Abstract
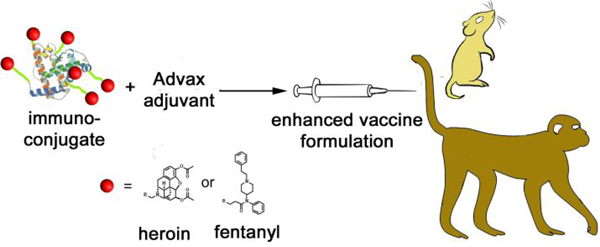
The near insurmountable adversity that accompanies opioid use disorder (OUD) creates life-altering complications for opioid users. To worsen matters, existing small molecule drugs continue to inadequately address OUD due to their engagement of the opioid receptor, which can leave the user to deal with side effects and financial hardships from their repeated use. An alternative therapeutic approach utilizes endogenously-generated antibodies through active vaccination to reduce the effect of opioids without modulating the opioid receptor. Here, we explore different adjuvants and storage conditions to improve opioid vaccine efficacy and shelf-life. Our results revealed that inulin-based formulations (Advax™) containing a CpG oligodeoxynucleotide (ODN) acted as effective adjuvants when combined with a heroin conjugate: immunized mice showed excellent recovery from heroin-induced antinociception accompanied by high titer, high opioid affinity serum antibodies similar to the immunopotentiating properties of traditional alum-based adjuvants. Moreover, non-human primates vaccinated with a heroin/fentanyl combination vaccine demonstrated potent antibody responses against opioids when formulated with both inulin and alum adjuvants. Finally, storing a freeze-dried opioid vaccine formulation maintained efficacy for up 1 year at room temperature. The results from our studies represent an advance toward a clinically feasible opioid vaccine.
Keywords: heroin, fentanyl, vaccine, adjuvants, carrier protein, opioids, immunopharmacotherapy
Graphical Abstract
INTRODUCTION
With no end in sight, the opioid epidemic continues to ravage the US where the annual rate of overdose-related deaths over the past 20 years has steadily risen from 8,000 lives in 1999 to 46,802 in 2018.1 Together, heroin, a Schedule 1 semisynthetic opioid with no medicinal value, and fentanyl, a synthetic prescription opioid, contributed to more than 50% of these deaths in 2016.2 Most people transition to heroin or fentanyl because of the higher cost and lower availability of prescription analgesics but inadvertently end up abusing those illicit opioids due to their addictiveness. Furthermore, to make matters worse for the user, street dealers tend to “cut” heroin with a cheap but more potent filler like fentanyl resulting in a higher chance of a lethal overdose by the unaware drug user. Aside from the impact on the user, opioid use disorder (OUD) can take a toll on the affected family in the form of domestic abuse and developmental delays in children and on society at large with an economic burden estimated to be at least $631 billion from 2015 – 2018 in the US.3
The widespread recreational use of opioids such as heroin and fentanyl stems from their euphoric, analgesic effects on the individual after crossing the blood-brain barrier into the central nervous system (CNS). Unlike fentanyl, heroin is metabolized into pharmacologically active species: 6-acetyl morphine (6AM) and morphine. There heroin metabolites and fentanyl act as agonists for G protein-coupled μ-opioid receptors in the brain resulting in most of the downstream physiological effects that are typically associated with opioid use such as pleasure and relaxation.4–5 However long term side effects from repeated usage involve structural changes6 in the gray and white matter of the brain which lead to neuronal and hormonal imbalances,7–8 impaired decision-making capability and inappropriate responses to stressful situations.9–10
Escaping the deleterious impact of these opioids is a daunting challenge for an opioid abuser due to the crippling withdrawal symptoms. Current therapy for overcoming OUD includes agonists such as methadone and buprenorphine which are used in opioid replacement therapy11 and antagonists such as naloxone which can mitigate the effects of an excessive opioid dose. Although these pharmacological agents allow a user to detoxify and gradually wean off of the drug, the path toward sobriety is grueling to maintain without relapse because of cognitive issues, negative emotional effects and anxiety that are associated with opioid withdrawal.12–13 Because small molecule OUD therapeutics also act on the μ-opioid receptor, treatment regimens can exacerbate symptoms of withdrawal in the case of antagonists14 or precipitate dependency on the OUD medication in the case of agonists.15
An alternative treatment of OUD entails active immunization where endogenously-generated antibodies bind opiates in the blood stream. The sequestration of opiates prevents them from crossing the blood-brain barrier and engaging the μ-opioid receptor although withdrawal symptoms such as craving may still occur. The components of a vaccine against a drug of abuse typically incorporate the drug itself in the form of hapten that is structurally similar to the target opiate and is covalently conjugated to an immunogenic carrier protein that can raise antibodies against the drug-like epitope. The resulting immunoconjugate is then mixed with an adjuvant to yield a formulation that can more strongly stimulate the immune system through T cell-dependent B-cell activation.16 Specifically, the FDA-approved Al(OH)3 (alum) adjuvant with either keyhole limpet hemocyanin (KLH) or tetanus toxoid (TT) carrier protein have commonly been a part of recent attempts to develop translational fentanyl, oxycodone and heroin vaccines.17–20 Also, natural19, 21–22 and other synthetic23–24 adjuvants have been investigated to improve vaccine efficacy. We recently developed vaccines that reduced the in vivo effects of heroin (5–10X ED50 shift)25 and fentanyl (30X ED50 shift)26 in mice. Both vaccines were formulated with TT protein as the immunogenic scaffold for the opiate and combined with alum and CpG oligodeoxynucleotide (ODN) 1826 as adjuvant.
Although the aforementioned vaccine formulations reduced the physiological impact of opiates, we endeavored in this work to improve the clinical viability of our vaccine candidate by exploring less costly and less toxic components and storage conditions to extend their shelf life. Herein, we detail these new formulations, their impact on serum antibody levels and response to heroin-induced antinociception in mice and monkeys.
EXPERIMENTAL SECTION
Preparation, Formulation, and Administration of Vaccine.
All studies were performed in compliance with the Scripps Institutional Animal Care and Use Committee and all protocols adhered to the National Institute of Health Guide for the Care and Use of Laboratory Animals. Heroin HCl was provided by NIDA Drug Supply and was dissolved in bacteriostatic 0.9% NaCl solution with a concentration of 0.4 mg/mL for animal studies. Heroin25 and fentanyl26 haptens were synthesized per our literature procedure, and protein conjugation proceeded as previously described.27 Tetanus toxoid was purchased from MassBiologics, and rTT-Hc and CRM197 were purchased from FinaBio. Dextran-linked CRM was generously provided by Dr. Andrew Lees at FinaBio.
Mouse Immunization Protocol for Adjuvant Screening.
Five groups of 6–8 week old male BALB/c mice (Taconic Farms), n= 6 per group were immunized subcutaneously at weeks 0, 2, and 4. One group received a pH 7.4 PBS solution (control) and the other four received 50 μg Her-TT with 1) 1 mg δ-inulin + 10 μg CpG55.2 (AV-1); 2) 0.1 mg alum + 10 μg CpG55.2 (AV-2); 3) 1 mg modified δ-inulin + 10 μg CpG55.2 (AV-3); and 4) 0.1 mg alum + 50 μg CpG ODN 1826 (alum + CpG). Her-TT was mixed with adjuvant formulations by shaking them in solution for 30 min at room temperature and 4°C overnight. Bleeds were taken at weeks 3 and 6, and antinociception testing was performed on weeks 6 and 7. Adjuvants alum was obtained from InvivoGen as 10 mg/mL suspension and Advax™ adjuvants were obtained from Vaxine Pty Ltd including CpG55.2 (5’-ATCGACTCTCGAGCGTTCTC-3’). CpG ODN 1826 (5’-TCCATGACGTTCCTGACGTT-3’) was obtained as a phosphorothioated oligonucleotide from Eurofins. Weights and general health of mice were monitored by both the scientists conducting the studies, and the veterinary staff of Scripps Research Institute.
Mouse Immunization Protocol for Carrier Protein Screening.
Six groups of 6–8 week old male BALB/c mice (Taconic Farms), n= 6 per group were immunized subcutaneously at weeks 0, 2, and 4. One group received a pH 7.4 PBS solution (control) and the other five received 50 μg CpG ODN 1826, 200 μg alum and 50 μg of heroin hapten conjugated to 1) TT; 2) rTT-Hc; 3) CRM; 4) dextran-CRM and 5) CRM+trehalose. Immunoconjugates were mixed with alum by shaking them in solution for 30 min at room temperature and overnight at 4 °C. Bleeds were taken at weeks 3 and 6, and antinociception testing would be performed on weeks 6 and 7.
Enzyme-linked immunosorbent assay (ELISA).
Half-area, high-binding, 96-well plates were coated for 12 h at 37°C with 1 μg/mL heroin-BSA conjugate in pH 7.4 PBS. Blocking was achieved with 5% skim milk in pH pH 7.4 PBS. Mouse or monkey sera diluted 1:100 into 1% BSA in pH 7.4 PBS were used for twelve 1:1 serial dilutions across the plate followed by 2.5 h incubation at 25°C. Washing before and after the addition of the secondary antibody was performed 5X with pH 7.4 PBS. Donkey anti-mouse IgG, Fcγ specific HRP secondary antibody (Jackson ImmunoResearch) and goat anti-monkey, Fcγ specific HRP (Novus Biologicals) were used for detection at 0.1 μg/mL, incubated for 45 min at 25°C. Plates were developed with TMB substrate (Thermo Fisher) and 2M H2SO4 as a stopping solution. Midpoint titers were calculated by applying a non-linear [inhibitor] vs. normalized response curve in GraphPad Prism to the dilution series data of each serum sample.
Surface Plasmon Resonance (SPR) Assay.
Affinity measurements were performed on a Biacore 3000 instrument using previously described protocols.25–26 Briefly, serum samples were diluted in running buffer to give approximately 100 RU signal on fentanyl or heroin-BSA coated sensor chips. At the predetermined serum dilution, samples were incubated prior to the SPR run with 12 dilutions of fentanyl or 6-acetylmorphine including a drug-free control sample. Competitive IC50 values were calculated by applying a non-linear [inhibitor] vs. normalized response curve in GraphPad Prism to the competition series data of each serum sample.
Hapten Density Determination by Matrix-Assisted Laser Desorption Ionization.
The heroin and fentanyl hapten densities on carrier proteins were assessed using MALDI-TOF (matrix-assisted laser desorption ionization-time-of-flight) and electrospray ionization-TOF mass spectrometry analysis as described in our previous publications.27 For CRM conjugates, hapten to protein ratios were determined to be 12:1 for heroin and 18:1 for fentanyl (Figures S4 – S8).
Antinociceptive Behavioral Evaluation.
Mice were tested for cumulative drug response in supraspinal (hot plate) and spinal (tail flick) behavioral tests at week 6 as described in our prior study.27 After a baseline measurement, cumulative heroin doses administered were 2, 4, 6, 8, 10, 14 and 18 mg/kg and each dose increment was given IP in 15 minute intervals until the maximum cutoff times of 35 s for hot plate and 10 s for tail flick. After normalizing data as % maximum possible effect from baseline and cutoff measurements, a non-linear [agonist] vs. normalized response curve was applied to calculate effective dose 50% values (ED50). At week 7 mice were administered a single IP 4 mg/kg heroin dose and were tested in antinociception assays at 15, 30- and 45-min post-injection.
Long Term Stability Study.
Similar to previous heroin vaccine stability experiments,28 heroin-TT and CRM conjugates were formulated in pH 7.4 PBS 15% w/v trehalose at 1 mg/mL with 1 mg (or 0.1 mg for CRM) alum + 50 μg CpG ODN 1826. The heroin-CRM formulation was sterile filtered prior to the addition of sterile alum. After end-over-end mixing at 4°C, the lyophilized formulations were frozen in liquid N2 and placed under high vacuum to dry completely while the liquid formulations were stored at 4°C in sealed tubes with no further modification until injected. Freeze-dried formulations were stored at room temperature in sealed tubes placed within a desicator. Prior to injection, lyophilized vaccines were reconstituted in sterile water to match the volume of liquid vaccines and mixed for 15 min. Both formulations were stored for either 1, 6 or 12 months before initiating the standard 0, 2, 4-week immunization schedule.
Vaccine Study in Non-Human Primates.
Sixteen cynomolgus monkeys (n = 3–4 per group) were immunized at months 0, 1, 2 and 4 via deltoid muscle with 80 μg fentanyl-CRM + 160 μg heroin-CRM formulated with 1) no adjuvant, 2) 1 mg alum, 3) 10 mg δ-inulin + 200 μg CpG55.2, 4) 10 mg modified δ-inulin and 5) 1 mg alum + 500 μg CpG55.2 at a total volume of 400 μL per injection. As previously described, the modified inulin was an oxidized form of inulin containing surface aldehydes.29 Blood samples were taken at the indicated time points, and serum samples were analyzed by SPR and ELISA. Monkey were housed and monitored by Alpha Genesis, Inc., an AAALAC facility. Animal care and use protocols were approved by the Alpha Genesis IACUC committee prior to implementation.
Statistical Analysis.
Starred groups are compared to the control group and data points represent means ± SEM. One-way ANOVAs compare ED50 values and two-way ANOVAs are used when opioid antinociception is observed over time. *P<0.05, **P<0.01, ***P<0.001 by one or two-way ANOVA with Bonferroni’s post-hoc test versus control.
RESULTS AND DISCUSSION
Screening potential adjuvants.
Over the past decade, Advax™, an adjuvant comprising δ-inulin-based microparticles, has been shown to have superior performance over alum in microbial, viral and toxin vaccine formulations.30 For example compared to alum, it was characterized by enhanced CD4 / CD8 T-cell response from hepatitis B vaccines in mice,31 increased IgG titers and accelerated seroprotection by several days in guinea pigs.32 Moreover alum is known to trigger site injection inflammation33 while Advax is not marred by necrosis-inducing inflammasomes.34 Advax’s favorable properties would instill a vaccine formulation with a better safety profile. Often combined with inulin and alum are CpG oligodeoxynucleotides (ODNs) that activate the innate immune receptor Toll-like receptor 9 (TLR-9). Many studies have established the ability of CpG ODNs to enhance inulin and alum vaccine efficacy35–38 even in the context of vaccines targeting drugs of abuse.27 In considering these promising adjuvants, we decided to compare our original heroin-conjugated TT (Her-TT) vaccine formulation containing alum and CpG182625 to Advax formulations containing different forms of δ-inulin in combination with CpG55.2.
To determine the Advax formulation (AV) with the best efficacy, one of five groups of mice were vaccinated with either: 1) PBS solution (control); 2) Her-TT with δ-inulin + CpG55.2 (AV-1); 3) Her-TT with alum + CpG55.2 (AV-2); 4) Her-TT with modified δ-inulin29 + CpG55.2 (AV-3); and 5) Her-TT with alum + CpG ODN 1826 (alum + CpG). Five weeks after immunization, we evaluated the ability of the vaccines to reduce heroin-triggered antinociceptive behavior by subjecting these mice to a battery of hot plate and tail flick experiments. When the mice were injected intraperitoneally (i.p.) with heroin at increasing doses, the alum + CpG group underwent the greatest ED50 shift while the three Advax groups (AV-1, AV-2 and AV-3) together experienced an 8X ED50 shift and 5X ED50 shift relative to the control in the hot plate (Figure 1A) and tail flick (Figure 1B) experiments, respectively. Surprisingly, when the mice were injected i.p. at a single dose (4 mg / kg) of heroin, the AV-2 group saw a quicker recovery than the alum + CpG group from antinociception in the hot plate experiment (Figure 1C; with error bars included in Figure S1A) while both AV-1 and AV-2 experienced faster recovery than the alum + CpG group in the tail flick experiment (Figure 1D; with error bars included in Figure S1B). ELISA revealed that alum + CpG produced the highest anti-hapten titers while competitive affinity measurements by surface plasmon resonance (SPR) showed that antibodies from the alum + CpG and AV-2 formulations had similar affinities but 10-fold stronger affinity than AV-1 and AV-3 to 6AM (Figure 1E). This discrepancy between AV-1 and AV-2’s smaller ED50 shift and quicker recovery from antinociception compared to alum + CpG suggests that the antibodies generated from AV-1 and AV-2 can more rapidly neutralize a heroin dose while alum + CpG produces antibodies with a larger capacity to neutralize heroin but at a slower rate; however, further studies are needed to elucidate the opioid-antibody binding kinetics. Overall the adjuvant study demonstrates better efficacy of the alum containing vaccines over inulin vaccines, although inulin did show respectable adjuvant performance. Furthermore, CpG55.2 while administered at a 5-fold lower dose compared to CpG1826 showed better efficacy in the time course antinociception experiment. A definitive conclusion on which CpG is superior in the context of our heroin vaccine cannot be made given the current data, but certainly follow up studies are warranted to further refine adjuvant formulations.
Figure 1.

Comparison of Advax against alum + CpG adjuvant formulations in reducing antinociception through tail flick (A, C) and hot plate (B, D) experiments. (E) Antihapten midpoint titers in sera obtained by ELISA with anti-6AM competitive IC50 values (nM) shown above each bar.
Screening potential carrier proteins.
We next investigated a selection of recombinant carrier proteins to identify one that is as effective as TT in blunting the effects of heroin but is more cost effective. We examined a negative control (PBS solution) along with five vaccine formulations containing alum, CpG and a heroin hapten conjugated to: 1) TT; 2) recombinant TT heavy chain fragment C (rTT-Hc); 3) CRM197, a recombinant non-toxic mutant of diphtheria toxin (CRM); 4) dextran linked-CRM; and 5) CRM + trehalose (15% w/v). Following immunization, we evaluated the vaccines’ capacity to reduce heroin-induced antinociception by subjecting these groups of mice to tail flick tests. When the mice were injected i.p. with heroin at increasing doses, the CRM and rTT-Hc groups experienced the largest ED50 shifts at a range of 2.2 – 2.5X relative to the control and 1.5X relative to TT (Figure 2A). Also, the CRM group saw the quickest recovery from antinociception compared to the others when they were injected with heroin at a single dose (Figure 2C; with error bars included in Figure S2). The CRM and rTT-Hc groups demonstrated superior performance over TT despite their relatively lower antihapten titer levels (Figure 2B). SPR resolved this discrepancy by revealing that antibodies from the CRM and rTT-Hc groups had the strongest affinity to 6AM (Table 1); however, affinities differed by a factor of 10 from formulations in Figure 1 possibly due to batch variability in conjugate preparation.
Figure 2.

Influence of carrier proteins on the reduction of antinociception through tail flick assay (A, C). (B) Antihapten midpoint titers in sera obtained by ELISA. *P<0.05, ***P<0.001 by one or two-way ANOVA with Bonferroni’s post-hoc test versus control.
Table 1.
6AM antiserum binding affinities generated from immunization with various heroin-carrier protein conjugates formulated with alum + CpG ODN 1826.
| Vaccine formulationa | IC50 (nM) |
|---|---|
| TT | 42.2 |
| rTT-Hc | 25.2 |
| CRM | 26.8 |
| dextran-CRM | 85.6 |
| CRM + trehalose | 53.9 |
Adjuvant formulation for all conjugates includes alum + CpG ODN l826
Based on our results, CRM is the best choice of carrier protein to advance toward future opioid vaccine development given its slight efficacy advantage, lower cost and easier to characterize nature compared to TT. Furthermore, a previous study comparing these carrier proteins in an oxycodone vaccine also found similar efficacy between the different proteins.39 Linkage of heroin-CRM to a dextran polymer was initially hypothesized to boost vaccine response via increased antigen valency, however, results showed no benefit of this conjugate over monomeric CRM. We attribute the absence of this enhanced response to dextran presumably interfering with hapten loading during the conjugation step. Lastly, the addition of trehalose, a common vaccine stabilizing excipient40 potentially diminished vaccine immunogenicity, indicating that it is not productive to add trehalose to the liquid heroin-CRM vaccine formulation. It is in fact crucial for protecting lyophilized alum-containing vaccines during the freeze-drying process.28
Evaluating vaccine storage conditions.
The ability to store a vaccine formulation for the long-term without reduction in efficacy becomes critical for clinically-viability; therefore, we explored two ways of storing a Her-TT vaccine formulation over 12 months: 4º C in liquid form or at room temperature in lyophilized form. After the 12-month period, mice were vaccinated with either: 1) the lyophilized form; 2) the liquid form (liquid); or 3) unconjugated keyhole limpet hemocyanin control (KLH Ctrl). KLH was chosen as a benchmark to assess efficacy because it does not induce any anti-heroin immune response as we demonstrated previously,41 yet effectively acts as a cost-effective, non-endogenous immunogenic substance similar to other more expensive carrier proteins CRM and TT.
Six weeks after immunization, we evaluated the vaccines’ capacity to reduce heroin-induced antinociception by subjecting the three groups of mice to tail flick and hot plate experiments. When the mice were injected i.p. with heroin at increasing doses, the hot plate and tail flick experiments showed that the lyophilized group experienced the largest ED50 shift at 1.3X and 2X relative to the liquid group, respectively (Figure 3A). SPR studies corroborated the superiority of the lyophilized formulation when they indicated the presence of serum antibodies with tighter binding than the liquid formulation to heroin and 6AM and, as expected, greater selectivity to 6AM (Table 2).25 In addition, over a 6-month storage period, liquid and lyophilized vaccines showed no measurable difference between each other and no overall decrease in efficacy compared to the freshly-prepared batches (data not shown). Finally, over 1- and 6-month storage periods, both vaccine formulation types showed equivalent efficacy (Figure S3), indicating that significant vaccine degradation occurred sometime between 6 and 12 months. These studies demonstrate that storing the vaccine formulation over a one-year period in the lyophilized form at room temperature preserved vaccine efficacy unlike liquid form storage at 4ºC. An obvious site of chemical instability is the hapten acetate moieties in heroin which are known to undergo hydrolysis in aqueous solution;42 however, the result would be conversion to a morphine-like hapten contributing to an increase in morphine antiserum affinity, which was not observed (Table 2).
Figure 3.

Effect of storage conditions on vaccine performance. (A) Antinociception testing in hot-plate (HP) and tail-flick (TF) assays following immunization of liquid or lyophilized Her-TT (lyoph) vaccines stored over 12 months at 4 °C or room temperature, respectively. *P<0.05, **P<0.01, ***P<0.001 by one or two-way ANOVA with Bonferroni’s post-hoc test versus control. (B) Heroin ED50 in the hot plate test of liquid and lyophilized Her-CRM vaccines stored for 1 month prior to immunization. P<0.001 versus control. (C) Time-course of antinociception of immunized mice from panel B treated with 2 mg/kg heroin and subjected to hot plate test. P<0.001 versus control at 15 and 30 min.
Table 2.
Binding affinities of opioids to serum antibodies generated from Her-TT vaccine formulations after 12 months of storage in lyophilized or liquid form.
| Opioid | Liquid IC50 (nM) | Lyoph IC50 (nM) |
|---|---|---|
| 6AM | 89.9 | 36.9 |
| Heroin | 4090 | 617.8 |
| morphine | 13914 | 17069 |
In continuing to investigate CRM as a carrier protein for heroin (Her-CRM), a 1-month stability study was conducted, which showed equivalent efficacy between liquid and lyophilized formulations (Figure 3B), similar to what was observed for the heroin-TT conjugate.28 Both the liquid and lyophilized groups showed significant, equivalent mitigation of heroin antinociception from a single 4 mg/kg drug dose compared to the control group (Figure 3C). Thus, we anticipate that because the Her-CRM vaccine is clearly amenable to lyophilization, it would maintain stability at 12 months and beyond as shown with Her-TT (Figure 3A).
Efficacy testing in non-human primates (NHPs).
Although the Advax-formulated groups displayed lower ED50 shifts than the alum-formulated group in mice, observing the Advax groups’ (AV-1 and AV-2) quicker recovery from antinociception encouraged us to evaluate their efficacy in higher-order animals with the hope that the shortcomings would not translate across species. Specifically, we wanted to investigate the effectiveness of our new adjuvants with a dual fentanyl and heroin vaccine formulation on non-human primates, similar to our study with rats.43 Therefore, we immunized five groups of cynomolgus monkeys with a formulation containing a combination of heroin- and fentanyl-hapten immunoconjugates formulated with either: 1) No adjuvant; 2) alum; 3) δ-inulin + CpG55.2; 4) modified δ-inulin29 and 5) alum + CpG55.2. Over the course of the 14-week immunization period, serum antibodies against heroin or fentanyl were monitored by ELISA. On weeks 14 and 22 where titer levels were at a maximum, the CpG55.2 + alum showed the highest titer levels against heroin (Figure 4A) while on week 14, modified δ-inulin showed the highest against fentanyl (Figure 4B). Although a drop in titer levels was observed following a month long period in which monkeys were not given booster injections, the magnitude of the drop is consistent with previous heroin and fentanyl NHP vaccine studies which have established the long-term immunological efficacy of these opioid vaccines for >50 weeks.25, 44 Based on binding data from SPR, the modified δ-inulin group showed the strongest binding antibodies (Figure 4C). We posit that this aldehyde-containing inulin may interact with our opioid-CRM antigen via Schiff base formation with surface lysine residues. As a result, the inulin may have acted as an oligomeric multi-antigen display scaffold to enhance the anti-opioid immune response observed in this vaccine group.45 Additionally, inulin has been known for its immunomodulatory properties46 potentially making it a better crosslinking material for vaccine efficacy.
Figure 4.

Effects of alum, δ-inulin and CpG ODN containing heroin/fentanyl combination vaccines in NHPs. (A) Anti-heroin and (B) anti-fentanyl titer levels measured by ELISA against corresponding opioid-BSA coating antigens. Arrows indicate IM vaccine injections. C) Binding affinities of week 14 serum antibodies to fentanyl and 6AM by SPR. Heroin titer significance vs. no adjuvant: Alum + CpG week 14***, 22***; vs. Alum: Alum + CpG week 14*. Fentanyl titer significance vs. no adjuvant: Alum week 14**, 22*; Inulin week 10*, 14***; Alum + CpG week 14*, 22*; vs. Alum: Inulin + CpG week 14*; *P<0.05, **P<0.01, ***P<0.001; n = 3 monkeys per group except n = 4 for inulin group.
Although the lack of performing OUD behavioral models is a clear limitation of our monkey study, vaccine composition and immunochemical data such as titer levels (10,000 – 20,000) and affinity (IC50 ~5 nM) from our previous fentanyl vaccine monkey study44 are similar to the results from the current study (Figure 4B and 4C). This suggests that the vaccines at hand would significantly mitigate opioid effects in OUD models. While most adjuvant formulations (inulin + CpG, modified inulin and alum + CpG) performed well compared to the non-adjuvant control, modified δ-inulin elicited the overall best anti-opioid antibody response in NHPs. This form of inulin appears to be the most promising adjuvant candidate for further testing, and its molecular attributes should be elucidated.
By replacing the original vaccine formulation containing TT carrier and alum adjuvant with CRM carrier and δ-inulin adjuvants, we have achieved new opioid vaccine formulations that show excellent performance in mitigating heroin and fentanyl in preclinical models. Furthermore, lyophilization appears to be an effective method for storing vaccines for over a year at room temperature. The results from this study represent an advance toward a clinically-viable conjugate vaccine that could be used to treat opioid use disorder or prevent opioid overdose.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported by National Institutes of Health Grant No. 5UH3DA041146 (K.D.J)
We would like to thank Dr. Andrew Lees at Fina Biosolutions, LLC for providing dextran-CRM.
Footnotes
ASSOCIATED CONTENT
Supporting Information
The following files are available free of charge at
Efficacy curves for stored Her-TT formulations (PDF)
Effect of Advax on heroin antinociception (PDF)
Effect of carrier proteins on heroin antinociception (PDF)
MALDI-TOF spectra of immunoconjugates (PDF)
The authors declare no competing financial interest.
PTB is an employee of Cessation Therapeutics, which has licensed KDJ opioid vaccine patents from TSRI.
Advax™ is a patented, proprietary formulation containing δ-inulin from Vaxine Pty Ltd
REFERENCES
- 1.Overdose Death Rates. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates (accessed 2020–6-23).
- 2.Hedegaard HB; Bastian BA; Trinidad JP; Spencer M; Warner M Drugs Most Frequently Involved in Drug Overdose Deaths: United States (2011–2016); NVSR67_09-508; CDC: Atlanta, GA, 2018. [PubMed] [Google Scholar]
- 3.Davenport S; Weaver A; Caverly M Economic Impact of Non-Medical Opioid Use in the United States (2015 – 2019); Society of Actuaries: Schaumburg, IL, 2019. [Google Scholar]
- 4.Selley DE; Cao C-C; Sexton T; Schwegel JA; Martin TJ; Childers SR, μ Opioid receptor-mediated G-protein activation by heroin metabolites: evidence for greater efficacy of 6-monoacetylmorphine compared with morphine. Biochem. Pharmacol 2001, 62 (4), 447–455. [DOI] [PubMed] [Google Scholar]
- 5.Traynor J, μ-Opioid receptors and regulators of G protein signaling (RGS) proteins: From a symposium on new concepts in mu-opioid pharmacology. Drug Alcohol Depend 2012, 121 (3), 173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X; Li B; Zhou X; Liao Y; Tang J; Liu T; Hu D; Hao W, Changes in brain gray matter in abstinent heroin addicts. Drug Alcohol Depend 2012, 126 (3), 304–308. [DOI] [PubMed] [Google Scholar]
- 7.Ignar DM; Kuhn CM, Effects of specific mu and kappa opiate tolerance and abstinence on hypothalamo-pituitary-adrenal axis secretion in the rat. J. Pharmacol. Exp. Ther 1990, 255 (3), 1287. [PubMed] [Google Scholar]
- 8.Kreek MJ; Ragunath J; Plevy S; Hamer D; Schneider B; Hartman N, ACTH, cortisol and β-endorphin response to metyrapone testing during chronic methadone maintenance treatment in humans. Neuropeptides 1984, 5 (1), 277–278. [DOI] [PubMed] [Google Scholar]
- 9.Li W; Li Q; Zhu J; Qin Y; Zheng Y; Chang H; Zhang D; Wang H; Wang L; Wang Y; Wang W, White matter impairment in chronic heroin dependence: A quantitative DTI study. Brain Res. 2013, 1531, 58–64. [DOI] [PubMed] [Google Scholar]
- 10.Liu J; Qin W; Yuan K; Li J; Wang W; Li Q; Wang Y; Sun J; von Deneen KM; Liu Y; Tian J, Interaction between Dysfunctional Connectivity at Rest and Heroin Cues-Induced Brain Responses in Male Abstinent Heroin-Dependent Individuals. PLoS One 2011, 6 (10), e23098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borodovsky JT; Levy S; Fishman M; Marsch LA, Buprenorphine treatment for adolescents and young adults with opioid use disorders: a narrative review. J. Addict. Med 2018, 12 (3), 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anton B; Salazar A; Florez A; Matus M; Marin R; Hernandez J-A, Vaccines against morphine/heroine and its use as effective medication for preventing relapse to opiate addictive behaviors. Hum. Vaccin. Immunother 2009, 5 (4), 214–229. [DOI] [PubMed] [Google Scholar]
- 13.Nestler EJ, From neurobiology to treatment: progress against addiction. Nat. Neurosci 2002, 5 (11), 1076–1079. [DOI] [PubMed] [Google Scholar]
- 14.Kanof PD; Handelsman L; Aronson MJ; Ness R; Cochrane KJ; Rubinstein KJ, Clinical characteristics of naloxone-precipitated withdrawal in human opioid-dependent subjects. J. Pharmacol. Exp. Ther 1992, 260 (1), 355–63. [PubMed] [Google Scholar]
- 15.Lugoboni F; Zamboni L; Cibin M; Tamburin S; Gruppo Inter, S. d. C. S., Intravenous Misuse of Methadone, Buprenorphine and Buprenorphine-Naloxone in Patients Under Opioid Maintenance Treatment: A Cross-Sectional Multicentre Study. Eur Addict Res 2019, 25 (1), 10–19. [DOI] [PubMed] [Google Scholar]
- 16.Bremer PT; Janda KD, Conjugate vaccine immunotherapy for substance use disorder. Pharmacol. Rev 2017, 69 (3), 298–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Raleigh MD; Baruffaldi F; Peterson SJ; Le Naour M; Harmon TM; Vigliaturo JR; Pentel PR; Pravetoni M, A fentanyl vaccine alters fentanyl distribution and protects against fentanyl-induced effects in mice and rats. J. Pharmacol. Exp. Ther 2019, 368 (2), 282–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raleigh MD; Laudenbach M; Baruffaldi F; Peterson SJ; Roslawski MJ; Birnbaum AK; Carroll FI; Runyon SP; Winston S; Pentel PR, Opioid dose-and route-dependent efficacy of oxycodone and heroin vaccines in rats. J. Pharmacol. Exp. Ther 2018, 365 (2), 346–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matyas GR; Mayorov AV; Rice KC; Jacobson AE; Cheng K; Iyer MR; Li F; Beck Z; Janda KD; Alving CR, Liposomes containing monophosphoryl lipid A: a potent adjuvant system for inducing antibodies to heroin hapten analogs. Vaccine 2013, 31 (26), 2804–2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sulima A; Jalah R; Antoline JF; Torres OB; Imler GH; Deschamps JR; Beck Z; Alving CR; Jacobson AE; Rice KC; Matyas GR, A stable heroin analogue that can serve as a vaccine hapten to induce antibodies that block the effects of heroin and its metabolites in rodents and that cross-react immunologically with related drugs of abuse. J. Med. Chem 2018, 61 (1), 329–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreno AY; Azar MR; Warren NA; Dickerson TJ; Koob GF; Janda KD, A critical evaluation of a nicotine vaccine within a self-administration behavioral model. Mol. Pharm 2010, 7 (2), 431–441. [DOI] [PubMed] [Google Scholar]
- 22.Sanderson SD; Cheruku SR; Padmanilayam MP; Vennerstrom JL; Thiele GM; Palmatier MI; Bevins RA, Immunization to nicotine with a peptide-based vaccine composed of a conformationally biased agonist of C5a as a molecular adjuvant. Int. Immunopharmacol 2003, 3 (1), 137–146. [DOI] [PubMed] [Google Scholar]
- 23.Byrnes-Blake KA; Carroll FI; Abraham P; Owens SM, Generation of anti- (+) methamphetamine antibodies is not impeded by (+) methamphetamine administration during active immunization of rats. Int. Immunopharmacol. 2001, 1 (2), 329–338. [DOI] [PubMed] [Google Scholar]
- 24.Kosten TA; Shen XY; O’Malley PW; Kinsey BM; Lykissa ED; Orson FM; Kosten TR, A morphine conjugate vaccine attenuates the behavioral effects of morphine in rats. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 45, 223–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bremer PT; Schlosburg JE; Banks ML; Steele FF; Zhou B; Poklis JL; Janda KD, Development of a clinically viable heroin vaccine. J. Am. Chem. Soc 2017, 139 (25), 8601–8611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bremer PT; Kimishima A; Schlosburg JE; Zhou B; Collins KC; Janda KD, Combatting synthetic designer opioids: a conjugate vaccine ablates lethal doses of fentanyl class drugs. Angew. Chem. Int. Ed 2016, 55 (11), 3772–3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bremer PT; Schlosburg JE; Lively JM; Janda KD, Injection Route and TLR9 Agonist Addition Significantly Impact Heroin Vaccine Efficacy. Mol. Pharm 2014, 11 (3), 1075–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hwang CS; Bremer PT; Wenthur CJ; Ho SO; Chiang S; Ellis B; Zhou B; Fujii G; Janda KD, Enhancing Efficacy and Stability of an Antiheroin Vaccine: Examination of Antinociception, Opioid Binding Profile, and Lethality. Mol. Pharm 2018, 15 (3), 1062–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Afinjuomo F; Barclay TG; Parikh A; Song Y; Chung R; Wang L; Liu L; Hayball JD; Petrovsky N; Garg S, Design and characterization of inulin conjugate for improved intracellular and targeted delivery of pyrazinoic acid to monocytes. Pharmaceutics 2019, 11 (5), 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Petrovsky N; Cooper PD, Advax™, a novel microcrystalline polysaccharide particle engineered from delta inulin, provides robust adjuvant potency together with tolerability and safety. Vaccine 2015, 33 (44), 5920–5926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cooper PD; Petrovsky N, Delta inulin: a novel, immunologically active, stable packing structure comprising β-D-[2→ 1] poly (fructo-furanosyl) α-D-glucose polymers. Glycobiology 2011, 21 (5), 595–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saade F; Honda-Okubo Y; Trec S; Petrovsky N, A novel hepatitis B vaccine containing Advax™, a polysaccharide adjuvant derived from delta inulin, induces robust humoral and cellular immunity with minimal reactogenicity in preclinical testing. Vaccine 2013, 31 (15), 1999–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Desmet CJ, Adjuvants targeting the DNA sensing pathways–Alum based adjuvants. In Biological DNA Sensor, Elsevier: 2014; pp 271–312. [Google Scholar]
- 34.Cullen SP; Kearney CJ; Clancy DM; Martin SJ, Diverse activators of the NLRP3 inflammasome promote IL-1β secretion by triggering necrosis. Cell Rep 2015, 11 (10), 1535–1548. [DOI] [PubMed] [Google Scholar]
- 35.Davtyan H; Zagorski K; Rajapaksha H; Hovakimyan A; Davtyan A; Petrushina I; Kazarian K; Cribbs DH; Petrovsky N; Agadjanyan MG; Ghochikyan A, Alzheimer’s disease Advax(CpG)- adjuvanted MultiTEP-based dual and single vaccines induce high-titer antibodies against various forms of tau and Abeta pathological molecules. Sci Rep 2016, 6, 28912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Counoupas C; Pinto R; Nagalingam G; Britton WJ; Petrovsky N; Triccas JA, Delta inulin-based adjuvants promote the generation of polyfunctional CD4(+) T cell responses and protection against Mycobacterium tuberculosis infection. Sci Rep 2017, 7 (1), 8582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stronsky SM; Cooper CL; Steffens J; Van Tongeren S; Bavari S; Martins KA; Petrovsky N, Adjuvant selection impacts the correlates of vaccine protection against Ebola infection. Vaccine 2020, 38 (29), 4601–4608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eichinger KM; Kosanovich JL; Gidwani SV; Zomback A; Lipp MA; Perkins TN; Oury TD; Petrovsky N; Marshall CP; Yondola MA; Empey KM, Prefusion RSV F Immunization Elicits Th2-Mediated Lung Pathology in Mice When Formulated With a Th2 (but Not a Th1/Th2-Balanced) Adjuvant Despite Complete Viral Protection. Front Immunol 2020, 11, 1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Baruffaldi F; Kelcher AH; Laudenbach M; Gradinati V; Limkar A; Roslawski M; Birnbaum A; Lees A; Hassler C; Runyon S; Pravetoni M, Preclinical Efficacy and Characterization of Candidate Vaccines for Treatment of Opioid Use Disorders Using Clinically Viable Carrier Proteins. Mol. Pharm 2018, 15 (11), 4947–4962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peek LJ; Martin TT; Elk Nation C; Pegram SA; Middaugh CR, Effects of stabilizers on the destabilization of proteins upon adsorption to aluminum salt adjuvants. J. Pharm. Sci 2007, 96 (3), 547–57. [DOI] [PubMed] [Google Scholar]
- 41.Hwang CS; Bremer PT; Wenthur CJ; Ho SO; Chiang S; Ellis B; Zhou B; Fujii G; Janda KD, Enhancing efficacy and stability of an antiheroin vaccine: examination of antinociception, opioid binding profile, and lethality. Mol. Pharm 2018, 15 (3), 1062–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bremer PT; Janda KD, Investigating the Effects of a Hydrolytically Stable Hapten and a Th1 Adjuvant on Heroin Vaccine Performance. J. Med. Chem 2012, 55 (23), 10776–10780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Townsend EA; Bremer PT; Faunce KE; Negus SS; Jaster AM; Robinson HL; Janda KD; Banks ML, Evaluation of a dual fentanyl/heroin vaccine on the antinociceptive and reinforcing effects of a fentanyl/heroin mixture in male and female rats. ACS Chem. Neurosci 2020, 11 (9), 1300–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tenney RD; Blake S; Bremer PT; Zhou B; Hwang CS; Poklis JL; Janda KD; Banks ML, Vaccine blunts fentanyl potency in male rhesus monkeys. Neuropharmacology 2019, 158, 107730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lees A; Finkelman F; Inman JK; Witherspoon K; Johnson P; Kennedy J; Mond JJ, Enhanced immunogenicity of protein-dextran conjugates: I. Rapid stimulation of enhanced antibody responses to poorly immunogenic molecules. Vaccine 1994, 12 (13), 1160–6. [DOI] [PubMed] [Google Scholar]
- 46.Skwarczynski M, Inulin: A new adjuvant with unknown mode of action. EBioMedicine 2017, 15, 8–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


