Abstract
Background
Frail older adults experience higher rates of adverse health outcomes. Therefore, assessing pre-hospital frailty early in the course of care is essential to identify the most vulnerable patients and determine their risk of deterioration. The Clinical Frailty Scale (CFS) is a frailty assessment tool that evaluates pre-hospital mobility, energy, physical activity, and function to generate a score that ranges from very fit to terminally ill.
Purpose
To synthesize the evidence of the association between the CFS degree and all-cause mortality, all-cause readmission, length of hospital stay, adverse discharge destination, and functional decline in patients >65 years in acute clinical settings.
Design
Systematic review with narrative synthesis.
Methods
Electronic databases (PubMed, EMBASE, CINAHL, Scopus) were searched for prospective or retrospective studies reporting a relationship between pre-hospital frailty according to the CFS and the outcomes of interest from database inception to April 2020.
Results
Our search yielded 756 articles, of which 29 studies were included in this review (15 were at moderate risk and 14 at low risk of bias). The included studies represented 26 cohorts from 25 countries (N = 44166) published between 2011 and 2020. All included studies showed that pre-hospital frailty according to the CFS is an independent predictor of all adverse health outcomes included in the review.
Conclusion
A primary purpose of the CFS is to grade clinically increased risk (i.e. risk stratification). Our results report the accumulated knowledge on the risk-predictive performance of the CFS and highlight the importance of routinely including frailty assessments, such as the CFS, to estimate biological age, improve risk assessments, and assist clinical decision-making in older adults in acute care. Further research into the potential of the CFS and whether implementing the CFS in routine practice will improve care and patients’ quality of life is warranted.
Keywords: clinical frailty scale, risk stratification, acute clinical settings, literature review
Introduction
The functional heterogeneity of the growing older population is not captured by chronological age or morbidity estimates. The concept of frailty may add to the understanding and assessment of the aged individual by indicating biological age. Frailty develops due to age-related decline in multiple physiological systems.1–4 It is a distinctive late-life condition where minor stress factors are associated with adverse health outcomes, including falls, cognitive impairment, disability, hospitalization, institutionalization, and death.4,5 Although frailty is often clinically recognizable, operational criteria vary, and there is no golden standard for its detection.6 Among persons ≥80 years accessing urgent care settings, about 25–50% are frail.4 Assessing frailty early in the course of care is essential to identify the most vulnerable patients,7–9 enabling patients to be directed towards appropriate clinical care and allowing targeted interventions to improve patients’ medical, psychological, and functional capabilities, and prognosis.10,11
The frailty phenotype and the accumulated deficit model are the two dominating frameworks used to conceptualize frailty,3,8 and various assessment tools have been developed to operationalize frailty, for example, judgment-based, summing the number of impairments, and performance measures.1,12,13 The frailty phenotype is operationalized as the presence of at least three out of five criteria (i.e. unintentional weight loss, weakness, poor endurance, slowness, and low physical activity level).1 Alternatively, the accumulated deficit model has been operationalized through the frailty index based on the accumulation of specific deficits (including functional limitations and disabilities, cognitive and sensory impairment, psychosocial variables, and diseases). The Clinical Frailty Scale (CFS) is a judgments-based assessment based on the cumulative deficit model that mixes items such as comorbidity, cognitive impairment, and disability and is validated against the Frailty Index.12,14 The CFS focuses on items such as mobility, balance, the use of walking aids, and the ability to dress, shop, prepare meals, do housework, and handle finances.3,8,12,13 The CFS is routinely used to screen pre-hospital frailty in patients ≥65 years admitted to hospitals via the Emergency Department in several European countries.15,16 The scale is scored so that higher scores mean greater risk, has good criterion validity and inter-rater reliability, and it uses descriptors and figures to stratify older adults according to their level of vulnerability, ranging from very fit (i.e. robust, active, and energetic) to terminally ill.12–15 The degree of frailty generally corresponds to the degree of dementia.13 Mild dementia, for example, corresponds to mild frailty. In both cases, the individual is independent in their activities of daily living (ADLs) but dependent in one or more instrumental activities of daily living (IADLs). When dementia is suspected, although not diagnosed, the CFS assessment should be completed with validated cognitive tests. The CFS was developed to study frailty in older adults. Disability in younger people (including both acquired and life-long) does not have the same relevance for prognosis as for older adults and age-related disability. Numerous previous studies show a strong association between frailty and death in various clinical settings.7,13,16–20 The key to CFS scoring is determining the baseline health state of the older adult, which is especially needed in clinical settings where health can change quickly. Many older adults in the emergency department who were physically fit two weeks previously (i.e. their baseline state) may appear frail while ill.
Two versions of the CFS have been extensively used in studies and clinical practice. Initially, it was scored from one (very fit) to seven (severely frail), and in 2007 it was modified to a nine-point scale to include very severely frail and terminally ill since these groups may need different care plans. By definition, CFS degrees 1–4 denote non-frailty (declining degrees of robustness), whereas degrees ≥5 indicate frailty. Previous systematic reviews have examined the psychometric properties of different frailty assessment tools in various clinical settings.7,16–18,21,22 The CFS shows good accuracy and feasibility, a strong association with mortality, a higher care level,23,24 and good inter-rater reliability.19 Although these literature reviews on frailty suggest that the CFS is a promising frailty assessment tool, none of these have explicitly focused on the CFS in older patients in acute clinical settings in which frailty assessment is fundamental for guiding patient care and helping clinicians determine which interventions will be beneficial or harmful to the older patient. To our knowledge, this is the first systematic review of the research evidence focusing on the ability of the CFS to grade clinically increased risk (risk stratification), i.e. the association between the CFS and clinically relevant outcomes among older patients. Thus, this systematic review aims to synthesize the evidence of the association between pre-hospital frailty as determined by the CFS and all-cause mortality, all-cause readmission, length of hospital stay (LOS), adverse discharge destination (i.e. discharge to nursing homes, residential care, or settings with a higher level of care), and functional decline in patients ≥65 years in acute clinical settings.
Materials and Methods
This systematic review was registered in the prospective international register of systematic reviews PROSPERO (CRD42020178746) and reported in accordance with the Preferred Reporting Items for Systematic Reviews (PRISMA) statement.25
Data Sources and Search Strategy
A computer-aided search strategy in PubMed, EMBASE, CINAHL, and Scopus was performed from database inception to April 2020. Prospective or retrospective observational studies that reported a relationship between the CFS scale and all-cause mortality, readmission, length of hospital stay, adverse discharge destination, and functional decline in older patients in acute care settings were considered. Studies were limited to the English language. All database search strategies are presented in Appendix 1.
Study Selection
A protocol was followed for study selection (Appendix 2). All identified citations were imported into Rayyan (rayyan.qcri.org). After removing duplicates, three authors independently screened the titles and abstracts of the studies and excluded those not meeting the inclusion criteria. Two out of three authors needed to be in favor in order for the study to be included. If the title and abstract seemed to fulfill the inclusion criteria, the full-text version of the study was retrieved and reviewed independently by at least two authors for a final decision on eligibility. Conference abstracts, editorial letters, commentaries, and pilot studies were excluded. Studies were also excluded if they had a cross-sectional design or a pre-test/post-test without predictive analysis, method development studies, qualitative studies, literature reviews, or study protocols not presenting data. Further exclusion criteria were studies investigating patients undergoing elective procedures or those living in long-term care facilities, nursing- or retirement homes.
Quality Assessment
The methodological quality of eligible studies was assessed by the Quality in Prognosis Studies (QUIPS) tool.26 The Swedish Agency for Health Technology Assessment and Assessment of Social Services recommended the QUIPS as a suitable tool for evaluating the risk of bias in studies regarding risk prediction. Each QUIPS domain was evaluated as having a high, moderate, or low risk of bias (RoB). Seven authors were involved in the quality assessment, and at least two out of seven authors independently assessed each eligible study’s methodological quality. All discrepancies were resolved by consensus or by a third author who independently assessed that specific study. To reach a decision, the majority rule was used. For QUIPS, no rules are available that indicate how a study’s overall RoB should be assessed. In this review, we used criteria as suggested by Grooten et al.27 If all domains were assessed as having low RoB or up to one moderate RoB, the study was classified as low RoB. If one or more domains were assessed as having high RoB, or ≥four moderate RoB, this study was classified as high RoB. All studies in between were classified as having moderate RoB. Only studies with an overall low or moderate RoB were included in this review.
Data Extraction and Synthesis
For each study, three authors independently extracted data on study design, participant demographics (sex and age), clinical setting, CFS version (i.e. seven- or the nine-item), CFS cut-offs, the prevalence of pre-hospital frailty, and whether pre-hospital frailty was treated as a discrete, dichotomous, or grouped variable. The association between CFS, all-cause mortality, all-cause readmission within 30 days, LOS, adverse discharge destination, and functional decline was reported as adjusted odds ratio (OR), hazard ratio (HR), and risk ratio (RR), with 95% confidence intervals and presented in a table. All-cause mortality was the most commonly used outcome in the included studies, and we therefore synthesized the estimates (i.e. OR and HR respectively) in two separate Forest Plots using the Statistical Analysis System (SAS) version 9.4 (SAS Institute Inc.).
Results
Literature Flow
We found 756 potentially eligible studies. Fifty-seven studies were assessed for bias after removing duplicates and studies not meeting the inclusion criteria (i.e. wrong publication type, design, population, or outcome). A further 28 studies were excluded due to the high risk of bias. Finally, 29 were included in this review. The PRISMA flowchart is presented in Appendix 3.
Risk of Bias Within Studies
Out of the 57 studies reviewed for RoB using the QUIPS tool, 49% (n = 28) were overall high risk, often due to confounding and measurement bias, rendering study exclusion (Appendix 4). The overall RoB of the included studies is presented in Table 1, out of which 15 were at moderate risk,28–42 and 14 were at low risk.43–56 Common methodological strengths in studies with low or moderate RoB were detailed descriptions of study participants and thorough explanations of potential determinants, confounders, and outcome measurements.
Table 1.
Risk of Bias Within Studies
| Study | Selection Bias | Attrition Bias | Measurement Bias Related to CFS | Measurement Bias Related to Outcomes | Confounding Bias | Analysis/Presentation Bias | The Overall Risk of Bias |
|---|---|---|---|---|---|---|---|
| Anand et al 202028 | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
| Bagshaw et al 201443 | Low | Low | Low | Low | Low | Low | Low |
| Basic & Shanley 201544 | Low | Low | Low | Low | Low | Low | Low |
| Chan et al 201929 | Low | Low | Low | Low | Moderate | Moderate | Moderate |
| Cheung et al 201730 | Moderate | Low | Low | Low | Moderate | Low | Moderate |
| Chong et al 201731 | Moderate | Low | Low | Moderate | Low | Moderate | Moderate |
| Chong et al 201832 | Moderate | Low | Moderate | Low | Low | Moderate | Moderate |
| Chua et al 202045 | Low | Low | Low | Low | Moderate | Low | Low |
| Curtis et al 201846 | Low | Low | Low | Low | Moderate | Low | Low |
| Darvall et al 201947 | Moderate | Low | Low | Low | Moderate | Low | Low |
| Darvall et al 202048 | Moderate | Low | Low | Low | Low | Low | Low |
| Ekerstad et al 201133 | Low | Low | Low | Low | Moderate | Moderate | Moderate |
| Ekerstad et al 201434 | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Ekerstad et al 201835 | Low | Moderate | Low | Moderate | Moderate | Low | Moderate |
| Ellis et al 202036 | Low | Low | Low | Low | Moderate | Moderate | Moderate |
| Evans et al 201949 | Low | Low | Low | Low | Moderate | Low | Low |
| Fernando et al 201937 | Low | Low | Moderate | Moderate | Low | Low | Moderate |
| Flaatten et al 201750 | Low | Low | Low | Low | Low | Low | Low |
| Fronczek et al 201851 | Low | Low | Low | Low | Moderate | Low | Low |
| Guidet et al 202052 | Low | Low | Moderate | Low | Low | Low | Low |
| Lewis et al 201938 | Low | Low | Moderate | Moderate | Low | Low | Moderate |
| Li et al 201839 | Low | Low | Moderate | Low | Moderate | Moderate | Moderate |
| MacKenzie et al 201953 | Low | Low | Low | Low | Low | Low | Low |
| Moore et al 201840 | Low | Low | Low | Moderate | Moderate | Moderate | Moderate |
| Ritt et al 201741 | Low | Low | Moderate | Low | Moderate | Low | Moderate |
| Silva-Obregon et al 202054 | Low | Low | Moderate | Low | Low | Low | Low |
| Sze et al 201755 | Low | Low | Moderate | Low | Low | Low | Low |
| Ticinesi et al 201956 | Low | Low | Moderate | Low | Low | Low | Low |
| Wallis et al 201542 | Low | Moderate | Moderate | Low | Moderate | Low | Moderate |
Notes: Risk of bias (RoB) according to the six domains of the Quality in Prognosis Studies (QUIPS) tool. 21 The overall RoB was determined using the following criteria as previously suggested by Grooten et al 22 If all domains were assessed as having low RoB or up to one moderate RoB, the study was classified as low RoB. If one or more domains were assessed as having high RoB, or ≥four moderate RoB, this study was classified as high RoB. All studies in between were classified as having moderate RoB.
Study Characteristics
The study details and characteristics are presented in Table 2. In total, the included studies represented 26 cohorts from 25 countries (N = 44,166) published between 2011 and 2020. Twenty-one (72%) of the studies were prospective28,31–39,41,43–45,48–53,55 and eight (28%) studies were retrospective.29,30,40,42,46,47,54,56 Sample sizes of the included studies ranged from 11856 to15,613 participants.47 The mean or median age of the samples ranged between 67 years43 and 89 years,31,32 and the proportion of females ranged between 38%54,55 and 70%.31,32,41 The follow-up period ranged from in-hospital (i.e. days or weeks) to the end of follow-up (i.e. years). Ten studies (34%) used the seven-item version,28,30,33–35,38,39,44,46,56 and 19 studies (66%) used the nine-item version of the CFS scale.29,31,32,36,37,40–43,45,47–55 The prevalence of pre-hospital frailty, defined as either CFS ≥4, CFS ≥5, or CFS ≥6, ranged between 14%30 to 91%.36 In all included studies, frail patients were older, more likely to be female, had more comorbid diseases, greater functional dependence, and had fewer social contacts than non-frail patients.
Table 2.
Included Study Details and Characteristics
| Study | Country | Design | Sample | Setting | Age, Years Mean (SD), or Median [IQR] | Female (%) | CFS Version | CFS Cut-Off | Pre-Hospital Frailty (%) |
|---|---|---|---|---|---|---|---|---|---|
| Anand et al 202028 | UK | P | 198 | TC | 79 (6) | 42 | 7-item | CFS ≥5 | 20 |
| Bagshaw et al 201443 | Canada | P | 421 | ICU | 67 (10) | 39 | 9-item | CFS ≥4 | 33 |
| Basic & Shanley 201544 | Australia | P | 2125 | TC | 83 (8) | 60 | 7-item | CFS ≥5 | 89 |
| Chan et al 201929 | Canada | R | 423 | TC | 83 (8) | 63 | 9-item | CFS ≥6 | 83 |
| Cheung et al 201730 | Canada | R | 260 | TC | 77 (8) | 47 | 7-item | CFS ≥6 | 14 |
| Chong et al 2017, 201831,32 | Singapore | P | 206 | TC | 89 (5) | 70 | 9-item | CFS ≥5 | 81 |
| Chua et al 202045 | Singapore | P | 314 | ED | 84 (7) | 60 | 9-item | CFS ≥5 | 65 |
| Curtis et al 201846 | US | R | 1403 | TC | 78 (9) | NS | 7-item | NS | NS |
| Darvall et al 201947 | Australia | R | 15613 | ICU | 85 [82–88] | 47 | 9-item | CFS ≥5 | 40 |
| Darvall et al 20204 | Australia | P | 218 | TC | 74 [69–80] | 45 | 9-item | CFS ≥5 | 28 |
| Ekerstad et al 2011, 2014, 201833–35 | Sweden | P | 307 | TC | 83 (NS); 85 (NS) | 49 | 7-item | CFS ≥5 | 49 |
| Ellis et al 202036 | UK | P | 2254 | ED | 85 (14) | 55 | 9-item | CFS ≥5 | 91 |
| Evans et al 201949 | UK | P | 433 | TC | 83 [77–86]; 87 [83–92] | 48–63 | 9-item | CFS ≥5 | 54 |
| Fernando et al 201937 | Canada | P | 1510 | TC | 73 (7); 80 (8) | 44 | 9-item | CFS ≥5 | 34 |
| Flaatten et al 201750 | ESICM | P | 5021 | ICU | 84 [81–86] | 48 | 9-item | CFS ≥5 | 43 |
| Fronczek et al 201851 | Poland | P | 272 | ICU | 84 [81–87] | 59 | 9-item | CFS ≥5 | 63 |
| Guidet et al 202052 | ESICM | P | 3920 | ICU | 84 [81–87] | 47 | 9-item | CFS ≥5 | 40 |
| Lewis et al 201938 | Australia | P | 899 | ED | 80 (8) | 51 | 7-item | CFS ≥5 | 44 |
| Li et al 201839 | Canada | P | 308 | TC | 75 [65–94] | 45 | 7-item | CFS ≥5 | 22 |
| MacKenzie et al 201953 | Canada | P | 400 | TC | 81 (8) | 57 | 9-item | CFS ≥5 | 79 |
| Moore et al 201840 | UK | R | 924 | TC | 85 (9); 87 (9) | 54–69 | 9-item | CFS ≥5 | 71–84 |
| Ritt et al 201741 | Germany | P | 305 | TC | 85 (7); 82 (6) | 60–70 | 9-item | CFS ≥5 | 72 |
| Silva-Obregon et al 202054 | Spain | R | 285 | ICU | 78 (4) | 38 | 9-item | CFS ≥5 | 19 |
| Sze et al 201755 | UK | P | 265 | TC | 80 [72–86] | 38 | 9-item | CFS ≥4 | 53 |
| Ticinesi et al 201956 | US | R | 118 | TC | 84 (5) | 61 | 7-item | CFS ≥5 | 45 |
| Wallis et al 201542 | UK | R | 5764 | TC | 84 (6) | 56 | 9-item | CFS ≥5 | 57 |
Abbreviations: ESICM (European Society of Intensive Care Medicine) includes Austria, Belgium, Cyprus, Czech Republic, Denmark, France, Germany, Greece, Italy, Libya, the Netherlands, Norway, Poland, Portugal, Romania, Russia, Spain, Sweden, Switzerland, Turkey, United Kingdom; P, prospective; R, retrospective; ICU, intensive care unit; ED, emergency department; TC, tertiary care including specialized medical care, trauma care, surgical care, University Hospitals, or tertiary referral hospitals; NS, not stated; SD, standard deviation; IQR, interquartile range.
The association between frailty as determined by the CFS and all-cause mortality, all-cause readmission, LOS, adverse discharge destination, and functional decline is presented in Table 3. Fourteen studies treated the CFS as a dichotomous variable.30–35,37,38,40,42,44,48,51,54 Seven studies treated the CFS as a discrete variable where each point increase predicted an increased risk or probability of the adverse health outcome of interest.28,36,41,46,49,52,55 Three studies created separate CFS groups (i.e. mild, moderate, or severe frailty),50,53,56 and five studies used mixed approaches.29,39,43,45,47 All included studies adjusted their analysis using different confounders. Twenty-two studies adjusted their analyses for age,28–46,48,50,52 20 studies for sex,28,29,31–36,38–45,47,50,53,54 and 18 studies adjusted for both age and sex.28,29,31–36,38–45,48,50
Table 3.
Association Between CFS Degree and All-Cause Mortality, All-Cause Readmission, LOS, Adverse Discharge Destination, and Functional Decline
| Study | CFS Variable | Control Factors | Outcome (95% CI) |
|---|---|---|---|
| Anand et al 202028 | CFS (discrete)* | Age, sex, comorbidity, cardiovascular risk |
|
| Bagshaw et al 201443 | CFS (dichotomous) CFS groups (i.e. mild, moderate, severe) |
Age, sex, comorbidity, severity of illness, hospital type |
|
| Basic & Shanley 201544 | CFS (dichotomous) | Age, sex, comorbidity |
|
| Chan et al 201929 | CFS (dichotomous) CFS (discrete)* |
Age, sex, time to surgery, mode of anesthesia |
|
| Cheung et al 201730 | CFS (dichotomous) | Age, severity of injury, comorbidity |
|
| Chong et al 201731 | CFS (dichotomous) | Age, sex, comorbidity |
|
| Chong et al 201832 | CFS (dichotomous) | Age, sex, comorbidity |
|
| Chua et al 202045 | CFS (dichotomous) CFS groups (i.e. mild, moderate, severe) |
Age, sex, comorbidity, discharge placement |
|
| Curtis et al 201846 | CFS (discrete)* | Age, consciousness at hospital admission |
|
| Darvall et al 201947 | CFS (dichotomous) CFS (discrete)* |
Sex, region, hospital type, and severity of illness |
|
| Darvall et al 202048 | CFS (dichotomous) | Age, sex, admission source, comorbidity |
|
| Ekerstad et al 201133 | CFS (dichotomous) | Age, sex, previous myocardial infarction, ejection fraction, diabetes, cardiovascular risk, classification of myocardial infarction, comorbidity |
|
| Ekerstad et al 201434 | CFS (dichotomous) | Age, sex, previous myocardial infarction, ejection fraction, diabetes, cardiovascular risk, classification of myocardial infarction, comorbidity |
|
| Ekerstad et al 201835 | CFS (dichotomous) | Age, sex, ejection fraction, cardiovascular risk, comorbidity |
|
| Ellis et al 202036 | CFS (discrete)* | Age, sex, delirium, laboratory tests |
|
| Evans et al 201949 | CFS (discrete)* | Thrombolysis, illness severity |
|
| Fernando et al 201937 | CFS (dichotomous) | Age, long-term care recipient, illness severity, comorbidity |
|
| Flaatten et al 201750 | CFS groups (i.e. mild, moderate, severe) | Age, sex, illness severity |
|
| Fronczek et al 201851 | CFS (dichotomous) | Illness severity, urgency |
|
| Guidet et al 202052 | CFS (discrete)* | Age, admission source, urgency, illness severity, comorbidity |
|
| Lewis et al 201938 | CFS (dichotomous) | Age, sex, comorbidity, urgency |
|
| Li et al 201839 | CFS (discrete)* CFS groups (i.e. mild, moderate, severe) |
Age, sex, type of surgery |
|
| MacKenzie et al 201953 | CFS groups (i.e. mild, moderate, severe) | Sex, admission glucose |
|
| Moore et al 201840 | CFS (dichotomous) | Age, sex, delirium, living alone, discharged to a higher level of care |
|
| Ritt et al 201741 | CFS (discrete)* | Age, sex, comorbidity, disability (IADL/ADL) |
|
| Silva-Obregon et al 202054 | CFS (dichotomous) | Sex, comorbidity, illness severity, treatment intensity, complications |
|
| Sze et al 201755 | CFS (discrete)* | Malnourishment |
|
| Ticinesi et al 201956 | CFS groups (i.e. mild, moderate, severe) | Comorbidity |
|
| Wallis et al 201542 | CFS (dichotomous) | Age, sex, comorbidity |
|
Notes: *CFS used as a discrete variable meant that each point increase in CFS score predicted an increased risk or probability of the adverse health outcome of interest. **Adverse discharge destinations included nursing homes, residential care, hospitalization, or higher level of care.
Abbreviation: CI, confidence interval.
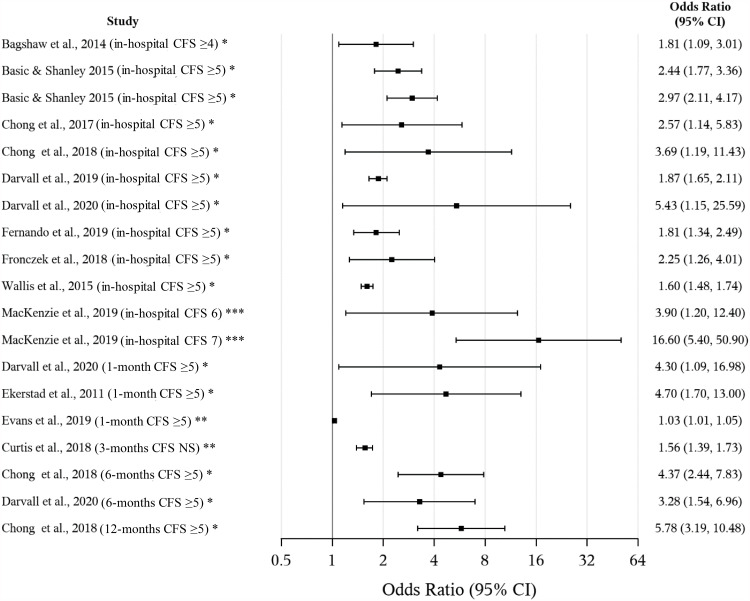
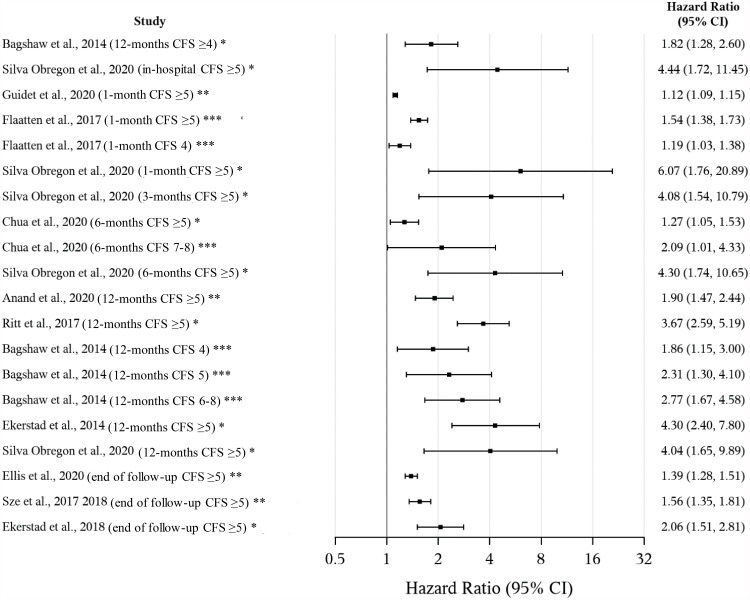
Association Between CFS and All-Cause Mortality
The difference in odds of all-cause mortality between frail and non-frail patients and the risk of all-cause mortality in-hospital, at 1-, 3-, 6-, 12- months, and end of follow-up are presented in Figure 1. Ten studies31–33,37,43,44,46–48,51,53 reported a significant difference in the odds of in-hospital mortality, with the largest difference reported by MacKenzie et al53 (OR 16.6, 95% CI 5.4–50.9), and Darvall et al48 (OR 5.43, 95% CI 1.15–25.59). At 1-month follow-up, the largest difference was reported by Ekerstad et al33 (OR 4.7, 95% CI 1.7–13.0), at 6 and 12 months, the largest difference was reported by Chong et al32 (OR 4.37, 95% CI 2.44–7.83 and OR 5.78, 95% CI 3.19–10.48). In two studies, a single point increase in the CFS scale showed an increased likelihood of dying at both 1-month (OR 1.03, 95% CI 1.01–1.05),49 and 3-months (OR 1.56, 95% CI 1.39–1.73).46 The increased risk of all-cause mortality in-hospital, within 1-, 3- 6-, 12-months, and end of follow-up are presented in Figure 2. Silva-Obregón et al54 showed that frail patients suffered more than a four-fold increased risk of dying in hospital (HR 4.44, 95% CI 1.72–11.45), a six-fold increased risk within 1 month (HR 6.07, 95% CI 1.76–20.89), and a four-fold increased risk within 3 months (HR 4.08, 95% CI 1.54–10.79), and 6 months (HR 4.30, 95% CI 1.74–10.65). Nine studies28,34–36,41,43,54–56 reported that pre-hospital frailty increased the risk of dying within 12 months or at the end of follow-up, with the largest risk reported by Ekerstad et al34 (HR 4.3, 95% CI 2.4–7.8). A single point increase in the CFS showed a nearly four-fold increased risk of dying within 12 months or at the end of follow-up as reported by Ritt et al41 (HR 3.76, 95% CI 2.59–5.19), and a nearly two-fold increase in risk as reported by Anand et al28 (HR 1.72, 95% CI 1.37–2.16).
Figure 1.
The adjusted difference in the odds of all-cause mortality between frail and non-frail patients (in-hospital, within 1-, 3-, 6-, 12-months, or end of follow-up). *CFS was treated as a dichotomous variable, **as a discrete variable, ***or a grouped variable in the analysis.
Figure 2.
The adjusted risk of all-cause mortality (in-hospital, within 1-, 3-, 6-, 12-months, or end of follow-up). *CFS was treated as a dichotomous variable, **as a discrete variable, ***or a grouped variable in the analysis.
Association Between CFS and All-Cause Readmission
Four studies36,37,39,48 showed a significant difference in the odds of all-cause readmission within 30 days between frail and non-frail patients, with the most significant difference reported by Li et al39 (OR 3.97, 95% CI 1.00–15.78). In the study by Ellis et al36 an additional point increase on the CFS scale increased the risk of hospital readmission (HR 1.26, 95% CI 1.17–1.37).
Association Between CFS and LOS
Three studies40,42,53 showed a significant difference in the odds of an extended LOS between frail and non-frail patients, with the most significant difference reported by MacKenzie et al53 (OR 3.6, 95% CI 1.8–7.3). Two studies29,36 showed a dose-response relationship between increasing pre-hospital frailty and LOS, with the most significant risk observed by Chan et al29 (RR 2.2, 95% CI 2.0–2.4).
Association Between CFS and Adverse Discharge Destination
Six studies36,42,43,46–48 showed a significant difference in the odds of adverse discharge destination between frail and non-frail participants, with the largest difference reported by Darvall et al48 (OR 3.70, 95% CI 1.46–9.41), as well as a nearly three-fold increased risk (RR 2.66, 95% CI 1.15–6.13). Ellis et al36 reported that a single point increase in the CFS increased the odds of adverse discharge destination by 30% (OR 1.30, 95% CI 1.16–1.47).
Association Between CFS and Functional Decline
Two studies32,43 reported a difference in the odds of functional decline at 12 months post-discharge between frail and non-frail patients, with the largest difference reported by Bagshaw et al43 (OR 2.25, 95% CI 1.03–4.89).
Association Between CFS and Composite Outcome
Six studies reported differences in odds of various composite outcomes between frail and non-frail patients.29,32,33,35,38,39 A difference in the odds of death or discharge to a nursing home or long-term facility was reported by Chan et al29 (OR 23, 95% CI 3.0–173.5), Chong et al32 (OR 3.14, 95% CI 1.94–5.07 and OR 3.69, 95% CI 2.31–5.88), and Ekerstad et al33 (OR 2.2, 95% CI 1.3–3.7). Lewis et al38 reported a difference in the odds of death, poor or fair self-reported health, poor or fair quality of life, new presentation to an emergency department, or need for community services (OR 2.20, 95% CI 1.55–3.12). Li et al39 reported a difference in the odds of being readmitted or deceased one-month post-discharge (OR 4.51, 95% CI 1.13–17.94), and a single-point increase in the CFS more than tripled the odds (OR 3.27, 95% CI 1.32–8.12).
Discussion
The explicit purpose of this systematic review was to study the ability of the CFS to grade clinically increased risk (risk stratification), i.e. the association between the CFS and clinically relevant outcomes in patients >65 years in acute clinical settings. Twenty-nine studies were included out of which 15 were at moderate risk of RoB,28–42 and 14 at low risk of RoB.43–56 Our results show that there is a significant difference between frail and non-frail patients in the risk of mortality in-hospital, at 1-, 3-, 6-, and 12 months, and at the end of follow-up (i.e. 6.7 years) and that the CFS is a strong and independent predictor of mortality at all time-points. Our result also showed a significant difference in the odds of all-cause readmission within 30 days, extended LOS, adverse discharge destination, and functional decline between pre-hospital frail and non-frail patients as defined by the CFS, and CFS was an independent risk factor. Taken together, this is a strong indication that the CFS provides robust risk predictions in patients >65 years in acute clinical settings.
Although the CFS is commonly used in research and clinical care, there is currently only one previous scoping review showing that it is widely used in multiple settings and has a good predictive ability for mortality, length of stay, and functional decline.7 The results of this review, also judging the bias in the included studies, confirms these results and further support the use of the CFS in clinical practice.
Since the population of frail older adults is growing and healthcare utilization among this population is increasing, prevention of frailty, maintenance, or reduction of the level of frailty should be prioritized. Dementia confers a unique challenge, although the degree of frailty generally corresponds to the degree of dementia.13 When dementia is suspected, although not diagnosed, the CFS assessment should be completed with cognitive tests. There is a pressing need to understand how a population with potentially complex medical, physical, and psychosocial concerns could be supported. Therefore, an assessment tool with good clinimetric properties is needed. The CFS provides a simple clinical measure of biological age, combining comorbidity, disability, and cognitive impairment. The use of the CFS to stratify risk is not particularly time-consuming and is relatively easy to implement in daily clinical practice.7,8,12 Although one primary purpose of the CFS is risk stratification, it may also be used as a screening tool to identify frail patients needing further geriatric evaluation, i.e. comprehensive geriatric assessment (CGA). In addition, reliable information on long-term prognosis may improve informed decision-making on the individual level for patients and their families.
It is beyond the scope of this review to compare the CFS with other frailty instruments, as well as to comprehensively describe the different concepts or models of frailty, including multidimensionality and different components or domains. Measuring the level of frailty may be challenging for several reasons. Multiple theoretical and operational frailty definitions have been suggested in the last decade,21,22, and there is no international standard measurement for frailty.6,9,18 Different frailty models (and corresponding instruments) serve different purposes and it is important to point out that measuring frailty has several objectives requiring different forms of assessment. Some measures are better for population-level frailty screening (e.g. self-reported questionnaires), whereas others are best suited for clinical assessment.9 In addition, there are some measures that are better suited to direct the patient toward a more complex multidimensional, interdisciplinary diagnostic process. In contrast, others are best suited to describe health status changes over time. In a recent consensus document from the European Society of Cardiology, the following was stated:
Therefore, albeit under the same definition, these two different concepts (accumulated deficit-model and phenotype-model) currently recognize entirely different subjects and, more importantly, generate different clinical and prognostic implications that may be considered as complementary.57
Frail patients pose particular challenges, have higher rates of adverse outcomes, and have complex healthcare needs.4,19 In several hospitals in Sweden, the CFS scale is routinely included in the assessment of all patients older than 65 years in emergency departments and other acute settings. A primary purpose of the CFS is to grade clinically increased risk (i.e. risk stratification), and in these contexts, the CFS is generally used to identify patients presenting an increased risk profile that warrants comprehensive assessments allowing care plans to be more tailored and holistic.12 Our results indicate that the CFS is a robust tool for predicting adverse health outcomes and that it is essential to report the accumulated knowledge on the risk-predictive performance of CFS in a scientific review that can guide clinical decision-making. Since the CFS has been validated against the Frailty Index, and the correlation between the two scales is high,14 it is argued that the CFS also can be used to identify older patients’ capacity to accumulate deficits which lies beyond categorically defining the presence/absence of frailty or risk of frailty.6 Our results report the accumulated knowledge on the risk-predictive performance of CFS and highlight the importance of routinely including frailty assessments, such as the CFS, to estimate biological age, improve risk assessments, and assist clinical decision-making in older adults in acute care.
Limitations
Firstly, there was large variability between the studies regarding how the CFS was used in the analysis (i.e. dichotomous, discrete, grouped), controlling factors, and study settings. Therefore, we chose to present our comprehensive overview of the research evidence in a narrative synthesis using tables and figures instead of performing a meta-analysis, which would have strengthened our results. Also, the lack of adjustment for psychosocial factors and polypharmacy across studies might have influenced our results. Although most studies controlled for age, frail patients tend to be older than non-frail patients, and the risk of mortality generally increases with advancing age which might have affected the predictive performance of CFS. Frail patients might not receive the same level of care/care interventions as non-frail patients, which might influence the predictiveness of the CFS. However, there are studies that show that although the type of therapy or level of care is used as a controlling factor in the analysis, the predictive ability of the CFS remains unchanged.20,24,56,58 Secondly, we used the QIUPS tool as recommended by the Swedish Agency for Health Technology Assessment and Assessment of Social Services. It is possible that utilizing another quality assessment tool would have influenced our final sample of included studies. Instead of using GRADE to weigh the results of the included studies against each other, three authors independently screened and extracted the data. Seven authors independently assessed the risk of bias using the QUIPS tool. In addition, the data extracted from the included studies were reviewed and discussed by the authors, who all have extensive clinical and scientific experience of frailty and the use of different frailty assessment tools. Thirdly, the literature review was stopped in 2020 with the plan of publishing in 2021. Due to the Covid-19 pandemic, the methodological quality assessment of eligible studies and publication of the final literature review was delayed. Including research studies published after 2020 would have further strengthened our literature review.
Conclusion
A primary purpose of the CFS is to grade clinically increased risk (i.e. risk stratification). Our results report the accumulated knowledge on the risk-predictive performance of CFS and highlight the importance of routinely including frailty assessments, such as the CFS, to estimate biological age, improve risk assessments, and assist clinical decision-making in older adults in acute care. This review revealed that frailty, according to the CFS, is a strong predictor of adverse health outcomes in patients >65 years in acute settings. Further research into the potential of the CFS and whether implementing the CFS in routine clinical practice will improve care outcomes and patients’ quality of life is warranted. Due to the strong association between frailty according to the CFS and adverse health outcomes, more research on acute management and rehabilitation potential in frail older adults is needed.
Disclosure
Dr Joakim Alfredsson reports personal fees from Boehringer Ingelheim, MSD, and Astra Zeneca, outside the submitted work. Dr Tommy Cederholm reports personal fees from Nutricia, Nestle, Fresenius-Kabi, Abbott, and Pfizer, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.Fried LP, Tangen CM, Walston J, et al Frailty in older adults: evidence for a phenotype. J Gerontol a Biol Sci Med Sci. 2001;56:M146–M157. [DOI] [PubMed] [Google Scholar]
- 2.Walston J, Hadley EC, Ferrucci L, et al Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on aging research conference on frailty in older adults. J Am Geriatr Soc. 2006;54:991–1001. doi: 10.1111/j.1532-5415.2006.00745.x [DOI] [PubMed] [Google Scholar]
- 3.Rockwood K, Andrew M, Mitnitski A, et al A comparison of two approaches to measuring frailty in elderly people. J Gerontol a Biol Sci Med Sci. 2007;62(7):738–743. doi: 10.1093/gerona/62.7.738 [DOI] [PubMed] [Google Scholar]
- 4.Clegg A, Young J, Iliffe S, et al Frailty in elderly people. Lancet. 2013;9868:752–762. doi: 10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hopkins SA, Bentley A, Phillips V, et al Advance care plans and hospitalized frail older adults: a systematic review. BMJ Support Palliat Care. 2020;10:164–174. doi: 10.1136/bmjspcare-2019-002093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cesari M, Gambassi G, Abellan van Kan G, et al The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing. 2014;43(1):10–12. [DOI] [PubMed] [Google Scholar]
- 7.Church S, Rogers E, Rockwood K, et al A scoping review of the Clinical Frailty Scale. BMC Geriatr. 2020;20:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Theou O, Brothers TD, Mitnitski A, et al Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all‐cause mortality. J Am Geriatr Soc. 2013;61:1537–1551. [DOI] [PubMed] [Google Scholar]
- 9.Rockwood K, Theou O, Mitnitski A. What are frailty instruments for? Age Ageing. 2015;44(4):545–547. [DOI] [PubMed] [Google Scholar]
- 10.Sirois MJ, Griffith L, Perry J, et al Measuring frailty can help emergency departments identify independent seniors at risk of functional decline after minor injuries. J Gerontol a Biol Sci Med Sci. 2017;72(1):68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Belga S, Majumdar SR, Kahlon S, et al Comparing three different measures of frailty in medical inpatients: multicenter prospective cohort study examining the 30‐day risk of readmission or death. J Hosp Med. 2016;11:556–562. [DOI] [PubMed] [Google Scholar]
- 12.Rockwood K, Song X, MacKnight C, et al A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rockwood K, Theou O. Using the clinical frailty scale in allocating scarce health care resources. Can Gertartr J. 2020;23:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreno-Ariño M, Torrente Jiménez I, Cartanyà Gutiérrez A, et al Assessing the strengths and weaknesses of the Clinical Frailty Scale through correlation with a frailty index. Aging Clin Exp Res. 2020;32(11):2225–2232. doi: 10.1007/s40520-019-01450-w [DOI] [PubMed] [Google Scholar]
- 15.Romero-Ortuno R, Forsyth DR, Wilson KJ, et al The association of geriatric syndromes with hospital outcomes. J Hosp Med. 2017;12:83–89. doi: 10.12788/jhm.2685 [DOI] [PubMed] [Google Scholar]
- 16.Cords CI, Spronk I, Mattace-Raso FU, et al The feasibility and reliability of frailty assessment tools applicable in acute in-hospital trauma patients: a systematic review. J Trauma Acute Care Surg. 2022;92:615–626. doi: 10.1097/TA.0000000000003472 [DOI] [PubMed] [Google Scholar]
- 17.Aucoin SD, Hao M, Sohi R, et al Accuracy and feasibility of clinically applied frailty instruments before surgery: a systematic review and meta-analysis. Anesthesiology. 2020;133:78–95. doi: 10.1097/ALN.0000000000003257 [DOI] [PubMed] [Google Scholar]
- 18.Dent E, Kowal P, Hoogendijk EO, et al Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10. doi: 10.1016/j.ejim.2016.03.007 [DOI] [PubMed] [Google Scholar]
- 19.Pugh RJ, Ellison A, Pye K, et al Feasibility and reliability of frailty assessment in the critically ill: a systematic review. Crit Care. 2018;22:1–11. doi: 10.1186/s13054-017-1923-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ekerstad N, Javadzadeh D, Alexander K, et al Clinical Frailty Scale-classes are independently associated with six-month mortality for patients after acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2022;11:89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sutton JL, Gould RL, Daley S, et al Psychometric properties of multicomponent tools designed to assess frailty in older adults: a systematic review. BMC Geriatr. 2016;16:55. doi: 10.1186/s12877-016-0225-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Vries NM, Staal JB, Van Ravensberg CD, et al Outcome instruments to measure frailty: a systematic review. Ageing Res Rev. 2011;10:104–114. doi: 10.1016/j.arr.2010.09.001 [DOI] [PubMed] [Google Scholar]
- 23.Ritt M, Bollheimer LC, Sieber CC, et al Prediction of one-year mortality by five different frailty instruments: a comparative study in hospitalized geriatric patients. Arch Gerontol Geriat. 2016;66:66–72. doi: 10.1016/j.archger.2016.05.004 [DOI] [PubMed] [Google Scholar]
- 24.Leiner T, Nemeth D, Hegyi P, et al Frailty and emergency surgery: results of a systematic review and meta-analysis. Front Med. 2022;9:811524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Page MJ, McKenzie JE, Bossuyt PM, et al The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):1–11. doi: 10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hayden JA, van der Windt DA, Cartwright JL, et al Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. doi: 10.7326/0003-4819-158-4-201302190-00009 [DOI] [PubMed] [Google Scholar]
- 27.Grooten WJA, Tseli E, Äng BO, et al Elaborating on the assessment of the risk of bias in prognostic studies in pain rehabilitation using QUIPS; aspects of interrater agreement. Diag Prog Res. 2019;3:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anand A, Cudmore S, Robertson S, et al Frailty assessment and risk prediction by GRACE score in older patients with acute myocardial infarction. BMC Geriatr. 2020;20(1):1–9. doi: 10.1186/s12877-020-1500-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan S, Wong EK, Ward SE, et al The predictive value of the clinical frailty scale on discharge destination and complications in older Hip fracture patients. J Orthop Trauma. 2019;33:497–502. doi: 10.1097/BOT.0000000000001518 [DOI] [PubMed] [Google Scholar]
- 30.Cheung A, Haas B, Ringer TJ, et al Canadian study of health and aging clinical frailty scale: does it predict adverse outcomes among geriatric trauma patients? JACS. 2017;225:658–665. [DOI] [PubMed] [Google Scholar]
- 31.Chong E, Ho E, Baldevarona-Llego J, et al Frailty and risk of adverse outcomes in hospitalized older adults: a comparison of different frailty measures. J Am Med Dir Assoc. 2017;18(7):638–e7. doi: 10.1016/j.jamda.2017.04.011 [DOI] [PubMed] [Google Scholar]
- 32.Chong E, Ho E, Baldevarona-Llego J, et al Frailty in hospitalized older adults: comparing different frailty measures in predicting short-and long-term patient outcomes. J Am Med Dir Assoc. 2018;19:450–457. doi: 10.1016/j.jamda.2017.10.006 [DOI] [PubMed] [Google Scholar]
- 33.Ekerstad N, Swahn E, Janzon M, et al Frailty is independently associated with short-term outcomes for elderly patients with non–ST-segment elevation myocardial infarction. Circulation. 2011;124:2397–2404. doi: 10.1161/CIRCULATIONAHA.111.025452 [DOI] [PubMed] [Google Scholar]
- 34.Ekerstad N, Swahn E, Janzon M, et al Frailty is independently associated with 1-year mortality for elderly patients with non-ST-segment elevation myocardial infarction. Eur J Prev Cardiol. 2014;21:1216–1224. doi: 10.1177/2047487313490257 [DOI] [PubMed] [Google Scholar]
- 35.Ekerstad N, Pettersson S, Alexander K, et al Frailty as an instrument for evaluation of elderly patients with non-ST-segment elevation myocardial infarction: a follow-up after more than 5 years. Eur J Prev Cardiol. 2018;25(17):1813–1821. doi: 10.1177/2047487318799438 [DOI] [PubMed] [Google Scholar]
- 36.Ellis HL, Wan B, Yeung M, et al Complementing chronic frailty assessment at hospital admission with an electronic frailty index (FI-Laboratory) comprising routine blood test results. CMAJ. 2020;192:E3–E8. doi: 10.1503/cmaj.190952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fernando SM, McIsaac DI, Perry JJ, et al Frailty and associated outcomes and resource utilization among older ICU patients with suspected infection. Crit Care Med. 2019;47:e669–e676. doi: 10.1097/CCM.0000000000003831 [DOI] [PubMed] [Google Scholar]
- 38.Lewis ET, Dent E, Alkhouri H, et al Which frailty scale for patients admitted via emergency department? A cohort study. Arch Gerontol Geriatr. 2019;80:104–114. doi: 10.1016/j.archger.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 39.Li Y, Pederson JL, Churchill TA, et al Impact of frailty on outcomes after discharge in older surgical patients: a prospective cohort study. CMAJ. 2018;190:E184–E190. doi: 10.1503/cmaj.161403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moore G, Hartley P, Romero‐Ortuno R. Health and social factors associated with a delayed discharge amongst inpatients in acute geriatric wards: a retrospective observational study. Geriatr Gerontol Int. 2018;18:530–537. doi: 10.1111/ggi.13212 [DOI] [PubMed] [Google Scholar]
- 41.Ritt M, Ritt JI, Sieber CC, et al Comparing the predictive accuracy of frailty, comorbidity, and disability for mortality: a 1-year follow-up in patients hospitalized in geriatric wards. Clin Interv Aging. 2017;12:293–304. doi: 10.2147/CIA.S124342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wallis SJ, Wall JBRWS, Biram RWS, et al Association of the clinical frailty scale with hospital outcomes. QJM. 2015;108:943–949. doi: 10.1093/qjmed/hcv066 [DOI] [PubMed] [Google Scholar]
- 43.Bagshaw SM, Stelfox HT, McDermid RC, et al Association between frailty and short-and long-term outcomes among critically ill patients: a multicenter prospective cohort study. CMAJ. 2014;186:E95–E102. doi: 10.1503/cmaj.130639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Basic D, Shanley C. Frailty in an older inpatient population: using the clinical frailty scale to predict patient outcomes. JAH. 2015;27:670–685. doi: 10.1177/0898264314558202 [DOI] [PubMed] [Google Scholar]
- 45.Chua XY, Toh S, Wei K, et al Evaluation of clinical frailty screening in geriatric acute care. J Eval Clin Pract. 2020;26:35–41. doi: 10.1111/jep.13096 [DOI] [PubMed] [Google Scholar]
- 46.Curtis E, Romanowski K, Sen S, et al Frailty score on admission predicts mortality and discharge disposition in elderly trauma patients over the age of 65 y. J Surg Res. 2018;230:13–19. doi: 10.1016/j.jss.2018.04.017 [DOI] [PubMed] [Google Scholar]
- 47.Darvall JN, Bellomo R, Paul E, et al Frailty in very old critically ill patients in Australia and New Zealand: a population‐based cohort study. Med J Aust. 2019;211:318–323. doi: 10.5694/mja2.50329 [DOI] [PubMed] [Google Scholar]
- 48.Darvall JN, Loth J, Bose T, et al Accuracy of the Clinical Frailty Scale for perioperative frailty screening: a prospective observational study. Can J Anaesth. 2020;67:694–705. doi: 10.1007/s12630-020-01610-x [DOI] [PubMed] [Google Scholar]
- 49.Evans NR, Wall J, To B, et al Clinical frailty independently predicts early mortality after ischaemic stroke. Age Ageing. 2020;49:588–591. doi: 10.1093/ageing/afaa004 [DOI] [PubMed] [Google Scholar]
- 50.Flaatten H, De Lange DW, Morandi A, et al The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017;43:1820–1828. doi: 10.1007/s00134-017-4940-8 [DOI] [PubMed] [Google Scholar]
- 51.Fronczek J, Polok K, Nowak-Kózka I, et al Frailty increases mortality among patients ≥80 years old treated in Polish ICUs. Anaesthesiol Intensive Ther. 2018;50:245–251. doi: 10.5603/AIT.a2018.0032 [DOI] [PubMed] [Google Scholar]
- 52.Guidet B, De Lange DW, Boumendil A, et al The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Medicine. 2020;46(1):57–69. doi: 10.1007/s00134-019-05853-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.MacKenzie HT, Tugwell B, Rockwood K, et al Frailty and diabetes in older hospitalized adults: the case for routine frailty assessment. Can J Diabetes. 2020;44(3):241–245. doi: 10.1016/j.jcjd.2019.07.001 [DOI] [PubMed] [Google Scholar]
- 54.Silva-Obregón JA, Quintana-Díaz M, Saboya-Sánchez S, et al Frailty as a predictor of short-and long-term mortality in critically ill older medical patients. J Crit Care. 2020;55:79–85. [DOI] [PubMed] [Google Scholar]
- 55.Sze S, Zhang J, Pellicori P, et al Prognostic value of simple frailty and malnutrition screening tools in patients with acute heart failure due to left ventricular systolic dysfunction. Clin Res Cardiol. 2017;106:533–541. [DOI] [PubMed] [Google Scholar]
- 56.Ticinesi A, Nouvenne A, Prati B, et al Profiling the hospital-dependent patient in a large academic hospital: an observational study. Eur J Intern Med. 2019;64:41–47. [DOI] [PubMed] [Google Scholar]
- 57.Richter D, Guasti L, Walker D, et al Frailty in cardiology: definition, assessment and clinical implications for general cardiology. A consensus document of the Council for Cardiology Practice (CCP), Association for Acute Cardio Vascular Care (ACVC), Association of Cardiovascular Nursing and Allied Professions (ACNAP), European Association of Preventive Cardiology (EAPC), European Heart Rhythm Association (EHRA), Council on Valvular Heart Diseases (VHD), Council on Hypertension (CHT), Council of Cardio-Oncology (CCO), Working Group (WG). Eur Journal Prev Car. 2022;29:216–227. [DOI] [PubMed] [Google Scholar]
- 58.Dodson JA, Hajduk AM, Geda M, et al Predicting 6-month mortality for older adults hospitalized with acute myocardial infarction. Ann Intern Med. 2020;172:12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]