Abstract
Aims
Excision of chronic osteomyelitic bone creates a dead space which must be managed to avoid early recurrence of infection. Systemic antibiotics cannot penetrate this space in high concentrations, so local treatment has become an attractive adjunct to surgery. The aim of this study was to present the mid- to long-term results of local treatment with gentamicin in a bioabsorbable ceramic carrier.
Methods
A prospective series of 100 patients with Cierny-Mader Types III and IV chronic ostemyelitis, affecting 105 bones, were treated with a single-stage procedure including debridement, deep tissue sampling, local and systemic antibiotics, stabilization, and immediate skin closure. Chronic osteomyelitis was confirmed using strict diagnostic criteria. The mean follow-up was 6.05 years (4.2 to 8.4).
Results
At final follow-up, six patients (six bones) had recurrent infection; thus 94% were infection-free. Three infections recurred in the first year, two in the second year, and one 4.5 years postoperatively. Recurrence was not significantly related to the physiological class of the patient (1/20 Class A (5%) vs 5/80 Class B (6.25%); p = 0.833), nor was it significantly related to the aetiology of the infection, the organisms which were cultured or the presence of nonunion before surgery (1/10 with nonunion (10%) vs 5/90 without nonunion (5.6%); p = 0.570). Organisms with intermediate or high-grade resistance to gentamicin were significantly more likely in polymicrobial infections (9/21; 42.8%) compared with monobacterial osteomyelitis (7/79 (8.9%); p < 0.001). However, recurrence was not significantly more frequent when a resistant organism was present (1/16 for resistant cases (6.25%) vs 5/84 in those with a microbiologically sensitive infection (5.95%); p = 0.958).
Conclusion
We found that a single-stage protocol, including the use of a high-delivery local antibiotic ceramic carrier, was effective over a period of several years. The method can be used in a wide range of patients, including those with significant comorbidities and an infected nonunion.
Cite this article: Bone Joint J 2022;104-B(9):1095–1100.
Keywords: Osteomyelitis, Fracture-related infection, Local antibiotics, Outcome, Infected nonunion, chronic osteomyelitis, gentamicin, infections, antibiotics, medical comorbidities, nonunions, organisms, recurrent infection, debridement
Introduction
Chronic osteomyelitis remains common, as a sequela of acute haematogenous infection of bone mainly in low- and middle-income countries, and after injury throughout the world. 1,2 Treatment has often been staged, with repeated debridement, delayed skin closure, and secondary reconstruction of bony defects. 1,3-5 The use of polymethyl-methacrylate (PMMA) antibiotic-loaded beads was pioneered more than 50 years ago, 6-8 and there is now increasing interest in local antibiotic treatment. 9-11 This has the potential to deliver very high concentrations of antibiotics, without adverse systemic effects. 12,13 It also removes concerns about compliance with treatment.
Calcium sulphate has been used as a carrier of antibiotics for many years. There is good evidence from animal and human studies that bacteria may be eradicated from bony defects in this way, 14,15 and that this is superior to the use of systemic antibiotics alone. 16 Human studies have been encouraging, 17,18 but calcium sulphate does not promote good bone formation. Postoperative fractures may occur and secondary surgery is still needed. 10,17-19
In order to address this shortcoming, a combination of calcium sulphate with hydroxyapatite (Cerament; Bonesupport AB, Lund, Sweden) was introduced, and this has been shown to form an osteoconductive scaffold, which allows an early biological response and may be osteoinductive and osteoconductive. 20,21 In 2013, this biphasic ceramic was licenced to deliver a high dose of gentamicin (17.5 mg per ml). Animal studies suggested that the rate of infection could be decreased using this carrier with the promotion of bone formation in bony defects following debridement. 22,23
We postulated that this material could facilitate a single-stage treatment algorithm for the management of chronic osteomyelitis in humans. We performed a prospective evaluation of 100 consecutively recruited patients, with established chronic osteomyelitis and published the results with a mean follow-up of 19.5 months (12 to 34) in 2016. 24 This short follow-up would clearly not identify later recurrences, which can often present after treatment of bony infections. We acknowledged this in the paper, and now present a further review of these patients reporting the effectiveness of our protocol when using Cerament G, at a follow-up of between four and eight years.
Methods
All patients presenting with Cierny-Mader (C-M) Type III (localized) or Type IV (diffuse anatomical type) chronic osteomyelitis, 25 between March 2013 and February 2015, were eligible for recruitment. Chronic osteomyelitis was defined as the presence of symptoms for a minimum of six months, with clinical and radiological features accompanied by at least one of the following: a sinus, abscess or intraoperative pus, supportive histology, or two or more microbiological cultures with indistinguishable organisms. 24,26 When cultures were negative, a patient was only included if there was positive histology and a draining sinus or intraoperative pus. Infected nonunions were included if the segmental bone loss was < 1 cm at the time of presentation.
The patients were classified by the C-M anatomical type and the physiological status of the host (Class A, healthy; Class BL, local compromise in the limb; Class BS, systemic compromise; Class BLS, local and systemic compromise). 25
All patients were treated with a single-stage procedure (Figures 1 to 3). 2 They were optimized preoperatively to reduce the effect of modifiable risk factors. Under tourniquet, a minimum of five deep samples were obtained for microbiology and two for histology, 27,28 before giving empirical intravenous antibiotics (Vancomycin and Meropenem). 26 Sinus tracts and implants were removed, dead bone was excised, and the resulting defect washed with 0.05% aqueous chlorhexidine. Stability was ensured, when required, using internal or external fixation. The defect was filled with Cerament G (Figure 2). No other materials or antibiotic agents were used in the bone. Skin closure was always performed at the same operation, either by direct closure or with the use of local or free microvascular transfer (Figure 3).
Fig. 1.

This Cierny-Mader Type 3 osteomyelitis developed after an intraosseus infusion following major trauma. The anterior cortex and medullary bone were necrotic with much overlying skin loss.
Fig. 3.

The soft-tissue defect was covered with a local gastrocnemius muscle flap and split skin graft from the thigh.
Fig. 2.

The dead tissue has been debrided and the large metaphyseal defect filled with gentamicin-loaded ceramic.
Appropriate oral or intravenous postoperative antibiotic treatment was given as soon as the culture results were obtained, and continued for between six and 12 weeks, as advised by the infectious disease team.
The primary outcome measure was the eradication of infection. Failure was defined as: recurrent infection with positive cultures from further radiologically guided aspiration or open biopsy; recurrent sinus formation; further surgery performed for infection; or any patient requiring antibiotic treatment for persistent symptoms. Patients were reviewed for the eradication of infection at three, six, 12, 24, and 48 months after surgery. Final follow-up was undertaken in 2021, by telephone review, for all contactable patients who had not been physically reviewed during the previous 48 months. Adverse events and complications were recorded at all timepoints. Secondary outcomes were death, the need for further surgery, pathological fracture at the site of surgery, and disturbed wound healing. The study had institutional ethical approval (Oxford University Hospitals 2022/7657) and patients gave informed consent.
Statistical analysis
Data were analyzed using SPSS v. 20 (IBM, USA). The data were regarded as non-parametric and groups were compared using the chi-squared test for low-frequency variables. A p-value < 0.05 was considered significant. A Kaplan-Meier survival analysis was used to record the timing of recurrent infection.
Results
A total of 106 eligible patients presented. Six were excluded as they did not meet the strict postoperative criteria, with infection not being confirmed microbiologically or histologically. Thus, a total of 100 consecutive patients with confirmed infection in 105 bones were included. The mean age was 51.6 years (23 to 88). Osteomyelitis followed open fracture or internal fixation of closed fractures in 71 patients (71%; 72 bones). There were 19 patients who had haematogenous osteomyelitis and ten with infection after orthopaedic surgery or invasion of bone from a local soft-tissue infection. Nine had septic arthritis, complicating periarticular osteomyelitis involving three ankles, three shoulders, two elbows, and one wrist. A total of 80 (80%) had significant local or systemic comorbidities (C-M Class B hosts). Ten had an infected nonunion with short segment bony defects (< 1 cm). Table I summarizes the demographic data.
Table I.
The demographic data of the patients by anatomical location, Cierny-Mader stage, soft-tissue cover, and requirement for stabilization.
| Bone | n | Cierny-Mader stage* | Soft-tissue cover | Fixation | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| III A | III BL | III BS | III BLS | IV A | IV BL | IV BS | IV BLS | Direct closure | Local flap | Free flap | None | External | Internal | ||
| Tibia | 38 | 7 | 14 | 4 | 9 | 1 | 1 | 1 | 1 | 21 | 4 | 13 | 32 | 6† | |
| Femur | 24 | 5 | 7 | 3 | 4 | 1 | 1 | 3 | 23 | 1 | 19 | 4 mono | 1 IMN | ||
| Humerus | 16 | 2 | 2 | 4 | 2 | 1 | 1 | 4 | 15 | 1 | 11 | 3 mono | 2 plates | ||
| Radius + ulna | 10 | 4 | 4 | 1 | 1 | 10 | 10 | ||||||||
| Calcaneum | 3 | 2 | 1 | 1 | 2 | 1 | 3 | ||||||||
| Clavicle | 2 | 2 | 2 | 2 | |||||||||||
| Fibula | 1 | 1 | 1 | 1 | |||||||||||
| Sacrum | 1 | 1 | 1 | 1 | |||||||||||
| Scapula + humerus | 1 | 1 | 1 | 1 Ilizarov | |||||||||||
| Femur + tibia | 1 | 1 | 1 | 1 Ilizarov | |||||||||||
| Tibia + talus | 3 | 1 | 1 | 1 | 1 | 2 | 2 Ilizarov | 1 IMN | |||||||
| Total | 100 | 18 | 25 | 19 | 16 | 2 | 4 | 5 | 11 | 77 | 5 | 18 | 79 | 17 | 4 |
A = Normal host; BL = Host with local compromise; BS = Host with systemic compromise; BLS = Host with local and systemic compromise.
Four monolateral and two Ilizarov fixators.
IMN, intramedullary nail; mono, monolateral external fixator.
Stabilization was required in 21 patients (25 bones), usually with external fixation, and five required arthrodesis as part of the initial surgery, due to destruction of the joint by infection. Plastic surgical skin closure was needed in 23 patients (23 bones; 18 free flaps and five local flaps). The mean volume of the defect was 10.9 ml (1 to 30).
Staphylococci were the commonest organisms (41.8%), with Methicillin-resistant Staphylococcus aureus in six patients. Proteus mirabilis and Pseudomonas spp. were more common in polymicrobial infection, often with a gram-positive organism (usually S. aureus).
All patients were reviewed at one year, except for one who died five months postoperatively. A total of 97 patients (102 bones) were reviewed at two years; one patient died and two were lost to follow-up; 92 (97 bones) at four years; three further patients died and two were lost to follow-up; and 91 (96 bones) were finally reviewed at a mean of 6.05 years (4.2 to 8.4); one further patient died. All five deaths were unrelated to the surgery or to the infection, and all of these patients were infection-free at time of death.
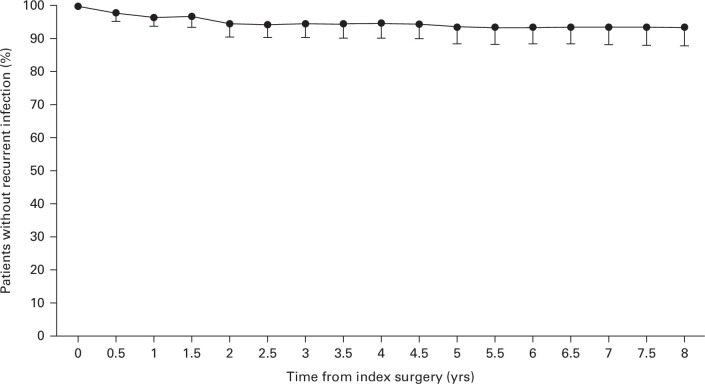
At one year after surgery 97 patients (97%; 101 bones) were infection-free. There were two recurrences by two years and one further recurrence at 4.5 years. A total of six patients (seven bones) had a recurrence, giving an overall success rate of 94% at a mean of six years’ follow-up. Analysis of the survival is shown in Figure 4.
Fig. 4.
Kaplan-Meier graph of survival until eight years after surgery.
Further analysis of the patients with a recurrence showed that failure to eradicate infection was not significantly related to the physiological class of the host (1/20 Class A (5%) vs 5/80 Class B (6.25%); p = 0.833), nor was it significantly related to the aetiology of the infection, microbiological culture, or the presence of an infected nonunion before surgery (1/10 with nonunion (10%) vs 5/90 without nonunion (5.6%); p = 0.570).
A total of 16 patients (18 bones) had organisms with intermediate or high-grade resistance to gentamicin. This was significantly more likely in polymicrobial infections (9/21; 42.8%) compared with monobacterial osteomyelitis (7/79 (8.9%); p < 0.001). However, recurrence was not significantly more frequent when a resistant organism was present (1/16 for resistant cases (6.25%) vs 5/84 for bacteriologically sensitive infections (5.95%); p = 0.958).
All six patients with recurrent infection had revision surgery. One with a recurrent hindfoot infection, culturing Acinetobacter, chose a below-knee amputation. The others had a further excision of the infection or drainage of a soft-tissue abscess. All were clinically infection-free, without subsequent medical or surgical treatment at final follow-up. The details of the patients with recurrent infection are shown in Table II.
Table II.
Details of the patients who had a recurrence of infection.
| Site | Aetiology | C-M stage | Initial surgery | Months to recurrence |
Initial microbiology | Recurrent microbiology | Revision treatment |
|---|---|---|---|---|---|---|---|
| Calcaneum | Heel shift osteotomy | III BL | Excision 6 ml CG Direct closure of previous ALT flap |
4.8 | MSSA | MSSA | Revision excision 8 ml CG Gracilis muscle flap |
| Distal radius | Fracture with ORIF | III A | Excision 4 ml CG |
5.2 | No growth | MSSA Serratia marcescens |
Drainage of abscess only |
| Tibial diaphysis | Gunshot wound to tibia | III BL | Excision 30 ml CG LD flap |
7.1 | MSSA | MSSA Streptococcus agalactiae |
Revision excision 20 ml CG |
| Femoral diaphysis | Open fracture with ORIF | III BL | Excision 20 ml CG external fixator |
18.8 | Resistant Pseudomonas spp | Resistant Pseudomonas spp | Revision excision+ Amikacin in CaSO4 |
| Femoral diaphysis | Open fracture with ORIF | III BL | Excision 10 ml CG direct closure | 23.8 | MSSA | MSSA | Revision with 20 ml CG |
| Tibia + talus | Charcot ankle with failed fusion | IV BLS | Excision, 20 ml CG+ IMN | 53.1 | Acinetobacter | Acinetobacter | Amputation |
ALT, anterolateral thigh flap; CG, Cerament with gentamicin; C-M, Cierny-Mader; IMN, intramedullary nail; LD, latissimus dorsi free flap; MSSA, methicillin-sensitive Staphylococcus aureus; ORIF, open reduction and internal fixation.
All five arthrodeses healed and eight of ten nonunions healed after the initial surgery. Of the two patients with a nonunion, one humeral nonunion healed after revision of the fixation, with no sign of active infection and negative cultures. The second had an asymptomatic stiff tibial nonunion and has declined further treatment.
Four patients underwent arthroplasty for degenerative arthritis in the same limb as the infection, between two and six years after the initial single-stage surgery for osteomyelitis. None of these suffered a recurrence of osteomyelitis or periprosthetic joint infection at a mean of 18.6 months (11 to 49) after the arthroplasty.
Adverse events were uncommon, with three fractures occurring between one and 11 months after surgery. Two of these occurred after significant new trauma and healed well with splintage alone. The third was a frail patient with multiple comorbidities who had a low-energy fracture through the defect in the radius. She declined fixation and the fracture remains ununited, but the symptoms are well controlled by a splint. There were no subsequent fractures, beyond the first year after surgery.
Six patients (6%; six bones) had early leakage of ceramic material from the wound, which was treated expectantly and dried up without intervention or later recurrence of infection.
Discussion
This study presents a prospective, consecutive series of patients with the more severe stages of osteomyelitis. Recent studies have frequently reported higher rates of recurrence in these patients, 5,29,30 ranging from 10% to 45% in much shorter periods of follow-up. As our patients now present with more complex infections and comorbidities, we need forms of treatment which can be applied widely. With traditional forms of treatment, patients with comorbidities and polymicrobial infections have had worse outcomes. 31,32 This may be related to difficulties with antibiotic intolerance, interactions with other medications, poor compliance, and adverse reactions due to the toxicity of systemic treatment. These are all common in older or more comorbid patients.
The use of local antibiotics offers the possibility of removing concerns about compliance and may allow less dependence on systemic treatment, 33 which is often associated with toxicity. 34 Even very high doses of systemically toxic drugs, such as gentamicin, can be safely administered locally in bone. The use of up to 525 mg of gentamicin in Cerament has been shown to have no clinically significant effect on renal function, 13 as systemic levels eluted from this carrier are very low. 12
Our protocol, facilitated by the absorbable local antibiotic, was highly effective, with few recurrences. Our initial results, presented in 2016, 24 revealed that four patients (five bones) had recurrent infection at a mean of 1.5 years postoperatively. The longer follow-up period confirms that the treatment remains effective over several years, with only two further patients with a recurrent infection (a total of six patients with recurrence in seven bones) up to eight years postoperatively. Despite the continuing follow-up of 91 of the 95 surviving patients, we did not discover any other recurrence or need for further treatment. This is important because this unselected, consecutive cohort included many patients with medical comorbidities (80% C-M Grade B hosts), polymicrobial infection (21%), and diffuse involvement (22% C-M Type IV). However, we know that chronic osteomyelitis may recur several decades after the initial treatment, so these figures will almost certainly overestimate the final success rate.
We found that the presence of gentamicin-resistant bacteria did not significantly correlate with failure. Resistance is reported in laboratory testing based on the levels of antibiotic which can be expected when the drug is given systemically (European Committee on Antimicrobial Susceptibility Testing breakpoints). 35 The local application of gentamicin using Cerament achieves levels of antibiotic which are much greater than serum levels and well above the minimum inhibitory concentration (MIC) and minimum biofilm eradication concentration for many organisms. It has been shown that only bacteria with very high MICs (> 1,024 mg/l) can survive these local levels of antibiotics. 36 No cultures identified new resistance to gentamicin in patients with recurrent infection.
In the past, we and others have reported a higher incidence of fracture through osteomyelitic defects after surgery, 17,18 and many patients have required secondary bone grafting to prevent fracture. In this series, no patient had a bone graft and only three suffered a fracture. Cerament G is injected as a thick liquid and can coat the surface of the bone. It hardens to a material with similar compressive strength to cancellous bone. 20 Remodelling occurs over a period of at least two years, with the initial formation of woven bone which is slowly remodelled to lamellar bone. This occurs without a cartilage phase and represents direct bone formation on the biomaterial. 23,37 All three of our fractures occurred within 11 months of surgery, supporting the view that continued new bone formation in the defect, over many months, may protect from subsequent fracture.
The ability to fill the dead space completely with a material which will deliver antibiotics over several weeks, and then be remodelled, allows a single operation, which is more patient-friendly. With no further hospital admissions, it may also offer cost savings when compared with routine staged treatment.
In conclusion, we have applied this protocol to all patients, regardless of comorbidities, requirement for flaps, or nature of infection. Single-stage management, facilitated by the bioabsorbable antibiotic carrier, was robust, giving effective treatment in all these groups in the mid to long term.
Take home message
- Single-stage surgery, facilitated by a bioabsorbable local antibiotic, was highly effective in the treatment of chronic osteomyelitis over a prolonged period.
- Adverse events were infrequent and easily managed.
- The protocol, delivered by a multidisciplinary team, was more patient-friendly than previous treatments.
Author contributions
M. A. McNally: Methodology, Investigation, Formal analysis, Writing – original draft.
J. Ferguson: Investigation, Formal analysis, Writing – original draft.
D. Stubbs: Investigation, Writing – review & editing.
M. Scarborough: Writing – review & editing.
A. Ramsden: Investigation, Writing – review & editing.
B. Atkins: Methodology, Formal analysis, Writing – review & editing.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement
A. Ramsden reports speaker payments from Cerament/Bonesupport, unrelated to this study. J. Ferguson reports consulting fees from DePuy Synthes and payment for educational symposia from Bonesupport AB, unrelated to this study. M. A. McNally reports meeting expenses from Bonesupport AB for this study, and consulting fees from Bonesupport AB, royalties from Oxford University Press, and expenses from the European Bone & Joint Infection Society, all of which are unrelated to this study.
Acknowledgements
We would like to thank the staff of the Oxford Bone Infection Unit for their commitment to the care of the patients in this study and to all our infection patients.
Open access funding
The open access fee for this study was funded by Oxford Bone Infection Consultancy Ltd.
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
This article was primary edited by J. Scott.
Contributor Information
Martin A. McNally, Email: martin.mcnally@ouh.nhs.uk.
Jamie Y. Ferguson, Email: jamie.ferguson@ouh.nhs.uk, jamieferguson@doctors.org.uk.
Matthew Scarborough, Email: Matthew.Scarborough@ouh.nhs.uk.
Alex Ramsden, Email: Alex.ramsden@ouh.nhs.uk.
David A. Stubbs, Email: david.stubbs@ouh.nhs.uk.
Bridget L. Atkins, Email: bridget.atkins@ouh.nhs.uk.
References
- 1. Cierny G. Chronic osteomyelitis: results of treatment. Instr Course Lect. 1990;39:495–508. [PubMed] [Google Scholar]
- 2. McNally MA. Osteomyelitis. In Chen A. ed. Management of Orthopaedic Infections: A Practical Guide. New York, New York, USA: Thieme, 2021: 61–87. [Google Scholar]
- 3. McNally MA, Small JO, Tofighi HG, Mollan RA. Two-stage management of chronic osteomyelitis of the long bones. The Belfast technique. J Bone Joint Surg Br. 1993;75-B(3):375–380. [DOI] [PubMed] [Google Scholar]
- 4. Cierny G, DiPasquale D. Treatment of chronic infection. J Am Acad Orthop Surg. 2006;14(10 Spec No):S105-10. [DOI] [PubMed] [Google Scholar]
- 5. Lazzarini L, Mader JT, Calhoun JH. Osteomyelitis in long bones. J Bone Joint Surg Am. 2004;86-A(10):2305–2318. [DOI] [PubMed] [Google Scholar]
- 6. Klemm K. The treatment of chronic bone infections with gentamicin-PMMA-chains and beads. Unfallchirurgie. 1977;3(1):20–25. [Google Scholar]
- 7. Walenkamp GH, Kleijn LL, de Leeuw M. Osteomyelitis treated with gentamicin-PMMA beads: 100 patients followed for 1-12 years. Acta Orthop Scand. 1998;69(5):518–522. [DOI] [PubMed] [Google Scholar]
- 8. Wahlig H, Dingeldein E. Antibiotics and bone cements. Experimental and clinical long-term observations. Acta Orthop Scand. 2009;51(1–6):49–56. [DOI] [PubMed] [Google Scholar]
- 9. McLaren AC. Alternative materials to acrylic bone cement for delivery of depot antibiotics in orthopaedic infections. Clin Orthop Relat Res. 2004;427:101–106. [DOI] [PubMed] [Google Scholar]
- 10. Ferguson J, Diefenbeck M, McNally M. Ceramic biocomposites as biodegradable antibiotic carriers in the treatment of bone infections. J Bone Jt Infect. 2017;2(1):38–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ruppen C, Hemphill A, Sendi P. In vitro activity of gentamicin as an adjunct to penicillin against biofilm group B Streptococcus. J Antimicrob Chemother. 2017;72(2):444–447. [DOI] [PubMed] [Google Scholar]
- 12. Stravinskas M, Horstmann P, Ferguson J, et al. Pharmacokinetics of gentamicin eluted from a regenerating bone graft substitute: In vitro and clinical release studies. Bone Joint Res. 2016;5(9):427–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Muir R, Birnie C, Hyder-Wilson R, Ferguson J, McNally MA. Does local implantation of gentamicin impair renal function in patients undergoing surgery for chronic bone infection? Int J Res Orthop. 2021;7(3):438. [Google Scholar]
- 14. Xie Z, Liu X, Jia W, Zhang C, Huang W, Wang J. Treatment of osteomyelitis and repair of bone defect by degradable bioactive borate glass releasing vancomycin. J Control Release. 2009;139(2):118–126. [DOI] [PubMed] [Google Scholar]
- 15. Branstetter JG, Jackson SR, Haggard WO, Richelsoph KC, Wenke JC. Locally-administered antibiotics in wounds in a limb. J Bone Joint Surg Br. 2009;91-B(8):1106–1109. [DOI] [PubMed] [Google Scholar]
- 16. Rand BCC, Penn-Barwell JG, Wenke JC. Combined local and systemic antibiotic delivery improves eradication of wound contamination: An animal experimental model of contaminated fracture. Bone Joint J. 2015;97-B(10):1423–1427. [DOI] [PubMed] [Google Scholar]
- 17. McKee MD, Li-Bland EA, Wild LM, Schemitsch EH. A prospective, randomized clinical trial comparing an antibiotic-impregnated bioabsorbable bone substitute with standard antibiotic-impregnated cement beads in the treatment of chronic osteomyelitis and infected nonunion. J Orthop Trauma. 2010;24(8):483–490. [DOI] [PubMed] [Google Scholar]
- 18. Ferguson JY, Dudareva M, Riley ND, Stubbs D, Atkins BL, McNally MA. The use of a biodegradable antibiotic-loaded calcium sulphate carrier containing tobramycin for the treatment of chronic osteomyelitis: a series of 195 cases. Bone Joint J. 2014;96-B(6):829–836. [DOI] [PubMed] [Google Scholar]
- 19. Gitelis S, Brebach GT. The treatment of chronic osteomyelitis with a biodegradable antibiotic-impregnated implant. J Orthop Surg (Hong Kong). 2002;10(1):53–60. [DOI] [PubMed] [Google Scholar]
- 20. Nilsson M, Wang JS, Wielanek L, Tanner KE, Lidgren L. Biodegradation and biocompatability of a calcium sulphate-hydroxyapatite bone substitute. J Bone Joint Surg Br. 2004;86-B(1):120–125. [PubMed] [Google Scholar]
- 21. Raina D, Gupta A, Petersen M, et al. A biphasic bone substitute with gentamicin regenerates bone in osteomyelitis with muscle acting as an osteoinductive niche. Orthopaedic Proceedings. 2015;97(SUPP 16):24. [Google Scholar]
- 22. Dvorzhinskiy A, Perino G, Chojnowski R, van der Meulen MCH, Bostrom MPG, Yang X. Ceramic composite with gentamicin decreases persistent infection and increases bone formation in a rat model of debrided osteomyelitis. J Bone Jt Infect. 2021;6(7):283–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hettwer W, Horstmann PF, Bischoff S, et al. Establishment and effects of allograft and synthetic bone graft substitute treatment of a critical size metaphyseal bone defect model in the sheep femur. APMIS. 2019;127(2):53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McNally MA, Ferguson JY, Lau ACK, et al. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite: a prospective series of 100 cases. Bone Joint J. 2016;98-B(9):1289–1296. [DOI] [PubMed] [Google Scholar]
- 25. Cierny G, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res. 2003;414(414):7–24. [DOI] [PubMed] [Google Scholar]
- 26. Dudareva M, Hotchen AJ, Ferguson J, et al. The microbiology of chronic osteomyelitis: Changes over ten years. J Infect. 2019;79(3):189–198. [DOI] [PubMed] [Google Scholar]
- 27. Morgenstern M, Athanasou NA, Ferguson JY, Metsemakers W-J, Atkins BL, McNally MA. The value of quantitative histology in the diagnosis of fracture-related infection. Bone Joint J. 2018;100-B(7):966–972. [DOI] [PubMed] [Google Scholar]
- 28. Dudareva M, Barrett LK, Morgenstern M, Atkins BL, Brent AJ, McNally MA. Providing an evidence base for tissue sampling and culture interpretation in suspected fracture-related infection. J Bone Joint Surg Am. 2021;103-A(11):977–983. [DOI] [PubMed] [Google Scholar]
- 29. Cho SH, Song HR, Koo KH, Jeong ST, Park YJ. Antibiotic-impregnated cement beads in the treatment of chronic osteomyelitis. Bull Hosp Jt Dis. 1997;56(3):140–144. [PubMed] [Google Scholar]
- 30. Steinhausen E, Lefering R, Glombitza M, et al. Bioactive glass S53P4 vs. autologous bone graft for filling defects in patients with chronic osteomyelitis and infected non-unions - a single center experience. J Bone Jt Infect. 2021;6(4):73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zimmerli W, Sendi P. Pathogenesis of implant-associated infection: the role of the host. Semin Immunopathol. 2011;33(3):295–306. [DOI] [PubMed] [Google Scholar]
- 32. Lew DP, Waldvogel FA. Osteomyelitis. Lancet. 2004;364(9431):369–379. [DOI] [PubMed] [Google Scholar]
- 33. Dudareva M, Kümin M, Vach W, et al. Short or Long Antibiotic Regimes in Orthopaedics (SOLARIO): a randomised controlled open-label non-inferiority trial of duration of systemic antibiotics in adults with orthopaedic infection treated operatively with local antibiotic therapy. Trials. 2019;20(1):693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li H-K, Rombach I, Zambellas R, et al. Oral versus intravenous antibiotics for bone and joint infection. N Engl J Med. 2019;380(5):425–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. No authors listed . Clinical breakpoints - breakpoints and guidance. EUCAST. http://www.eucast.org/clinical_breakpoints/(date last accessed 12 July 2022).
- 36. Bezstarosti H, Croughs PD, van den Hurk MKB, et al. Antimicrobial effect of Cerament-G on bacterial isolates, with various levels of gentamicin resistance, found in fracture-related infection; an in vitro study. eCM online. https://www.ecmconferences.org/abstracts/2019/Collection5/posters.pdf(date last accessed 12 July 2022).
- 37. Ferguson J, Athanasou N, Diefenbeck M, McNally MA. Radiographic and histological analysis of a synthetic bone graft substitute eluting gentamicin in the treatment of chronic osteomyelitis. J Bone Jt Infect. 2019;4(2):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]