Abstract
Background
In the US, diabetes affects 13.2% of African Americans, compared to 7.6% of Caucasians. Behavioral factors, such as poor diet, low physical activity, and general lack of good self-management skills and self-care knowledge are associated with poor glucose control among African Americans. African Americans are 77% more likely to develop diabetes and its associated health complications compared to non-Hispanic whites. A higher disease burden and lower adherence to self-management among this populations calls for innovative approaches to self-management training. Problem solving is a reliable tool for the behavior change necessary to improve self-management. The American Association of Diabetes Educators identifies problem-solving as one of seven core diabetes self-management behaviors.
Methods
We are using a randomized control trial design. Participants are randomized to either traditional DECIDE or eDECIDE intervention. Both interventions run bi-weekly over 18 weeks. Participant recruitment will take place through community health clinics, University health system registry, and through private clinics. The eDECIDE is an 18-week intervention designed to deliver problem-solving skills, goal setting, and education on the link between diabetes and cardiovascular disease.
Conclusion
This study will provide feasibility and acceptability of the eDECIDE intervention in community populations. This pilot trial will help inform a powered full-scale study using the eDECIDE design.
Keywords: Digital intervention, Diabetes, African American, Problem-solving
1. Introduction
1.1. Background and rationale
Type 2 diabetes is a major public health concern disproportionally affecting African Americans [1], and more than 4.9 million African American adults 20 years or older are living with the disease [2]. African Americans experience worse health outcomes from diabetes complications compared to non-Hispanic whites [1,2]. Uncontrolled, diabetes can lead to both macrovascular (e.g., coronary artery disease [CAD], stroke, lower-extremity amputations) and microvascular complications (blindness, renal or nervous system damage) [[3], [4], [5]] Medication/insulin adherence, and monitoring blood glucose are pieces of important self-management behaviors for proper glycemic control [1,6]. Previous studies have examined the relationship between diabetes self-management and race/ethnicity [[6], [7], [8]], with significant differences between African Americans and non-Hispanic whites. African American participants had lower adherence with self-management practices compared to non-Hispanic whites [1,7,8]. Some barriers to self –management were driven by fear of lack of control of diabetes, time factors for monitoring of glucose, and maintaining dietary restrictions [9]. Those with uncontrolled diabetes require some level of behavior change to increase knowledge of and adherence to self-management behaviors, lessening the impact of associated poor health outcomes.
1.2. Problem-solving to improve diabetes self-management
Problem-solving skills training is beneficial in increasing success with maintaining certain self-management behaviors and managing barriers to self-care, while improving health outcomes [10]. In chronic disease self-management, problem-solving is complex. It involves applying self-management knowledge in the context of everyday life, using a rational problem-solving process (i.e. recognizing and identifying problems, generating solutions, and making decisions to surmount specific barriers to completing self-management tasks), learning from past experiences, and maintaining a positive orientation toward managing self-management challenges [[11], [12], [13], [14]]. Patients may struggle with taking medications as prescribed, but problem-solving skills can help them identify which barriers impede them the most [3]. Problem solving is named one of the seven core diabetes self-management behaviors and the behavior essential for carrying out all other self-management behaviors [15]. However, only a handful of studies have used stand-alone problem-solving programs to improve diabetes self-management, and better interventions are needed to help patients reach optimal problem-solving skills [13,[16], [17], [18]]. Traditional DECIDE is one of these programs that successfully utilizes problem-solving skills for diabetes self-management.
1.2.1. Traditional DECIDE program
Hill-Briggs and colleagues created the DECIDE (Decision-Making Education for Choices in Diabetes Everyday) intervention, a stand-alone diabetes and cardiovascular disease education and problem-solving self-management program. DECIDE was first was evaluated with high-risk African American adults who had uncontrolled diabetes. DECIDE provides participants with education and knowledge about their diabetes, related CVD risk such as blood pressure and cholesterol and problem-solving skills. Traditional DECIDE is delivered through nine sessions over 18-weeks. There is a facilitator in the group session delivery that helps guide the group session through the problem-solving process. In the original DECIDE intervention participants (n = 56, 100% African American) were randomized to either the intensive group (one diabetes and cardiovascular education session plus 8 bi-weekly problem-solving sessions) or the condensed intervention (one diabetes and cardiovascular education session plus one additional problem-solving session). The DECIDE intensive group showed improvements in dietary patterns, physical activity, as well as lowered HbA1c [11,12]. DECIDE was also effective in improving self-management behaviors for cardiovascular disease (CVD) risk factors [19]. Lilly and colleagues [19] used DECIDE for a CVD intervention across three states (North Caroline, Colorado, and West Virginia) and found similar improvements in a multi-ethnic population, to include African Americans. Interventions and programs that require more than four sessions and teach tangible skills in the problem-solving method, as opposed to just using problem-solving skills in a counseling session, are most effective [13,14]. Less is known about efficacious approaches for delivering problem-solving skills training with new technology in a more self-directed format. Delivery modalities including self-study materials, in-person group sessions, and in-person individual sessions have been tested with DECIDE and found to increase self-management knowledge, problem-solving skills, and behaviors [20] Home and phone visit modalities have also been utilized for delivery of DECIDE within health system care models [20]. The proposed work will test the efficacy of translating the proven DECIDE diabetes problem-solving program into a web-based format.
1.3. Internet use by African Americans
African Americans report increased Internet use and availability over the past several years [21]. Historically, they are less likely to use the Internet and experience a severe “digital divide.” [22] While some divide still exist, recent studies have focused on web-based interventions and usage with African American populations and report success in getting this population to use the Internet for health communication needs [[23], [24], [25], [26], [27]]. According to a Pew Internet study, 71% of African Americans have home access to the Internet and 69% have a home computer [26], and a previous web-based intervention indicated 80% of urban African Americans living with diabetes were using computers [27]. Arab and colleagues [24] found a web-based dietary recall study was feasible with African American populations, reporting a 91% completion rate for the 8 week trial [24]. Jackson and colleagues [25] conducted a cross-sectional study on internet usage among urban African Americans with diabetes and found African Americans were already using the Internet (58%), 40% were using the internet for health information, and 89% were willing to use a web-based program to help manage their diabetes.48 These previous studies show digital interventions are feasible with African American populations. However, there is still a need for more research in this area which eDECIDE is well-suited to address.
1.4. Purpose
Problem-solving skills training interventions have typically used group methods, one-on-one sessions, and DVDs [13,[16], [17], [18]]. Delivering a problem-solving intervention through a web-based component is an innovative way to reach the desired target population for the eDECIDE intervention. This approach will empower the population with greater resources and tools to improve self-management and health outcomes. In addition, the web-based format allows participants to receive tailored real-time feedback on potential problem-solving issues that emerge (e.g., self-care issues) on self-management knowledge and skills in a more self-directed manner, allowing for future studies of mobile applications to examine best practices for the type of problem-solving skills training most effective to improve diabetes health outcomes. We believe web-based interventions will have great utility for the target population. The eDECIDE intervention will be accessible through desk top computer, tablet, or a smartphone (non-app).
1.5. Objectives
Aim 1 and 2 of this study, which focus on the development of eDECIDE, will be described in a separate paper. The current paper presents the protocol for the 18-week pilot randomized clinical trial examining the efficacy of the web-based program (eDECIDE) relative to Traditional DECIDE in improving HbA1c through increased adherence to glucose monitoring, compliance to diabetes-related medications, and patient-provider communication in African American participants with uncontrolled diabetes.
2. Methods
2.1. Study setting
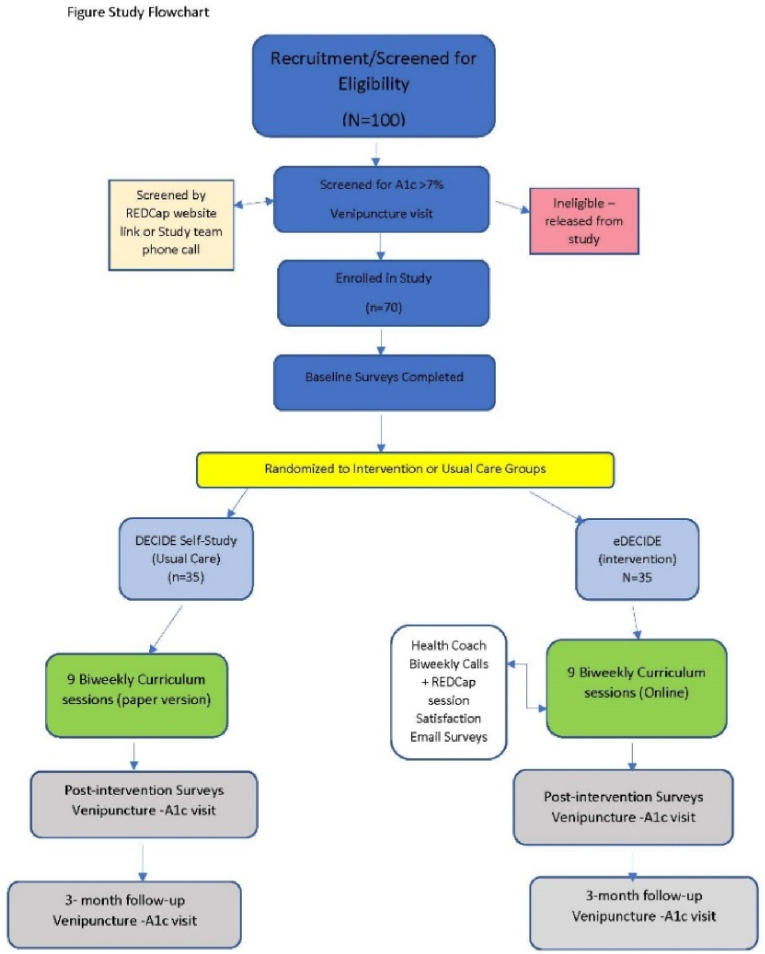
Eligible participants (n = 70) will be recruited from at least two clinical study sites in Kansas as well as open community recruitment. The first study site will be the university faculty/resident clinic within the city. The second or additional study site will be a local health clinic who serves a majority population of African Americans. We will also utilize a patient registry through the university health system. Open community recruitment will take place with filer distribution and social media (e.g., Facebook, Twitter). See Fig. 1 for study flowchart.
Fig. 1.
Study flowchart.
2.2. Screening and enrollment
Potential participants will be screened for eligibility based on age, race, medical status, and access to the Internet. Initially, all interested participants will complete an online screen via REDCap or have the option to complete a telephone screen with study staff. Once screened participants will then go through the consent process and complete baseline study questionnaires. Participants will be scheduled to complete a venipuncture through a university sponsored clinic to record their accurate A1c measure. Once venipuncture is complete those participants who have an A1c within study range will be randomized to either the intervention (eDECIDE group) or control group (DECIDE Self-study). The following provide the inclusion and exclusion criteria for participation in the eDECIDE study.
2.2.1. Inclusion criteria
-
•
African American (determined by self-report)
-
•
Age 18 and older
-
•
Fluent in English
-
•
Current diagnosis of diabetes type 2 based at least one of the following: Fasting plasma glucose ≥126 mg/dL, 2-hr plasma glucose ≥200 mg/dL, Glycosylated hemoglobin (A1c) ≥ 7.0%, Random plasma glucose ≥200 mg/dL
-
•
Has access to the Internet on a computer or smartphone (no stipulations on version)
-
•
Be able to give informed consent
2.2.2. Exclusion criteria
-
•
Pregnancy-to distinguish from gestational diabetes
-
•
Dementia that would limit ability to complete the cognitive study measures
-
•
Currently undergoing chemotherapy treatment for cancer which could limit daily diabetes self-management behaviors
-
•
Severe visual or hearing impairment or any existing condition that would limit one's ability to use the Internet
2.3. Intervention
The eDECIDE intervention is guided by problem-solving theory and techniques [[11], [12], [13], [14]] and includes goal setting, positive and negative problem orientation, cardiovascular disease risk and knowledge, and diabetes self-care knowledge [11,14]. The primary objective is to decrease HbA1c levels that are above 7% and increase the use of problem-solving skills to help participants manage their diabetes. The intervention components described below have shown empirical support for effectiveness in adult groups [11,12,14]. eDECIDE is an online replication of the current DECIDE diabetes intervention [11], which uses problem-solving skills as a base to help those with uncontrolled diabetes and chronic disease [11], previous trials of the original DECIDE intervention have shown success in reducing A1c for participants [11].
2.4. Trial description
This study is an 18-week randomized controlled trial (RCT) with two study arms: (DECIDE self-study) and intervention (eDECIDE). What follows is the conceptual model for the study design, description of the eDECIDE intervention and methods.
2.5. Conceptual model
Intervention: Three main goals will be the focus of the eDECIDE pilot: glucose monitoring, medication adherence, and patient-provider communication. In addition, participants will self-identify which diabetes self-management behaviors are problems for them and are areas they need to work on throughout the program. The goal is for participants to improve in these self-care behaviors using the problem-solving skill building tools and improve their HbA1c.
Comparison DECIDE Problem-solving Skills Training Curriculum: Traditional problem-solving skills training created by D'Zurilla, and Maydeu-Olivares [28] were 12–15 group sessions. Hill-Briggs and colleagues' adaptation of this skills training consists of nine bi-weekly in-person group sessions over 18- weeks.
The DECIDE curriculum (Table 1) is unique because it introduces problem-solving skills to those who lack them or struggle with disease-management barriers. Also, DECIDE combines problem-solving-skill building with education (diabetes, diabetes self-care, and CVD risk factor knowledge), as a combination of skill and education has immense potential to increase behavior change [11,12]. DECIDE's curriculum helps patients understand their issues with managing their disease how to recognize problems, find solutions, set goals, and then put it all into practice.
Table 1.
eDECIDE Bi-Weekly Sessions.
| Sessions | Problem-solving Skills Training Bi-weekly Sessions |
|---|---|
| Week 1 | “All the Facts About Managing Your Diabetes”: Your What to Know Workbook. Educational information about diabetes and diabetes self-management. Participants receive information on cardiovascular risk factors, knowledge of clinical targets for A1c, blood pressure, cholesterol, and self-management behaviors. |
| Week 2 | “Overview of Problem-solving”: orients participants to the problem-solving process and provides a rationale for using problem-solving as a self-management tool. |
| Week 3 | “Taking Control of Stress and Emotions”: Helps participant identify positive and negative emotions around diabetes self-management |
| Week 4 | “What Makes a Problem a Problem?“: Participants begin to keep track of their problems that are stopping them from managing their diabetes |
| Week 5 | “Set Goals that Fit Your Life and Know Your Options”: Engages participants to set goals for problems identified in previous sessions |
| Week 6 | “Different Ways to Reach Health Goals”: Participants use problem-solving options to find solutions and reach health goals. |
| Week 7 | “That Sounds Good … but Does it Work for Me”: Reviews the four types of problem-solving styles and helps participants identify the one that fits them |
| Week 8 | “Take Action and Know the Signs”: Helps participants identify when their self-management strategies are working or not working. |
| Week 9 | “Putting it All Together”: A review of the past 8 sessions and problem-solving approach |
2.6. Intervention group
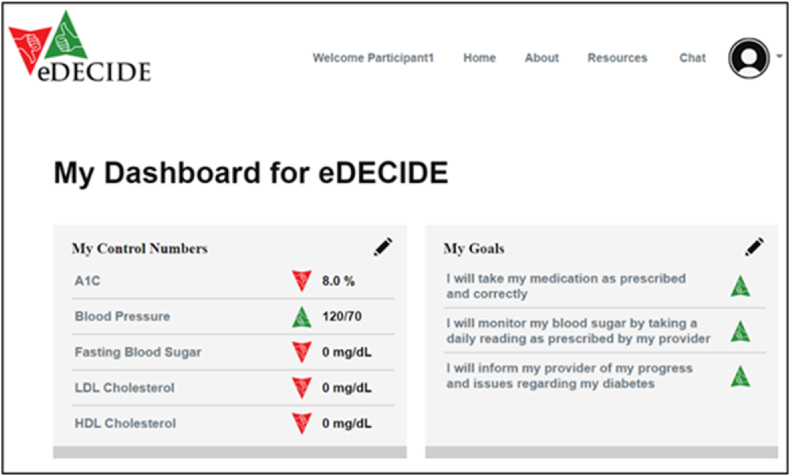
The eDECIDE sessions will consist of the newly translated online method. For eDECIDE, participants will have access to the bi-weekly curriculum through a password-protected, interactive website. On the website they can access their eDECIDE Dashboard (See Fig. 2). Session one will cover the five self-management behaviors needed for diabetes self-management, the link between diabetes and cardiovascular disease and control numbers. The remaining sessions are interactive and require participants to respond to questions and provide feedback to questions. Once they complete a session, a health coach will have access to their responses via a dropbox embedded within the eDECIDE website and can communicate with participants via a chat feature. The personal health coach is equivalent to an online facilitator, who provides feedback and guidance as participants go through the virtual program. Participants will receive a brief follow-up survey via REDCap to ask about their sessions and they will receive a phone call from their health coach every two weeks to check on their progress, go over their workbook pages, and check-in. Participants will continue to have access to the eDECIDE portal once they complete the intervention as an ongoing resource to help them manage their diabetes.
Fig. 2.
eDECIDE Participant Dashboard for Tracking Control Numbers.
2.6.1. Control group
Following baseline assessment, participants randomized to the control arm will receive paper copy of the DECIDE curriculum workbook via mail. Every two weeks, participants will receive a new DECIDE session plus brief written instructions on how to complete the session. After session four, a study team member will check in on their progress to ascertain how they are doing with the curriculum and answer any questions. Once participants have completed the final session (Session 9), a study team member will check in with them again to complete the second survey assessments and schedule the post-intervention blood draw. Due to risk of completing in-person group sessions since SARS -CoV-2 pandemic, study team has opted to use the individual at home self-study modality.
2.7. Problem-solving approach: positive and negative problem orientation
Participants in both conditions will undergo structured problem-solving skill building with the only difference being the mode of delivery, i.e., web-based eDECIDE versus workbook DECIDE self-study. In session two, participants will spend time figuring out which self-management behaviors are problems for them and what is getting in the way of their ability to perform those behaviors. The problem identification session will be a building block for participants as they go through each session until the last one. Participants will learn about negative and positive problem orientation as well as the role of stress and emotions in the problem-solving process.
2.7.1. Goal setting
Participants will complete goal setting during session five. This is a key part of their curriculum to help them reach optimal diabetes self-care. The goals will center around medical adherence, patient-provider communication, and glucose monitoring. Participants will create SMART goals, allowing them to work through specific issues and to make measurable, objective, and reachable goals. During goal setting, participants identify the specific problems they can change and goals to tackle those problems they cannot change.
2.7.2. CVD knowledge and diabetes
Participants in eDECIDE and DECIDE self-study will also work on their CVD knowledge and the link to diabetes. Session covers the linkage between diabetes and risk for cardiovascular disease. Session one also helps participants understand the important of their numbers for blood pressure, cholesterol, and their A1c.
2.7.3. Diabetes self-care
Session one also covers the importance of maintaining five key diabetes self-management behaviors. Participants go through the first session which allows them to build their knowledge about diabetes and CVD and self-management.
2.8. Outcomes and sample size
The primary outcome of interest is HbA1c measurement at week eighteen in the DECIDE Self-study (control) group and eDECIDE (intervention) group. A 0.5% change in HbA1c is clinically meaningful. The standard deviation in both arms is assumed to be 1.3% [29]. Based on 2 sample t-test, assuming type I error rate of 5%, and attrition rate of 20%, with 35 participants in each group (n = 70), the study is powered at 80% to detect a change in HbA1c level of at least 1% between the 2 groups [11,12]. As such, we expect to have full pre/post A1c data on 70 participants. This will allow us to detect clinically meaningful small to medium effects. We believe this sample size is adequate for the planned pilot study. Hill-Briggs’ intervention was successful in detecting HbA1c change of at least 0.5% in a previous study [11,12]. Block randomization with block size of ten will be employed. Within each block 5 participants will be assigned at random to control and five to intervention group using computer derived labels.
2.8.1. Data collection methods
Clinical data (i.e., A1c) and non-clinical data (i.e., data from self-administered surveys) will be collected at designated time periods (see Table 2). Non-clinical data are secondary outcomes and are collected via scheduled phone calls with study participants. All data will be collected and housed through the Research Electronic Data Capture software (REDCap). REDCap is a secure software system often used in housing and managing study related data. Both intervention and control groups will complete a baseline, post-intervention, and 3-month follow-up A1c measurement and survey data completion.
Table 2.
Clinical and non-clinical data collection measures at each timepoint for eDECIDE Trial.
| Instrument/Data Point | Baseline | Post-intervention 18-weeks |
3-month follow-up 30-weeks |
|---|---|---|---|
| Demographic Characteristics | |||
| Age | X | ||
| Sex assigned at birth | X | ||
| Gender identity | X | ||
| Employment Status | X | ||
| Education level | X | ||
| Health Insurance | X | ||
| Income | X | ||
| Cohabitation Status | X | ||
| X | |||
| Clinical Measures | |||
| HbA1c | X | X | X |
| Blood Pressure | X | X | X |
| Self-report measures | |||
| Summary of Diabetes Self-Care Survey (SDSCA) | X | X | X |
| Health Problem-Solving Scale (HPSS) | X | X | X |
| Diabetes & CVD Knowledge Test | X | X | X |
| Patient/Provider Communication Survey | X | X | |
| Engagement Outcomes | |||
| Number of times a participant logged in | X | ||
| Number of sessions started | X | ||
| Number of sessions completed | X | ||
| Treatment Satisfaction Outcomes | |||
| End of session satisfaction survey: Occurs after the completion of each eDECIDE Session |
X | X | |
| Final intervention satisfaction survey | X | ||
| Participant semi-structured interview (intervention group only) | X | ||
2.8.2. Primary outcome
The primary outcome for the intervention will be Hemoglobin A1c. The eDECIDE program helps participants understand their problems in maintaining the A1c and how to navigate those areas to have better control of their disease. Participants in this study will have three blood draws to evaluate their A1c at baseline, post-intervention, and again at 3-month follow-up. We expect to see a 0.5% change (decrease in their reported A1c).
2.8.3. Survey instrument data
Surveys will measure demographics, process outcomes, diabetes self-care behaviors, diabetes and CVD knowledge, and barriers to problem-solving for specific health behaviors. We will also collect data on an exploratory outcome-patient- provider communication. A brief satisfaction survey after each session (eDECIDE group only) will be administered via REDCap.
Diabetes self-management behaviors are measured through the Summary of Diabetes Self-Care Activities Measure (SDSCA) [30], which is a self-report questionnaire on the level of self-care of these diabetes self-management behaviors: general diet, specific diet, exercise, blood-glucose testing, foot care, and smoking. The SDSCA's 11 core items ask respondents to report their behavior over the last seven days. The additional fourteen items on the scale ask respondents about self-care recommendations (from a health care professional or diabetes educator) as well as more questions about diet, medication, foot care, and exercise activities. Respondents rate their responses on a scale from 0 to 7 (for questions pertaining to the last 7 days) or to select a multiple-choice question for the self-care recommendation section.
Problem-solving ability for related health problems will be measured by the Health Problem-Solving Scale [31], which is a 50-item instrument with 7 subscales: 1) effective problem-solving, 2) impulsive/careless problem-solving, 3) avoidant problem-solving, 4) positive transfer of past experience and learning, 5) negative transfer of past experience and learning, 6) positive motivation and orientation, and 7) negative motivation and orientation. The HPSS measures problems dealing with managing symptoms, treatment, dealing with emotions, social relationships, and health, as well as issues that occur in everyday life. Respondents rate their responses on a 5-pont Likert scale ranging from 0- “not at all true of me”, 2- “moderately true of me”, to 4-“Extremely true of me.” [31] HPSS: This score quantifies aspects of health-related problem-solving skills, with higher scores indicating better problem-solving skills.
Diabetes & CVD Knowledge are measured by The All the Facts Survey [11] administered at baseline, post-intervention and 3-month follow-up to assess participants knowledge on diabetes and cardiovascular disease. This is a 14- item scale previously used in the traditional DECIDE program [11].
Patient-Provider Communication will be assessed by the interpersonal process of care survey (IPC-18). The domains measure patient-provider communication (communication, decision-making, and interpersonal style). This measure was validated in multi-ethnic populations [32] and with populations living with diabetes [33].
2.8.3.1. Process measures
Because this is a pilot study, we will collect process measures on usability and user engagement of the eDECIDE website. Usability will be captured through satisfaction surveys administered to participants after completion of each online session. User engagement will be captured time spent in session, log on, completion of the session, and completion of interactive pages by participant.
2.8.4. Statistical management
For baseline characteristics of data, descriptive statistics will be reported as mean and standard deviation for continuous variables; and as count and percentage for categorical variables. Descriptive analyses of baseline characteristics and outcomes will be conducted for both groups including follow-up measurements. Pearson chi-Square or/and likelihood chi-square and Bowker's symmetry tests will be used to assess the association between categorical variables and the two groups. The analysis will be based on “Intention-to-treat” principle. A 2-sided p-value of 0.05 will be used to assess statistical significance. Given the nature of the study population, we expect few or no missing observations on the outcome and predictor variables at the baseline and at subsequent measurements at 18-weeks and 30-weeks. If the proportion of missing observations for outcome and predictor variables is 5% or lower, complete case analysis will be conducted. If the proportion is higher, any missing observation that can be attributed to either attrition or nonresponse will be considered missing at random. Therefore, we will perform multiple imputations by chained equations of the outcome and predictor variables. Therefore, 100 imputation tables with 100 iterations each will be conducted. The characteristics of individuals in the study will be assumed to concede plausibility to the missing-at-random, and, for the comparison, sensitivity analysis will be performed afterward with the complete-case population.
Primary outcome analysis: The post-intervention HbA1c levels in the intervention group will be compared to the control group using a random coefficient in general linear mixed model (for normally distributed outcomes) or generalized linear mixed model (non-normally distributed outcomes). These individual-centered statistical approaches will enable us to: i) interpret the individual fluctuations from baseline to last measurement time points, ii) to address questions about trajectories for each individual units, and iii) to consider the within-individual and among-individual variations in the analyses [34]. Information criteria (i.e. A1c or HbA1c) will be used to select the correct set of variance/covariance patterns that better fit the outcome variables. Additionally, average change in HbA1c level across the 2 groups will be computed and compared using paired t-test or Wilcoxon rank sum test (depending on the distribution of outcome).
Secondary Outcome analysis: The secondary outcomes of interest behavioral measures: diabetes self-management behaviors, Diabetes and CVD knowledge, and problem-solving skills for health-related problems, and patient-provider communication. As explained in primary outcome analyses, random coefficient mixed effect model will be conducted for the secondary outcome variables for compressions between intervention and control groups.
Additionally, we will conduct latent transitional analysis (LTA) to examine progression and regression of an individual's stage of change. LTA is an extension of latent class analysis (LCA) that uses longitudinal data to identify movement between the subgroups over time. LTA is a new technique for analyzing behavioral change patterns over time, which extends traditional Markov modeling to allow use of more complex latent structures. LTA models are fit using maximum likelihood. The effect of intervention and control arms, therefore, may be evaluated by comparing hierarchical models using the likelihood ratio statistic.
3. Discussion
The higher disease burden and lower adherence to self-management among African Americans with diabetes calls for innovative approaches to improve self-management behaviors [15]. Problem solving is a reliable tool for the behavior change necessary to improve self-management [20], The problem-solving approach has utility because it is a technique delivered to help patients identify their problems, learn skills to solve them, and implement solutions for particular challenges or obstacles in their disease self-management [28,35,36]. Therefore, this new modality of DECIDE known as eDECIDE has promise.
eDECIDE has the potential to be a more feasible approach to skills training and innovative. This approach is also cost-effective allowing more flexibility, control, and self-directed access to training than face-to-face group sessions. This new modality to deliver problem-solving interventions has the potential to reach more of the African American population by providing easier access to diabetes self-management education.
3.1. Advancing the field
The long-term goal of this work is to understand how problem-solving skills training, delivered by novel technology, can improve self-management in African American patients with uncontrolled diabetes. Creating the eDECIDE website has potential to increase the use of this type of program by more individuals and health care organizations (e.g., HMOs, ACOs). Thus, allowing providers to tie improvements in clinical markers to behavioral novel technology tools. Engaging the patient in improved self-management, collecting clinical markers (e.g., A1c), and including the health provider communication (e.g., health coach) can increase the utility for tools such as eDECIDE in real-world setting, collecting useful data to help patients manage their health.
3.2. Possible limitations
While this pilot study allows the study team to better understand the feasibility of conducting eDECIDE within an online platform, there could be limitations. We acknowledge all participants may start at a different knowledge level for using the Internet and navigating its usage. We also acknowledge issues with data usage and device use (i.e., smartphone vs. tablet or desktop). To mitigate access, knowledge and device usage limitations, we will provide a tutorial for participants on how to log-in and get started with eDECIDE. The study team will also provide resources for where to access the Internet (i.e., public library, local computer lab at a city community center), if a participate has limited access at home. Understanding these limitations will help the study team move beyond the pilot study for future full-scale interventions.
3.3. Innovation
If successful, long-term goal of this work will help provide greater reach to online diabetes self-management education and care. This approach will empower the population with greater resources and tools to improve self-management and health outcomes. In addition, the web-based format allows participants to receive tailored real-time feedback on potential problem-solving issues that emerge (e.g., dietary, and physical activity issues, other self-care issues, stressful events), on self-management knowledge and skills in a more self-directed manner. Tools such as eDECIDE will provide patients, providers, and the health care community the opportunity to collect behavioral data tied to clinical markers to track improvement. This approach will allow for future studies of mobile applications to examine best practices for the type of problem-solving skills training most effective to improve diabetes health outcomes.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number K01HL135472 (PI: M, Redmond). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Michelle L. Redmond, Email: mredmond@kumc.edu.
Nicole Nollen, Email: NNOLLEN@kumc.edu.
Hayrettin Okut, Email: hokut@kumc.edu.
Tracie C. Collins, Email: TCCollins@salud.unm.edu.
Barbara Chaparro, Email: Barbara.chaparro@erau.edu.
Paigton Mayes, Email: paigton.mayes@wichita.edu.
Kara Knapp, Email: kknapp5@kumc.edu.
Amanda Perkins, Email: a396p640@kumc.edu.
Felicia Hill-Briggs, Email: FHillBriggs@northwell.edu.
References
- 1.Centers for Disease Control and Prevention . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2011. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Pre-diabetes in the United States, 2011. [Google Scholar]
- 2.Karter A.J., Ferrara A., Liu J.Y., Moffet H.H., Ackerson L.M., Selby J.V. Ethnic disparities in diabetic complications in an insured population. JAMA. 2002;287(19):2519–2527. doi: 10.1001/jama.287.19.2519. [DOI] [PubMed] [Google Scholar]
- 3.Stratton I.R., Adler A.I., Neil H.A.W., Matthews D.R., Manley S.E., Cull C.A., Hadden D., Turner R.C., Holman R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. SMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nathan D.M. Long-term complications of diabetes mellitus. N. Engl. J. Med. 1993;328:1676–1685. doi: 10.1056/NEJM199306103282306. [DOI] [PubMed] [Google Scholar]
- 5.Fowler M.J. Microvascular and macrovascular complications of diabetes. Clinical diabetes. 2008;26(2):77–82. [Google Scholar]
- 6.Norris S.L., Engelgau M.M., Venkat Narayan K.M. Effectiveness of self-management training in type 2 diabetes a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 7.Hausmann L.R., Ren D., Sevick M.A. Racial differences in diabetes-related psychosocial factors and glycemic control in patients with type 2 diabetes. Patient Prefer. Adherence. 2010;4:291. doi: 10.2147/ppa.s12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adams A.S., Zhang F., Mah C., Gant R.W., Kleinman K., Meigs J.B., Ross-Degnan D. Race differences in long-term diabetes management in an HMO. Diabetes Care. 2005;28(12):2844–2849. doi: 10.2337/diacare.28.12.2844. [DOI] [PubMed] [Google Scholar]
- 9.Chlebowy D.O., Hood S., LaJoie A.S. Facilitators and barriers to self-management of type 2 diabetes among urban African American adults: focus group findings. Diabetes Educat. 2010;36(6):897–905. doi: 10.1177/0145721710385579. [DOI] [PubMed] [Google Scholar]
- 10.Schumann K.P., Sutherland J., Majid H.M., Hill-Briggs F. Evidence-based behavioral treatments for diabetes: problem-solving therapy. Diabetes Sepctrum. 2011;24(2):64–69. [Google Scholar]
- 11.Hill-Briggs F., Lazo M., Peyrot M., Doswell A., Chang Y.T., Hill M.N., Levine D., Wang N.Y., Brancati F.L. Effect of problem-solving-based diabetes self-management training on diabetes control in a low-income patient sample. J. Gen. Intern. Med. 2011;26(9):972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hill-Briggs F., Gary T.L., Yeh H.C., Batts-Turner M., Powe N.R., Saudek C.D., Brancati F.L. Association of social problem solving with glycemic control in a sample of urban African Americans with type 2 diabetes. J. Behav. Med. 2006;29(1):69–78. doi: 10.1007/s10865-005-9037-0. [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick S.L., Schumann K.P., Hill-Briggs F. Problem solving interventions for diabetes self- management and control: a systematic review of the literature. Diabetes Res. Clin. Pract. 2013;100:145–161. doi: 10.1016/j.diabres.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hill-Briggs F. Problem solving in diabetes self-management: a model of chronic illness self-management behavior. Ann. Behav. Med. 2003;25(3):182–193. doi: 10.1207/S15324796ABM2503_04. [DOI] [PubMed] [Google Scholar]
- 15.Association of Diabetes Care. Education Specialists, Kolb L. An effective model of diabetes care and education: the ADCES7 self-care Behaviors™. Sci Diabetes Self Manag Care. 2021;47(1):30–53. doi: 10.1177/0145721720978154. [DOI] [PubMed] [Google Scholar]
- 16.Tang T.S., Funnell M.M., Brown M.B., Kurlander J.E. Self-management support in “real-world” settings: an empowerment-based intervention. Patient Educ. Counsel. 2010;79(2):178–184. doi: 10.1016/j.pec.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King D.K., Glasgow R.E., Toobert D.J., Strycker L.A., Estabrooks P.A., Osuna D., Faber A.J. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self- management behaviors. Diabetes Care. 2010;33(4):751–753. doi: 10.2337/dc09-1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glasgow R.E., Edwards L.L., Whitesides H., Carroll N., Sanders T.J., McCray B.L. Reach and effectiveness of DVD and in-person diabetes self-management education. Chron. Illness. 2009;5(4):243–249. doi: 10.1177/1742395309343978. [DOI] [PubMed] [Google Scholar]
- 19.Lilly C.L., Bryant L.L., Lear J.M., Vu M.B., Hill-Briggs F., Samuel-Hodge C.D., McMilin C.R., Keyserling T.C. Evaluation of the effectiveness of a problem-solving intervention addressing barriers to cardiovascular disease prevention behaviors in 3 underserved populations: Colorado, North Carolina, West Virginia, 2009. Prev. Chronic Dis. 2011;11:E32. doi: 10.5888/pcd11.130249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fitzpatrick S.L., Papajorgji-Taylor D., Schneider J.L., Lindberg N., Francisco M., Smith N., Vaughn K., Vrany E.A., Hill-Briggs F. Bridge to Health/Puente a la Salud: a pilot randomized trial to address diabetes self-management and social needs among high-risk patients. Translational behavioral medicine. 2022 Jul;12(7):783–792. doi: 10.1093/tbm/ibac016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brodie M., Flournoy R.E., Altman D.E., Blendon R.J., Benson J.M., Rosenbaum M.D. Health information, the Internet, and the digital divide. Health Aff. 2000;19(6):255–265. doi: 10.1377/hlthaff.19.6.255. [DOI] [PubMed] [Google Scholar]
- 22.Smith A. Pew Research Center; Washington, D.C.: January 6, 2014. African Americans and Technology Use.http://www.pewinternet.org/2014/01/06/african-americans-and-technology-use/ [Google Scholar]
- 23.Kim B.H., Glanz K. Text messaging to motivate walking in older African Americans: a randomized controlled trial. Am. J. Prev. Med. 2013;44(1):71–75. doi: 10.1016/j.amepre.2012.09.050. [DOI] [PubMed] [Google Scholar]
- 24.Arab L., Wesseling-Perry K., Jardack P., Henry J., Winter A. Eight self-administered 24-hour dietary recalls using the Internet are feasible in African Americans and Whites: the energetics study. J. Am. Diet Assoc. 2010;110(6):857–864. doi: 10.1016/j.jada.2010.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jackson M.C.L., Batts-Turner M.M.L., Falb M.M.D., Yeh H.C., Brancati F.L. Computer and internet use among urban African Americans with type 2 diabetes. J. Urban Health. 2005;82(4):575–583. doi: 10.1093/jurban/jti126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pew Research Center Black and hispanic adults in the U.S. Are less likely than white adults to have a traditional computer, home broadband. https://www.pewresearch.org/fact-tank/2021/07/16/home-broadband-adoption-computer-ownership-vary-by-race-ethnicity-in-the-u-s/ft_21-07-15_techregulation_01/ Retrieved August 25, 2022:
- 27.Samal L., Yeh H.C., Gary-webb T.L., Jackson C.L., Brancati F.L. Computer and Internet use of urban African Americans with type 2 diabetes in relation to glycemic control, emergency department use, diabetes-related knowledge, and health literacy. Diabetes Care. 2010;33(1):e9. doi: 10.2337/dc09-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.D'Zurilla T.J., Maydeu-Olivares A. Conceptual and methodological issues in social problem-solving assessment. Behav. Ther. 1995;26(3):409–432. [Google Scholar]
- 29.Dixon J.B., O'Brien P.E., Playfair J., Chapman L., Schachter L.M., Skinner S., Proietto J., Bailey M., Anderson M. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA. 2008 Jan 23;299(3):316–323. doi: 10.1001/jama.299.3.316. [DOI] [PubMed] [Google Scholar]
- 30.Toobert D.J., Hampson S.E., Glasgow R.E. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 31.Hill-Briggs F., Gemmell L., Kulkarni B., Klick B., Brancati F.L. Associations of patient health-related problem solving with disease control, emergency department visits, and hospitalizations in HIV and diabetes clinic samples. J. Gen. Intern. Med. 2007;22(5):649–654. doi: 10.1007/s11606-006-0091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stewart A.L., Nápoles-Springer A.M., Gregorich S.E., Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv. Res. 2007;42(3 Pt 1):1235–1256. doi: 10.1111/j.1475-6773.2006.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.White R.O., Eden S., Wallston K.A., et al. Health communication, self-care, and treatment satisfaction among low-income diabetes patients in a public health setting. Patient Educ. Counsel. 2015;98(2):144–149. doi: 10.1016/j.pec.2014.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguefack L.R.H., Pagé M.G., Katz J., Choinière M., Vanasse5 A., Dorais M., Samb M.O., Lacasse A. Trajectory modelling techniques useful to epidemiological research: a comparative narrative review of approaches. Dove Press journal: Clin. Epidemiol. 2020;12 doi: 10.2147/CLEP.S265287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D'Zurilla T.J., Goldfried M.R. Problem solving and behavior modification. J. Abnorm. Psychol. 1971;78(1):107. doi: 10.1037/h0031360. [DOI] [PubMed] [Google Scholar]
- 36.Schumann K.P., Sutherland J., Majid H.M., Hill-Briggs F. Evidence-based behavioral treatments for diabetes: problem-solving therapy. Diabetes Sepctrum. 2011;24(2):64–69. [Google Scholar]