Learning objectives.
By reading this article you should be able to:
-
•
Outline the common reasons for failure of peripheral nerve block.
-
•
Detail the ways to mitigate failure in relation to different risk factors.
-
•
Explain the anatomical relationship between dermatomes and myotomes, and common anatomical variations.
-
•
Discuss the safe management of a failed nerve block.
Key points.
-
•
Understanding the reasons behind nerve block failure will help reduce its incidence.
-
•
Detailed knowledge of the anatomy is essential, and the differing dermatomes, myotomes and osteotomes must be considered.
-
•
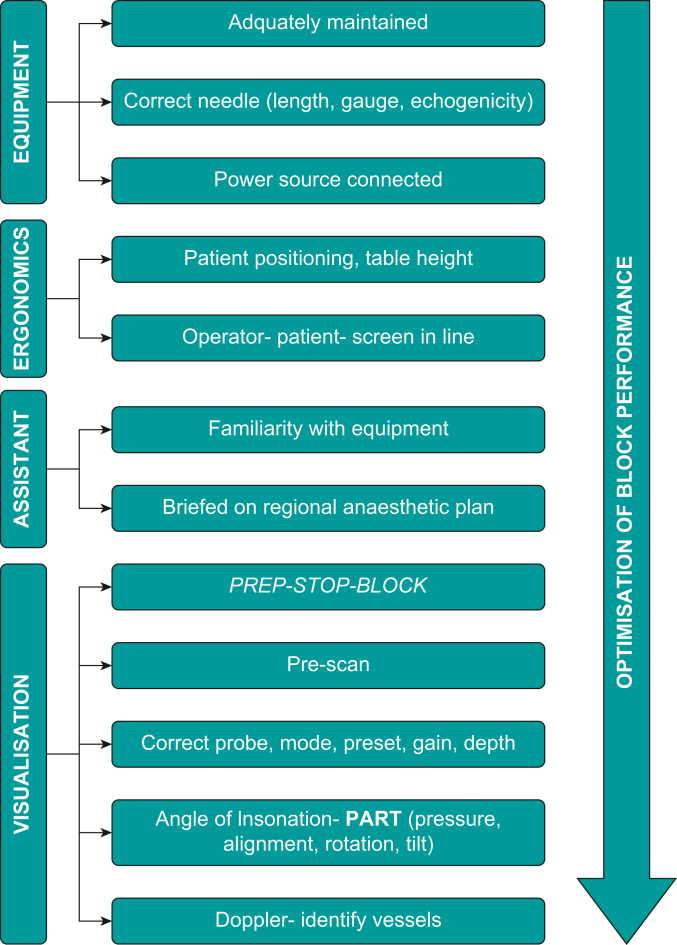
A structured approach to the placement of a block, ensuring equipment, ergonomic, assistance and ultrasound visualisation techniques, will improve success.
-
•
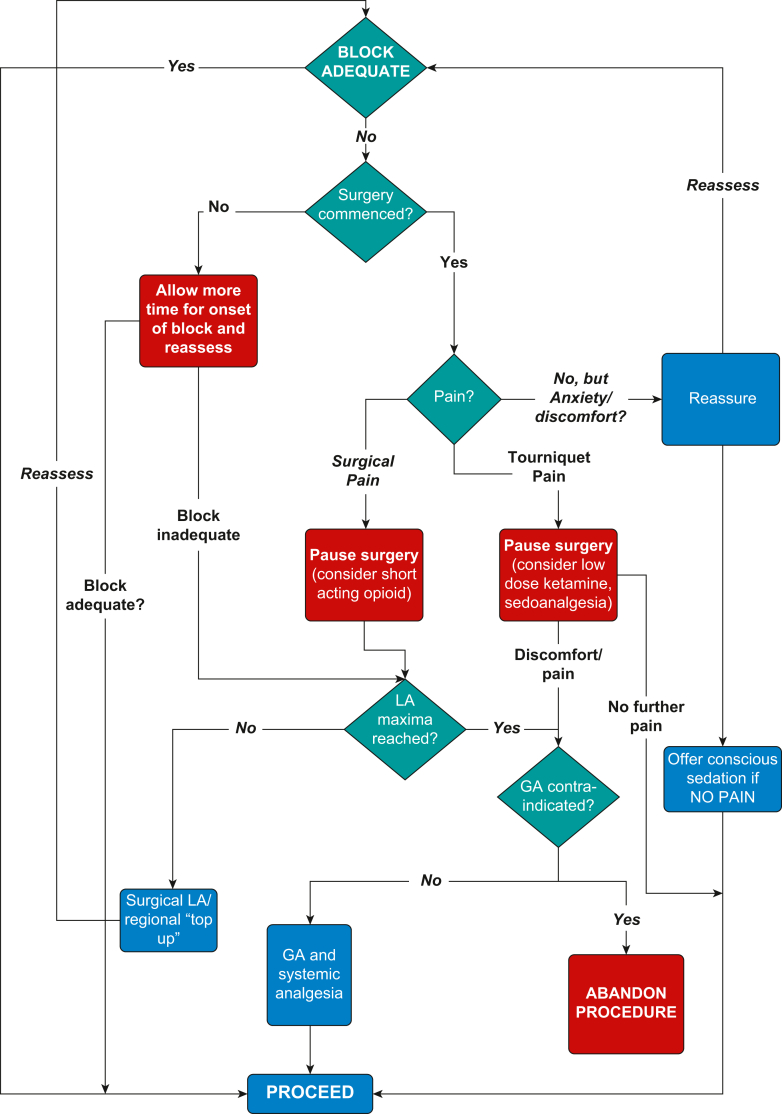
The management of a failed nerve block must be systematic, ensuring local anaesthetic maxima are not exceeded.
Failed nerve blocks can cause delays, cancellations, patient distress and contribute to a significant proportion of legal claims against the NHS relating to inadequate anaesthesia.1 In contrast, there is good evidence that effective regional anaesthesia (RA) reduces postoperative pain and opioid requirements, whilst increasing patient satisfaction.2
This article only considers failure of the perioperative peripheral nerve block (PNB) to limit the breadth. The failure of PNBs of the upper and lower limbs will be defined, along with possible reasons and methods to reduce it, whilst outlining the management when failure does occur.
Defining the failed block
To better understand the success or failure of the PNB, we must consider its definition, incidence and the context of what is expected from the block. There is currently no widespread accepted definition of block failure and lack of widespread and published formal follow up has led to difficulties in understanding the incidence of block failure. However, one comprehensive study of more than 7000 patients found an overall ‘success rate’ of 89%, meaning that around 1 in 10 PNBs was not effective.3
We, the authors, define a failed perioperative PNB as one that does not provide the anticipated level of anaesthesia or analgesia, within an adequate time frame, to allow the planned procedure to take place with adequate patient comfort, without the addition of further unplanned interventions; be that additional nerve blocks, systemic analgesia, sedation or general anaesthesia (GA).
It must be noted that this definition does not include failed fascial plane blocks or non-surgical blocks, where the expected outcomes are less clear cut.
Confounding factors complicate analysis of the success of perioperative PNBs. These include PNBs that are combined with GA, local anaesthetic (LA) agent not matching the duration of surgery, patients with successful nerve block but who require conversion to GA for unrelated reasons (e.g. anxiety, disinhibition, tourniquet pain) and PNBs that are technically successful but were inappropriately chosen for a given indication (e.g. femoral nerve block for tibial shaft fracture repair).
Mechanisms of block failure and methods to reduce them
The two key components in managing the failed nerve block are techniques to reduce the chance of it occurring, and methods to manage it if does occur. These are summarised in Table 1 and are discussed below.
Table 1.
Mechanisms of block failure and mitigation strategies. LA, local anaesthetic; US, ultrasound.
| Mechanism of failure | Mitigation |
|---|---|
| Patient-related factors | |
| Anxiety | Adequate communication – information leaflets, consent process, interpreter if needed |
| Obesity | Choice of block, correct US probe, experienced clinician |
| Positioning difficulties (e.g. contractures, arthritides) | Choice of block, patient supports |
| Conditions associated with reduced sensitivity to LAs (e.g. Ehlers–Danlos syndrome) | Detailed history |
| Anatomical variability | Prior knowledge of variations, prescan |
| Surgical factors | |
| Surgical approaches | Team brief – discuss surgical plan and possible variations to standard approaches |
| Backup plan if block fails | |
| Tourniquet pain | Anticipation using additional blocks, i.v. Analgesia |
| Anaesthesia-related factors | |
| Inadequate experience | Training, senior support |
| Familiarity with equipment | US, needle, positions, alignment, ergonomics |
| LA choice | LA for correct duration |
| US optimisation | Probe, mode, preset, gain, depth |
| PART (pressure, alignment, rotation, tilt) | |
Patient-related factors
The careful selection of patients is an essential component of success in RA. Many patients are understandably anxious during the perioperative period, and lessons learned from other specialties that utilise awake techniques, such as neurosurgery, show that success can be affected by language barriers and altered mental status.4 Therefore, hurdles to communication including language, hearing and visual impairments can lead to inadequate understanding and compliance by the patient, both during the placement of a PNB and during the intraoperative period, if awake surgery is planned. The use of language or sign interpreters, and visual aids and information leaflets, will help to overcome these hurdles, and although awake surgery is not contraindicated in these patients, there should be provision to ensure communication is possible throughout. Effectively addressing expectations before surgery with information and education can produce near 100% satisfaction rate in awake surgery.5
Obesity can lead to difficulty in identification of anatomical landmarks and increase the skin-to-nerve depth, reducing image quality on ultrasound (US).6 Beam distortion, occurring with some types of adipose tissue, can disrupt the linear path of US waves, further affecting image quality. Experienced input is essential when performing blocks on patients who are morbidly obese. A lower frequency probe should also be considered, although while penetration is improved, image resolution will decrease. Nerve stimulation as an adjunct to US guidance can increase the operator's confidence that the identified structure is indeed the nerve or plexus. Finally, choosing the right block in obese patients may convey benefits. An axillary brachial plexus block may be preferable to a supraclavicular block for upper limb surgery, as there will be relatively less adipose tissue in this approach. Similarly, unusual sonographic appearances of neural tissues may occur in patients with sarcopenia, making their identification difficult.
Positioning the patient is an important factor in ensuring block success (both in placing blocks and for comfort during awake surgery), but this can be hampered by conditions such as arthritis and contractures. Some rare conditions, such as Ehlers–Danlos syndrome, can lead to sodium channel mutations that convey a relative reduction in sensitivity to LAs. A thorough patient history beforehand may identify these conditions and alert the anaesthetist to potential difficulties.
Anatomy and variations
A detailed knowledge of dermatome, myotome and osteotome distribution is essential to provide effective RA. This, in combination with knowledge of the planned procedure, including tourniquet use, and the correct choice of LA, will enable anaesthesia of the appropriate nerve(s) at the appropriate level.
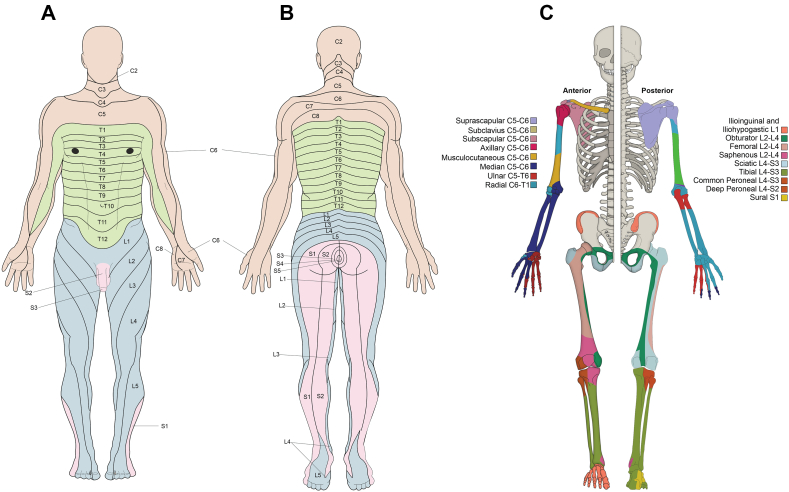
Figure 1 details the expected distribution of dermatomes and osteotomes. Although these are the images convey the accepted ‘normal’, there is considerable interindividual variation and overlap of innervation, and this cannot be predicted.
Fig 1.
(A) Anterior dermatome distribution. (B) Posterior dermatome distribution. (C) Anterior and posterior osteotomes.
To use US effectively, a thorough knowledge of both classical and US anatomy is essential, so that any abnormalities can be identified and the block can be adjusted accordingly. The location of the nerves and established landmarks, such as vasculature and bones, can vary.
In the upper limb, anatomical variations of the brachial plexus, from roots to branches, are well documented. Scanning back and forth to identify the origin and course of the target nerve is required to provide context to ensure correct identification. This traceback method has been shown to improve visualisation of the brachial plexus in novices.7 However, in the case of pre-fixed (C4, rather than C5) and post-fixed (T2, rather than T1) brachial plexuses the roots can be confused if inadequate traceback is performed. Although some may argue this may be of little clinical relevance to the success of brachial plexus root block, it may confuse pattern recognition and learning.
At the supraclavicular level, the plexus exists as a collection of trunks and divisions and has the sonographic appearance of a bunch of grapes. Although often tightly packed superolateral to the subclavian artery, the plexus can be spread over a large anatomical area, with elements residing medial to the artery. This variation is a well-recognised source of the ‘non-zero’ rate of block failure with the supraclavicular approach, especially when the LA is deposited in only one or two discrete locations.
Even greater variation is seen at the level of the terminal branches. There is a high degree of disparity of these nerves around the axillary artery, and in the case of the musculocutaneous nerve, it can be completely absent.8 Furthermore, individual visualisation of the terminal nerves can at times be complicated by their lack of separation from one another, even after injection of LA.9 This may potentially lead to a fruitless search for a nerve.
In the lower limb, variations of the femoral nerve course can lead to difficulty in its identification. For example, its established position lateral to the femoral artery can vary in some, moving more posterior, whereas on occasion, it can lie in the belly of the iliacus muscle.10 Likewise, there is a high degree of variability in the branches and course of the lateral femoral cutaneous nerve, leading to differing cutaneous innervation.11 Moving distally, the complex innervation of the anterior and posterior capsules of the knee varies considerably. The nerve to the vastus medialis, which is thought to contribute significantly to the knee capsule innervation can run in a fascial plane separate to the adductor canal and its sensory branches can have both intra- and extramuscular routes.12 There is substantial disparity in the innervation of the posterior capsule by the obturator, sciatic, tibial and peroneal nerves.13 These variations have led to development of blocks such as the iPACK block. This involves placement of LA into a specific field, as opposed to targeting individual nerves, which ensures that the articular branches of these nerves supplying the posterior capsule are anaesthetised.
These anatomical variations mean that the complexity of the nerves and branches increase more distally. Therefore, proximal blocks can reduce this. For example, a popliteal sciatic nerve block provides anaesthesia for most of the foot (except the medial aspect – saphenous nerve), negating the need to individually block each of the distal nerves. However, there is a greated degree of motor block with proximal blocks, which may affect physiotherapy and discharge from hospital.
Patients may also have artificial anatomical variations, such as tattoos and implants (e.g. ventriculoperitoneal shunts, pacemakers). Often practitioners avoid the use of RA around these anatomical variations, for fear of introducing infection, or causing damage to implants. Their presence can also alter the approach and obscure the path of the needle, whilst hindering the views. In these cases, alternate blocks or approaches should be considered altogether.
Surgical factors
The correct PNB for the type of surgery should provide effective anaesthesia under the correct conditions. However, if the surgical plan evolves during the procedure, extension of the incision or alternate surgical approaches may render the block ineffective. Furthermore, the length of the procedure may extend beyond the effective window for the block.
Surgical checklists, such as the WHO checklist or the ‘five steps to safer surgery’ protocol, use a team brief to provide the opportunity for the theatre teams to discuss the surgical and anaesthetic plans for each patient, and raise any concerns.14 The anaesthetist should highlight the plan for RA and state the area that will be anaesthetised. Complicating factors such as duration of surgery, difficult steps or alternate surgical approaches should be discussed to ensure the anaesthetic and surgical plans marry up. This is also an opportunity to create dialogue between team members to ensure that if the surgical plan evolves, the anaesthetist is made aware at the earliest opportunity, so that amendments to the anaesthetic can be made. In addition, this is an opportunity to outline an alternative plan in the event of block failure.
Tourniquet pain must also be considered. The proximal location of the tourniquet, often far from the surgical site, may not be covered by the PNB serving the surgical site. In addition, the complex mechanism surrounding the transmission of this pain, which is thought to be via C-fibres that are relatively resistant to the effects of LA, suggests that RA may not be sufficient to block this pain, even if the area is covered.15 Tourniquet pain tends to begin around 30–60 min after inflation. Management strategies to reduce this pain are challenging but include anticipating the issue before the procedure and subsequent block of the intercostobrachial nerve (via subcutaneous infiltration of LA along the axillary crease or via US guidance) to relieve localised skin discomfort for high arm tourniquets, or block of sympathetic fibres surrounding the femoral artery for lower limb tourniquets. If encountered during the procedure, the tourniquet can be deflated (after consultation with the surgical team) to provide relief. Low dose ketamine (0.1 mg kg−1) has been shown to alleviate some of the discomfort, but ultimately conversion to GA may be required if increasing sedoanalgesia does not facilitate tourniquet tolerance.15
Anaesthesia-related factors
Developing proficiency with RA takes time and there is a ‘learning curve’, with failure being more likely in the early stages of training. There is no defined minimum number of blocks to achieve competency and adequate experience is required to choose the correct block, localise the target neural structure and give the LA effectively. The inappropriate choice of LA can lead to slow onset, or inadequate duration, whereas hasty progression from block to surgery may lead to an appropriate block being suboptimal, by not allowing enough time for onset.
A lack of familiarity with the US equipment and its basic science will lead to poor image quality. Acoustic and anatomical artifacts can complicate the image whereas needle artifacts can cause confusion.6 In addition, sub-optimal ergonomics will hinder the operator further.
Training has evolved, and the classic adage of ‘see one, do one, teach one’ does not hold true for performing blocks, which are relatively complex procedures. As discussed, the amount of time required for assimilation and maintenance of these skills varies between individuals so cannot be based solely on number of blocks placed, and therefore senior, experienced support should be on hand to provide guidance if required. The development of needle trainers and guidance systems, which incorporate artificial intelligence, may provide a synergistic way to teach RA and could be useful tools in the future to improve block success, but are at present limited by cost and the need for a greater evidence base.
The recent emergence of the block room model conveys many benefits. It creates an environment with appropriate expertise, in a space with appropriate ergonomics, with time pressures removed. Evidence shows block rooms provide excellent teaching opportunities, and can also contribute to increased efficiency.16,17 The model works to reduce many of the obstacles to effective RA.
Choice of LA agent
The choice of LA can influence the onset, duration and effectiveness of the block and must be carefully considered in conjunction with the planned procedure. This is especially important when considering rescue blocks, or surgical infiltration of LA, as overdosing must be avoided.
The ED95 for LA depends on the location on the block and the type of LA. It is important that the clinician is familiar with these doses to ensure adequate LA is injected, whilst avoiding overdosing to minimise adverse effects (such as phrenic nerve palsy in the interscalene block).
In addition to using single LAs, efforts have been made to combine these to provide synergy of onset, density and duration. When comparing short-acting agents alone (lidocaine or mepivacaine) and bupivacaine alone vs a combination solution for brachial plexus blocks, the combination solutions did not always shorten the onset time, but the duration of action was significantly reduced.18,19 Therefore, the proposed benefits of LA mixtures do not seem to hold true. However, multiple agents are commonly used separately and in a complementary manner, for example with a proximal short-acting LA to provide analgesia for tourniquet pain, whereas a longer-acting LA is used for the distal block (within safe maximal doses).
Extensive research has been conducted to investigate the benefits of adjuncts to the local anaesthetic preparation. Agents such as dexamethasone and clonidine can increase the duration of analgesia significantly, although none seem to have any effect on block failure rates. This topic has been detailed comprehensively in a recent article in this journal.20
Novel agents, such as liposomal bupivacaine, are available, with FDA approval for their use in RA. However, despite promising initial studies, a recent systematic review suggests liposomal bupivacaine does not provide added overall clinical benefits when compared with plain bupivicaine.21
Ultrasound and optimisation
Guidelines from the European Society of Anaesthesiology recommend the use of US for most upper and lower limb blocks.22 These recommendations are supported by studies that show US guidance compared with nerve stimulation alone led to reduced procedural pain, reduced analgesic or anaesthetic requirements, and a reduction in vascular puncture.
The use of nerve stimulation in combination with US guidance remains fairly common practice. It cannot only confirm the target nerve, but aids in avoiding nerves that are in the needle's trajectory.23 However, there has been no difference in the rate of postoperative neurological adverse effects or the requirement for rescue blocks shown, regardless of whether or not the US technique was supplemented with nerve stimulation.24
Figure 2 summarises the steps that help the operator to perform a successful block using US guidance. Compliance with these steps allows optimum visualisation of the target nerves and surrounding tissues, whilst helping to minimise the adverse events such as damage to structures and wrong-sided blocks. Performance of the block should be underpinned by a checklist before the procedure (in the UK, this is the 'Prep, stop, block' procedure), which aims to reduce the incidence of wrong-sided blocks.25
Fig 2.
Factors to assist in successful block performance.
Spread of LA
Visualising the deposition of LA in relation to the neural tissue using US must also be considered. Although intraplexus (compared with extraplexus) LA deposition leads to a faster onset of motor and sensory block in the brachial plexus, there is ultimately no difference in efficacy of the block.26
The needle-to-nerve distance required for an effective block also varies depending on site (and on dose and volume of LA) and this distance is perhaps greater than previously thought. For example, a study into the maximum effective distance for US guided interscalene blocks found this to be 8.3 mm.27 Pattern of local anaesthetic spread may also be important. Some studies suggest that circumferential spread is associated with faster sensory onset, whereas longitudinal deposition of LA along the neural sheath (rather than single point injection) may also be a positive predictor of nerve block success.28, 29
Assessment of the block
Despite assessment of the PNB being a vital stage of RA, there is no consensus on how a block should be tested to ensure its efficacy.30 Sympathetic changes are first to appear after a successful block, followed by sensory and then motor block. Common methods include testing the sensation for temperature over the relevant dermatomes, and sensation to pain and soft touch, and motor block. In patients with pre-existing pain of the corresponding area, cessation of the pain is an encouraging indicator of block success. Although the onset time for RA is highly variable and dependent on the LA used, the block performed and the individual patient, it is vital to allow adequate time and not to test too early. This requires a compliant, awake patient as recommended by the American Society of Regional Anesthesia (ASRA).31
Temperature change compared with the contralateral side seems to convey a higher positive and negative predictive value of block success than the above measures in patients undergoing axillary brachial plexus block.32 Quantifying these with thermography is currently limited to the research setting, as is the more comprehensive quantitative sensory testing. However, it does suggest that even a subjective assessment of skin temperature change could support block success.
Motor block can be assessed by asking the patient to perform simple movements, and the absence of these suggest myotome block, with their associate nerve supply. Table 2 details the expected myotome distribution and corresponding movements. Mnemonic devices such as asking the patient to make ‘rock, paper and scissors’ shapes with their hand can test function of the median, radial and ulnar nerves, respectively, and enable operator recall.
Table 2.
Common tests for myotome block.
| Upper limb |
Lower limb |
||
|---|---|---|---|
| Test | Nerve | Test | Nerve |
| Abduction of shoulder | Axillary | Hip flexion; knee extension | Femoral |
| Initial shoulder abduction (0–15°); external rotation of humerus | Suprascapular nerve | Hip adduction | Obturator |
| Elbow flexion | Musculocutaneous | Knee flexion | Sciatic |
| Forearm supination; wrist extension; elbow extension ('paper' sign) |
Radial | Ankle plantar flexion; foot inversion; flexion of toes | Tibial |
| Forearm pronation; thumb flexion, opposition; second and third digit flexion; wrist flexion, abduction ('rock' sign) | Median | Foot eversion | Superficial peroneal |
| Finger abduction/adduction; fourth and fifth digit flexion; thumb adduction ('scissors' sign) | Ulnar | Ankle dorsiflexion; toe extension | Deep peroneal |
Management of block failure
Failure or incomplete effectiveness of a PNB is a recognised complication. Reasons have been described above, but it is the management of this failure that is a critical skill for anyone performing RA. Consent for any interventions considered should be sought before the surgical procedure (‘plan B’), including abandoning surgery if appropriate.
The protocols for management depend on whether the patient is awake or asleep. With adequate planning, there should be a clear course of action in the event of block failure, as outlined in Fig 3.
Fig 3.
Flowchart to guide management of the failing nerve block in the awake patient. GA, general anaesthetic; LA, local anaesthetic.
Failure may be identified before or during the procedure. If there is failure before incision, ‘top-up’ or ‘rescue’ blocks can be performed. Commonly, in the upper limb the ulnar, median and radial nerves can be individually targeted. In the lower limb, the peripheral nerves can be targeted at the ankle level (saphenous, tibial, superficial and deep peroneal, and sural nerves) or more proximally with femoral or popliteal sciatic nerve blocks, depending on the type of surgery. These can also be performed after the surgery has commenced, but the risk benefit should be carefully considered if the patient is anaesthetised given the ASRA guidelines advise that blocks should not routinely be performed in patients who are anaesthetised or deeply sedated.31 Rescue blocks also tend to be more complex if the patient is already draped.31 The depth of the chosen rescue block is important to minimise the risk of local anaesthetic systemic toxicity (LAST). Deeper blocks may pose an increased risk of vascular puncture and therefore more caution should be demonstrated. Alternatively, the surgeon can administer LA, again ensuring judicious calculation of LA, to minimise the risk of LAST. For example, the British National Formulary states bupivacaine doses can be repeated every 3 h, but should not exceed 400 mg in 24 h.33
Additional blocks must be conducted with caution. If a top-up block is placed distal to the original block, the target area may be insensate despite the block not providing surgical anaesthesia. Additional equipment such as injection pressure monitors or nerve stimulators should therefore be considered to minimise the risk of nerve damage.
If the procedure has started, and block failure is suspected in the awake patient, surgery must be paused and clear communication is necessary to ascertain whether there is pain, or another issue, such as discomfort or anxiety. If it is the latter, then these can often be managed with reassurance, or conscious sedation. It must be stressed, however, that pain should not be managed with sedation alone.
Sedoanalgesia provides an alternative option and is used by some anaesthetists. The principle is to combine the anaesthetic effects of agents such as propofol or midazolam, with the analgesic effects of opioids such as fentanyl, alfentanil or remifentanil. However, there is currently a lack of evidence on the efficacy of this technique in inadequate RA, so it must be used with caution.
The failed nerve catheter
Mechanisms responsible for the failure of the peripheral nerve catheter (PNC) are similar to those for single-shot PNBs but are confounded by the fact that the catheter needs to remain in situ for up to 5 days. To be effective, the PNC needs to be correctly deployed in close proximity to the correct nerve and to not migrate; LA at an appropriate dose then needs to be delivered. The catheter must be secured, and the depth clearly documented, as slippage is a common cause of failure. Several fixation devices are commercially available, but the use of tissue glue helps to mitigate migration. This should then be covered with a clear dressing to allow inspection.
A systematic approach is essential when troubleshooting a failing PNC. A detailed review of the block documentation, followed by a history and examination is required to ascertain if the failure is new and whether it is complete or patchy. Equipment must then be checked to ensure that there is no failure in LA delivery such as infusion device malfunction or giving set disconnection. LA bolus and reassessment may indicate if the catheter remains in the same plane. Alternate pathologies such as compartment syndrome must also be considered.
One detailed assessment protocol involves scanning the presumed catheter tip site with US, while giving a bolus of normal saline in order to precisely determine catheter tip location and whether displacement has occurred. Colour Doppler US can be used in more challenging scans to more easily visualise the spread of saline injectate on the screen.
Clear guidelines and regular staff training are required to correctly manage PNCs and to ensure that failing PNCs are identified and managed effectively. Ultimately, if troubleshooting fails, the catheter can be re-sited or alternate analgesia can be provided.
Conclusions
Block failure is a recognised complication of RA. Familiarity with the reasons for block failure and methods to reduce them should help lower the incidence. However, as with all areas in medicine, it is essential to have the knowledge, understanding and skills to manage the situation when a procedure fails or does not go according to plan.
Declaration of Interest
SW has received honoraria from Avanos for teaching. JG consults for Pacira Biosciences and Pajunk Medical, and received research funding from Mallinckrodt Pharmaceuticals. TB declares no conflicts of interest.
Biographies
Thomas Bottomley BSc (Hons) FRCA is a specialty registrar in anaesthesia and has recently completed a regional fellowship at University College London Hospitals NHS Foundation Trust.
Jeff Gadsden MD is a professor of anaesthesiology at Duke University Hospital, North Carolina, where he is the chief of regional anaesthesiology and has ongoing commitments to clinical innovation, scholarship and education.
Simeon West FRCA is a consultant anaesthetist at University College London Hospitals NHS Foundation Trust, honorary senior research associate in medical physics and bioengineering and a board member of Regional Anaesthesia UK.
Matrix codes: 1H02, 2G02, 3A09
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
References
- 1.Mihai R., Scott S., Cook T.M. Litigation related to inadequate anaesthesia: an analysis of claims against the NHS in England 1995–2007. Anaesthesia. 2009;64:829–835. doi: 10.1111/j.1365-2044.2009.05912.x. [DOI] [PubMed] [Google Scholar]
- 2.Kessler J., Marhofer P., Hopkins P.M., Hollmann M.W. Peripheral regional anaesthesia and outcome: lessons learned from the last 10 years. Br J Anaesth. 2015;114:728–745. doi: 10.1093/bja/aeu559. [DOI] [PubMed] [Google Scholar]
- 3.Barrington M.J., Watts S.A., Gledhill S.R., et al. Preliminary results of the Australasian Regional Anaesthesia Collaboration: a prospective audit of more than 7000 peripheral nerve and plexus blocks for neurologic and other complications. Reg Anesth Pain Med. 2009;34:534–541. doi: 10.1097/aap.0b013e3181ae72e8. [DOI] [PubMed] [Google Scholar]
- 4.Dreier J.D., Williams B., Mangar D., Camporesi E.M. Patients selection for awake neurosurgery. HSR Proc Intensive Care Cardiovasc Anesth. 2009;1:19–27. [PMC free article] [PubMed] [Google Scholar]
- 5.Turbitt L., Johnston D. Setting up a regional anesthesia pathway to improve value of care in upper limb surgery: a European perspective. Am Soc Reg Anesth News. 2018;17:21. [Google Scholar]
- 6.Henderson M., Dolan J. Challenges, solutions, and advances in ultrasound-guided regional anaesthesia. BJA Educ. 2016;16:374–380. [Google Scholar]
- 7.Tsui B.C., Lou L. Learning the ‘traceback’ approach for interscalene block. Anaesthesia. 2014;69:83–85. doi: 10.1111/anae.12556. [DOI] [PubMed] [Google Scholar]
- 8.Hunter D., Zdilla M. The absent musculocutaneous nerve: a systematic review. Transl Res Anat. 2021;22 [Google Scholar]
- 9.Christophe J.L., Berthier F., Boillot A., et al. Assessment of topographic brachial plexus nerves variations at the axilla using ultrasonography. Br J Anaesth. 2009;103:606–612. doi: 10.1093/bja/aep207. [DOI] [PubMed] [Google Scholar]
- 10.Woodworth G., Lee T., Ivie R., Becket B. Anatomical variation of the femoral nerve in the femoral triangle. Reg Anesth Pain Med. 2019;44:907–908. doi: 10.1136/rapm-2019-100599. [DOI] [PubMed] [Google Scholar]
- 11.Haładaj R., Wysiadecki G., Macchi V., et al. Anatomic variations of the lateral femoral cutaneous nerve: remnants of atypical nerve growth pathways revisited by intraneural fascicular dissection and a proposed classification. World Neurosurg. 2018;118:e687–e698. doi: 10.1016/j.wneu.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 12.Dooley J., Bullock W.M., Kumar A.H., MacLeod D.B., Gadsden J. Systematic sonographic and evoked motor identification of the nerve to vastus medialis during adductor canal block. Reg Anesth Pain Med. 2020;45:937–938. doi: 10.1136/rapm-2019-101232. [DOI] [PubMed] [Google Scholar]
- 13.Tran J., Peng P.W.H., Gofeld M., Chan V., Agur A.M.R. Anatomical study of the innervation of posterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2019;44:234–238. doi: 10.1136/rapm-2018-000015. [DOI] [PubMed] [Google Scholar]
- 14.Vickers R. Five steps to safer surgery. Ann R Coll Surg Engl. 2011;93:501. doi: 10.1308/147870811X599334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deloughry J.L., Griffiths R. Arterial tourniquets. Contin Educ Anaesth Crit Care Pain. 2009;9:56–60. [Google Scholar]
- 16.Chazapis M., Kaur N., Kamming D. Improving the peri-operative care of patients by instituting a ‘Block Room’ for regional anaesthesia. BMJ Qual Improv Rep. 2014;3 doi: 10.1136/bmjquality.u204061.w1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Boghdadly K., Nair G., Pawa A., Onwochei D.N. Impact of parallel processing of regional anesthesia with block rooms on resource utilization and clinical outcomes: a systematic review and meta-analysis. Reg Anesth Pain Med. 2020;45:720–726. doi: 10.1136/rapm-2020-101397. [DOI] [PubMed] [Google Scholar]
- 18.Gadsden J., Hadzic A., Gandhi K., et al. The effect of mixing 1.5% mepivacaine and 0.5% bupivacaine on duration of analgesia and latency of block onset in ultrasound-guided interscalene block. Anesth Analg. 2011;112:471–476. doi: 10.1213/ANE.0b013e3182042f7f. [DOI] [PubMed] [Google Scholar]
- 19.Almasi R., Rezman B., Kriszta Z., Patczai B., Wiegand N., Bogar L. Onset times and duration of analgesic effect of various concentrations of local anesthetic solutions in standardized volume used for brachial plexus blocks. Heliyon. 2020;6 doi: 10.1016/j.heliyon.2020.e04718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Desai N., Albrecht E., El-Boghdadly K. Perineural adjuncts for peripheral nerve block. BJA Educ. 2019;19:276–282. doi: 10.1016/j.bjae.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hussain N., Brull R., Sheehy B., et al. Perineural liposomal bupivacaine is not superior to nonliposomal bupivacaine for peripheral nerve block analgesia: a systematic review and meta-analysis. Anesthesiology. 2021;134:147–164. doi: 10.1097/ALN.0000000000003651. [DOI] [PubMed] [Google Scholar]
- 22.Boselli E., Hopkins P., Lamperti M., et al. European Society of Anaesthesiology and Intensive Care Guidelines on peri-operative use of ultrasound for regional anaesthesia (PERSEUS regional anesthesia): peripheral nerves blocks and neuraxial anaesthesia. Eur J Anaesthesiol. 2021;38:219–250. doi: 10.1097/EJA.0000000000001383. [DOI] [PubMed] [Google Scholar]
- 23.Gadsden JC. The role of peripheral nerve stimulation in the era of ultrasound-guided regional anaesthesia. Anaesthesia; 76: 65–73. [DOI] [PubMed]
- 24.Munirama S., McLeod G. A systematic review and meta-analysis of ultrasound versus electrical stimulation for peripheral nerve location and blockade. Anaesthesia. 2015;70:1084–1091. doi: 10.1111/anae.13098. [DOI] [PubMed] [Google Scholar]
- 25.Haslam N., Bedforth N., Pandit J.J. ‘Prep, stop, block’: refreshing ‘stop before you block’ with new national guidance. Anaesthesia. 2022;77:372–375. doi: 10.1111/anae.15647. [DOI] [PubMed] [Google Scholar]
- 26.Harbell M.W., Kolodzie K., Behrends M., et al. Extraplexus versus intraplexus ultrasound-guided interscalene brachial plexus block for ambulatory arthroscopic shoulder surgery: a randomized controlled trial. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Albrecht E., Kirkham K.R., Taffé P., et al. The maximum effective needle-to-nerve distance for ultrasound-guided interscalene block: an exploratory study. Reg Anesth Pain Med. 2014;39:56–60. doi: 10.1097/AAP.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 28.Brull R., Macfarlane A.J.R., Parrington S.J., Koshkin A., Chan V.W.S. Is circumferential injection advantageous for ultrasound-guided popliteal sciatic nerve bBlock? A proof-of-concept study. Reg Anesth Pain Med. 2011;36:266–270. doi: 10.1097/AAP.0b013e318217a6a1. [DOI] [PubMed] [Google Scholar]
- 29.Madsen M.H., Christiansen C.B., Rothe C., Lundstrøm L.H., Lange K.H.W. Longitudinal neural exposure to local anesthetic and nerve block duration: a retrospective analysis of experimental data from healthy volunteer trials. Reg Anesth Pain Med. 2020;45:192–197. doi: 10.1136/rapm-2019-100988. [DOI] [PubMed] [Google Scholar]
- 30.Ode K., Selvaraj S., Smith A.F. Monitoring regional blockade. Anaesthesia. 2017;72:70–75. doi: 10.1111/anae.13742. [DOI] [PubMed] [Google Scholar]
- 31.Neal J.M., Barrington M.J., Brull R., et al. The second ASRA practice advisory on neurologic complications associated with regional anesthesia and pain medicine: executive summary. Reg Anesth Pain Med. 2015;40:401–430. doi: 10.1097/AAP.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 32.Galvin E.M., Niehof S., Medina H.J., et al. Thermographic temperature measurement compared with pinprick and cold sensation in predicting the effectiveness of regional blocks. Anesth Analg. 2006;102:598–604. doi: 10.1213/01.ane.0000189556.49429.16. [DOI] [PubMed] [Google Scholar]
- 33.Joint Formulary Committee. British national formulary (online). London: BMJ Group and Pharmaceutical Press. Available from: https://bnf.nice.org.uk/drugs/levobupivacaine (accessed 20 August 2022).