Introduction
Pediatric acral dermatitis represents a diagnostic challenge, as it can have various origins [1], including SARS-CoV-2 infection [2], that can cause acro-ischemic lesions, also called pseudo-chilblain or pernio-like lesions, or “COVID toe”. Due to the mild systemic symptoms, the role of dermatologists is fundamental in the early recognition of the infection and the consequent pandemic containment [2].
We described our real-life experience with teledermatology management of 6 pediatric acral dermatites during the first COVID-19 pandemic. Telemedicine-assisted consultations were conducted to collect anamnestic history and perform skin examination; skin lesions images were independently analyzed by three different dermatologists (GLC, ZE, GF).
Cases Presentation
Case 1: a 6-year-old boy with asymptomatic and symmetrical shiny erythematous-edematous plaques on the toe pads and the fingertips of both hands (Figure 1, A–E). The child had no signs or symptoms and frequented a private pool.
Figure 1.

Clinical aspect of Case 1 (A–E, 6-year-old child) and 2 (F–G, 13-year-old girl): redness and edema symmetrically involving the palmar (A,B,F) and plantar (C,D,E,G) surface of all the distal phalanges of the feet and hands, with the sole exception of the fifth toe; the palms of the hands and feet, in correspondence with the metacarpophalangeal and metatarsophalangeal joints, are also partially affected in case 1. Vesicle-bullous evolution is possible in areas subject to friction on rough pool surfaces (G). Clinical aspect of Case 3 (H–L, 13- and 15-year-old girls) and 4 (M–O, 3-year-old girl): Chilblain-like edematous and erythematous lesions involving the feet, on the dorsal surface (H-I-L), or both on the palmar-plantar and dorsal side (M-N-O). Note the presence of exulcerations on the third and fourth toes (H, L).
Case 2: a 13-year-old girl with partially exulcerated erythematous-edematous plaques on the toes, fingertips and palms (Figure 1, F–G). Lesions were mildly painful, bilateral and symmetric. The girl attended the family private pool, with a 12 years-old cousin who showed identical lesions.
Case 3: two 13- and 15-year-old girls, with chilblain-like burning-aching edematous and erythematous lesions asymmetrically involving the feet, that completely resolved in about 3 weeks.
Case 4: a 3-year-old girl with bilateral and asymmetrical, painful and burning erythemato-violaceous and edematous macules involving the toes and fingers, both on the palmar-plantar and dorsal side (Figure 1, M–O) without systemic symptoms.
SARS-CoV-2 IgG antibodies were positive in both cases 3 and 4.
All 3 dermatologists agreed on the diagnosis of Pool palms (PM), also named “juvenile palmar dermatitis of swimming pools” in cases 1 and 2. Otherwise, in cases 3 and 4 all dermatologists hypothesized COVID-19-related skin lesions, subsequently confirmed by laboratory investigations.
PM is a benign acquired acral dermatosis, typically occurring during childhood (mean age of 6.4 years) [3], probably frequently misdiagnosed with bilateral and symmetrical hand involvement. Table 1 reviews all the 15 PM cases published [3–6]. PM is characterized by erythematous-edematous violaceous asymptomatic lesions with a smooth surface, generally non-infiltrated; in some cases, a painful vesicular-bullous evolution has been described [3–5].
Table 1.
Clinical findings of all reported PM cases, since the first description, dated in 1992*
| Reference | Age, Sex | Anatomical Sites Involved | Symptoms | Geographical Origin |
|---|---|---|---|---|
|
Morgado-Carrasco et al. 2019 PMID: 31921496 |
5-year-old, F | Palmar surface of the fingers** | Painful lesions | Spain |
|
Novoa et al. 2016 PMID: 26424817 |
5-year-old, F | Palmar surface of the fingers** | Asymptomatic lesions | Spain |
| 4-year-old, F | Plantar surface of the fingers, toe pads and heels** | |||
|
Martin JM et al. 2009 PMID: 19709557 |
6-year-old, F | Palm and palmar surface of the fingers** | Asymptomatic lesions | Spain |
|
Lopez-Neyra et al. 2009 PMID: 19951653 |
6-year-old, M | Palmar surface of the fingers** | Asymptomatic lesions | Spain |
|
Wong et al. 2007 PMID: 17300665 |
5-year-old, F | Palmar and plantar surface of the fingers** | Not specified | Australia |
|
Sassolas et al. 1996 PMID: 9033728 |
10-year-old, M | Palmar surface of the fingers and palms and toe pads** | Painful lesions | France |
| 8-year-old, M | ||||
| 4-year-old, M | ||||
|
Lacour et al. 1995 PMID: 8687057 |
6-year-old, M | Palmar surface of the fingers and palms** | Not specified | France |
| 4-year-old, F | Asymptomatic lesions | |||
|
Blauvelt et al. 1992 PMID: 1619059 |
12-year-old, F | Palmar surface of the fingers and palms** | Asymptomatic lesions | U.S.A. |
| 11-year-old, F | ||||
| 3 ½-year-old, M | ||||
| Age not specified, M |
Notes:
We performed a systematic review in MEDLINE using the following keywords: “Pool palms”, “juvenile palmar dermatitis of swimming pools” and “dermatite palmaire juvenile des piscines”. Every reference cited in all the articles included has also been verified. Every article that met the search criteria was analyzed, regardless of language (English, Italian, Spanish and French). Gray literature, any document that hasn’t gone through peer review for a publication and conference abstracts were excluded.
lesions present bilaterally and symmetrically
This mechanical dermatosis is caused by repeated rubbing of the palmar and/or plantar skin with the hard and rough walls of the swimming pool. Consequently, the convex areas of the palmar and plantar surface are more affected [3–5]. It is mostly seen in subjects who are learning to swim and so who tend to cling to the pool walls. The dermatosis typically is self-limiting with the interruption of exposure to the pool environment [3–5].
Conclusions
In the pre-COVID-19 era, allergic contact dermatitis and atopic pulpitis were the main differential diagnoses suggested by several authors [3]. We report the first PM cases reported during the COVID-19 pandemic, proposing a possible potentially underestimated differential diagnosis among childhood acral dermatosis. PM may indeed present clinical features like the acral lesions observed in mild COVID-19 patients; nevertheless, an accurate clinical and anamnestic evaluation can properly orient clinicians (Figure 2).
Figure 2.
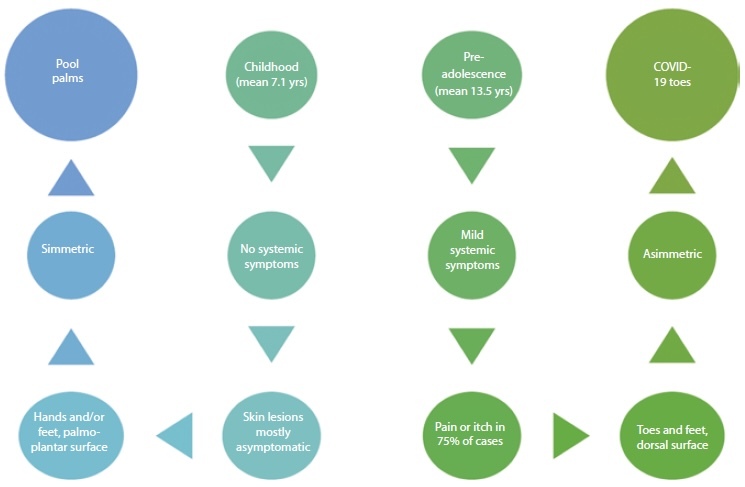
Diagnostic algorithm for the differential diagnosis between Pool palms and COVID-19 toes dermatoses.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication
References
- 1.Caccavale S, Ruocco E. Acral manifestations of systemic diseases: Drug-induced and infectious diseases. Clin Dermatol. 2017 Jan–Feb;35(1):55–63. doi: 10.1016/j.clindermatol.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 2.Molaee H, Emadi SN, M’Imunya JMN, Davoudi-Monfared E, Mohammed A, Razavi Z. Chilblain or Perniosis-like Skin Lesions in children during the COVID-19 pandemic: A Systematic Review of Articles. Dermatol Ther. 2022 Jan 3;:e15298. doi: 10.1111/dth.15298. [DOI] [PubMed] [Google Scholar]
- 3.Morgado-Carrasco D, Feola H, Vargas-Mora P. Pool Palms. Dermatol Pract Concept. 2019;10(1):e2020009. doi: 10.5826/dpc.1001a09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martín JM, Martín JM, Ricart JM. Lesiones eritematovioláceas en las palmas. Diagnóstico: Palmas de piscina [Erythematous-violaceous lesions on the palms] Actas Dermosifiliogr. 2009;100(6):507–8. [PubMed] [Google Scholar]
- 5.Novoa A, Klear S. Pool palms. Arch Dis Child. 2016;101(1):41. doi: 10.1136/archdischild-2015-309633. [DOI] [PubMed] [Google Scholar]
- 6.Wong LC, Rogers M. Pool palms. Pediatr Dermatol. 2007;24(1):95. doi: 10.1111/j.1525-1470.2007.00347.x. [DOI] [PubMed] [Google Scholar]


