Highlights
-
•
Cigarette smokers endorse reduced motivation to smoke for indulgence as body mass index (BMI) increases.
-
•
Lean smokers show heavier daily smoking and dependence when Addictive, Sedative, Stimulation, and indulgence motives are high.
-
•
Among smokers with obesity, smoking behavior was not associated with any measured smoking motivations.
Abstract
Objective
Cigarette smoking and obesity are the leading causes of premature morbidity and mortality and increase the risk of all-cause mortality four-fold when comorbid. Although research suggests that smoking motives may differ based on body mass index (BMI), it is unclear how these differences translate to smoking behavior.
Method
Three groups of adults who smoke cigarettes (N = 79; obese n = 25, overweight n = 30, and lean n = 24) completed measures of smoking and the Smoking Motivations Questionnaire. Groups did not differ on age, education, cigarettes per day (CPD), pack-years, or nicotine dependence, as measured by the Fagerström Test for Cigarette Dependence (FTCD).
Results
Analyses revealed different associations between reasons for smoking and smoking behavior depending on lean, overweight, or obesity status. Participants (N = 37 female, average age 39.8 years) self-reported smoking was positively associated with Addictive, and Automatic subscale scores among lean participants, with only the Addictive subscale score among those with overweight, and only the Automatic subscale score among those with obesity. Post hoc MANCOVA analysis revealed a significant interaction effect of Group x Automatic Smoking on Pack-years (F(2, 79)=3.34, p = 0.04).
Conclusion
Findings suggest smoking motives are differentially associated with smoking behavior in adults who smoke depending on weight status. The daily smoking rate of participants with obesity may be less related to the addictive quality of smoking, and automaticity may be less associated with smoking history in those with overweight. Additional research on the influence of BMI on cigarette smoking is necessary to fully elucidate how obesity may impact treatment outcomes to optimize smoking cessation treatment among those with excess body weight.
1. Introduction
Cigarette smoking and obesity are leading causes of premature morbidity and mortality (Goodchild et al., 2018; Seidell and Halberstadt, 2015). Individuals with obesity who smoke incur four times the risk of all-cause mortality than lean individuals who have never smoked (Freedman et al., 2006). Up to 40% of people with obesity in the United States smoke cigarettes (Hales et al., 2018), versus less than 15% of the general population (Creamer, 2019). Adults with obesity who smoke also smoke more heavily and for more years (Dare et al., 2015). Individuals at higher body weights comprise 70% of those seeking treatment for smoking (LaRowe et al., 2009). They gain the most weight after quitting, are the least accepting of that weight gain (Bush et al., 2008; M. D. Levine et al., 2013), and are more likely to relapse as a result (Audrain‐McGovern and Benowitz, 2011). Despite public health significance, little research has focused on understanding what motivates smoking among individuals with excess body weight.
Self-report questionnaires measuring smoking motives, such as automaticity (e.g., habit), addictive properties of smoking (e.g., strength of cravings), psychosocial motivations (e.g., smoking for confidence or social acceptance), indulgence, sedative properties (e.g., removing stress or negative affect), or sensorimotor aspects of smoking, can offer insight into why individuals continue to smoke despite known adverse consequences, and subsequently, help improve treatment outcomes among those with excess body weight. Heavier smoking (e.g., greater than 15 cigarettes per day (CPD)) and greater nicotine dependence have been linked to all of these motivations (Berg et al., 2011; Bommelé et al., 2014; Oksuz et al., 2007; Russell et al., 1974; Shiffman et al., 2012). More cigarettes smoked in one's lifetime, as measured by pack-years, is related to smoking for addictive aspects of smoking, automaticity (Rocha et al., 2019) and psychosocial motives (Bommelé et al., 2014; Rocha et al., 2019). Individuals who have smoked more cigarettes over time (i.e., those with more pack-years) report smoking for the sedative effects (Bommelé et al., 2014; Rocha et al., 2019); however, lighter smoking is linked to automatic, addictive, and sensorimotor reasons for smoking (Shiffman et al., 2012). Nondependent adults who smoke endorse smoking for relaxing or emotional effects (Carim-Todd et al., 2016) and social pressure (Berg et al., 2011; Oksuz et al., 2007; Shiffman et al., 2012).
Smoking motivations have received little attention among individuals who smoke and have a body mass index (BMI) consistent with overweight or obesity. One study (Hovland and Ceballos, 2007) examined reasons for smoking among participants who were motivated to quit smoking, comparing lean adults who smoke with those who had a BMI above 25.0 kg/m2, including participants in both the overweight and obese weight ranges. The authors used the Reasons for Smoking Questionnaire, an 18-item survey assessing the strength of six smoking motives: stimulation, pleasure, handling, tension reduction, craving, and habit. Their findings suggest that lean participants endorsed handling (sensorimotor) and tension reduction (sedative) motivations at higher rates than those with overweight; however, these differences were no longer significant when age was included as a covariate. Overweight in smoking was associated with greater stimulation motives than a BMI under 25 kg/m2 (Hovland and Ceballos, 2007). Whether these differences in smoking motivations translate to differences in smoking behavior is unknown. This exploratory analysis would be the first investigation of the relationship between BMI, smoking motivations, and smoking behavior (CPD, pack-years, and nicotine dependence). We aimed to explore 1) the relationship between smoking behavior and smoking motives, 2) the relationship between BMI and smoking motives, and 3) if the relationship between smoking motives and behavior differ as a function of BMI.
2. Method
2.1. Participants
A total of 216 participants were recruited via advertisements, online listservs, and word of mouth and enrolled in two brain imaging/treatment studies (Franklin et al., 2009, 2011), of which 149 completed the Smoking Motives Questionnaire as a part of the eligibility protocol, and 114 completed the physical screening during which BMI was assessed. Of those, 82 participants completed all demographic and self-report measures for the current analyses. Scores for variables > 3 standard deviations (SD) from the mean for each group were excluded. Three participants met criteria for exclusion, leaving a final sample of 79 (37 female). Eligible and interested participants consented and completed medical and psychiatric evaluations. All participants were over age 18, met criteria for DSM-IV tobacco use disorder (TUD) and smoked at least six cigarettes/day for six months before the study started. Exclusion criteria included current unmanaged psychiatric diagnosis, substance use disorder other than TUD, pregnancy, or contraindications to magnetic resonance imaging which occurred as a part of a larger study. Uncontrolled medical diagnoses (e.g., uncontrolled diabetes) and the use of psychoactive medication were also exclusionary.
The two studies, investigating baclofen and varenicline as smoking cessation aids and examining their effect on brain function, had identical criteria for participation and baseline visit procedures. The studies were conducted concurrently. Demographics and variables of interest did not differ between studies. Data used in the current analyses were acquired before medication assignment. Because these data were derived from smoking cessation studies, non-smoking participants were excluded, and information regarding weight history and eating behavior was not assessed. Participants were categorized into three groups for analysis depending on their BMI: lean participants (n = 25, 13 female) defined as those with a BMI less than 25.0 kg/m2, participants with overweight (n = 30, 9 female) with a BMI of 25.01 – 29.99 kg/m2, and participants with obesity (n = 24, 15 female) with BMIs of 30 kg/m2 or greater. The study was approved by the University of Pennsylvania Institutional Review Board and adhered to the Declaration of Helsinki.
2.2. Measures
2.2.3. Demographics
Demographic characteristics were obtained using a comprehensive background questionnaire.
2.2.4. Mini-International Neuropsychiatric interview (MINI)
(Sheehan et al., 1998). The MINI is a structured diagnostic measure administered to determine a diagnosis of other substance dependence or severe psychiatric symptoms.
2.2.5. Smoking History questionnaire (SHQ)
The severity and duration of nicotine dependence were determined from a laboratory-developed questionnaire that included the Fagerström Test for Cigarette Dependence (FTCD; (Fagerström, 2012; Heatherton et al., 1991)). Number of cigarettes smoked per day (CPD) and pack-years were also assessed. Pack-years, a quantification of cigarette smoking across the number of years a person has smoked, describes the approximate number of cigarettes a person has smoked over time, where one pack-year equals 20 manufactured cigarettes smoked per day for one year.
2.2.6. Smoking motivations questionnaire (SMQ)
(Russell et al., 1974; Tate et al., 1994). Participants’ motives for smoking were assessed using the SMQ, a 34-item measure divided into subscales ranging from three to six items, measuring Automatic (e.g. “I find myself smoking without remembering lighting up”), Sedative (e.g. “I light up a cigarette when I feel angry about something”), Addictive (e.g. “When I have run out of cigarettes I find it almost unbearable until I can get them”), Stimulation (e.g. “Smoking helps to keep me going when I'm tired”), Psychosocial (e.g. “It is easier to talk and get on with other people when smoking”), Indulgent (e.g. “I usually only smoke when I can really sit back and enjoy it”), and Sensorimotor (e.g. “Handling a cigarette is part of the enjoyment of smoking it”) reasons for smoking. A 4-point Likert scale, ranging from 0 (“not at all”) to 3 (“very much so”) is used with higher scores indicating greater motivation to smoke for these reasons. Subscale scores range from 0 to 9 for Automatic and Sedative motives, 0 to 12 for Addictive and Indulgent motives, 0 to 15 for Sensorimotor motives, and 0 to 18 for the Stimulation and Psychosocial motives subscales.
2.3. Statistical analyses
Analyses were conducted in SPSS version 28. Analyses of variance (ANOVAs) compared BMI groups on demographic and smoking data. Post hoc analyses and correction for multiple comparisons were conducted using Tukey's HSD test. Partial Pearson correlations determined relationships between variables, controlling for age and sex. Following correlational analysis, a 3-group multivariate analyses of covariance (MANCOVAs) compared groups on smoking characteristics (CPD; pack-years; and nicotine dependence) as a function of SMQ subscale scores, controlling for age and sex. Although age and sex did not differ based on weight status, there were correlations between both and other variables of interest (Supplemental Material).
3. Results
3.1. Demographic and descriptive data
Participants ranged in age from 19 to 59 years (M = 38.8, SD=11.8) and had an average of 14 years of education (SD=2.27). Groups did not differ on age, education, CPD, pack-years, or FTCD (Table 1). BMI was significantly different across groups, as expected (p<0.001). The sample identified as 21.1% White, 31.7% African American, 0.6% Asian, and 3.7% Multiracial. Of the full sample, 6.5% of participants identified as of Hispanic ethnicity and 93.5% as Non-Hispanic. Weight groups did not significantly differ in racial or ethnic background.
Table 1.
Descriptive characteristics.
| Total |
Lean |
Overweight |
Obese |
F | Sig. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | M | SD | M | SD | M | SD | M | SD | ||||
| BMI | 111 | 27.8 | 5.6 | 22.0 | 2.2 | 27.5 | 1.2 | 34.3 | 4.0 | 187.59 | <0.001 | |
| Education | 97 | 14.0 | 2.3 | 13.7 | 2.0 | 14.0 | 2.3 | 14.3 | 2.6 | 0.53 | 0.59 | |
| Age | 111 | 39.8 | 11.8 | 38.0 | 12.0 | 41.4 | 12.1 | 39.6 | 11.1 | 0.82 | 0.45 | |
| CPD | 111 | 13.9 | 6.0 | 13.8 | 5.3 | 14.1 | 6.0 | 13.8 | 6.7 | 0.03 | 0.97 | |
| PackYears | 97 | 14.8 | 12.0 | 14.0 | 11.0 | 15.7 | 11.6 | 14.3 | 13.6 | 0.21 | 0.81 | |
| FTCD | 99 | 30.5 | 31.8 | 32.2 | 33.2 | 36.9 | 31.6 | 21.2 | 29.4 | 2.15 | 0.12 | |
| Automatic | 145 | 2.7 | 2.1 | 2.6 | 2.3 | 2.6 | 2.1 | 2.8 | 2.1 | 0.13 | 0.88 | |
| Sedative | 145 | 5.9 | 2.0 | 6.0 | 2.0 | 5.9 | 2.0 | 5.9 | 2.0 | 0.04 | 0.96 | |
| Addictive | 145 | 6.8 | 2.5 | 6.7 | 2.3 | 7.0 | 2.6 | 6.6 | 2.6 | 0.30 | 0.75 | |
| Smoking Motives | Stimulative | 145 | 8.7 | 3.5 | 9.5 | 3.7 | 8.7 | 3.5 | 7.8 | 3.4 | 1.70 | 0.19 |
| Psychosocial | 145 | 4.2 | 3.4 | 4.6 | 3.5 | 4.4 | 3.6 | 3.4 | 2.8 | 1.14 | 0.32 | |
| Indulgent | 145 | 6.6 | 2.5 | 6.6 | 2.9 | 6.8 | 2.3 | 5.9 | 2.5 | 1.64 | 0.20 | |
| Sensorimotor | 145 | 5.1 | 3.3 | 5.5 | 3.0 | 5.3 | 3.3 | 4.3 | 3.7 | 1.10 | 0.33 | |
|
All measures completed |
79 |
N = 25 (13 female) |
N = 30 (9 female) |
N = 24 (15 female) |
||||||||
3.2. Relationship between smoking characteristics and smoking motives
Controlling for age and sex, cigarette dependence was not correlated with any motives for smoking. CPD was positively associated with Automatic (r = 0.28, p = 0.013) and Addictive (r = 0.33, p = 0.003) subscales. Pack-years was significantly positively correlated with Automatic subscale scores r = 0.24, p = 0.034, such that heavier daily smoking and more cigarette smoking over time were associated with greater endorsement of smoking for Automatic motivations, and greater daily smoking was also linked to more Addictive motivation to smoke.
3.3. Relationship between smoking characteristics and BMI
Controlling for age and sex, there were negative relationships between BMI and Stimulation (r = −0.24, p = 0.04) and Indulgent (r = −0.23, p = 0.048) subscales such that higher BMI was associated with lower smoking for these reasons. Groups did not differ on smoking motivations overall (Pillai's Trace = 0.74, p = 0.73) or smoking characteristics (Pillai's Trace = 0.055, p = 0.57).
3.4. Relationship between smoking characteristics and smoking motives as a function of BMI
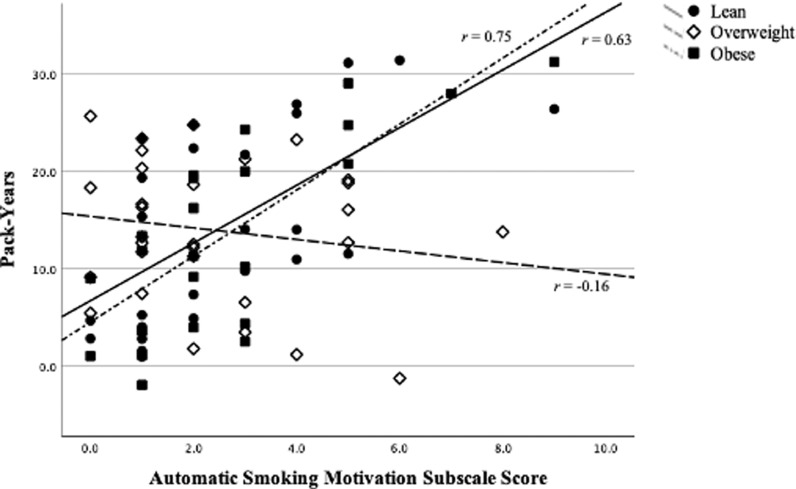
Within-group correlations revealed differing patterns of results (Supplemental Material Table 1). Among Lean participants, Automatic motives positively correlated with pack-years (r = 0.41, p = 0.05). Addictive smoking positively correlated with CPD (r = 0.64, p = 0.001) in the Lean group. Addictive smoking motives (r = 0.44, p = 0.02) were significantly associated with CPD among overweight participants, but no smoking motives were correlated with pack-years or dependence. Among participants with obesity, Automatic smoking motives were significantly correlated with pack-years (r = 0.47, p = 0.03). No other smoking motives were associated with smoking characteristics in any group. In other words, past heavier smoking was linked to automaticity in lean participants and those with obesity, but not overweight. Current heavier smoking was linked to the level of addictive motivation in lean participants and those with overweight, but not obesity (Fig. 1).
Fig. 1.
Within-group partial correlations demonstrating associations between Addictive Smoking Motivation subscale scores and cigarettes per day (CPD) controlling for age and sex. Among Lean participants and those with overweight, greater endorsement of Addictive Motivation was significantly positively correlated with heavier daily smoking. There was no correlation with CPD among participants with obesity.
Post hoc MANCOVAs (Supplemental Material Table 2) compared groups on smoking characteristics as a function of smoking motivations, controlling for age and sex. Obesity group interacted only with Automatic smoking in relation to smoking characteristics (Pillai's trace = 0.22, p = 0.009, η2 = 0.11). An interaction effect of Group x Automatic Smoking (Fig. 2) was revealed for pack-years (F(2, 79) = 3.34, p = 0.041, η2 = 0.09). Automatic smoking motives were significantly related to cigarette smoking exposure, and this relationship depended on a participant's weight status. A significant main effect of Automatic smoking was shown for pack-years (F(1, 79)=5.5, p = 0.02, η2 = 0.07) and CPD (F(1, 79) = 6.01, p = 0.017, η2 = 0.08), but not for dependence. Independent of weight status, age, and sex, Automatic smoking motives were significantly related to past and current smoking behavior. There were no main effects of group.
Fig. 2.
MANCOVAs comparing groups on smoking characteristics as a function of reasons for smoking showed interactive relationships only with Addictive Smoking. The interaction of BMI group and Automatic Smoking subscale scores was significantly associated with number of pack-years, with those in lean and overweight groups reporting greater pack-years with higher automatic motivation when controlling for age and sex, while there was no such relationship shown in the group with overweight.
There was a significant main effect of Addictive smoking on smoking characteristics (Pillai's trace = 0.14, p = 0.016, η2 = 0.14), specifically for CPD (F(1, 79)=10.76, p = 0.002, η2 = 0.13), suggesting Addictive smoking motives are related to daily smoking rate regardless of weight status or covariates. No other model demonstrated an interaction effect between group and motivation on smoking characteristics.
4. Discussion
These preliminary findings offer the first evidence that smoking motives may be differentially related to smoking behavior depending on BMI. The relationships between smoking motives and self-reported smoking behavior differed by BMI group. More cigarette smoking over time among lean participants and those with obesity was linked to greater endorsement of automatic smoking, but not among participants with overweight. Alternatively, the higher the daily smoking rate among lean and overweight groups, the more they endorsed smoking for addictive motivations, but this was not seen in those with obesity. In other words, adults seeking treatment for smoking endorsed similar automatic or addictive motivation to smoke regardless of weight status; however, these motives were not uniformly related to self-reported smoking behavior.
Given that pack-years is a retrospective variable and CPD measures current smoking, we can make some cautious inferences about directionality in hopes that future studies will explore these associations longitudinally. Through classical conditioning, internal (e.g., craving) and external (e.g., advertisements) cues that predict smoking or eating acquire reward properties over time, while receipt of the reward becomes comparatively less evocative (Day et al., 2007; Schultz, 1998). This phenomenon, known as incentive sensitization (Robinson and Berridge, 2008), is hypothesized to drive craving, motivating continued drug use and/or relapse. Neuroadaptations in corticolimbic circuitry may perpetuate craving and compulsive reward-seeking behavior, subsequently overriding homeostatic processes and cognitive control (Baler and Volkow, 2006; Volkow et al., 2017). A history of heavier smoking would thus lead to more automatic smoking (e.g., smoking as a conditioned response rather than an intentional, voluntary act), as our results show in lean participants and those with obesity. In turn, greater addictive smoking would be related to heavier current smoking, as our results show in participants with overweight. It is less clear, however, why these relationships would differ depending on overweight. There is some evidence that reward sensitivity or salience-related brain function may be elevated with overweight compared to lean individuals or those with obesity (Davis et al., 2004; Doornweerd et al., 2017; Ely et al., 2021), which might, in turn, influence the acquisition and maintenance of conditioned responses to smoking cues and smoking-related behaviors.
Elevated motivation to smoke to relieve cravings would also be hypothesized to drive heavier current smoking, as we show in lean participants and those with overweight. Our findings show current smoking behavior in those with obesity does not appear to be driven by addictive motives as in the other groups. A prior study has shown that adults with obesity smoke nicotine and denicotinized cigarettes at an equal rate, suggesting current smoking in this population may be less driven by the pharmacological reward from nicotine (Blendy et al., 2005). This suggests that motivation not assessed by the SMQ may underlie smoking rate or dependence in this population. Notably, the SMQ does not assess weight management as a reason for smoking, nor weight concerns, which research has highlighted as an important obstacle to smoking cessation. Weight loss or avoidance of weight gain motives have been shown to contribute to smoking uptake and resisting quitting (Taylor et al., 2019; Watanabe et al., 2016). Individuals with overweight or obesity who smoke describe elevated concern about weight gain following smoking cessation (Bush et al., 2008; M. D. Levine et al., 2013), which is a barrier to quitting smoking (Tuovinen et al., 2018). Furthermore, overweight and obesity are associated with the most weight gain after quitting smoking and finding the weight gain more intolerable (Bush et al., 2008; LaRowe et al., 2009; A. Levine et al., 2007; M. D. Levine et al., 2013). As a result, individuals who smoke are more likely to return to smoking when they have overweight and obesity than those who are lean (Audrain‐McGovern and Benowitz, 2011; Borrelli et al., 1999).
Evidence shows that individual differences in smoking motives may influence treatment outcomes. For example, higher addictive motives for smoking are associated with more difficulty weaning off of nicotine gum and less likely to abstain at long-term follow-up. (Murray et al., 2000). Further, individuals engaging in a nicotine replacement smoking cessation trial who endorsed smoking for emotion regulation were less likely to have successful cessation outcomes than those who did not (Murray et al., 2000). Psychosocial motives, such as identifying as “a smoker” due to factors such as affiliation or belongingness, are related to less successful cessation attempts and intentions to quit (Falomir and Invernizzi, 1999; Putte et al., 2009). Given that greater personalization increases efficacy and acceptability (Haokip et al., 2020; Rose et al., 2010), cessation interventions tailored to individuals’ smoking motives may improve outcomes. For adults who smoke cigarettes with obesity, targeting weight concerns in the context of treatment is a possible way to personalize treatment. Cessation interventions targeting weight concerns are more effective than interventions focusing solely on weight control or smoking cessation (Perkins et al., 2001). Similarly, for those seeking treatment to quit with high rates of addictive motivation or automaticity, incorporating strategies to manage cravings or increase mindfulness of smoking triggers respectively may likewise improve effectiveness.
There are limitations to the current study that should be addressed. This analysis was not a prospective examination, and as such, certain variables of interest relevant to obesity, such as weight concerns or diet history, were not collected. Future research would benefit from examinating both the motives in the SMQ and other motives such as weight concerns among BMI groups. Further, given this was a cross-sectional study, we are unable to determine if smoking motivations differentially influence smoking behavior prospectively, which would allow for stronger causative inferences. Nonetheless, these findings are notable given that these studies were not expressly designed to assess the influence of BMI, suggesting that this effect may be largely generalizable to treatment-seeking adults who smoke cigarettes. Conversely, results may not generalize to non-treatment-seeking individuals. Additional prospective research in larger samples is warranted, particularly to investigate the impact of these variables on treatment success.
5. Conclusions
BMI and obesity are frequently not reported or controlled for in smoking research; these findings demonstrate the importance of taking weight-related variables into account when examining smoking behavior or motives. Further, BMI is often not treated as a continuous variable, neglecting the unique presentation of individuals in the overweight range. Interventions addressing smoking and overweight independently have had limited success (Foster et al., 2005; Pacek et al., 2018; Pi-Sunyer et al., 2007). This high-risk population may require intervention specifically targeting their motivations to continue smoking in order to optimize the success of cessation attempts. Understanding how BMI influences smoking behavior and motivation can inform treatment to promote smoking cessation.
Author statement
Role of Funding Sources Funding for this study was provided by NIH NIDA grants, R01DA030394 and R01DA029845.
Dr. Ely is supported by NIDA grant 5T32DA028874–10.
Contributors
All authors take responsibility for the content, gave approval of the submission and made substantive intellectual contributions to the submitted work. AVE contributed to conception and design; NHS and HK contributed to data acquisition; AVE, TF, and RRW contributed to data analyses; AVE and HK drafted the manuscript; TF, RRW, JAM provided critical revision.
Declaration of Competing Interest
The authors declare no financial interests or conflicts of interest.
Acknowledgments
The authors would like to thank Melanie Maron, M.S., Wetherill Lab Manager for supervision of staff and study procedures.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2021.100008.
Appendix. Supplementary materials
References
- Audrain-McGovern J., Benowitz N.L. Cigarette smoking, nicotine, and body weight. Clin. Pharmacol. Ther. 2011;90(1):164–168. doi: 10.1038/clpt.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baler R.D., Volkow N.D. Drug addiction: the neurobiology of disrupted self-control. Trends Mol. Med. 2006;12(12):559–566. doi: 10.1016/j.molmed.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Berg C.J., An L.C., Thomas J.L., Lust K.A., Sanem J.R., Swan D.W., Ahluwalia J.S. Smoking patterns, attitudes and motives: unique characteristics among 2-year versus 4-year college students. Health Educ. Res. 2011;26(4):614–623. doi: 10.1093/her/cyr017. [DOI] [PubMed] [Google Scholar]
- Blendy J.A., Strasser A., Walters C.L., Perkins K.A., Patterson F., Berkowitz R., Lerman C. Reduced nicotine reward in obesity: cross-comparison in human and mouse. Psychopharmacology (Berl.) 2005;180(2):306–315. doi: 10.1007/s00213-005-2167-9. [DOI] [PubMed] [Google Scholar]
- Bommelé J., Schoenmakers T.M., Kleinjan M., van Straaten B., Wits E., Snelleman M., van de Mheen D. Perceived pros and cons of smoking and quitting in hard-core smokers: a focus group study. BMC Public Health. 2014;14(175) doi: 10.1186/1471-2458-14-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B., Spring B., Niaura R., Kristeller J., Ockene J.K., Keuthen N.J. Weight suppression and weight rebound in ex-smokers treated with fluoxetine. J. Consult. Clin. Psychol. 1999;67(1):124–131. doi: 10.1037/0022-006X.67.1.124. [DOI] [PubMed] [Google Scholar]
- Bush T., Levine M.D., Deprey M., Cerutti B., Zbikowski S.M., McAfee T., Mahoney L., Beebe L. Prevalence of weight concerns and obesity among smokers calling a quitline. J. Smok. Cessat. 2008;4(5):74–78. doi: 10.1375/jsc.4.2.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carim-Todd L., Mitchell S.H., Oken B.S. Impulsivity and stress response in nondependent smokers (tobacco chippers) in comparison to heavy smokers and nonsmokers. Nicotine Tob. Res. 2016;18(5):547–556. doi: 10.1093/ntr/ntv210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M.R. MMWR. Morbidity and Mortality Weekly Report, 68. 2019. Tobacco product use and cessation indicators among adults—United States, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dare S., Mackay D.F., Pell J.P. Relationship between smoking and obesity: a cross-sectional study of 499,504 middle-aged adults in the UK general population. PLoS ONE. 2015;10(4) doi: 10.1371/journal.pone.0123579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C., Strachan S., Berkson M. Sensitivity to reward: implications for overeating and overweight. Appetite. 2004;42(2):131–138. doi: 10.1016/j.appet.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Day J.J., Roitman M.F., Wightman R.M., Carelli R.M. Associative learning mediates dynamic shifts in dopamine signaling in the nucleus accumbens. Nat. Neurosci. 2007;10(8):1020–1028. doi: 10.1038/nn1923. [DOI] [PubMed] [Google Scholar]
- Doornweerd S., van Duinkerken E., de Geus E.J., Arbab-Zadeh P., Veltman D.J., IJzerman R.G. Overweight is associated with lower resting state functional connectivity in females after eliminating genetic effects: a twin study. Hum Brain Mapp. 2017;38(10):5069–5081. doi: 10.1002/hbm.23715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely A.V., Jagannathan K., Spilka N., Keyser H., Rao H., Franklin T.R., Wetherill R.R. The influence of obesity and overweight on intra-network resting-state connectivity in chronic cigarette smokers. Drug Alcohol Depend. 2021 doi: 10.1016/j.drugalcdep.2021.108911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerstrom Test for Cigarette Dependence. Nicotine Tob. Res. 2012;14(1):75–78. doi: 10.1093/ntr/ntr137. [DOI] [PubMed] [Google Scholar]
- Falomir J.M., Invernizzi F. The role of social influence and smoker identity in resistance to smoking cessation. Swiss J. Psychol. 1999;58(2):73–84. [Google Scholar]
- Foster G.D., Makris A.P., Bailer B.A. Behavioral treatment of obesity. Am. J. Clin. Nutr. 2005;82(1):230S–235S. doi: 10.1093/ajcn/82.1.230S. [DOI] [PubMed] [Google Scholar]
- Franklin T.R., Harper D., Kampman K., Kildea-McCrea S., Jens W., Lynch K.G., O'Brien C.P., Childress A.R. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol Depend. 2009;103(1):30–36. doi: 10.1016/j.drugalcdep.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin T.R., Wang Z., Suh J.J., Hazan R., Cruz J., Li Y., Goldman M., Detre J.A., O'Brien C.P., Childress A.R. Effects of varenicline on smoking cue–triggered neural and craving responses. Arch. Gen. Psychiatry. 2011;68(5):516–526. doi: 10.1001/archgenpsychiatry.2010.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman D.M., Sigurdson A.J., Rajaraman P., Doody M.M., Linet M.S., Ron E. The mortality risk of smoking and obesity combined. Am. J. Prev. Med. 2006;31(5):355–362. doi: 10.1016/j.amepre.2006.07.022. [DOI] [PubMed] [Google Scholar]
- Goodchild M., Nargis N., d'Espaingnet E.T. Global economic cost of smoking-attributable diseases. Tob Control. 2018;27:58–64. doi: 10.1136/tobaccocontrol-2016-053305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales C.M., Fryar C.D., Carroll M.D., Freedman D.S., Aoki Y., Ogden C.L. Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013-2016. JAMA. 2018;319(23):2419–2429. doi: 10.1001/jama.2018.7270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haokip H.R., Kumar R., Rawat V.S. Efficacy of standard nicotine replacement therapy (NRT) versus videoassisted nurse-led NRT on tobacco cessation: a randomized controlled pilot trial. Clin. Epidemiol. Glob Health. 2020 [Google Scholar]
- Heatherton T.F., Kozlowski L.T., Frecker R.C., Fagerstrom K.-.O. The fagerström test for nicotine dependence: a revision of the fagerstrom tolerance questionnaire. Br J Addict. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hovland J., Ceballos N.A. Are smokers’ reasons for smoking related to their body mass indices? Subst Use Misuse. 2007;42(8):1337–1344. doi: 10.1080/10826080701212212. [DOI] [PubMed] [Google Scholar]
- LaRowe T.L., Piper M.E., Schlam T.R., Fiore M.C., Baker T.B. Obesity and smoking: comparing cessation treatment seekers with the general smoking population. Obesity (Silver Spring) 2009;17(6):1301–1305. doi: 10.1038/oby.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine A., Zagoory-Sharon O., Feldman R., Lewis J.G., Weller A. Measuring cortisol in human psychobiological studies. Physiol. Behav. 2007;90(1):43–53. doi: 10.1016/j.physbeh.2006.08.025. [DOI] [PubMed] [Google Scholar]
- Levine M.D., Bush T., Magnusson B., Cheng Y., Chen X. Smoking-related weight concerns and obesity: differences among normal weight, overweight, and obese smokers using a telephone tobacco quitline. Nicotine Tob. Res. 2013;15(6):1136–1140. doi: 10.1093/ntr/nts226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray R.P., Gerald L.B., Lindgren P.G., Connett J.E., Rand C.S., Anthonisen N.R. Characteristics of participants who stop smoking and sustain abstinence for 1 and 5 years in the lung health study. Prevent. Med. 2000;30:392–400. doi: 10.1006/pmed.2000.0642. [DOI] [PubMed] [Google Scholar]
- Oksuz E., Mutlu E.T., Malhan S. Characteristics of daily and occasional smoking among youths. J. R. Inst. Public Health. 2007;121:349–356. doi: 10.1016/j.puhe.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Pacek L.R., McClernon F.J., Bosworth H.B. Adherence to pharmacological smoking cessation interventions: a literature review and synthesis of correlates and barriers. Nicotine Tob. Res. 2018;20(10):1163–1172. doi: 10.1093/ntr/ntx210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins K.A., Marcus M.D., Levine M.D., D'Amico D., Miller A., Broge M., Ashcom J., Shiffman S. Cognitive–behavioral therapy to reduce weight concerns improves smoking cessation outcome in weight-concerned women. J. Consult. Clin. Psychol. 2001;69(4):604–613. doi: 10.1037/0022-006X.69.4.604. [DOI] [PubMed] [Google Scholar]
- Pi-Sunyer X., Blackburn G., Brancati F.L., Bray G.A., Bright R., Clark J.M., Curtis J.M., Espeland M.A., Foreyt J.P., Graves K., Haffner S.M., Harrison B., Hill J.O., Horton E.S., Jakicic J., Jeffery R.W., Johnson K.C., Kahn S., Kelley D.E.…Yanovski S.Z. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putte B., van den, Yzer M., Willemsen M.C., Bruijn G.-J.de. The effects of smoking self-identity and quitting self-identity on attempts to quit smoking. Health Psychol. 2009;28(5):535–544. doi: 10.1037/a0015199. [DOI] [PubMed] [Google Scholar]
- Robinson T.E., Berridge K.C. The incentive sensitization theory of addiction: some current issues. Philosoph. Trans. R. Soc. B. 2008;363(1507):3137–3146. doi: 10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha S.A.V., Hoepers A.T., de C., Fröde T.S., Steidle L.J.M., Pizzichini E., Pizzichini M.M.M. Prevalence of smoking and reasons for continuing to smoke: a population-based study. J. Brasileiro de Pneumologia. 2019;45(4) doi: 10.1590/1806-3713/e20170080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose J.E., Behm F.M., Drgon T., Johnson C., Uhl G.R. Personalized smoking cessation: interactions between nicotine dose, dependence, and quit-success genotype score. Mol. Med. 2010;16:247–253. doi: 10.2119/molmed.2009.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell M.a.H., Peto J., Patel U.A. The Classification of Smoking by Factorial Structure of Motives. Journal of the Royal Statistical Society: Series A (General) 1974;137(3):313–333. doi: 10.2307/2344953. [DOI] [Google Scholar]
- Schultz W. Predictive Reward Signal of Dopamine Neurons. J. Neurophysiol. 1998;80(1):1–27. doi: 10.1152/jn.1998.80.1.1. [DOI] [PubMed] [Google Scholar]
- Seidell J.C., Halberstadt J. The Global Burden of Obesity and the Challenges of Prevention. Ann. Nutr. Metab. 2015;66(Suppl. 2):7–12. doi: 10.1159/000375143. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V., Lecrubier Y., Sheehan K.H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G.C. The mini-international neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Shiffman S., Dunbar M.S., Scholl S.M., Tindle H.A. Smoking motives of daily and non-daily smokers: a profile analysis. Drug Alcohol Depend. 2012;126:362–368. doi: 10.1016/j.drugalcdep.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate J.C., Pomerleau C.S., Pomerleau O.F. Pharmacological and non-pharmacological smoking motives: a replication and extension. Addiction. 1994;89(3):321–330. doi: 10.1111/j.1360-0443.1994.tb00899.x. [DOI] [PubMed] [Google Scholar]
- Taylor A.E., Richmond R.C., Palviainen T., Loukola A., Wootton R.E., Kaprio J., Relton C.L., Davey Smith G., Munafò M.R. The effect of body mass index on smoking behaviour and nicotine metabolism: a Mendelian randomization study. Hum. Mol. Genet. 2019;28(8):1322–1330. doi: 10.1093/hmg/ddy434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuovinen E.-.L., Saarni S.E., Kinnunen T.H., Ollila H., Ruokolainen O., Patja K., Männistö S., Jousilahti P., Kaprio J., Korhonen T. Weight concerns as a predictor of smoking cessation according to nicotine dependence: a population-based study. Nordic Stud. Alcohol Drugs. 2018;35(5):344–356. doi: 10.1177/1455072518800217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N.D., Wise R.A., Baler R. The dopamine motive system: implications for drug and food addiction. Nat. Rev. Neurosci. 2017;18(12):741–752. doi: 10.1038/nrn.2017.130. [DOI] [PubMed] [Google Scholar]
- Watanabe T., Tsujino I., Konno S., Ito Y.M., Takashina C., Sato T., Isada A., Ohira H., Ohtsuka Y., Fukutomi Y., Nakamura H., Kawagishi Y., Okada C., Hizawa N., Taniguchi M., Akasawa A., Nishimura M. Association between smoking status and obesity in a nationwide survey of japanese adults. PLoS ONE. 2016;11(3) doi: 10.1371/journal.pone.0148926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.