Highlights
-
•
An overdose reversal/naloxone distribution program were initiated in Mexicali.
-
•
The program was successful in distributing naloxone.
-
•
Reported overdoses increased in the period during the early COVID-19 pandemic.
Keywords: Overdose, Naloxone, Prevention, Safe consumption site, Mexico, LMIC, Latin America
Abstract
Background
Drug overdoses are prevalent in low- and middle-income countries but are scarcely reported in the literature. We report on an opioid overdose reversal and naloxone distribution program that was instituted at the first safe consumption site in Latin America.
Methods
A cross-sectional analysis of witnessed drug overdoses and naloxone distribution between 1 June 2019 and 31 May 2021 in Mexicali, Mexico. Case report forms were entered in an electronic database. Trends in overdose and naloxone distribution were described. Comparisons were made before and after the COVID-19 pandemic was declared in the city. Maps were created to represent the geographic distribution of overdose in the city.
Results
During the study period 1,534 doses of naloxone were distributed throughout the community. In addition, there were 464 overdoses reported during this period, of which 4 were fatal. There was a 30% increase in reported overdoses from the period before the COVID-19 pandemic to the period after the pandemic was declared (p = 0.03). Most common substance reported included heroin (93%), sedatives (21%), methamphetamine (16%) and fentanyl (14%). Naloxone was given in 96% of cases (median 1 dose, IQR 1–2 doses) and emergency services were called in 20% of cases.
Conclusions
An opioid overdose reversal program in Mexicali, Mexico was able to distribute naloxone and register drug overdoses between 2019 and 2021 as a harm reduction strategy. This adds to the growing body of literature on the impact of community-based programs on preventing fatal overdoses and the potential for implementation in low-resource settings.
1. Introduction
Deaths due to unintentional drug overdoses are on the rise in many geographic settings, including both low- and high-income countries (Martins et al., 2015). Fatal and non-fatal overdoses have further increased with the introduction of fentanyl in multiple drug markets (Spencer et al., 2019), and early studies during the COVID-19 pandemic report a further increase in overdoses (Friedman and Akre, 2021; Mason et al., 2021). The hypothesized reasons for this increase during the COVID-19 pandemic are related to changes in drug availability and closures to the harm reduction infrastructure, among others (Volkow, 2020). Interventions implemented in different settings to curb the drug overdose epidemic include naloxone distribution (Enteen et al., 2010; Madah-Amiri et al., 2019; Maxwell et al., 2006; Moustaqim-Barrette et al., 2021; Nolen et al., 2021), low-threshold access to substance use treatment and medication for opioid use disorder (Andersson et al., 2021), safer prescribing of controlled substances (Lee et al., 2021), and institution and expansion of safe consumption sites (SCS) (Kerr et al., 2017; Saloner et al., 2018). Most, if not all of the reports of the outcomes of these programs, are centered in high-income countries, and little is known in low- and middle-income countries (Dutta et al., 2012).
In Mexico, areas along the United States (US)-Mexico border are known for a high prevalence of high-risk drug use (Cepeda et al., 2020; Fleiz et al., 2020; Ospina-Escobar et al., 2018). Integracion Social Verter A.C. (Verter), a community-based organization in Mexicali, Mexico, opened an unsanctioned safe consumption service called La Sala in this city along the US-Mexico border in 2018 (Agren, 2019). The Verter SCS is the first in Latin America, and one of only four in the world that is exclusive to women (Beletsky et al., 2018). Since 2019, the organization initiated a community-based overdose reversal program (ORP), with peer-oriented naloxone training and targeted naloxone dispensing, as well as overdose assistance outside of the SCS. The program was available to the general community beyond the women who use the SCS. This report highlights the outcomes of the program and some lessons to draw a path towards a national overdose prevention strategy in Mexico that could also be extrapolated to other low- and middle-income countries.
2. Methods
This is a retrospective analysis of case report forms collected by Verter's staff over a two-year period between 1 June 2019 and 31 May 2021. A case report form was completed by Verter's staff either after responding to an overdose or collected from reports by community members after they witnessed or assisted an overdose in the community. Overdoses assisted at the SCS were not included in the analysis. Staff and researchers culturally adapted naloxone utilization forms and protocols designed by the British Columbia Center for Disease Control harm reduction services in Canada (Moustaqim-Barrette et al., 2021) and other US based naloxone distribution services, like the Chicago Recovery Alliance Opioid Prevention Program (Maxwell et al., 2006) and the DOPE project in San Francisco (Enteen et al., 2010).
Community members who used services at Verter were provided with training on how to use naloxone and 2 doses of injectable or nasal naloxone (based on what formulation was available). Individuals were encouraged to return for more naloxone after any use of the medication. In some situations, if the overdose was close to the SCS, Verter's staff would rush to the site to help reverse it. Data captured after each overdose event included the date of the incident, age, gender, neighborhood it happened, type of location (e.g. house, street, shooting gallery, etc.), if naloxone was used, what type of naloxone (i.e. injectable, intranasal), how many doses were given, the suspected drug involved in the overdose, if emergency services were called, and any additional resuscitation techniques. Data were captured in an electronic databased for programmatic and administrative purposes. Retrospective analysis was approved by the Institutional Review Board (IRB) at Prevencasa, A.C (IRB00012509) in Mexico. For investigators at UCLA, the IRB deemed this study exempt from review as researchers at this institution did not have access to personally identifiable information.
We provide descriptive statistics of the reported overdoses that include means and standard deviations, medians and interquartile ranges, counts and percentages where applicable. We compared the number of reported overdoses before the COVID-19 pandemic was declared (15 March 2020) and reported overdoses during the pandemic using a Poisson means test. We compared nine months before and during the pandemic to have equal time periods. To graphically represent the reach of the SCS while simultaneously protecting confidentiality, we created a map where each reported overdose was randomly distributed within the neighborhood it was reported in. All analyses were performed in R version 3.6.2 (Vienna, Austria).
3. Results
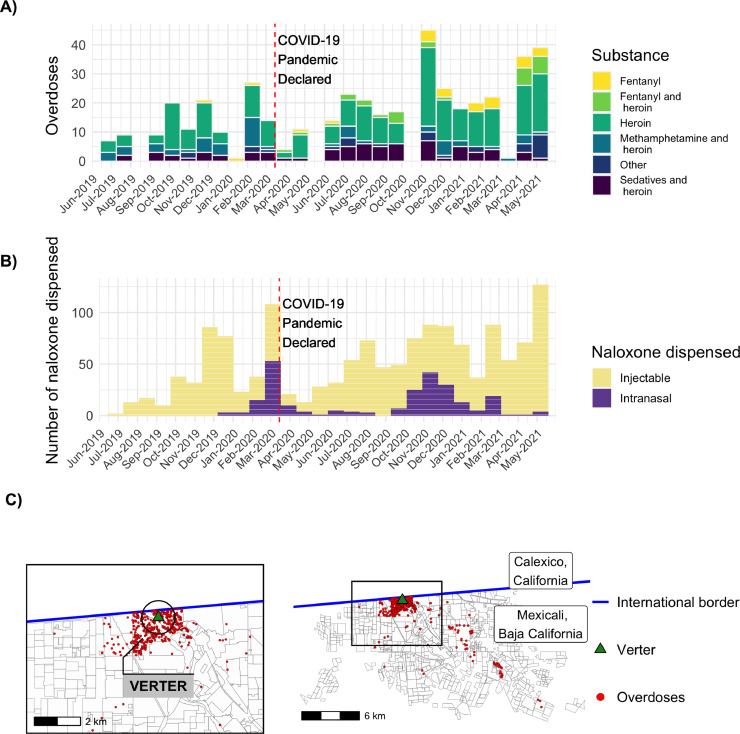
Between 1 June 2019 and 31 May 2021, there were 464 overdoses reported. Overdose events increased during the COVID-19 pandemic (165 overdoses) compared to before the pandemic (127 overdoses) by 30% (p = 0.03) (Fig. 1, Panel A). During the study period, Verter distributed 1286 doses of injectable naloxone and 248 doses of nasal naloxone, for a total of 1534 doses (Fig. 1, Panel B). Overdoses were reported most from the two neighborhoods adjacent to Verter and that were located in Mexicali's downtown: Pueblo Nuevo, 42% and Primera Sección, 30% (Fig. 1, Panel C).
Fig. 1.
Overdose reported and naloxone distributed in Mexicali, Mexico between 1 June 2019 and 31 May 2021. A) Overdoses over time. B) Naloxone distributed. C) Geographic distribution of overdoses. Verter is the location of the safe consumption site in Mexicali, Mexico.
The mean age of cases who overdosed was 33.7 years (SD 9.8), and 80% were male (Table 1). The most common places where an overdose occurred were in a shooting gallery (29%), on the street (21%), and at home (16%). Substances involved included heroin (93%), sedatives (21%), methamphetamine (16%) and fentanyl (14%). The most common combinations of substances were sedatives and heroin (16%), and methamphetamine and heroin (13%). Before the pandemic, only four fentanyl-related overdoses were reported. Since the pandemic, 29 fentanyl-related overdoses were reported. Four individuals died (0.8%).
Table 1.
Descriptive statistics of overdose cases in Mexicali, Mexico between 1 June 2019 and 31 May 2021 (N = 464).
| Name | Overall |
|---|---|
| Age (mean (SD)) | 33.7 (9.8) |
| Gender (%) | |
| Female | 87 (18.8) |
| Male | 370 (79.7) |
| Transgender | 7 (1.5) |
| Naloxone applied | 445 (95.9) |
| Naloxone doses (median [IQR]) | 1.00 [1.00, 2.00] |
| Product applied (%) | |
| Naloxone, injection | 345 (74.4) |
| Naloxone, intranasal | 82 (17.7) |
| None | 19 (4.1) |
| Both | 18 (3.9) |
| Substance reported (%) | |
| Heroin | 433 (93.3) |
| Sedatives | 99 (21.3) |
| Methamphetamine | 73 (15.7) |
| Fentanyl | 66 (14.2) |
| Combinations of substances reported | |
| Heroin alone | 243 (52.4) |
| Sedatives and heroin | 75 (16.2) |
| Methamphetamine and heroin | 60 (12.9) |
| Fentanyl and heroin | 29 (6.2) |
| Fentanyl alone | 26 (5.6) |
| Methamphetamine and sedatives and heroin | 9 (1.9) |
| Sedatives and fentanyl and heroin | 7 (1.5) |
| Methamphetamine and sedatives and heroin and fentanyl | 4 (0.9) |
| Sedatives and alcohol and heroin | 4 (0.9) |
| Unknown | 3 (0.6) |
| Alcohol alone | 2 (0.4) |
| Alcohol and heroin | 2 (0.4) |
| Died | 4 (0.9) |
Any type of naloxone was given in 96% of cases (median 1 dose, IQR 1–2 doses) and emergency services were called in 20% of cases. The most common reasons for not calling emergency services included the responder felt it was not necessary (47%), fear of the authorities (24%), and not having a way to call (5%). Other resuscitation responses physical stimulation (19%), mouth-to-mouth resuscitation (17%), hitting the sternum (16%), injecting salt water (13%), chest compressions (10%), and placing ice in the neck or groin area (8%).
4. Discussion
During a two-year period, up to 460 community overdose-related death events were potentially averted. Considering that other ORP in the US have reported a lower average number of events during the early stages of their programs (Enteen et al., 2010), the number reported at Verter is noteworthy, and only expected to increase with increased community awareness of the program. Similar to previous studies, our analysis found a high post–naloxone administration survival (Clark et al., 2014). Also, comparable to what has happened in other areas in North America (Glober et al., 2020; Slavova et al., 2020), we saw an increase in reported overdoses after the COVID-19 pandemic public emergency was declared in the city. This increase coincided with an uptick in confiscated fentanyl in the region (Fleiz et al., 2020; Friedman et al., 2020). However, the growth in overdose reports may also be expected due to increased knowledge in the availability of naloxone in the area over time, and not exclusively to the COVID-19 pandemic and the increase in fentanyl in the region.
It is important to note that in most cases emergency services were not called. This might reflect the fear of police arriving to the site of an overdose, as they are generally the first responders (Beletsky et al., 2013). Police trainings designed to increase awareness around harm reduction could help improve knowledge and attitudes towards programs such as naloxone distribution (Arredondo et al., 2017). Prior research at the US-Mexico border showed low levels of drug policy knowledge among municipal police officers (Arredondo et al., 2017). At the same time, educational intervention in police officers in the region led to positive changes in attitudes toward referrals to harm reduction services like needle exchange and overdose prevention programs (Olgin et al., 2020). Continued implementation of interventions like these are extremely important in a country known for its systemic police abuse toward people who use drugs.
While Verter's ORP included training on resuscitation techniques, other non-medical strategies were still used on many occasions. However, while a previous study at the border documented high rates of usage of salt water and almost no naloxone utilization (Fleiz-Bautista et al., 2019), our numbers may indicate a behavioral shift in the way people are approaching overdoses by shifting strategies (e.g., using naloxone). Person-centered and culturally competent harm reduction messaging around the importance of effective medical responses (e.g., naloxone, cardiopulmonary resuscitation, calling an ambulance) to overdose, and the potential to avert death are important and necessary (Wilkinson et al., 2020). Due to COVID-19 restrictions in the Mexicali, in person meetings such as those designed to train people in overdose response, were suspended. It is the expectation to resume in-person peer training to address misinformation and potentially harmful responses to overdose situations.
It is important to note that naloxone for overdose reversal is exceedingly difficult to access in Mexico. Within the country's pharmaceutical market, naloxone is exclusively used within hospitals and surgical centers. This increases the price considerably, and there is little to no support from the federal government for this harm reduction infrastructure (Lopez Obrador, 2019). Although a similar phenomenon related to elevated cost occurred in the US (Gupta et al., 2016), in that country many state or federal programs exist to maintain naloxone availability at a low-cost or free of charge to harm reduction centers. The Verter SCS site has been able to receive donated naloxone or procure it from abroad, but a legislative framework is lacking to import naloxone across the border hampering this effort. Currently, naloxone is still considered a prescription drug, and in theory, community members and staff could run into administrative or legal sanctions if they use it. A bill was proposed in the Mexican Senate to reschedule naloxone, but the initiative failed to discuss a broad national strategy against overdose (Monreal-Avila, 2021). At the time of publication, the authorship group and staff members from Verter were working with other key stakeholders, like research institutions, community organizations and health practitioners, to develop a national overdose monitoring and reporting strategy. This designed to increase evidence around the need for free and widely available naloxone for at risk populations around Mexico.
While we believe that these numbers and efforts are important, placing these in the population level context of overdose mortality reduction is challenging to address. Mexico currently lacks accurate data reporting on overdoses (West et al., 2020). For example, in 2017, Mexico reported 147 overdose deaths nation-wide to the United Nations (United Nations Office on Drugs and Crime, 2021). This number is small for a country of over 110 million people with a long known drug market, especially present along the US-Mexico border (Ospina-Escobar et al., 2018). Mexico has a public data system for registering mortality that is compiled annually by the National Statistical and Geographical Institute. These numbers are generated locally by each coroner's office at the city level, however, the lack of proficiency to identify overdose deaths by these forensic teams is well documented across the country (Dirección General de Información en Salud, 2020). While the lack of overdose deaths reported by official statistics calls into question the accuracy of the national mortality data, the increasing infiltration of fentanyl in the border area (Fleiz et al., 2020; Friedman et al., 2020) and the ORP data suggests that a hidden overdose epidemic may be evolving. Comprehensive mortality reporting on drug-related deaths in Mexico is needed to accurately capture this important health metric.
The data we present has several limitations linked to the self-reported nature of the data collection, that can lead to social desirability or recall bias among individuals that complete the report forms. Some events might not be recorded by the staff, due to Verter not opening at all hours of the day or on weekends, resulting in underreported numbers (Bennett et al., 2018). Though there was an increase in the number of events during the COVID-19 pandemic, this is still likely an underestimate. As data is collected anonymously multiple events may be in the same person over time decreasing the number of fatal overdose actually averted. Lastly, substances involved were collected by self-report from individuals suffering the overdose or witnesses. No testing was performed, hence, misclassification bias is likely.
The data herein exemplifies the importance of naloxone to prevent overdose deaths, the programmatic reach of a SCS beyond its walls, and the successful implementation of an ORP in the low- and middle-income country setting. The data also speaks to the importance of supporting existing community-based organizations that provide harm reduction services (Bennett et al., 2018). In Mexico, this may be even more important given the lack of trust and constant discrimination people who use drugs suffer each day in their local interactions with government and health services (Arredondo et al., 2018; Beletsky et al., 2013). Further education is necessary to promote evidence-based resuscitation techniques. Finally, at the time of writing this article, the Mexican Federal government removed all funding support to non-governmental agencies (Lopez Obrador, 2019). Continued support of programs like the ORP program established at Verter are necessary to save lives of vulnerable populations like those of people who use drugs.
Author's contributions
D.G.M. and J.A. conceived the study and collaborated in designing the procedures. S.S. and L.A. coordinated the study and data collection. D.G.M. and P.G. performed the data analyses. D.G.M. and J.A. drafted the manuscript. M.C.C., A.L. and S.S. provided aided in interpreting the results and worked on the manuscript. All authors provided critical revisions, read, and approved the final manuscript.
Role of funding source
The funders had no role in the content of this manuscript. This work was funded by a UCLA Center for HIV Identification, Prevention, and Treatment Services (CHIPTS) (U.S. National Institute of Mental Health [NIMH] grant P30MH58107) pilot grant. D.G.M. was supported by the U.S. National Institute on Drug Abuse (grant K08DA048163). M.C.C. was supported by NIMH (T32MH080634, PI: Currier and Gorbach). S.S was supported by CHIPTS, the UCLA Center for AIDS Research (grant 5P30AI028697), and the UCLA Clinical Translational Science Institute (grant UL1TR001881). The views expressed in this publication are those of the authors and not necessarily those of their institution or funders.
Data statement
Data and code are available at: https://github.com/davigood1/OPP_Verter
Declaration of Interests
The authors declare no competing interests.
Acknowledgements
We would like to thank the Sonoran Prevention Works, the Chicago Recovery Alliance and Maya Doe-Simkins for their advice and help to set up the overdose prevention program. We would also like to thank the individuals and organizations that provided naloxone for the program. Finally, we acknowledge the community members who took part in the trainings, used naloxone and other resuscitation measures to save lives, and reported the cases.
References
- Agren D. Verter: helping drug users near the USA-Mexico border. Lancet HIV. 2019;6(8):e495. doi: 10.1016/S2352-3018(19)30223-1. [DOI] [PubMed] [Google Scholar]
- Andersson L., Håkansson A., Berge J., Johnson B. Changes in opioid-related deaths following increased access to opioid substitution treatment. Subst. Abuse Treat. Prev. Policy. 2021;16(1):15. doi: 10.1186/s13011-021-00351-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arredondo J., Gaines T., Manian S., Vilalta C., Bañuelos A., Strathdee S.A., Beletsky L. The law on the streets: evaluating the impact of Mexico’s drug decriminalization reform on drug possession arrests in Tijuana, Mexico. Int. J. Drug Policy. 2018;54:1–8. doi: 10.1016/j.drugpo.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arredondo J., Strathdee S.A., Cepeda J., Abramovitz D., Artamonova I., Clairgue E., Bustamante E., Mittal M.L., Rocha T., Bañuelos A., Olivarria H.O., Morales M., Rangel G., Magis C., Beletsky L. Measuring improvement in knowledge of drug policy reforms following a police education program in Tijuana, Mexico. Harm. Reduct. J. 2017;14(1):72. doi: 10.1186/s12954-017-0198-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beletsky L., Baker P., Arredondo J., Emuka A., Goodman-Meza D., Medina-Mora M.E., Werb D., Davidson P., Amon J.J., Strathdee S., Magis-Rodriguez C. The global health and equity imperative for safe consumption facilities. Lancet. 2018;392(10147):553–554. doi: 10.1016/S0140-6736(18)31469-7. [DOI] [PubMed] [Google Scholar]
- Beletsky L., Lozada R., Gaines T., Abramovitz D., Staines H., Vera A., Rangel G., Arredondo J., Strathdee S.A. Syringe confiscation as an HIV risk factor: the public health implications of arbitrary policing in Tijuana and Ciudad Juarez, Mexico. J. Urban Health. 2013;90(2):284–298. doi: 10.1007/s11524-012-9741-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett A.S., Bell A., Doe-Simkins M., Elliott L., Pouget E., Davis C. From Peers to Lay Bystanders: findings from a Decade of Naloxone Distribution in Pittsburgh, P.A.J. Psychoactive Drugs. 2018;50(3):240–246. doi: 10.1080/02791072.2018.1430409. [DOI] [PubMed] [Google Scholar]
- Cepeda J.A., Bórquez A., Magana C., Vo A., Rafful C., Rangel G., Medina-Mora M.E., Strathdee S., Martin N.K. Modelling integrated antiretroviral treatment and harm reduction services on HIV and overdose among people who inject drugs in Tijuana, Mexico. J. Int. AIDS Soc. 2020;23 Suppl 1(Suppl 1):e25493. doi: 10.1002/jia2.25493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A.K., Wilder C.M., Winstanley E.L. A systematic review of community opioid overdose prevention and naloxone distribution programs. J. Addict. Med. 2014;8(3):153–163. doi: 10.1097/ADM.0000000000000034. [DOI] [PubMed] [Google Scholar]
- Dirección General de Información en Salud, 2020. Datos Abiertos. http://www.dgis.salud.gob.mx/contenidos/basesdedatos/Datos_Abiertos_gobmx.html.
- Dutta A., Wirtz A.L., Baral S., Beyrer C., Cleghorn F.R. Key harm reduction interventions and their impact on the reduction of risky behavior and HIV incidence among people who inject drugs in low-income and middle-income countries. Curr. Opin. HIV AIDS. 2012;7(4):362–368. doi: 10.1097/COH.0b013e328354a0b5. [DOI] [PubMed] [Google Scholar]
- Enteen L., Bauer J., McLean R., Wheeler E., Huriaux E., Kral A.H., Bamberger J.D. Overdose prevention and naloxone prescription for opioid users in San Francisco. J. Urban Health. 2010;87(6):931–941. doi: 10.1007/s11524-010-9495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleiz C., Arredondo J., Chavez A., Pacheco L., Segovia L.A., Villatoro J.A., Cruz S.L., Medina-Mora M.E., Fuente J.R. Fentanyl is used in Mexico’s northern border: current challenges for drug health policies. Addiction. 2020;115(4):778–781. doi: 10.1111/add.14934. [DOI] [PubMed] [Google Scholar]
- Fleiz-Bautista C, D.-G.M., Villatoro-Velázquez J.A., Vázquez-Quiroz F., Zafra-Mora E., Sánchez-Ramos R., Medina-Mora M.E. Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz; 2019. Cuqueando La Chiva: Contextos del Consumo De Heroína En La Frontera Norte De México. [Google Scholar]
- Friedman J., Akre S. COVID-19 and the Drug Overdose Crisis: uncovering the Deadliest Months in the United States, January‒July 2020. Am. J. Public Health. 2021:e1–e8. doi: 10.2105/AJPH.2021.306256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Arredondo J., Beletsky L., Bourgois P. APHA's 2020 VIRTUAL Annual Meeting and Expo. 2020. The introduction of fentanyl on the US-Mexico border: an ethnographic account triangulated with drug checking data from Tijuana. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glober N., Mohler G., Huynh P., Arkins T., O'Donnell D., Carter J., Ray B. Impact of COVID-19 Pandemic on Drug Overdoses in Indianapolis. J. Urban Health. 2020;97(6):802–807. doi: 10.1007/s11524-020-00484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R., Shah N.D., Ross J.S. The Rising Price of Naloxone — Risks to Efforts to Stem Overdose Deaths. N. Engl. J. Med. 2016;375(23):2213–2215. doi: 10.1056/NEJMp1609578. [DOI] [PubMed] [Google Scholar]
- Kerr T., Mitra S., Kennedy M.C., McNeil R. Supervised injection facilities in Canada: past, present, and future. Harm. Reduct. J. 2017;14(1):28. doi: 10.1186/s12954-017-0154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee B., Zhao W., Yang K.C., Ahn Y.Y., Perry B.L. Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018. JAMA Netw. Open. 2021;4(2) doi: 10.1001/jamanetworkopen.2020.36687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez Obrador, A., 2019. Circular Uno. https://reunionnacional.tecnm.mx/RND_2019/sa/CIRCULAR%20UNO.pdf.
- Madah-Amiri D., Gjersing L., Clausen T. Naloxone distribution and possession following a large-scale naloxone programme. Addiction. 2019;114(1):92–100. doi: 10.1111/add.14425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S.S., Sampson L., Cerdá M., Galea S. Worldwide Prevalence and Trends in Unintentional Drug Overdose: a Systematic Review of the Literature. Am. J. Public Health. 2015;105(11):e29–e49. doi: 10.2105/AJPH.2015.302843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason M., Welch S.B., Arunkumar P., Post L.A., Feinglass J.M. Notes from the Field: opioid Overdose Deaths Before, During, and After an 11-Week COVID-19 Stay-at-Home Order - Cook County, Illinois, January 1, 2018-October 6, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021;70(10):362–363. doi: 10.15585/mmwr.mm7010a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell S., Bigg D., Stanczykiewicz K., Carlberg-Racich S. Prescribing Naloxone to Actively Injecting Heroin Users. J. Addict. Dis. 2006;25(3):89–96. doi: 10.1300/J069v25n03_11. [DOI] [PubMed] [Google Scholar]
- Monreal-Avila, R., 2021. Iniciativa Con Proyecto De Decreto Por El Que Se Reforma La Fracción IV Del Artículo 245 De La Ley General De Salud En Materia De Atención A Casos De Sobredosis. https://infosen.senado.gob.mx/sgsp/gaceta/64/3/2021-02-18-1/assets/documentos/Inic_Morena_Sen_Monrela_Art_245_Salud_Sobredosis.pdf.
- Moustaqim-Barrette A., Papamihali K., Williams S., Ferguson M., Moe J., Purssell R., Buxton J.A. Adverse events related to bystander naloxone administration in cases of suspected opioid overdose in British Columbia: an observational study. PLoS One. 2021;16(10) doi: 10.1371/journal.pone.0259126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen S., Zang X., Chatterjee A., Behrends C.N., Green T.C., Kumar A., Linas B.P., Morgan J.R., Murphy S.M., Walley A.Y., Yan S., Schackman B.R., Marshall B.D.L. Addiction; 2021. Community-based Naloxone Coverage Equity For the Prevention of Opioid Overdose Fatalities in Racial/Ethnic Minority Communities in Massachusetts and Rhode Island. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olgin G.K., Bórquez A., Baker P., Clairgue E., Morales M., Bañuelos A., Arredondo J., Harvey-Vera A., Strathdee S., Beletsky L., Cepeda J.A. Preferences and acceptability of law enforcement initiated referrals for people who inject drugs: a mixed methods analysis. Subst Abuse Treat Prev Policy. 2020;15(1):75. doi: 10.1186/s13011-020-00319-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ospina-Escobar A., Magis-Rodríguez C., Juárez F., Werb D., Bautista Arredondo S., Carreón R., Ramos M.E., Strathdee S. Comparing risk environments for HIV among people who inject drugs from three cities in Northern Mexico. Harm. Reduct. J. 2018;15(1) doi: 10.1186/s12954-018-0225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner B., McGinty E.E., Beletsky L., Bluthenthal R., Beyrer C., Botticelli M., Sherman S.G. A Public Health Strategy for the Opioid Crisis. Public Health Rep. 2018;133(1_suppl):24s–34s. doi: 10.1177/0033354918793627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S., Rock P., Bush H.M., Quesinberry D., Walsh S.L. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214 doi: 10.1016/j.drugalcdep.2020.108176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer M.R., Warner M., Bastian B.A., Trinidad J.P., Hedegaard H. Drug Overdose Deaths Involving Fentanyl, 2011-2016. Natl. Vital Stat. Rep. 2019;68(3):1–19. [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime, 2021. Drug related deaths and mortality rates per million persons, aged (15-64). https://dataunodc.un.org/data/drugs/Mortality. (Accessed 4/13/2021 2021).
- Volkow N.D. Collision of the COVID-19 and Addiction Epidemics. Ann. Intern. Med. 2020;173(1):61–62. doi: 10.7326/M20-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West B.S., Abramovitz D.A., Gonzalez-Zuniga P., Rangel G., Werb D., Cepeda J., Beletsky L., Strathdee S.A. Drugs, discipline and death: causes and predictors of mortality among people who inject drugs in Tijuana, 2011–2018. Int. J. Drug Policy. 2020;75 doi: 10.1016/j.drugpo.2019.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R., Hines L., Holland A., Mandal S., Phipps E. Rapid evidence review of harm reduction interventions and messaging for people who inject drugs during pandemic events: implications for the ongoing COVID-19 response. Harm. Reduct. J. 2020;17(1):95. doi: 10.1186/s12954-020-00445-5. [DOI] [PMC free article] [PubMed] [Google Scholar]