Online Appendix E we present results describing the effects of the reform on the summary measures of long-term care spending in our data, with our findings indicating no effect of the reform on this outcome.
Private plan premium payments include $50 per person per month in administrative costs (Texas Health and Human Services Commission, 2007). Because administrative costs are not observed for public Medicaid enrollees, in examining the effects of the shift to private provision on total Medicaid spending we remove $600 per person-year from private Medicaid premium payments. This allows us to study the effects of private provision on Medicaid spending related to healthcare. These estimates necessarily abstract from any additional spending or savings on administrative costs due to private provision.
An alternative strategy would be to use urban counties where STAR+Plus was not rolled out as control counties. These counties would potentially include the El Paso and Houston areas. Unfortunately, the state rolled out other programs in these cities around this time, making this approach infeasible.
In our analyses we drop all beneficiaries who are enrolled in a private plan at any point before February 2007. These individuals are not excluded from Panel (b) of Figure 1.
While take-up of private plans is sharp, it is not complete for two reasons. First, some groups within the disabled population were exempted from the requirement that they enroll in a private managed care plan. Unfortunately, our data does not allow us to directly identify these exempted groups. Second, upon enrolling in Medicaid, new beneficiaries receive retroactive coverage for any healthcare expenditures they may have incurred in the previous three months. This retroactive coverage is provided by the public Medicaid program, meaning that some new Medicaid beneficiaries (including those in private managed care plans) may be denoted as having at some point been covered under the public program.
The F statistic on the first stage is 998.73.
We define high-value drugs as drugs in the following classes: “Antidiabetic Agents, Insulin”, “Antidiabetic Agents, Sulfonylureas”, “Antidiabetic Agents, Misc”, “Antihyperlipidemic Drugs, NEC”, “Antidepressants”, “Anticonvulsants, Benzodiazepines”, “Tranquilizers/Antipsychotics”, “ASH, Benzodiazepines”, “ACE Inhibitors”, “Alpha-Beta Blockers”, “Beta Blockers”, “Anticoagulants”, “Adrenals and Combinations, NEC”, “Contraceptive Creams/Foams/Devices”, and “Contraceptive, Oral Combinations”. Note that this classification is obviously very incomplete. We chose only drugs that are typically considered obviously high-value for anyone to whom they are prescribed. Other drugs obviously can also provide significant value to patient health.
We define outpatient days as the number of days with at least one outpatient claim.
Online Appendix Table A4 provides regression estimates for additional outpatient outcomes. We observe that, similar to drugs, there is no long-run extensive margin effect on outpatient utilization once we take into account the initial drop in the quarters immediately following the reform. Again, this is not particularly surprising given that 72% of beneficiaries are using some outpatient care during the pre-reform period. Online Appendix Table A4 also shows effects on ED visits. We find a statistically insignificant decrease in ED visits in the short run, and a larger, but still insignificant, decrease in the long-run. We take these results as evidence that the transition to private provision did not increase rates of ED use and may have even lowered them, especially given that the direction of the effect on ED visits is the opposite of the direction of the effect on other types of outpatient care.
We use pre-period data to construct comorbidity measures in order to avoid contamination by the causal effects of the reform on the probability of being diagnosed with chronic conditions.
In Online Appendix Figure A3 and Online Appendix Table A6 we repeat the same analysis, but divide the population into quartiles based on pre-period spending and find similar results.
Event studies for these outcomes are found in Online Appendix Figure A4.
Online Appendix Table D1 shows summary statistics for the included control and treatment zip codes.
This type of spillover is unlikely to be important for the relaxation of the drug cap, as doctors likely write prescriptions without considering the cap (patients just have to deal with the cap when choosing which prescriptions to fill), but it may be important for the shift to managed care plans, which may affect provider behavior for all of their patients rather than just for their patients enrolled in managed care.
The average claim from a beneficiary in a control county is submitted to a provider whose share of claims from control counties is 57%, and the average claim from a beneficiary in a treatment county is submitted to a provider whose share of claims from treatment counties is 90%.
Our data do not allow for the generation of many conventional quality measures, as reporting of diagnoses and procedure codes used to construct these complex measures are reported inconsistently over time and across payers in the other therapy file. Note that this is not a problem for inpatient- and drug-related measures for which reporting is consistent.
The Clinical Classifications Software (CCS) is a classification developed as part of the Healthcare Cost and Utilization Project (HCUP) by the Agency for Healthcare Research and Quality (AHRQ). It groups diagnosis codes into clinically meaningful categories. For our analysis, we used the highest level of aggregation with 18 groups and present results for the 10 most common categories. The CCS classification is available online at https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
While there is no direct financial benefit to private plans for stinting on inpatient care, there could be an indirect benefit in the form of deterring enrollment from beneficiary types who are likely to need inpatient treatment. See Geruso and Layton (2017) for a detailed treatment of these types of contract distortions.
Note that the healthiest groups had larger percentage increases in drug spending, but this is largely driven by very low baseline levels and likely some amount of regression to the mean. Regression to the mean would push against the drug spending increases for the sickest groups.
Contributor Information
Timothy J. Layton, Harvard University and NBER
Nicole Maestas, Harvard University and NBER.
Daniel Prinz, Institute for Fiscal Studies.
Boris Vabson, Harvard University.
REFERENCES
- Aizer Anna, Currie Janet, and Moretti Enrico. 2007. “Does Managed Care Hurt Health? Evidence from Medicaid Mothers.” Review of Economics and Statistics, 89(3): 385–399. [Google Scholar]
- Alexander Diane, and Schnell Molly. 2019. “The Impacts of Physician Payments on Patient Access, Use, and Health.” National Bureau of Economic Research Working Paper 26095.
- Alpert Abby, Duggan Mark, and Hellerstein Judith. 2013. “Perverse Reverse Price Competition: Average Wholesale Prices and Medicaid Pharmaceutical Spending.” Journal of Public Economics, 108(1): 44–62. [Google Scholar]
- Baicker Katherine, Mullainathan Sendhil, and Schwartzstein Joshua. 2015. “Behavioral Hazard in Health Insurance.” Quarterly Journal of Economics, 130(4): 1623–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brot-Goldberg Zarek C. Chandra Amitabh, Handel Benjamin R. and Kolstad Jonathan T.. 2017. “What Does a Deductible Do? The Impact of Cost–Sharing on Health Care Prices, Quantities, and Spending Dynamics.” Quarterly Journal of Economics, 132(3): 1261–1318. [Google Scholar]
- Cabral Marika, Geruso Michael, and Mahoney Neale. 2018. “Do Larger Health Insurance Subsidies Benefit Patients or Producers? Evidence from Medicare Advantage.” American Economic Review, 108(8): 2048–2087. [PMC free article] [PubMed] [Google Scholar]
- Chandra Amitabh, Gruber Jonathan, and McKnight Robin 2010. “Patient Cost-Sharing and Hospitalization Offsets in the Elderly.” American Economic Review, 100(1): 193–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Alice. 2017. “Do the Poor Benefit From More Generous Medicaid Policies?” Mimeo
- Clemens Jeffrey, and Gottlieb Joshua D.. 2014. “Do Physicians’ Financial Incentives Affect Medical Treatment and Patient Health?” American Economic Review, 104(4): 1320–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Congressional Budget Office. 2018. “Exploring the Growth of Medicaid Managed Care” https://www.cbo.gov/publication/54235.
- Council of State Governments Midwest. 2013. “Details of State Limits on Prescriptions for Medicaid Recipients” http://www.csgmidwest.org/policyresearch/documents/scriptlimits.pdf. [Google Scholar]
- Currie Janet, and Fahr John. 2005. “Medicaid Managed Care: Effects on Children’s Medicaid Coverage and Utilization.” Journal of Public Economics, 89(1): 85–108. [Google Scholar]
- Curto Vilsa, Einav Liran, Finkelstein Amy, Levin Jonathan, and Bhattacharya Jay. 2019. “Healthcare Spending and Utilization in Public and Private Medicare.” American Economic Journal: Applied Economics, 11(2): 302–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curto Vilsa, Einav Liran, Levin Jonathan, and Bhattacharya Jay. 2021. “Can Health Insurance Competition Work? Evidence from Medicare Advantage.” Journal of Political Economy, 129(2): 570–606. [Google Scholar]
- Dranove David, Ody Christopher, and Starc Amanda. 2021. “A Dose of Managed Care: Controlling Drug Spending in Medicaid.” American Economic Journal: Applied Economics, 13(1): 170–197. [Google Scholar]
- Duggan Mark, Starc Amanda, and Vabson Boris. 2016. “Who Benefits when the Government Pays More? Pass-Through in the Medicare Advantage Program.” Journal of Public Economics, 141(1): 50–67. [Google Scholar]
- Duggan Mark, and Hayford Tamara. 2013. “Has the Shift to Managed Care Reduced Medicaid Spending? Evidence from State and Local-Level Mandates.” Journal of Policy Analysis and Management, 32(3): 505–535. [DOI] [PubMed] [Google Scholar]
- Duggan Mark, Garthwaite Graig, and Wang Adelina Yanyue. 2021. “Heterogeneity in the Impact of Privatizing Social Insurance: Evidence from California’s Medicaid Program.” National Bureau of Economic Research Working Paper 28944.
- Duggan Mark, Gruber Jonathan, and Vabson Boris. 2018. “The Consequences of Health Care Privatization: Evidence from Medicare Advantage Exits.” American Economic Journal: Economic Policy, 10(1): 153–186. [Google Scholar]
- Duggan Mark, Kearney Melissa S. and Rennane Stephanie. 2015. “The Supplemental Security Income Program.” Economics of Means-Tested Transfer Programs in the United States Vol. 2, 1–58. University of Chicago Press. [Google Scholar]
- Einav Liran, Finkelstein Amy, and Polyakova Maria. 2018. “Private Provision of Social Insurance: Drug-Specific Price Elasticities and Cost Sharing in Medicare Part D.” American Economic Journal: Economic Policy, 10(3): 122–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geruso Michael, and Layton Timothy. 2017. “Selection in Health Insurance Markets and Its Policy Remedies.” Journal of Economic Perspectives, 31(4): 23–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross Tal, Layton Timothy, and Prinz Daniel. 2021. “The Liquidity Sensitivity of Healthcare Consumption: Evidence from Social Security Payments.” American Economic Review: Insights, Forthcoming [DOI] [PMC free article] [PubMed]
- Hackmann Martin B. 2019. “Incentivizing Better Quality of Care: The Role of Medicaid and Competition in the Nursing Home Industry.” American Economic Review, 109(5): 1684–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. 2016. “Medicaid Spending Growth Compared to Other Payers: A Look at the Evidence” https://www.kff.org/report-section/medicaid-spending-growth-compared-to-other-payers-issue-brief/.
- Kaiser Family Foundation. 2017. “The Effects of Premiums and Cost Sharing on Low-Income Populations: Updated Review of Research Findings” https://www.kff.org/medicaid/issue-brief/the-effects-of-premiums-and-cost-sharing-on-low-income-populations-updated-review-of-research-findings/.
- Kaiser Family Foundation. 2018. “Medicaid-to-Medicare Fee Index” https://www.kff.org/medicaid/state-indicator/medicaid-to-medicare-fee-index/.
- Kuziemko Ilyana, Meckel Katherine, and Rossin-Slater Maya. 2018. “Does Managed Care Widen Infant Health Disparities? Evidence from Texas Medicaid.” American Economic Journal: Economic Policy, 10(3): 255–283. [Google Scholar]
- Layton Timothy J. Maestas Nicole, Prinz Daniel, and Vabson Boris. 2019. “Private vs. Public Provision of Social Insurance: Evidence from Medicaid.” National Bureau of Economic Research Disability Research Center Paper NB 18–13.
- Lewin Group. 2004. “Medicaid Managed Care Cost Savings – A Synthesis of 24 Studies” https://leg.mt.gov/content/Committees/Interim/2011-2012/Children-Family/Topics/Medicaid%20Monitoring/lewin-synthesis-of-managed-care-studies.pdf.
- Lewin Group. 2012. “Evaluating Encounter Data Completeness” https://www.ccwdata.org/documents/10280/19002254/evaluating-encounter-data-completeness.pdf.
- Lieberman Daniel A. Polinski Jennifer M. Choudhry Niteesh K. Avorn Jerry, and Fischer Michael A.. 2016. “Medicaid Prescription Limits: Policy Trends and Comparative Impact on Utilization.” BMC Health Services Research, 16(15): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicaid and CHIP Payment and Access Commission. 2019. “Physician Acceptance of New Medicaid Patients” https://www.macpac.gov/wp-content/uploads/2019/01/Physician-Acceptance-of-New-Medicaid-Patients.pdf.
- Newhouse Joseph, and McGuire Thomas. 2014. “How Successful Is Medicare Advantage?” Milbank Quarterly, 92(2): 351–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oostrom Tamar, Einav Liran, and Finkelstein Amy. 2017. “Outpatient Office Wait Times and Quality of Care for Medicaid Patients.” Health Affairs, 36(5): 826–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky Daniel, Richards Michael, Basseyn Simon, Wissoker Douglas, Kenney Genevieve M. Zuckerman Stephen, and Rhodes Karin V.. 2015. “Appointment Availability After Increases in Medicaid Payments for Primary Care.” New England Journal of Medicine, 372(6): 537–545. [DOI] [PubMed] [Google Scholar]
- Silberman Pam, Poley Stephanie, James Kerry, and Slifkin Rebecca. 2002. “Tracking Medicaid Managed Care In Rural Communities: A Fifty-State Follow-Up.” Health Affairs, 21(4): 255–263. [DOI] [PubMed] [Google Scholar]
- Sparer Michael. 2012. “Medicaid Managed Care: Costs, Access, and Quality of Care.” Robert Wood Johnson Foundation Research Synthesis Report 23.
- Starc Amanda, and Town Robert. 2020. “Externalities and Benefit Design in Health Insurance.” Review of Economic Studies, 87(6): 2827–2858. [Google Scholar]
- Texas Health and Human Services Commission. 2007. “Medicaid Managed Care Star+Plus Program Rate Setting State Fiscal Year 2008” https://rad.hhs.texas.gov/sites/rad/files/documents/managed-care/2008/2008-star-plus-actuarial-info.pdf.
- Texas Health and Human Services Commission. 2017. “Texas Medicaid and CHIP in Perspective” https://hhs.texas.gov/sites/default/files/documents/laws-regulations/reports-presentations/2017/medicaid-chip-perspective-11th-edition/11th-edition-complete.pdf.
- Texas Health and Human Services Commission. 2018. “Texas Vendor Drug Program Pharmacy Provider Procedure Manual — Drug Policy” https://www.txvendordrug.com/sites/txvendordrug/files/docs/manuals/drug-policy.pdf.
- Vabson Boris. 2017. “Efficiency Gains Under Incomplete Contracting: Evidence from Medicaid.” Mimeo
- Van Parys Jessica 2015. “How Do Managed Care Plans Reduce Healthcare Costs?” Mimeo
- Zeckhauser Richard. 1970. “Medical Insurance: A Case Study of the Tradeoff Between Risk Spreading and Appropriate Incentives.” Journal of Economic Theory, 2(1): 10–26. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


