Abstract
Background
Restrictions on international travel were widely applied to contain cross-border COVID-19 diffusion, while such applications varied globally, and little was known about their impacts on the long-term epidemic progression.
Methods
We explored the global diversity in maintaining border policies classified to four levels (screening, quarantine, ban on regions and total border closure) using data of 185 countries and regions between 01 January 2020 to 31 December 2021. By using Ordinary least squares (OLS) regression and quantile regression (QR) models, we examined the relationship between total COVID-19 incidence and the cumulative duration of each policy level in 2020–2021, and the heterogeneity of such association across different transmission severity countries.
Results
Firstly, “ban on regions” was the most durable policy applied in high-income countries, while in low-income countries, less stringent measures of screening and quarantine arrivals were applied the longest. Secondly, the cumulatively longer maintenance of the border quarantine was significantly associated with lower infections (log) in COVID-19 high-prevalent countries (75th QR, coefficient estimates [β] = −0.0038, 95% confidence interval: −0.0066 to −0.0010). By contrast, in medium and high transmission severity countries, those with longer duration of imposing bans on regions showed no suppressing effects but significantly higher COVID-19 incidence (OLS regression, β = 0.0028, 95% CI: 0.0009–0.0047; 75th QR, β = 0.0039, 95% CI: 0.0014–0.0063). No other significant results were found.
Conclusion
From the long-term perspective, inbound quarantine was effective in mitigating severe epidemics. However, in countries with medium or high COVID-19 prevalence, our findings of ban on regions highlighted its ineffectiveness in the long-term epidemic progression.
Keywords: COVID-19, Screening, Quarantine, Border closure, Travel restriction, Cross-border transmission
1. Background
Due to the increasing convenience of international air travel, global populations generally have more cross-border mobility than in previous times. Such movements were considered as the major route that facilitated infectious disease development from regional outbreaks to global spreading events [[1], [2], [3]]. As countermeasures, worldwide administrations established muti-level border control policies to protect susceptible individuals from both existing and emerging infections, including yellow fever [4], COVID-19 and its variants [5,6], and monkeypox which was also once characterized as public health emergency of international concern (PHEIC) by World Health Organization (WHO) [7].
Before and after the COVID-19 pandemic declaration of WHO [8], restrictions on international travel were adopted with large disparities by global countries [[9], [10], [11]]. Some of them repatriated tourists from regions with high COVID-19 prevalence and even totally closed the border [12,13], whereas there were other tourism-dependent nations that preferred more moderate measures, including screening (e.g. testing for the reverse transcription polymerase chain reaction (RT-PCR) or antibodies) and quarantining travelers upon their arrival [14,15]. Throughout numerous waves of COVID-19 transmissions, such border controls were dynamically updated by either being tightening or easing according to the real-time epidemic situation. Therefore, the adherence of those travel limitations also varied globally to date, which necessitated the descriptive analysis of global border policies considering both the stringency level and the length of time, in order to improve the border policy formulation.
Currently, the enormous global health burden imposed by COVID-19 which continued to constitute PHEIC [16], as well as the recent re-emergence of monkeypox, jointly urged the identification of effective border policies and the optimal long-term implementation strategy with minimum negative impacts [17]. However, there remained many knowledge gaps and arguments about whether implementing border policies were useful in the overall epidemic control. To be specific, border restrictions were once identified effective in suppressing early COVID-19 epidemics [18,19], whereas they were considered ineffective in regions where there already existed severe community spreads [[20], [21], [22]], implicating that conclusions may vary in different timings of observations. In fact, since outbreaks usually precede the adoption of border policies, previous observational studies performing in relatively short-term (Ranged form 14–153 days. See the literature review in Supplementary Table S1) may hard to untangle such confused ordinal relationship, which may introduce bias and uncertainty to the effectiveness evaluation of border policies. On the other hand, despite model simulations, the impact of border policies on long-term epidemics was yet to be assessed by using real-world evidence, which is also necessary for comparisons with those short-term explorations. Besides, handful studies compared different stringency border controls and identified effective measures for specific epidemic severity countries, and the extent was far from sufficient to inform border policy optimization.
Reliable quantification of the border policy effectiveness with real-world empirical evidences will not only offer advice on the extent of reopening the border during COVID-19 pandemic, but also contribute to improving the global preparedness and responses in future disease outbreaks. To overcome aforementioned deficiencies, in this study we collected international responses and COVID-19 transmission data in 2020–2021, years with major global waves of COVID-19 and its variants, in order to map the global spatiotemporal disparity of adopting and maintaining border policies and more importantly, to estimate their effectiveness in long-term epidemic control across different transmission severity countries.
2. Methods
2.1. Data source and collection
2.1.1. Global responses, transmission and tourism data
We obtained international travel policy data recorded between 01 January 2020 to 31 December 2021 from the Oxford COVID-19 Government Response Tracker (OxCGRT) database [23]. All information of policies have been classified to four stringency levels (from level-1 to 4: screening, quarantine, ban on regions and total border closure). Such classification has been widely used in previously published studies [[24], [25], [26]]. We then manually identified the daily stringency level for each country according to its highest policy level. For example, assuming that there were policies of screening, quarantine and ban on regions simultaneously, then the third measure represented the overall stringency level for the day. With aggregated data, we firstly described the varying proportion of global border policy adoption throughout the study period. Subsequently, country-specific cumulative duration of each policy level in 2020–2021 was separately calculated.
Global COVID-19 transmission data was gathered from Johns Hopkins University Coronavirus Research Centre dataset [27]. Similarly, the cumulative morbidity and mortality between 01 January 2020 to 31 December 2021 were calculated by country. We also screened other databases regarding global responses and transmissions (e.g. the WHO Public Health and Social Measures Dataset [28], the ACAPS government measures dataset [29] and United States Centers for Disease Control and Prevention COVID Data Tracker Weekly Review [30]) as supplements for validation. Tourism data including the total number of inbound arrivals during the study period was collected from United Nations World Tourism Organization (UNWTO) dataset [31].
2.1.2. Control variables
To control for the latest country-specific social-economic and health resource situation, at the initial step of model development, we included a list of factors that were known or believed to affect COVID-19 spreading. For example, socio-demographic index (SDI) and the number of physicians per 1000 people, reflecting the socio-demographic level and health capacity of countries respectively, were proven to correlate with health outcomes [32]. Besides, population density and the share of the population aged over 65 may influence the COVID-19 morbidity and mortality [33]. Moreover, we also control for the political characteristics of the quality of government and the economic conditions including GDP (gross domestic product) per capita, unemployment rate and globalization index, since countries with higher government capacity may better cope with such crisis, and the healthy economic may ensure sufficient resources to combat with COVID-19 [34]. The detailed description and source of these control variables were listed in Table 1 .
Table 1.
Data source and information of control variables.
| Variable | Description | Source |
|---|---|---|
| Unemployment | The share of the labor force without work. | World Bank [35] |
| KOF globalization index | An index measured the economic, social and political dimensions of globalization. | KOF Swiss Economic Institute [36] |
| Quality of government | The assessment of government capacity considering three dimensions of “corruption”, “law and order” and “bureaucracy quality”. | University of Gothenburg [37] |
| Socio-demographic index | An index used to evaluate social development based on average income per person, educational attainment, and total fertility rate (TFR). | Institute for Health Metrics and Evaluation [38] |
| Population density | A measurement of the number of people per square kilometre. | World Bank [39] |
| Population ages 65+ | The proportion of individuals aged 65 and over among the total population | World Bank [40] |
| GDP per capita | A financial metric of gross domestic product (GDP) per person | World Bank [41] |
| Physicians (per 1000 people) | Number of medical doctors include generalist physicians and specialist medical practitioners per 1000 population. | World Health Organization [42] |
2.2. Statistical analysis
Firstly, despite the aforementioned descriptive analysis, we further estimated the cumulative distribution with important percentiles of global border policy duration for within- and between-policy comparisons. To be specific, international duration data of each policy was separately incorporated into the accelerated failure time model with three time-to-event parametric distribution (i.e. Log-normal, Weibull, and Gamma) [43,44]. The best fitted model were selected based on Akaike Information Criterion, and 95% confidence intervals for each estimated percentile were generated by using Bootstrapped and Markov chain Monte Carlo methods. Such estimation was further stratified by world bank income groups and WHO regions, and the significance of differences between groups and regions were examined using non-parametric Kruskal-Wallis tests.
Secondly, we applied multivariable quantile regression model with aforementioned control variables to comprehensively examine the relationship between the cumulative duration of each policy and total COVID-19 case incidence. By modeling different quantiles of the latter, we were able to the study border policy effectiveness in suppressing epidemics across low (25th quantile), medium (50th quantile) and high (75th quantile) level of transmission severity countries. Such method also enable us to avoid the influence of the timing of the policy adoption and its confusing relationship with short-term transmission fluctuations. As comparisons, such association was also analyzed by using Ordinary least squares (OLS) regression models. To further control for the vaccination progression and the domestic response intensity of countries, we collected country-specific vaccination information and re-calculated the cumulative stringency index [23] in 2020–2021 which combined information of seven domestic interventions (e.g. school closure, restrictions on gathering). However, we here did not include these two variables in the final model due to the considerable colinearity (Assessed by using the variance infation factor, VIF; See results in Supplementary Table S2) when introducing them to the regression model, as well as the consideration of the limited effect of currently available vaccine in blocking COVID-19 transmissions (especially when confronting Delta [45] and Omicron variants [46]).
To explore the potential determinant to border policy effectiveness, we quantified the capability of four policies in managing the total arrivals by examining the relationship between cumulative border policy duration and the total number of inbound tourists. Sensitivity analysis of the association between policy duration and COVID-19 mortality was conducted to examine the robustness of our results. In addition, the role of imported travelers in the epidemic progression was assessed by using total arrivals to forecast COVID-19 cases and deaths. All analyses were conducted by using R software (version 4.1.2, R Foundation; Vienna, Austria).
3. Results
3.1. The adoption and maintenance of international travel restrictions
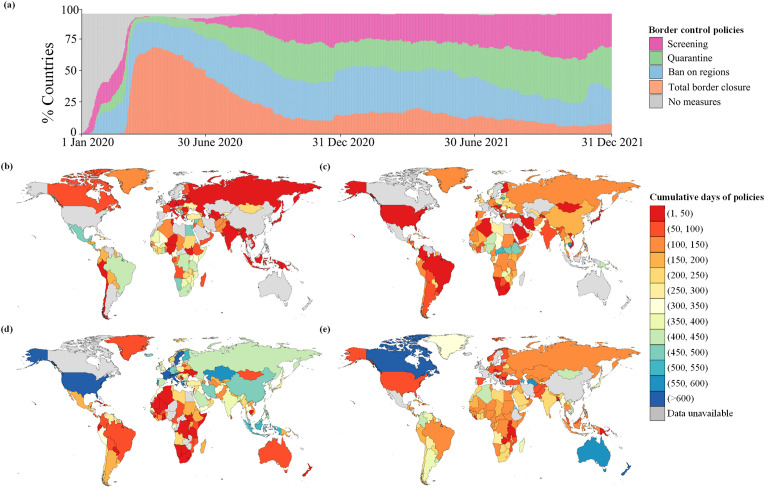
We found vast disparities existed between countries in applying and maintaining international travel restrictions. Fig. 1 a visualized the varying proportion of global travel restrictions implementing from 01 January 2020 to 31 December 2021 (See country-specific visualization in Supplementary Fig. S2). Among 185 countries and regions that were identified with border policy data, 77.3% (n = 143) countries have introduced the policy of screening inbound arrivals in 2020–2021, 84.9% (157) have applied border quarantine, 92.4% (171) have imposed travel bans on high-risk regions, and 83.2% (154) have conducted total border closure. Globally, total border closure was cumulatively applied over 100 days in 34.1% (63) countries, while 0.09% (17) implemented such policy over 300 days and 0.01% (2) over 600 days. Besides, the policy of ban on regions was maintained over 100 days in 41.6% (77) countries, over 300 days in 20.1% (38) countries and over 600 days in 0.04% (7) countries. The diversity of border policy maintenance across countries was also reflected in the context of quarantine and screening arrivals (Fig. 1d‒e). Countries not shown in the map due to without any information of border policy adoptions (n = 34) were listed in Supplementary Table S3.
Fig. 1.
The proportion and cumulative duration of international travel restrictions in 2020–2021. Daily proportion of global border policy implementation (a); Country-specific cumulative duration in maintaining screening (b), quarantine (c), ban on regions (d) and total border closure (e). “No measures” represented no restrictions on international travel (level-0); “Data unavailable” indicated regions with no records of the specific policy implementation; Administrative boundaries were adapted from the database of Global Administrative Areas (GADM).
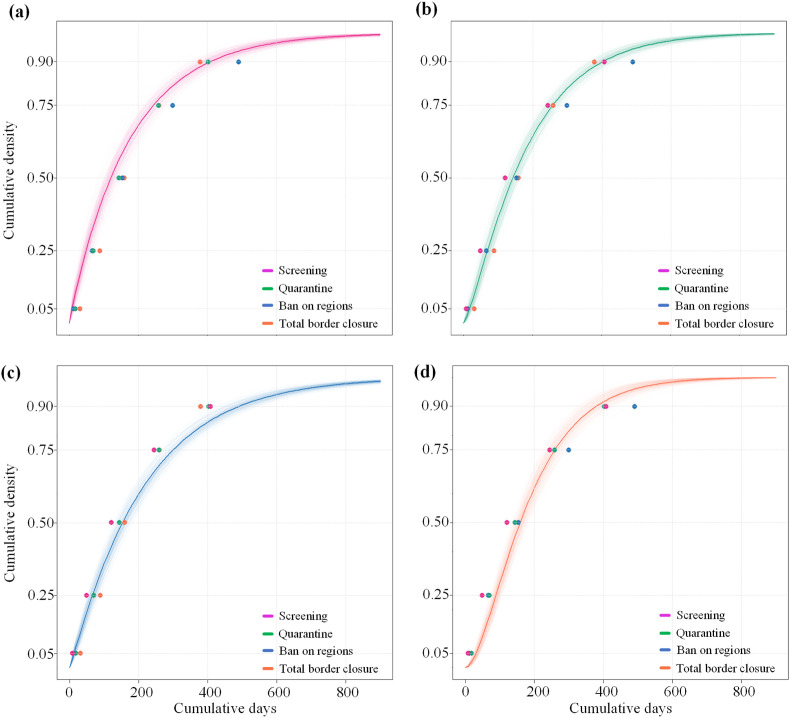
We also found the global preference of border policy implementations was different between in short-term and long-term (Fig. 2 ). According to the global border policy duration distribution, ban on regions was generally the most durable policy among all long-lasting applications (according to percentile estimates above the median) in 2020–2021, while in the short run (percentiles below the median), total border closure was applied the longest among all policies.
Fig. 2.
Estimated cumulative distribution of global border policy duration. Screening (a); Quarantine (b); Ban on regions (c); Total border closure (d). Colored points represented the mean percentile estimates of each policy.
Moreover, border policies were maintained with significant differences between different income groups and WHO regions (except for the inbound quarantine maintenance between WHO regions, Table 2 ). While high income countries hold the longest median duration of ban on regions (284.5 days, 95% confidence interval: 234.4–340.4) and the shortest of the level of screening (55.2, 95% CI: 36.5–81.2) simultaneously, low income countries applied lower level measures of screening (164.2, 95% CI: 106.3–230.0) and quarantine (197.2, 95% CI: 147.2–255.2) the longest. Similar trend can also be found in estimations stratified by WHO regions, with the longest median estimates of screening (180.0, 95% CI:134.3–236.7) in the Africa Region and that of ban on regions (263.2, 95% CI: 203.8–327.5) in the European Region. Other percentile estimates of the distribution can be found in Supplementary Table S6‒9.
Table 2.
Median estimates of the border policy durationadistribution stratified by income groups and WHO regions. Values are days (95% confidence interval).
| Analyses | Screening | Quarantine | Ban on regions | Total border closure |
|---|---|---|---|---|
| Income groups | ||||
| Low | 164.2 (106.3–230.0) | 197.2 (147.2–255.2) | 82.0 (49.1–128.9) | 123.8 (85.5–173.8) |
| Lower-middle | 150.1 (107.2–198.2) | 137.0 (101.5–180.2) | 116.0 (85.5–158.6) | 172.7 (142.5–207.3) |
| Upper-middle | 154.9 (108.1–215.2) | 117.2 (86.0–158.0) | 134.5 (94.3–192.0) | 166.4 (132.7–206.1) |
| High | 55.2 (36.5–81.2) | 130.9 (91.6–176.1) | 284.5 (234.4–340.4) | 162.1 (123.3–209.3) |
| Kruskal-Wallis test | p < 0.05 | p < 0.10 | p < 0.05 | p < 0.05 |
| WHO regions | ||||
| EUR | 71.3 (44.6–107.6) | 148.8 (112.8–193.9) | 263.2 (203.8–327.5) | 104.0 (80.2–134.5) |
| AMR | 166.9 (109.8–234.2) | 125.2 (84.2–179.5) | 108.9 (75.4–154.1) | 205.3 (163.0–258.1) |
| AFR | 180.0 (134.3–236.7) | 171.1(132.7–215.2) | 62.0 (40.0–89.9) | 141.9 (111.7–175.7) |
| SEAR | 47.2 (29.2–73.7) | 189.3 (123.5–271.0) | 222.1 (126.3–347.9) | 151.6 (88.1–237.7) |
| WPR | 30.3 (15.8–58.8) | 94.5 (48.9–158.2) | 208.0 (137.6–293.6) | 270.8 (182.7–383.4) |
| EMR | 129.2 (74.9–200.6) | 147.6 (83.9–230.7) | 208.4 (142.8–273.0) | 137.4 (116.4–160.2) |
| Kruskal-Wallis test | p < 0.05 | p > 0.10 | p < 0.05 | p < 0.05 |
Note: WHO: World Health Organization; EUR: Europe; AMR: Americas; AFR: Africa; SEAR: South-East Asia; WPR: Western Pacific; EMR: Eastern Mediterranean.
Border policy duration: cumulative time of each border policy applied in 2020–2021.
3.2. Effectiveness of border policies in restraining long-term epidemics
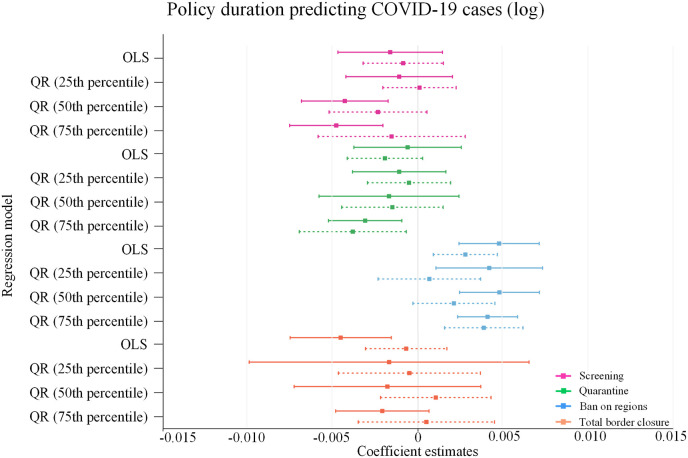
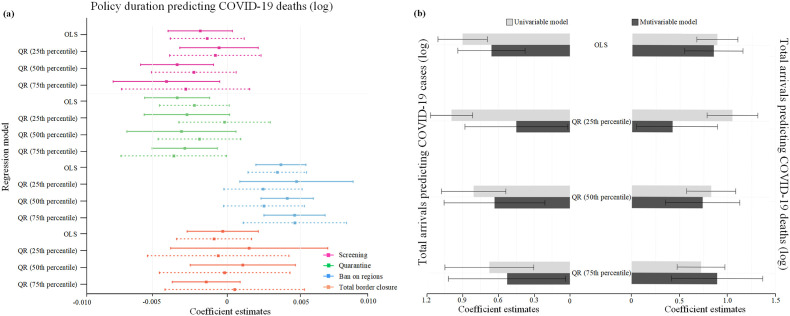
Notably, in the regression analysis, the significant association between the policy duration increment and lower COVID-19 infections was only presented in the 75th quantile regression of the border quarantine policy (coefficient estimates [β] = −0.0038, 95% confidence interval: −0.0066 to −0.0010), while countires with longer time of ban on regions, showed strong associations with higher COVID-19 cases in the OLS (β = 0.0028, 95% confidence interval: 0.0009–0.0047) and 75th quantile regression (β = 0.0039, 95%CI: 0.0014–0.0063) analyses, indicating its ineffective role in the long-term epidemic of countries with medium and high level of transmission severity. Besides, no significant effects were found in other policies, including the most restrictive measure of total border closure (Fig. 3 ).
Fig. 3.
Coefficients of cumulative border policy duration predicting COVID-19 infections. Solid and dashed lines represented univariate and multivariate regression estimates respectively. See full regression results in Supplementary Table S10‒13. OLS: Ordinary least squares regression, QR: quantile regression.
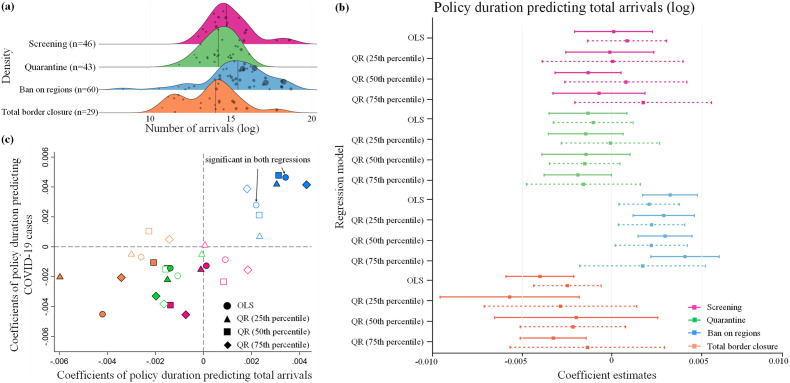
We also found that the effectiveness of border policies in suppressing COVID-19 epidemics was associated with their capability in managing total inbound arrivals. As shown in the density plot (Fig. 4 a), those countries applying the policy of ban on regions the longest among all measures also obtained the highest median number of total arrivals. Besides, in OLS and quantile regression analyses (Fig. 4b) with control variables (Table 1), countries with longer duration of ban on regions were showed positive associations with higher volume of total arrivals (OLS regression, β = 0.0022, 95% CI: 0.0004–0.0040; 25th quantile regression, β = 0.0023, 95% CI: 0.0004–0.0043; 50th quantile regression, β = 0.0023, 95% CI: 0.0002–0.0044). In addition, the upper right location of the scatter plot (Fig. 4c), which combined regression results of policy duration predicting COVID-19 cases and total arrivals, demonstrated the limited capability of countries with longer duration of ban on regions in managing both total arrivals and COVID-19 infections.
Fig. 4.
The relationship between cumulative border policy duration, the number of total arrivals and COVID-19 incidence. Density plots of the tourist volume in four categories countries that applied each policy the longest. Size of the circle represented the quantity of confirmed COVID-19 cases and the vertical line marked the median of total arrivals (a); Coefficients of cumulative border policy duration predicting total arrivals (b); Scatter plot by combining coefficient estimates of border policy duration predicting total arrivals and COVID-19 infections (c). Solid and hollow shapes represented univariate and multivariate regression estimates respectively. See full regression results in Supplementary Table S14‒17.
Multiple sensitivity analyses ensured the robustness of our findings. Firstly, results using policy duration predicting the number of COVID-19 deaths (log) were generally consistent with those of predicting COVID-19 morbidity (Fig. 5 a). In particular, countries with longer duration of ban on regions remained significantly associated with higher mortality in OLS (β = 0.0036, 95% CI: 0.0015–0.0056) and 75th quantile regression (β = 0.0048, 95% CI: 0.0011–0.0085), while the coefficients of border quarantine policy remained positive in 75th quantile regression (β = −0.0030, 95% CI: −0.0054 to −0.0007). On the other hand, in all regression analyses with control variables, countries with higher number of total arrivals obtained significant association with more COVID-19 infections and deaths (Fig. 5b).
Fig. 5.
Sensitivity analysis of the border policy effectiveness in suppressing COVID-19 mortality and using total arrivals in COVID-19 forecasting. Coefficients of cumulative border policy duration predicting COVID-19 deaths. (a); Coefficients of total arrivals predicting COVID-19 morbidity and mortality (b). See full regression results in Supplementary Table S18‒23.
4. Discussion
This study mapped the global diversity of border policy maintenance in 2020–2021 and assessed international and regional border policy adherence. Moreover, we systematically evaluated the relationship between the cumulative duration of four policy levels and COVID-19 morbidity and mortality. As the results, inbound quarantine were identified as effective policies in mitigating severe epidemics. Besides, the policy of ban on regions was demonstrated with the ineffective and potentially facilitating role in long-term epidemic progression, which contradicted to the results in previous studies [[47], [48], [49]]. Such findings revealed the difference of border policy effectiveness between in short-term and long-term applications, and may help improve decision-making on long-term border strategies against COVID-19 and other emerging global health threats. Additionally, we observed the concurrent uptrend between the tourist growth and higher COVID-19 infections and deaths, which was generally consistent with the evidence in prior studies [50,51].
As Bickley et al. [26] previously concluded that countries with higher globalization may be less likely to implement highly restrictive travel measures in the beginning of the pandemic, in this study, we found that more developed countries (i.e. high income groups and European Region) applied higher stringency policies (i.e. ban on regions) the longest in 2020–2021, indicating that the preferred border policies of those countries may vary as the pandemic progressed. Besides, we here offered insights for international tourists to improve their travel schedules before the departure.
Amid the COVID-19 pandemic, COVID-safe travel zone referred to as “travel bubbles” was established to ease travel restrictions between member countries and reconnect their economic and trade (e.g. Austria and Germany, Croatia and Slovenia, Denmark and Norway) [52]. However, except the potential discrimination and inequality for non-member countries, according to our results, such policy did not fulfill the long-term mission in the aspect of suppressing COVID-19 epidemics, since the uncontrolled number of tourists from partner nations may also increase the importing transmission risk. Considering its negative impacts and the imperfect performance in epidemic control, ban on high-risk regions may not be the ideal long-term border strategy. On the other hand, we found that longer duration of total border closure was significantly associated with higher tourist reduction but remained insignificant in reducing COVID-19 mortality and morbidity. One possible reason is that such extremely stringent measures were usually adopted by countries with rather severe transmissions, and the comprehensive community spreading might be already beyond control even for total lockdown [53].
Additional sensitivity analyses were performed to further examine the robustness of our results. We explored the impact of country-specific population size and domestic measures on the relationship between border policy duration and COVID-19 incidence (Supplementary Fig. S3‒5) respectively. Results of those analyses were generally in consistent with our findings in the main analysis. Notably, when we set the studying period to the beginning of the pandemic (January to October 2020) [26], we found that the policy of ban on regions showed no significance of ineffectiveness in the regression and correlation analysis (Supplementary Fig. S6). One possible reason is that in the initial stage of pandemic, the epicenters were restricted to certain countries, and such implementation may be more effective than in latter time [[47], [48], [49]].
Important strengths were presented in this study. To the best of our knowledge, it is the first attempt to broadly assess the effectiveness across all levels of border policies against COVID-19 from the long-term perspective. Our real-world data based analyses successfully captured the heterogeneous effectiveness of border policies across various transmission severity countries, and revealed the ineffectiveness of ban on regions in suppressing long-term epidemics. Admittedly, several limitations existed in this study. Since all policy information have been generally classified to four levels, variations within each policy level remained to be assessed by future studies with available data. On the other hand, although the robustness of our results were verified by multiple sensitivity analyses, our quantification was still based on the association rather than casuation. Besides, with currently available methodology, we were unable to decompose the independent effect from the combination of vaccination, domestic interventions and border policy implementations on COVID-19 epidemic control. Developing more powerful analytic tools to deal with this issue was challenging but necessary.
5. Conclusion
Vast disparities existed between countries in applying and maintaining international travel restrictions, especially between high and low-income countries. According to our findings, lower level border polices of quarantine arrivals were effective and sufficient for mitigating severe COVID-19 epidemics. On the contrary, as more stringent measures, the long-lasting implementation of bans on regions was not recommended in countries where there already existed medium or high COVID-19 transmissions, since it did not well suppress the total number of inbound tourists and subsequent cross-border disease diffusion. Our findings offered valuable evidences for long-term border strategy optimization against COVID-19 pandemic and future global concerns.
Funding
This work was supported by the grant of the major science and technology project of Shanxi province (Grant number: 202102130501003, 202005D121008; Recipient: Tong Wang), special foundation on COVID-19 of Shanxi health commission (16; Tong Wang), National Key Research and Development Program of China (2021YFC2301603), and the project of Institutional Development of the Sun Yat-sen Center for Migrant Health Policy funded by United States China Medical Board (12–111; Li Ling).
Authors’ contributions
Study design and methodology: ZY L, JG X, L L, T W; Parameters and data collection: BR Y, JL W, YC W; Statistical analysis: ZY L, BR Y, JL W; Writing and visualization: ZY L, BR Y. Supervision: JG X, L L, T W. All authors have read and approved the final manuscript.
CRediT authorship contribution statement
Zhiyao Li: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Formal analysis, Validation, Visualization. Boran Yang: Data curation, Visualization. Jiale Wang: Data curation. Yanchao Wen: Data curation. Jianguo Xu: Supervision. Li Ling: Funding acquisition, Supervision. Tong Wang: Methodology, Funding acquisition, Supervision.
Declaration of competing interest
The authors declare that they have no actual or potential competing interests.
Acknowledgments
We would like to thank Shanxi department of science and technology for the grant of major science and technology project of Shanxi province (Grant number: 202102130501003, 202005D121008), Shanxi health commission for the grant of the special foundation on COVID-19 (16), National Nature Science Foundation of China for the grant of National Key Research and Development Program of China (2021YFC2301603), and United States China Medical Board for funding the project of Institutional Development of the Sun Yat-sen Center for Migrant Health Policy(12–111). We also appreciate the contribution of data collecting team (Zichun Han, Ruifan Li, Yanchao Wen, Jiale Wang, Boran Yang).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.tmaid.2023.102556.
Abbreviations
- WHO
World Health Organization
- PHEIC
Public health emergency of international concern
- RT-PCR
Reverse transcription polymerase chain reaction
- OxCGRT
Oxford COVID-19 Government Response Tracker
- SDI
Socio-demographic index
- GDP
Gross domestic product
- OLS
Ordinary least squares
- QR
Quantile regression
- CI
Confidence interval
- NPIs
Non-pharmaceutical interventions
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Chinazzi M., Davis J.T., Ajelli M., et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gu W., Deng X., Reyes K., et al. Associations of early COVID-19 cases in san francisco with domestic and international travel. Clin Infect Dis. 2020;71(11):2976–2980. doi: 10.1093/cid/ciaa599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Erim D.O., Oke G.A., Adisa A.O., et al. Associations of government-mandated closures and restrictions with aggregate mobility trends and SARS-CoV-2 infections in Nigeria. JAMA Netw Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.32101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vanderslott S., Marks T. Travel restrictions as a disease control measure: lessons from yellow fever. Global Publ Health. 2021;16(3):340–353. doi: 10.1080/17441692.2020.1805786. [DOI] [PubMed] [Google Scholar]
- 5.Rahman Qureshi U.U., Saleem S., Khan A., et al. Outbreak of novel Corona virus (2019-nCoV); implications for travelers to Pakistan. Trav Med Infect Dis. 2020;34 doi: 10.1016/j.tmaid.2020.101571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Z.B., Li L., Qin P.Z., et al. Countries of origin of imported COVID-19 cases into China and measures to prevent onward transmission. J Trav Med. 2020;27(8) doi: 10.1093/jtm/taaa139. taaa139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Monkeypox: situation report. 14 june 2022. https://www.who.int/health-topics/monkeypox
- 8.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ohlsen E.C., Porter K.A., Mooring E., et al. Airport traveler testing Program for SARS-CoV-2 - Alaska, june-november 2020. MMWR Morb Mortal Wkly Rep. 2021;70(16):583–588. doi: 10.15585/mmwr.mm7016a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bisanzio D., Reithinger R., Alqunaibet A., et al. Estimating the effect of non-pharmaceutical interventions to mitigate COVID-19 spread in Saudi Arabia. BMC Med. 2022;20(1):51. doi: 10.1186/s12916-022-02232-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lin C., Braund W.E., Auerbach J., et al. Policy decisions and use of information technology to fight COVID-19, Taiwan. Emerg Infect Dis. 2020;26(7):1506–1512. doi: 10.3201/eid2607.200574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gómez-Ríos D., Ramirez-Malule D., Ramirez-Malule H. The effect of uncontrolled travelers and social distancing on the spread of novel coronavirus disease (COVID-19) in Colombia. Trav Med Infect Dis. 2020;35 doi: 10.1016/j.tmaid.2020.101699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwok W.C., Wong C.K., Ma T.F., et al. Modelling the impact of travel restrictions on COVID-19 cases in Hong Kong in early 2020. BMC Publ Health. 2021;21(1):1878. doi: 10.1186/s12889-021-11889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burki T.K. COVID-19 in the caribbean. Lancet Respir Med. 2021;9(4):e46. doi: 10.1016/S2213-2600(21)00090-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quach H.L., Hoang N.T., Nguyen C.K., et al. Successful containment of a flight-imported COVID-19 outbreak through extensive contact tracing, systematic testing and mandatory quarantine: lessons from Vietnam. Trav Med Infect Dis. 2021;42 doi: 10.1016/j.tmaid.2021.102084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization COVID-19: situation report. 14 june 2022. https://www.who.int/health-topics/monkeypox
- 17.Besançon L., Flahault A., Meyerowitz-Katz G. Mobility during the pandemic: how did our movements shape the course of COVID-19? J Trav Med. 2022;29(3) doi: 10.1093/jtm/taac055. taac055. [DOI] [PubMed] [Google Scholar]
- 18.Liebig J., Najeebullah K., Jurdak R., et al. Should international borders re-open? The impact of travel restrictions on COVID-19 importation risk. BMC Publ Health. 2021;21(1):1573. doi: 10.1186/s12889-021-11616-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gwee S.X.W., Chua P.E.Y., Wang M.X., et al. Impact of travel ban implementation on COVID-19 spread in Singapore, Taiwan, Hong Kong and South Korea during the early phase of the pandemic: a comparative study. BMC Infect Dis. 2021;21(1):799. doi: 10.1186/s12879-021-06449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Espinoza B., Castillo-Chavez C., Perrings C. Mobility restrictions for the control of epidemics: when do they work? PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0235731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russell T.W., Wu J.T., Clifford S., et al. Effect of internationally imported cases on internal spread of COVID-19: a mathematical modelling study. Lancet Public Health. 2021;6(1):e12–e20. doi: 10.1016/S2468-2667(20)30263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Timur L., Xie Y. Is border closure effective in containing COVID-19? Trav Med Infect Dis. 2021;44 doi: 10.1016/j.tmaid.2021.102137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee K., Grépin K.A., Worsnop C., et al. Managing borders during public health emergencies of international concern: a proposed typology of cross-border health measures. Glob Health. 2021;17(1):62. doi: 10.1186/s12992-021-00709-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.University of Oxford Coronavirus government response tracker. Blavatnik school of government. https://www.bsg.ox.ac.uk/research/research-projects/coronavirus-government-response-tracker
- 25.Yang B., Sullivan S.G., Du Z., et al. Effectiveness of international travel controls for delaying local outbreaks of COVID-19. Emerg Infect Dis. 2022;28(1):251–253. doi: 10.3201/eid2801.211944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bickley S.J., Chan H.F., Skali A., et al. How does globalization affect COVID-19 responses? Glob Health. 2021;17(1):57. doi: 10.1186/s12992-021-00677-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johns Hopkins University. coronavirus https://coronavirus.jhu.edu.html
- 28.WHO. Tracking Public Health and Social Measures, A Global Dataset. Geneva. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/phsm.2021. Accessed 1 August 2022.
- 29.ACAPS COVID-19 – government measures. https://www.acaps.org/projects/covid19/data
- 30.US Centers for Disease Control and Prevention COVID data tracker WeeklyReview. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html
- 31.World tourism organization Unwto tourism data dashboard. https://www.unwto.org/unwto-tourism-dashboard
- 32.Chen Z., Zheng W., Wu Q., et al. Global diversity of policy, coverage, and demand of COVID-19 vaccines: a descriptive study. BMC Med. 2022;20(1):130. doi: 10.1186/s12916-022-02333-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sebhatu A., Wennberg K., Arora-Jonsson S., et al. Explaining the homogeneous diffusion of COVID-19 nonpharmaceutical interventions across heterogeneous countries. Proc Natl Acad Sci U S A. 2020;117(35):21201–21208. doi: 10.1073/pnas.2010625117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Capano G., Howlett M., Jarvis D.S.L., et al. Mobilizing policy (In)Capacity to fight COVID-19: understanding variations in state responses. Polic Soc. 2020;39(3):285–308. doi: 10.1080/14494035.2020.1787628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Bank. Unemployment https://data.worldbank.org/indicator/SL.UEM.TOTL.NE.ZS
- 36.Gygli S., Haelg F., Potrafke N., Sturm J.E. The KOF globalisation index–revisited. Rev Ind Organ. 2019;14:543–574. doi: 10.1007/s11558-019-09344-2. [DOI] [Google Scholar]
- 37.University of Gothenburg The quality of government. https://www.gu.se/en/quality-government/qog-data
- 38.Institute for Health Metrics and Evaluation Socio-demographic index. https://www.healthdata.org/taxonomy/glossary/socio-demographic-index-sdi
- 39.World Bank Population density. https://data.worldbank.org/indicator/EN.POP.DNST?name_desc=false
- 40.World Bank Population ages 65 and above. https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?view=bar
- 41.World Bank GDP per capita. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?name_desc=false
- 42.World Health Organization Indicators. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/physicians-density-(per-1000-population
- 43.Li Z.Y., Zhang Y., Peng L.Q., et al. Demand for longer quarantine period among common and uncommon COVID-19 infections: a scoping review. Infect Dis Poverty. 2021;10(1):56. doi: 10.1186/s40249-021-00847-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reich N.G., Lessler J., Cummings D.A., et al. Estimating incubation period distributions with coarse data. Stat Med. 2009;28(22):2769–2784. doi: 10.1002/sim.3659. [DOI] [PubMed] [Google Scholar]
- 45.Elliott P., Haw D., Wang H., et al. Exponential growth, high prevalence of SARS-CoV-2, and vaccine effectiveness associated with the Delta variant. Science. 2021;374(6574) doi: 10.1126/science.abl9551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chenchula S., Karunakaran P., Sharma S., et al. Current evidence on efficacy of COVID-19 booster dose vaccination against the Omicron variant: a systematic review. J Med Virol. 2022;94(7):2969–2976. doi: 10.1002/jmv.27697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schermerhorn J., Case A., Graeden E., et al. Fifteen days in December: capture and analysis of Omicron-related travel restrictions. BMJ Glob Health. 2022;7(3) doi: 10.1136/bmjgh-2022-008642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang J., Li J., Lai S., et al. Uncovering two phases of early intercontinental COVID-19 transmission dynamics. J Trav Med. 2020;27(8) doi: 10.1093/jtm/taaa200. taaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsuboi M., Hachiya M., Ohtsu H., et al. Epidemiology and risk of coronavirus disease 2019 among travelers at airport and port quarantine stations across Japan: a nationwide descriptive analysis and an individually matched case-control study. Clin Infect Dis. 2022;74(9):1614–1622. doi: 10.1093/cid/ciab659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Salazar P.M., Niehus R., Taylor A., et al. Identifying locations with possible undetected imported severe acute respiratory syndrome coronavirus 2 cases by using importation predictions. Emerg Infect Dis. 2020;26(7):1465–1469. doi: 10.3201/eid2607.200250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gu W., Deng X., Reyes K., et al. Associations of early COVID-19 cases in san francisco with domestic and international travel. Clin Infect Dis. 2020;71(11):2976–2980. doi: 10.1093/cid/ciaa599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sharun K., Tiwari R., Natesan S., et al. International travel during the COVID-19 pandemic: implications and risks associated with 'travel bubbles. J Trav Med. 2020;27(8):taaa184. doi: 10.1093/jtm/taaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kwok W.C., Wong C.K., Ma T.F., et al. Modelling the impact of travel restrictions on COVID-19 cases in Hong Kong in early 2020. BMC Publ Health. 2021;21(1):1878. doi: 10.1186/s12889-021-11889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.