To the Editor
Human papilloma viruses (HPVs) are associated with a wide spectrum of cutaneous and mucosal infections and neoplasms. Though angiokeratoma can clinically mimic warts, koilocytes and presence of high-risk HPV DNA have not been reported in angiokeratoma. We describe a case of extragenital solitary angiokeratoma associated with high-risk types of HPV in a child.
A 10-year-old girl presented with two-year history of an asymptomatic bluish-black plaque on the left elbow. There was no history of preceding trauma, bleeding from the lesion or immunosuppression. Cutaneous examination revealed a well-circumscribed dark blue to black colored verrucous plaque of size 2.5 x 1.5 cm on the left elbow (Figure 1A). Dermatoscopic examination showed dark blue, violaceous and black colored round to ovoid lacunae with bluish-white veil (Figure 1B). Excisional biopsy revealed hyperkeratosis, hypergranulosis, acanthosis and papillomatosis. Numerous keratinocytes with raisinoid nuclei and perinuclear halo, characteristic of koilocytes were seen in stratum spinosum. Multiple thin-walled dilated vascular channels filled with erythrocytes were noted in papillary dermis (Figures 1C, 1D). HPV genotyping was performed with extracted DNA from biopsy tissue using Applied Biosystem 7500 Fast Dx real-time polymerase chain reaction (PCR) instrument. Target DNA was amplified for identifying either high-risk HPV (HPV types 16/ 18/ 31/ 33/ 35/ 39/ 45/ 51/ 52/ 56/ 58/ 59/ 66 and 68) or low-risk HPV genotypes (HPV 6/11) respectively. Test results identified HPV high-risk genotypes in the sample. TRUPCR high risk genotyping kit designed to qualitatively detect DNA of high-risk HPV of 14 genotypes by amplifying E6/E7 region by primers and probes specific for the particular genotype by Real time PCR confirmed the presence of HPV-58 and HPV-59 genotypes (Cycle Threshold values 30.32 and 25.94 respectively), with a cut off value of 36 (Figures 2 A and B).
Figure 1.
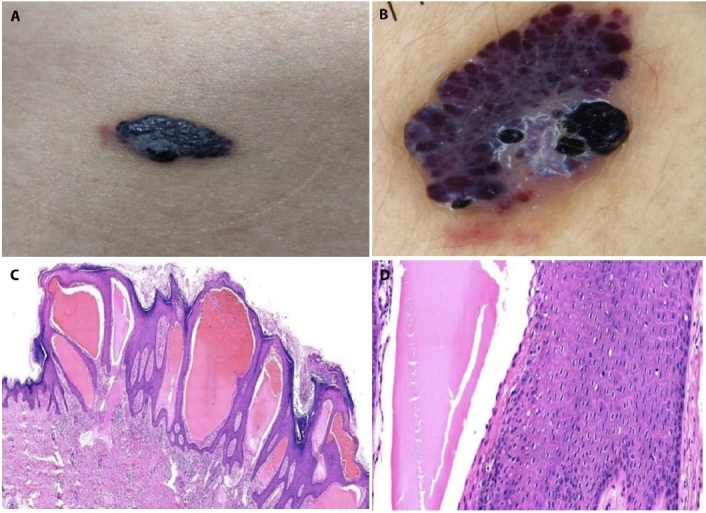
(A) Well-circumscribed bluish-black verrucous plaque of size 2.5 x1.5 cm. (B) Dermoscopic examination revealed dark blue, violaceous and black round to ovoid lacunae with bluish-white veil (DermLite 4, original magnification x10). (C) There is marked hyperkeratosis, hypergranulosis, acanthosis and papillomatosis. Papillary dermis shows thin-walled dilated vascular channels impinging onto the overlying epidermis (H&E, x100). (D) Stratum spinosum showing koilocytes characterized by raisinoid nuclei and perinuclear halo (H&E, x200).
Figure 2.

(A) Real-time polymerase chain reaction amplification plot showing curves of 14 high risk genotypes, with HPV-58 and HPV-59 DNA amplification curves above the cycle threshold value. (B) Cycle threshold (Ct) values for 14 high risk genotypes (cut-off value = 36) obtained by performing real-time polymerase chain reaction of DNA isolated from skin biopsy sample
The role of HPV in the pathogenesis of non-melanoma skin cancers was initially described in epidermodysplasia verruciformis and transplant recipients. High-risk types, mainly HPV 16, are strongly linked with anogenital carcinomas and among cutaneous lesions, implicated in Bowen’s disease and squamous cell carcinoma (SCC) [1]. High-risk genital-mucosal HPV 58 and HPV 59 are risk factors for cervical carcinoma and uncommonly detected in cutaneous lesions [2–4]. HPV 58 has been identified in cutaneous premalignant and malignant lesions including, Bowen disease on the fingers and elbow, SCC and keratoacanthoma [2,3]. HPV 59 genome is most closely related to HPV 18, and has been reported in Bowen disease [4].
HPV infection associated with angiokeratoma has been described in a case presenting on vulva with coexisting positivity for HPV-6 [5]. High-risk genital-mucosal HPV types have not been associated with angiokeratoma. HPV proteins may promote cell proliferation through many signal transduction pathways. The reactive inflammation associated with viral infection results in tumor necrosis factor (TNF)-α production, which in turn stimulates the release of NF-κB. The latter induces production of vascular endothelial growth factor, causing vascular ectasia [6].
Our patient had angiokeratoma on elbow, without any present or past history of anogenital lesions. Interestingly, koilocytes were noted and PCR demonstrated HPV-58 and HPV-59 genotypes. The mode of acquisition of HPV infection in our case could be close contact with some family member having HPV infection. The limitation of this report is we did not assess the presence of HPV in healthy samples of perilesional and distant skin.
It remains to be determined, whether HPV merely occurs as a commensal infection due to ubiquitous presence or is related to disease pathogenesis in angiokeratoma. Nonetheless, detection of high-risk HPV types warrants close follow-up for malignant transformation.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Aoki R, Clanner-Engelshofen BM, Charnowski S, Ruzicka T, Reinholz M. Distribution of high-risk alpha-genus human papillomavirus genotypes impacts cutaneous neoplasms. J Eur Acad Dermatol Venereol. 2019;33(7):1304–1311. doi: 10.1111/jdv.15547. Epub 2019 Apr 10. [DOI] [PubMed] [Google Scholar]
- 2.Mitsuishi T, Kawashima M, Matsukura T, Sata T. Human papillomavirus type 58 in Bowen’s disease of the elbow. Br J Dermatol. 2001;144(2):384–386. doi: 10.1046/j.1365-2133.2001.04033.x. [DOI] [PubMed] [Google Scholar]
- 3.Kobayashi K, Tanese K, Kubo A, et al. Identification of a human papillomavirus type 58 lineage in multiple Bowen’s disease on the fingers: Case report and published work review. J Dermatol. 2018;45(10):1195–1198. doi: 10.1111/1346-8138.14574. [DOI] [PubMed] [Google Scholar]
- 4.Murao K, Kubo Y, Fukuhara K, Matsumoto K, Arase S. Three cases of Bowen’s disease on the lower abdomen associated with high-risk types 16, 33, and 59 of human papillomavirus. J Am Acad Dermatol. 2005;52(4):723–724. doi: 10.1016/j.jaad.2004.11.042. [DOI] [PubMed] [Google Scholar]
- 5.Baruah J, Roy KK, Rahman SM, Kumar S, Pushparaj M, Mirdha AR. Angiokeratoma of vulva with coexisting human papilloma virus infection: a case report. Arch Gynecol Obstet. 2008;278(2):165–167. doi: 10.1007/s00404-007-0539-6. [DOI] [PubMed] [Google Scholar]
- 6.Molho-Pessach V, Lotem M. Viral carcinogenesis in skin cancer. Curr Probl Dermatol. 2007;35:39–51. doi: 10.1159/000106409. [DOI] [PubMed] [Google Scholar]


