Abstract
Background
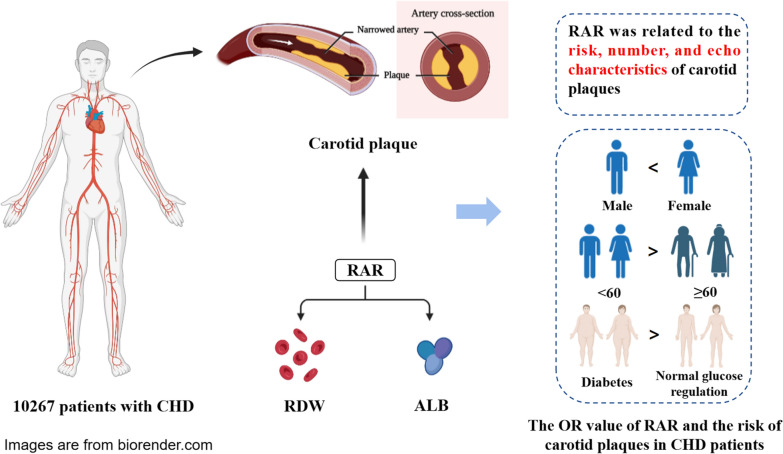
Red cell distribution width/albumin ratio (RAR) is thought to be associated with the prognosis of a variety of diseases, including diabetes and heart failure. To date, no studies have focused on the relationship between RAR and carotid plaque in patients with coronary heart disease (CHD).
Methods
A total of 10,267 patients with CHD were divided according to RAR quartiles (Q1: RAR ≤ 2.960; Q2: 2.960 < RAR ≤ 3.185; Q3: 3.185 < RAR < 3.441; Q4: RAR ≥ 3.441). Logistic regression was used to analyze the relationship between RAR and carotid plaques in CHD patients. The relationship between RAR and carotid plaques in according to sex, age and glucose regulation state groups were also assessed.
Results
Among the 10,267 participants, 75.43% had carotid plaques. After adjusting for confounding factors, RAR was found to be associated with carotid plaque formation (OR: 1.23; 95% CI 1.08–1.39). The risk of carotid plaque formation in the Q4 group was 1.24 times higher than that in the Q1 group. After multivariate adjustment, RAR was associated with the risk of carotid plaque in female (OR: 1.29; 95% CI 1.09–1.52). And the relationship between RAR and carotid plaques in patients younger than 60 years old (OR: 1.43; 95% CI 1.16–1.75) was stronger than that in those older than 60 years old (OR: 1.29; 95% CI 1.10–1.51). Under different glucose metabolism states, RAR had the highest correlation with the risk of carotid plaques in diabetes patients (OR: 1.28; 95% CI 1.04–1.58).
Conclusions
RAR was significantly related to carotid plaques in patients with CHD. In addition, the correlation between RAR and the incidence of carotid plaque in patients with CHD was higher in women and middle-aged and elderly patients. In patients with CHD and diabetes, the correlation between RAR and carotid plaque was higher.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-023-01768-w.
Keywords: Coronary heart disease, Red cell distribution width, Albumin, RDW/ALB ratio, Carotid plaque, Glucose metabolism states
Introduction
Coronary heart disease (CHD) is a common disease of the cardiovascular system. Its pathogenesis is caused by coronary artery atherosclerosis, which causes coronary artery stenosis or occlusion, hinders the blood and oxygen supply of myocardial tissue, and then causes the necrosis of myocardial tissue, leading to the occurrence of the disease. Coronary atherosclerosis is a risk factor for CHD. Carotid plaque is related to coronary atherosclerotic lesions, and carotid atherosclerotic plaques are similar to coronary atherosclerotic plaques in terms of pathogenesis and pathophysiological basis [1]. Studies have found that the existence of carotid plaque is independently related to the risk of CHD [2]. Increased carotid plaque and carotid intima-media thickness (IMT) may increase the risk of cardiovascular disease (CVD) [3]. The condition of carotid atherosclerosis may indicate the occurrence and development of CHD.
Red cell distribution width (RDW) is a simple and readily available parameter that represents the heterogeneity of red cell volume and has traditionally been used in the differential diagnosis of anemia. In recent years, RDW has been found to be associated with a variety of disease processes and prognosis, such as CVD, venous thromboembolism, etc. [4]. RDW has prognostic value for heart failure and CHD, and is an independent risk factor for frailty in elderly patients with CHD [5, 6]. And RDW is associated with a higher risk of developing diabetes [7]. Some researchers believe that chronic hyperglycaemia may mediate the relationship between high RDW and cardiovascular disease [8], RDW may be a useful clinical marker of vascular complications in diabetes (DM) [9]. Serum albumin (ALB) is a biochemical marker of nutritional status [10]. ALB level is strongly negatively correlated with the risk of death from CVD, as well as with the reduction of anti-inflammatory activity and oxidative stress [11]. RDW/ALB ratio (RAR) is a new combination parameter that can be quickly and easily obtained during laboratory tests on admission and can be used in a variety of clinical environments. Studies have shown that RAR is closely associated with CHD, and in addition, RAR showed a better predictive effect than RDW or albumin alone [12, 13].
No studies have shown the relationship between RAR and carotid plaque in patients with CHD. In this study, we sought to explore the impact of RAR on carotid plaque and clarify the association between RAR and carotid plaque in the different glucose metabolic statuses of CHD patients.
Methods
Study participants
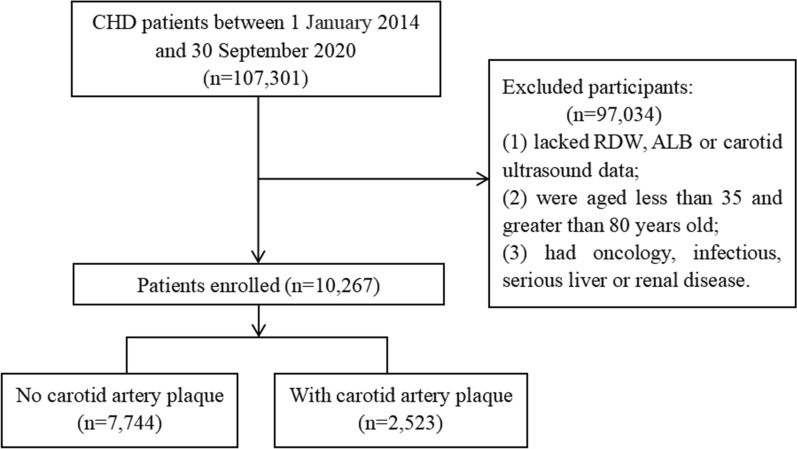
This large-scale, multi-center, retrospective, cross-sectional study included 107,301 CHD patients hospitalized in 6 hospitals in Tianjin from January 1, 2014 to September 30, 2020 [14]. This study excluded patients younger than 35 years or older than 80 years old, patients with tumor, infectious disease, or severe liver or kidney disease, and patients lacking data on RDW, ALB, and carotid ultrasound measurements. A total of 10,267 participants were included in the study. A flowchart of the patients recruitment was shown in Fig. 1.
Fig. 1.
Flowchart of case recruitment
This study was approved by the ethics committee of Tianjin University of Traditional Chinese Medicine (TJUTCM-EC20190008) and registered with the Chinese Clinical Trial Registry (ChiCTR-1900024535) and ClinicalTrials.gov (NCT04026724).
Data collection
Trained medical staff collected data of age, sex, smoking and drinking status, medical history, and prior medication history by means of a standard structured questionnaire [15, 16]. The systolic and diastolic blood pressures (SBP and DBP) were measured by experienced physicians using an electronic device. Hypertension was defined as SBP ≥ 130 mmHg or DBP ≥ 80 mmHg [17].
Fasting venous blood samples were taken from all participants on the second day of hospitalization. RDW, ALB, fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), total cholesterol (TC), triglyceride (TG), high-density lipoprotein-cholesterol (HDL-C), and low-density lipoprotein-cholesterol (LDL-C) levels were measured using an automatic haematology analyzer. Standard laboratory procedure for quality control were strictly followed [18]. Hyperlipidemia was defined as: TC ≥ 6.2 mmol/L (240 mg/dL), TG ≥ 2.3 mmol/L (200 mg/dL) or LDL-C ≥ 4.1 mmol/L (160 mg/dL) or HDL-C ≤ 1.0 mmol/L (40 mg/dL) [19]. Normal glucose tolerance (NGT) was defined as FPG < 5.6 mmol/L or HbA1c < 5.7%, prediabetes (Pre-DM) was defined as FPG 5.6–6.9 mmol/L or HbA1c of 5.7–6.4%, DM was defined as FPG ≥ 7.0 mmol/L or HbA1c ≥ 6.5% [20].
Carotid ultrasound examinations were performed by trained and certified physicians using an ultrasound diagnostic system. In B-mode imaging, the common carotid artery, internal carotid artery, and carotid artery bifurcation were scanned and imaged. Carotid artery color-Doppler was analyzed by professional physicians according to the results of Doppler ultrasound, and the number of carotid plaque and echo characteristics were recorded. The number of carotid plaque was divided into single (n = 1) or multiple (n ≥ 2). The echo properties of carotid plaque can be divided into hypoechoic, isoechoic, hyperechoic, and mixed types. Implement strict quality control procedures for image acquisition and analysis, and inter-laboratory quality evaluations by certified personnel.
Statistical analyses
The χ2 test and Kruskal–Wallis H test were used to compare the characteristics of the participants in the different groups. Odds ratios (ORs) and 95% confidence intervals (CIs) of carotid plaques were estimated for RAR using logistic regression. Four logistic regression models were constructed: Model a, unadjusted; Model b, adjusted for age, sex, SBP, DBP; Model c, adjusted for age, sex, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic; and Model d was adjusted based on Model c with haematologic, rheumatical, diabetes, WBC, CRP, and Hb. The collinearity of the different models was tested before logistic regression. Missing values were imputed using the multiple imputation method. All statistical analyses were performed using SPSS 24.0 (IBM Corp, New York, NY, USA). P < 0.05 was considered statistically significant.
Results
Baseline characteristics
The baseline characteristics of participants are shown in Table 1. 10,267 participants were included for data analysis, the median age was 64 years old, and 5222 was female (50.86%). Among them, 7744 (75.43%) patients had carotid plaques. Based on the RAR quartering method, the participants were divided into four groups: Q1 (RAR ≤ 2.960), Q2 (2.960 < RAR ≤ 3.185), Q3 (3.185 < RAR < 3.441), and Q4 (RAR ≥ 3.441). There were differences in the risk, number, and echo characteristics of carotid plaques among the four RAR groups (P < 0.001). Compared with the Q1 group, the number of patients with carotid plaques in the Q4 group was higher. They were more likely to be older, and had lower levels of TC, TG, HDL-C and LDL-C.
Table 1.
Characteristics of participants according to RAR quartile
| Characteristic | Total (N = 10,267) | RAR quartile | P value | |||
|---|---|---|---|---|---|---|
| Q1 (n = 2564) | Q2 (n = 2561) | Q3 (n = 2576) | Q4 (n = 2566) | |||
| Sex, n (%) | 0.033 | |||||
| Male | 5045 (49.14) | 1300 (50.70) | 1206 (47.09) | 1248 (48.45) | 1291 (50.31) | |
| Female | 5222 (50.86) | 1264 (49.30) | 1355 (52.91) | 1328 (51.55) | 1275 (49.69) | |
| Age (y) | ||||||
| Total, median (IQR) | 64 (59, 69) | 62 (56, 67) | 64 (58, 69) | 65 (60, 70) | 66 (61, 71) | < 0.001 |
| < 60, n (%) | 2856 (27.82) | 970 (37.83) | 768 (29.99) | 611 (23.72) | 507 (19.76) | < 0.001 |
| ≥ 60, n (%) | 7411 (72.18) | 1594 (62.17) | 1793 (70.01) | 1965 (76.28) | 2059 (80.24) | |
| SBP, mmHg, median (IQR) | 140 (128, 156) | 140 (129, 157) | 140 (129, 157) | 140 (127, 157) | 140 (125, 155) | 0.002 |
| DBP, mmHg, median (IQR) | 83 (77, 90) | 83 (79, 91) | 83 (77, 91) | 82 (77, 90) | 80 (75, 90) | < 0.001 |
| TC, mmol/L, median (IQR) | 4.58 (3.81, 5.36) | 4.82 (4.06, 5.58) | 4.66 (3.91, 5.42) | 4.53 (3.80, 5.25) | 4.30 (3.52, 5.09) | < 0.001 |
| TG, mmol/L, median (IQR) | 1.44 (1.04, 2.05) | 1.61 (1.14, 2.27) | 1.52 (1.11, 2.10) | 1.41 (1.03, 2.01) | 1.26 (0.91, 1.77) | < 0.001 |
| LDL-C, mmol/L, median (IQR) | 2.76 (2.15, 3.42) | 2.94 (2.31, 3.59) | 2.82 (2.20, 3.47) | 2.71 (2.13, 3.34) | 2.57 (1.97, 3.25) | < 0.001 |
| HDL-C, mmol/L, median (IQR) | 1.06 (0.89, 1.26) | 1.12 (0.95, 1.32) | 1.07 (0.90, 1.27) | 1.05 (0.89, 1.24) | 1.01 (0.85, 1.20) | < 0.001 |
| RDW-CV, (%), median (IQR) | 12.70 (12.30, 13.30) | 12.20 (11.90, 12.60) | 12.60 (12.20, 12.90) | 12.90 (12.50, 13.30) | 13.50 (13.00, 14.20) | < 0.001 |
| ALB, g/dL, median (IQR) | 4.01 (3.78, 4.25) | 4.40 (4.24, 4.58) | 4.09 (3.97, 4.21) | 3.89 (3.78, 4.03) | 3.63 (3.45, 3.80) | < 0.001 |
| RAR | 3.19 (2.96, 3.44) | 2.81 (2.71, 2.89) | 3.07 (3.02, 3.13) | 3.30 (3.24, 3.37) | 3.68 (3.54, 3.99) | < 0.001 |
| Smoking, n (%) | 4432 (43.17) | 1094 (42.67) | 1069 (41.74) | 1108 (43.01) | 1161 (45.25) | 0.074 |
| Drinking, n (%) | 3164 (30.82) | 871 (33.97) | 778 (30.38) | 770 (29.89) | 745 (29.03) | 0.001 |
| Hypertension, n (%) | 7516 (73.21) | 1941 (75.70) | 1905 (74.39) | 1848 (71.74) | 1822 (71.01) | < 0.001 |
| Hyperlipidemia, n (%) | 3172 (30.90) | 914 (35.65) | 828 (32.33) | 774 (30.05) | 656 (25.57) | < 0.001 |
| Use of antihypertensive, n (%) | 7559 (73.62) | 1862 (72.62) | 1853 (72.35) | 1919 (74.50) | 1925 (75.02) | 0.071 |
| Use of antilipidemic, n (%) | 7584 (73.87) | 1968 (76.76) | 1957 (76.42) | 1917 (74.42) | 1742 (67.89) | < 0.001 |
| CIMT, mm, median (IQR) | 0.10 (0.09, 0.12) | 0.10 (0.09, 0.11) | 0.10 (0.09, 0.12) | 0.10 (0.09, 0.12) | 0.10 (0.09, 0.12) | < 0.001 |
| Carotid artery plaque, n (%) | 7744 (75.43) | 1829 (71.33) | 1885 (73.60) | 1954 (75.85) | 2076 (80.90) | < 0.001 |
| No. of carotid artery plaque, n (%) | < 0.001 | |||||
| 0 | 2523 (24.57) | 735 (28.67) | 676 (26.40) | 622 (24.15) | 490 (19.10) | |
| 1 | 421 (4.10) | 132 (5.15) | 118 (4.61) | 79 (3.07) | 92 (3.59) | |
| ≥ 2 | 7323 (71.33) | 1697 (66.19) | 1767 (69.00) | 1875 (72.79) | 1984 (77.32) | |
| Carotid artery plaque echo property, n (%) | < 0.001 | |||||
| Hypoechoic plaque | 512 (6.61) | 124 (6.78) | 130 (6.90) | 135 (6.91) | 123 (5.92) | |
| Isoechoic plaque | 574 (7.41) | 163 (8.91) | 151 (8.01) | 132 (6.76) | 128 (6.17) | |
| Hyperechoic plaque | 4312 (55.68) | 1048 (57.30) | 1062 (56.34) | 1080 (55.27) | 1122 (54.05) | |
| Mixture plaque | 2346 (30.29) | 494 (27.01) | 542 (28.75) | 607 (31.06) | 703 (33.86) | |
Relationship between RAR and the risk of carotid plaques
As shown in Table 2, when used as a continuous variable, after adjusting for confounding factors, RAR was significantly associated with the risk of carotid plaque (OR: 1.23; 95% CI 1.08–1.39). When RAR as a categorical variable, the risk of carotid plaque in the Q4 group was 1.24 times higher than that in the Q1 group. In further analysis, in the unadjusted or adjusted model, the Ptrend of RAR and carotid plaques was consistent with the results of RAR as a continuous variable (P < 0.01).
Table 2.
Relationship between the RAR and the risk of carotid plaques
| Variables | Carotid artery plaques | |||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | P-value | OR (95% CI)b | P-value | OR (95% CI)c | P-value | OR (95% CI)d | P-value | |
| RAR | 1.52 (1.37, 1.69) | < 0.001 | 1.22 (1.09, 1.36) | < 0.001 | 1.25 (1.12, 1.40) | < 0.001 | 1.23 (1.08, 1.39) | 0.001 |
| Q1 | Reference | Reference | Reference | Reference | ||||
| Q2 | 1.12 (0.99, 1.27) | 0.069 | 0.98 (0.85, 1.11) | 0.706 | 0.98 (0.86, 1.12) | 0.747 | 0.97 (0.85, 1.12) | 0.689 |
| Q3 | 1.26 (1.12, 1.43) | < 0.001 | 0.98 (0.86, 1.13) | 0.804 | 0.99 (0.86, 1.14) | 0.876 | 0.96 (0.84, 1.11) | 0.591 |
| Q4 | 1.70 (1.49, 1.94) | < 0.001 | 1.25 (1.08, 1.44) | 0.003 | 1.28 (1.10, 1.48) | 0.001 | 1.24 (1.07, 1.45) | 0.006 |
| P-trend | < 0.001 | 0.003 | 0.001 | 0.008 | ||||
aModel1: unadjusted
bModel2: adjusted for sex, age, SBP, DBP
cModel3: adjusted for sex, age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic
dModel4: adjusted for sex, age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic, haematologic, rheumatical, diabetes, WBC, CRP, Hb
Relationship between RAR and carotid plaques based on sex and age
As shown in Tables 3 and 4, we observed that there was a significant relationship between RAR and carotid plaque in different sex or age stratification. After multivariate adjustment, RAR was associated with the risk of carotid plaque in female (OR: 1.29; 95% CI 1.09–1.52). After multivariate adjustment, the relationship between RAR and carotid plaques in patients younger than 60 years old (OR: 1.43; 95% CI 1.16–1.75) was stronger than that in those older than 60 years old (OR: 1.29; 95% CI 1.10–1.51). Regardless of sex or age, with Q1 as a reference, Q4 was significantly associated with an increased risk of carotid plaque, which was still significant after multifactorial adjustment.
Table 3.
Relationship between the RAR and the risk of carotid plaques according to sex
| Sex | Variables | Carotid artery plaques | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | P-value | OR (95% CI)b | P-value | OR (95% CI)c | P-value | OR (95% CI)d | P-value | ||
| Male | RAR | 1.59 (1.34, 1.88) | < 0.001 | 1.16 (0.98, 1.36) | 0.082 | 1.19 (1.01, 1.40) | 0.044 | 1.16 (0.96, 1.40) | 0.133 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 1.30 (1.07, 1.59) | 0.010 | 1.07 (0.86, 1.32) | 0.546 | 1.07 (0.87, 1.33) | 0.512 | 1.07 (0.86, 1.33) | 0.553 | |
| Q3 | 1.38 (1.13, 1.68) | 0.002 | 0.99 (0.80, 1.23) | 0.945 | 0.99 (0.80, 1.23) | 0.947 | 0.97 (0.78, 1.21) | 0.816 | |
| Q4 | 1.94 (1.57, 2.39) | < 0.001 | 1.24 (0.99, 1.56) | 0.060 | 1.29 (1.02, 1.62) | 0.035 | 1.27 (0.99, 1.63) | 0.064 | |
| Female | RAR | 1.49 (1.30, 1.72) | < 0.001 | 1.27 (1.10, 1.47) | 0.001 | 1.31 (1.12, 1.52) | 0.001 | 1.29 (1.09, 1.52) | 0.002 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 1.07 (0.91, 1.26) | 0.391 | 0.92 (0.77, 1.09) | 0.345 | 0.92 (0.77, 1.10) | 0.348 | 0.91 (0.77, 1.09) | 0.313 | |
| Q3 | 1.24 (1.05, 1.46) | 0.011 | 0.98 (0.82, 1.17) | 0.797 | 0.98 (0.82, 1.18) | 0.861 | 0.95 (0.79, 1.14) | 0.569 | |
| Q4 | 1.61 (1.36, 1.91) | < 0.001 | 1.25 (1.04, 1.50) | 0.020 | 1.27 (1.05, 1.53) | 0.014 | 1.23 (1.01, 1.50) | 0.042 | |
aModel1: unadjusted
bModel2: adjusted for age, SBP, DBP
cModel3: adjusted for age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic
dModel4: adjusted for age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic, haematologic, rheumatical, diabetes, WBC, CRP, Hb
Table 4.
Relationship between the RAR and the risk of carotid plaques according to age
| Age | Variables | Carotid artery plaques | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | P-value | OR (95% CI)b | P-value | OR (95% CI)c | P-value | OR (95% CI)d | P-value | ||
| < 60 | RAR | 1.30 (1.11, 1.53) | 0.001 | 1.36 (1.14, 1.62) | 0.001 | 1.43 (1.20, 1.71) | < 0.001 | 1.43 (1.16, 1.75) | 0.001 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 1.12 (0.93, 1.36) | 0.244 | 1.13 (0.92, 1.39) | 0.236 | 1.13 (0.92, 1.39) | 0.245 | 1.13 (0.92, 1.40) | 0.248 | |
| Q3 | 0.99 (0.81, 1.21) | 0.908 | 1.01 (0.81, 1.25) | 0.940 | 1.04 (0.83, 1.29) | 0.747 | 1.01 (0.81, 1.26) | 0.950 | |
| Q4 | 1.43 (1.15, 1.79) | 0.002 | 1.51 (1.19, 1.91) | 0.001 | 1.61 (1.26, 2.05) | < 0.001 | 1.60 (1.23, 2.08) | < 0.001 | |
| ≥ 60 | RAR | 1.35 (1.18, 1.54) | < 0.001 | 1.32 (1.15, 1.52) | < 0.001 | 1.34 (1.16, 1.54) | < 0.001 | 1.29 (1.10, 1.51) | 0.002 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 0.96 (0.81, 1.14) | 0.662 | 1.00 (0.84, 1.19) | 0.982 | 1.00 (0.84, 1.19) | 0.960 | 1.00 (0.84, 1.19) | 0.967 | |
| Q3 | 1.11 (0.94, 1.32) | 0.215 | 1.13 (0.95, 1.34) | 0.182 | 1.11 (0.94, 1.33) | 0.228 | 1.09 (0.92, 1.31) | 0.317 | |
| Q4 | 1.37 (1.15, 1.63) | < 0.001 | 1.37 (1.15, 1.64) | < 0.001 | 1.38 (1.15, 1.65) | 0.001 | 1.33 (1.10, 1.60) | 0.003 | |
aModel1: unadjusted
bModel2: adjusted for sex, SBP, DBP
cModel3: adjusted for sex, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic
dModel4: adjusted for sex, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic, haematologic, rheumatical, diabetes, WBC, CRP, Hb
Relationship between the RAR and the risk of carotid plaques according to glucose regulation state
As shown in Table 5, after multivariate adjustment, under different glucose metabolism states, RAR had the highest correlation with the risk of carotid plaques in DM status (OR: 1.28; 95% CI 1.04–1.58). Taking the Q1 as a reference, Q4 was associated with an increased risk of carotid plaques in diabetes. In joint effect analyses, there was a significant additive interaction between RAR and diabetes on the risk of carotid plaque in patients with CHD (RERI 0.337; 95% CI 0.142, 0.532; AP 0.183; 95% CI 0.077, 0.290; SI 1.668; 95% CI 1.107, 2.514) (Additional file 1: Table S1).
Table 5.
Relationship between the RAR and the risk of carotid plaques according to glucose regulation state
| Glucose regulation state | Variables | Carotid artery plaques | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | P-value | OR (95% CI)b | P-value | OR (95% CI)c | P-value | OR (95% CI)d | P-value | ||
| Normal glucose regulation | RAR | 1.68 (1.40, 2.00) | < 0.001 | 1.23 (1.02, 1.49) | 0.030 | 1.23 (1.02, 1.49) | 0.033 | 1.26 (1.02, 1.56) | 0.032 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 1.16 (0.95, 1.42) | 0.138 | 0.99 (0.79, 1.24) | 0.910 | 0.99 (0.79, 1.24) | 0.934 | 0.97 (0.77, 1.22) | 0.806 | |
| Q3 | 1.34 (1.09, 1.65) | 0.006 | 0.99 (0.79, 1.25) | 0.929 | 0.98 (0.77, 1.24) | 0.845 | 0.95 (0.75, 1.21) | 0.671 | |
| Q4 | 1.91 (1.54, 2.37) | < 0.001 | 1.32 (1.04, 1.68) | 0.024 | 1.31 (1.02, 1.67) | 0.035 | 1.33 (1.02, 1.72) | 0.034 | |
| Prediabetes | RAR | 1.34 (1.11, 1.63) | 0.002 | 1.07 (0.88, 1.31) | 0.487 | 1.09 (0.89, 1.33) | 0.409 | 1.11 (0.88, 1.40) | 0.368 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 1.18 (0.94, 1.48) | 0.143 | 1.04 (0.82, 1.34) | 0.736 | 1.06 (0.82, 1.35) | 0.669 | 1.05 (0.82, 1.35) | 0.699 | |
| Q3 | 1.38 (1.10, 1.74) | 0.006 | 1.05 (0.81, 1.35) | 0.718 | 1.03 (0.80, 1.34) | 0.810 | 1.05 (0.81, 1.37) | 0.697 | |
| Q4 | 1.48 (1.17, 1.87) | 0.001 | 1.07 (0.82, 1.39) | 0.612 | 1.09 (0.83, 1.42) | 0.541 | 1.12 (0.84, 1.49) | 0.453 | |
| Diabetes | RAR | 1.53 (1.28, 1.84) | < 0.001 | 1.31 (1.09, 1.58) | 0.004 | 1.41 (1.16, 1.70) | < 0.001 | 1.28 (1.04, 1.58) | 0.021 |
| Q1 | Reference | Reference | Reference | Reference | |||||
| Q2 | 1.06 (0.85, 1.31) | 0.614 | 0.93 (0.74, 1.17) | 0.553 | 0.94 (0.74, 1.18) | 0.586 | 0.92 (0.73, 1.16) | 0.488 | |
| Q3 | 1.11 (0.89, 1.37) | 0.356 | 0.92 (0.73, 1.15) | 0.449 | 0.96 (0.76, 1.20) | 0.697 | 0.91 (0.72, 1.15) | 0.442 | |
| Q4 | 1.71 (1.35, 2.15) | < 0.001 | 1.32 (1.03, 1.69) | 0.029 | 1.42 (1.10, 1.82) | 0.007 | 1.27 (0.97, 1.66) | 0.079 | |
aModel1: unadjusted
bModel2: adjusted for sex, age, SBP, DBP
cModel3: adjusted for sex, age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic
dModel4: adjusted for sex, age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic, haematologic, rheumatical, WBC, CRP, Hb
In addition, we also observed the relationship between age and sex of RAR and the risk of carotid plaque under different glucose metabolism states. RAR was associated with the risk of carotid plaque in female with DM status (OR: 1.33; 95% CI 1.01–1.76) (Table 6). The association in patients younger than 60 years old (OR: 1.59; 95% CI 1.13–2.24) with DM status was stronger than that in those older than 60 years old (OR: 1.35; 95% CI 1.03–1.76) (Table 7).
Table 6.
Relationship between RAR and the risk of carotid plaques according to different glucose regulation state and sex
| Glucose regulation state | Sex | Variables | Carotid artery plaques | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | P-value | OR (95% CI)b | P-value | OR (95% CI)c | P-value | OR (95% CI)d | P-value | |||
| Normal glucose regulation | Male | RAR | 1.62 (1.23, 2.13) | 0.001 | 1.17 (0.89, 1.53) | 0.266 | 1.22 (0.92, 1.61) | 0.169 | 1.25 (0.91, 1.71) | 0.167 |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.40 (1.01, 1.93) | 0.045 | 1.18 (0.83, 1.67) | 0.364 | 1.21 (0.85, 1.73) | 0.293 | 1.16 (0.81, 1.66) | 0.426 | ||
| Q3 | 1.61 (1.16, 2.24) | 0.005 | 1.18 (0.83, 1.69) | 0.365 | 1.20 (0.83, 1.72) | 0.334 | 1.14 (0.79, 1.64) | 0.495 | ||
| Q4 | 2.22 (1.57, 3.13) | < 0.001 | 1.45 (1.00, 2.11) | 0.051 | 1.52 (1.04, 2.23) | 0.031 | 1.54 (1.02, 2.31) | 0.038 | ||
| Female | RAR | 1.62 (1.27, 2.07) | < 0.001 | 1.30 (1.00, 1.68) | 0.048 | 1.26 (0.97, 1.65) | 0.085 | 1.30 (0.98, 1.74) | 0.074 | |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.07 (0.82, 1.39) | 0.619 | 0.87 (0.65, 1.17) | 0.359 | 0.85 (0.64, 1.14) | 0.283 | 0.84 (0.62, 1.13) | 0.248 | ||
| Q3 | 1.14 (0.87, 1.50) | 0.345 | 0.87 (0.64, 1.18) | 0.380 | 0.84 (0.62, 1.15) | 0.272 | 0.82 (0.60, 1.13) | 0.223 | ||
| Q4 | 1.69 (1.27, 2.24) | < 0.001 | 1.24 (0.90, 1.69) | 0.188 | 1.17 (0.85, 1.62) | 0.335 | 1.20 (0.85, 1.68) | 0.302 | ||
| Prediabetes | Male | RAR | 1.46 (1.07, 1.99) | 0.018 | 1.03 (0.76, 1.39) | 0.856 | 1.01 (0.74, 1.37) | 0.968 | 0.98 (0.68, 1.41) | 0.922 |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.37 (0.94, 2.00) | 0.101 | 1.11 (0.74, 1.68) | 0.604 | 1.13 (0.74, 1.71) | 0.572 | 1.12 (0.74, 1.71) | 0.594 | ||
| Q3 | 1.35 (0.93, 1.96) | 0.110 | 0.85 (0.57, 1.29) | 0.453 | 0.82 (0.54, 1.24) | 0.344 | 0.82 (0.54, 1.25) | 0.357 | ||
| Q4 | 1.58 (1.07, 2.33) | 0.021 | 0.91 (0.60, 1.40) | 0.679 | 0.89 (0.57, 1.38) | 0.604 | 0.89 (0.55, 1.45) | 0.641 | ||
| Female | RAR | 1.29 (1.00, 1.66) | 0.047 | 1.11 (0.85, 1.44) | 0.444 | 1.17 (0.89, 1.53) | 0.253 | 1.24 (0.92, 1.67) | 0.154 | |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.18 (0.88, 1.58) | 0.260 | 1.02 (0.75, 1.39) | 0.902 | 1.03 (0.76, 1.42) | 0.837 | 1.03 (0.75, 1.41) | 0.868 | ||
| Q3 | 1.48 (1.09, 2.00) | 0.012 | 1.18 (0.86, 1.64) | 0.310 | 1.19 (0.86, 1.65) | 0.302 | 1.24 (0.89, 1.73) | 0.211 | ||
| Q4 | 1.51 (1.11, 2.05) | 0.009 | 1.17 (0.84, 1.63) | 0.360 | 1.23 (0.88, 1.74) | 0.230 | 1.27 (0.89, 1.82) | 0.184 | ||
| Diabetes | Male | RAR | 1.70 (1.27, 2.29) | < 0.001 | 1.29 (0.97, 1.73) | 0.080 | 1.40 (1.04, 1.89) | 0.025 | 1.25 (0.90, 1.75) | 0.182 |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.20 (0.85, 1.68) | 0.296 | 0.98 (0.69, 1.40) | 0.909 | 0.97 (0.68, 1.39) | 0.875 | 0.95 (0.67, 1.37) | 0.792 | ||
| Q3 | 1.22 (0.87, 1.71) | 0.249 | 0.95 (0.66, 1.35) | 0.760 | 0.98 (0.68, 1.41) | 0.915 | 0.94 (0.65, 1.36) | 0.748 | ||
| Q4 | 2.04 (1.41, 2.97) | < 0.001 | 1.39 (0.94, 2.07) | 0.100 | 1.57 (1.05, 2.36) | 0.029 | 1.41 (0.91, 2.18) | 0.122 | ||
| Female | RAR | 1.49 (1.18, 1.90) | 0.001 | 1.34 (1.05, 1.71) | 0.019 | 1.42 (1.10, 1.83) | 0.007 | 1.33 (1.01, 1.76) | 0.041 | |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.01 (0.76, 1.35) | 0.940 | 0.91 (0.67, 1.23) | 0.527 | 0.91 (0.67, 1.24) | 0.547 | 0.89 (0.65, 1.22) | 0.471 | ||
| Q3 | 1.11 (0.84, 1.47) | 0.452 | 0.90 (0.67, 1.21) | 0.483 | 0.94 (0.69, 1.27) | 0.667 | 0.88 (0.65, 1.20) | 0.417 | ||
| Q4 | 1.60 (1.18, 2.16) | 0.002 | 1.29 (0.93, 1.78) | 0.122 | 1.34 (0.97, 1.87) | 0.081 | 1.21 (0.86, 1.71) | 0.281 | ||
aModel1: unadjusted
bModel2: adjusted for age, SBP, DBP
cModel3: adjusted for age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic
dModel4: adjusted for age, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic, haematologic, rheumatical, WBC, CRP, Hb
Table 7.
Relationship between RAR and the risk of carotid plaques according to different glucose regulation state and age
| Glucose regulation state | Age | Variables | Carotid artery plaques | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI)a | P-value | OR (95% CI)b | P-value | OR (95% CI)c | P-value | OR (95% CI)d | P-value | |||
| Normal glucose regulation | < 60 | RAR | 1.46 (1.10, 1.94) | 0.009 | 1.50 (1.10, 2.04) | 0.011 | 1.55 (1.13, 2.13) | 0.007 | 1.51 (1.06, 2.16) | 0.022 |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.09 (0.80, 1.50) | 0.578 | 1.09 (0.78, 1.53) | 0.618 | 1.07 (0.76, 1.51) | 0.695 | 1.06 (0.75, 1.51) | 0.743 | ||
| Q3 | 1.11 (0.79, 1.55) | 0.552 | 1.10 (0.77, 1.57) | 0.612 | 1.08 (0.75, 1.56) | 0.673 | 1.05 (0.72, 1.53) | 0.808 | ||
| Q4 | 1.56 (1.09, 2.24) | 0.016 | 1.63 (1.10, 2.40) | 0.014 | 1.67 (1.12, 2.49) | 0.011 | 1.62 (1.05, 2.49) | 0.028 | ||
| ≥ 60 | RAR | 1.40 (1.12, 1.76) | 0.003 | 1.28 (1.01, 1.61) | 0.040 | 1.23 (0.97, 1.57) | 0.084 | 1.26 (0.97, 1.64) | 0.080 | |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.00 (0.76, 1.32) | 0.999 | 1.02 (0.76, 1.37) | 0.886 | 1.03 (0.77, 1.38) | 0.847 | 1.03 (0.76, 1.38) | 0.873 | ||
| Q3 | 1.15 (0.86, 1.53) | 0.340 | 1.09 (0.81, 1.46) | 0.576 | 1.06 (0.78, 1.44) | 0.707 | 1.04 (0.77, 1.41) | 0.796 | ||
| Q4 | 1.50 (1.13, 2.01) | 0.006 | 1.41 (1.04, 1.90) | 0.025 | 1.35 (0.99, 1.85) | 0.056 | 1.38 (1.00, 1.91) | 0.051 | ||
| Prediabetes | < 60 | RAR | 1.05 (0.78, 1.42) | 0.736 | 1.08 (0.79, 1.48) | 0.645 | 1.10 (0.79, 1.53) | 0.570 | 1.20 (0.81, 1.79) | 0.372 |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.05 (0.73, 1.50) | 0.812 | 1.01 (0.69, 1.49) | 0.950 | 1.04 (0.71, 1.54) | 0.827 | 1.08 (0.72, 1.61) | 0.704 | ||
| Q3 | 0.83 (0.56, 1.23) | 0.357 | 0.89 (0.59, 1.36) | 0.599 | 0.90 (0.59, 1.37) | 0.617 | 0.90 (0.59, 1.40) | 0.651 | ||
| Q4 | 1.02 (0.66, 1.56) | 0.947 | 1.04 (0.66, 1.64) | 0.854 | 1.07 (0.67, 1.70) | 0.793 | 1.20 (0.71, 2.04) | 0.495 | ||
| ≥ 60 | RAR | 1.22 (0.95, 1.56) | 0.113 | 1.23 (0.95, 1.58) | 0.119 | 1.22 (0.94, 1.59) | 0.126 | 1.23 (0.92, 1.64) | 0.163 | |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.11 (0.82, 1.51) | 0.511 | 1.19 (0.87, 1.64) | 0.269 | 1.19 (0.87, 1.64) | 0.273 | 1.20 (0.87, 1.65) | 0.269 | ||
| Q3 | 1.35 (0.99, 1.84) | 0.056 | 1.39 (1.01, 1.91) | 0.041 | 1.35 (0.98, 1.86) | 0.069 | 1.37 (0.99, 1.90) | 0.056 | ||
| Q4 | 1.27 (0.94, 1.73) | 0.124 | 1.34 (0.98, 1.84) | 0.071 | 1.33 (0.96, 1.85) | 0.083 | 1.33 (0.95, 1.87) | 0.100 | ||
| Diabetes | < 60 | RAR | 1.37 (1.04, 1.82) | 0.027 | 1.45 (1.08, 1.96) | 0.015 | 1.64 (1.20, 2.24) | 0.002 | 1.59 (1.13, 2.24) | 0.008 |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 1.26 (0.90, 1.76) | 0.176 | 1.30 (0.91, 1.84) | 0.145 | 1.31 (0.92, 1.87) | 0.139 | 1.31 (0.92, 1.88) | 0.140 | ||
| Q3 | 1.00 (0.71, 1.42) | 0.998 | 1.01 (0.71, 1.46) | 0.944 | 1.12 (0.78, 1.63) | 0.537 | 1.09 (0.75, 1.59) | 0.653 | ||
| Q4 | 1.70 (1.15, 2.52) | 0.008 | 1.84 (1.22, 2.77) | 0.004 | 2.16 (1.41, 3.30) | < 0.001 | 2.10 (1.33, 3.33) | 0.002 | ||
| ≥ 60 | RAR | 1.39 (1.11, 1.75) | 0.005 | 1.43 (1.12, 1.81) | 0.004 | 1.52 (1.19, 1.94) | 0.001 | 1.35 (1.03, 1.76) | 0.031 | |
| Q1 | Reference | Reference | Reference | Reference | ||||||
| Q2 | 0.83 (0.62, 1.12) | 0.220 | 0.84 (0.62, 1.14) | 0.260 | 0.83 (0.61, 1.13) | 0.242 | 0.83 (0.61, 1.12) | 0.219 | ||
| Q3 | 0.91 (0.69, 1.22) | 0.535 | 0.95 (0.71, 1.27) | 0.712 | 0.95 (0.71, 1.28) | 0.740 | 0.91 (0.67, 1.23) | 0.530 | ||
| Q4 | 1.31 (0.97, 1.78) | 0.078 | 1.34 (0.98, 1.83) | 0.065 | 1.39 (1.02, 1.91) | 0.040 | 1.23 (0.88, 1.71) | 0.219 | ||
aModel1: unadjusted
bModel2: adjusted for sex, SBP, DBP
cModel3: adjusted for sex, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic
dModel4: adjusted for sex, SBP, DBP, TC, TG, smoking, drinking, use of antihypertensives, use of antilipidemic, haematologic, rheumatical, WBC, CRP, Hb
Relationship between RAR and the number and echo characteristics of carotid plaques
As shown in Additional file 1: Table S2, when RAR was included as a categorical variable, RAR was significantly correlated with multiple carotid plaques, the Q4 group was 1.26 times higher than the Q1 group. As shown in Additional file 1: Table S3, when RAR was included as a continuous variable, after adjustment for confounding factors, RAR was significantly correlated with hypoechoic plaque (OR: 1.27; 95% CI 1.00–1.59), and mixture plaque (OR: 1.48; 95% CI 1.28–1.71). When RAR was included as a categorical variable, RAR was significantly associated with mixture plaque, the Q4 group was 1.66 times higher than the Q1 group.
Discussion
Our study found that RAR was significantly related to carotid plaque formation in CHD patients and was strongest in diabetic glycemic state. To the best of our knowledge, this is the first study to investigate the predictive value of RAR, a novel combined biomarker, with carotid plaque in patients with CHD.
RDW reflects the size distribution of red blood cells. Traditionally, it is used together with other hematological indicators for the differential diagnosis of anemia. Research shows that RDW can be considered as an indicator of chronic inflammation [21]. In recent years, it has been gradually found that RDW is associated with CVD mortality [22, 23], RDW can also be used as a predictor of adverse outcomes in patients with carotid atherosclerosis [24]. High RDW correlates with an increased risk of carotid atherosclerosis [25]. In a cross-sectional study of middle-aged and elderly hypertensive patients, the results showed that with the increase of RDW, the proportion of carotid atherosclerosis patients increased [26]. In a cohort study, it was found that RDW was associated with plaque in carotid atherosclerosis, and the association between RDW and the development of CVD could be explained by atherosclerosis [27]. The erythrocyte membrane contains a large amount of free cholesterol [28], the accumulation of erythrocytes within the atherosclerotic plaque may promote plaque growth and instability [29]. Unstable plaques rich in cholesterol are easy to rupture, so prone to cause acute atherosclerosis events.
ALB is an essential protein in human plasma, widely used to evaluate the nutritional status and reflect the systemic information [30]. Hypoalbuminemia results from and reflects the inflammatory state [31]. Atherosclerosis is an inflammatory disease, which participates in the process of CVD [32]. ALB plays an anti-inflammatory role in this process, and once ALB decreases, the disease process will deteriorate. Several studies have reported an association between low ALB and an increased risk of cardiovascular events [33, 34]. In addition, the prognostic value of low ALB in acute coronary syndrome and stable CHD has also been reported [35–37]. The synthesis rate of ALB is affected by nutrient intake and systemic inflammation [38]. Moreover, the decrease of ALB level is related to the increase of blood viscosity, impairment of endothelial function, and the increase of synthesis of an important mediator of platelet-derived carotid stenosis [39–42]. These may be a potential mechanism to link serum ALB with the severity of carotid artery disease.
RAR is a combination of two classic clinical evaluation parameters, and RAR is a potential novel biomarker, which can be quickly and easily obtained in the laboratory tests on admission. In recent years, studies have shown that RAR is closely related to CHD, and it may be a key indicator for evaluating the severity of CVD. Li et al. found that RAR is a simple and a risk factor for poor prognosis in acute myocardial infarction (AMI) patients, the lower RAR level, the higher the short-term and long-term survival rate of patients [43]. Weng et al. believed that RAR had a better predictive ability for all-cause mortality of patients after PCI, and was superior to RDW or ALB alone. The RAR of patients with CHD may be positively correlated with the severity of CAD [44]. The rupture of atherosclerotic plaque and subsequent thrombosis are the main causes of acute cardiovascular events [27]. Our results suggest that the formation and development of carotid atherosclerosis may play a role in the relationship between RAR and cardiovascular incidence rate and mortality.
We also observed the relationship between RAR and carotid plaque by sex and age. RAR was associated with the risk of carotid plaque in female. And the relationship between RAR and carotid plaque was stronger in patients under 60 years of age than in those over 60 years of age. Similar results were found in a previous retrospective cohort study of the association of RAR in patients with AMI, the subgroup analysis showed that the effect of RAR was higher in female patients than in male patients [43]. We thought it might have something to do with women’s hormone levels. In the study on the influence of RDW and RAR on the all-cause mortality of patients with type 2 diabetes mellitus and foot ulcer, it was found that RAR was associated with high all-cause mortality of patients aged < 65 years old and patients aged ≥ 65 years old, but the association was stronger in younger and middle-aged patients [45], which was similar to our results.
Moreover, under different glucose metabolism states, RAR has the highest correlation with the risk of carotid plaque in diabetic blood glucose state. Studies have shown that RAR is strongly associated with all-cause mortality in diabetes [45], which may be because diabetes is related to changes in deformability and mechanical properties of red blood cells, increased adhesion and increased osmotic vulnerability [7]. Research shows that in the sample of adult diabetes patients, higher RDW values are associated with an increased risk of CVD [9]. It is known that chronic hyperglycemia accelerates atherosclerosis by increasing oxidative stress [46], which may be one of the potential mechanisms of increased RDW and increased risk of carotid plaque. Inflammation can affect erythropoiesis, red blood cell cycle half-life and red blood cell deformability, promote cell heterotopia, and thus improve the level of RDW [47]. Higher RDW levels are independently associated with higher CRP levels [48], which is a recognized marker of inflammation and CVD [49]. Diabetes is associated with chronic inflammation [50]. Inflammatory activity has been confirmed to increase in patients with type 2 diabetes. Similarly, the increase in the concentration of inflammatory markers (such as CRP) is also involved in the occurrence and progression of long-term macrovascular complications in diabetes [50]. Thus, the relationship between RDW and inflammation can at least partially explain the relationship between CVD and RDW that we found in diabetes patients.
At the same time, among the plaque echo property, RAR has the strongest relationship with mixture plaque. The hypoechoic plaque contains relatively more lipid components and more inflammatory substances, and the plaque are easy to rupture, with poor stability, while hyperechoic plaques have the opposite. RAR showed no obvious specificity between hyperechoic and isoechoic plaque properties.
This study was a multicenter, retrospective clinical study. To our knowledge, this is the first study on the correlation between RAR and carotid plaque in patients with CHD. This study has a large number of participants, and we have established several confounding factor models and adjusted them, and the results are convincing. However, this study has several limitations. First of all, this is a multi-center study, and there may be deviations in the measurement methods of different research centers. However, the quality of external clinical laboratories in each center is evaluated by practitioners, which greatly improves the reliability. Furthermore, body mass index (BMI) is an important confounding factor in CHD and carotid plaques. Because much BMI data were missing from this study, it was not included in the model. Finally, this is a cross-sectional study. It is difficult to draw a causal conclusion without taking time as a factor. We plan to further explore this relationship in a prospective study in future.
Conclusion
Our study demonstrated that RAR in patients with CHD was significantly related to carotid plaque. This association was more significant in women and patients aged < 60 years people. In addition, under different glucose metabolism states, RAR has a higher correlation with the risk of carotid plaque in DM patients. In conclusion, RAR, as a simple and practical parameter, provided reference value for the prevention and risk stratification of carotid plaque in patients with CHD.
Supplementary Information
Additional file 1: Table S1. Additive interaction between RAR and diabetes for the risk of carotid plaques. Table S2. Relationship between the RAR and the risk of number of carotid plaque. Table S3. Relationship between the RAR and the risk of carotid plaque echo property.
Acknowledgements
We thank all the participants in the study and the members of the survey teams, as well as the financial support.
Abbreviations
- ALB
Serum albumin
- CIs
Confidence intervals
- CHD
Coronary heart disease
- CVD
Cardiovascular disease
- DBP
Diastolic blood pressures
- DM
Diabetes
- FPG
Fasting plasma glucose
- HbA1c
Glycated hemoglobin
- HDL-C
High-density lipoprotein-cholesterol
- IMT
Intima-media thickness
- LDL-C
Low-density lipoprotein-cholesterol
- ORs
Odds ratios
- Pre-DM
Prediabetes
- RAR
Red cell distribution width/albumin ratio
- RDW
Red cell distribution width
- SBP
Systolic blood pressures
- TC
Total cholesterol
- TG
Triglyceride
Author contributions
CY, HW, SG, and MH participated in the study design and statistical analysis. MH, FL, and ZL analyzed the data together and drafted the manuscript. YL, JS, MM, YH participated in data collection, and HB participated in statistical analysis. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (82074140, 82104565, and 82204142), Tianjin Hongrentang Pharmaceutical Co., Ltd., Tianjin, China (No. HX2020-16), Shanghai Hutchison Pharmaceuticals Ltd. (No. HX2020-39), and Key Discipline Development in Preventive Medicine of Traditional Chinese Medicine (2023).
Availability of data and materials
The datasets used and/or analyzed in the present study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Tianjin University of Traditional Chinese Medicine (approval number: TJUTCM-EC20190008) and registered with the Chinese Clinical Trial Registry on July 14, 2019 (registration number ChiCTR-1900024535) and in Clinical Trials.gov on July 18, 2019 (registration number: NCT04026724).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Mengnan Huang, Fanfan Liu and Zhu Li are co-first authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shan Gao, Email: gaoshan@tjutcm.edu.cn.
Hongwu Wang, Email: tjwanghw55@163.com.
Chunquan Yu, Email: ycqtjutcm@foxmail.com.
References
- 1.Polak JF, Szklo M, Kronmal RA, Burke GL, Shea S, Zavodni AE, O'Leary DH. The value of carotid artery plaque and intima-media thickness for incident cardiovascular disease: the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2013;2(2):e000087. doi: 10.1161/JAHA.113.000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mehta A, Rigdon J, Tattersall MC, German CA, Barringer TA, 3rd, Joshi PH, Sperling LS, Budoff MJ, Bertoni A, Michos ED, Blaha MJ, Stein JH, Shapiro MD. Association of carotid artery plaque with cardiovascular events and incident coronary artery calcium in individuals with absent coronary calcification: the MESA. Circ Cardiovasc Imaging. 2021;14(4):e011701. doi: 10.1161/CIRCIMAGING.120.011701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gepner AD, Young R, Delaney JA, Tattersall MC, Blaha MJ, Post WS, Gottesman RF, Kronmal R, Budoff MJ, Burke GL, Folsom AR, Liu K, Kaufman J, Stein JH. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Imaging. 2015;8(1):e002262. doi: 10.1161/CIRCIMAGING.114.002262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015;52(2):86–105. doi: 10.3109/10408363.2014.992064. [DOI] [PubMed] [Google Scholar]
- 5.Baggen VJM, van den Bosch AE, van Kimmenade RR, Eindhoven JA, Witsenburg M, Cuypers JAAE, Leebeek FWG, Boersma E, Roos-Hesselink JW. Red cell distribution width in adults with congenital heart disease: a worldwide available and low-cost predictor of cardiovascular events. Int J Cardiol. 2018;260:60–65. doi: 10.1016/j.ijcard.2018.02.118. [DOI] [PubMed] [Google Scholar]
- 6.Qu J, Zhou T, Xue M, Sun H, Shen Y, Chen Y, Tang L, Qian L, You J, Yang R, Liu Y. Correlation analysis of hemoglobin-to-red blood cell distribution width ratio and frailty in elderly patients with coronary heart disease. Front Cardiovasc Med. 2021;8:728800. doi: 10.3389/fcvm.2021.728800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engström G, Smith JG, Persson M, Nilsson PM, Melander O, Hedblad B. Red cell distribution width, haemoglobin A1c and incidence of diabetes mellitus. J Intern Med. 2014;276(2):174–183. doi: 10.1111/joim.12188. [DOI] [PubMed] [Google Scholar]
- 8.Veeranna V, Zalawadiya SK, Panaich SS, Ramesh K, Afonso L. The association of red cell distribution width with glycated hemoglobin among healthy adults without diabetes mellitus. Cardiology. 2012;122(2):129–132. doi: 10.1159/000339225. [DOI] [PubMed] [Google Scholar]
- 9.Malandrino N, Wu WC, Taveira TH, Whitlatch HB, Smith RJ. Association between red blood cell distribution width and macrovascular and microvascular complications in diabetes. Diabetologia. 2012;55(1):226–235. doi: 10.1007/s00125-011-2331-1. [DOI] [PubMed] [Google Scholar]
- 10.Che R, Huang X, Zhao W, Jiang F, Wu L, Zhang Z, Bian T, Ma Q, Yu Z, Zhang Q, Dong K, Song H, Ji X. Low serum albumin level as a predictor of hemorrhage transformation after intravenous thrombolysis in ischemic stroke patients. Sci Rep. 2017;7(1):7776. doi: 10.1038/s41598-017-06802-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grimm G, Haslacher H, Kampitsch T, Endler G, Marsik C, Schickbauer T, Wagner O, Jilma B. Sex differences in the association between albumin and all-cause and vascular mortality. Eur J Clin Invest. 2009;39(10):860–865. doi: 10.1111/j.1365-2362.2009.02189.x. [DOI] [PubMed] [Google Scholar]
- 12.Ni Q, Wang X, Wang J, Chen P. The red blood cell distribution width-albumin ratio: a promising predictor of mortality in heart failure patients—a cohort study. Clin Chim Acta. 2022;527:38–46. doi: 10.1016/j.cca.2021.12.027. [DOI] [PubMed] [Google Scholar]
- 13.Long J, Xie X, Xu D, Huang C, Liu Y, Meng X, Cai X, Fang X. Association between red blood cell distribution width-to-albumin ratio and prognosis of patients with aortic aneurysms. Int J Gen Med. 2021;14:6287–6294. doi: 10.2147/IJGM.S328035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Li Z, Wang X, Ni T, Ma M, He Y, Yang R, Luo M. Effects of adjuvant Chinese patent medicine therapy on major adverse cardiovascular events in patients with coronary heart disease angina pectoris: a population-based retrospective cohort study. Acupunct Herb Med. 2022;2(2):110–118. doi: 10.1097/HM9.0000000000000028. [DOI] [Google Scholar]
- 15.Barua RS, Rigotti NA, Benowitz NL, Cummings KM, Jazayeri MA, Morris PB, Ratchford EV, Sarna L, Stecker EC, Wiggins BS. 2018 ACC expert consensus decision pathway on tobacco cessation treatment: a report of the American college of cardiology task force on clinical expert consensus documents. J Am Coll Cardiol. 2018;72(25):3332–3365. doi: 10.1016/j.jacc.2018.10.027. [DOI] [PubMed] [Google Scholar]
- 16.Fan AZ, Ruan WJ, Chou SP. Re-examining the relationship between alcohol consumption and coronary heart disease with a new lens. Prev Med. 2019;118:336–343. doi: 10.1016/j.ypmed.2018.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30(3):160–164. doi: 10.1016/j.tcm.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Li Z, Cheng Q, Liu Y, Cheng X, Wang S, He Y, Wang X, Huang M, Li Y, Xue X, Xu Y, Li L, Zheng Y, Yang R, Gao S, Yu C. Low-/high-density lipoprotein cholesterol ratio and carotid plaques in patients with coronary heart disease: a Chinese cohort study. Lipids Health Dis. 2021;20(1):144. doi: 10.1186/s12944-021-01575-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang L, Li Z, Song Y, Liu Y, Zhao H, Liu Y, Zhang T, Yuan Y, Cai X, Wang S, Wang P, Gao S, Li L, Li Y, Yu C. Study on urine metabolic profiling and pathogenesis of hyperlipidemia. Clin Chim Acta. 2019;495:365–373. doi: 10.1016/j.cca.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 20.American Diabetes Association 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S15–S33. doi: 10.2337/dc21-S002. [DOI] [PubMed] [Google Scholar]
- 21.Targoński R, Sadowski J, Starek-Stelmaszczyk M, Targoński R, Rynkiewicz A. Prognostic significance of red cell distribution width and its relation to increased pulmonary pressure and inflammation in acute heart failure. Cardiol J. 2020;27(4):394–403. doi: 10.5603/CJ.a2018.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arbel Y, Weitzman D, Raz R, Steinvil A, Zeltser D, Berliner S, Chodick G, Shalev V. Red blood cell distribution width and the risk of cardiovascular morbidity and all-cause mortality. A population-based study. Thromb Haemost. 2014;111(2):300–307. doi: 10.1160/TH13-07-0567. [DOI] [PubMed] [Google Scholar]
- 23.Pascual-Figal DA, Bonaque JC, Redondo B, Caro C, Manzano-Fernandez S, Sánchez-Mas J, Garrido IP, Valdes M. Red blood cell distribution width predicts long-term outcome regardless of anaemia status in acute heart failure patients. Eur J Heart Fail. 2009;11(9):840–846. doi: 10.1093/eurjhf/hfp109. [DOI] [PubMed] [Google Scholar]
- 24.Wonnerth A, Krychtiuk KA, Mayer FJ, Minar E, Wojta J, Schillinger M, Koppensteiner R, Hoke M. Red cell distribution width and mortality in carotid atherosclerosis. Eur J Clin Invest. 2016;46(2):198–204. doi: 10.1111/eci.12584. [DOI] [PubMed] [Google Scholar]
- 25.Furer A, Finkelstein A, Halkin A, Revivo M, Zuzut M, Berliner S, Herz I, Solodukhin A, Ofer H, Keren G, Banai S, Arbel Y. High red blood cell distribution width and preclinical carotid atherosclerosis. Biomarkers. 2015;20(6–7):376–381. doi: 10.3109/1354750X.2015.1096304. [DOI] [PubMed] [Google Scholar]
- 26.Wen Y. High red blood cell distribution width is closely associated with risk of carotid artery atherosclerosis in patients with hypertension. Exp Clin Cardiol. 2010;15(3):37–40. [PMC free article] [PubMed] [Google Scholar]
- 27.Lappegård J, Ellingsen TS, Vik A, Skjelbakken T, Brox J, Mathiesen EB, Johnsen SH, Brækkan SK, Hansen JB. Red cell distribution width and carotid atherosclerosis progression. The Tromsø Study. Thromb Haemost. 2015;113(3):649–654. doi: 10.1160/TH14-07-0606. [DOI] [PubMed] [Google Scholar]
- 28.Kolodgie FD, Burke AP, Nakazawa G, Cheng Q, Xu X, Virmani R. Free cholesterol in atherosclerotic plaques: where does it come from? Curr Opin Lipidol. 2007;18(5):500–507. doi: 10.1097/MOL.0b013e3282efa35b. [DOI] [PubMed] [Google Scholar]
- 29.Kolodgie FD, Gold HK, Burke AP, Fowler DR, Kruth HS, Weber DK, Farb A, Guerrero LJ, Hayase M, Kutys R, Narula J, Finn AV, Virmani R. Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med. 2003;349(24):2316–2325. doi: 10.1056/NEJMoa035655. [DOI] [PubMed] [Google Scholar]
- 30.Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: pathogenesis and clinical significance. JPEN. 2019;43(2):181–193. doi: 10.1002/jpen.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gatta A, Verardo A, Bolognesi M. Hypoalbuminemia. Intern Emerg Med. 2012;7(Suppl 3):S193–S199. doi: 10.1007/s11739-012-0802-0. [DOI] [PubMed] [Google Scholar]
- 32.Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 33.Schalk BW, Visser M, Bremmer MA, Penninx BW, Bouter LM, Deeg DJ. Change of serum albumin and risk of cardiovascular disease and all-cause mortality: longitudinal aging study Amsterdam. Am J Epidemiol. 2006;164(10):969–977. doi: 10.1093/aje/kwj312. [DOI] [PubMed] [Google Scholar]
- 34.Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, Tang WW, Methvin A, Smith AL, Bauer DC, Newman AB, Kim L, Harris TB, Kritchevsky SB, Butler J, Health ABC Study Serum albumin concentration and heart failure risk the health, aging, and body composition study. Am Heart J. 2010;160(2):279–285. doi: 10.1016/j.ahj.2010.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kurtul A, Murat SN, Yarlioglues M, Duran M, Ocek AH, Koseoglu C, Celık IE, Kilic A, Aksoy O. Usefulness of serum albumin concentration to predict high coronary SYNTAX score and in-hospital mortality in patients with acute coronary syndrome. Angiology. 2016;67(1):34–40. doi: 10.1177/0003319715575220. [DOI] [PubMed] [Google Scholar]
- 36.Oduncu V, Erkol A, Karabay CY, Kurt M, Akgün T, Bulut M, Pala S, Kirma C. The prognostic value of serum albumin levels on admission in patients with acute ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron Artery Dis. 2013;24(2):88–94. doi: 10.1097/MCA.0b013e32835c46fd. [DOI] [PubMed] [Google Scholar]
- 37.Chien SC, Chen CY, Leu HB, Su CH, Yin WH, Tseng WK, Wu YW, Lin TH, Chang KC, Wang JH, Wu CC, Yeh HI, Chen JW. Association of low serum albumin concentration and adverse cardiovascular events in stable coronary heart disease. Int J Cardiol. 2017;241:1–5. doi: 10.1016/j.ijcard.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 38.Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17(6):432–437. doi: 10.1111/j.0894-0959.2004.17603.x. [DOI] [PubMed] [Google Scholar]
- 39.Joles JA, Willekes-Koolschijn N, Koomans HA. Hypoalbuminemia causes high blood viscosity by increasing red cell lysophosphatidylcholine. Kidney Int. 1997;52(3):761–770. doi: 10.1038/ki.1997.393. [DOI] [PubMed] [Google Scholar]
- 40.Zhang WJ, Frei B. Albumin selectively inhibits TNF alpha-induced expression of vascular cell adhesion molecule-1 in human aortic endothelial cells. Cardiovasc Res. 2002;55(4):820–829. doi: 10.1016/s0008-6363(02)00492-3. [DOI] [PubMed] [Google Scholar]
- 41.Gresele P, Deckmyn H, Huybrechts E, Vermylen J. Serum albumin enhances the impairment of platelet aggregation with thromboxane synthase inhibition by increasing the formation of prostaglandin D2. Biochem Pharmacol. 1984;33(13):2083–2088. doi: 10.1016/0006-2952(84)90577-x. [DOI] [PubMed] [Google Scholar]
- 42.Mikhailidis DP, Ganotakis ES. Plasma albumin and platelet function: relevance to atherogenesis and thrombosis. Platelets. 1996;7(3):125–137. doi: 10.3109/09537109609023571. [DOI] [PubMed] [Google Scholar]
- 43.Li D, Ruan Z, Wu B. Association of red blood cell distribution width-albumin ratio for acute myocardial infarction patients with mortality: a retrospective cohort study. Clin Appl Thromb Hemost. 2022;28:10760296221121286. doi: 10.1177/10760296221121286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weng Y, Peng Y, Xu Y, Wang L, Wu B, Xiang H, Ji K, Guan X. The ratio of red blood cell distribution width to albumin is correlated with all-cause mortality of patients after percutaneous coronary intervention—a retrospective cohort study. Front Cardiovasc Med. 2022;9:869816. doi: 10.3389/fcvm.2022.869816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hong J, Hu X, Liu W, Qian X, Jiang F, Xu Z, Shen F, Zhu H. Impact of red cell distribution width and red cell distribution width/albumin ratio on all-cause mortality in patients with type 2 diabetes and foot ulcers: a retrospective cohort study. Cardiovasc Diabetol. 2022;21(1):91. doi: 10.1186/s12933-022-01534-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khaw KT, Wareham N. Glycated hemoglobin as a marker of cardiovascular risk. Curr Opin Lipidol. 2006;17(6):637–643. doi: 10.1097/MOL.0b013e3280106b95. [DOI] [PubMed] [Google Scholar]
- 47.Weiss G, Goodnough LT. Anemia of chronic disease. N Engl J Med. 2005;352(10):1011–1023. doi: 10.1056/NEJMra041809. [DOI] [PubMed] [Google Scholar]
- 48.Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC. Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Arch Pathol Lab Med. 2009;133(4):628–632. doi: 10.5858/133.4.628. [DOI] [PubMed] [Google Scholar]
- 49.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105(9):1135–1143. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 50.King GL. The role of inflammatory cytokines in diabetes and its complications. J Periodontol. 2008;79(8 Suppl):1527–1534. doi: 10.1902/jop.2008.080246. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Additive interaction between RAR and diabetes for the risk of carotid plaques. Table S2. Relationship between the RAR and the risk of number of carotid plaque. Table S3. Relationship between the RAR and the risk of carotid plaque echo property.
Data Availability Statement
The datasets used and/or analyzed in the present study are available from the corresponding author on reasonable request.