Introduction
Micro-melanomas, or melanomas < 2 mm in diameter, are increasingly reported making screening methods like the ABCD(E) acronym outdated. Early detection of melanoma remains the utmost important prognostic factor, therefore understanding how to utilize different diagnostic tools is necessary to optimize detection of melanoma at its earliest, most treatable stage. Using a combination of imaging and molecular techniques, we detected and confirmed a micro-melanoma in situ measuring 0.65 mm in diameter.
Case Presentation
A 61-year-old female with no prior history of skin cancer presented for a skin examination. Clinical examination of her right cheek revealed a tiny, hyperpigmented dot not previously noticed by the patient. Dermoscopy showed sun-damaged skin with a dark brown macule and asymmetric perifollicular hyperpigmentation. Reflectance confocal microscopy (RCM) revealed dendritic cells concentrated around a single hair follicle, consistent with folliculotropism (Figure 1). The final diameter incorporated the farthest-reaching dendritic cell projections measuring at 0.65 mm. Initial histopathology showed a solar lentigo without atypia. Due to discordance with clinical-dermoscopic concern, deeper sections were requested and stained with Melan-A and SOX10 revealing irregular and heterogenous melanocytic nests and single melanocytosis, consistent with melanoma in situ (MIS) (Figure 2). Additionally, the sample underwent a diagnostic 23-gene expression profile (GEP) test which returned a positive result (suggestive of malignancy). National Comprehensive Cancer Network (NCCN) guidelines make note of multiple ancillary diagnostic tests, which includes diagnostic GEP, that can help to differentiate equivocal melanocytic lesions and may be useful in cases of clinical discordance [1]. In the context of these ancillary findings final diagnosis of MIS was achieved. For control, four 5×5 mm RCM image sets of the epidermis, dermal-epidermal junction and upper dermis and two 2-mm punch biopsies were completed adjacent to the biopsy site in the most pigmented areas and no atypical features were found confirming the absence of residual tumor in nearby locations.
Figure 1.
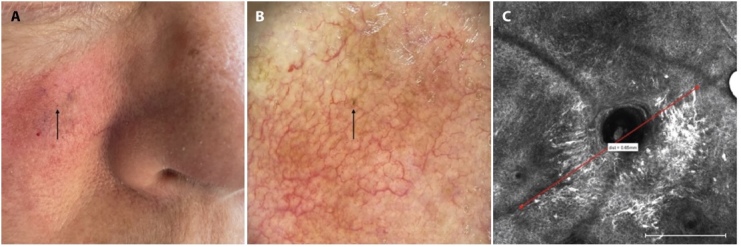
(A) Clinical image of pigmented skin lesion (arrow). (B) Zoomed digital dermoscopy image of the pigmented skin lesion presenting with folliculotropism (circle). Sites of control punch biopsies in areas of increased pigmentation (triangles). (C) Reflectance confocal microscopy image (0.75 mm × 0.75 mm, measuring line bottom right corner: 0.25 mm) with presence of folliculotropism of pleomorphic melanocytes. Melanoma in-situ maximal diameter measured: 0.65 mm.
Figure 2.
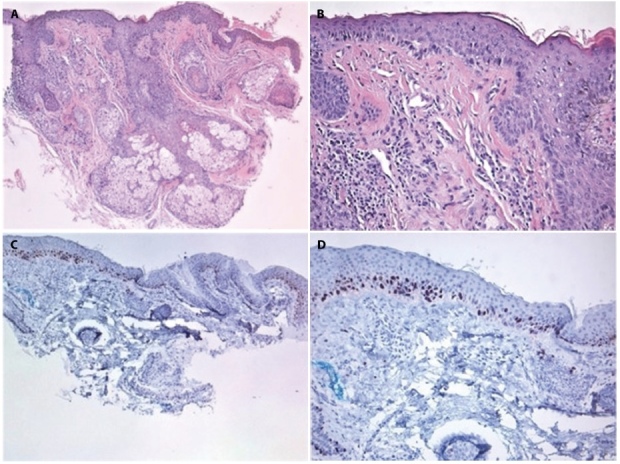
Histopathology of the smallest reported melanoma. (A, B) H&E staining (A: 5X and B: 20X) showed an increased density of mostly solitary melanocytes at the dermal-epidermal junction. (C, D) SOX10 immunostaining (C: 5X and D: 20X) showed a continuous proliferation of melanocytes at the dermal-epidermal junction, consistent with melanoma in-situ.
Conclusions
With the widespread adoption of dermoscopy, increasing numbers of micro-melanomas have been identified. Relying on dermoscopy alone, the smallest melanoma recorded measured at 1.3 mm [2] and another case enhanced by total-body imaging system reported a 0.9 mm diameter melanoma [3]. RCM is also a valuable second-level examination tool that combined with digital follow-up facilitates recognition of early-stage disease. Some argue that such small lesions cannot be malignant and investing in its detection is wasteful, however Regio Pereira et al evaluated 86 melanomas <5 mm in diameter which found 44% were invasive melanomas [4] highlighting the importance of investigating suspicious lesions regardless of size. Although our case demonstrated suspicious dermoscopy and RCM findings, initial histopathology reports were benign. Recognizing histopathology has limitations due to sampling bias, potentially missing up to 10% of melanomas [5], we requested additional staining and 23-GEP testing that ultimately revealed a diagnosis of MIS with a diameter of 0.65 mm. This case attests to the heightened diagnostic capabilities of multiple imaging and molecular tools when used in conjunction to confirm an early melanoma, which may result in better cosmetic, financial and patient morbidity.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Fried L, Tan A, Bajaj S, Liebman TN, Polsky D, Stein JA. Technological advances for the detection of melanoma: Advances in molecular techniques. J Am Acad Dermatol. 2020;83(4):996–1004. doi: 10.1016/j.jaad.2020.03.122. [DOI] [PubMed] [Google Scholar]
- 2.Saleh K. Dermoscopy of a Lentigo Maligna Less Than 1.5 mm in Diameter. Dermatol Pract Concept. 2021;11(2):e2021027. doi: 10.5826/dpc.1102a27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akay BN, Okcu Heper A, Clark S, et al. Dermatoscopy of a melanoma less than one millimeter in diameter. Int J Dermatol. 2017;56(12):1498–1499. doi: 10.1111/ijd.13728. [DOI] [PubMed] [Google Scholar]
- 4.Regio Pereira A, Corral-Forteza M, Collgros H, et al. Dermoscopic features and screening strategies for the detection of small-diameter melanomas. Clin Exp Dermatol. 2022;47(5):932–941. doi: 10.1111/ced.15094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elmore JG, Barnhill RL, Elder DE, et al. Pathologists’ diagnosis of invasive melanoma and melanocytic proliferations: observer accuracy and reproducibility study. BMJ. 2017;357:j2813. doi: 10.1136/bmj.j2813. [DOI] [PMC free article] [PubMed] [Google Scholar]


