Abstract
Ductal adenocarcinoma is an aggressive prostate cancer often presenting late due to low serum PSA. A variant presentation of ductal adenocarcinoma occurs with formation of large cystic structures in the prostate, often associated with lower urinary tract symptoms. We present a case illustrating investigation and successful management of a macrocytic ductal carcinoma in a 90 year old patient.
Highlights
-
•
Consider ductal prostate cancer as a differential diagnosis for pelvic cystic mass.
-
•
Macrocystic ductal carcinoma can often present with obstructive urinary symptoms.
-
•
TURP may provide adequate management for macrocystic ductal carcinoma in the frail.
1. Introduction
Macroscopic cyst formation by ductal adenocarcinoma of the prostate is rare with only a small number of cases reported in the literature, with incidence thought to be 0.32%.1 Ductal adenocarcinomas are traditionally managed as a high risk cohort and are considered more aggressive than acinar adenocarcinoma of the prostate. These cancers typically present with lower mean serum Prostate Specific Antigen (PSA) levels,2 and can have local treatment failure and metastases with a low PSA.
Presentations of macrocystic ductal adenocarcinoma can vary, at times asymptomatic, presenting with obstructive urinary or gastrointestinal symptoms, or even with painful defecation. We present a case of a large macrocystic mass found to be ductal adenocarcinoma treated with minimal intervention showing a favorable short to medium term outcome.
2. Case report
A 90 year old man presented for review of lower urinary tract symptoms (LUTS) including nocturia, hesitancy, intermittency and dribbling as well as constipation. He had an International Prostate Symptom Score (IPSS) of 24 + 5. Past medical history included diabetes mellitus, hypertension, dyslipidemia, chronic obstructive pulmonary disease being an ex-smoker and gout. He had undergone a transurethral resection of his prostate (TURP) 25 years prior. Digital rectal examination revealed a large, non-tender, smooth pelvic mass arising from the right side of the prostate. Serum PSA returned at 5.0 ng/ml, having been 2.49 ng/ml a year prior.
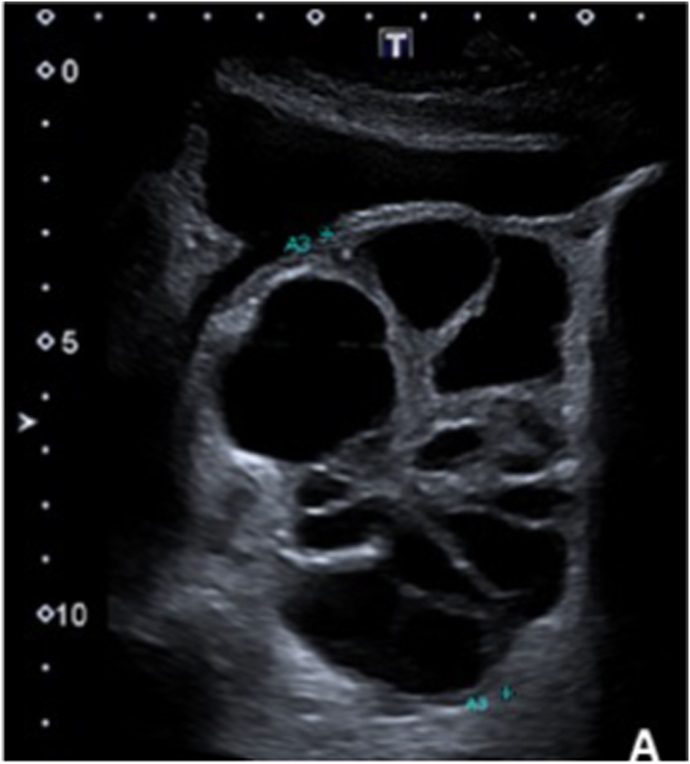
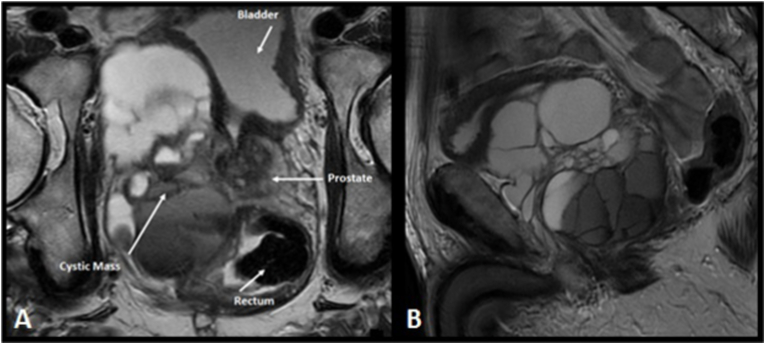
An ultrasound was arranged which revealed a cystic lesion closely related to the prostate (Fig. 1). Magnetic Resonance Imaging revealed a 10 cm septated cystic mass in the pelvis, displacing the right side of the prostate, bladder and rectum (Fig. 2). The right seminal vesicle could not be seen.
Fig. 1.
Ultrasound of cystic pelvic mass. “Long view” showing cystic mass in pelvis. Index highlighting centimetres on x and y axis.
Fig. 2.
Pre-operative Magnetic Resonance Imaging of cystic pelvic mass. A) Axial T2 magnetic resonance imaging of pelvis highlighting relationship between prostate, cystic mass, bladder and rectum. B) Sagittal T2 Magnetic resonance imaging.
Cystoscopy revealed a small TURP cavity with no evidence of regrowth. Due to a tight bladder neck, a bladder neck incision (BNI) was performed. Prostate tissue on the right lateral wall was resected and a large, septated, cystic cavity was entered which drained copious blood stained fluid. The wall and septae of the cavity showed tumour with a papillary configuration. Further resection was carried out in order to marsupialize the cystic structure. The walls and septae were highly vascular and there was significant bleeding encountered, requiring Floseal to be injected via the cystoscope, in addition to copious diathermy. An indwelling catheter was left for 5 days. Histology of the resection specimens revealed pure prostatic ductal adenocarcinoma (Gleason 4 + 4 = 8, Grade Group 4).
Post procedure the patient had complete resolution of his urinary and bowel symptoms. Staging imaging with computerised tomography (CT) and bone scan showed no evidence of metastatic disease. In the context of his age and comorbidities, a conservative approach to management was adopted, with androgen deprivation therapy (ADT).
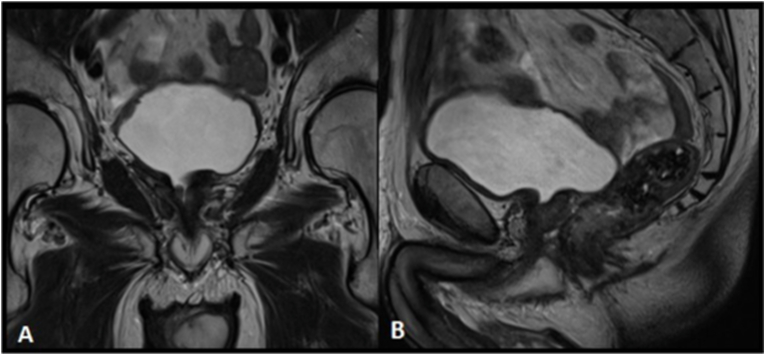
On most recent follow up, almost 2 years post TURP, his PSA remains undetectable (<0.01ng/ml). In the context of recurrence of mild LUTS an MRI was arranged (Fig. 3), which showed complete resolution of the large cystic mass.
Fig. 3.
Post-operative surveillance Magnetic Resonance Imaging illustrating resolution of cystic mass. A) Coronal T2 magnetic resonance imaging. B) Sagittal T2 magnetic resonance imaging.
3. Discussion
Ductal carcinoma is known to typically progress aggressively, however management specifically for patients with macrocystic disease is not well documented, with a recent review in Nature failing to mention this variation of disease presentation.3 Although ductal carcinoma can be seen within all regions of the prostate including the peripheral zones, it is typically seen in the central transition zone. Malignant growth in this area is in keeping with associated symptoms of the lower urinary as well as macroscopic heamaturia.
As this malignancy is frequently seen in the transition zone and able to be appreciated macroscopically due to the gross cystic appearance, local resection with TURP may be an appropriate initial step for surgical management in select cases. Current guidelines suggest management with either radical surgical or radiation treatments, but do not outline any role for local resection alone.3 We propose that frail and comorbid patients, presenting with macrocystic ductal prostate adenocarcinoma may be adequately treated by a surgically conservative approach with TURP and marsupialisation of the cystic sac, as previously suggested by Aydin et al.4
4. Conclusion
Macrocystic ductal carcinoma of the prostate should be considered as a rare differential for patients presenting with LUTS with an associated cystic pelvic mass. Our case illustrates an example of favorable short-medium term outcome after minimally invasive operative management combined with ADT. Despite ductal carcinoma typically progressing aggressively we would advocate that in the context of advanced age, frailty and comorbidity, a conservative transurethral marsupialisation management approach can produce encouraging results.
Declaration of competing interest
None to declare.
References
- 1.Kojima F., Koike H., Matsuzaki I., et al. Macrocystic ductal adenocarcinoma of prostate: a rare gross appearance of prostate cancer. Ann Diagn Pathol. 2017;27:7–13. doi: 10.1016/j.anndiagpath.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 2.Morgan T.M., Welty C.J., Vakar-Lopez F., Lin D.W., Wright J.L. Ductal adenocarcinoma of the prostate: increased mortality risk and decreased serum prostate specific antigen. J Urol. 2010;184(6):2303–2307. doi: 10.1016/j.juro.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ranasinghe W., Shapiro D.D., Zhang M., et al. Optimizing the diagnosis and management of ductal prostate cancer. Nat Rev Urol. 2021;18(6):337–358. doi: 10.1038/s41585-021-00447-3. [DOI] [PubMed] [Google Scholar]
- 4.Aydin H., Zhang J., Samaratunga H., et al. Ductal adenocarcinoma of the prostate diagnosed on transurethral biopsy or resection is not always indicative of aggressive disease: implications for clinical management. BJU Int. 2010;105(4):476–480. doi: 10.1111/j.1464-410X.2009.08812.x. [DOI] [PubMed] [Google Scholar]