Highlights
-
•
Interventions versus controls had a small positive effect on PTSD and none on SUD.
-
•
One of the two studies reporting emotion regulation found a small positive effect.
-
•
Attrition and effects were similar for the subset with high substance use severity.
-
•
The review support recommendations to assess ACE history during addiction treatment.
-
•
The transdiagnostic role of emotion regulation in PTSD/SUD/ACEs needs more research.
Key words: adverse childhood experiences, substance use disorder, posttraumatic stress disorder, emotion regulation, psychological interventions, systematic review
Abbreviations used: ACEs, adverse childhood experiences; PTSD, post-traumatic stress disorder; CPTSD, complex PTSD; SUD, substance use disorder; ER, emotion regulation; EMDR, eye movement desensitisation and reprocessing; RCT, randomised control trial; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SWiM, Synthesis Without Meta-Analysis; DERS, Difficulties in Emotion Regulation Scale; FSP, family and social problems; TREM, Trauma Recovery and Empowerment Model; ATREM, Attachment-informed TREM; SS, Seeking Safety; CBT, Cognitive–Behavioural Therapy; ICBT, Integrated CBT; OR, odds ratio; CI, confidence intervals; M, mean; SD, standard deviation; AEs, adverse events
Abstract
Background
Adverse childhood experiences (ACEs) have long-term effects on adult health, including unresolved trauma and substance use disorder (SUD). There are hypotheses of a mediating role of emotion regulation. This systematic literature review and narrative synthesis assessed the effectiveness of psychological interventions on emotion regulation, PTSD and SUD symptoms.
Methods
Searches were conducted using the Cochrane Handbook for Systematic Reviews methodology. Eligible studies were randomised controlled trials (RCTs) and quasi-experimental psychological interventions published between 2009 and 2019. Study characteristics, results and methodological quality were systematically analysed.
Results
Thirteen studies, including nine RCTs, were selected. Integrated SUD and PTSD treatments consisted of Seeking Safety, exposure-based treatment, Trauma Recovery and Empowerment Model, and integrated cognitive behavioural therapy. Two studies reported emotion regulation. Five studies found a small to medium positive effect size of psychological interventions on PTSD outcomes. Two studies had a small positive effect size on SUD outcomes and two a small negative effect size. Attrition was high across most studies. Characteristics likely to affect the applicability of the review were described.
Conclusion
The review found some evidence of a small inconsistent positive effect of psychological interventions on PTSD outcomes, and no evidence of effect on SUD outcomes. The range of theoretical models was narrow. Overall quality was low with high clinical heterogeneity and missing key information, particularly on emotion regulation, an important transdiagnostic feature. Further research is required to establish interventions that can treat these multiple conditions with a focus on effectiveness, acceptability, and implementation in real life clinical practice.
1. Introduction
1.1. Impact of adverse childhood experiences
Adverse childhood experiences*2 (ACEs) are described as negative events related to emotional, physical or sexual abuse, emotional or physical neglect, domestic violence, parental substance use, mental illness, imprisonment, parental separation and loss of a parent (Korotana et al., 2016). Several studies also include low socioeconomic status, witnessing neighbourhood violence, experiencing racial or ethnic discrimination and intergenerational trauma (McEwen and Gregerson, 2019). ACEs is an important risk factor for premature mortality, risk-taking behaviours, and addictions (Berens et al., 2017; Classen et al., 2011; Kelly-Irving and Delpierre, 2019). However, universal routine screening for ACEs to identify potential risk for certain conditions may stigmatize disadvantaged populations (Finkelhor, 2018; Kelly-Irving and Delpierre, 2019), and focusing on trauma arising from ACEs, without considering other adversities or protective factors, provides a limited approach (McEwen and Gregerson, 2019; Turner et al., 2018).
Exposure to traumatic events, including ACEs, increases the risk of various mental illnesses (Brewin et al., 2017; Danese et al., 2009; Hughes et al., 2017; Korotana et al., 2016), such as post-traumatic stress disorder* (PTSD) and complex PTSD* (CPTSD). Strong associations with problematic alcohol, heroin or other drug use have been found in individuals with multiple ACEs (Afifi et al., 2012; Gerra et al., 2014; Grundmann et al., 2018; Hughes et al., 2017; Leza et al., 2021; Wolff et al., 2016) and it is hypothesised that substance use may be initiated as a protective response and an avoidance coping strategy to self-medicate (Chandler et al., 2018; Korotana et al., 2016). In samples of problematic substance users, the prevalence of PTSD is estimated between 25 and 42% with a strong graded positive association (Driessen et al., 2008; Farrugia et al., 2011; Mills et al., 2006).Compared to individuals with adulthood only trauma, a history of ACEs is associated with longer PTSD, greater risk of CPTSD or re-traumatisation, more severe dependence and more polydrug use histories (Ehring et al., 2014; Farrugia et al., 2011; Hughes et al., 2017; Karatzias et al., 2019).
1.2. Emotion dysregulation
Neurobiological research brings evidence that chronic exposure to stress in early life leads to molecular mechanisms affecting neuroendocrine stress regulation, chronic inflammation, and disruption of central neural networks (Berens et al., 2017; McEwen and Gregerson, 2019). These alterations, possibly linked to epigenetic changes (Nöthling et al., 2020), can impede normal mental development necessary for healthy emotion regulation* (ER) and trigger difficulties in attachment (Ehring et al., 2014; Kober, 2014). Indeed, a history of ACEs is associated with increased avoidance of negative emotions, emotion dysregulation* and psychological distress (Afifi et al., 2012; Cloitre et al., 2008; Gerra et al., 2014; Hughes et al., 2017; Weiss et al., 2013).
Current theories on PTSD suggest that traumatised people may over utilize avoidant ER strategies (expressive suppression) and underutilise effective ER strategies (cognitive reappraisal) (Boden et al., 2013). Neuroimaging literature indicates that PTSD is associated with dysfunction of brain areas (prefrontal cortex, insula, amygdala, hippocampus) involved in fear conditioning or control of emotional responses functioning (Jak et al., 2018). This is supported by a strong association between PTSD and emotion dysregulation (Ehring and Quack, 2010). Specific difficulties in ER (avoidance, nonacceptance of emotions) could exacerbate PTSD symptoms, prevent emotional processing of the trauma and perpetuate a cycle of dysregulation (Burns et al., 2010; Cloitre et al., 2005; Tull et al., 2007).
In continuation of the “self-medication hypothesis”, Kober (2014) proposed a model with substance use seen as a form of ER, particularly to regulate negative emotions and to decrease craving*. Chronic substance use may then lead to a vicious cycle of reduced prefrontal cortex-based ER, more craving and higher relapse rates, and further impaired ER, with difficulties in awareness, expression, and regulation of emotions (Dingle et al., 2018). A recent metanalysis found stronger relations between suppression strategies and substance use in studies with SUD participants compared to participants without SUD (Weiss et al., 2021). Experimental studies demonstrated a significantly higher use of inefficient ER strategies in adults with alcohol use disorders (Petit et al., 2015; Veilleux et al., 2014), and an association between emotion dysregulation and marijuana problems (Vilhena-Churchill and Goldstein, 2013). Wolff (2016) found a relationship between severity of ACEs and SUD, mediated by emotion dysregulation and Gerra (2014) reported a significant link between reaction to stressful emotional stimuli and addiction severity, with a correlation with childhood neglect perception.
Although the nature of the direct and indirect relationships between ER, ACEs, SUD and PTSD/CPTSD needs to be further explored, ER plays a mediating role between severity of ACEs and SUD (Afifi et al., 2012; Gerra et al., 2014; Schäfer et al., 2017; Wolff et al., 2016) and PTSD/CPTSD (Burns et al., 2010; Demir et al., 2020; Korotana et al., 2016; Weiss et al., 2013).
1.3. Effect of psychological interventions
There is evidence of the effectiveness of psychological therapies for PTSD, including trauma-focused cognitive behavioural therapy* (CBT) and eye movement desensitization and reprocessing* (EMDR), but SUD populations are often excluded from studies (NICE, 2018; Roberts et al., 2016). A meta-analysis of psychological interventions for complex PTSD, officially included as a separate diagnosis in 2016 (Karatzias et al., 2019) reported limited evidence of positive effects of individual trauma-focused treatments, EMDR, mindfulness* and interpersonal psychotherapy, albeit smaller effects for patients with ACEs.
Findings that people with comorbid SUD+PTSD have poorer treatment outcomes, higher relapse and treatment dropout rates than people with one condition have led to the development of models addressing both conditions (Back et al., 2009; Farrugia et al., 2011; Najavits and Hien, 2013). They are delivered in a sequential, concurrent, or integrated way (Najavits and Hien, 2013; Torchalla et al., 2012). It is hypothesised that the administration of cognitive training and emotion regulation skills during psychological therapies may induce changes in thoughts and belief systems and could enable patients with comorbid SUD+PTSD to identify and regulate negative emotions. These effects could allow an increased tolerance to traumatic memories and to craving urges, preventing subsequent maladjustment (Boden et al., 2013; Burns et al., 2010; Hien et al., 2017; Jak et al., 2018; Karatzias et al., 2019; Kober, 2014).
1.4. Why is this review important
Considering the burden of concurrent ACEs, SUD and PTSD/CPTSD, for example among people facing homelessness, sexual health, or criminal justice issues, it is essential to understand which interventions are effective and how to deliver them in the most successful way (Ehring et al., 2014; Farrugia et al., 2011; Karatzias et al., 2019; Korotana et al., 2016). Recent literature review findings revealed that only a few studies showed positive effects of psychological therapies on SUD and PTSD symptoms, with low quality of evidence, poor generalisability, and problems with tolerability (Najavits and Hien, 2013; Roberts et al., 2016). Adults with SUD, PTSD and a history of ACEs are underrepresented in reviews, often regarded as difficult to engage (Sin et al., 2017), there is no consensus on the best treatment approaches and more research data are needed. Provision of psychological interventions can be limited because of fear that interventions may increase symptoms (Back et al., 2009; Ehring et al., 2014; Karatzias et al., 2019), although some empirical research does not support this fear (Norman and Hien, 2020; Wagenmans et al., 2018). Effectiveness and acceptability of interventions in population subgroups is needed (Hien et al., 2012; Najavits and Hien, 2013; Roberts et al., 2016; Torchalla et al., 2012). Finally, the growing recognition of the role of ER as a transdiagnostic* feature calls for an examination of emotion regulation outcomes as well (Burns et al., 2010; Ehring et al., 2014; Gratz et al., 2015; Kober, 2014; Sloan et al., 2017).
This article presents a systematic literature review and a narrative synthesis to examine the effectiveness of psychological interventions for comorbid SUD and PTSD in adults with a history of ACEs, with a focus on reported ER outcomes. The research questions were:
-
•
Are psychological interventions more effective than controls to improve SUD and PTSD symptoms and ER in adults with a history of ACEs?
-
•
What contributes to intervention effectiveness in this difficult to treat population?
2. Design and methods
The conduct of the review was done using systematic, explicit, and reproducible methods and following the Cochrane collaboration methodology for systematic reviews (Higgins et al., 2011). A statistical synthesis was not possible because of the clinical diversity of the interventions and a narrative synthesis of quantitative data was performed. The review was conducted following the PRISMA guidelines Moher et al., 2009 with an expansion of the ‘synthesis of results’ items, for which an alternative method of synthesis without meta-analysis was used. Reporting guidelines were followed to enhance transparency, decrease bias and allow examination of differences in results (Campbell et al., 2018; Popay et al., 2006).
2.1. Eligibility criteria
The inclusion criteria were
-
(a)
studies published in English, French, or Spanish in a peer-reviewed journal after 2008.
-
(b)
randomized controlled trial, controlled clinical trial including quasi-experimental studies and before-and-after studies.
-
(c)
study participants were adults with SUD and a diagnosis of PTSD or complex PTSD and a history of childhood adversity.
-
(d)
studies which included the effect and the implementation of any trauma-focused or trauma-informed psychological intervention, in an individual, couple or group format.
-
(e)
psychological interventions compared with treatment as usual, waiting list, no intervention, other psychosocial intervention.
The exclusion criteria were
-
(a)
not experimental studies, surveys, case studies, editorials, reviews.
-
(b)
sample size less than 20 participants.
-
(c)
participants aged under 18 years.
2.1.1. Rationale for the choice of criteria
In addition to randomised control trials (RCTs), non RCTs were considered for inclusion, despite their higher risk of bias, because of the limited number of RCTs including adults with PTSD and SUD or PTSD and ACEs (Ehring et al., 2014; Roberts et al., 2016).
To maximize the breadth of this review, we set a less conservative limit than in other reviews for diagnostic criteria (Roberts et al., 2016), with a threshold of 50% of participants with PTSD and a threshold of 50% of participants with SUD. At least 50% of participants must have reported a history of childhood adversity. Studies where participants had also experienced adult trauma were included but studies specific to adulthood trauma (natural disaster, war, family or domestic violence) were excluded.
Although trauma-focused CBT is considered as a first line treatment for PTSD (NICE, 2018), poorer outcomes in populations with a history of ACEs (Karatzias et al., 2019) call for a consideration of other types of intervention. Treatment settings had no restrictions to include different populations and to acknowledge for cultural, economic and health service systems differences between countries (Schäfer et al., 2018). The search was restricted to contemporary (last 10 years) evidence to assess the most up-to-date research.
2.2. Outcomes of interest
2.2.1. Primary outcomes
The primary outcome of interest was severity of emotion regulation difficulties, using a standardised measure such as the Difficulties in Emotion Regulation Scale (DERS) or the Emotion Regulations Skills Questionnaire.
2.2.2. Secondary outcomes
Secondary outcomes of interest were validated measure of substance use, toxicology or breathalyser test reports; severity of post-traumatic stress symptoms; retention, completion rates, and dose-effects; adverse events; measure of recurrence of trauma; general functioning and quality of life.
2.2.3. Timing of outcome assessment
Outcomes measures were divided into baseline, end of treatment and follow-up post treatment measures if available.
2.3. Search methods and selection strategy
The construction of the research question and the search strategy was based on the “Population, Intervention, Comparison, and Outcome” (PICO) tool (Higgins et al., 2011). Searches were conducted in March and April 2019.
Search terms are described in Supplement 1 Table S.1.
2.3.1. Information sources
The search strategy included electronic searches in four databases, websites and journal hand searches and reference lists searches.
The Cochrane Database of Systematic Reviews was first searched. CINAHL, PubMed and PsycINFO were searched separately on EBSCOhost platform. An additional search was conducted with keywords found in titles of retrieved articles. The International Clinical Trial Registry Platform (ICTRP) was searched with trauma in title and substance use disorder in condition.
Reference lists of relevant systematic reviews, meta-analyses and studies identified in the search were inspected. Searches of the following websites were conducted: European Society for Traumatic Stress Studies (https://www.estss.org), United Kingdom Psychological Trauma Society (http://www.ukpts.co.uk), International Society for Traumatic Stress Studies (http://www.istss.org), Australian psychological Society (https://www.psychology.org.au), International Harm Reduction Association (http://www.ihra.net/) and French Addiction Federation (https://www.federationaddiction.fr).
2.4. Data collection and analysis
2.4.1. Selection of studies
All search results were imported, title and abstracts were single screened, selected full text articles were read and screened for eligibility, with the second reviewer checking a random sample of screened records. Studies were excluded by type of intervention, population (proportion of ACEs history, PTSD or SUD diagnosis less than 50%), sample size (<20), outcomes (no PTSD or substance-related measurements).
2.4.2. Data extraction and management
After verifying inclusion criteria for each study, relevant characteristics were systematically extracted by one reviewer using the Cochrane Collaboration data collection form (Cochrane Effective Practice and Organisation of Care EPOC, 2017). A free version of Review Manager software (The Nordic Cochrane center, The Cochrane Collaboration, 2014) permitted calculations of standardised mean differences between intervention and control groups using study data on ER, PTSD and SUD severity outcomes. For the abstinence outcome, odds ratios were calculated. Double checking was performed.
2.4.3. Assessment of risk of bias
The Cochrane Collaboration's Risk of bias assessment tool was used for selection, performance, detection, and attrition biases and was adapted to non RCT studies (Higgins et al., 2011). The two authors applied the tool to each included study, and any discrepancies in judgements were resolved by discussion to reach consensus. Dropout of intervention (lost to follow-up) is particularly important in SUD populations and a close examination of attrition rates was performed (De Giorgi et al., 2018; Najavits and Hien, 2013). Methodological and topic relevance of individual study designs and focus were appraised according to the applicability of the findings. Implementations issues were examined looking for factors that may affect feasibility, deliverability, and acceptability (Atkins et al., 2011).
2.4.4. Data analysis and synthesis methods
Analysis and synthesis were conducted following the Cochrane Handbook for Systematic Reviews of Interventions (Higgins, 2019) and the Cochrane Consumers and Communication Review Group (Ryan, 2013). Reporting was guided by Synthesis Without Meta-Analysis (SWiM) reporting guideline (Campbell et al., 2020).
-
(a)
The following characteristics were explored in a systematic structured way and descriptive data were collated in tables allowing for visual examination: design, age, sex and number of participants, type of population, type of intervention, duration, completion rate, treatment settings, and delivery format.
-
(b)
Study findings were analysed for each outcome including intervention direction and size of effect. Though it was hypothesised that studies would differ regarding comparator, it was decided to summarize effect estimates for each outcome when five or more RCTs were selected.
-
(c)
Included studies were grouped together and ordered by key characteristics, looking at similarities and differences.
-
(d)
To investigate heterogeneity in the findings, statistical and descriptive data were systematically examined across different groups, trying to identify patterns, and looking for variables that could act as mediators or moderators.
-
(e)
Explicit tables and graphs were designed to allow comparison across studies and to reflect the grouping of the studies.
-
(f)
For the summary of results, the review prioritised studies of more than 100 participants, those with women only participants and those including more severe SUD participants.
-
(g)
The certainty of the evidence was assessed through the following domains: risk of bias, consistency of effects, applicability of the evidence (Atkins et al., 2011; Campbell et al., 2020).
3. Results
3.1. Study selection and characteristics
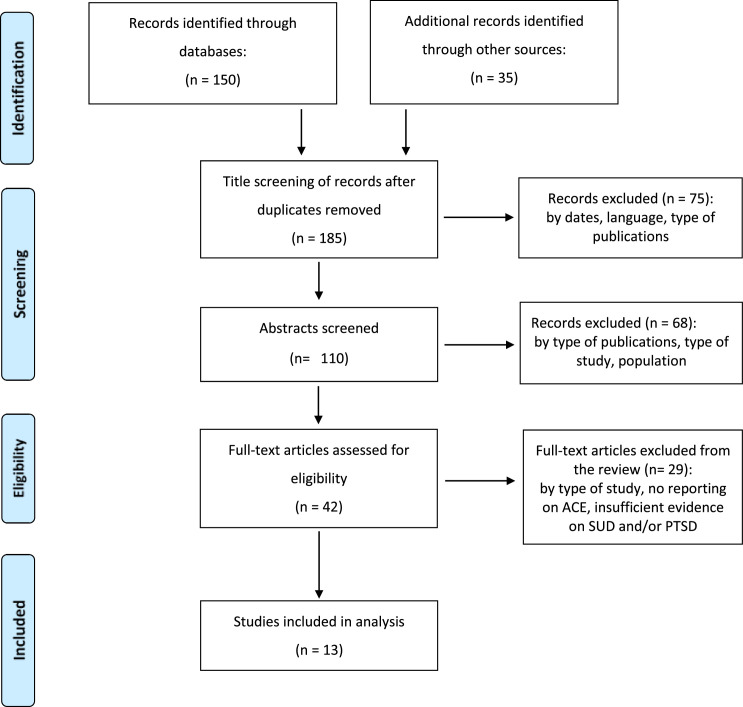
Among 185 identified records, 42 full text articles were assessed for eligibility and 13 studies were included (See Fig. 1: Study flow diagram).
Fig. 1.
Adapted preferred reporting items for systematic reviews and meta-analyses (PRISMA) study flow diagramMoher et al., 2009.
3.2. Sample overview
General characteristics of the included studies are presented in Supplement 2 Table.S.2.
3.2.1. Study design
There were nine RCTs (Coffey et al., 2016; Ghee et al., 2009; Hien et al., 2015; Mills et al., 2012; Morgan-Lopez et al., 2014; Sannibale et al., 2013; Saunders et al., 2016; Schäfer et al., 2019; Wolff et al., 2015), two quasi experimental studies (Fallot et al., 2011; Masin-Moyer et al., 2019) and two before-and-after studies (Benton et al., 2012; Wolff, Nancy et al., 2012), taking place in four developed countries (Australia, Germany, the USA and New Zealand) and were conducted in addiction or mental health out-patient settings (n = 7), addiction residential settings (n = 2), out-patient and residential settings (n = 2), and in prison (n = 2). Sample size ranged from 20 to 353.
3.2.2. Population
The total number of participants was 2189, with 1692 women (77%) and 497 men (33%). Mean age was between 33.7 and 43 years. Sample ethnic composition was heterogeneous in nine studies and not representative of the general population in eight studies (minorities too low or too high). Socioeconomic features were partly described in nine studies (employment and/or income, marital status and/or housing status) with employment rate below 40% in eight studies.
3.2.3. Symptoms severity at baseline
In eight studies, PTSD or subthreshold PTSD was diagnosed in more than 90% of the participants and in ten studies more than 90% of the participants were diagnosed with SUD. Types of substance use (alcohol, drug or both) were not distinguished in seven studies. In one RCT, higher family and social problems (FSP) severity at baseline was associated with higher drug problem and PTSD severity (Saunders et al., 2016). High levels of mental health comorbidities (50% to 82%) were detailed in seven studies
3.2.4. Type of ACEs
All participants reported one or several forms of ACEs (see Supplement 3). Eight studies reported types of ACEs: 26.2% to 72.1% sexual abuse and 15.9% to 76.7% physical abuse.
3.2.5. Type of interventions
Type of interventions are described in Table 1.
Table 1.
Psychological interventions models used in the included studies.
| Psychological interventions | Description | Sessions | Studies using this model |
|---|---|---|---|
| Seeking safety |
|
12 to 16 1 or 2 sessions per week Manualised |
Benton et al., 2012 Ghee et al. (2009) Hien et al. (2015) Morgan-Lopez et al. (2014) Schäfer et al. (2019) Wolff et al. (2012) Wolff et al. (2015) |
| Trauma Recovery and Empowerment Model (TREM) |
|
16 to 33 Weekly Manualised |
Fallot et al., 2011 |
| Attachment informed Trauma Recovery and Empowerment Model (ATREM) |
|
16 Weekly Manualised |
Masin-Moyer et al., 2019 |
| Integrated Cognitive–Behavioural Therapy (ICBT) |
|
12 to 14 Weekly Manualised |
Saunders et al., 2016 |
| Modified Prolonged Exposure (MPE) |
|
9 to 12 Bi-weekly Audiotaped |
Coffey et al. (2016) |
| Concurrent treatment of PTSD and Substance Use Disorders using Prolonged Exposure (COPE) |
|
13 Weekly Manualised |
Mills et al., 2012 |
| Integrated exposure-based CBT for PTSD and AUD |
|
12 Weekly Manualised |
Sannibale et al., 2013 |
No study was found targeting explicitly ER for adults with comorbid SUD+PTSD and a history of ACEs. Thus, specific skills considered important for improving ER (Berking et al., 2008) and the interventions (italic font) incorporating them were explored and are listed below:
-
-
Consciously process emotions, identify and label emotions: ATREM
-
-
Interpret emotion related body sensations correctly: ATREM, high dose SS
-
-
Understand the prompts of emotions: ICBT
-
-
Support oneself in emotionally distressing situations: TREM/ATREM; high dose SS
-
-
Actively modify negative emotions in order to feel better: Individual Modified Prolonged Exposure*; ATREM/TREM; ICBT; high dose SS
-
-
Be resilient to /tolerate negative emotions: SS
-
-
Confront emotionally distressing situations to attain important goals: past-focused (exposure-based) interventions
3.2.6. Comparisons
Comparators were addiction counselling (n = 1), treatment as usual (n= 2), waitlist (n = 2), psychoeducational intervention (n = 1), another psychological intervention (n = 1). For one RCT (Hien et al., 2015) comparing pharmacological and psychological interventions (Seeking Safety) versus control, only methodological and descriptive data could inform the synthesis.
3.2.7. Outcomes
Reported primary and secondary outcomes are described in Supplement 4.
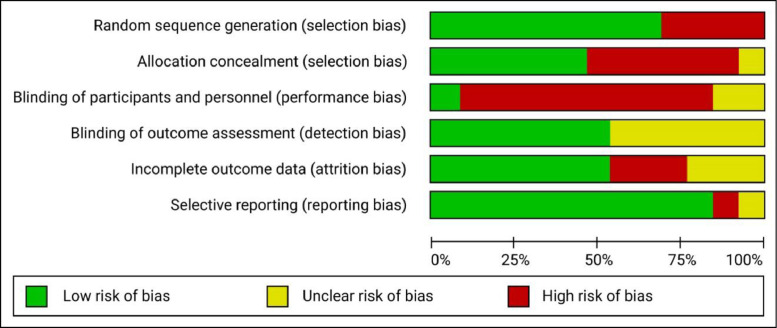
3.3. Quality appraisal
The general risk of bias was moderate to high, with high variability across studies. Graphical representations of the authors judgements were generated within a systematic review software (Review Manager RevMan, 2014) and are presented in Fig. 2. The risk of bias judgements for each RCT are reported in Fig. 3.
Fig. 2.
Risk of bias graph.
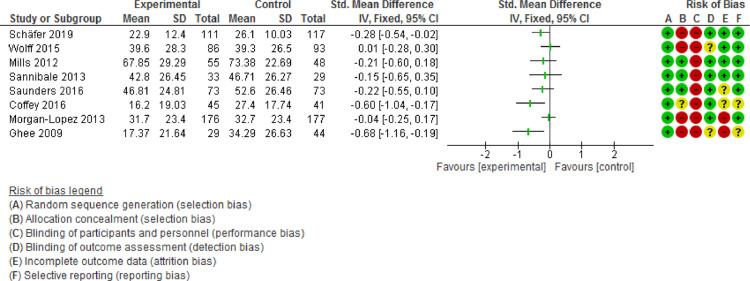
Fig. 3.
Forest plot of comparison: 1 IT, outcome: PTSD Severity post treatment. Ordered by lowest attrition bias and then biggest sample size.
The psychological nature of the intervention rendered a double-blind methodology impossible (Roberts et al., 2016). Blinding of the outcome assessments was reported in seven studies. The presence of active components in control groups (Najavits and Hien, 2013) and the use of self-reported questionnaires to assess ER, PTSD and SUD outcomes in many studies (Grundmann et al., 2018) was a limitation to the data validity.
3.4. Summary of effects of interventions
An overview of the thirteen studies and the effects of interventions for emotion regulation, PTSD and SUD outcomes are reported in Table 2.
Table 2.
Selected characteristics of included studies ordered by type of intervention, study design, study size.
| Refs. Country |
Study design | Format and type of intervention | Participants Substances |
Setting | Sample size | Outcomes | Results1 | Quality Assessment | Comments2 |
|---|---|---|---|---|---|---|---|---|---|
| Intervention: trauma present-focused models, n = 10 | |||||||||
| Morgan-Lopez 2013, USA | RCT | I: Group Seeking Safety C: Women's Health Education Duration: 12 bi-weekly 90 min sessions Delivered by: women accredited therapists in the interventions from 7 sites Monitoring for fidelity to treatment manuel |
Women Alcohol: 56% Opiates: 26% Cocaine: 70% |
Out-patient | 353 Expected sample size |
1) Severity of PTSD symptoms 2) Substance use 3) Abstinence rate |
1) Clinician-Administered PTSD Scale Post treatment I: 31,7 (23,4), C: 32.7 (23,4) Average over FU I: 24.3 (22.1), C: 27.1 (23.4) 2) Days using drugs or alcohol (ASI) Post treatment I: 0.8 (1.8), C: 0.78 (1.8) Average over FU I: 1.4 (2.1), C: 1.5 (2.1) 3) Abstinence rate (alcohol saliva test) Post treatment I: 54%, C: 55% Average over FU I: 46%, C: 43% |
Medium | 29% of assessed patients enrolled Recuitment over 21 months Financial compensation Exclusions: older than 65; active schizophrenia or psychosis; non English speakers; refusing to be video or audiotaped Mandatory enrolment in community treatment program |
| Schäfer et al. (2019), Germany | RCT | I: Group Seeking Safety C: Treatment as usual Duration: 16 weekly 90-minute sessions Delivered by: 39 trained therapists in the interventions Monitoring for fidelity to treatment manuel |
Women Alcohol: 85% Opiates: 21% Cocaine: 28% |
Out-patient | 343 Expected sample size |
1) Emotion regulation difficulties 2) Severity of PTSD symptoms 3) Substance use |
1) Difficulties in Emotion Regulation Scale (DERS) Post treatment I: 95.6 (24.7), C: 109.1 (24.5) 6-month FU I: 92.7 (24.7), C: 107.3 (25.4) 2) PTSD Symptom Scale Interview (PSS-I) Post treatment I: 22.9 (12.4), C: 26.1 (10.3) 6-month FU I: 22.1 (11.5), C: 24.3 (11.4) 3) Addiction Severity Index-lite Post treatment I: 0.22 (0.24), C: 0.30 (0.28) 6-month FU I: 0.24 (0.26), C: 0.27 (0.28) |
Medium | 56 % of assessed patients enrolled Recuitment over 33 months Exclusion: active intra-veinous drug users |
| Saunders et al., 2016, USA | RCT | I: Individual Integrated Cognitive–Behavioral Therapy C: Treatment as usual Duration: 12 weekly 45–50-minute sessions Delivered by: 23 addiction counselors trained in interventions Monitoring for fidelity to treatment manuel |
Women and Men Alcohol: 60% Heroine: 33% Cocaine: 46% |
Out-patient | 284 Expected sample size |
1) Severity of PTSD symptoms 2) Days of substance use 3) Abstinence rate |
1) Clinician-Administered PTSD Scale Post treatment I: 46.81 (24.81), C: 52.6 (26.46) 2) Alcohol Time-Line Follow-Back Interview Post treatment I: 4.95 (12.25), C: 4.92 (16.1) 3) Abstinence rate (drug urine test) Post treatment I: 81.5%, C: 61.2% |
High | 61 % of assessed patients enrolled Recuitment over 25 months Financial compensation Exclusion: attempted suicide in last 30 days Relationships with social problems reported |
| Wolff et al. (2015), USA | RCT | I: Group Seeking Safety C: Waitlist Duration: 28 bi-weekly 90 min sessions Delivered by: 2 therapists trained in the intervention Monitoring for fidelity to treatment manuel |
Men Not specified |
High security prison with 4000 persons |
1793 Expected sample size |
1) Severity of PTSD symptoms | 1) Clinician-Administered PTSD Scale Post treatment I: 39.6 (28.3), C: 39.3 (26.5) |
Medium | 39 % of assessed patients enrolled Recuitment over 20 months Exclusions: non English speakers; on suicide watch in the past 3 months; light sentence prisoners |
| Ghee et al. (2009), USA | RCT | I: Group Seeking Safety booster C: Standard addiction treatment Duration: 6 bi-weekly 90 min sessions Delivered by: not specified |
Women Any drug |
Residential | 1044 Sample lower than expected |
1) Severity of PTSD symptoms 2) Abstinence rate |
1) Modified PTSD Symptom Scale -Self-Report Post treatment I: 17.37 (21.64), C: 34.29 (26.63) 2) Abstinence rate (drug urine test) Post treatment I: 53%, C: 87% |
Low | Exclusions: severe medical conditions; active psychosis; non English speakers Low socioecomic population included No details on ACEs, PTSD and SUD |
| Hien et al., 2015,5 USA | RCT | I: Group Seeking Safety + sertraline C: Seeking Safety + Placebo Duration: 12 weekly 90-minute sessions Delivered by: 8 accreditated therapists, Monitoring for fidelity to treatment manuel |
Women and Men Alcohol: 93% Cocaine: 30% |
Out-patient |
69 Sample lower than expected |
1) Severity of PTSD symptoms 2) Substance use 3) Abstinence rate |
1) Clinician-Administered PTSD Scale 2) Alcohol Time-Line Follow-Back Interview 3) Abstinence rate (drug urine test and alcohol breathalyzer test) |
35 % of assessed patients enrolled Recruitment process lasting 6 years Financial compensation Numerous exclusion criteria |
|
| Fallot et al. (2011), USA | Quasi-experimental study | I: Individual Trauma Recovery and Empowerment Model C: Treatment as usual Duration: 33 weekly 75 min sessions Delivered by: cross-trained community support specialists Monitoring for fidelity to treatment manuel |
Women Alcohol, any drug |
Out-patient | 255 Expected sample size |
1) Severity of PTSD symptoms 2) Substance use |
1) PTSD Symptom Scale (PSS) Post treatment I: 20.77 (11.86), C: 25.68 (12.31) 12-month FU I: 18.41 (10.73), C: 24.32 (12.08) 2) Alcohol severity Index (ASI) Post treatment I: 0.10 (0.18), C: 0.18 (0.25) 12-month FU I: 0.15 (0.25), C: 0.15 (0.21) |
Low | Recuitment over 14 months High psychiatric comorbidities No details on PTSD and SUD diagnosis Urban settings only |
| Masin-Moyer et al., 2019, USA | Quasi-experimental study | I: Group Attachment-informed Trauma Recovery and Empowerment Model (ATREM) C: TREM Duration: 16 weekly 90 min sessions Delivered by: 10 trained female therapists in the interventions |
Women Not specified |
Residential or Out-patient | 1296 Sample lower than expected |
1) Emotion regulation difficulties 2) Severity of PTSD symptoms 3) Substance use |
1) Difficulties in Emotion Regulation Scale (DERS) Mean diff: 0.8 (6.0) 2)PTSD Symptom Scale–Self-Report Mean diff: 2.2 (3.4) 3) Addiction severity Index (ASI) Mean diff: 0.0 |
Low | Recruitment only within community treatment program users Exclusions: active psychosis; being under the influence of drugs or alcohol Low SUD severity Suburban and rural settings |
| Wolff et al. (2012), USA | Before-after study | I: Group Seeking Safety Duration: 14 bi-weekly 90 min sessions Delivered by: 2 trained therapists in the intervention |
Women Not specified |
Adults prison with 850 persons |
111 | 1) Severity of PTSD symptoms | 1) PTSD Checklist (PCL) Before: 38.4 (15.8), After: 29.9 (11.6) |
Low | 70 % of assessed patients enrolled Recuitment over 9 months Exclusions: non English speakers Very high level of psychiatric comorbidities |
| Benton 2011, New Zealand | Before-after study | I: Group Seeking Safety Duration: 12 weekly 90 minutes session Delivered by: one senior counsellor |
Women Alcohol: 75% Opiates: 10% |
Out-patient |
20 | 1) Severity of PTSD symptoms 2) Substance use |
1) Modified PTSD Symptom Scale Self-Report Before: 48.1 (11.8), post treatment: 40.1 (14.3), 6-month FU: 36.5 (13.8) 2) Alcohol Outcome measure Before: 3.3 (4.8), post treatment: 1.7 (2.4), 6-month FU: 11.1 (12.0) |
Low | Exclusion: schizophrenia, active bipolar disorder Low SUD severity Little information on ACE |
| Intervention: trauma past-focused models, n=3 | |||||||||
| Coffey et al. (2016), USA | RCT | I: Individual Modified Prolonged Exposure C: Healthy lifestyles sessions Duration: 9–12 bi-weekly 60 min sessions Delivered by: 8 trained therapists in the interventions Monitoring for fidelity to treatment manuel |
Women and Men Alcohol: 100% Any drug: 98% |
Residential | 126 Expected sample size |
1) Severity of PTSD symptoms 2) Substance use 3) Abstinence rate (6 month FU) |
1) Impact of Event Scale-Revised–Self-Report Post treatment I: 16.20 (19.3), C: 27.40 (17.74) 6-month FU I: 16.45 (18.67), C: 26.5 (19) 2) Percent days abstinent Post treatment I: 97.32 (21,83), C: 97.08 (21.54) 6-month FU I: 94.49 (21.8), C: 93.58 (21.54) 3) Abstinence rate (drug urine test) Post treatment I: 95.2%, C: 87.5% 6-month FU I: 89.5%, C: 87.5% No significant difference between groups |
Medium | 53 % of assessed patients enrolled Recuitment over 3 years Financial compensation Exclusions: acute psychosis or imminent suicide risk; current use of craving reducing or benzodiazepine medication; medical condition limiting cooperation; illiteracy in English Private clinic |
| Mills et al., 2012, Australia | RCT | I: Individual COPE Prolonged Exposure C: Treatment as usual Duration: 13 weekly 90-minute sessions Delivered by: 2 clinical psychologists Monitoring for fidelity to treatment manuel |
Women and Men Polysubstance use History of injected drug: 80% |
Residential or Out-patient |
103 Sample lower than expected |
1) Severity of PTSD symptoms 2) Severity of substance dependence |
1) Clinician-Administered PTSD Scale Post treatment I: 67.85 (29.29), C: 73.38 (22.69) 9-month FU I: 52.89 (33.92), C: 67.23 (27.62) 2) Composite International Diagnostic Interview Post treatment I: 2.49 (2.74), C: 3.41 (2.44) 9-month FU I: 2.27 (2.55), C: 2.98 (2.45) |
High | 31 % of assessed patients enrolled Recuitment over 26 months Financial compensation Exclusion: not fluent in English; history of self harm in past 6 months Median age at first trauma: 8 years |
| Sannibale et al., 2013, Australia | RCT | I: Individual Integrated Exposure-Based CBT C: Alcohol support Duration: 12 weekly 90-minute sessions Delivered by: 4 trained clinical psychologists in the interventions Monitoring for fidelity to treatment manuel |
Women and Men Alcohol: 100% |
Out-patient |
62 Sample lower than expected |
1) Severity of PTSD symptoms 2) Substance use |
1) Clinician-Administered PTSD Scale Post treatment I: 42.80 (26.45), C: 46.71 (26.27) 9-month FU I: 43.3 (28.25), C: 41.19 (34.17) 2) Drinks per Drinking Days (TLFB) Post treatment I: 7.47 (5.22), C: 8.74 (9.51) 9-month FU I: 6.97 (4.16), C: 7.9 (6.24) |
High | 42 % of assessed patients enrolled Recuitment over 2 years Exclusions: severe substance dependence; severe suicide risks; limited English comprehension 23% of participants with sexual/physical ACEs |
In bold: significant difference favouring intervention; in italic: significant difference favouring control
Recruitment, exclusions, severity of diagnosis, settings
Random assignement sample, total participants 230
Results on 86 (study completers)
Results of the effect of intervention not included in the review
Results on 69 (study completers)
Abbreviations: RCT: Randomised Controlled Trial; I: Intervention; C: Control; PTSD: Posttraumatic Stress Disorder; SUD: Substance Use Disorder; ACE: Adverse Childhood Event; FU: Follow-up; CBT: Cognitive Behavioural Therapy; COPE: Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure; ASI: Alcohol Severity Index; TLFB:TIme-Line Follow-Back.
3.4.1. Primary outcome
The RCT reporting emotion regulation found a significant positive effect of Seeking Safety intervention compared to control, with a moderate effect size (−0.54 [−0.81, −0.28]) post treatment and a small effect size (−0.41 [−0.71, −0.10]) at 6-month follow-up (Schäfer et al., 2019). The non RCT reporting emotion regulation found no difference between intervention and control and a significant pre- to post-treatment decrease of difficulties in emotional regulation scales for both groups (no follow-up measures): Mean difference = - 18.0, Standard Deviation (SD) = 23.8 for ATREM and Mean difference = -18.8, SD = 26.4 for TREM (Masin-Moyer et al., 2019).
3.4.2. Secondary outcomes
3.4.2.1. PTSD
Effects of intervention on PTSD were reported for twelve studies. Eight were RCTs and enrolled 1230 patients, four used individual interventions (Integrated CBT and exposure-based), four used SS group interventions. Effect estimates for PTSD outcomes and risk of bias are reported in Fig. 3 (post treatment). Three RCTs (Coffey et al., 2016; Ghee et al., 2009; Mills et al., 2012) found a positive effect of the interventions with a small to medium effect size and five found no difference between intervention and control groups. In one non RCT (Benton et al., 2012), the Modified PTSD Symptom-Self Reported score (119-point scale), was 11.6 points better after 6-month follow up (M = 36.5, SD = 13.8) than before (M = 48.1, SD = 11.8; t = 2.40, df = 16, p = 0.029). In another non RCT (Wolff et al., 2012), the PTSD Checklist score (87-point scale) was 8.5 points better after (M = 29.9, SD = 11.6) than before (M = 38.4, SD = 15.8; t = 2, p < 0.01) for the whole sample (n = 74) and 9.2 points better after than before for the subgroup (n = 61) with serious mental disorders. There were no group differences in the two quasi experimental studies.
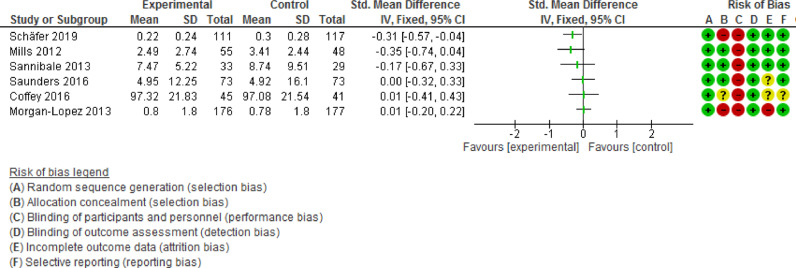
SUD: Effects of intervention on SUD were reported for ten studies. Effect estimates for SUD outcomes are reported in Fig. 4 (post treatment). One non RCT found a small positive significant effect on the Addiction Severity Index score (group by time interaction) (Fallot et al., 2011) and another (Benton et al., 2012) found an increase in substance use at 6 months follow-up with a significant difference on the Alcohol and Drug Outcome Measure score: before (M = 48.1, SD=11.8), after (M = 36.5, SD = 13.8); t = 2.40, df = 16, p = 0.029). Abstinence measured by toxicologic analysis worsened post-treatment for one RCT (odds ratio (OR) = 0.17, confidence intervals (CI) 95: 0.03, 1.01) (Ghee et al., 2009) and improved for one (OR = 2.68, CI95: 1.11, 6.49) (Saunders et al., 2016).
Fig. 4.
Forest plot of comparison: 1 IT, outcome: SUD severity post treatment. Ordered by lowest attrition bias and then biggest sample size.
Retention: In two studies, attrition analysis revealed higher SUD severity at baseline for participants present at follow-up compared to those not attending follow-up: 52.7% (n = 109) versus 31.8% (n = 14) (χ2 (I) = 6.31, p = 0.01) for alcohol problems (Fallot et al., 2011); positive toxicology screens for 25.1% (n = 51) versus 13% (n = 10) (χ2 (I) = 4.83, p = 0.05) (Saunders et al., 2016); in (Mills et al., 2012), participants in follow-up were more likely to have experienced rape than those who did not: 73.2% (60) vs 47.6% (10); OR, 3.00 [95% CI, 1.12 to 8.04] at 3-month and 74.0% (57) vs 50.0% (13); OR, 2.85 [95% CI, 1.13 to 7.17] at 9-month.
Treatment completion: Treatment completion rates ranged from 32.7% (Schäfer et al., 2019) to 100%. (Benton et al., 2012). Dropout rate ranged from 22 to 60% in eleven studies. Minimum dose analyses in one RCT (Schäfer et al., 2019) found a greater improvement in PTSD and SUD outcomes for participants attending at least eight out of 14 sessions of Seeking Safety compared to controls. In (Coffey et al., 2016), treatment completers (attending 8 out of 12 sessions) realised significantly larger PTSD treatment gains compared to non-completers. One non RCT (Wolff et al., 2012) simply stated that ‘change score for the primary outcomes were not correlated with the number of group sessions attended’ without reporting results.
Adverse events: No adverse events (AEs) were found in one RCT reporting them (Saunders et al., 2016) (n=284), three were mentioned without details in another (Hien et al., 2015) (n=69); three, including suicide risk, were reported in (Sannibale et al., 2013); in Morgan-Lopez (Killeen et al., 2008; Morgan-Lopez et al., 2014) (n= 353), increased PTSD, depression or substance use were reported in 20% of the treatment group versus 14% of the control group, with a positive association with the number of sessions attended; AEs were also reported following the screening assessment by 15% (19/62) of the participants who dropped out before starting and by 7% (19/291) of the participants who started the intervention; in (Schäfer et al., 2019), the incidence rate was 4.17 severe AEs per 100 person months, most frequently increases in suicidal thoughts, without significant differences between groups. One non RCT (Wolff et al., 2012) simply stated that ‘there were no adverse events associated with any aspect of the intervention’.
Recurrence of trauma and quality of life: There was no significant difference for recurrence of trauma and quality of life (Lifetime and Current Trauma History) between groups in one study (Fallot et al., 2011).
3.4.3. Subgroup analysis
ER, PTSD, SUD and treatment completion outcomes were investigated according to the characteristics of the studies and to identify potential subgroups (Popay et al., 2006). In one RCT (Saunders et al., 2016), baseline FSP severity was not predictive of treatment outcomes but improvement or deterioration in FSP during the intervention were associated with improvement or deterioration in PTSD and alcohol use, not drug use.
No pattern emerged when grouping studies by sex, countries, ethnicity, type of substance used, level or type of ACEs, severity of PTSD at baseline. Relevant findings reported with respect to synthesis of direction of effect, using vote counting, are outlined below.
Age: For PTSD outcomes, there were positive outcomes for four of the five studies with younger participants (mean age of 36 years or less) compared to only one of seven studies with older participants; and for none of the five larger samples (more than 200) compared to five of the seven smaller (129 or less).
For SUD outcomes, there were positive outcomes for one of four studies with younger participants (mean age of 36 years or less) compared to one of six studies with older participants; and for two of four larger samples compared to none of the six smaller.
Women only studies: Among the seven studies with women only participants (n = 1315), six were group format with no exposure-based treatment, and the level of substance use and overall quality were lower. In the four women only studies which reported ACEs type, there was a high proportion of childhood sexual (more than 64%) and physical (more than 39%) trauma among participants.
Highest SUD severity: The six studies with the highest SUD severity at baseline (Coffey et al., 2016; Fallot et al., 2011; Mills et al., 2012; Sannibale et al., 2013; Saunders et al., 2016; Schäfer et al., 2019), included 254 male and 919 female participants and used four different intervention models, including past-focused models for three of them. One study had a positive effect on ER outcomes, two on PTSD outcomes and two on SUD outcomes. Between 22 and 34% of participants were lost to follow-up.
Type of interventions: For ER outcomes, there were positive outcomes for one of the two group format studies. For models of intervention, there were positive outcomes for the study with SS, and no difference between ATREM and TREM in the other one.
For PTSD outcomes, there were positive outcomes for two of five individual format studies and for three of seven group format studies. For models of intervention, there were positive outcomes for three of the six studies with SS, two of the three with exposure-based treatment, none for IT, ATREM or TREM.
For SUD outcomes, there were positive outcomes for two of five individual format and none of five group format studies. For models, there were positive outcomes for the one with IT, the one for TREM, none for exposure-based treatment and negative outcomes for two of the four with SS.
Attendance: Four of five studies with a higher dropout rate were group interventions. Studies lasting more than three months had an average session attendance of less than 60%. Residential and prison studies had higher completion rates (more than 75% of sessions completed) than studies conducted in outpatient settings.
3.5. Applicability
Characteristics likely to affect the applicability of the review are reported in Table 2 including the comment's column.
3.5.1. Population
Most of the studies excluded populations with medical or cognitive impairment limiting cooperation. Four studies excluded current substance users (Hien et al., 2015; Masin-Moyer et al., 2019; Sannibale et al., 2013; Schäfer et al., 2019) and one excluded craving reducing or benzodiazepine medication users (Coffey et al., 2016). Few studies recruited participants that were not users of community treatment programs. All the studies had language-based restrictions and none of them mentioned translators or multilanguage therapists nor the availability of translated manuals. No studies reported data on lesbian, gay, bisexual, transgender, queer or similar (LGBTQ+) populations.
3.5.2. Intervention
Recruitment was slow and final sample size lower than expected in five out of eleven studies reporting it. Three studies modified conventional interventions, delivering briefer sessions to facilitate implementation of exposure-based therapy in SUD treatment settings (Coffey 2016), halving the number of sessions to render the treatment model feasible given time and financial constraints (Hien et al., 2009; Morgan-Lopez et al., 2014) or condensing integrated treatment to fit within brief residential programs (Ghee et al., 2009). No cost analysis was made. Financial compensations were given in five studies, summing up to 200–400 dollars per participants. One study reported that daily physical presence of the research staff was crucial for implementation (Wolff et al., 2015). Participant satisfaction was high (more than 75%) in the three studies reporting it: the two prison-setting studies (Wolff et al., 2015; Wolff et al., 2012) using the end of treatment questionnaire, and in the New Zealander study (Benton et al., 2012) using the treatment perception questionnaire. Exploration of group cohesion found a feeling of trust and safety during the group discussions (Wolff et al., 2015).
3.5.3. Comparisons
In most studies control groups had potential active “ingredients”: support from staff or participants, body-centered exercises, nonspecific psychotherapy components, social skills training, pharmacotherapy.
3.5.4. Outcomes
One study only performed subgroup analysis based on sociodemographic characteristics (Wolff et al., 2012) and none on type of substance use.
3.5.5. Settings
Settings were predominantly in urban or suburban locations and within public health systems. Possible exclusion of disadvantaged populations because of financial cost of private clinics was reported in one study (Coffey et al., 2016).
4. Discussion
4.1. Statement of principal findings
The treatment of post-traumatic stress disorders (PTSD/CPTSD) and substance use disorders (SUD) in adults who have a history of adverse childhood experiences (ACEs) represents a considerable clinical and public health challenge. This systematic review and narrative analysis examined evidence from RCTs and quasi-experimental studies of psychological interventions with a focus on emotion regulation (ER) outcomes. Among the thirteen included studies, the two most recent assessed this primary outcome, using group interventions and including 472 women. Beneficial effect was found in one RCT, without improvement of PTSD and SUD. Nonetheless, there is a growing body of evidence that difficulties in ER mediate relationships between ACEs, SUD and PTSD/CPTSD (Burns et al., 2010; Demir et al., 2020; Ehring and Quack, 2010; Karatzias et al., 2018; Kober, 2014; Wolff et al., 2016). Furthermore, research indicates that ER difficulties could be a good intervention target for patients with high levels of psychological complexity (Gratz et al., 2015; Sloan et al., 2017) and that ER strength (anger management and general emotion regulation capacity) could be a sensitive predictor of differential outcome (Cloitre et al., 2016).
There were mitigated effects of interventions for PTSD outcomes compared to control, with three of the models used (Seeking Safety, exposure-based and integrated cognitive-behavioural therapy) demonstrating small positive effects with low-quality evidence. PTSD severity did not increase. This is in line with the mixed findings from the literature for integrated treatment (Torchalla et al., 2012), Seeking Safety (Najavits & Hien, 2013) and exposure-based (Roberts et al., 2016).
The failure of most interventions to improve SUD outcomes compared to control could be expected as relapse is common during SUD treatments (Kober, 2014). Additionally, the experimental nature of interventions limited the possibility of therapeutic alliance* (De Giorgi et al., 2018). No study improved both PTSD and SUD outcomes compared to control, which confirms the challenge of treating this complex comorbid population (Najavits and Hien, 2013; Roberts et al., 2016).
Presence of follow up assessments, monitoring of fidelity to the treatment manuals, and report of effect sizes in most of the studies indicate some improvement over past methodological weaknesses (Cloitre et al., 2016; Najavits and Hien, 2013). High attrition rates described are in line with other reviews (Najavits and Hien, 2013; Torchalla et al., 2012). Studies with individual format, longer duration interventions and outpatient settings had higher attrition rates.
Examination of population-based characteristics revealed that younger participants reported better PTSD outcomes. It may be hypothesized that older people with a longer history of trauma symptoms/substance use and potential revictimization are more resistant to treatment (Grundmann et al., 2018). The different characteristics found in the women-only studies call for a gendered approach toward PTSD and a history of ACEs (Rasmussen et al., 2018). Similar dropout rates and non-inferior effects for the subset with highest substance use severity support recommendations not to delay psychological interventions for current substance users (Classen et al., 2011; Karatzias et al., 2019; Roberts et al., 2016).
4.2. Limitations of the study
Although this review increases our knowledge on the treatment of PTSD/CPTSD and SUD in adults who have a history of ACEs, some limitations must be considered. First, consistent with a recent systematic review (Roberts et al., 2016), the high variability of settings, controls, measurements, content, and format of programmes delivered, and population characteristics, affected the comparability of the studies and the consistency of results (Higgins et al., 2011). The insufficient details about substance use could also affect these results (Torchalla et al., 2012). The severity of reported adverse effects and the small number of studies reporting them raise questions about assumptions of well tolerated interventions (Najavits and Hien, 2013; Roberts et al., 2016) and warrant strong considerations of safety procedures in designing intervention studies (Vrana et al., 2017).
Second, the range of theoretical models was narrow, based on psychoeducational cognitive behavioural therapies. Studies of other models such as couple therapy (McCrady et al., 2016) or EMDR (Perez-Dandieu and Tapia, 2014) were not found for the target population, mindfulness meditation being included in an on-going study (Vrana et al., 2017). Effects on SUD outcomes of self-help groups from various cultural backgrounds, like the 12-Step approach or the “healing circles” (Mehl-Madrona and Mainguy, 2014), have rarely been published (De Giorgi et al., 2018). Moving forward from theoretical debates on the advantage of one model, programs combining interventions from multiple models (Karatzias et al., 2018; Norton and Paulus, 2015; Roberts et al., 2016) need further development.
Third, overall quality of the studies was low, and risk of bias was high or unclear in most domains. Power in most studies was reduced by difficulties in recruitment, smaller than expected sample sizes and large dropout rates, already reported in other reviews (Najavits and Hien, 2013; Roberts et al., 2016).
Fourth, key information was missing. Patient-relevant outcomes such as difficulties in emotion regulation, general functioning or quality of life were rarely assessed. Despite the potential role of social support, family, and interpersonal relationships on treatment outcomes (Cloitre et al., 2016; Ehring et al., 2014; Kim et al., 2010), insufficient reporting of socioeconomic details impeded the identification of contextual barriers and facilitators of the interventions. Thorough examination of the studies characteristics revealed little information on dose effect and no relevant information on quality of the participation, two potential moderators described in the literature (Hien et al., 2012). Emotional abuse, an important and understudied area (Burns et al., 2010), was rarely mentioned.
Acceptability, accessibility, and reach were poorly studied, and overall, there was little information related to implementation issues (Atkins et al., 2011). Several questions remained unanswered about which PTSD interventions work best, for who (populations with specific needs, people living in unstable circumstances) (Nosè et al., 2017), when (duration and frequency) (Korotana et al., 2016), how (format, content, group composition) (Najavits and Hien, 2013) and in what contexts (socioeconomic) (Kim et al., 2010).
Finally, the application of rigorous scientific methods, attention to transparency reporting and investigation of heterogeneity could assure robustness of the review findings, but some limitations could not be avoided. The review was not registered. Although literature searches included various individual adversity types, studies using a different nomenclature for ACEs may have been missed (McKay and Clarke, 2021). Double-checking and thorough inspection will have minimised potential biases in data extraction and analysis, particularly for studies using complex designs or statistical tools (Higgins et al., 2011). The specific focus on ER, a common feature across PTSD and SUD and ACEs, and an important target for treatment (Dingle et al., 2018; Gratz et al., 2015; Sloan et al., 2017; Wagenmans et al., 2018) overlooked the limited data available. The review found studies from only four developed countries, limiting cultural adaptability and applicability (Schäfer et al., 2018).
5. Conclusion
In terms of implications for practice, the multiple types of ACEs underscored in this review support recommendations to assess ACEs history during addiction treatment and to deliver trauma-informed care (Afifi et al., 2012; Farrugia et al., 2011; Grundmann et al., 2018; Leza et al., 2021). Survivors of childhood abuse who develop CPTSD show emotion dysregulation and disturbances in self-organization which impact their social skills and increases the risk of conflict with services providers (Ehring et al., 2014; Wagenmans et al., 2018).
In terms of implication for policy, the expected benefits of current psychological interventions need to be balanced with their associated costs. The organization of treatment requires resources and an available competent workforce, with clear guidance to help clinicians address common challenges and deliver successful interventions (Back et al., 2009). Training to assess and respond to ACEs among SUD patients is necessary to help the dissemination of these treatments (Schäfer et al., 2017).
Further examination of ER as one mechanism and predictor of change is recommended to increase evidence for treatments addressing complex comorbidities at the same time (Gratz et al., 2015; Sloan et al., 2017) and to apply flexibly multiple modalities of evidence-based strategies, tailored to individual emotional experiences (Kring and Sloan, 2009; Norton and Paulus, 2015). More research is needed to identify sociodemographic factors associated with intervention engagement and attrition. Designing future studies with acceptability and deliverability in mind could better inform the implementation of interventions at scale. In the context of health and social inequalities, interventions to improve difficulties in emotion regulation could enable better engagement with health and social care services, reduce rates of harm and improve health.
CRediT authorship contribution statement
Genevieve Molina: Visualization, Formal analysis, Writing – original draft. Anne Whittaker: Visualization, Formal analysis, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Role of funding source
Nothing declared.
Footnotes
Words marked with an * are defined in the Glossary in Supplement 5
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2022.100028.
Contributor Information
Genevieve Molina, Email: xtofgene@orange.fr.
Anne Whittaker, Email: Anne.Whittaker@stir.ac.uk.
Appendix. Supplementary materials
References
- Afifi T.O., Henriksen C.A., Asmundson G.J.G., Sareen J. Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Can. J. Psychiatry. 2012;57(11):677–686. doi: 10.1177/070674371205701105. [DOI] [PubMed] [Google Scholar]
- Atkins, et al. Assessing applicability when comparing medical interventions: AHRQ and the effective health care program. J. Clin. Epidemiol. 2011;64(11):1198–1207. doi: 10.1016/j.jclinepi.2010.11.021. [DOI] [PubMed] [Google Scholar]
- Back S.E., Waldrop A.E., Brady K.T. Treatment challenges associated with comorbid substance use and posttraumatic stress disorder: clinicians' perspectives. Am. J. Addict. 2009;18(1):15–20. doi: 10.1080/10550490802545141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benton D.M., Deering D.E.A., Adamson S.J. Treating co-occurring posttraumatic stress disorder and substance use disorders in an outpatient setting in New Zealand. N. Z. J. Psychol. 2012;41(1):30–37. [Google Scholar]
- Berens A.E., Jensen S.K.G., Nelson C.A. Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 2017;15(1):135. doi: 10.1186/s12916-017-0895-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M., Wupperman P., Reichardt A., Pejic T., Dippel A., Znoj H. Emotion-regulation skills as a treatment target in psychotherapy. Behav. Res. Ther. 2008;46(11):1230–1237. doi: 10.1016/j.brat.2008.08.005. [DOI] [PubMed] [Google Scholar]
- Boden, et al. Emotion regulation and posttraumatic stress disorder: a prospective investigation. J. Soc. Clin. Psychol. 2013;32(3):296–314. doi: 10.1521/jscp.2013.32.3.296. [DOI] [Google Scholar]
- Brewin C.R., Cloitre M., Hyland P., Shevlin M., Maercker A., Bryant R.A., Humayun A., Jones L.M., Kagee A., Rousseau C., Somasundaram D., Suzuki Y., Wessely S., van Ommeren M., Reed G.M. A review of current evidence regarding the ICD-11 proposals for diagnosing PTSD and complex PTSD. Clin. Psychol. Rev. 2017;58:1–15. doi: 10.1016/j.cpr.2017.09.001. [DOI] [PubMed] [Google Scholar]
- Burns E.E., Jackson J.L., Harding H.G. Child maltreatment, emotion regulation, and posttraumatic stress: the impact of emotional abuse. J. Aggress. Maltreatment Trauma. 2010;19(8):801–819. doi: 10.1080/10926771.2010.522947. [DOI] [Google Scholar]
- Campbell M., Katikireddi S.V., Sowden A., McKenzie J.E., Thomson H. Improving conduct and reporting of narrative synthesis of quantitative data (ICONS-Quant): protocol for a mixed methods study to develop a reporting guideline. BMJ Open. 2018;8(2) doi: 10.1136/bmjopen-2017-020064. [DOI] [Google Scholar]
- Campbell M., McKenzie J.E., Sowden A., Katikireddi S.V., Brennan S.E., Ellis S., Hartmann-Boyce J., Ryan R., Shepperd S., Thomas J., Welch V., Thomson H. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler G.E., Kalmakis K.A., Murtha T. Screening adults with substance use disorder for adverse childhood experiences. J. Addict. Nurs. 2018;29(3):172–178. doi: 10.1097/JAN.0000000000000233. (Lippincott Williams & Wilkins) [DOI] [PubMed] [Google Scholar]
- Classen C.C., Palesh O.G., Cavanaugh C.E., Koopman C., Kaupp J.W., Kraemer H.C., Aggarwal R., Spiegel D. A comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual abuse: a randomized controlled trial. Psychol. Trauma Theory Res. Pract. Policy. 2011;3(1):84–93. doi: 10.1037/a0020096. [DOI] [Google Scholar]
- Cloitre M., Miranda R., Stovall-McClough K.C., Han H. Beyond PTSD: Emotion regulation and interpersonal problems as predictors of functional impairment in survivors of childhood abuse. Behav. Ther. 2005;36(2):119–124. doi: 10.1016/S0005-7894(05)80060-7. [DOI] [Google Scholar]
- Cloitre M., Petkova E., Su Z., Weiss B.J. Patient characteristics as a moderator of posttraumatic stress disorder treatment outcome: combining symptom burden and strengths. BJPsych Open. 2016;2(2):101–106. doi: 10.1192/bjpo.bp.115.000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M., Stovall-McClough C., Zorbas P., Charuvastra A. Attachment organization, emotion regulation, and expectations of support in a clinical sample of women with childhood abuse histories. J. Trauma Stress. 2008;21(3):282–289. doi: 10.1002/jts.20339. [DOI] [PubMed] [Google Scholar]
- Coffey S.F., Schumacher J.A., Nosen E., Littlefield A.K., Henslee A.M., Lappen A., Stasiewicz P.R. Trauma-focused exposure therapy for chronic posttraumatic stress disorder in alcohol and drug dependent patients: a randomized controlled trial. Psychol. Addict. Behav. 2016;30(7):778–790. doi: 10.1037/adb0000201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A., Moffitt T.E., Harrington H., Milne B.J., Polanczyk G., Pariante C.M., Poulton R., Caspi A. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatr. Adolesc. Med. 2009;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Giorgi R., Cassar C., Loreto D'alò G., Ciabattini M., Minozzi S., Economou A., Tambelli R., Lucchese F., Saulle R., Amato L., Janiri L., De Crescenzo F. Psychosocial interventions in stimulant use disorders: a systematic review and qualitative synthesis of randomized controlled trials. Riv. Di Psichiatr. 2018;53(5):233–255. doi: 10.1708/3000.30003. [DOI] [PubMed] [Google Scholar]
- Demir Z., Böge K., Fan Y., Hartling C., Harb M.R., Hahn E., Seybold J., Bajbouj M. The role of emotion regulation as a mediator between early life stress and posttraumatic stress disorder, depression and anxiety in Syrian refugees. Transl. Psychiatry. 2020;10(1):371. doi: 10.1038/s41398-020-01062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingle G.A., Neves D.D.C., Alhadad S.S.J., Hides L. Individual and interpersonal emotion regulation among adults with substance use disorders and matched controls. Br. J. Clin. Psychol. 2018;57(2):186–202. doi: 10.1111/bjc.12168. [DOI] [PubMed] [Google Scholar]
- Driessen M., Schulte S., Luedecke C., Schaefer I., Sutmann F., Ohlmeier M., Kemper U., Koesters G., Chodzinski C., Schneider U., Broese T., Dette C., Havemann-Reinicke U. Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcohol. Clin. Exp. Res. 2008;32(3):481–488. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Ehring T., Quack D. Emotion regulation difficulties in trauma survivors: the role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41(4):587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Ehring T., Welboren R., Morina N., Wicherts J.M., Freitag J., Emmelkamp P.M.G. Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clin. Psychol. Rev. 2014;34(8):645–657. doi: 10.1016/j.cpr.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Fallot R.D., McHugo G.J., Harris M., Xie H. The trauma recovery and empowerment model: a quasi-experimental effectiveness study. J. Dual Diagn. 2011;7(1):74–89. doi: 10.1080/15504263.2011.566056. [DOI] [PubMed] [Google Scholar]
- Farrugia P.L., Mills K.L., Barrett E., Back S.E., Teesson M., Baker A., Sannibale C., Hopwood S., Rosenfeld J., Merz S., Brady K.T. Childhood trauma among individuals with co-morbid substance use and post traumatic stress disorder. Mental Health Subst. Use Dual Diagn. 2011;4(4):314–326. doi: 10.1080/17523281.2011.598462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D. Screening for adverse childhood experiences (ACEs): cautions and suggestions. Child Abuse Negl. 2018;85:174–179. doi: 10.1016/j.chiabu.2017.07.016. [DOI] [PubMed] [Google Scholar]
- Gerra G., Somaini L., Manfredini M., Raggi M.A., Saracino M.A., Amore M., Leonardi C., Cortese E., Donnini C. Dysregulated responses to emotions among abstinent heroin users: Correlation with childhood neglect and addiction severity. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2014;48:220–228. doi: 10.1016/j.pnpbp.2013.10.011. [DOI] [PubMed] [Google Scholar]
- Ghee A.C., Bolling L.C., Johnson C.S. Adult survivors of child sexual abuse. The efficacy of a condensed Seeking Safety intervention for women in residential chemical dependence treatment at 30 days posttreatment. J. Child Sex. Abus. 2009;18(5):475–488. doi: 10.1080/10538710903183287. [DOI] [PubMed] [Google Scholar]
- Gratz K.L., Weiss N.H., Tull M.T. Examining emotion regulation as an outcome, mechanism, or target of psychological treatments. Curr. Opin. Psychol. 2015;3:85–90. doi: 10.1016/j.copsyc.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundmann J., Lincoln T.M., Lüdecke D., Bong S., Schulte B., Verthein U., Schäfer I. Traumatic experiences, revictimization and posttraumatic stress disorder in German inpatients treated for alcohol dependence. Subst. Use Misuse. 2018;53(4):677–685. doi: 10.1080/10826084.2017.1361997. [DOI] [PubMed] [Google Scholar]
- Hien D.A., Levin F.R., Ruglass L.M., López-Castro T., Papini S., Hu M., Cohen L.R., Herron A. Combining seeking safety with sertraline for PTSD and alcohol use disorders: a randomized controlled trial. J. Consult. Clin. Psychol. 2015;83(2):359–369. doi: 10.1037/a0038719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D.A., Lopez-Castro T., Papini S., Gorman B., Ruglass L.M. Emotion dysregulation moderates the effect of cognitive behavior therapy with prolonged exposure for co-occurring PTSD and substance use disorders. J. Anxiety Disord. 2017;52:53–61. doi: 10.1016/j.janxdis.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D.A., Morgan-Lopez A., Campbell A.N.C., Saavedra L.M., Wu E., Cohen L., Ruglass L., Nunes E.V. Attendance and substance use outcomes for the seeking safety program: sometimes less is more. J. Consult. Clin. Psychol. 2012;80(1):29–42. doi: 10.1037/a0026361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien D.A., Wells E.A., Jiang H., Suarez-Morales L., Campbell A.N.C., Cohen L.R., Miele G.M., Killeen T., Brigham G.S., Zhang Y., Hansen C., Hodgkins C., Hatch-Maillette M., Brown C., Kulaga A., Kristman-Valente A., Chu M., Sage R., Robinson J.A., Nunes E.V. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J. Consult. Clin. Psychol. 2009;77(4):607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M.J., Welch V.A. Cochrane; 2019. Cochrane Handbook for Systematic Reviews of Interventions.https://www.training.cochrane.org/handbook version 6.0 (2019) Accessed July 2019. [Google Scholar]
- Higgins J.P.T., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A.C. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ: Br. Med. J. 2011;343(7829):1–9. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C., Jones L., Dunne M.P. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet.Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Cochrane Effective Practice and Organisation of Care (EPOC), 2017. Good practice data extraction form. EPOC resources for review authors 2017.https://epoc.cochrane.org/epoc-resources-review-authors. Accessed September 2020
- Jak A.J., Crocker L.D., Aupperle R.L., Clausen A., Bomyea J. Neurocognition in PTSD: treatment insights and implications. Curr. Top. Behav. Neurosci. 2018;38:93–116. doi: 10.1007/7854_2016_62. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Murphy P., Cloitre M., Bisson J., Roberts N., Shevlin M., Hyland P., Maercker A., Ben-Ezra M., Coventry P., Mason-Roberts S., Bradley A., Hutton P. Psychological interventions for icd-11 complex ptsd symptoms: Systematic review and meta-analysis. Psychol. Med. 2019 doi: 10.1017/S0033291719000436. [DOI] [PubMed] [Google Scholar]
- Karatzias T., Shevlin M., Hyland P., Brewin C.R., Cloitre M., Bradley A., Kitchiner N.J., Jumbe S., Bisson J.I., Roberts N.P. The role of negative cognitions, emotion regulation strategies, and attachment style in complex post-traumatic stress disorder: implications for new and existing therapies. Br. J. Clin. Psychol. 2018;57(2):177–185. doi: 10.1111/bjc.12172. [DOI] [PubMed] [Google Scholar]
- Kelly-Irving M., Delpierre C. A critique of the adverse childhood experiences framework in epidemiology and public health: uses and misuses. Soc. Policy Soc. 2019 doi: 10.1017/S1474746419000101. [DOI] [Google Scholar]
- Killeen T., Hien D., Campbell A., Brown C., Hansen C., Jiang H., Kristman-Valente A., Neuenfeldt C., Rocz-de la Luz N., Sampson R., Suarez-Morales L., Wells E., Brigham G., Nunes E. Adverse events in an integrated trauma-focused intervention for women in community substance abuse treatment. J. Subst. Abuse Treat. 2008;35(3):304–311. doi: 10.1016/j.jsat.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, et al. Assessing trauma, substance abuse, and mental health in a sample of homeless men. Health Soc. Work. 2010;35(1):39–48. doi: 10.1093/hsw/35.1.39. [DOI] [PubMed] [Google Scholar]
- Kober H., Bolling D., Gross J. Handbook of Emotion Regulation. 2nd ed. Guilford; New York, NY: 2014. Emotion regulation in substance use disorders; pp. 428–446. [Google Scholar]
- Korotana L.M., Dobson K.S., Pusch D., Josephson T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clin. Psychol. Rev. 2016;46:59–90. doi: 10.1016/j.cpr.2016.04.007. [DOI] [PubMed] [Google Scholar]
- Kring A.M., Sloan D.M. Guilford Publications; 2009. Introduction and Overview. Emotion Regulation and Psychopathology; pp. 1–9. [Google Scholar]
- Leza L., Siria S., López-Goñi J.J., Fernández-Montalvo J. Adverse childhood experiences (ACEs) and substance use disorder (SUD): a scoping review. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108563. [DOI] [PubMed] [Google Scholar]
- Masin-Moyer M., Engstrom M., Solomon P. A comparative effectiveness study of a shortened trauma recovery empowerment model and an attachment-informed adaptation. Violence Against Women. 2019 doi: 10.1177/1077801219836730. 1077801219836730. [DOI] [PubMed] [Google Scholar]
- McCrady B.S., Epstein E.E., Hallgren K.A., Cook S., Jensen N.K. Women with alcohol dependence: a randomized trial of couple versus individual plus couple therapy. Psychol. Addict. Behav. 2016;30(3):287–299. doi: 10.1037/adb0000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen C.A., Gregerson S.F. A critical assessment of the adverse childhood experiences study at 20 years. Am. J. Prev. Med. 2019 doi: 10.1016/j.amepre.2018.10.016. [DOI] [PubMed] [Google Scholar]
- McKay M.T., Clarke M.C. Adverse childhood experiences (ACEs) and substance use disorder (SUD): A scoping review. Drug Alcohol Depend. 2021;225 doi: 10.1016/j.drugalcdep.2021.108782. [DOI] [PubMed] [Google Scholar]
- Mehl-Madrona L., Mainguy B. Introducing healing circles and talking circles into primary care. Perm. J. 2014;18(2):4–9. doi: 10.7812/TPP/13-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills K.L., Teesson M., Back S.E., Brady K.T., Baker A.L., Hopwood S., Sannibale C., Barrett E.L., Merz S., Rosenfeld J., Ewer P.L. Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence: a randomized controlled trial. JAMA. 2012;308(7):690–699. doi: 10.1001/jama.2012.9071. [DOI] [PubMed] [Google Scholar]
- Mills K.L., Teesson M., Ross J., Peters L. Trauma, PTSD, and substance use disorders: findings from the australian national survey of mental health and well-being. Am. J. Psychiatry. 2006;163(4):652–658. doi: 10.1176/ajp.2006.163.4.652. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group T.P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan-Lopez A.A., Saavedra L.M., Hien D.A., Campbell A.N., Wu E., Ruglass L., Patock-Peckham J.A., Bainter S.C. Indirect effects of 12-session seeking safety on substance use outcomes: overall and attendance class-specific effects. Am. J. Addict. 2014;23(3):218–225. doi: 10.1111/j.1521-0391.2014.12100.x. [DOI] [PubMed] [Google Scholar]
- Najavits L.M., Hien D. Helping vulnerable populations: a comprehensive review of the treatment outcome literature on substance use disorder and PTSD. J. Clin. Psychol. 2013;69(5):433–479. doi: 10.1002/jclp.21980. [DOI] [PubMed] [Google Scholar]
- NICE. (2018). Post-traumatic stress disorder. NICE clinical guideline No. 116. Manchester: National Institute for Health and Care Excellence. https://www.nice.org.uk/guidance/ng116. Accessed March 2019
- Norton P.J., Paulus D.J. Toward a unified treatment for emotional disorders: update on the science and practice. Behav. Ther. 2015;47(6):854–868. doi: 10.1016/j.beth.2015.07.002. [DOI] [PubMed] [Google Scholar]
- Nosè M., Ballette F., Bighelli I., Turrini G., Purgato M., Tol W., Priebe S., Barbui C. Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: systematic review and meta-analysis. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0171030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nöthling J., Malan-Müller S., Abrahams N., Hemmings S.M.J., Seedat S. Epigenetic alterations associated with childhood trauma and adult mental health outcomes: a systematic review. World J. Biol. Psychiatry. 2020;21(7):493–512. doi: 10.1080/15622975.2019.1583369. [DOI] [PubMed] [Google Scholar]
- Perez-Dandieu B., Tapia G. Treating trauma in addiction with EMDR: a pilot study. J. Psychoact. Drugs. 2014;46(4):303–309. doi: 10.1080/02791072.2014.921744. [DOI] [PubMed] [Google Scholar]
- Petit G., Luminet O., Maurage F., Tecco J., Lechantre S., Ferauge M., Gross J.J., de Timary P. Emotion regulation in alcohol dependence. Alcohol Clin. Exp. Res. 2015;39(12):2471–2479. doi: 10.1111/acer.12914. [DOI] [PubMed] [Google Scholar]
- Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., Britten, N., Roen, K., & Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A Product from the ESRC Methods Programme, 2006. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006. Accessed Mai 2019.
- Rasmussen I.S., Arefjord K., Winje D., Dovran A. Childhood maltreatment trauma: a comparison between patients in treatment for substance use disorders and patients in mental health treatment. Eur. J. Psychotraumatol. 2018;9(1) doi: 10.1080/20008198.2018.1492835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts N.P., Roberts P.A., Jones N., Bisson J.I. Psychological therapies for post-traumatic stress disorder and comorbid substance use disorder. Cochrane Database Syst. Rev. 2016 doi: 10.1002/14651858. 4, CD010204CD010204.pub2Accessed March 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Review Manager (RevMan), 2014. Version 5.3 [computer program]. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. https://revman.cochrane.org. Accessed Mai 2019
- Ryan R, 2013. Cochrane Consumers and Communication Review Group: data synthesis and analysis, 2013. http://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/Analysis.pdf. Accessed June 2019
- Sannibale C., Teesson M., Creamer M., Sitharthan T., Bryant R.A., Sutherland K., Taylor K., Bostock-Matusko D., Visser A., Peek-O’Leary M. Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction. 2013;108(8):1397–1410. doi: 10.1111/add.12167. [DOI] [PubMed] [Google Scholar]
- Saunders E.C., McLeman B.M., McGovern M.P., Xie H., Lambert-Harris C., Meier A. The influence of family and social problems on treatment outcomes of persons with co-occurring substance use disorders and PTSD. J. Subst. Use. 2016;21(3):237–243. doi: 10.3109/14659891.2015.1005184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer I., Hopchet M., Vandamme N., Ajdukovic D., El-Hage W., Egreteau L., Javakhishvili J.D., Makhashvili N., Lampe A., Ardino V., Kazlauskas E., Mouthaan J., Sijbrandij M., Dragan M., Lis-Turlejska M., Figueiredo-Braga M., Sales L., Arnberg F., Nazarenko T., Murphy D. Trauma and trauma care in Europe. Eur. J. Psychotraumatol. 2018;9(1) doi: 10.1080/20008198.2018.1556553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer I., Lotzin A., Hiller P., Sehner S., Driessen M., Hillemacher T., Schäfer M., Scherbaum N., Schneider B., Grundmann J. A multisite randomized controlled trial of Seeking Safety vs. Relapse Prevention Training for women with co-occurring posttraumatic stress disorder and substance use disorders. Eur. J. Psychotraumatol. 2019;10(1) doi: 10.1080/20008198.2019.1577092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer I., Pawils S., Driessen M., Härter M., Hillemacher T., Klein M., Muehlhan M., Ravens-Sieberer U., Schäfer M., Scherbaum N., Schneider B., Thomasius R., Wiedemann K., Wegscheider K., Barnow S. Understanding the role of childhood abuse and neglect as a cause and consequence of substance abuse: the German CANSAS network. Eur. J. Psychotraumatol. 2017;8(1) doi: 10.1080/20008198.2017.1304114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin J., Spain D., Furuta M., Murrells T., Norman I. Psychological interventions for post-traumatic stress disorder (PTSD) in people with severe mental illness. Cochrane Database Syst. Rev. 2017 doi: 10.1002/14651858.CD011464.pub2. 1, CD011464Accessed March 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan E., Hall K., Moulding R., Bryce S., Mildred H., Staiger P.K. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clin. Psychol. Rev. 2017;57:141–163. doi: 10.1016/j.cpr.2017.09.002. [DOI] [PubMed] [Google Scholar]
- Torchalla I., Nosen L., Rostam H., Allen P. Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: a systematic review and meta-analysis. J. Subst. Abuse Treat. 2012;42(1):65–77. doi: 10.1016/j.jsat.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Tull M.T., Barrett H.M., McMillan E.S., Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behav. Ther. 2007;38(3):303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Turner H.A., Finkelhor D., Henly M. Exposure to family and friend homicide in a nationally representative sample of youth. J. Interpers. Violence. 2018 doi: 10.1177/0886260518787200. 886260518787200. [DOI] [PubMed] [Google Scholar]
- Veilleux J.C., Skinner K.D., Reese E.D., Shaver J.A. Negative affect intensity influences drinking to cope through facets of emotion dysregulation. Personal. Individ. Differ. 2014;59:96–101. doi: 10.1016/j.paid.2013.11.012. [DOI] [Google Scholar]
- Vilhena-Churchill N., Goldstein A.L. Child maltreatment and marijuana problems in young adults: Examining the role of motives and emotion dysregulation. Child Abus. Negl. 2013;38(5):962–972. doi: 10.1016/j.chiabu.2013.10.009. [DOI] [PubMed] [Google Scholar]
- Vrana C., Killeen T., Brant V., Mastrogiovanni J., Baker N.L. Rationale, design, and implementation of a clinical trial of a mindfulness-based relapse prevention protocol for the treatment of women with comorbid post traumatic stress disorder and substance use disorder. Contemp. Clin. Trials. 2017;61:108–114. doi: 10.1016/j.cct.2017.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagenmans A., Van Minnen A., Sleijpen M., De Jongh A. The impact of childhood sexual abuse on the outcome of intensive trauma-focused treatment for PTSD. Eur. J. Psychotraumatol. 2018;9(1) doi: 10.1080/20008198.2018.1430962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N.H., Kiefer R., Goncharenko S., Raudales A.M., Forkus S.R., Schick M.R., Contractor A.A. Emotion regulation and substance use: a meta-analysis. Drug Alcohol Depend. 2021;230 doi: 10.1016/j.drugalcdep.2021.109131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss N.H., Tull M.T., Lavender J., Gratz K.L. Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abus. Negl. 2013;37(11):944–954. doi: 10.1016/j.chiabu.2013.03.014. [DOI] [PubMed] [Google Scholar]
- Wolff N., Huening J., Shi J., Frueh B.C., Hoover D.R., McHugo G. Implementation and effectiveness of integrated trauma and addiction treatment for incarcerated men. J. Anxiety Disord. 2015;30:66–80. doi: 10.1016/j.janxdis.2014.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff N., Frueh B.C., Shi J., Schumann B.E. Effectiveness of cognitive-behavioral trauma treatment for incarcerated women with mental illnesses and substance abuse disorders. J. Anxiety Disord. 2012;26(7):703–710. doi: 10.1016/j.janxdis.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Norman, S.B. & Hien, D.A. (2020). Behavioral interventions for comorbid PTSD and substance use disorder. PTSD Research Quaterly 31(2). https://www.ptsd.va.gov/publications/rq_docs/V31N2.pdf. Accessed september 2020.
- Wolff, S., Holl, J., Stopsack, M., Arens, E.A., Höcker, A., Staben, K.A., Hiller, P., Klein, M., Schäfer, I., & Barnow, S. (2016). Does emotion dysregulation mediate the relationship between early maltreatment and later substance dependence? Findings of the CANSAS study. Karger. doi: 10.11588/heidok.00027251. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.