Abstract
The existence of coronaviruses has been known for many years. These viruses cause significant disease that primarily seems to affect agricultural species. Human coronavirus disease due to the 2002 outbreak of Severe Acute Respiratory Syndrome and the 2012 outbreak of Middle East Respiratory Syndrome made headlines; however, these outbreaks were controlled, and public concern quickly faded. This complacency ended in late 2019 when alarms were raised about a mysterious virus responsible for numerous illnesses and deaths in China. As we now know, this novel disease called Coronavirus Disease 2019 (COVID-19) was caused by Severe acute respiratory syndrome-related-coronavirus-2 (SARS-CoV-2) and rapidly became a worldwide pandemic. Luckily, decades of research into animal coronaviruses hastened our understanding of the genetics, structure, transmission, and pathogenesis of these viruses. Coronaviruses infect a wide range of wild and domestic animals, with significant economic impact in several agricultural species. Their large genome, low dependency on host cellular proteins, and frequent recombination allow coronaviruses to successfully cross species barriers and adapt to different hosts including humans. The study of the animal diseases provides an understanding of the virus biology and pathogenesis and has assisted in the rapid development of the SARS-CoV-2 vaccines. Here, we briefly review the classification, origin, etiology, transmission mechanisms, pathogenesis, clinical signs, diagnosis, treatment, and prevention strategies, including available vaccines, for coronaviruses that affect domestic, farm, laboratory, and wild animal species. We also briefly describe the coronaviruses that affect humans. Expanding our knowledge of this complex group of viruses will better prepare us to design strategies to prevent and/or minimize the impact of future coronavirus outbreaks.
Abbreviations: BCoV, Bovine coronavirus; CCoV, canine coronavirus; CoV(s), coronavirus(es); COVID-19, Coronavirus Disease 2019; CRCoV, canine respiratory coronavirus; E, Coronaviral envelope protein; ECoV, equine coronavirus; FCoV, feline coronavirus; FIPV, feline infectious peritonitis virus; GfCoV, guinea fowl coronavirus; HCoV, Human coronavirus; IBV, infectious bronchitis virus; M, Coronaviral membrane protein; MERS, Middle East Respiratory Syndrome-Coronavirus; MHV, mouse hepatitis virus; PEDV, porcine epidemic diarrhea virus; PDCoV, porcine deltacoronavirus; PhCoV, pheasant coronavirus; PHEV, porcine hemagglutinating encephalomyelitis virus; PRCoV, porcine respiratory coronavirus; RT-PCR, Reverse transcriptase polymerase chain reaction; S, Coronaviral spike protein; SADS-CoV, swine acute diarrhea syndrome-coronavirus; SARS-CoV, Severe Acute Respiratory Syndrome-Coronavirus; SARS-CoV-2, Severe Acute Respiratory Syndrome–Coronavirus–2; TCoV, turkey coronavirus; TGEV, transmissible gastroenteritis virus
Introduction
In the last 2 decades, 3 major Coronavirus (CoV) outbreaks, including the current Coronavirus Disease 2019 (COVID-19) pandemic, have affected hundreds of millions and killed millions of people. In all 3 outbreaks, the etiologic agents were novel coronaviruses (CoVs) that crossed species barriers and adapted to humans. CoVs infect a wide range of both wild and domestic species.11 Their large genome size, the largest among RNA viruses, limited dependency on host cellular proteins, and frequent recombination allow CoVs to efficiently cross species.174,278 In fact, all known human CoVs originated in animals.257 Bats and birds are believed to be the ancestral hosts and natural reservoirs for all CoVs, with occasional transmission to other animals, including humans.174,203,257,427,431 While the natural reservoir for the virus that causes COVID-19, Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2), has not been formally identified, the genome sequence of the virus is most closely related to bat coronaviruses.335,397 In 1968, the name “coronavirus” was first proposed to describe this group of viruses based on their distinctive morphology by electron microscopy examination and other characteristics common to avian infectious bronchitis virus, mouse hepatitis virus, and human coronavirus strains.184 In this review, we describe the CoVs, their origins, transmission mechanisms, pathogenesis, clinical signs, diagnosis, treatment, and prevention. Better understanding of this complex group of viruses should allow the development of strategies to prevent and/or minimize the impact of potential future outbreaks.
Coronaviral Classification and General Information
The International Committee on Taxonomy of Viruses (ICTV) in its latest release (March 2021) classifies coronaviruses as members of the Nidovirales order, suborder Cornidovirineae, family Coronaviridae, subfamily Orthocoronavirinae. The relevant coronaviruses affecting animals are further subdivided into 4 genera, the Alphacoronavirus with 14 subgenera, the Betacoronavirus with 5 subgenera, the Deltacoronavirus with 3 subgenera, and the Gammacoronavirus with 3 subgenera (Figure 1).206 Alpha- and betacoronaviruses infect mammals while delta- and gammacoronaviruses infect, with a few exceptions, mostly birds.469
Figure 1.
Coronavirus classification according to the International Committee on Taxonomy of Viruses. Adapted from reference 206.
All members of the Nidovirales order are enveloped, nonsegmented, positive-sense RNA viruses with genomes of around 30 kilobases. They possess a highly conserved genomic organization, express many nonstructural genes, have several unique enzymatic activities, and express downstream genes by synthesis of 3′ nested subgenomic mRNAs.146 Coronavirus virions are spherical with diameters of approximately 125 nm, with the most prominent feature being club-shaped spike projections (peplomers) on the surface that resemble a solar corona (Latin corona, crown), leading to the name coronavirus.22,333 The virion contains a helically symmetrical nucleocapsid that is not common in positive-sense RNA viruses.146
CoVs contain 4 main structural proteins (Figure 2): the spike (S), membrane (M), envelope (E), and nucleocapsid (N) proteins, all of which are encoded within the 3′ end of the viral genome.146 The S protein, the main antigenic component against which neutralizing antibodies are created during natural infection, is cleaved by host cell proteases into 2 polypeptides, the S1 which constitutes the large receptor binding domain of the S protein, and the S2 which constitutes the stalk of the spike molecule.1,113,292 S1 is responsible for viral attachment to specific host cell receptors, and S2 undergoes major conformational changes that lead to the fusion of the virion envelope and the host cell plasma membrane.1,40,56,292,315 The M protein is the most abundant structural protein in the virion, essential for the morphogenesis process, and it is thought to give the virion its shape.16 The M protein is a type III glycoprotein that directs most of the protein-protein interactions required for assembly of CoVs and binds to the nucleocapsid, promoting the completion of virion assembly. Glycosylation of the M protein affects organo-tropism and interferon (IFN) inducing capacity in some CoVs.114,264 The E protein is found in small quantities in coronaviruses and is highly diverse, with its main function thought to be the assembly and release of the virus.123 The E proteins from different CoVs are highly divergent but share a common architecture, have ion channel activity, facilitate assembly and release of the virus, and are required for pathogenesis.68,337,390 The N protein is a highly basic phosphoprotein in the nucleocapsid and has 2 different domains, an N-terminal domain (NTD) and a C-terminal domain (CTD), both of which bind RNA.246 In association with genomic viral RNA (gRNA), the N protein forms the helical nucleocapsid that is stabilized by binding to the M protein. The viral genome and helical nucleocapsid are surrounded by a host-derived lipid bilayer that anchors the S, E, and M proteins. In addition to its function in the virion, N protein also modulates viral RNA synthesis.80,204,246,413,418,467 A fifth structural protein that is present only in a subset of betacoronaviruses in the subgenus Embecovirus is hemagglutinin-esterase (HE), which binds sialic acids on surface glycoproteins and contains acetyl-esterase activity that functions as a receptor-destroying enzyme, enhancing viral S protein-mediated mucosal cell invasion and spread.100 In human CoVs OC43 and HKU1, HE-mediated receptor binding was selected against and ultimately lost through progressive accumulation of mutations in the HE lectin domain as an adaptation to the human upper respiratory tract.18 Phylogenetic analysis suggests that the HE genes of CoVs and influenza C virus have a common ancestral origin, and that bovine coronaviruses and HCoV-OC43 are closely related.506
Figure 2.
Summary of Coronavirus structural proteins composition and function.
Viral cell attachment and invasion are initiated by the interaction of the S1 protein and its receptor binding domain (RBD) with the host cell receptors. Most alphacoronaviruses use aminopeptidase N as their host cellular receptor (that is, Canine Coronavirus, Feline Infectious Peritonitis Virus, Transmissible Gastroenteritis Virus, and Human Coronavirus-229E), while betacoronaviruses use the angiotensin-converting enzyme receptor (Severe Acute Respiratory Syndrome-Coronavirus and Severe Acute Respiratory Syndrome-Coronavirus-2), the dipeptidyl-peptidase 4 receptor (Middle East Respiratory Syndrome-Coronavirus), the N-acetyl-9-O-acetylneuraminic acid receptor (Bovine Coronavirus), the murine carcinoembryonic antigen-related cell adhesion molecule 1 receptor (Mouse Hepatitis Virus), and possibly others yet to be identified.42,125,194,273,277,329,370,391,437,476,495,508
Once the virus binds to the cell, fusion of the viral and cellular membranes occurs as a result of S protein cleavage exposing a fusion peptide that inserts into the cell membrane. Once the viral genome is released into the cytoplasm, translation of the replicase gene from the virion genomic RNA occurs by means of 2 large open reading frames (ORFs) that express 2 coterminal polyproteins.21 These polyproteins contain nonstructural proteins whose main role is to assemble the replicase-transcriptase complex (RTC) to create an environment suitable for RNA synthesis; they are ultimately responsible for RNA replication and transcription of subgenomic RNAs that serve as mRNAs for the structural and accessory genes.405,512 The accessory genes are coded by additional ORFs and are not essential for virus replication but are important in virus-host interactions including regulating innate immunity, viral proliferation, and pathogenicity.144 Loss of accessory genes through spontaneous mutations, or reversed genetics, reduces virulence.248 Nonstructural proteins (nsp) also have several functions related to viral cell invasion and can block host innate immune responses.405,432 For example, nsp1 proteins from alpha- and beta-CoVs can suppress host gene expression and protein synthesis and can block innate immune responses by direct inhibition of translation or by promoting degradation of host IFN mRNA.200,270,328,435,500 In addition, nsp3, nsp5, nsp8, nsp15, and nsp16 can, by different mechanisms, interfere with or block host innate immunity, contributing to immune evasion and facilitating viral infection.83,244,309,375
After replication and subgenomic RNA synthesis, the viral structural proteins S, E, and M are translated and inserted into the endoplasmic reticulum and follow the secretory pathway endoplasmic reticulum-Golgi intermediate compartment (ERGIC); there the viral genomes encapsidated by the N protein will bud into membranes of the ERGIC containing viral structural proteins, forming mature virions. Virions are then transported to the cell surface in vesicles and released by exocytosis.241,436 In some coronaviruses, S protein that is not assembled into virions migrates to the cell surface where it mediates cell-cell fusion between infected and adjacent uninfected cells, leading to the formation of giant multinucleated cells (syncytia) and allowing the virus to spread by evading the host immune response.146 Coronaviruses are well known for their ability to recombine using both homologous and nonhomologous recombination, which are thought to be important in viral evolution and adaptation to new hosts.225,249,420 The viral replicase does not have a good proof-reading ability, incorporating incorrect nucleotides at each replication cycle and leading to accumulation of mutations in the viral genome; this results in the progressive differentiation of the viral progeny from the parental strain.20,251 This characteristic replication of CoVs also allows recombination events during CoV coinfections; RNA polymerase from one strain can transfer to the RNA of the other strain to produce a hybrid RNA containing sequences from both viruses (a homologous recombination).20,251 Recombination can also occur between a CoV and another RNA virus (heterologous recombination).199,291 These mutations and recombination events may increase viral transmissibility and pathogenicity or support adaptation to a new host species.20
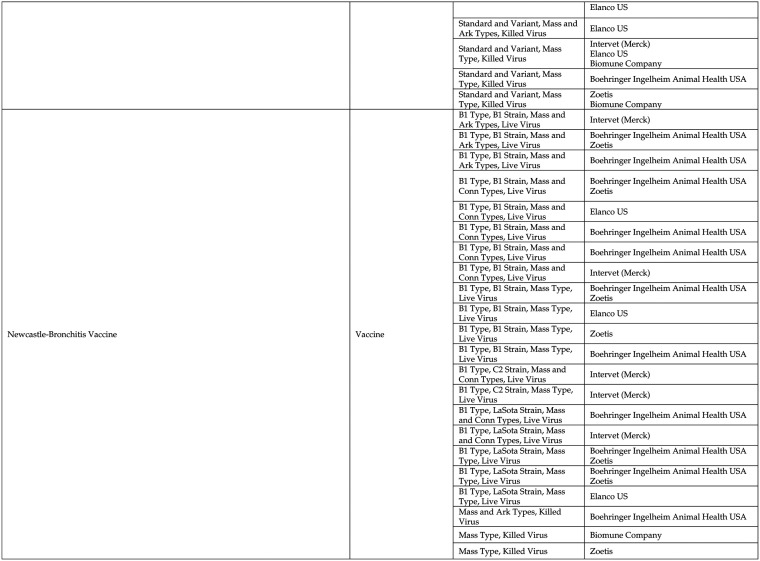
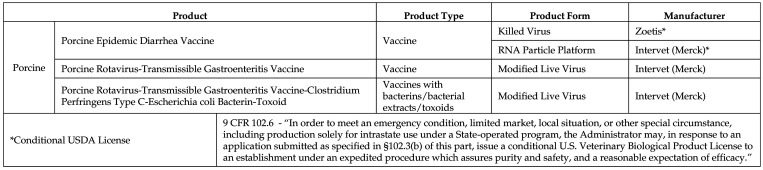
CoVs cause disease in many different species of mammals and birds. Clinical signs depend on the organs affected, which is determined by the S protein–receptor interaction between the virus and the host cell. Figure 3 summarizes salient features of the coronaviral infections. The majority of CoVs cause more severe disease in neonatal, young, or immunocompromised animals. In contrast, a few CoVs, most prominently ferret coronavirus, can cause severe disease in older ferrets while young ferrets often show mild disease.475 Age susceptibility is relevant to determining the best age for vaccination. Reverse transcriptase polymerase chain reaction (RT-PCR) is the most common method of diagnosis followed by serologic assays. Currently more than 80 USDA-licensed animal vaccines are available; however, their effectiveness is highly variable because natural mucosal infections usually do not provide immunity to prevent subsequent infections, and the propensity of the virus for recombination makes the vaccine less effective, or in some cases, the vaccine itself may lead to enhanced disease.433,450,456 In addition, no effective or approved antiviral treatments are available for animal CoVs.
Figure 3.
Summary of Clinical and Pathologic Features of Select Coronaviral Infections.
Human Coronaviruses
Seven different species of CoVs are known to cause disease in humans. Four of these viruses are well adapted to humans and found endemically across the globe; they cause seasonal, mild to moderate upper respiratory disease in temperate climates.420,446 The other 3 can cause severe respiratory disease in humans, with SARS-CoV-2 being highly transmissible and currently prevalent across all continents.107,146
Human Coronavirus: HCoV-229E.
Human coronavirus (HCoV) 229E belongs to the genus Alphacoronavirus (subgenus Duvinacovirus). In 1965, a previously unidentified virus was isolated in human embryonic tracheal organ culture of sample B814, a nasal swab and a washing sample from a boy with common cold symptoms.441 The following year, a new virus was isolated from adult patients with common cold symptoms and was designated as strain 229E.185 Other viruses similar to strain 229E were successfully cultured in human embryonic intestine cell cultures from patients with upper respiratory tract illnesses. In 1967, strains 229E and B814 were found to be indistinguishable from the viral particles of avian infectious bronchitis virus (IBV) when examined by electron microscopy.440 HCoV-229E is endemic in human populations and causes upper respiratory infections that are more severe in neonates, the elderly, and those with underlying conditions such as a compromised immune system or chronic pulmonary disease.146 Serum-neutralizing antibody titers are not correlated with protection from reinfection or severity of infection.184 HCoV-229E uses aminopeptidase N (APN) as a cellular receptor for viral entry, and isolates from around the world having minimal genetic variation.85 HCoV-229E is closely related to the species Alpaca alphacoronavirus and Dromedary camel alphacoronavirus. A recent study suggested an evolutionary origin of 229E-related CoVs in hipposiderid bats, hypothetically with camelids as intermediate hosts preceding the establishment of HCoV-229E.98 HCoV-229E is thought to have emerged in human populations 200 y ago.155
Human Coronavirus: HCoV-OC43.
Human coronavirus OC43 (Betacoronavirus 1) belongs to the genus Betacoronavirus (subgenus Embecovirus). In 1967, 6 viral strains that were similar to avian IBV were isolated from adults with upper respiratory illness by using tracheal organ culture.305 Two strains of this virus, designated OC 38 and OC 43, were subsequently adapted for growth in suckling mouse brain, and reagents prepared from these strains were serologically identical by complement fixation and neutralization tests.304 Like HCoV-229E, HCoV-OC43 is endemic globally and is the most common human coronavirus; it causes upper respiratory infections in humans. In contrast to HCoV-229E, HCoV-OC43 uses sialic acids on the cell surface as a cellular receptor for viral entry423 and isolates have significant genetic variability.452 HCoV-OC43 is naturally capable of invading the central nervous system (CNS), with neurons preferentially targeted for infection.15 HCoV-OC43 E protein is critical for infectious virus production and for dissemination in epithelial and neuronal cell cultures and mouse CNS and is an important determinant of neurovirulence.412 Fatal human coronavirus HCoV-OC43 encephalitis has been reported in humans with immune deficiency and, in retrospective studies, associated with multiple sclerosis.15,223,412 HCoV-OC43 carries an additional structural protein, hemagglutinin-esterase (HE), that binds to sialic acids.423 HCoV-OC43 is thought to have evolved from ancestral Bovine coronavirus (BCoV) strains that crossed the interspecies barrier and established human infections in around 1890.107,155 However, BCoV appears to have a rodent origin, China Rattus coronavirus HKU24, which crossed species and became established in bovines centuries before the emergence of HCoV-OC43.262 Enteric coronaviruses antigenically related to HCoV-OC43 have been associated with acute necrotizing gastroenteritis in humans.166
Human Coronavirus: HCoV-NL63.
Human coronavirus NL63 belongs to the genus Alphacoronavirus (subgenus Setracovirus) and was first isolated in 2003 from a 7-mo-old child in the Netherlands who had bronchiolitis and conjunctivitis. The virus was later found to be widespread globally.446,447 HCoV-NL63 infections usually cause nonfatal upper and lower respiratory tract infections in infants, the elderly, and immunocompromised adults, and have been associated with obstructive laryngitis (‘croup’) in children.448 In addition to human primary tracheobronchial cells, HCoV-NL63 replicates and causes a cytopathic effect in tertiary monkey kidney cells and the monkey kidney LLC-MK2 cell line.160,447 HCoV-NL63 is genetically closely related to HCoV-229E, and its viral genome has distinctive features, including a unique N-terminal fragment in the spike protein.446 HCoV-NL63 uses human angiotensin-converting enzyme 2 (ACE2) as its cellular receptor.446 Thought to be of bat origin due to similarity to NL63-related bat coronavirus strain BtKYNL63-9b, HcoV-NL63 appears to have emerged in the human population approximately 560 to 820 y ago.155
Human Coronavirus: HCoV-HKU1.
Human coronavirus HKU1 (for Hong Kong University) belongs to the genus Betacoronavirus (subgenus Embecovirus) and was first isolated from a 71-y-old Chinese man admitted to a hospital in Hong Kong in January 2004 because of fever and productive cough with purulent sputum.483 HCoV-HKU1 is found worldwide and usually causes mild respiratory disease with rhinorrhea, fever, and cough, but it can also cause more severe disease with febrile seizures, wheezing, pneumonia, and bronchiolitis in very young children, the elderly, adults with chronic respiratory disease, and the immunocompromised; it has also been associated with acute asthmatic exacerbation.258 Like HCoV-OC43, HCoV-HKU1 carries an additional structural protein, hemagglutinin-esterase, and uses cell surface sialic acids as its cellular receptor for viral entry.484 HCoV-HKU1 is thought to have emerged in the human population in the early 1950s; a rodent coronavirus is a possible ancestor based on its close relationship to the Betacoronavirus 1 group and other rodent-associated coronaviruses in the subgenus Embecovirus.107,155,458
Human Coronavirus: SARS-CoV.
Severe acute respiratory syndrome-related coronavirus (SARS-CoV) belongs to the genus Betacoronavirus (subgenus Sarbecovirus). First reported in late 2002 as “atypical pneumonia” in people linked to live animal markets in Guangdong Province of China, SARS-CoV rapidly spread in human populations in China and more than 2 dozen countries in Asia, Europe, North America, and South America, causing the first, well-documented pandemic in modern history.242,348 By the time SARS-CoV was declared contained in July 2003, over 8,000 cases and 780 deaths had been reported worldwide.75 Clinical signs included myalgia, headache, fever, malaise, and chills, followed by dyspnea, cough, and respiratory distress; approximately 20% to 30% of the patients required intensive care and mechanical ventilation.507 In contrast to seasonal coronaviruses, SARS-CoV can affect multiple organs, resulting in high mortality associated with exacerbated host cytokine response.263
Autopsy of patients who died due to SARS showed edematous lungs with greyish-brown irregular patches of consolidation, foci of pale tissue of up to several millimeters in diameter, and mucopurulent material in the tracheobronchial tree.336 Microscopically, bronchial epithelial denudation, loss of cilia, squamous metaplasia, and diffuse alveolar damage were common. Alveolar pneumocytes showed cytomegaly with granular amphophilic cytoplasm along with a giant-cell infiltrate and a pronounced increase in macrophages in the alveoli and interstitium.336 Coronaviral particles were seen on electron microscopy in the cytoplasm of epithelial cells, and SARS-CoV antigen was found in airways and alveolar epithelial cells, vascular endothelial cells, macrophages, monocytes, and lymphocytes.177,336 SARS-CoV-infected macrophages expressed CXCL10/IFN-γ-inducible protein 10 and CCL2/monocyte chemotactic protein 1, with poor induction of IFN-β.84 SARS-CoV-infected dendritic cells showed low expression of antiviral cytokines (IFN-α, IFN-β, IFN-γ, and interleukin 12p40), moderate upregulation of proinflammatory cytokines tumor necrosis factor (TNF)-α and interleukin (IL)-6, and significant upregulation of inflammatory chemokines (macrophage inflammatory protein 1α, regulated on activation normal T cell expressed and secreted [RANTES], interferon-inducible protein of 10 kDa, and monocyte chemoattractant protein 1 [MCP-1]).266 In addition, pneumocytes and lung macrophages expressed P-selectin and DC-SIGN.496 Serum from SARS patients had marked elevation of Th1 IFN-γ, inflammatory cytokines IL-1, IL-6, and IL-12, but no significant elevation of inflammatory cytokine TNF-α, antiinflammatory cytokine IL-10, Th1 cytokine IL-2, and Th2 cytokine IL-4. The serum chemokine profile showed significant elevation of neutrophil chemokine IL-8, MCP-1, and Th1 chemokine IFN-γ-inducible protein-10.86,482
Masked palm civets (Paguma larvata) and raccoon dogs (Nyctereutes procyonoides) in live animal markets in Guangdong Province of China were identified as carriers of SARS-CoV-like viruses that are almost identical to SARS-CoV.178 However, wild masked palm civets and farms that were not exposed to live animal markets were negative for SARS-CoV-like viruses, suggesting that these species were intermediate hosts.398 Although limited research has been conducted to survey wild or farmed raccoon dog populations, they are also considered an intermediate host. The comparative analysis between human and civet SARS-CoVs isolates suggests that SARS-CoV rapidly adapts to different hosts, particularly with mutations at the RBD of the S protein.407 Like HCoV-NL63, SARS-CoV uses ACE2 as the cellular receptor for viral entry.277 The search for the natural host of SARS-CoV resulted in the discovery of several SARS-like-CoVs in Chinese horseshoe bats, Rhinolophus spp.198 However, none are considered the immediate parental virus of SARS-CoV.198 The current model of the origin of SARS-CoV that caused the 2003 pandemic suggests that it is the result of multiple recombination events from several SARS-CoV ancestors in horseshoe bat species in China.289
Human Coronavirus: MERS-CoV.
Middle East respiratory syndrome-related coronavirus (MERS-CoV) belongs to the genus Betacoronavirus (subgenus: Merbecovirus) and was first reported in June 2012 in Saudi Arabia in a 60-y-old patient with acute pneumonia and renal failure.501 Clinical signs are similar to those of SARS, characterized by severe respiratory distress; however, a significant number of patients also show renal failure, diarrhea, and vomiting.5,14,380 MERS cases were mostly independent clusters in Middle Eastern countries, with limited spread to European countries, South Korea, and the United States of America by infected individuals traveling from the Middle East.145 Since April 2012 and as of May 3rd,2021, 2,589 cases of MERS-CoV, including 940 deaths, have been reported by health authorities worldwide.141
Gross lesions reported in a fatal case of MERS-CoV included massive pleural effusion, substantial pericardial effusion, abdominal effusion, edematous and consolidated lungs, and generalized congestion.334 Microscopic lesions included exudative-phase diffuse alveolar damage with denuding of bronchiolar epithelium, prominent hyaline membranes, alveolar fibrin deposits, type 2 pneumocyte hyperplasia, rare multinucleated syncytial cells, alveolar septal edema with lymphocytes, fewer plasma cells, neutrophils, and macrophages.334 MERS-CoV antigens were found predominantly in the cytoplasm of pneumocytes and syncytial cells.334 MERS-CoV infection of human airway epithelial cells induces higher expression of IL-1β, IL-6, and IL-8 than those induced by SARS-CoV.259 High viral loads, weak antibody responses, and lymphopenia accompanied by thrombocytopenia were associated with disease mortality; persistent lymphocyte responses may be required for effective immunity against MERS-CoV infection.316 Leukocytosis, primarily due to an increase in neutrophils and monocytes, was generally observed in severe and fatal cases, and blood levels of IL-6, IL-10, IL-15, CXCL-10, TGF-β, and EGF were correlated with disease severity.233,316
With a fatality rate of around 35%, MERS-CoV is the deadliest of all coronaviruses known to infect humans.490 Phylogenetic analysis places MERS-CoV in the same subgenus as bat CoV-HKU4 and bat CoV-HKU5.486 Bat CoV-HKU4 and MERS-CoV use the same host cell receptor, dipeptidyl peptidase 4 (DPP4), for viral entry.261,375 However, a bat CoV has not been found that is genetically close enough to be the immediate parental virus of MERS-CoV. Live MERS-CoV identical to the virus found in humans was isolated from the nasal swabs of dromedary camels (Camelus dromedarius).231 Infected camels shed MERS-CoV not only through the respiratory route but also through feces, which is the main route for virus shedding in bats.187 Another survey found viral RNA and neutralizing antibodies in dromedary camel milk, raising concerns about food-borne transmission of MERS.372 A recent study in Saudi Arabia found high prevalence (39%) and seropositivity (71%) of MERS-CoV in slaughtered dromedary camels, indicating previous and ongoing MERS infection in this species.9 The close relationship of MERS-CoV to bat coronaviruses in the Merbecovirus subgenus suggests a possible ancestor that crossed host species, adapting to and establishing in camels, which in turn, due to the close contact with humans in the Middle East, sporadically crossed the species barrier and caused outbreaks in humans.107,188
Human Coronavirus: SARS-CoV-2 (COVID-19).
Coronavirus disease 19 (COVID-19) is recognized by the Coronaviridae Study Group of the International Committee on Taxonomy of Viruses as forming a sister clade to the prototype human and bat SARS-CoVs of the species Severe acute respiratory syndrome-related coronavirus and designates it as SARS-CoV-2 (Severe acute respiratory syndrome-related coronavirus-2) belonging to the genus Betacoronavirus, subgenus Sarbecovirus.171 First reported in the city of Wuhan, China in December 2019, COVID-19 has since spread worldwide. As of March 2nd, 2022, COVID-19 has resulted in more than 438 million confirmed cases and more than 5.9 million deaths.217 Clinical signs may include fever or chills, cough, shortness of breath or difficulty breathing, fatigue, malaise, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea.76 The majority of the cases are thought to be asymptomatic or mild, with up to 9% of cases, mostly in older people, requiring hospitalization.308
The strongest risk factor for severe COVID-19 is age, followed by sex (male), diabetes, hypertension, obesity, chronic kidney disease, and potentially other chronic inflammatory diseases.426,477 Lung changes at postmortem examination were similar to those seen in SARS and MERS cases characterized by exudative and proliferative phases of diffuse alveolar damage, with capillary congestion, necrosis of pneumocytes, hyaline membranes, interstitial and intraalveolar edema, type 2 pneumocyte hyperplasia, squamous metaplasia with atypia, and platelet-fibrin thrombi.64 The inflammatory infiltrate was largely composed of macrophages in the alveolar lumen and lymphocytes in the interstitium.64 Electron microscopy revealed that viral particles were predominantly located in pneumocytes.64 SARS-CoV-2 evades innate immunity response through the expression of viral nonstructural proteins that block IFN pathways, resulting in lower levels of IFN-I and IFN-III in the lungs and peripheral blood.224 Genetic mutations or autoantibodies that interfere with IFN pathways may also increase the susceptibility to severe COVID-19 disease. On the other hand, prolonged secretion of IFN during the late phase of the infection correlates with disease severity, most likely due to the induction of chemokines that recruit inflammatory cells.268,288 Patients with severe COVID-19 have a marked decline in the number of dendritic cells, T cells, and NK cells in the blood, along with depleted alveolar macrophages and dendritic cells in the lungs, all of which result in a severe reduction of the host’s ability to mount an effective immune response.288,300,473,511 CD4+ and CD8+ T cells directed against multiple SARS-CoV-2 antigens, including structural and nonstructural proteins, are significantly associated with milder disease, suggesting that a coordinated CD4+ T cell, CD8+ T cell, and antibody response is required for protection against severe disease.379 In severe cases, tissue damage persists after viral clearance due to an exacerbated immune response that can cause pulmonary endothelial injury, excess vascular permeability and microthrombi deposition.357 Extrapulmonary pathology is predominantly seen in the liver and spleen, with intravascular thrombosis commonly being widespread and with disseminated intravascular coagulation often present.313 Other common findings are gastrointestinal symptoms and cardiac, renal, and olfactory dysfunction.286,357,494 The pathogenesis of the extrapulmonary lesions is most likely multifactorial due to direct viral injury to cells and to an exacerbated/dysfunctional immune response damaging multiple tissues.
Similar to HCoV-NL63 and SARS-CoV, SARS-CoV-2 uses host ACE2 as the cellular receptor for viral entry.425 Many of the initial cases of COVID-19 were associated with the Huanan Seafood Wholesale Market, which sells wildlife species, suggesting a probable zoonotic origin.274 Pangolins (Manis javanica) were recently found to carry beta-CoVs that have 85% to 92% nucleotide sequence homology with SARS-CoV-2.295 In addition, the intermediate horseshoe bat (Rhinolophus affinis) carries a coronavirus (CoV RaTG13) that has 96% nucleotide homology with SARS-CoV-2.295 However, despite these close relationships, the sequence divergence is too great for these animal CoVs to be the immediate parental strain for SARS-CoV-2.295 The animal reservoir and origin of SARS-CoV-2 remain to be determined.
Coronaviruses of Domestic Animals
Domestic fowl coronaviruses.
While the SARS-CoV-2 pandemic has placed the spotlight on human CoVs, the first CoV ever described was Infectious Bronchitis Virus (IBV) in domestic chickens over 80 y ago.72 All bird CoVs described to date are either gamma- or deltacoronaviruses, whereas most mammalian CoVs are alpha- or betacoronaviruses.130 Domestic fowl CoVs belong to the genus Gammacoronavirus (subgenus Igacovirus), species Avian coronavirus. The study of IBV and other bird CoVs has provided a wealth of information on coronaviral structure and function, disease pathogenesis, and vaccine strategies. However, despite decades of research on IBV, the disease still causes significant economic losses around the world.130 CoVs of domestic and wild bird populations have been found on all continents,474 and migratory, wild birds are the suspected reservoir for recurring outbreaks in domestic fowl.
Infectious bronchitis virus (IBV).
Infectious bronchitis of newborn domestic chickens (Gallus gallus domesticus) was first reported in 1931, and a viral etiology was described in 1936.474 Clinical signs in young chicks included ocular/nasal discharge, coughing, sneezing, swollen sinuses and respiratory rales, and reduced feed consumption and weight gain, with mortality reaching 90%.211 Although the clinical signs in young chicks are primarily respiratory, the virus can replicate in numerous epithelial surfaces, including the GI tract, kidney, and reproductive tract.71 IBV uses the host cell sialic acids for attachment.478 The respiratory lesions caused by IBV often lead to secondary viral and bacterial infections that exacerbate disease severity.92 Some strains cause severe renal disease and high mortality in adults; whereas others cause reduced egg production and egg quality.211 Persistent infections of the cecal lymphoid tissue and kidneys are likely to be a source of recurrent outbreaks in flocks.92 Morbidity in flocks quickly reaches 100%, resulting in high viral replication and the emergence of mutant strains. To date, at least 32 different IBV serotypes or strains have been reported around the world.474 Transmission is by direct contact with infected birds or contaminated fomites such as bedding and equipment.211 Vertical transmission does not appear to occur.92 Sialic acids are the dominant cellular receptors to which IBV binds and enters cells.
Turkey coronavirus (TCoV).
Coronaviral infection in domestic turkeys (Meleagris gallopavo domesticus) was first reported in the US in 1951 as severe gastrointestinal disease in young poults with high morbidity and mortality.360 The disease also caused cyanosis of the head and was termed ‘Bluecomb disease.’ The etiological agent was identified as a coronavirus in the 1970s.385 Turkey coronavirus (TCoV) was not found in European turkey poults until 2008.130 Poults up to 4 wk of age are the most susceptible to severe disease and mortality. The virus targets the intestinal epithelium and cloacal bursa.385 Clinical signs include anorexia, depression, decreased feed consumption, watery diarrhea, and high mortality.208 The virus causes atrophy of the thymus and bursa of Fabricus, leading to immune dysfunction and the promotion of secondary infections.60 Turkey coronavirus is one of several infectious agents involved in poultry enteritis-mortality syndrome (PEMS).130 TCoV is antigenically similar to IBV, and chickens can develop asymptomatic infections with TCoV.208 Experimentally, turkeys can be infected with bovine coronavirus (BCoV) and develop mild enteritis; however, natural BCoV infections have not been reported.71
Pheasant coronavirus (PhCoV).
Farmed, domestic pheasants (Phasianus colchicus) were first reported to develop coronaviral disease in the UK in the early 1980s.408 The disease causes high mortality (45%) in young birds with nonspecific clinical signs such as hunched posture and drooping wings, although some reports found mild respiratory signs.71,186 Affected adult females had reduced egg production and occasional abnormalities in egg quality.186 Nephritis has also been reported.71,186 Similar to TCoV, chickens experimentally inoculated with PhCoV developed neutralizing antibodies but no disease.71 The cellular receptor used by PhCoV is currently unknown but likely is sialic acids similar to IBV.186
Guinea fowl coronavirus (GfCoV).
Acute enteritis in farmed guinea fowl (Numida meleagris), known as Fulminating Disease (or X-disease), was first described in France in the 1980s; however, an etiology was not identified until 2011.280 While initial reports appeared to point to an avian Gammacoronavirus as the sole etiological agent,133,280 no studies have reported successful, experimental infection with purified guinea fowl coronavirus (GfCoV). To date, Fulminating Disease of guinea fowl is associated with infections of both GfCoV and either a guinea fowl astrovirus (GfAstV)434 or a guinea fowl picornavirus (GfPic).101 In vitro experiments have shown that GfCoV binds to sialic acid receptors.57 The disease has a very high mortality rate; lesions are most often limited to the GI tract but may occasionally be found in the pancreas.57
Canine coronaviruses.
Canine coronaviruses are usually associated with mild, self-limiting disease. The 2 forms of canine coronavirus are canine enteric coronavirus (CCoV), which belongs to the genus Alphacoronavirus (subgenus Tegacovirus) species Alphacoronavirus 1, and the canine respiratory coronavirus (CRCoV), which belongs to the genus Betacoronavirus (subgenus Embecovirus) species Betacoronavirus 1.115,116,139,321
Canine enteric coronavirus (CCoV).
CCoV is associated with enteric disease and was first isolated in 1971 from military dogs with mild enteritis.53 Currently, CCoV has worldwide distribution, is commonly associated with gastrointestinal disease of varied severity, and is caused by 2 subtypes.115,410,460 It also has been found in wild canids.8,324 CCoV is related to feline coronavirus (FCoV) and swine transmissible gastroenteritis virus (TGEV).65,282 More recently, a CCoV strain recombinant with TGEV has been isolated (CCoV-2b).122 Two serotypes (CCoV-1 and CCoV-2) and mixed serotype infections are common in outbreaks.115,460 Based on genetic sequencing, the 2 serotypes differ in their S proteins, 116,282,361 which have different amino acid sequences in the N-terminal region.121 In addition, the detection of the recombinant strains resulted in the serotype 2 reclassification as CCoV-2a and CCoV-2b for the recombinant strains.121,122 CCoVs are transmitted via the fecal-oral route using APN as the cellular receptor.42 Outbreaks are associated with young dogs in kennels or shelters.410 Based on the virulence of CCoV, 2 different pathogenic phenotypes have emerged but do not coincide with the serotype.428 CCoV-1 and CCoV-2 can cause asymptomatic or self-limiting (mild) enteritis or systemic disease with fever, enteritis, and/or neurologic signs.61 A highly virulent CCoV-2a strain has emerged, resulting in pantropic (systemic) infection not restricted to the gastrointestinal system.119 More severe disease has also often been associated with mixed infection with other pathogens and are age dependent, with puppies being more susceptible to clinical disease.91,116 Infected dogs usually present with an acute onset of diarrhea, vomiting, loss of appetite and lethargy. Clinical signs of less virulent strains resolve in 8 to 10 d. CCoV-1 isolates do not propagate easily in cell culture; CCoV-2 does propagate in cell cultures such as canine tumor fibroblast.282
Canine respiratory coronavirus (CRCoV).
First described in 2003, CRCoV is associated with respiratory disease with mild to severe clinical signs.139,363 It is considered an infectious agents in canine infectious respiratory disease (CIRD) and is commonly associated with respiratory disease outbreaks in kennels.139,321,363 CRCoV is closely related to bovine coronavirus.139 CRCoV is most likely transmitted via respiratory secretions, with dogs older than 1 y having greater seroprevalence.139 It has a high tropism for canine upper respiratory tissues, causing an acute mild respiratory infection with clinical signs such as a dry cough or nasal discharge.139,321,363 Clinical disease can worsen with coinfections of other respiratory pathogens.363 The cellular receptor used by CRCoV to infect host cells is currently unknown.
Feline coronavirus (FCoV).
Feline Coronavirus (FCoV), first described in 1977, can cause disease in both domestic and wild cats.229,417 Like CCoV, FCoV belong to the Alphacoronavirus genus (subgenus Tegacovirus) species Alphacoronavirus 1. FCoV has 2 serotypes (type 1 and type 2).213 FCoV-1 is considered the ancestor lineage and is the predominant virus circulating in domestic cat populations, which are approximately 20% to 60% seropositive.3,214,429 FCoV-2 emerged from a recombination between FCoV-1 and CCoV-2 and is less common.213,429 However, FCoV-2 is easier to propagate in cell culture, such that most studies use the less common virus.213 FCoVs are related to both canine enteric coronavirus and transmissible gastroenteritis virus of pigs.192 FCoVs have been studied intensely because the 2 biotypes can cause either asymptomatic or mild enteric clinical signs (Feline Enteric Coronavirus, or FECV), or a virulent, fatal systemic disease (Feline Infectious Peritonitis Virus, or FIPV).213,265,417 Both biotypes can occur with either serotype.213,429
FCoV is a highly contagious pathogen with a fecal-oral route of transmission.73,147,235 In animal shelters, multicat households, or catteries, an estimate of 90% seropositive rate may occur.74,429 The biotype FECV is often subclinical or causes mild transient gastrointestinal signs in cats.346,429 During primary infection, FECV is shed at higher levels in kittens than in adult cats.346 Cats may remain persistently infected, which results in a high seropositive rate in settings that house multiple cats. In contrast, the virulent biotype FIPV causes an immune mediated lethal disease known as Feline Infectious Peritonitis (FIP). The disease is most common in young cats (less than 3-y-old).209,230 Although the initial infection is like FECV, with the viral tropism affecting the intestinal epithelial cells, the virus mutates and gains the ability to enter and replicate in monocytes and macrophages.214,230 The mutation occurs on the S protein glycoprotein and allows more efficient replication in macrophages and monocytes,230,283 resulting in systemic distribution and severe disease in the affected cat. However, FIPV either is not shed or is shed at low levels, and therefore does not cause FIP epidemics.213,230,429 The severity of disease varies on host factors such as major histocompatibility complex (MHC) characteristics, cytokine responses, and the cell-mediated immune (CMI) response.2,230 Cats that with FIP mount a more robust humoral as opposed to CMI response; these varying responses result in the different clinical signs.230 FIP is characterized by its clinical presentation as effusive (wet), noneffusive (dry), or a combination of the 2.429 The effusive form has a rapid course due to vasculitis causing protein-rich fluid in body cavities. Cats with the noneffusive form have a stronger T-cell response than do cats with the effusive form.429 Genetic predisposition and immunosuppression caused by stress or other disease increase the risk of overt disease.230,429 FCoV uses APN as a cellular receptor.437
Swine Enteric Coronavirus Disease (SECD).
SECD refers to all swine coronaviruses that cause gastrointestinal disease, including swine transmissible gastroenteritis virus (TGEV), porcine epidemic diarrhea virus (PEDV), porcine deltacoronavirus (PDCoV), swine acute diarrhea syndrome-coronavirus (SADS-CoV), and the recently described chimeric swine enteric coronavirus (SeCoV).
TGEV belongs to the genus Alphacoronavirus (subgenus Tegacovirus), species Alphacoronavirus 1 (along with canine coronavirus, feline coronavirus, and porcine respiratory coronavirus). TGEV was first reported in 1946 in the United States as a highly infectious disease causing acute severe diarrhea and vomiting in pigs. TGEV is the oldest known swine disease caused by a coronavirus.132 The host cell receptor used by TGEV is APN, a multifunction protein that is expressed in several tissues including intestinal, renal, respiratory, and nervous.125,317 In addition, a second, unidentified cell receptor has been proposed for the intestinal villi of neonatal pigs.464 TGEV has an affinity for sialic acids, which facilitates enteric infections.394 Fatal infections are more common in piglets born to seronegative sows, approaching 100% piglet mortality rate.162,189 An endemic form of the disease occurs in herds with partial immunity or concurrent viral respiratory infections, with less severe signs and very low mortality.39,189,364 TGEV in piglets cause small intestinal epithelium atrophy and necrosis with reduced crypt height and depth, resulting in malabsorption syndrome; it also impairs the intestinal mucosal immune response, predisposing piglets to infection by other pathogens and by elevated expression of inflammatory cytokines.492 Infected sows can transmit virus to piglets in their milk or feces. Although small intestine villous epithelial cells are the main site of viral replication and feces are the major source of infection through the fecal-oral route, the virus also replicates in the upper respiratory epithelial cells and is shed through nasal secretions with potential airborne spread for over a short distance.58,449 Depending on the age of the pig, infection with TGEV results in viremia with wide viral distribution in the body.157 Fecal shedding generally lasts for 2 wk after exposure, and respiratory shedding for up to 11 d after exposure, but chronic carriers can shed for up to 104 d after infection.226,227,351,442 Transmission also occurs through fomites.
PEDV belongs to the genus Alphacoronavirus (subgenus Pedacovirus). Genetic analysis found that PEDV is closely related to the species Scotophilus bat coronavirus 512, suggesting that cross-species transmission possibly occurred between bats and pigs.19 PEDV was first described in Europe in 1971, in the 1990s in Asia, and not until 2013 in North America, as a highly infectious enteric disease characterized by acute gastroenteritis with watery diarrhea, vomiting, and dehydration.77,81,202,352,421,488 Infections are nearly 100% fatal in piglets born to seronegative sows. Transmission is fecal-oral but airborne transmission via the fecal-nasal route has also been described.10,103 PEDV was originally reported to use APN as a cell receptor,273 but later studies suggest an additional cellular receptor independent of APN for PEDV entry.215,399,472 Similar to TGEV, PEDV can also bind sialic acids.126,275 PEDV can infect multiple cell lines in vitro from species other than pigs, porcine including bats and primates.284 The virus can infect nasal epithelial cells and the dendritic cells in the nasal submucosa, which in turn delivers the virus to CD3 + T cells that are carried by blood and lymph circulation to the intestinal epithelial cells.279 PEDV mainly infects small intestine epithelial cells, causing atrophy of the intestinal villi and resulting in malabsorption and dyspepsia.221 One report suggests PEDV infects pig alveolar macrophages and may cause lesions in the lungs.343 Two different PEDV genotypes have been described based on the S gene; these are Genogroup 1 and Genogroup 2, which are further divided into subgenotypes.455 Natural recombination between the PEDV genotypes has been described along with recombination between PEDV and TGEV.4,55 This novel chimeric swine enteric coronavirus (SeCoV) contains a genome background identical to TGEV but expresses the S gene and 3a protein sequences from PEDV.41 SeCoV was isolated from all cases of diarrhea, supporting its virulence.4,41,55 SeCoV appears to continue to circulate in Europe and cause a disease very similar to PEDV.41 In addition to the novel chimeric SeCoV, the full-length genome sequence analysis of a PEDV field isolate in China (CH/HNQX-3/14) showed unique deletion regions in the S and ORF3 genes.275 Further analyses suggested that CH/HNQX-3/14 is a natural recombinant of the attenuated vaccine strains (CV777 and DR13) and the circulating wild-type strain (CH/ZMDZY/11).275 The recombination occurred not only in the structural protein-coding region (S1 and N genes) but also in the nonstructural protein-coding region (replicases 1a and ORF3 genes). These findings suggest that PEDV strains circulating in China underwent recombination between vaccine and field strains, contributing to the genetic diversity of PEDV.275
PDCoV belongs to the genus Deltacoronavirus (subgenus Buldecovirus), species Coronavirus HKU15. PDCoV was first described in 2012 in Hong Kong during a large coronavirus molecular survey of mammals and birds.487 Genetic analysis found PDCoV to be closely related to 2 avian deltacoronaviruses, suggesting a common avian coronavirus as an ancestor.220 Similar to PEDV and TGEV, PDCoV causes gastroenteritis characterized by watery diarrhea and vomiting in sows and nursing pigs. However, mortality in piglets is lower than that of PEDV and TGEV infections.406 Microscopic lesions include acute necrosis of intestinal epithelial cells with villus shortening and intestinal wall thinning, resulting in malabsorption.460 The main infection route appears to be fecal-oral.220 PDCoV uses APN as a cell receptor and have a second receptor that is not yet identified.497 PDCoV can experimentally infect calves, poultry, and human cell lines, making it a potential threat to public health and other farm animal species.497
SADS-CoV, also called swine enteric alphacoronavirus (SeACoV), belongs to the genus Alphacoronavirus (subgenus Rhinacovirus), and is considered the same species as bat coronavirus Rhinolophus bat coronavirus HKU2; both appear to descend from a common ancestor.509 SADS-CoV is the most recent swine coronavirus, first reported in China in 2017 as a cause of severe diarrhea with high mortality in neonatal piglets.342 Transmission is through the fecal-oral route.342,509 The cell receptor is currently unknown but in vitro studies suggest that SADS-CoV does not require any of the known coronavirus cell receptors to infect a variety of mammalian cell lines.136 Clinical signs are similar to other porcine enteric coronaviruses, which produce acute gastroenteritis characterized by vomiting, diarrhea, and high mortality in newborn piglets.342,509 The virus affects the small intestine, mainly the jejunum and ileum, causing necrosis of the epithelial cells resulting in atrophy and shortening of the villi.509
Porcine hemagglutinating encephalomyelitis virus (PHEV).
PHEV belongs to the genus Betacoronavirus (subgenus Embecovirus) species Betacoronavirus 1 along with bovine coronavirus, human coronavirus OC43, equine coronavirus, alpaca coronavirus, dromedary camel coronavirus UAE-HKU23, and canine respiratory coronavirus, and they likely share a common ancestor.206 PHEV was first described in Canada in1957 as causing vomiting, wasting disease, and encephalomyelitis in piglets; the virus was isolated a few years later.176,374 The disease is relatively infrequent because piglets are usually protected by maternal colostral antibodies until they develop resistance to the disease.293,325 Clinically, the piglets typically vomit after feeding and show anorexia, depression, and progressive emaciation. Piglets with neurologic signs may show dog-sitting posture, muscle tremors, opisthotonos, convulsions, paddling movements, or paralysis.67,175,176 The virus is shed in nasal secretions, and infection occurs through aerosols and contact with secretions from infected pigs.326 The virus first multiplies in the nasal epithelium, tonsils, lungs, and small intestine before spreading to the CNS via peripheral nerves.12,13 PHEV uses 9-O-acetylated sialic acid as a host cell receptor.301 The clinical signs appear to be related to viral infection of vagal sensory ganglia, inducing vomiting, and gastric myenteric plexuses, causing delayed emptying of the stomach.12 At necropsy, PHEV-affected pigs show cachexia, stomach distention containing nondigested milk, and, in chronically infected piglets, abdominal distension.293 Microscopic changes in piglets with neurologic signs may include lymphoplasmacytic perivascular cuffing and mononuclear cell infiltration, gliosis, neuronal death, and satellitosis affecting the gray matter of the cerebrum.468 In piglets with vomiting and wasting, degeneration of the ganglia of the stomach wall and lymphoplasmacytic perivascular cuffing are the most common findings.108,389
Porcine respiratory coronavirus (PRCoV).
PRCoV belongs to the genus Alphacoronavirus (subgenus Tegacovirus), species Alphacoronavirus 1, along with canine coronavirus, feline coronavirus, and TGEV. First described in Europe in1986, PRCoV causes a mild or subclinical respiratory disease in swine of all ages.350 PRCoV is a genetic variant of TGEV with a deletion of variable size in the spike protein that causes the loss of sialic acid binding activity with consequent changes in major tissue tropism from enteric to respiratory epithelium.392,394 PRCoV shares some epitopes for neutralizing antibodies with TGEV, resulting in PRCoV antibodies providing strong immunity against TGEV infection.45,112,138,470 Transmission is through respiratory droplets and aerosols. The virus uses APN as a cell receptor and preferentially targets nonciliated, nonmucus producing cells in the respiratory epithelium, replicating in tonsils, respiratory mucosal epithelium, and in both type I and II pneumocytes and causing inflammation and necrosis.102 PRCoV also infects, but to a very low degree, cells from the small intestine.102 The infection is usually asymptomatic but can cause mild fever, dyspnea, polypnea, anorexia, and, at necropsy, bronchiointerstitial pneumonia.102
Bovine coronavirus (BCoV).
Bovine coronavirus (BCoV) belongs to the genus Betacoronavirus (subgenus Embecovirus), a prototype of the species Betacoronavirus 1 along with HCoV-OC43, equine coronavirus, alpaca coronavirus, dromedary camel coronavirus UAE-HKU23, PHEV, and CRCoV, all caused by Betacoronavirus 1 species.206 The virus was first reported in 1972 as a coronavirus-like agent associated with spontaneous neonatal calf diarrhea with high mortality.409 Shortly thereafter a coronavirus was confirmed to be the cause of diarrhea by experimental infection of neonatal calves, and the virus was then quickly isolated and characterized.306,307 BCoV attaches to host cell surface sialic acids and appears to use human leukocyte antigen class I (HLA-1) as the entry receptor, resulting in wide viral cellular tropism.423 BCoV also contains a surface hemagglutinin-esterase (HE) glycoprotein that mediates reversible attachment to O-acetylated sialic acids by acting both as lectins and as a receptor-destroying enzyme (esterase) to reverse hemagglutination.384,503 BCoV causes 3 distinct clinical syndromes in cattle: neonatal calf diarrhea, “winter dysentery” in lactating cows, and “shipping fever”, a respiratory disease in feedlot cattle.384 Morbidity is high, but mortality is generally low, except in calves in which passive immunity from mother’s milk begins to wane.117 Viral shedding occurs through feces and nasal secretions, and transmission is via the fecal-oral route or through the inhalation of aerosols. Shedding usually lasts up to 10 d in calves and up to 45 d in adult cattle, but prolonged intermittent shedding has been reported in asymptomatic animals.222,338,384 Low titers of ocular viral shedding has also been reported.117 The virus initially replicates in the nasal mucosa and is believed to spread to the gastrointestinal tract after the animal swallows large quantities of the virus that is protected by mucous secretions, resulting in intestinal infection and fecal shedding.384 BCoV causes extensive necrosis of the large intestinal mucosa, resulting in malabsorption and severe loss of water and electrolytes that is more severe in very young animals.307 In adult cattle, the extensive mucosal intestinal necrosis is usually accompanied by hemorrhage.54,117 BCoV infection of the respiratory tract appears to predispose cattle to secondary bacterial infections aggravated by transport stress resulting in “shipping fever” pneumonia, characterized by an often-fatal fibrinous bronchopneumonia.143,416 BCoV-like coronaviruses have been found in different species of wild ruminants suggesting a potential role as reservoirs.7,439 BCoV was recently suggested to originate from a rodent CoV after a novel CoV species, phylogenetically intermediate between BCoV and MHV, was described in Norway rats in China (China Rattus Coronavirus HKU24). The finding of this new virus suggests rodents as possible reservoirs for CoVs in the subgenus Embecovirus and possible ancestors of BCoV.99,262
Equine coronavirus (ECoV).
Equine coronavirus (ECoV) belongs to the genus Betacoronavirus (subgenus Embecovirus), assigned to the species Betacoronavirus 1 along with HCoV-OC43, BCoV, alpaca coronavirus, dromedary camel coronavirus UAE-HKU23, PHEV, and CRCoV.206 ECoV was first isolated and characterized in 2000 from a neonatal foal with enterocolitis.110,180 However, reports of the association between coronaviruses and gastroenteritis in foals goes back to 1975.38,201 ECoV causes sporadic outbreaks and infections in horses in America, Europe, and Asia.151,167,170,188,320,332,368 The most common clinical signs include anorexia, fever, lethargy, and leukopenia, followed by diarrhea, colic, and less often, neurologic signs.46,151,167,302,368,369 ECoV infections are usually self-limiting or subclinical; however, one report in miniature horses found that 27% of the animals died or were euthanized.151,387 In severe cases, mortality may occur due to loss of intestinal mucosa barrier function, resulting in septicemia, endotoxemia, and hyperammonemia-associated encephalopathy.167 Pathology findings include diffuse necrotizing enteritis characterized by marked intestinal villus attenuation, necrosis of apical enterocytes with pseudomembrane formation, and hemorrhage with mucosal microthrombi.167 Horses with neurologic signs may have diffuse Alzheimer type II astrocyte hypertrophy and hyperplasia in the cerebral cortex.167 Experimental infection of horses with ECoV showed that infected horses intermittently excreted large amounts of virus in their feces for over 9 d after inoculation, regardless of the presence or absence of clinical signs, highlighting the significance of fecal-oral transmission.331,367,387 ECoV was also detected in nasal swabs from experimentally infected horses, suggesting that respiratory transmission may occur.331,367,387 Viremia was detected only in symptomatic horses.331 The cellular entry receptor has yet to be identified. Complete genome sequences of ECoV isolates from the United States and Japan show close sequence homology ranging from 98 to 99%.332 Phylogenetic analysis showed ECoV is most closely related to BCoV, HCoV-OC43, and PHEV, and may have emerged earlier despite not being isolated until 1999 from a foal with diarrhea.180,505 The ECoV nsp3 protein has considerable amino acid deletions and insertions compared with the nsp3 proteins of BCoV, HCoV-OC43, and PHEV.505
Ferret coronavirus.
Ferret coronaviruses belong to the genus Alphacoronavirus (subgenus Minacovirus). Ferret coronaviruses are closely related to Mink coronavirus 1 with a new species designation, Alphacoronavirus 2, more recently suggested for both ferret and mink coronaviruses.254 First reported in the United States in 1993 as epizootic catarrhal enteritis in domestic ferrets (Mustela putorius furo), the disease was associated with a coronavirus in 2000.475 Infection with ferret coronavirus can result in enteric or systemic disease. Systemic disease could be caused by a mutation of the coronavirus in the infected ferret; recombination in ferret coronaviruses resulting in novel strains have been recently described.254,318,428,493 Complete genome sequencing of enteric and systemic ferret coronavirus strains shows 89% nucleotide similarity, with much less similarity to other known alphacoronaviruses (50% to 69% nucleotide identity).276,431,479,480 The cellular entry receptors used by ferret coronaviruses have not been identified. Clinically, the enteric disease is characterized by profuse, bright green, mucoid diarrhea with a foul smell, along with anorexia, lethargy, and vomiting.475 Mortality is usually low. Severe disease is more common in older ferrets with concurrent diseases such as insulinoma, adrenal-associated endocrinopathy, and long-standing gastric infection with Helicobacter mustelae, while young ferrets often show mild disease and may be subclinical carriers.475 Lesions are limited to the gastroenteric tract and characterized by fusion and blunting of villi, vacuolar degeneration and necrosis of apical villous enterocytes, and lymphocytic enteritis.475 A second clinical form of the disease, ferret systemic coronavirus, was first reported in Spain in 2004; genetic analysis found this virus to be closely related to ferret enteric coronavirus.298 The disease is similar to the dry form of FIP in cats, with ferrets showing a systemic and progressive pyogranulomatous inflammatory disease with high mortality.161 Affected ferrets are usually young and may show a wide range of clinical signs including chronic weight loss, anemia, anorexia, vomiting, cough, fever, weakness, diarrhea, rectal prolapse, icterus, skin erythema, abdominal masses/organomegaly, heart murmurs, and neurologic signs.161,359 Blood and serum chemistry panels commonly show anemia, neutrophilic leukocytosis, thrombocytopenia, hyperproteinemia, hypergammaglobulinemia, hypoalbuminemia, azotemia, elevated alanine aminotransferase, and serum lipase.161,359
Mink coronavirus (MCoV).
Mink coronavirus (MCoV), or Mink Epizootic Catarrhal Gastroenteritis, belongs to the genus Alphacoronavirus (subgenus Minacovirus), species Mink coronavirus 1. The disease was first described in the United States in 1975 as mucoid diarrhea and anorexia over a 2 to 6-d course, particularly during the fall, with what seems genetic predilection in dark colored mink.256 Mortality is generally low (<5%) unless a concurrent viral or bacterial infection occurs.172,256 The etiological agent was identified in 1990 by electron microscopy as a coronavirus.172 Serologic studies showed that MCoV cross reacts with pig TGEV and PEDV.172 A more recent genomic analysis placed MCoV isolates in the Alphacoronavirus genus, closely related to ferret coronaviruses.454 MCoV appears to be common in farmed mink in North America, Denmark, the Netherlands, Russia, Belarus, Estonia, Latvia, Lithuania, and China.172 The presence of coronavirus particles in feces after natural and and experimental infection suggests that transmission may be fecal-oral with viral shedding beginning 2 d after infection and continuing for 2 wk.172 Some mink are asymptomatic carriers.172 The cellular receptor has not yet been identified.
Alpaca coronaviruses.
Alpaca enteric coronavirus.
Alpaca enteric coronavirus (ACoV) belongs to the genus Betacoronavirus (subgenus Embecovirus), a member of the Betacoronavirus 1 species complex, with sequence analysis showing a close relationships to BCoV (> 99.5% nucleotide identity), HCoV-OC43 (> 96%), and PHEV (> 93%).216 The disease was first reported in 1998 associated with outbreaks of severe diarrhea in young and adult llamas and alpacas.290,376,471 Other members of the Betacoronavirus 1 species complex use sialic acids or heparan sulfate on the cell surface for attachment but this has not been determined for ACoV.423 Gross lesions reported on a single animal included mixed watery and mucoid intestinal contents, diffuse thickening of the wall of the third gastric compartment, and mesenteric lymphadenopathy. Microscopically, the small intestine showed diffuse edema of the lamina propria and submucosa with multifocal petechia, necrotic debris within intestinal crypts, and fibrinopurulent hemorrhagic mesenteric lymph nodes.164 BCoV may be the ancestor of ACoV, with cross-species transmission occurring when cattle were introduced in South America 500 y ago, as New World camelids graze at lower altitudes during winter and share pastures with cattle.74,290,373
Alpaca respiratory coronavirus.
Alpaca respiratory coronavirus belongs to the genus Alphacoronavirus (subgenus Duvinacovirus). The virus was isolated in 2007 in association with an outbreak of acute respiratory disease and abortions in alpacas after participation in a large animal exposition.105 Genome sequencing suggests alpaca alphacoronavirus is closely related to HCoV-229E with 92% nucleotide identity.106 Spike gene sequences from alpaca alphacoronavirus and from HCoV-229E isolates recovered over several decades showed alpaca respiratory coronavirus to be most similar to HCoV-229E viruses isolated in the 1960s to early 1980s, suggesting that cross species transmission might have occurred during that time.106 No other outbreaks have been reported. Clinical signs vary from mild upper respiratory disease to severe respiratory distress, fever, and death.105 Abortions appear to be related to severe fetal hypoxia in pregnant alpacas with severe respiratory distress.105 Necropsy findings include marked pulmonary congestion with edema and pleural effusion.105 Microscopically, diffuse interstitial to bronchointerstitial pneumonia with congestion and edema were the most prominent findings, along with fibrin deposition and hyaline membrane formation on terminal airways and epithelial necrosis.105 The cellular receptor used by alpaca alphacoronavirus to infect the host cell is unknown but based on the close genetic relationship to HcoV-229E, and like most alphacoronaviruses, it may use APN for cell attachment.106
Coronaviruses in Research Species
Mouse hepatitis virus (MHV).
The species Murine coronavirus, better known as Mouse Hepatitis Virus (MHV), belongs to the genus Betacoronavirus (subgenus Embecovirus). Isolated in 1949, the virus was named Murine Virus JHM after J. Harold Mueller.29 This virus caused disseminated encephalomyelitis accompanied by extensive destruction of myelin in the CNS and focal necrosis of the liver.82 Two years later, a similar virus was isolated from young mice dying from hepatitis; the new virus was called Mouse Hepatitis Virus.168 The name mouse hepatitis virus prevailed, and later “lethal intestinal virus of infant mice” (LIVIM), a disease known for years and suspected to be of viral origin, was found to be caused by MHV.66,207 MHV is a natural pathogen of mice, with multiple strains described that differ in organotropism, virulence, and pathogenicity, and are broadly classified in 2 groups, enterotropic and polytropic.293 However, due to the inherent property of these viruses to constantly mutate and recombine within mouse populations, isolates show considerable overlap.293
Enterotropic MHV (LIVIM) is a, highly contagious infection, causing close to 100% mortality among infant mice when introduced to a naïve population.240 Common enteric strains of MHV that cause the characteristic intestinal disease in infant mice include MHV-Y, MHV-RI, MHV-D, and MHV-S/CDC.193,196,197,250,293 Enterotropic strains tend to be highly contagious and restricted largely to the intestine but, depending on the virus strain and host factors, can spread to other organs, mainly the liver, lymphoid tissue, spleen, and sometimes the brain.25,27,31 In neonates, enterotropic MHV induces rapid cytolysis of terminally differentiated enterocytes that line the intestinal villi. Infant mice have shallow slow-replicating intestinal crypt progenitors, allowing rapid loss of enterocytes after infection with enterotropic MHV. Affected mice show segmental epithelial necrosis, villus attenuation, mucosal erosion, and epithelial syncytia affecting the terminal small intestine, cecum, and proximal colon.27 As mice get older, the intestinal mucosa responds more quickly to the virus, regenerating at a higher pace and allowing replacement of the damaged mucosa.27 However, this usually results in mucosal hyperplasia, particularly in older pups, contributing to intestinal malabsorption and loss of fluids and electrolytes.28 Immunocompetent mice shed MHV in high titers in feces but clear the infection within 3 to 4 wk;25,30,35 however, several factors may influence the duration of infection, including the animal, genotype, and immune status of the mouse and the virus strain and route of infection.25,27,31,32 Disease susceptibility varies among immunodeficient mice depending on the specific genetic defect.28,37,196 Immune competent adult mice are susceptible to infection but do not normally show clinical disease.196,197 Once the virus becomes enzootic in a mouse breeding colony, no clinical disease is seen because the newborn pups are protected from infection by colostral maternal antibodies; however, subclinical infection occurs as passive immunity declines after weaning.26,195
Polytropic strains of MHV have primary tropism for upper respiratory epithelium, where they initially replicate and then disseminate hematogenously to other tissues and organs, primarily, pulmonary vascular endothelium, with secondary infection of hepatic, hemopoietic, and lymphoid tissues, causing acute necrosis and syncytia formation.28,29,36 Neurotropic strains can migrate hematogenously or directly from the olfactory epithelium to the brain through olfactory neural pathways, causing necrotizing encephalitis that affects neurons, glia, and endothelium.17,28,29,36 Surviving mice usually develop posterior paresis due to immune-mediated demyelination.422 Polytropic strains of MHV spread by direct contact but are usually less contagious than are enterotropic strains. Vertical transmission can occur in some polytropic MHV strains but does not appear to be the main mode of transmission.26 Like the enterotropic strains, disease outcome from polytropic strains depends on both host (genotype, age, and immune status) and viral factors (strain pathogenicity and tropism). In general, infant mice are more susceptible to severe disease, showing runting and neurologic signs, with reduced numbers weaned due to maternal cannibalism.28 Enzootic infections are subclinical in immune-competent mice but immune-deficient mice, particularly T cell deficient mice, may show wasting, neurologic signs, and death.29,197 Interferon-γ deficient mice may develop abdominal distention due to polyserositis.156 Some MHV strains, such as JHM, contain an additional structural protein, hemagglutinin-esterase (HE), which binds sialic acids on surface glycoproteins and contains acetyl-esterase activity, enhancing viral S protein-mediated mucosal cell invasion and spread.100 In contrast to MHV enterotropic strains, polytropic strains replicate in a wide variety of cells in vitro and can be a source of infection when injected into naïve mice.293 MHV uses carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1), a transmembrane glycoprotein that is expressed on epithelial, endothelial, and immune cells, as a virus cell receptor for attachment and invasion.424 However, susceptibility to some MHV strains appears to be related to an allelic variation of CEACAM1. For example, a strain-specific allelic variant (Ceacam1b) in SJL/J mice makes this strain resistant to infection as compared with C57BL/6J and other mouse strains that express the Ceacam1a allele.169,424 In addition, neurovirulent strains appear to use a different, yet to be determined, receptor-independent mechanism to infect neurons.43,44,322 Some common polytropic MHV strains include MHV-1, MHV-2, MHV-3, MHV-JHM (MHV-4), MHV-A59, and MHV-S.27,30–32,36,197 These polytropic viruses have been extensively studied as models of human neurologic diseases, hepatitis, and respiratory CoV infection.111,120,232,239,386 Clinically, hepatic lesions caused by MHV infection result in elevated liver enzymes, affect protein synthesis, increase iron uptake, cause anemia, thrombocytopenia, leukopenia, pancytopenia, and increase monocyte procoagulant activity leading to thrombosis.272,294 MHV causes marked immune modulation affecting both cell mediated and humoral responses.96,104,371,453,461 In addition, mice infected with the neurotropic strain MHV-JHM display an increase in multiple chemotactic cytokines in the CNS (MCP-1, MCP-3, MIP-1, MIP-2, and RANTES); spinal cord astrocytes of chronically-infected mice express TNF-α, IL-1 β, and IL-6.371,422 Astrocytes are considered to have a dual role in CNS pathophysiology, as they can both support regeneration and exert detrimental effects on surrounding cells and brain parenchyma.6,205
In infected colonies, mouse pups are initially protected by antibodies present in the colostrum of MHV-seropositive mothers, but the passive immunity lasts only 3 to 4 wk, after which the weanlings are susceptible to infection.26,195–197 Mice that survive the infection and recover develop strain-specific immunity.33,34 Genetically modified mice (that is, B cell-deficient mice, tumor necrosis factor knockout mice, and interferon-γ deficient mice) may shed MHV for prolonged duration and require rederivation of the affected colony using hysterectomy or embryo transfer.93,196,345,366 Although MHV is considered a mouse specific pathogen, persistent infection promotes cross-species transmissibility by selection of MHV strains that recognize phylogenetic homologues of the normal MHV receptor.23,190,191 Further supporting the potential cross-species transmissibility of Murine coronavirus, neurotropic MHV-JHM infected nonhuman primate brain tissue after peripheral inoculation.62 Regarding the origin of MHV, a new species of Betacoronavirus (subgenus Embecovirus), isolated from Rattus norvegicus in China, China Rattus coronavirus HKU24 (ChRCoV HKU24), is the parental strain of Betacoronavirus-1; interspecies transmission from rodents to other mammals occurred centuries ago, giving rise to human and bovine coronaviruses in the subgenus Embecovirus.262
Rat coronavirus (RCoV-P/SDAV).
In 1970, an MHV variant, later named Parker’s rat coronavirus (RCoV-P), was identified in a colony of research rats as the cause of respiratory epidemics in young rats.344 Two years later, another coronavirus was described in rats that caused infection in the lower respiratory tract, eye, lacrimal glands, and salivary glands; it was called sialodacryoadenitis virus (SDAV).51 Subsequent study revealed that RCoV-P can also cause sialodacryoadenitis, suggesting that RCoV-P and SDAV are most likely different strains of a coronavirus indigenous to rats.355 Despite having different glycoproteins as cellular receptors, mice can be experimentally infected with SDAV and develop a similar disease to SDAV in rats, but natural SDAV disease in mice has not been reported.50,159 Like MHV, rat coronavirus appears to have multiple strains.94,95,237,299 The structural proteins of the rat coronaviruses, RCoV-P and SDAV, are closely related to those of MHV and are not divergent enough to be considered a new species. All 3 viruses appear to have the same parental strain, most likely the recently identified China Rattus coronavirus HKU24 (ChRCoV HKU24) within the genus Betacoronavirus (subgenus Embecovirus).24,163,245,262,459,498 Like other coronaviruses, RCoV is highly contagious with direct, aerosol, and fomite transmission causing epizootics in naïve rat populations.50,94,158,247,293,344 Similar to MHV, genetics and age affect susceptibility to RCoV.49,50,94,344,355 Primary tropism is to nasal respiratory epithelium, with secondary spread to lacrimal glands, salivary glands, and lungs.48 Enzootic infections are usually inapparent or manifest as mild symptoms in very young rats.344 Epizootics are characterized by respiratory signs or keratitis with corneal ulceration, conjunctivitis, porphyrin staining around the eyes, and cervical swelling due to edema around the submandibular salivary glands.212,252 In both cases young rats are more susceptible to severe disease than are weanlings and older rats.344,481 Mortality is unusual but can occur in newborn rats or when secondary opportunistic infections occur.344 Microscopic changes include mild necrotizing rhinitis, laryngitis, tracheitis, bronchitis, bronchiolitis, and multifocal pneumonitis with a mostly lymphocytic inflammatory response.48,94,299,344,355,481 Recovered rats often show marked squamous metaplasia, more prominently in the Harderian glands.293 Permanent eye damage can occur as a result of lesions affecting the lacrimal gland function and filtration angle of the eye (that is, keratitis sicca, corneal ulcerations, hyphema, and megaloglobus).252,293 Recovered rats show short-lived immunity, with no cross-protection; reinfection with homologous rat coronaviruses can occur as early as 6 mo after the initial infection, with milder disease and less viral shedding than occurs after contact infection of virus-naïve controls.356,465 Immune deficient rats become chronically infected, can shed virus for at least 10 wk, and may progress to wasting syndrome and die from pneumonia.182,466 Acute infection with SDAV is diagnosed based on clinical signs and lesions; however, respiratory tract lesions cannot be distinguished from those caused by Sendai virus.281 SDAV infection strongly exacerbates Mycoplasma pulmonis disease, and RCoV infection enhanced nasal colonization with Haemophilus influenzae type B in infant rats.311,393
Guinea pig coronavirus.
In 1990, typical coronavirus-like virions were reported in association with diarrhea, anorexia, and wasting in 3 to 4-wk-old guinea pigs.210 Microscopically, the lesions were characterized by necrotizing enteritis with blunting and fusion of villi and syncytia that mostly affected the distal ileum.210 Persistent excretion of coronavirus-like particles in guinea pigs was reported.296 The prevalence of coronavirus-like virions in guinea pig colonies and its relationship to other coronaviruses is currently unknown, as is the cellular receptor the virus uses to attach and infect guinea pigs.293
Rabbit coronaviruses.
Rabbit enteric coronavirus (RECoV).
Initially described in the early 1980s, Rabbit Enteric Coronavirus (RECoV) has not been fully characterized.135,255,340,347 Analysis of structural polypeptides of the purified viral particles revealed a pattern similar to that of other coronaviruses, with the polypeptides cross reacting with 2 other coronavirus specific immune sera, avian IBV and porcine TGEV.128 RECoV appears to have some antigenic relationship with the HCoV-229-E.255RECoV has been reported in commercial rabbitries and research colonies in Canada and Europe.135,255,340,347 Serologic surveys suggest that RECoV is present in rabbitries in the United States with a prevalence ranging from 3% to 40%, with most seropositive rabbits being 4 mo of age or older.124,135 RECoV usually causes transient mild diarrhea in young (3- to 8-wk-old) rabbits, although one study reported very high mortality.127,135,340 In severe cases, rabbits can show lethargy, diarrhea, dehydration, emaciation, perineal fecal staining, and abdominal distention before dying.135,255,340 Gross lesions are usually characterized by cecal distention with mucosal inflammation and edema; cecal contents are watery and colored white to tan.135,255,340 The small and/or large intestines may also be affected.135 Microscopically, the lesions are characterized by villous blunting with vacuolation and necrosis of intestinal epithelial cells along with mucosal edema and polymorphonuclear and mononuclear inflammatory infiltrates.127,135,255,340 The virus shows tropism for gastrointestinal epithelium, but the cellular receptor is currently unknown. Rabbits acquire immunity as they age. The clinical signs of RECoV are not specific and should be differentiated from other causes of diarrhea in young rabbits (for example, coccidiosis, clostridiosis, colibacilosis, and rotavirus infection).353 In 2012, a novel Betacoronavirus, rabbit coronavirus HKU14 (RbCoV HKU14), was isolated and characterized from fecal samples from domestic rabbits in animal markets in Guangzhou, China.260 Molecular clock analysis using RNA-dependent RNA polymerase genes suggests that RbCoV HKU14 emerged relatively recently.260 Its relationship to RECoV is currently unknown.
Rabbit pleural effusion disease/Infectious cardiomyopathy virus (PED/ICV).
Pleural effusion disease/infectious cardiomyopathy virus (PED/ICV) was reported in Scandinavian countries in 1968 as a febrile illness causing deaths in rabbits inoculated with Treponema pallidum.179,219 A viral origin was suspected, and the virus was described by electron microscopy in 1982 as a coronavirus.179,340 PED/ICV was found as a contaminant in treponemal suspensions in laboratories in Europe, the United States, and Japan.148 The viral gene sequence is unknown, but the available data suggest that it is an alphacoronavirus. PED/ICV is unlikely to be a natural pathogen of rabbits because it is only found in rabbits inoculated with contaminated stocks of Treponema pallidum, suggesting a different species, possibly human, as its origin.340 PED/ICV is a multisystemic disease resembling some aspects of FIP with pathogenicity varying according to the isolate.149 Clinical signs vary and may include fever, anorexia, weight loss, muscular weakness, tachypnea, iridocyclitis, circulatory compromise, and death.88,149,150,152,340,402 Infected rabbits can show transient lymphopenia and hypoalbuminemia, heterophilia, and increased serum levels of potassium, lactate dehydrogenase, and γ-globulin.150 Necropsy findings depend on the stage of the disease; the acute phase may include pleural effusion, lung edema, and right ventricular dilatation, while rabbits surviving the first week may have ascites and subepicardial and subendocardial hemorrhages.150,340 Microscopic findings include multifocal myocardial degeneration and necrosis with little or no inflammatory response, hepatic focal necrosis, hepatosplenomegaly, lymphoid depletion of splenic follicles, lymph node depletion or reactive hyperplasia, depletion and focal degenerative changes of the thymus, mild proliferative changes in glomerular tufts, and mild anterior uveitis.88,150,152,340,402 The cellular receptor used by PED/ICV is currently unknown.
Nonhuman primate coronavirus.
Coronavirus-like particles in nonhuman primate fecal samples were first reported in 1979.69 Coronavirus-like particles have been reported in both normal and diarrheal stool samples from chimpanzees, baboons, macaques, and marmosets.377,404,462 The virus or viruses have not been isolated and lack characterization. Infection prevalence of up to 43% was reported in a large NHP colony with a prevalence of 49% in animals with diarrhea and 38% in those with normal feces.404 Infection prevalence appears to be higher in older animals, and rarely affects nonweaned monkeys, suggesting colostral protection against infection and the fecal-oral route of infection.404 Fecal viral excretion appears to persist after weaning.69,404 Immunoblotting studies done on serum from marmosets with coronavirus-like particles and diarrhea suggest the virus is antigenically related to bovine enteric coronavirus but not the porcine transmissible gastroenteritis virus.377 The cellular receptor used by the virus to attach to and infect nonhuman primates is unknown.
Coronaviruses of Wild Animals
All known human CoVs originated in animals,257 with bats and birds believed to be the ancestral hosts for all CoVs.174,203,257,427 The natural reservoir of the SARS-related CoV and the most likely origin for the 2002 SARS-CoV outbreak was the horseshoe bat (Rhinolophus spp.).257,451 While the natural reservoir for the SARS-CoV-2 has not been formally identified, the genome sequence of the virus is most closely related to bat coronaviruses.335,397,510 While bats are considered the natural reservoir for most alpha- and beta-coronaviruses, other mammals usually act as intermediate hosts before eventually infecting humans. In the 2002 SARS-CoV outbreak, the Himalayan palm civet (Paguma larvata) was identified as the primary, intermediate host for the virus between bats and humans.131,178,278 The intermediate mammalian host for SARS-CoV-2 was initially thought to be the Malayan pangolin (Manis javanica) due to sequence similarity in coronaviral isolates from captive pangolins;253,285 however, more recent analysis has questioned this determination.463 Ferrets and cats are highly susceptible to SARS-CoV-2 [via experimental infection];297 whereas dogs have low susceptibility, and pigs, chickens, and ducks are not susceptible to the virus.397 SARS-CoV2 has been transmitted from humans to farmed mink in the Netherlands and back to humans.339,341 SARS-CoV isolated from humans can infect and be transmitted by domestic cats and ferrets; however, these animals can also clear the infection.278 The porcine CoV, TGEV, and canine and feline CoVs can cross-infect pigs, dogs, and cats with varying disease phenotypes and levels of cross-protection in the heterologous host.236,381,382 Several BCoVs or bovine-like CoVs were identified as pathogens of enteric and/or respiratory diseases in ruminants, dogs, birds, and even humans.7,11
The capture, farming, and trade of wild animals are suspected to be major contributors to the emergence and spread of coronaviruses to humans, especially SARS-CoV and SARS-CoV-2.203,487 The stress of poor nutrition and overcrowded conditions lowers their immune competence and makes them more susceptible to infections. These factors also result in increased shedding of coronaviruses by infected animals around human habitation and along the supply chain for human consumption.203,487 In the 2002 SARS-CoV outbreak, captive, Himalayan palm civets (Paguma larvata) at Chinese wet markets tested positive for SARS-CoV, with some developing respiratory disease; whereas, palm civets in the wild were negative.278 Evidence of SARS-CoV-like infections has also been observed in many other marketed species, including the cat (Felis catus), the red fox (Vulpes vulpes), and the Chinese ferret badger (Melogale moschata).278 Farms that raise wild species are abundant in Asia, with over 6,000 registered wildlife farms in Vietnam in 2014 holding over 1 million animals.203 In Vietnam, 34% of wild, captive, field rats (Rattus spp. and Bandicota spp.) and 75% of insectivorous bats in guano farms were PCR-positive for coronaviruses.203
As discussed in the previous section on domestic animals, coronaviruses can significantly affect domestic agricultural species. BCoVs cause significant respiratory and enteric disease in cows and other domestic ruminants and are also an important pathogen in a wide variety of captive and free-range wild ruminants around the world (Figure 4). Most of the viruses isolated from wild ruminants are biologically and genetically similar to BCoV and are often called bovine-like CoVs.11
Figure 4.
Bovine-like Coronaviruses reported in captive or free-range, wild ruminants between 1981–2019. ND: not defined. Adapted from reference 11.
Most cases of CoV disease in wild ruminants have been reported in wild animal parks around the world and include dromedary camels (Camelus dromedarius) in Wisconsin, giraffes (Giraffa camelopardalis) in Ohio, and musk oxen (Ovibox moschatus) in England.11 Most reports of disease in wild ruminants have involved the gastrointestinal tract. A survey of free-roaming deer found that 7% of the white-tailed deer (Odocoileus virginianus) in Ohio and 9% of the mule deer (Odocoileus hemionus) in Wyoming were seropositive for antibodies to BCoV.382 SARS-CoV-2 also infects white-tailed deer, presumably binding to their ACE2 receptor,109 and could be an important reservoir host in the United States.97,183,243
FCoVs have been widely reported in both domestic and wild cats. Most cases of FCoV cause mild enteric disease, termed feline enteric coronavirus (FECV); however, feline infectious peritonitis (FIP) is caused by a rare but highly lethal “mutant” form of FECV (FIPV) that can be found in approximately 10% of domestic or feral cats that are seropositive for FCV.59,73 The cheetah (Acinonyx jubatus) is especially sensitive to FIPV.142,417 FIP has also been reported in a wild mountain lion (Puma concolor) in California.411 FCoVs were detected in numerous captive Felidae species in zoological parks in the United States (Figure 5). As stated before, the Himalayan palm civet (Paguma larvata) was found to be the intermediate host for SARS-CoV.278 CoV has been detected in Asian leopard cats (Prionailurus bengalensis) in Chinese wet markets.131 In 2020, multiple large cats, including a Malayan tiger (Panthera tigris jacksoni), 2 Siberian tigers (Panthera tigris tigris), and 3 African lions (Panthera leo), at the Bronx Zoo tested positive for SARS-CoV-2. All were reported to have developed a dry cough.271 In addition, 9 Asiatic lions (Panthera leo persica) tested positive for the SARS-CoV-2 B.1.617.2 (Delta variant) at a zoological park in Chennai, India, with 4 developing acute respiratory signs, 3 of which died.319
Figure 5.
Feline Coronavirus reported in US captive wild cats (2002). Adapted from reference 229.
Canine coronavirus has most often been associated with mild enteric disease,430 but some strains have caused severe respiratory disease139,362 or lethal systemic disease in domestic canines.61 Reports of disease in wild canines are sparse. Coyotes (Canis latrans) with enteritis are often found to be infected with both canine parvovirus and CCoV.502 In 1985, 61% of the captive coyotes maintained at a U.S. Sheep Experiment Station in Idaho had antibodies to CCoV,154 and 70% (167/240) of wolves (Canis lupus) captured during spring in Alaska between 1994 to 1999 tested positive for CCoV antibodies502
Swine coronaviruses can be found in wild or feral swine populations and are believed to provide a reservoir for domestic swine exposures.310 The feral swine population in the United States is estimated at approximately 5 to 6 million.47 Between 2012 to 2015, approximately 8,000 feral swine were tested for CoV in the United States, with 253 (3%) testing positive for either PEDV or TGEV.47
Avian coronaviruses fall into the Deltacoronavirus or Gammacoronavirus genera and are known to infect numerous domestic and wild birds. Avian coronaviruses have been found in wild birds on every continent.78 Several CoVs, including the most economically important, avian CoV, IBV, have been detected in healthy wild birds, which are believed to serve as a reservoir for domestic birds.89,314 Gammacoronaviruses are found predominantly in Anseriformes birds (waterfowl, for example, geese, ducks, and swans), whereas Deltacoronaviruses have been detected in Ciconiiformes (storklike), Pelecaniformes (medium to large water birds), and Anseriformes birds.89 A list of coronaviruses isolated from wild birds is presented in Figure 6.
Figure 6.
Avian Coronaviruses reported in wild birds. Adapted from references 78, 89, and 134.
While most mammalian coronaviruses are classified into the Alphacoronavirus and Betacoronavirus genera, a few fall into the Gammacoronavirus (captive Beluga whale: Delphinapterus leucas; and Bottlenose dolphins:Tursiops aduncus and T. truncatus)312,457,485 and Deltacoronavirus (Asian leopard cat: Prionailurus bengalensis)131 genera.
Diagnosis and Treatment of Coronaviral Diseases
Currently reverse transcriptase polymerase chain reaction (RT-PCR), using clinical samples, is the most commonly used method for diagnosis of active infection, particularly in well characterized CoVs, like domestic fowl, canine, feline, swine, bovine, equine, ferret, alpaca, mouse, rat, and human coronaviruses.92 Serologic assays like, enzyme linked immunosorbent assay (ELISA), immunofluorescence (IF), and serum neutralization tests are used to test for prior exposure, and IF and immunohistochemistry (IHC) are used for detection of viral antigens in affected tissues.71 Virus culture and isolation are used to confirm diagnosis and electron microscopy (EM) is used to demonstrate characteristic virus morphology in clinical samples after ruling out other diseases that can cause similar clinical signs.106,195,304,418,449 EM is more often used in less studied/characterized coronaviruses like guinea pig, rabbit, and nonhuman primate coronaviruses.347,353
This section provides examples of the diagnostic methods used to detect and diagnose CoVs in some of the different species. For felines, diagnosis of FIP is based on a combination of signalment, history, clinical signs, and clinical assays along with RT-PCR and IHC in clinical samples.230 In the case of swine coronaviruses, diagnosis of the specific virus causing SECD can be complicated because CoV coinfections can occur in swine. TGEV diagnosis can be made by IF, IHC, ELISA, and virus isolation, but these methods do not differentiate TGEV from PRCoV.293 ELISA using monoclonal antibodies against the TGEV peplomer and RT-PCR using specific primers can be used to detect and differentiate TGEV from PRCoV.63,489 PEDV diagnosis can be confirmed by virus isolation in primary porcine cell culture or in Vero cells with added trypsin, or IF or IHC to detect viral antigens in affected tissues, or RT-PCR molecular assays using clinical samples, or serologic assays like ELISA to monitor for prior exposure by demonstration of antibodies in convalescent animals.129 SeCoV-infected pigs seroconvert against PEDV but test negative in a TGEV-specific ELISA that detects antibodies against the S protein. Specific detection of the chimeric SeCoVs either requires the development of a new diagnostic RT-qPCR assay or the combined use of assays targeting the PEDV S-gene and another part of the TGEV genome.41 PDCoV diagnosis can be made using virus culture and isolation and observation of the cytopathic effect, and with IF, IHC, ELISA, and RT-PCR.504 RT-PCR based tests have been designed to diagnose SADS-CoV.342,509 An indirect ELISA to detect IgG antibodies using a recombinant plasmid that expresses the spike protein of SADS-CoV was recently reported.349 PRCoV diagnosis is made by virus isolation or RT-PCR testing of nasal swabs or tissue samples collected from the trachea and lungs, with specific primers used to differentiate it from TGEV.234 In addition, IF, IHC, and ELISA, using monoclonal antibodies to detect PRCoV antigen in specimens, is preferred over serology due to crossreactivity with TGEV.401 Because the disease is usually mild and recovered pigs are resistant to TGEV, little effort has been made to develop specific treatments or vaccines to prevent the disease.293 MCoV cross react with pig TGEV and PEDV on serologic assays.172 PED/ICV cross react with several alphacoronaviruses in serologic assays, including HCoV-229E, FIPV, CCoV, and swine TGEV.402,403
Currently, specific treatments are not available for CoVs that affect companion and farm animals but active research is ongoing.209,230 When vaccines are available, they will provide only partial protection because immunity is strain-specific and CoVs are known for their high mutation rates and frequent recombination.52,354 Primary medical management is supportive and includes treatments for fluid and electrolyte balance, resolution of severe leukopenia, systemic inflammation, and metabolic disturbances.46,369 In the case of ferret systemic coronavirus, immune suppressive drugs may slow down disease progression.327 Two approaches are available for FIP. As FIP is an immune-mediated disease, the first treatment approach is to modulate the immune response using drugs such as corticosteroids. This is a palliative treatment, with cats surviving weeks or months.209,230 Cytokines have also been used to modulate the immune response with limited success and higher survival rates in cats with the dry form of FIP.230 The second approach is to use experimental antiviral compounds to inhibit FCoV replication by targeting proteases necessary for viral protein cleavage.230,303
Control measures for CoVs include strict sanitation and management practices to eliminate the virus from the environment and prevent reintroduction because animal populations may clear the virus with time if new introductions are avoided.414 For example, spread of MHV can be prevented by temporary cessation of breeding and avoiding the introduction of MHV-naive mice.
Extensive research during the COVID-19 pandemic has resulted in the United States Food and Drug Administration (FDA) approval of the first antiviral drug, remdesivir (Veklury), specific for the treatment of COVID-19 patients. Remdesivir may be prescribed for people who are hospitalized with COVID-19 and need supplemental oxygen or have a higher risk of serious illness. In addition, the FDA has given emergency use authorization to several drugs that have antiviral and/or antiinflammatory properties (Paxlovid, Molnupiravir, Baricitinib, and Tocilizumab), monoclonal antibodies (Sotrovimab, Evusheld, and Bebtelovimab), and convalescent immune plasma to treat and/or prevent COVID-19 infection.443
Coronaviral Vaccines
The 2019 SARS-CoV-2 pandemic spurred the most rapid vaccine development in history. Prior to 2020, the average timeline for vaccine development was 5 to 10 y.218 However, within 9 mo of the World Health Organization declaring SARS-CoV-2 a worldwide pandemic (March 2020), 3 vaccines were approved for emergency use in humans [Sputnick V – Gam-COVID-Vac,287 Moderna mRNA-1273,444 and Pfizer BNT162b2445]. As of September 2021, 8 SARS-CoV-2 vaccines are currently in use worldwide.491 Significant research into human coronaviral vaccines took place with the outbreak of SARS-CoV in 2003 and MERS-CoV in 2008, with some going to phase 1 clinical trials; however, vaccines for coronaviral diseases of animals have been used for over 50 y and played an important role in our understanding of mammalian and avian immune responses to coronaviruses.
Coronavirus vaccines for chickens.
Infectious Bronchitis Virus (IBV) is a major disease of domestic chickens (Gallus gallus domesticus) and causes significant morbidity and mortality and economic losses.72,433 Vaccines have been used against IBV since the 1960s, and before 2020 were the only licensed vaccines targeting respiratory coronaviral diseases.70,383 Hundreds of IBV serotypes (or strains) have been isolated, with the majority of differences occurring in the S1 subunit of the spike protein, which is the primary inducer of protective immunity.181 As such, vaccines used worldwide usually contain one or more variants affecting that specific region. For example, vaccines used in North America most often target the Massachusetts (M41), Arkansas, and Connecticut strains; vaccines in Europe most often cover the 4/91 and D274 strains; and vaccines in China target the QX strain.433 Newborn chicks are usually vaccinated at one day of age with a live attenuated vaccine via a course spray. Meat-producing chickens usually only receive the single dose; whereas birds for breeding and egg production will receive multiple doses at 2, 4, and 6 wk of age.433 Currently, over 80 USDA-licensed vaccines are available against IBV, with most containing multiple serotypes and used in combination with other viral vaccines and bacterin components (Figure 7).
Figure 7.
USDA-Licensed chicken coronaviral vaccines.
Coronaviral vaccines for canines.
Two separate coronaviruses cause mild enteric [Alphacoronavirus (CCoV-1)] or respiratory [Betacoronavirus (CRCoV)] disease in dogs. Commercially available inactivated and modified-live vaccines are available for the enterotropic but not the respiratory virus433 (Figure 8). Vaccination protects from disease but not from infection, and virus can be shed in the feces.433 The American Animal Hospital Association (AHAA) currently does not recommend canine coronaviral vaccinations because infection: (1) causes mild or subclinical disease, (2) generally occurs in dogs 6 wk of age and younger, and (3) is typically self-limiting.153
Figure 8.
USDA-Licensed canine coronaviral vaccines.
Coronaviral vaccines for felines.
FCoV infections generally cause subclinical or mild enteric disease. FIP is a lethal form of FECV that arises from an enhanced immunologic response in a subset of cats. Only one USDA-licensed vaccine (FeloCell FIP - Zoetis) is currently available against FIPV (Figure 9). The vaccine is an attenuated, temperature-sensitive strain for intranasal administration in healthy cats 16 wk of age or older. The manufacturer states that the attenuated strain can replicate only in the respiratory tract and cannot spread systemically. The AHAA does not recommend vaccination of pet cats for FIP “because of its questionable ability to uniformly prevent disease in North American cat populations.”415 Only FCoV-seronegative cats can receive the vaccine, and most cats born in environments with a high incidence of FCoV become infected prior to 16 wks of age, making vaccination ineffective.388
Figure 9.
USDA-Licensed feline coronaviral vaccines.
Coronaviral vaccines for swine.
Six known CoVs cause gastrointestinal or respiratory disease in swine, including the alphacoronaviruses TGEV, PRCoV, PEDV, and SADS-CoV; the betacoronavirus, PHEV; and the deltacoronavirus, PDCoV.433 To date, vaccines have been developed only for TGEV and PEDV.
Several vaccines have been developed worldwide against TGEV. Two USDA- licensed TGEV vaccines are currently available in the United States (Figure 10). Both contain a modified-live TGEV in combination with a modified-live rotavirus. One of these vaccines also contains Clostridium perfringens Type C toxoid and Escherichia coli bacterin components. Because suckling pigs (1 to 2 wk of age) are the most TGEV-susceptible population and vaccination of sucklings does not provide the protective immunity during the susceptible window for disease, vaccines are used in pregnant sows that in turn provide protective antibodies to sucklings via passive transfer in the milk.165,383 The vaccine is given to pregnant sows/gilts via both intranasal and intramuscular routes, usually about 2 to 4 wk before farrowing. PRCoV arose as an S protein variant of TGEV with tropism for the respiratory epithelium but shares many epitopes of TGEV. Respiratory disease from PRCoV is generally mild, and neutralizing antibodies to PRCoV cross react with TGEV and have dramatically reduced TGEV outbreaks.395 Therefore, PRCoV is considered a natural “vaccine” against TGEV, and little effort has been made to develop specific treatments or vaccines to prevent the disease.395
Figure 10.
USDA-Licensed porcine coronaviral vaccines.
Numerous vaccines have also been developed worldwide against PEDV.165 Two USDA-licensed vaccines for PEDV are currently available: a killed virus (Zoetis) and an RNA particle platform vaccine [Intervet (Harrisvaccines) – MERCK] (Figure 10). As with TGEV, the highest mortality from PEDV occurs in suckling piglets, 1 to 2 wk of age. Therefore, vaccination of pregnant sows to provide lactogenic passive immunity is the regimen currently used.
Coronaviral vaccines for bovines.
Bovine coronaviral diseases most often cause severe diarrhea in newborn calves, ‘winter dysentery’ in adult cows, or an infectious respiratory disease (‘shipping fever’) in cows of all ages.384 As with the swine enteric coronaviral diseases, the most susceptible population to enteric disease is newborn calves, and vaccination of pregnant cows prior to calving and lactogenic transfer of neutralizing antibodies is the primary method for protection against calf diarrhea.433 Oral and intranasal vaccines against neonatal calf diarrhea are also available for newborn calves. While many of the vaccines report protection against severe disease, their efficacy is been questionable because immunity does not prevent reinfection or viral shedding.79,87,137 A list of current USDA-licensed BCoV vaccines is provided in Figure 11. While no licensed vaccines are available for BCoV respiratory disease, the intranasal administration of a modified live virus vaccine against the enteric BCoVs seems to provide some protection.118 A commercially available BCoV vaccine induces modest antibody titers against ECoV in horses; however, challenge studies have not been performed to determine whether the generated antibodies will protect against ECoV.330,365
Figure 11.
USDA-Licensed bovine coronaviral vaccines.
Coronaviral vaccines for mustelids.
Domestic ferrets (Mustela putorius furo) and mink (European: Mustela lutreola and American: Neovison vison) are highly susceptible to infections with human coronaviruses including SARS-CoV and SARS-CoV-2.90,238,323,378,396 Since the start of the COVID-19 pandemic, numerous reports have appeared of SARS-CoV-2 infections in farmed and feral mink and passage of SARS-CoV-2 from captive mink to humans.238,339,341,400 While no coronavirus vaccines are currently licensed for pet ferrets or farmed mink, the US Department of Agriculture (USDA) Center for Veterinary Biologics issued a notice in November 2020 calling for product license and permit applications for vaccines against SARS-CoV-2 in mink. Two United States companies (Zoetis and Medgene Labs) are currently developing mink coronaviral vaccines for USDA licensure.173 While SARS-CoV-2 infection has not been reported in the endangered, black-footed ferret (Mustela nigripes), the US Geological Survey (USGS) under the authority of the Fish and Wildlife Services (USFWS) is testing a SARS-CoV-2 vaccine in a small population of captive black-footed ferrets.267
Vaccine-associated Disease Enhancement
The mammalian immunologic response to viral infections results from a combination of the innate and adaptive immune systems with the goal of clearing the virus. These immune responses often lead to host tissue destruction at the site of infection and in some cases can exacerbate the disease, as reported for human immunodeficiency virus (HIV), respiratory syncytial virus (RSV), hepatitis-B virus (HBV), hepatitis-C virus (HCV), and possibly SARS-CoV and SARS-CoV-2 infections in humans.269,358 One mechanism by which this can occur is antibody-dependent enhancement (ADE) of viral infectivity, in which the uptake of antibody bound viruses by macrophages allows their enhanced replication and dissemination. ADE is one of the primary mechanisms behind the pathogenesis of FIP.269,358 Vaccine-associated disease enhancement (VADE) has been reported for numerous viral vaccines and is associated with both ADE and immunopathological responses of Type 2 T helper cells.419 VADE has been reported with the FIP vaccine,358 PEDV,499 and experimental vaccines in mouse models of SARS-CoV.438
Conclusion
Many species of domestic and wild animals carry CoVs, with some known to carry beta-CoVs closely related to SARS-CoV, MERS, and SARS-CoV-2 and some having a wide geographic distribution in nature. With continued human population expansion, resulting in closer contact with animal ecosystems, an increased risk of virus spillover from animals to people is illustrated by the increased frequency of viral disease outbreaks of zoonotic origin in the last 20 y. Wild animal trade for human consumption and the exotic pet industry create high-risk situations for cross-species transmission of CoVs and other potential zoonotic pathogens. Captive wild animals may show increased susceptibility to infections due to immune suppression secondary to capture stress, poor husbandry and overcrowded conditions in unregulated “wet markets,” creating the perfect opportunity for potential interspecies transmission of disease. In the case of coronaviruses, this situation provides an environment that supports the creation of new pathogens through mutations and recombination in the new host. Experience has shown that developing effective therapeutics and vaccines for pathogenic agents can take years. Furthermore, a vaccine may not be available for a new infectious disease even after years of intensive research, as is the case with some diseases that have affected humans for many decades (for example, AIDS, dengue, and malaria). CoVs are notorious for responding poorly to therapeutics and vaccines, despite many years of research, and effective treatments or vaccines are not available for SARS-CoV, MERS, or any of the seasonal CoVs that affect humans. In domestic animals, most coronaviral vaccines provide only short, strain-specific protection against severe disease without sterile immunity, requiring multiple booster immunizations throughout the life of the animal. This feature allows coronaviruses to persist in animal populations and continue to be a significant threat to the farm animal industry. With the recent development of vaccines against SARS-CoV-2, we are learning that, as with veterinary coronaviral vaccines, the immunity provided by SARS-CoV-2 vaccines protects the infected person from developing severe disease but does not provide sterile immunity or stop viral shedding, with immunity appearing to be short-lived and requiring booster immunizations. Pandemics will continue to be a significant threat to human society. Preventing inter-species transmission by maintaining ecosystem boundaries at the animal/human interface is currently the best approach to avoiding future pandemics of zoonotic origin. We agree with others who recommend restricting or banning the trade of wild animals in live animal markets to reduce the risk of future coronavirus or other zoonotic pandemics.
Acknowledgments
This study was supported by the Intramural Research Program of the National Institutes of Health, National Institute of Allergy and Infectious Diseases, Comparative Medicine Branch, National Human Genome Research Institute, Office of Laboratory Animal Medicine, and the National Institute of Environmental Health Sciences, Comparative Medicine Branch.
References
- 1.Abraham S, Kienzle TE, Lapps W, Brian DA. 1990. Deduced sequence of the bovine coronavirus spike protein and identification of the internal proteolytic cleavage site. Virology 176:296–301. 10.1016/0042-6822(90)90257-R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Addie DD, Kennedy LJ, Ryvar R, Willoughby K, Gaskell RM, Ollier WER, Nart P, Radford AD. 2004. Feline leucocyte antigen class II polymorphism and susceptibility to feline infectious peritonitis. J Feline Med Surg 6:59–62. 10.1016/j.jfms.2003.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Addie DD, Schaap IAT, Nicolson L, Jarrett O. 2003. Persistence and transmission of natural type I feline coronavirus infection. J Gen Virol 84:2735–2744. 10.1099/vir.0.19129-0. [DOI] [PubMed] [Google Scholar]
- 4.Akimkin V, Beer M, Blome S, Hanke D, Höper D, Jencke lM, Pohlmann A. 2016. New Chimeric Porcine Coronavirus in Swine Feces, Germany, 2012. Emerg Infect Dis 22:1314–1315. 10.3201/eid2207.160179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Tawfiq JA, Hinedi K, Ghandour J, Khairalla H, Musleh S, Ujayli A, Memish ZA. 2014. Middle East respiratory syndrome coronavirus: a case-control study of hospitalized patients. Clin Infect Dis 59:160–165. 10.1093/cid/ciu226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albrecht PJ, Murtie JC, Ness JK, Redwine JM, Enterline JR, Armstrong RC, Levison SW. 2003. Astrocytes produce CNTF during the remyelination phase of viral-induced spinal cord demyelination to stimulate FGF-2 production. Neurobiol Dis 13:89–101. 10.1016/S0969-9961(03)00019-6. [DOI] [PubMed] [Google Scholar]
- 7.Alekseev KP, Vlasova AN, Jung K, Hasoksuz M, Zhang X, Halpin R, Wang S, Ghedin E, Spiro D, Saif LJ. 2008. Bovine-Like Coronaviruses Isolated from Four Species of Captive Wild Ruminants Are Homologous to Bovine Coronaviruses, Based on Complete Genomic Sequences. J Virol 82:12422–12431. 10.1128/JVI.01586-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alfano F, Dowgier G, Valentino MP, Galiero G, Tinelli A, Nicola D, Fusco G. 2019. Identification of pantropic canine coronavirus in a wolf (Canis lupus italicus) in Italy. J Wildl Dis 55:504–508. 10.7589/2018-07-182. [DOI] [PubMed] [Google Scholar]
- 9.Aljasim TA, Almasoud A, Aljami HA, Alenazi MW, Alsagaby SA, Alsaleh AN, Alharbi NK. 2020. High rate of circulating MERS-CoV in dromedary camels at slaughterhouses in Riyadh, 2019. Viruses 12:1215. 10.3390/v12111215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alonso C, Goede DP, Morrison RB, Davies PR, Rovira A, Marthaler DG, Torremorell M. 2014. Evidence of infectivity of airborne porcine epidemic diarrhea virus and detection of airborne viral RNA at long distances from infected herds. Vet Res 45:73. 10.1186/s13567-014-0073-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amer HM. 2018. Bovine-like coronaviruses in domestic and wild ruminants. Anim Health Res Rev 19:113–124. 10.1017/S1466252318000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andries K, Pensaert M, Callebaut P. 1978. Pathogenicity of hemagglutinating encephalomyelitis (vomiting and wasting disease) virus of pigs, using different routes of inoculation. ZentralblVeterinärmed B 25:461–468. 10.1111/j.1439-0450.1978.tb00754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andries K, Pensaert MB .1980. Virus isolated and immunofluorescence in different organs of pigs infected with hemagglutinating encephalomyelitis virus. Am J Vet Res 41:215–218. [PubMed] [Google Scholar]
- 14.Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A, Hawa H, Alothman A, Khaldi A, Al Raiy B. 2014. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med 160:389–397. 10.7326/M13-2486. [DOI] [PubMed] [Google Scholar]
- 15.Arbour N, Day R, Newcombe J, Talbot PJ. 2000. Neuroinvasion by human respiratory coronaviruses. J Virol 74:8913–8921. 10.1128/JVI.74.19.8913-8921.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armstrong J, Niemann H, Smeekens S, Rottier P, Warren G. 1984. Sequence and topology of a model intracellular membrane protein, E1 glycoprotein, from a coronavirus. Nature 308:751–752. 10.1038/308751a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bailey OT, Pappenheimer AM, Cheever FS, Daniels JB. 1949. A murine virus (jhm) causing disseminated encephalomyelitis with extensive destruction of myelin: II. Pathology. J Exp Med 90:195–212. 10.1084/jem.90.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bakkers MJG, Lang Y, Feitsma LJ, Hulswit RJG, de Poot SAH, van Vliet ALW, Margine I, de Groot-Mijnes JDF, van Kuppeveld FJM, Langereis MA, Huizinga EG, de Groot RJ. 2017. Betacoronavirus adaptation to humans involved progressive loss of hemagglutinin-esterase lectin activity. Cell Host Microbe 21:356–366. 10.1016/j.chom.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Banerjee A, Kulcsar K, Misra V, Frieman M, Mossman K. 2019. Bats and coronaviruses. Viruses 11:41. 10.3390/v11010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Banner LR, Lai MM. 1991. Random nature of coronavirus RNA recombination in the absence of selection pressure. Virology 185:441–445. 10.1016/0042-6822(91)90795-D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baranov PV, Henderson CM, Anderson CB, Gesteland RF, Atkins JF, Howard MT. 2005. Programmed ribosomal frameshifting in decoding the SARS-CoV genome. Virology 332:498–510. 10.1016/j.virol.2004.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bárcena M, Oostergetel GT, Bartelink W, Faas FGA, Verkleij A, Rottier PJM, Koster AJ, Bosch BJ. 2009. Cryo-electron tomography of mouse hepatitis virus: Insights into the structure of the coronavirion. Proc Natl Acad Sci USA 106:582–587. 10.1073/pnas.0805270106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baric RS, Sullivan E, Hensley L, Yount B, Chen W. 1999. Persistent infection promotes cross-species transmissibility of mouse hepatitis virus. J Virol 73:638–649. 10.1128/JVI.73.1.638-649.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barker MG, Percy DH, Hovland DJ, MacInnes JI. 1994. Preliminary characterization of the structural proteins of the coronaviruses, sialodacryoadenitis virus and Parker’s rat coronavirus. Can J Vet Res 58:99–103. [PMC free article] [PubMed] [Google Scholar]
- 25.Barthold SW. 1987. Host age and genotypic effects on enterotropic mouse hepatitis virus infection. Lab Anim Sci 37:36–40. [PubMed] [Google Scholar]
- 26.Barthold SW, Beck DS, Smith AL. 1988. Mouse hepatitis virus and host determinants of vertical transmission and maternally-derived passive immunity in mice. Arch Virol 100:171–183. 10.1007/BF01487681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barthold SW, Beck DS, Smith AL. 1993. Enterotropic coronavirus (mouse hepatitis virus) in mice: Influence of host age and strain on infection and disease. Lab Anim Sci 43:276–284. [PubMed] [Google Scholar]
- 28.Barthold SW, Griffey SM, Percy DH. 2016. Pathology of laboratory rodents and rabbits, 4th ed. Ames(IA): Wiley Blackwell. 10.1002/9781118924051 [DOI] [Google Scholar]
- 29.Barthold SW, Smith AL. Mouse Hepatitis Virus, p 141–178. In: Fox JG, Barthold SW, Davisson MT, Newcomer CE, Quimby FW, Smith AL, editors. The Mouse in Biomedical Research, vol 2. Burlington(MA): Academic Press-Elsevier. [Google Scholar]
- 30.Barthold SW, Smith AL.1983. Mouse hepatitis virus S in weanling Swiss mice following intranasal inoculation. Lab Anim Sci 33:355–360. [PubMed] [Google Scholar]
- 31.Barthold SW, Smith AL. 1984. Mouse hepatitis virus strain–related patterns of tissue tropism in suckling mice. Arch Virol 81:103–112. 10.1007/BF01309300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barthold SW, Smith AL. 1987. Response of genetically susceptible and resistant mice to intranasal inoculation with mouse hepatitis virus JHM. Virus Res 7:225–239. 10.1016/0168-1702(87)90030-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barthold SW, Smith AL. 1989. Duration of challenge immunity to coronavirus JHM in mice. Arch Virol 107:171–177. 10.1007/BF01317914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barthold SW, Smith AL. 1989. Virus strain specificity of challenge immunity to coronavirus. Arch Virol 104:187–196. 10.1007/BF01315542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barthold SW, Smith AL. 1990. Duration of mouse hepatitis virus infection: studies in immunocompetent and chemically immunosuppressed mice. Lab Anim Sci 40:133–137. [PubMed] [Google Scholar]
- 36.Barthold SW, Smith AL. 1992. Viremic dissemination of mouse hepatitis virus-JHM following intranasal inoculation of mice. Arch Virol 122:35–44. 10.1007/BF01321116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barthold SW, Smith AL, Povar ML. 1985. Enterotropic mouse hepatitis virus infection in nude mice. Lab Anim Sci 35:613–618. [PubMed] [Google Scholar]
- 38.Bass EP, Sharpee RL.1975. Coronavirus and gastroenteritis in foals. Lancet 306:822. 10.1016/S0140-6736(75)80058-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bay WW, Doyle LP, Hutchinigs LM. 1953. Transmissible gastroenteritis of swine; a study of immunity. J Am Vet Med Assoc 122:200–202. [PubMed] [Google Scholar]
- 40.Belouzard S, Millet JK, Licitra BN, Whittaker GR. 2012. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses 4:1011–1033. 10.3390/v4061011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Belsham GJ, Rasmussen TB, Normann P, Vaclavek P, Strandbygaard B, Bøtner A. 2016. Characterization of a novel chimeric swine enteric coronavirus from diseased pigs in central Eastern Europe in 2016. TransboundEmerg Dis 63:595–601. 10.1111/tbed.12579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Benbacer L, Kut E, Besnardeau L, Laude H, Delmas B. 1997. Interspecies aminopeptidase-N chimeras reveal species-specific receptor recognition by canine coronavirus, feline infectious peritonitis virus, and transmissible gastroenteritis virus. J Virol 71:734–737. 10.1128/jvi.71.1.734-737.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bender SJ, Phillips JM, Scott EP, Weiss SR. 2010. Murine coronavirus receptors are differentially expressed in the central nervous system and play virus strain-dependent roles in neuronal spread. J Virol 84:11030–11044. 10.1128/JVI.02688-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bender SJ, Weiss SR. 2010. Pathogenesis of murine coronavirus in the central nervous system. J Neuroimmune Pharmacol 5:336–354. 10.1007/s11481-010-9202-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bernard S, Bottreau E, Aynaud JM, Have P, Szymansky J. 1989. Natural infection with the porcine respiratory coronavirus induces protective lactogenic immunity against transmissible gastroenteritis. Vet Microbiol 21:1–8. 10.1016/0378-1135(89)90013-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berryhill EH, Magdesian KG, Aleman M, Pusterla N. 2019. Clinical presentation, diagnostic findings, and outcome of adult horses with equine coronavirus infection at a veterinary teaching hospital: 33 cases (2012-2018). Vet J 248:95–100. 10.1016/j.tvjl.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bevins SN, Lutman M, Pedersen K, Barrett N, Gidlewski T, Deliberto TJ, Franklin AB. 2018. Spillover of swine coronaviruses. Emerg Infect Dis 24:1390–1392. 10.3201/eid2407.172077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhatt PN, Jacoby RO. 1977. Experimental infection of adult axenic rats with Parker’s rat coronavirus. Arch Virol 54:345–352. 10.1007/BF01314779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bhatt PN, Jacoby RO. 1985. Epizootiological observations of natural and experimental infection with sialodacryoadenitis virus in rats. Lab Anim Sci 35:129–134. [PubMed] [Google Scholar]
- 50.Bhatt PN, Jacoby RO, Jonas AM. 1977. Respiratory infection in mice with sialodacryoadenitis virus, a coronavirus of rats. Infect Immun 18:823–827. 10.1128/iai.18.3.823-827.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bhatt PN, Percy DH, Jonas AM. 1972. Characterization of the virus of sialodacryoadenitis of rats: A member of the coronavirus group. J Infect Dis 126:123–130. 10.1093/infdis/126.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bihun CG, Percy DH. 1994. Coronavirus infections in the laboratory rat: Degree of cross protection following immunization with a heterologous strain. Can J Vet Res 58:224–229. [PMC free article] [PubMed] [Google Scholar]
- 53.Binn LN, Lazar EC, Keenan KP, Huxsoll DL, Marchwicki RH, Strano AJ. 1974. Recovery and characterization of a coronavirus from military dogs with diarrhea. Proc Annu Meet U S Anim Health Assoc 78:359–366. [PubMed] [Google Scholar]
- 54.Boileau MJ, Kapil S. 2010. Bovine coronavirus associated syndromes. Vet Clin North Am Food Anim Pract 26:123–146. 10.1016/j.cvfa.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Boniotti MB, Papetti A, Lavazza A, Alborali G, Sozzi E, Chiapponi C, Faccini S, Bonilauri P, Cordioli P, Marthaler D. 2016. Porcine epidemic diarrhea virus and discovery of a recombinant swine enteric coronavirus, Italy. Emerg Infect Dis 22:83–87. 10.3201/eid2201.150544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bosch BJ, van der Zee R, de Haan CA, Rottier PJ. 2003. The coronavirus spike protein is a class I virus fusion protein: Structural and functional characterization of the fusion core complex. J Virol 77:8801–8811. 10.1128/JVI.77.16.8801-8811.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bouwman KM, Delpont M, Broszeit F, Berger R, Weerts E, Lucas MN, Delverdier M, Belkasmi S, Papanikolaou A, Boons GJ, Guérin JL, de Vries RP, Ducatez MF, Verheije MH. 2019. Guinea fowl coronavirus diversity has phenotypic consequences for glycan and tissue binding. J Virol 93:e00067-19. 10.1128/JVI.00067-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brim TA, VanCott JL, Lunney JK, Saif LJ. 1995. Cellular immune responses of pigs after primary inoculation with porcine respiratory coronavirus or transmissible gastroenteritis virus and challenge with transmissible gastroenteritis virus. Vet Immunol Immunopathol 48:35–54. 10.1016/0165-2427(94)05416-P. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brown MA, Troyer JL, Pecon-Slattery J, Roelke ME, O’Brien SJ. 2009. Genetics and pathogenesis of feline infectious peritonitis virus. Emerg Infect Dis 15:1445–1452. 10.3201/eid1509.081573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brown PA, Courtillon C, Weerts EAWS, Andraud M, Allée C, Vendembeuche A, Amelot M, Rose N, Verheije MH, Eterradossi N. 2019. Transmission Kinetics and histopathology induced by European Turkey Coronavirus during experimental infection of specific pathogen free turkeys. TransboundEmerg Dis 66:234–242. 10.1111/tbed.13006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Buonavoglia C, Decaro N, Martella V, Elia G, Campolo M, Desario C, Castagnaro M, Tempesta M. 2006. Canine coronavirus highly pathogenic for dogs. Emerg Infect Dis 12:492–494. 10.3201/eid1203.050839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cabirac GF, Soike KF, Butunoi C, Hoel K, Johnson S, Cai GY, Murray RS. 1994. Coronavirus JHM OMP1 pathogenesis in owl monkey CNS and coronavirus infection of owl monkey CNS via peripheral routes. Adv Exp Med Biol 342:347–352. 10.1007/978-1-4615-2996-5_53. [DOI] [PubMed] [Google Scholar]
- 63.Callebaut P, Pensaert MB, Hooyberghs J. 1989. A competitive inhibition ELISA for the differentiation of serum antibodies from pigs infected with transmissible gastroenteritis virus (TGEV) or with the TGEV-related porcine respiratory coronavirus. Vet Microbiol 20:9–19. 10.1016/0378-1135(89)90003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, Zerbi P, Rech R, Colombo R, Antinori S, Corbellino M, Galli M, Catena E, Tosoni A, Gianatti A, Nebuloni M. 2020. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study. Lancet Infect Dis 20:1135–1140. 10.1016/S1473-3099(20)30434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carstens EB. 2010. Ratification vote on taxonomic proposals to the International Committee on Taxonomy of Viruses (2009). Arch Virol 155:133–146. 10.1007/s00705-009-0547-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carthew P. 1977. Lethal intestinal virus of infant mice is mouse hepatitis virus. Vet Rec 101:465. [PubMed] [Google Scholar]
- 67.Cartwright SF, Lucas M, Cavill JP, Gush AF, Blandford TB. 1969. Vomiting and wasting disease of piglets. Vet Rec 84:175–176. 10.1136/vr.84.7.175. [DOI] [PubMed] [Google Scholar]
- 68.Castaño-Rodriguez C, Honrubia JM, Gutiérrez-Álvarez J, DeDiego ML, Nieto-Torres JL, Jimenez-Guardeño JM, Regla-Nava JA, Fernandez-Delgado R, Verdia-Báguena C, Queralt-Martín M, Kochan G, Perlman S, Aguilella VM, Sola I, Enjuanes L, Denison MR, Kupperveld F, Machamer C, Thiel V. 2018. Role of Severe Acute Respiratory Syndrome Coronavirus Viroporins E, 3a, and 8a in replication and pathogenesis. MBio 9:e02325-17. 10.1128/mBio.02325-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Caul EO, Egglestone SI. 1979. Coronavirus-like particles present in simian faeces. Vet Rec 104:168–169. 10.1136/vr.104.8.168. [DOI] [PubMed] [Google Scholar]
- 70.Cavanagh D. 2003. Severe acute respiratory syndrome vaccine development: experiences of vaccination against avian infectious bronchitis coronavirus. Avian Pathol 32:567–582. 10.1080/03079450310001621198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cavanagh D. 2005. Coronaviruses in poultry and other birds. Avian Pathol 34:439–448. 10.1080/03079450500367682. [DOI] [PubMed] [Google Scholar]
- 72.Cavanagh D. 2007. Coronavirus avian infectious bronchitis virus. Vet Res 38:281–297. 10.1051/vetres:2006055. [DOI] [PubMed] [Google Scholar]
- 73.Cave TA, Golder MC, Simpson J, Addie DD. 2004. Risk factors for feline coronavirus seropositivity in cats relinquished to a UK rescue charity. J Feline Med Surg 6:53–58. 10.1016/j.jfms.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cebra CK, Mattson DE, Baker RJ, Sonn RJ, Dearing PL. 2003. Potential pathogens in feces from unweaned llamas and alpacas with diarrhea. J Am Vet Med Assoc 223:1806–1808. 10.2460/javma.2003.223.1806. [DOI] [PubMed] [Google Scholar]
- 75.Centers for Disease Control and Prevention. [Internet]. 2005. In the absence of SARS-CoV transmission worldwide: Guidance for surveillance, clinical and laboratory evaluation, and reporting. [Cited 28 March 2022]. Available at: https://www.cdc.gov/sars/surveillance/absence.html.
- 76.Centers for Disease Control and Prevention.[Internet]. 2021. Symptoms of COVID-19. [Cited 07 October 2021]. Available at: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
- 77.Chae C, Kim O, Choi C, Min K, Cho WS, Kim J, Tai JH. 2000. Prevalence of porcine epidemic diarrhoea virus and transmissible gastroenteritis virus infection in Korean pigs. Vet Rec 147:606–608. 10.1136/vr.147.21.606. [DOI] [PubMed] [Google Scholar]
- 78.Chamings A, Nelson TM, Vibin J, Wille M, Klaassen M, Alexandersen S. 2018. Detection and characterisation of coronaviruses in migratory and non-migratory Australian wild birds. Sci Rep 8:5980. 10.1038/s41598-018-24407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chamorro MF, Palomares RA. 2020. Bovine respiratory disease vaccination against viral pathogens: Modified-live versus inactivated antigen vaccines, intranasal versus parenteral, what is the evidence? Vet Clin North Am Food Anim Pract 36:461–472. 10.1016/j.cvfa.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chang CK, Sue SC, Yu TH, Hsieh CM, Tsai CK, Chiang YC, Lee SJ, Hsiao HH, Wu WJ, Chang WL, Lin CH, Huang TH. 2006. Modular organization of SARS coronavirus nucleocapsid protein. J Biomed Sci 13:59–72. 10.1007/s11373-005-9035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chasey D, Cartwright SF. 1978. Virus-like particles associated with porcine epidemic diarrhoea. Res Vet Sci 25:255–256. 10.1016/S0034-5288(18)32994-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cheever FS, Daniels JB, Pappenheimer AW, Bailey OT. 1949. A murine virus (JHM) causing disseminated encephalomyelitis with extensive destruction of myelin. J Exp Med 90:181–194. 10.1084/jem.90.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chen Y, Su C, Ke M, Jin X, Xu L, Zhang Z, Wu A, Sun Y, Yang Z, Tien P, Ahola T, Liang Y, Liu X, Guo D. 2011. Biochemical and structural insights into the mechanisms of SARS coronavirus RNA ribose 2′-O-methylation by nsp16/nsp10 protein complex. PLoS Pathog 7:e1002294. 10.1371/journal.ppat.1002294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cheung CY, Poon LL, Ng IH, Luk W, Sia SF, Wu MH, Chan KH, Yuen KY, Gordon S, Guan Y, Peiris JS. 2005. Cytokine responses in severe acute respiratory syndrome coronavirus-infected macrophages in vitro: Possible relevance to pathogenesis. J Virol 79:7819–7826. 10.1128/JVI.79.12.7819-7826.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chibo D, Birch C. 2006. Analysis of human coronavirus 229E spike and nucleoprotein genes demonstrates genetic drift between chronologically distinct strains. J Gen Virol 87:1203–1208. 10.1099/vir.0.81662-0. [DOI] [PubMed] [Google Scholar]
- 86.Chien JY, Hsueh PR, Cheng WC, Yu CJ, Yang PC. 2006. Temporal changes in cytokine/chemokine profiles and pulmonary involvement in severe acute respiratory syndrome. Respirology 11:715–722. 10.1111/j.1440-1843.2006.00942.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cho KO, Hasoksuz M, Nielsen PR, Chang KO, Lathrop S, Saif LJ. 2001. Cross-protection studies between respiratory and calf diarrhea and winter dysentery coronavirus strains in calves and RT-PCR and nested PCR for their detection. Arch Virol 146:2401–2419. 10.1007/s007050170011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Christensen N, Fennestad KL, Bruun L. 1978. Pleural effusion disease in rabbits. Histopathological observations. Acta Pathol Microbiol Scand A 86:251–256. [DOI] [PubMed] [Google Scholar]
- 89.Chu DKW, Leung CYH, Gilbert M, Joyner PH, Ng EM, Tse TM, Guan Y, Peiris JSM, Poon LLM. 2011. Avian coronavirus in wild aquatic birds. J Virol 85:12815–12820. 10.1128/JVI.05838-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chu Y-K, Ali GD, Jia F, Li Q, Kelvin D, Couch RC, Harrod KS, Hutt JA, Cameron C, Weiss SR, Jonsson CB. 2008. The SARS-CoV ferret model in an infection–challenge study. Virology 374:151–163. 10.1016/j.virol.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cohn LA, Langdon P. 2008. CHAPTER 112 - Viral Infections, p 1087–1103. In: Morgan RV, editor. Handbook of Small Animal Practice (Fifth Edition). Saint Louis (MO): W.B. Saunders. [Google Scholar]
- 92.Colina SE, Serena MS, Echeverría MG, Metz GE. 2021. Clinical and molecular aspects of veterinary coronaviruses. Virus Res 297:198382. 10.1016/j.virusres.2021.198382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Compton SR, Ball-Goodrich LJ, Johnson LK, Johnson EA, Paturzo FX, Macy JD. 2004. Pathogenesis of enterotropic mouse hepatitis virus in immunocompetent and immunodeficient mice. Comp Med 54:681–689. [PubMed] [Google Scholar]
- 94.Compton SR, Smith AL, Gaertner DJ. 1999. Comparison of the pathogenicity in rats of rat coronaviruses of different neutralization groups. Lab Anim Sci 49:514–518. [PubMed] [Google Scholar]
- 95.Compton SR, Vivas-Gonzalez BE, Macy JD. 1999. Reverse transcriptase polymerase chain reaction-based diagnosis and molecular characterization of a new rat coronavirus strain. Lab Anim Sci 49:506–513. [PubMed] [Google Scholar]
- 96.Cook-Mills JM, Munshi HG, Perlman RL, Chambers DA. 1992. Mouse hepatitis virus infection suppresses modulation of mouse spleen T-cell activation. Immunology 75:542–545. [PMC free article] [PubMed] [Google Scholar]
- 97.Cool K, Gaudreault NN, Morozov I, Trujillo JD, Meekins DA, McDowell C, Carossino M, Bold D, Mitzel D, Kwon T, Balaraman V, Madden DW, Artiaga BL, Pogranichniy RM, Sosa GR, Henningson J, Wilson WC, Balasuriya UBR, García-Sastre A, Richt JA. 2022. Infection and transmission of ancestral SARS-CoV-2 and its alpha variant in pregnant white-tailed deer. Emerg Microbes Infect 11:95–112. 10.1101/2021.08.15.456341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Corman VM, Baldwin HJ, Tateno AF, Zerbinati RM, Annan A, Owusu M, Nkrumah EE, Maganga GD, Oppong S, Adu-Sarkodie Y, Vallo P, da Silva Filho LV, Leroy EM, Thiel V, van der Hoek L, Poon LL, Tschapka M, Drosten C, Drexler JF. 2015. Evidence for an ancestral association of human coronavirus 229E with bats. J Virol 89:11858–11870. 10.1128/JVI.01755-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Corman VM, Muth D, Niemeyer D, Drosten C. 2018. Hosts and sources of endemic human coronaviruses. Adv Virus Res 100:163–188. 10.1016/bs.aivir.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cornelissen LA, Wierda CM, van der Meer FJ, Herrewegh AA, Horzinek MC, Egberink HF, de Groot RJ. 1997. Hemagglutinin-esterase, a novel structural protein of torovirus. J Virol 71:5277–5286. 10.1128/jvi.71.7.5277-5286.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Courtillon C, Briand FX, Allée C, Contrant M, Beven V, Lucas P, Blanchard Y, Mouchel S, Eterradossi N, Delforterie Y, Grasland B, Brown P. 2021. Description of the first isolates of guinea fowl corona and picornaviruses obtained from a case of guinea fowl fulminating enteritis. Avian Pathol 50:507–521. 10.1080/03079457.2021.1976725. [DOI] [PubMed] [Google Scholar]
- 102.Cox E, Hooyberghs J, Pensaert MB. 1990. Sites of replication of a porcine respiratory coronavirus related to transmissible gastroenteritis virus. Res Vet Sci 48:165–169. 10.1016/S0034-5288(18)30984-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Crawford K, Lager K, Miller L, Opriessnig T, Gerber P, Hesse R. 2015. Evaluation of porcine epidemic diarrhea virus transmission and the immune response in growing pigs. Vet Res 46:49. 10.1186/s13567-015-0180-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cray C, Mateo MO, Altman NH. 1993. In vitro and long-term in vivo immune dysfunction after infection of BALB/c mice with mouse hepatitis virus strain A59. Lab Anim Sci 43:169–174. [PubMed] [Google Scholar]
- 105.Crossley BM, Barr BC, Magdesian KG, Ing M, Mora D, Jensen D, Loretti AP, McConnell T, Mock R. 2010. Identification of a novel coronavirus possibly associated with acute respiratory syndrome in alpacas (Vicugna pacos) in California, 2007. J Vet Diagn Invest 22:94–97. 10.1177/104063871002200118. [DOI] [PubMed] [Google Scholar]
- 106.Crossley BM, Mock RE, Callison SA, Hietala SK. 2012. Identification and characterization of a novel alpaca respiratory coronavirus most closely related to the human coronavirus 229E. Viruses 4:3689–3700. 10.3390/v4123689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cui J, Li F, Shi Z-L. 2019. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol 17:181–192. 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cutlip RC, Mengeling WL. 1972. Lesions induced by hemagglutinating encephalomyelitis virus strain 67N in pigs. Am J Vet Res 33:2003–2009. [PubMed] [Google Scholar]
- 109.Damas J, Hughes GM, Keough KC, Painter CA, Persky NS, Corbo M, Hiller M, Koepfli KP, Pfenning AR, Zhao H, Genereux DP, Swofford R, Pollard KS, Ryder OA, Nweeia MT, Lindblad-Toh K, Teeling EC, Karlsson EK, Lewin HA. 2020. Broad host range of SARS-CoV-2 predicted by comparative and structural analysis of ACE2 in vertebrates. Proc Natl Acad Sci USA 117:22311–22322. 10.1073/pnas.2010146117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Davis E, Rush BR, Cox J, DeBey B, Kapil S. 2000. Neonatal enterocolitis associated with coronavirus infection in a foal: a case report. J Vet Diagn Invest 12:153–156. 10.1177/104063870001200210. [DOI] [PubMed] [Google Scholar]
- 111.De Albuquerque N, Baig E, Ma X, Zhang J, He W, Rowe A, Habal M, Liu M, Shalev I, Downey GP, Gorczynski R, Butany J, Leibowitz J, Weiss SR, McGilvray ID, Phillips MJ, Fish EN, Levy GA. 2006. Murine hepatitis virus strain 1 produces a clinically relevant model of severe acute respiratory syndrome in A/J mice. J Virol 80:10382–10394. 10.1128/JVI.00747-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.De Diego M, Laviada MD, Enjuanes L, Escribano JM. 1992. Epitope specificity of protective lactogenic immunity against swine transmissible gastroenteritis virus. J Virol 66:6502–6508. 10.1128/jvi.66.11.6502-6508.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.de Groot RJ, Luytjes W, Horzinek MC, van der Zeijst BA, Spaan WJ, Lenstra JA. 1987. Evidence for a coiled-coil structure in the spike proteins of coronaviruses. J Mol Biol 196:963–966. 10.1016/0022-2836(87)90422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.de Haan CA, de Wit M, Kuo L, Montalto-Morrison C, Haagmans BL, Weiss SR, Masters PS, Rottier PJ. 2003. The glycosylation status of the murine hepatitis coronavirus M protein affects the interferogenic capacity of the virus in vitro and its ability to replicate in the liver but not the brain. Virology 312:395–406. 10.1016/S0042-6822(03)00235-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Decaro N, Buonavoglia C. 2008. An update on canine coronaviruses: Viral evolution and pathobiology. Vet Microbiol 132:221–234. 10.1016/j.vetmic.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Decaro N, Buonavoglia C. 2011. Canine coronavirus: Not only an enteric pathogen. Vet Clin North Am Small Anim Pract 41:1121–1132. 10.1016/j.cvsm.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Decaro N, Campolo M, Desario C, Cirone F, D’Abramo M, Lorusso E, Greco G, Mari V, Colaianni ML, Elia G, Martella V, Buonavoglia C. 2008. Respiratory disease associated with bovine coronavirus infection in cattle herds in Southern Italy. J Vet Diagn Invest 20:28–32. 10.1177/104063870802000105. [DOI] [PubMed] [Google Scholar]
- 118.Decaro N, Campolo M, Mari V, Desario C, Colaianni ML, Di Trani L, Cordioli P, Buonavoglia C. 2009. A candidate modified-live bovine coronavirus vaccine: safety and immunogenicity evaluation. New Microbiol 32:109–113. [PubMed] [Google Scholar]
- 119.Decaro N, Cordonnier N, Demeter Z, Egberink H, Elia G, Grellet A, Le Poder S, Mari V, Martella V, Ntafis V, von Reitzenstein M, Rottier PJ, Rusvai M, Shields S, Xylouri E, Xu Z, Buonavoglia C. 2013. European surveillance for pantropic canine coronavirus. J Clin Microbiol 51:83–88. 10.1128/JCM.02466-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Decaro N, Lorusso A. 2020. Novel human coronavirus (SARS-CoV-2): A lesson from animal coronaviruses. Vet Microbiol 244:108693. 10.1016/j.vetmic.2020.108693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Decaro N, Mari V, Campolo M, Lorusso A, Camero M, Elia G, Martella V, Cordioli P, Enjuanes L, Buonavoglia C. 2009. Recombinant canine coronaviruses related to transmissible gastroenteritis virus of swine are circulating in dogs. J Virol 83:1532–1537. 10.1128/JVI.01937-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Decaro N, Mari V, Elia G, Addie DD, Camero M, Lucente MS, Martella V, Buonavoglia C. 2010. Recombinant canine coronaviruses in dogs, Europe. Emerg Infect Dis 16:41–47. 10.3201/eid1601.090726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.DeDiego ML, Alvarez E, Almazán F, Rejas MT, Lamirande E, Roberts A, Shieh WJ, Zaki SR, Subbarao K, Enjuanes L. 2007. A severe acute respiratory syndrome coronavirus that lacks the E gene is attenuated in vitro and in vivo. J Virol 81:1701–1713. 10.1128/JVI.01467-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Deeb BJ, DiGiacomo RF, Evermann JF, Thouless ME. 1993. Prevalence of coronavirus antibodies in rabbits. Lab Anim Sci 43:431–433. [PubMed] [Google Scholar]
- 125.Delmas B, Gelfi J, L’Haridon R, Vogel LK, Sjöström H, Norén O, Laude H. 1992. Aminopeptidase N is a major receptor for the entero-pathogenic coronavirus TGEV. Nature 357:417–420. 10.1038/357417a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Deng F, Ye G, Liu Q, Navid MT, Zhong X, Li Y, Wan C, Xiao S, He Q, Fu ZF, Peng G. 2016. Identification and comparison of receptor binding characteristics of the spike protein of two porcine epidemic diarrhea virus strains. Viruses 8:55. 10.3390/v8030055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Descôteaux JP, Lussier G. 1990. Experimental infection of young rabbits with a rabbit enteric coronavirus. Can J Vet Res 54:473–476. [PMC free article] [PubMed] [Google Scholar]
- 128.Descôteaux JP, Lussier G, Berthiaume L, Alain R, Seguin C, Trudel M. 1985. An enteric coronavirus of the rabbit: Detection by immunoelectron microscopy and identification of structural polypeptides. Arch Virol 84:241–250. 10.1007/BF01378976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Diel DG, Lawson S, Okda F, Singrey A, Clement T, Fernandes MHV, Christopher-Hennings J, Nelson EA. 2016. Porcine epidemic diarrhea virus: An overview of current virological and serological diagnostic methods. Virus Res 226:60–70. 10.1016/j.virusres.2016.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Domanska-Blicharz K, Sajewicz-Krukowska J. 2021. Recombinant turkey coronavirus: are some S gene structures of gammacoronaviruses especially prone to exchange? Poult Sci 100:101018. 10.1016/j.psj.2021.101018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dong BQ, Liu W, Fan XH, Dhanasekaran V, Tang XC, Gao F, Li LF, Li GJ, Zhang JX, Yang LQ, Poon LLM, Zhang SY, Peiris JSM, Smith GJD, Chen H, Guan Y. 2007. Detection of a Novel and Highly Divergent Coronavirus from Asian Leopard Cats and Chinese Ferret Badgers in Southern China. J Virol 81:6920–6926. 10.1128/JVI.00299-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Doyle LP, Hutchings LM. 1946. A transmissible gastroenteritis in pigs. J Am Vet Med Assoc 108:257–259. [PubMed] [Google Scholar]
- 133.Ducatez MF, Guérin JL. 2015. Identification of a novel coronavirus from guinea fowl using metagenomics. Methods Mol Biol 1282:27–31. 10.1007/978-1-4939-2438-7_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Durães-Carvalho R, Caserta LC, Barnabé AC, Martini MC, Ferreira HL, Felippe PA, Santos MB, Arns CW. 2015. Coronaviruses detected in brazilian wild birds reveal close evolutionary relationships with beta- and deltacoronaviruses isolated from mammals. J Mol Evol 81:21–23. 10.1007/s00239-015-9693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Eaton P. 1984. Preliminary observations on enteritis associated with a coronavirus-like agent in rabbits. Lab Anim 18:71–74. 10.1258/002367784780864938. [DOI] [PubMed] [Google Scholar]
- 136.Edwards CE, Yount BL, Graham RL, Leist SR, Hou YJ, Dinnon KH, 3rd, Sims AC, Swanstrom J, Gully K, Scobey TD, Cooley MR, Currie CG, Randell SH, Baric RS. 2020. Swine acute diarrhea syndrome coronavirus replication in primary human cells reveals potential susceptibility to infection. Proc Natl Acad Sci USA 117:26915–26925. 10.1073/pnas.2001046117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.El-Kanawati ZR, Tsunemitsu H, Smith DR, Saif LJ. 1996. Infection and cross-protection studies of winter dysentery and calf diarrhea bovine coronavirus strains in colostrum-deprived and gnotobiotic calves. Am J Vet Res 57:48–53. [PubMed] [Google Scholar]
- 138.Enjuanes L, Suñé C, Gebauer F, Smerdou C, Camacho A, Antón IM, González S, Talamillo A, Méndez A, Ballesteros ML, Sánchez C.1992. Antigen selection and presentation to protect against transmissible gastroenteritis coronavirus.Vet Microbiol 33:249–262. 10.1016/0378-1135(92)90053-V. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Erles K, Brownlie J. 2008. Canine respiratory coronavirus: An emerging pathogen in the canine infectious respiratory disease complex. Vet Clin North Am Small Anim Pract 38:815–825. 10.1016/j.cvsm.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Erles K, Shiu KB, Brownlie J. 2007. Isolation and sequence analysis of canine respiratory coronavirus. Virus Res 124:78–87. 10.1016/j.virusres.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.European Centre for Disease Prevention and Control. [Internet]. 2021. Geographical distribution of confirmed MERS-CoV cases by country of infection and year. [Cited 28 March 2022]. Available at: https://www.ecdc.europa.eu/en/publications-data/geographical-distribution-confirmed-mers-cov-cases-country-infection-and-year.
- 142.Evermann JF, Heeney JL, McKeirnan AJ, O’Brien SJ. 1989. Comparative features of a coronavirus isolated from a cheetah with feline infectious peritonitis. Virus Res 13:15–27. 10.1016/0168-1702(89)90084-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fahkrajang W, Sudaryatma PE, Mekata H, Hamabe S, Saito A, Okabayashi T. 2021. Bovine respiratory coronavirus enhances bacterial adherence by upregulating expression of cellular receptors on bovine respiratory epithelial cells. Vet Microbiol 255:109017. 10.1016/j.vetmic.2021.109017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fang P, Fang L, Zhang H, Xia S, Xiao S. 2021. Functions of coronavirus accessory proteins: Overview of the state of the art. Viruses 13:1139. 10.3390/v13061139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Fehr AR, Channappanavar R, Perlman S. 2017. Middle East Respiratory Syndrome: Emergence of a pathogenic human coronavirus. Annu Rev Med 68:387–399. 10.1146/annurev-med-051215-031152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Fehr AR, Perlman S. 2015. Coronaviruses: An overview of their replication and pathogenesis, p 1–23. In: Maier HJ, Bickerton E, Britton P, editors. Coronaviruses: Methods and Protocols. New York (NY): Springer New York. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Felten S, Klein-Richers U, Hofmann-Lehmann R, Bergmann M, Unterer S, Leutenegger CM, Hartmann K. 2020. Correlation of feline coronavirus shedding in feces with coronavirus antibody titer. Pathogens 9:598. 10.3390/pathogens9080598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Fennestad KL, Bruun L, Wedø E. 1980. Pleural effusion disease agent as passenger of Treponema pallidum suspensions from rabbits. Survey of laboratories. Br J Vener Dis 56:198–203. 10.1136/sti.56.4.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Fennestad KL, Mansa B, Christensen N, Larsen S, Svehag SE. 1986. Pathogenicity and persistence of pleural effusion disease virus isolates in rabbits. J Gen Virol 67:993–1000. 10.1099/0022-1317-67-6-993. [DOI] [PubMed] [Google Scholar]
- 150.Fennestad KL, Skovgaard Jensen HJ, Moller S, Weis Bentzon M. 1975. Pleural effusion disease in rabbits, Clinical and post mortem observations. Acta Pathol Microbiol Scand Suppl 83:541–548. [PubMed] [Google Scholar]
- 151.Fielding CL, Higgins JK, Higgins JC, McIntosh S, Scott E, Giannitti F, Mete A, Pusterla N. 2015. Disease associated with equine coronavirus infection and high case fatality rate. J Vet Intern Med 29:307–310. 10.1111/jvim.12480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fledelius H, Bruun L, Fennestad KL, Andersen SR. 1978. Uveitis in rabbits with pleural effusion disease. Clinical and histopathological observations. Acta Ophthalmol (Copenh) 56:599–606. 10.1111/j.1755-3768.1978.tb01372.x. [DOI] [PubMed] [Google Scholar]
- 153.Ford RB, Larson LJ, McClure KD, Schultz RD, Welborn LV. 2017. 2017 AAHA canine vaccination guidelines. J Am Anim Hosp Assoc 53:243–251. 10.5326/JAAHA-MS-6741. [DOI] [PubMed] [Google Scholar]
- 154.Foreyt WJ, Evermann JF. 1985. Serologic survey of canine coronavirus in wild coyotes in the western United States, 1972-1982. J Wildl Dis 21:428–430. 10.7589/0090-3558-21.4.428. [DOI] [PubMed] [Google Scholar]
- 155.Forni D, Cagliani R, Clerici M, Sironi M. 2017. Molecular evolution of human coronavirus genomes. Trends Microbiol 25:35–48. 10.1016/j.tim.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.France MP, Smith AL, Stevenson R, Barthold SW. 1999. Granulomatous peritonitis and pleuritis in interferon-gamma gene knockout mice naturally infected with mouse hepatitis virus. Aust Vet J 77:600–604. 10.1111/j.1751-0813.1999.tb13199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Furuuchi S, Shimizu Y. 1976. Effect of ambient temperatures on multiplication of attenuated transmissible gastroenteritis virus in the bodies of newborn piglets. Infect Immun 13:990–992. 10.1128/iai.13.3.990-992.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gaertner DJ, Compton SR, Winograd DF. 1993. Environmental stability of rat coronaviruses (RCVs). Lab Anim Sci 43:403–404. [PubMed] [Google Scholar]
- 159.Gagneten S, Scanga CA, Dveksler GS, Beauchemin N, Percy D, Holmes KV. 1996. Attachment glycoproteins and receptor specificity of rat coronaviruses. Lab Anim Sci 46:159–166. [PubMed] [Google Scholar]
- 160.Gard AL, Luu RJ, Miller CR, Maloney R, Cain BP, Marr EE, Burns DM, Gaibler R, Mulhern TJ, Wong CA, Alladina J, Coppeta JR, Liu P, Wang JP, Azizgolshani H, Fezzie RF, Balestrini JL, Isenberg BC, Medoff BD, Finberg RW, Borenstein JT. 2021. High-throughput human primary cell-based airway model for evaluating influenza, coronavirus, or other respiratory viruses in vitro. Sci Rep 11:14961. 10.1038/s41598-021-94095-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Garner MM, Ramsell K, Morera N, Juan-Sallés C, Jiménez J, Ardiaca M, Montesinos A, Teifke JP, Löhr CV, Evermann JF, Baszler TV, Nordhausen RW, Wise AG, Maes RK, Kiupel M. 2008. Clinicopathologic features of a systemic coronavirus-associated disease resembling feline infectious peritonitis in the domestic ferret (Mustela putorius). Vet Pathol 45:236–246. 10.1354/vp.45-2-236. [DOI] [PubMed] [Google Scholar]
- 162.Garwes DJ. 1988. Transmissible gastroenteritis. Vet Rec 122:462–463. 10.1136/vr.122.19.462. [DOI] [PubMed] [Google Scholar]
- 163.Ge XY, Yang WH, Zhou JH, Li B, Zhang W, Shi ZL, Zhang YZ. 2017. Detection of alpha- and betacoronaviruses in rodents from Yunnan, China. Virol J 14:98. 10.1186/s12985-017-0766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Genova SG, Streeter RN, Simpson KM, Kapil S. 2008. Detection of an antigenic group 2 coronavirus in an adult alpaca with enteritis. Clin Vaccine Immunol 15:1629–1632. 10.1128/CVI.00232-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Gerdts V, Zakhartchouk A. 2017. Vaccines for porcine epidemic diarrhea virus and other swine coronaviruses. Vet Microbiol 206:45–51. 10.1016/j.vetmic.2016.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gerna G, Passarani N, Battaglia M, Rondanelli EG. 1985. Human enteric coronaviruses: Antigenic relatedness to human coronavirus OC43 and possible etiologic role in viral gastroenteritis. J Infect Dis 151:796–803. 10.1093/infdis/151.5.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Giannitti F, Diab S, Mete A, Stanton JB, Fielding L, Crossley B, Sverlow K, Fish S, Mapes S, Scott L, Pusterla N. 2015. Necrotizing enteritis and hyperammonemic encephalopathy associated with equine coronavirus infection in equids. Vet Pathol 52:1148–1156. 10.1177/0300985814568683. [DOI] [PubMed] [Google Scholar]
- 168.Gledhill AW, Andrewes CH. 1951. A hepatitis virus of mice. Br J Exp Pathol 32:559–568. [PMC free article] [PubMed] [Google Scholar]
- 169.Godfraind C, Langreth SG, Cardellichio CB, Knobler R, Coutelier JP, Dubois-Dalcq M, Holmes KV. 1995. Tissue and cellular distribution of an adhesion molecule in the carcinoembryonic antigen family that serves as a receptor for mouse hepatitis virus. Lab Invest 73:615–627. [PubMed] [Google Scholar]
- 170.Goodrich EL, Mittel LD, Glaser A, Ness SL, Radcliffe RM, Divers TJ. 2020. Novel findings from a beta coronavirus outbreak on an American Miniature Horse breeding farm in upstate New York. Equine Vet Educ 32:150–154. 10.1111/eve.12938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, Haagmans BL, Lauber C, Leontovich AM, Neuman BW, Penzar D, Perlman S, Poon LLM, Samborskiy DV, Sidorov IA, Sola I, Ziebuhr J. 2020. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 5:536–544. 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Gorham JR, Evermann JF, Ward A, Pearson R, Shen D, Hartsough GR, Leathers C. 1990. Detection of coronavirus-like particles from mink with epizootic catarrhal gastroenteritis. Can J Vet Res 54:383–384. [PMC free article] [PubMed] [Google Scholar]
- 173.Gorman J. The coronavirus kills mink, so they too may get a vaccine, p 7. The New York Times. New York (NY): The New York Times Co. [Google Scholar]
- 174.Graham RL, Baric RS .2010. Recombination, reservoirs, and the modular spike: Mechanisms of coronavirus cross-species transmission. J Virol 84:3134–3146. 10.1128/JVI.01394-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Greig AS, Girard A. 1969. Serological comparison of hemagglutinating encephalomyelitis viruses isolated from different outbreaks. Can J Comp Med 33:25–28. [PMC free article] [PubMed] [Google Scholar]
- 176.Greig AS, Mitchell D, Corner AH, Bannister GL, Meads EB, Julian RJ. 1962. A hemagglutinating virus producing encephalomyelitis in baby pigs. Can J Comp Med Vet Sci 26:49–56. [PMC free article] [PubMed] [Google Scholar]
- 177.Gu J, Gong E, Zhang B, Zheng J, Gao Z, Zhong Y, Zou W, Zhan J, Wang S, Xie Z, Zhuang H, Wu B, Zhong H, Shao H, Fang W, Gao D, Pei F, Li X, He Z, Xu D, Shi X, Anderson VM, Leong ASY. 2005. Multiple organ infection and the pathogenesis of SARS. J Exp Med 202:415–424. 10.1084/jem.20050828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CL, Luo SW, Li PH, Zhang LJ, Guan YJ, Butt KM, Wong KL, Chan KW, Lim W, Shortridge KF, Yuen KY, Peiris JS, Poon LL. 2003. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science 302:276–278. 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 179.Gudjónsson H, Skog E. 1970. Fever after inoculation of rabbits with Treponema pallidum. Br J Vener Dis 46:318–322. 10.1136/sti.46.4.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Guy JS, Breslin JJ, Breuhaus B, Vivrette S, Smith LG. 2000. Characterization of a coronavirus isolated from a diarrheic foal. J Clin Microbiol 38:4523–4526. 10.1128/JCM.38.12.4523-4526.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Habibi M, Karimi V, Langeroudi AG, Ghafouri SA, Hashemzadeh M, Farahani RK, Maghsoudloo H, Abdollahi H, Seifouri P. 2017. Combination of H120 and 1/96 avian infectious bronchitis virus vaccine strains protect chickens against challenge with IS/1494/06 (variant 2)-like infectious bronchitis virus. Acta Virol 61:150–160. 10.4149/av_2017_02_04. [DOI] [PubMed] [Google Scholar]
- 182.Hajjar AM, DiGiacomo RF, Carpenter JK, Bingel SA, Moazed TC. 1991. Chronic sialodacryoadenitis virus (SDAV) infection in athymic rats. Lab Anim Sci 41:22–25. [PubMed] [Google Scholar]
- 183.Hale VL, Dennis PM, McBride DS, Nolting JM, Madden C, Huey D, Ehrlich M, Grieser J, Winston J, Lombardi D, Gibson S, Saif L, Killian ML, Lantz K, Tell RM, Torchetti M, Robbe-Austerman S, Nelson MI, Faith SA, Bowman AS. 2022. SARS-CoV-2 infection in free-ranging white-tailed deer. Nature 602:481–486. 10.1038/s41586-021-04353-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Hamre D, Beem M. 1972. Virologic studies of acute respiratory disease in young adults. V. Coronavirus 229E infections during six years of surveillance. Am J Epidemiol 96:94–106. 10.1093/oxfordjournals.aje.a121445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Hamre D, Procknow JJ. 1966. A new virus isolated from the human respiratory tract. Proc Soc Exp Biol Med 121:190–193. 10.3181/00379727-121-30734. [DOI] [PubMed] [Google Scholar]
- 186.Han Z, Liwen X, Ren M, Sheng J, Ma T, Sun J, Zhao Y, Liu S. 2020. Genetic, antigenic and pathogenic characterization of avian coronaviruses isolated from pheasants (Phasianus colchicus) in China. Vet Microbiol 240:108513. 10.1016/j.vetmic.2019.108513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hemida MG, Chu DK, Poon LL, Perera RA, Alhammadi MA, Ng HY, Siu LY, Guan Y, Alnaeem A, Peiris M. 2014. MERS coronavirus in dromedary camel herd, Saudi Arabia. Emerg Infect Dis 20:1231–1234. 10.3201/eid2007.140571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Hemida MG, Chu DKW, Perera R, Ko RLW, So RTY, Ng BCY, Chan SMS, Chu S, Alnaeem AA, Alhammadi MA, Webby RJ, Poon LLM, Balasuriya UBR, Peiris M. 2017. Coronavirus infections in horses in Saudi Arabia and Oman. TransboundEmerg Dis 64:2093–2103. 10.1111/tbed.12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Henning M. 1957. Transmissible gastro-enteritis of pigs (a review). J S Afr Vet Assoc 28:111–117. [Google Scholar]
- 190.Hensley LE, Baric RS. 1998. Human biliary glycoproteins function as receptors for interspecies transfer of mouse hepatitis virus. Adv Exp Med Biol 440:43–52. 10.1007/978-1-4615-5331-1_6. [DOI] [PubMed] [Google Scholar]
- 191.Hensley LE, Holmes KV, Beauchemin N, Baric RS. 1998. Virus-receptor interactions and interspecies transfer of a mouse hepatitis virus. Adv Exp Med Biol 440:33–41. 10.1007/978-1-4615-5331-1_5. [DOI] [PubMed] [Google Scholar]
- 192.Herrewegh AAPM, Smeenk I, Horzinek MC, Rottier PJM, De Groot RJ. 1998. Feline coronavirus type II trains 79-1683 and 79-1146 originate from a double recombination between feline coronavirus type I and canine coronavirus. J Virol 72:4508–4514. 10.1128/JVI.72.5.4508-4514.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Hierholzer JC, Broderson JR, Murphy FA. 1979. New strain of mouse hepatitis virus as the cause of lethal enteritis in infant mice. Infect Immun 24:508–522. 10.1128/iai.24.2.508-522.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Hofmann H, Pyrc K, van der Hoek L, Geier M, Berkhout B, Pöhlmann S. 2005. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proc Natl Acad Sci USA 102:7988–7993. 10.1073/pnas.0409465102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Homberger FR. 1992. Maternally-derived passive immunity to enterotropic mouse hepatitis virus. Arch Virol 122:133–141. 10.1007/BF01321123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Homberger FR. 1997. Enterotropic mouse hepatitis virus. Lab Anim 31:97–115. 10.1258/002367797780600189. [DOI] [PubMed] [Google Scholar]
- 197.Homberger FR, Zhang L, Barthold SW. 1998. Prevalence of enterotropic and polytropic mouse hepatitis virus in enzootically infected mouse colonies. Lab Anim Sci 48:50–54. [PubMed] [Google Scholar]
- 198.Hu B, Ge X, Wang LF, Shi Z. 2015. Bat origin of human coronaviruses. Virol J 12:221. 10.1186/s12985-015-0422-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Huang C, Liu WJ, Xu W, Jin T, Zhao Y, Song J, Shi Y, Ji W, Jia H, Zhou Y, Wen H, Zhao H, Liu H, Li H, Wang Q, Wu Y, Wang L, Liu D, Liu G, Yu H, Holmes EC, Lu L, Gao GF. 2016. A bat-derived putative cross-family recombinant coronavirus with a reovirus gene. PLoS Pathog 12:e1005883. 10.1371/journal.ppat.1005883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Huang C, Lokugamage KG, Rozovics JM, Narayanan K, Semler BL, Makino S. 2011. Alphacoronavirus transmissible gastroenteritis virus nsp1 protein suppresses protein translation in mammalian cells and in cell-free HeLa cell extracts but not in rabbit reticulocyte lysate. J Virol 85:638–643. 10.1128/JVI.01806-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Huang JC, Wright SL, Shipley WD. 1983. Isolation of coronavirus-like agent from horses suffering from acute equine diarrhoea syndrome. Vet Rec 113:262–263. 10.1136/vr.113.12.262. [DOI] [PubMed] [Google Scholar]
- 202.Huang YW, Dickerman AW, Piñeyro P, Li L, Fang L, Kiehne R, Opriessnig T, Meng XJ. 2013. Origin, evolution, and genotyping of emergent porcine epidemic diarrhea virus strains in the United States. MBio 4:e00737-13. 10.1128/mBio.00737-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Huong NQ, Thanh Nga NT, Van Long N, Luu BD, Latinne A, Pruvot M, Phuong NT, Vinh Quang LT, Van Hung V, Lan NT, Hoa NT, Minh PQ, Diep NT, Tung N, Ky VD, Roberton SI, Thuy HB, Van Long N, Gilbert M, Wicker L, Mazet JAK, Johnson CK, Goldstein T, Tremeau-Bravard A, Ontiveros V, Joly DO, Walzer C, Fine AE, Olson SH. 2020. Coronavirus testing indicates transmission risk increases along wildlife supply chains for human consumption in Viet Nam, 2013-2014. PLoS One 15:e0237129. 10.1371/journal.pone.0237129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Hurst KR, Koetzner CA, Masters PS. 2009. Identification of in vivo-interacting domains of the murine coronavirus nucleocapsid protein. J Virol 83:7221–7234. 10.1128/JVI.00440-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Hwang M, Bergmann CC. 2018. Alpha/beta interferon (IFN-α/β) signaling in astrocytes mediates protection against viral encephalomyelitis and regulates IFN-γ-dependent responses. J Virol 92:e01901-17. 10.1128/JVI.01901-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.International Committee on Taxonomy of Viruses (ICTV). [Internet]. 2021. Virus Taxonomy: 2020 Release. [Cited 5 October 2021]. Available at: https://talk.ictvonline.org/taxonomy/.
- 207.Ishida T, Taguchi F, Lee YS, Yamada A, Tamura T, Fujiwara K. 1978. Isolation of mouse hepatitis virus from infant mice with fatal diarrhea. Lab Anim Sci 28:269–276. [PubMed] [Google Scholar]
- 208.Ismail MM, Tang AY, Saif YM. 2003. Pathogenicity of turkey coronavirus in turkeys and chickens. Avian Dis 47:515–522. 10.1637/5917. [DOI] [PubMed] [Google Scholar]
- 209.Izes AM, Yu J, Norris JM, Govendir M. 2020. Current status on treatment options for feline infectious peritonitis and SARS-CoV-2 positive cats. Vet Q 40:322–330. 10.1080/01652176.2020.1845917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Jaax GP, Jaax NK, Petrali JP, Corcoran KD, Vogel AP. 1990. Coronavirus-like virions associated with a wasting syndrome in guinea pigs. Lab Anim Sci 40:375–378. [PubMed] [Google Scholar]
- 211.Jackwood MW, de Wit S. 2019. Infectious Bronchitis, p 167–188. In: Swayne DE, Boulianne M, Logue CM, McDougald LR, Venugopal N, Suarez DL, de Wit S, Grimes T, Johnson D, Kromm M, Prajitno TY, Rubinoff I, Zavala G, editors. Diseases of Poultry, 14th edition. Hoboken (NJ: ): Wiley & Sons. [Google Scholar]
- 212.Jacoby RO, Bhatt PN, Jonas AM. 1975. Pathogenesis of sialodacryoadenitis in gnotobiotic rats. Vet Pathol 12:196–209. 10.1177/030098587501200305. [DOI] [PubMed] [Google Scholar]
- 213.Jaimes JA, Millet JK, Stout AE, André NM, Whittaker GR. 2020. A tale of two viruses: The distinct spike glycoproteins of feline coronaviruses. Viruses 12:83. 10.3390/v12010083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Jaimes JA, Whittaker GR. 2018. Feline coronavirus: Insights into viral pathogenesis based on the spike protein structure and function. Virology 517:108–121. 10.1016/j.virol.2017.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Ji CM, Wang B, Zhou J, Huang YW. 2018. Aminopeptidase-N-independent entry of porcine epidemic diarrhea virus into Vero or porcine small intestine epithelial cells. Virology 517:16–23. 10.1016/j.virol.2018.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Jin L, Cebra CK, Baker RJ, Mattson DE, Cohen SA, Alvarado DE, Rohrmann GF. 2007. Analysis of the genome sequence of an alpaca coronavirus. Virology 365:198–203. 10.1016/j.virol.2007.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Johns Hopkins Universiry of Medicine. [Internet]. 2021. Coronavirus Resource Center. [Cited 23 September 2021]. Available at: https://coronavirus.jhu.edu/map.html. [Google Scholar]
- 218.Johns Hopkins University & Medicine. [Internet]. 2021. The Johns Hopkins Coronavirus Resource Center (CRC) - Vaccine Resarch& Development. [Cited 23 September 2021]. Available at: https://coronavirus.jhu.edu/vaccines/timeline#:~:text=A%20typical%20vaccine%20development%20timeline,vaccine%20doses%20for%20widespread%20distribution.
- 219.Jorgensen BB. 1968. Spontaneous deaths among rabbits inoculated with Treponema pallidum less than 2 weeks before. Abnormal susceptibility in apparently normal laboratory rabbits indicated by serological tests for human syphilis. Z Versuchstierkd 10:46–54. [PubMed] [Google Scholar]
- 220.Jung K, Hu H, Saif LJ. 2016. Porcine deltacoronavirus infection: Etiology, cell culture for virus isolation and propagation, molecular epidemiology and pathogenesis. Virus Res 226:50–59. 10.1016/j.virusres.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Jung K, Saif LJ. 2015. Porcine epidemic diarrhea virus infection: Etiology, epidemiology, pathogenesis and immunoprophylaxis. Vet J 204:134–143. 10.1016/j.tvjl.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Kanno T, Ishihara R, Hatama S, Uchida I. 2018. A long-term animal experiment indicating persistent infection of bovine coronavirus in cattle. J Vet Med Sci 80:1134–1137. 10.1292/jvms.18-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kasereka MC, Hawkes MT. 2021. Neuroinvasive potential of human coronavirus OC43: Case report of fatal encephalitis in an immunocompromised host. J Neurovirol 27:340–344. 10.1007/s13365-020-00926-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Kasuga Y, Zhu B, Jang KJ, Yoo JS. 2021. Innate immune sensing of coronavirus and viral evasion strategies. Exp Mol Med 53:723–736. 10.1038/s12276-021-00602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Keck JG, Makino S, Soe LH, Fleming JO, Stohlman SA, Lai MM. 1987. RNA recombination of coronavirus. Adv Exp Med Biol 218:99–107. 10.1007/978-1-4684-1280-2_11. [DOI] [PubMed] [Google Scholar]
- 226.Kemeny LJ, Wiltsey VL, Riley JL. 1975. Upper respiratory infection of lactating sows with transmissible gastroenteritis virus following contact exposure to infected piglets. Cornell Vet 65:352–362. [PubMed] [Google Scholar]
- 227.Kemeny LJ, Woods RD. 1977. Quantitative transmissible gastroenteritis virus shedding patterns in lactating sows. Am J Vet Res 38:307–310. [PubMed] [Google Scholar]
- 228.Kennedy M, Citino S, McNabb AH, Moffatt AS, Gertz K, Kania S. 2002. Detection of feline coronavirus in captive Felidae in the USA. J Vet Diagn Invest 14:520–522. 10.1177/104063870201400615. [DOI] [PubMed] [Google Scholar]
- 229.Kennedy M, Kania S, Stylianides E, Bertschinger H, Keet D, van Vuuren M. 2003. Detection of feline coronavirus infection in southern African nondomestic felids. J Wildl Dis 39:529–535. 10.7589/0090-3558-39.3.529. [DOI] [PubMed] [Google Scholar]
- 230.Kennedy MA. 2020. Feline infectious peritonitis: Update on pathogenesis, diagnostics, and treatment. Vet Clin North Am Small Anim Pract 50:1001–1011. 10.1016/j.cvsm.2020.05.002. [DOI] [PubMed] [Google Scholar]
- 231.Khalafalla AI, Lu X, Al-Mubarak AI, Dalab AH, Al-Busadah KA, Erdman DD. 2015. MERS-CoV in upper respiratory tract and lungs of dromedary camels, Saudi Arabia, 2013-2014. Emerg Infect Dis 21:1153–1158. 10.3201/eid2107.150070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Khanolkar A, Hartwig SM, Haag BA, Meyerholz DK, Epping LL, Haring JS, Varga SM, Harty JT. 2009. Protective and pathologic roles of the immune response to mouse hepatitis virus type 1: Implications for severe acute respiratory syndrome. J Virol 83:9258–9272. 10.1128/JVI.00355-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Kim ES, Choe PG, Park WB, Oh HS, Kim EJ, Nam EY, Na SH, Kim M, Song KH, Bang JH, Park SW, Kim HB, Kim NJ, Oh MD. 2016. Clinical progression and cytokine profiles of Middle East Respiratory Syndrome coronavirus infection. J Korean Med Sci 31:1717–1725. 10.3346/jkms.2016.31.11.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Kim L, Chang KO, Sestak K, Parwani A, Saif LJ. 2000. Development of a reverse transcription-nested polymerase chain reaction assay for differential diagnosis of transmissible gastroenteritis virus and porcine respiratory coronavirus from feces and nasal swabs of infected pigs. J Vet Diagn Invest 12:385–388. 10.1177/104063870001200418. [DOI] [PubMed] [Google Scholar]
- 235.Klein-Richers U, Hartmann K, Hofmann-Lehmann R, Unterer S, Bergmann M, Rieger A, Leutenegger C, Pantchev N, Balzer J, Felten S. 2020. Prevalence of feline coronavirus shedding in German catteries and associated risk factors. Viruses 12:1000. 10.3390/v12091000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K. 2004. Learning from SARS: Preparing for the next disease outbreak: Workshop summary. Forum on microbial threats. Washington (DC: ): National Academies Press. 10.17226/10915. [DOI] [PubMed] [Google Scholar]
- 237.Kojima A, Okaniwa A. 1991. Antigenic heterogeneity of sialodacryoadenitis virus isolates. J Vet Med Sci 53:1059–1063. 10.1292/jvms.53.1059. [DOI] [PubMed] [Google Scholar]
- 238.Koopmans M. 2021. SARS-CoV-2 and the human-animal interface: Outbreaks on mink farms. Lancet Infect Dis 21:18–19. 10.1016/S1473-3099(20)30912-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Körner RW, Majjouti M, Alcazar MAA, Mahabir E. 2020. Of mice and men: The coronavirus MHV and mouse models as a translational approach to understand SARS-CoV-2. Viruses 12:880. 10.3390/v12080880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Kraft LM. 1966. Epizootic diarrhea of infant mice and lethal intestinal virus infection of infant mice. Natl Cancer Inst Monogr 20:55–61. [PubMed] [Google Scholar]
- 241.Krijnse-Locker J, Ericsson M, Rottier PJ, Griffiths G. 1994. Characterization of the budding compartment of mouse hepatitis virus: evidence that transport from the RER to the Golgi complex requires only one vesicular transport step. J Cell Biol 124:55–70. 10.1083/jcb.124.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, Rollin PE, Dowell SF, Ling AE, Humphrey CD, Shieh WJ, Guarner J, Paddock CD, Rota P, Fields B, DeRisi J, Yang JY, Cox N, Hughes JM, LeDuc JW, Bellini WJ, Anderson LJ. 2003. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 348:1953–1966. 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 243.Kuchipudi SV, Surendran-Nair M, Ruden RM, Yon M, Nissly RH, Nelli RK, Li L, Jayarao BM, Vandegrift KJ, Maranas CD, Levine N, Willgert K, Conlan AJK, Olsen RJ, Davis JJ, Musser JM, Hudson PJ, Kapur V. 2021. Multiple spillovers and onward transmission of SARS-CoV-2 in free-living and captive white-tailed deer. Proc Natl Acade Sci U S A 119:e2121644119. 10.1101/2021.10.31.466677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Kumar P, Gunalan V, Liu B, Chow VT, Druce J, Birch C, Catton M, Fielding BC, Tan YJ, Lal SK. 2007. The nonstructural protein 8 (nsp8) of the SARS coronavirus interacts with its ORF6 accessory protein. Virology 366:293–303. 10.1016/j.virol.2007.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Kunita S, Mori M, Terada E. 1993. Sequence analysis of the nucleocapsid protein gene of rat coronavirus SDAV-681. Virology 193:520–523. 10.1006/viro.1993.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Kuo L, Masters PS. 2013. Functional analysis of the murine coronavirus genomic RNA packaging signal. J Virol 87:5182–5192. 10.1128/JVI.00100-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.La ReginaM, Woods L, Klender P, Gaertner DJ, Paturzo FX. 1992. Transmission of sialodacryoadenitis virus (SDAV) from infected rats to rats and mice through handling, close contact, and soiled bedding.Lab Anim Sci 42:344–346. [PubMed] [Google Scholar]
- 248.Laconi A, van Beurden SJ, Berends AJ, Krämer-Kühl A, Jansen CA, Spekreijse D, Chénard G, Philipp HC, Mundt E, Rottier PJM, Hélène Verheije M. 2018. Deletion of accessory genes 3a, 3b, 5a or 5b from avian coronavirus infectious bronchitis virus induces an attenuated phenotype both in vitro and in vivo. J Gen Virol 99:1381–1390. 10.1099/jgv.0.001130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Lai MM, Baric RS, Makino S, Keck JG, Egbert J, Leibowitz JL, Stohlman SA. 1985. Recombination between nonsegmented RNA genomes of murine coronaviruses. J Virol 56:449–456. 10.1128/jvi.56.2.449-456.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Lai MM, Fleming JO, Stohlman SA, Fujiwara K. 1983. Genetic heterogeneity of murine coronaviruses. Arch Virol 78:167–175. 10.1007/BF01311312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Lai MMC. 1995. Transcription, replication, recombination, and engineering of coronavirus genes, p 463–471. In: Talbot PJ, Levy GA, editors. Corona- and Related Viruses: Current Concepts in Molecular Biology and Pathogenesis. Boston (MA): Springer US. [DOI] [PubMed] [Google Scholar]
- 252.Lai YL, Jacoby RO, Bhatt PN, Jonas AM. 1976. Keratoconjunctivitis associated with sialodacryoadenitis in rats. Invest Ophthalmol 15:538–541. [PubMed] [Google Scholar]
- 253.Lam TT-Y, Jia N, Zhang Y-W, Shum MH-H, Jiang J-F, Zhu H-C, Tong Y-G, Shi Y-X, Ni X-B, Liao Y-S, Li W-J, Jiang B-G, Wei W, Yuan T-T, Zheng K, Cui X-M, Li J, Pei G-Q, Qiang X, Cheung WY-M, Li L-F, Sun F-F, Qin S, Huang J-C, Leung GM, Holmes EC, Hu Y-L, Guan Y, Cao W-C. 2020. Identifying SARS-CoV-2-related coronaviruses in Malayan pangolins. Nature 583:282–285. 10.1038/s41586-020-2169-0. [DOI] [PubMed] [Google Scholar]
- 254.Lamers MM, Smits SL, Hundie GB, Provacia LB, Koopmans M, Osterhaus A, Haagmans BL, Raj VS. 2016. Naturally occurring recombination in ferret coronaviruses revealed by complete genome characterization. J Gen Virol 97:2180–2186. 10.1099/jgv.0.000520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Lapierre J, Marsolais G, Pilon P, Descôteaux JP. 1980. Preliminary report on the observation of a coronavirus in the intestine of the laboratory rabbit. Can J Microbiol 26:1204–1208. 10.1139/m80-201. [DOI] [PubMed] [Google Scholar]
- 256.Larsen AE, Gorham JR. 1975. A new mink enteritis: An initial report. Vet Med Small Anim Clin 70:291–292. [PubMed] [Google Scholar]
- 257.Latinne A, Hu B, Olival KJ, Zhu G, Zhang L, Li H, Chmura AA, Field HE, Zambrana-Torrelio C, Epstein JH, Li B, Zhang W, Wang L-F, Shi Z-L, Daszak P. 2020. Origin and cross-species transmission of bat coronaviruses in China. Nat Commun 11:4235. 10.1038/s41467-020-17687-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 258.Lau SK, Woo PC, Yip CC, Tse H, Tsoi HW, Cheng VC, Lee P, Tang BS, Cheung CH, Lee RA, So LY, Lau YL, Chan KH, Yuen KY. 2006. Coronavirus HKU1 and other coronavirus infections in Hong Kong. J Clin Microbiol 44:2063–2071. 10.1128/JCM.02614-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Lau SKP, Lau CCY, Chan KH, Li CPY, Chen H, Jin DY, Chan JFW, Woo PCY, Yuen KY. 2013. Delayed induction of proinflammatory cytokines and suppression of innate antiviral response by the novel Middle East respiratory syndrome coronavirus: implications for pathogenesis and treatment. J Gen Virol 94:2679–2690. 10.1099/vir.0.055533-0. [DOI] [PubMed] [Google Scholar]
- 260.Lau SKP, Woo PCY, Yip CCY, Fan RYY, Huang Y, Wang M, Guo R, Lam CSF, Tsang AKL, Lai KKY, Chan K-H, Che X-Y, Zheng B-J, Yuen K-Y. 2012. Isolation and characterization of a novel betacoronavirus subgroup A coronavirus, rabbit coronavirus HKU14, from domestic rabbits. J Virol 86:5481–5496. 10.1128/JVI.06927-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Lau SKP, Zhang L, Luk HKH, Xiong L, Peng X, Li KSM, He X, Zhao PS, Fan RYY, Wong ACP, Ahmed SS, Cai JP, Chan JFW, Sun Y, Jin D, Chen H, Lau TCK, Kok RKH, Li W, Yuen KY, Woo PCY. 2018. Receptor usage of a novel bat lineage C betacoronavirus reveals evolution of Middle East Respiratory Syndrome-related coronavirus spike proteins for human dipeptidyl peptidase 4 binding. J Infect Dis 218:197–207. 10.1093/infdis/jiy018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Lau SKY, Woo PCY, Li KSM, Tsang AKL, Fan RYY, Luk HKH, Cai JP, Chan KH, Zheng BJ, Wang M, Yuen KY. 2015. Discovery of a novel coronavirus, China Rattus coronavirus HKU24, from norway rats supports the murine origin of Betacoronavirus 1 and has implications for the ancestor of Betacoronavirus lineage A. J Virol 89:3076–3092. 10.1128/JVI.02420-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Lau YL, Peiris JS. 2005. Pathogenesis of severe acute respiratory syndrome. Curr Opin Immunol 17:404–410. 10.1016/j.coi.2005.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Laude H, Gelfi J, Lavenant L, Charley B. 1992. Single amino acid changes in the viral glycoprotein M affect induction of alpha interferon by the coronavirus transmissible gastroenteritis virus. J Virol 66:743–749. 10.1128/jvi.66.2.743-749.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Lauzi S, Stranieri A, Giordano A, Luzzago C, Zehender G, Paltrinieri S, Ebranati E. 2020. Origin and transmission of Feline coronavirus type I in domestic cats from Northern Italy: A phylogeographic approach. Vet Microbiol 244:108667. 10.1016/j.vetmic.2020.108667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Law HK, Cheung CY, Ng HY, Sia SF, Chan YO, Luk W, Nicholls JM, Peiris JS, Lau YL. 2005. Chemokine up-regulation in SARS-coronavirus-infected, monocyte-derived human dendritic cells. Blood 106:2366–2374. 10.1182/blood-2004-10-4166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Learn JR. 2021. [Internet]. Black-footed ferret COVID-19 vaccination seems to be working. The Wildlife Society. [Cited 28 March 2022]. Available at: https://wildlife.org/black-footed-ferret-covid-19-vaccination-seems-to-be-working/ [Google Scholar]
- 268.Lee JS, Park S, Jeong HW, Ahn JY, Choi SJ, Lee H, Choi B, Nam SK, Sa M, Kwon JS, Jeong SJ, Lee HK, Park SH, Park SH, Choi JY, Kim SH, Jung I, Shin EC. 2020. Immunophenotyping of COVID-19 and influenza highlights the role of type I interferons in development of severe COVID-19. Sci Immunol 5:eabd1554. 10.1126/sciimmunol.abd1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Lee WS, Wheatley AK, Kent SJ, DeKosky BJ. 2020. Antibody-dependent enhancement and SARS-CoV-2 vaccines and therapies. Nat Microbiol 5:1185–1191. 10.1038/s41564-020-00789-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Lei L, Ying S, Baojun L, Yi Y, Xiang H, Wenli S, Zounan S, Deyin G, Qingyu Z, Jingmei L, Guohui C. 2013. Attenuation of mouse hepatitis virus by deletion of the LLRKxGxKG region of Nsp1. PLoS One 8:e61166. 10.1371/journal.pone.0061166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Leroy EM, ArGouilh M, Brugère-Picoux J. 2020. The risk of SARS-CoV-2 transmission to pets and other wild and domestic animals strongly mandates a one-health strategy to control the COVID-19 pandemic. One Health 10:100133. 10.1016/j.onehlt.2020.100133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Levy GA, Leibowitz JL, Edgington TS. 1981. Induction of monocyte procoagulant activity by murine hepatitis virus type 3 parallels disease susceptibility in mice. J Exp Med 154:1150–1163. 10.1084/jem.154.4.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Li BX, Ge JW, Li YJ. 2007. Porcine aminopeptidase N is a functional receptor for the PEDV coronavirus. Virology 365:166–172. 10.1016/j.virol.2007.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. 2020. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 382:1199–1207. 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Li R, Qiao S, Yang Y, Guo J, Xie S, Zhou E, Zhang G. 2016. Genome sequencing and analysis of a novel recombinant porcine epidemic diarrhea virus strain from Henan, China. Virus Genes 52:91–98. 10.1007/s11262-015-1254-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Li TC, Yoshizaki S, Kataoka M, Doan YH, Ami Y, Suzaki Y, Nakamura T, Takeda N, Wakita T. 2017. Determination of ferret enteric coronavirus genome in laboratory ferrets. Emerg Infect Dis 23:1568–1570. 10.3201/eid2309.160215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC, Choe H, Farzan M. 2003. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426:450–454. 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Li W, Wong S-K, Li F, Kuhn JH, Huang I-C, Choe H, Farzan M. 2006. Animal origins of the severe acute respiratory syndrome coronavirus: Insight from ACE2-S-protein interactions. J Virol 80:4211–4219. 10.1128/JVI.80.9.4211-4219.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Li Y, Wu Q, Huang L, Yuan C, Wang J, Yang Q. 2018. An alternative pathway of enteric PEDV dissemination from nasal cavity to intestinal mucosa in swine. Nat Commun 9:3811. 10.1038/s41467-018-06056-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Liais E, Croville G, Mariette J, Delverdier M, Lucas M-N, Klopp C, Lluch J, Donnadieu C, Guy JS, Corrand L, Ducatez MF, Guérin J-L. 2014. Novel avian coronavirus and fulminating disease in guinea fowl, France. Emerg Infect Dis 20:105–108. 10.3201/eid2001.130774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Liang SC, Schoeb TR, Davis JK, Simecka JW, Cassell GH, Lindsey JR. 1995. Comparative severity of respiratory lesions of sialodacryoadenitis virus and Sendai virus infections in LEW and F344 rats. Vet Pathol 32:661–667. 10.1177/030098589503200607. [DOI] [PubMed] [Google Scholar]
- 282.Licitra BN, Duhamel GE, Whittaker GR. 2014. canine enteric coronaviruses: Emerging viral pathogens with distinct recombinant spike proteins. Viruses 6:3363–3376. 10.3390/v6083363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Licitra BN, Millet JK, Regan AD, Hamilton BS, Rinaldi VD, Duhamel GE, Whittaker GR. 2013. Mutation in spike protein cleavage site and pathogenesis of feline coronavirus. Emerg Infect Dis 19:1066–1073. 10.3201/eid1907.121094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Liu C, Tang J, Ma Y, Liang X, Yang Y, Peng G, Qi Q, Jiang S, Li J, Du L, Li F. 2015. Receptor usage and cell entry of porcine epidemic diarrhea coronavirus. J Virol 89:6121–6125. 10.1128/JVI.00430-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Liu P, Jiang J-Z, Wan X-F, Hua Y, Li L, Zhou J, Wang X, Hou F, Chen J, Zou J, Chen J. 2020. Are pangolins the intermediate host of the 2019 novel coronavirus (SARS-CoV-2)? PLoS Pathog 16:e1008421. 10.1371/journal.ppat.1008421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Livanos AE, Jha D, Cossarini F, Gonzalez-Reiche AS, Tokuyama M, Aydillo T, Parigi TL, Ladinsky MS, Ramos I, Dunleavy K, Lee B, Dixon RE, Chen ST, Martinez-Delgado G, Nagula S, Bruce EA, Ko HM, Glicksberg BS, Nadkarni G, Pujadas E, Reidy J, Naymagon S, Grinspan A, Ahmad J, Tankelevich M, Bram Y, Gordon R, Sharma K, Houldsworth J, Britton GJ, Chen-Liaw A, Spindler MP, Plitt T, Wang P, Cerutti A, Faith JJ, Colombel JF, Kenigsberg E, Argmann C, Merad M, Gnjatic S, Harpaz N, Danese S, Cordon-Cardo C, Rahman A, Schwartz RE, Kumta NA, Aghemo A, Bjorkman PJ, Petralia F, van Bakel H, Garcia-Sastre A, Mehandru S. 2021. Intestinal host response to SARS-CoV-2 infection and COVID-19 outcomes in patients with gastrointestinal symptoms. Gastroenterology 160:2435–2450. 10.1053/j.gastro.2021.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, Kovyrshina AV, Lubenets NL, Grousova DM, Erokhova AS, Botikov AG, Izhaeva FM, Popova O, Ozharovskaya TA, Esmagambetov IB, Favorskaya IA, Zrelkin DI, Voronina DV, Shcherbinin DN, Semikhin AS, Simakova YV, Tokarskaya EA, Egorova DA, Shmarov MM, Nikitenko NA, Gushchin VA, Smolyarchuk EA, Zyryanov SK, Borisevich SV, Naroditsky BS, Gintsburg AL. 2021. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia. The Lancet 397:671–681. 10.1016/S0140-6736(21)00234-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Lucas C, Wong P, Klein J, Castro TBR, Silva J, Sundaram M, Ellingson MK, Mao T, Oh JE, Israelow B, Takahashi T, Tokuyama M, Lu P, Venkataraman A, Park A, Mohanty S, Wang H, Wyllie AL, Vogels CBF, Earnest R, Lapidus S, Ott IM, Moore AJ, Muenker MC, Fournier JB, Campbell M, Odio CD, Casanovas-Massana A, Herbst R, Shaw AC, Medzhitov R, Schulz WL, Grubaugh ND, Dela Cruz C, Farhadian S, Ko AI, Omer SB, Iwasaki A. 2020. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature 584:463–469. 10.1038/s41586-020-2588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Luk HKH, Li X, Fung J, Lau SKP, Woo PCY. 2019. Molecular epidemiology, evolution and phylogeny of SARS coronavirus. Infect Genet Evol 71:21–30. 10.1016/j.meegid.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Luna L, Brandão PE, Maturrano L, Rosadio R, Silva FDF, Soares RM, Gregori F. 2015. Betacoronavirus 1 in alpacas (Vicugna pacos) in the High Peruvian Andes. Small Rumin Res 133:7–9. 10.1016/j.smallrumres.2015.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Luytjes W, Bredenbeek PJ, Noten AF, Horzinek MC, Spaan WJ. 1988. Sequence of mouse hepatitis virus A59 mRNA 2: Indications for RNA recombination between coronaviruses and influenza C virus. Virology 166:415–422. 10.1016/0042-6822(88)90512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Luytjes W, Sturman LS, Bredenbeek PJ, Charite J, van der Zeijst BA, Horzinek MC, Spaan WJ. 1987. Primary structure of the glycoprotein E2 of coronavirus MHV-A59 and identification of the trypsin cleavage site. Virology 161:479–487. 10.1016/0042-6822(87)90142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.MacLachlan NJ, Dubovi EJ. 2017. Chapter 24 - Coronaviridae, p 435–462. In: MachLachlan NJ, Dubovi EJ, editors. Fenner’s Veterinary Virology, 5th edition. San Diego (CA: ): Academic Press. [Google Scholar]
- 294.Macphee PJ, Dindzans VJ, Fung LS, Levy GA. 1985. Acute and chronic changes in the microcirculation of the liver in inbred strains of mice following infection with mouse hepatitis virus type 3. Hepatology 5:649–660. 10.1002/hep.1840050422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Malaiyan J, Arumugam S, Mohan K, Gomathi Radhakrishnan G. 2021. An update on the origin of SARS-CoV-2: Despite closest identity, bat (RaTG13) and pangolin derived coronaviruses varied in the critical binding site and O-linked glycan residues. J Med Virol 93:499–505. 10.1002/jmv.26261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Marshall JA, Doultree JC. 1996. Chronic excretion of coronavirus-like particles in laboratory guinea pigs. Lab Anim Sci 46:104–106. [PubMed] [Google Scholar]
- 297.Martina BEE, Haagmans BL, Kuiken T, Fouchier RAM, Rimmelzwaan GF, Van Amerongen G, Peiris JSM, Lim W, Osterhaus ADME. 2003. Virology: SARS virus infection of cats and ferrets. Nature 425:915. 10.1038/425915a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Martínez J, Ramis AJ, Reinacher M, Perpiñán D. 2006. Detection of feline infectious peritonitis virus-like antigen in ferrets. Vet Rec 158:523. 10.1136/vr.158.15.523-b. [DOI] [PubMed] [Google Scholar]
- 299.Maru M, Sato K. 1982. Characterization of a coronavirus isolated from rats with sialoadenitis. Arch Virol 73:33–43. 10.1007/BF01341725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Mathew D, Giles JR, Baxter AE, Oldridge DA, Greenplate AR, Wu JE, Alanio C, Kuri-Cervantes L, Pampena MB, D’Andrea K, Manne S, Chen Z, Huang YJ, Reilly JP, Weisman AR, Ittner CAG, Kuthuru O, Dougherty J, Nzingha K, Han N, Kim J, Pattekar A, Goodwin EC, Anderson EM, Weirick ME, Gouma S, Arevalo CP, Bolton MJ, Chen F, Lacey SF, Ramage H, Cherry S, Hensley SE, Apostolidis SA, Huang AC, Vella LA, Betts MR, Meyer NJ, Wherry EJ. 2020. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science 375:1122–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Matrosovich M, Herrler G, Klenk HD. 2015. Sialic acid receptors of viruses. Top Curr Chem 367:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Mattei DN, Kopper JJ, Sanz MG. 2020. Equine Coronavirus-Associated Colitis in Horses: A Retrospective Study. J Equine Vet Sci 87:102906. 10.1016/j.jevs.2019.102906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.McDonagh P, Sheehy PA, Norris JM. 2011. In vitro inhibition of feline coronavirus replication by small interfering RNAs. Vet Microbiol 150:220–229. 10.1016/j.vetmic.2011.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.McIntosh K, Becker WB, Chanock RM. 1967. Growth in suckling-mouse brain of “IBV-like” viruses from patients with upper respiratory tract disease. Proc Natl Acad Sci USA 58:2268–2273. 10.1073/pnas.58.6.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.McIntosh K, Dees JH, Becker WB, Kapikian AZ, Chanock RM. 1967. Recovery in tracheal organ cultures of novel viruses from patients with respiratory disease. Proc Natl Acad Sci USA 57:933–940. 10.1073/pnas.57.4.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Mebus CA, Stair EL, Rhodes MB, Twiehaus MJ. 1973. Neonatal calf diarrhea: propagation, attenuation, and characteristics of a coronavirus-like agent. Am J Vet Res 34:145–150. [PubMed] [Google Scholar]
- 307.Mebus CA, Stair EL, Rhodes MB, Twiehaus MJ. 1973. Pathology of neonatal calf diarrhea induced by a coronavirus-like agent. Vet Pathol 10:45–64. 10.1177/030098587301000105. [DOI] [PubMed] [Google Scholar]
- 308.Menachemi N, Dixon BE, Wools-Kaloustian KK, Yiannoutsos CT, Halverson PK. 2021. How many SARS-CoV-2-infected people require hospitalization? Using random sample testing to better inform preparedness efforts. J Public Health Manag Pract 27:246–250. 10.1097/PHH.0000000000001331. [DOI] [PubMed] [Google Scholar]
- 309.Menachery VD, Gralinski LE, Mitchell HD, Dinnon KH, 3rd, Leist SR, Yount BL, Jr, Graham RL, McAnarney ET, Stratton KG, Cockrell AS, Debbink K, Sims AC, Waters KM, Baric RS. 2017. Middle East Respiratory Syndrome coronavirus nonstructural protein 16 is necessary for interferon resistance and viral pathogenesis. MSphere2:e00346-17. 10.1128/mSphere.00346-17. [DOI] [PMC free article] [PubMed]
- 310.Meng XJ, Lindsay DS, Sriranganathan N. 2009. Wild boars as sources for infectious diseases in livestock and humans. Philos Trans R Soc Lond B Biol Sci 364:2697–2707. 10.1098/rstb.2009.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Michaels RH, Myerowitz RL. 1983. Viral enhancement of nasal colonization with Haemophilus influenzae type b in the infant rat. Pediatr Res 17:472–473. 10.1203/00006450-198306000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Mihindukulasuriya KA, Wu G, St. Leger J, Nordhausen RW, Wang D. 2008. Identification of a novel coronavirus from a beluga whale by using a panviral microarray. J Virol 82:5084–5088. 10.1128/JVI.02722-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Mikhaleva LM, Cherniaev AL, Samsonova MV, Zayratyants OV, Kakturskiy LV, Vasyukova OA, Birukov AE, Kontorshchikov AS, Sorokina AV, Sinelnikov MY. 2021. Pathological features in 100 deceased patients with COVID-19 in correlation with clinical and laboratory data. Pathol Oncol Res 27:1609900. 10.3389/pore.2021.1609900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Miłek J, Blicharz-Domańska K. 2018. Coronaviruses in avian species - Review with focus on epidemiology and diagnosis in wild birds. J Vet Res 62:249–255. 10.2478/jvetres-2018-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Millet JK, Whittaker GR. 2014. Host cell entry of Middle East respiratory syndrome coronavirus after two-step, furin-mediated activation of the spike protein. Proc Natl Acad Sci USA 111:15214–15219. 10.1073/pnas.1407087111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Min C-K, Cheon S, Ha N-Y, Sohn KM, Kim Y, Aigerim A, Shin HM, Choi J-Y, Inn K-S, Kim J-H, Moon JY, Choi M-S, Cho N-H, Kim Y-S. 2016. Comparative and kinetic analysis of viral shedding and immunological responses in MERS patients representing a broad spectrum of disease severity. Sci Rep 6:25359. 10.1038/srep25359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Mina-Osorio P. 2008. The moonlighting enzyme CD13: Old and new functions to target. Trends Mol Med 14:361–371. 10.1016/j.molmed.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Minami S, Kuroda Y, Terada Y, Yonemitsu K, Van Nguyen D, Kuwata R, Shimoda H, Takano A, Maeda K. 2016. Detection of novel ferret coronaviruses and evidence of recombination among ferret coronaviruses. Virus Genes 52:858–862. 10.1007/s11262-016-1365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Mishra A, Kumar N, Bhatia S, Aasdev A, Kanniappan S, Sekhar AT, Gopinadhan A, Silambarasan R, Sreekumar C, Dubey CK, Tripathi M, Raut AA, Singh VP. 2021. SARS-CoV-2 delta variant among Asiatic Lions, India. Emerg Infect Dis 27:2723. 10.3201/eid2710.211500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Miszczak F, Tesson V, Kin N, Dina J, Balasuriya UB, Pronost S, Vabret A. 2014. First detection of equine coronavirus (ECoV) in Europe. Vet Microbiol 171:206–209. 10.1016/j.vetmic.2014.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Mitchell JA, Brooks HW, Szladovits B, Erles K, Gibbons R, Shields S, Brownlie J. 2013. Tropism and pathological findings associated with canine respiratory coronavirus (CRCoV). Vet Microbiol 162:582–594. 10.1016/j.vetmic.2012.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Miura TA, Travanty EA, Oko L, Bielefeldt-Ohmann H, Weiss SR, Beauchemin N, Holmes KV. 2008. The spike glycoprotein of murine coronavirus MHV-JHM mediates receptor-independent infection and spread in the central nervous systems of Ceacam1a−/− Mice. J Virol 82:755–763. 10.1128/JVI.01851-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Molenaar RJ, Vreman S, Hakze-van der Honing RW, Zwart R, de Rond J, Weesendorp E, Smit LAM, Koopmans M, Bouwstra R, Stegeman A, van der Poel WHM. 2020. Clinical and pathological findings in SARS-CoV-2 disease outbreaks in farmed mink (Neovison vison). Vet Pathol 57:653–657. 10.1177/0300985820943535. [DOI] [PubMed] [Google Scholar]
- 324.Molnar B, Duchamp C, Möstl K, Diehl P-A, Betschart B. 2014. Comparative survey of canine parvovirus, canine distemper virus and canine enteric coronavirus infection in free-ranging wolves of central Italy and south-eastern France. Eur J Wildl Res 60:613–624. 10.1007/s10344-014-0825-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Mora-Díaz JC, Piñeyro PE, Houston E, Zimmerman J, Giménez-Lirola LG. 2019. Porcine Hemagglutinating Encephalomyelitis Virus: A Review. Front Vet Sci 6:53. 10.3389/fvets.2019.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Mora-Díaz JC, Piñeyro PE, Rauh R, Nelson W, Sankoh Z, Gregg E, Carrillo-Ávila JA, Shen H, Nelli RK, Zimmerman JJ, Giménez-Lirola LG. 2021. Porcine Hemagglutinating Encephalomyelitis Virus infection in vivo and ex vivo. J Virol 95:e02335-20. 10.1128/JVI.02335-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Murray J, Kiupel M, Maes RK. 2010. Ferret coronavirus-associated diseases. Vet Clin North Am Exot Anim Pract 13:543–560. 10.1016/j.cvex.2010.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Narayanan K, Huang C, Lokugamage K, Kamitani W, Ikegami T, Tseng CT, Makino S. 2008. Severe acute respiratory syndrome coronavirus nsp1 suppresses host gene expression, including that of type I interferon, in infected cells. J Virol 82:4471–4479. 10.1128/JVI.02472-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Nédellec P, Dveksler GS, Daniels E, Turbide C, Chow B, Basile AA, Holmes KV, Beauchemin N. 1994. Bgp2, a new member of the carcinoembryonic antigen-related gene family, encodes an alternative receptor for mouse hepatitis viruses. J Virol 68:4525–4537. 10.1128/jvi.68.7.4525-4537.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Nemoto M, Kanno T, Bannai H, Tsujimura K, Yamanaka T, Kokado H. 2017. Antibody response to equine coronavirus in horses inoculated with a bovine coronavirus vaccine. J Vet Med Sci 79:1889–1891. 10.1292/jvms.17-0414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Nemoto M, Oue Y, Morita Y, Kanno T, Kinoshita Y, Niwa H, Ueno T, Katayama Y, Bannai H, Tsujimura K, Yamanaka T, Kondo T. 2014. Experimental inoculation of equine coronavirus into Japanese draft horses. Arch Virol 159:3329–3334. 10.1007/s00705-014-2205-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Nemoto M, Schofield W, Cullinane A. 2019. The first detection of equine coronavirus in adult horses and foals in Ireland. Viruses 11:946. 10.3390/v11100946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Neuman BW, Adair BD, Yoshioka C, Quispe JD, Orca G, Kuhn P, Milligan RA, Yeager M, Buchmeier MJ. 2006. Supramolecular architecture of Severe Acute Respiratory Syndrome Coronavirus revealed by electron cryomicroscopy. J Virol 80:7918–7928. 10.1128/JVI.00645-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Ng DL, Al Hosani F, Keating MK, Gerber SI, Jones TL, Metcalfe MG, Tong S, Tao Y, Alami NN, Haynes LM, Mutei MA, Abdel-Wareth L, Uyeki TM, Swerdlow DL, Barakat M, Zaki SR. 2016. Clinicopathologic, immunohistochemical, and ultrastructural findings of a fatal case of Middle East Respiratory Syndrome coronavirus infection in the United Arab Emirates, April 2014. Am J Pathol 186:652–658. 10.1016/j.ajpath.2015.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Ng LFP, Hiscox JA. 2020. Coronaviruses in animals and humans. BMJ 368:m634. 10.1136/bmj.m634. [DOI] [PubMed] [Google Scholar]
- 336.Nicholls JM, Poon LL, Lee KC, Ng WF, Lai ST, Leung CY, Chu CM, Hui PK, Mak KL, Lim W, Yan KW, Chan KH, Tsang NC, Guan Y, Yuen KY, Peiris JS. 2003. Lung pathology of fatal severe acute respiratory syndrome. Lancet 361:1773–1778. 10.1016/S0140-6736(03)13413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Nieto-Torres JL, DeDiego ML, Verdiá-Báguena C, Jimenez-Guardeño JM, Regla-Nava JA, Fernandez-Delgado R, Castaño-Rodriguez C, Alcaraz A, Torres J, Aguilella VM, Enjuanes L. 2014. Severe acute respiratory syndrome coronavirus envelope protein ion channel activity promotes virus fitness and pathogenesis. PLoS Pathog 10:e1004077. 10.1371/journal.ppat.1004077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Oma VS, Tråvén M, Alenius S, Myrmel M, Stokstad M. 2016. Bovine coronavirus in naturally and experimentally exposed calves; viral shedding and the potential for transmission. Virol J 13:100. 10.1186/s12985-016-0555-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Oreshkova N, Molenaar RJ, Vreman S, Harders F, Oude Munnink BB, Hakze-van der Honing RW, Gerhards N, Tolsma P, Bouwstra R, Sikkema RS, Tacken MG, de Rooij MM, Weesendorp E, Engelsma MY, Bruschke CJ, Smit LA, Koopmans M, van der Poel WH, Stegeman A. 2020. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Euro Surveill 25:2001005. 10.2807/1560-7917.ES.2020.25.23.2001005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Osterhaus AD, Teppema JS, van Steenis G. 1982. Coronavirus-like particles in laboratory rabbits with different syndromes in the Netherlands. Lab Anim Sci 32:663–665. [PubMed] [Google Scholar]
- 341.Oude Munnink BB, Sikkema RS, Nieuwenhuijse DF, Molenaar RJ, Munger E, Molenkamp R, van der Spek A, Tolsma P, Rietveld A, Brouwer M, Bouwmeester-Vincken N, Harders F, Hakze-van der Honing R, Wegdam-Blans MCA, Bouwstra RJ, GeurtsvanKessel C, van der Eijk AA, Velkers FC, Smit LAM, Stegeman A, van der Poel WHM, Koopmans MPG. 2021. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science 371:172–177. 10.1126/science.abe5901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Pan Y, Tian X, Qin P, Wang B, Zhao P, Yang YL, Wang L, Wang D, Song Y, Zhang X, Huang YW. 2017. Discovery of a novel swine enteric alphacoronavirus (SeACoV) in southern China. Vet Microbiol 211:15–21. 10.1016/j.vetmic.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Park JE, Shin HJ. 2014. Porcine epidemic diarrhea virus infects and replicates in porcine alveolar macrophages. Virus Res 191:143–152. 10.1016/j.virusres.2014.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Parker JC, Cross SS, Rowe WP. 1970. Rat coronavirus (RCV): a prevalent, naturally occurring pneumotropic virus of rats. Arch Gesamte Virusforsch 31:293–302. 10.1007/BF01253764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Parra B, Hinton DR, Marten NW, Bergmann CC, Lin MT, Yang CS, Stohlman SA. 1999. IFN-gamma is required for viral clearance from central nervous system oligodendroglia. J Immunol 162:1641–1647. [PubMed] [Google Scholar]
- 346.Pedersen NC, Allen CE, Lyons LA. 2008. Pathogenesis of feline enteric coronavirus infection. J Feline Med Surg 10:529–541. 10.1016/j.jfms.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Peeters JE, Pohl P, Charlier G. 1984. Infectious agents associated with diarrhoea in commercial rabbits: A field study. Ann Rech Vet 15:335–340. [PubMed] [Google Scholar]
- 348.Peiris JS, Lai ST, Poon LL, Guan Y, Yam LY, Lim W, Nicholls J, Yee WK, Yan WW, Cheung MT, Cheng VC, Chan KH, Tsang DN, Yung RW, Ng TK, Yuen KY. 2003. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet 361:1319–1325. 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Peng P, Gao Y, Zhou Q, Jiang T, Zheng S, Huang M, Xue C, Cao Y, Xu Z. 2021. Development of an indirect ELISA for detecting swine acute diarrhoea syndrome coronavirus IgG antibodies based on a recombinant spike protein. Transbound Emerg Dis 69:2065–2075. 10.1111/tbed.14196. [DOI] [PubMed] [Google Scholar]
- 350.Pensaert M, Callebaut P, Vergote J. 1986. Isolation of a porcine respiratory, non-enteric coronavirus related to transmissible gastroenteritis. Vet Q 8:257–261. 10.1080/01652176.1986.9694050. [DOI] [PubMed] [Google Scholar]
- 351.Pensaert MB. 1976. [Transmissible Gastroenteritis in Swine (author’s transl)] TijdschrDiergeneeskd 101:165–177. [Article in Dutch]. [PubMed] [Google Scholar]
- 352.Pensaert MB, de Bouck P. 1978. A new coronavirus-like particle associated with diarrhea in swine. Arch Virol 58:243–247. 10.1007/BF01317606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Percy DH, Muckle CA, Hampson RJ, Brash ML. 1993. The enteritis complex in domestic rabbits: A field study. Can Vet J 34:95–102. [PMC free article] [PubMed] [Google Scholar]
- 354.Percy DH, Scott RA. 1991. Coronavirus infection in the laboratory rat: immunization trials using attenuated virus replicated in L-2 cells. Can J Vet Res 55:60–66. [PMC free article] [PubMed] [Google Scholar]
- 355.Percy DH, Williams KL. 1990. Experimental Parker’s coronavirus infection in Wistar rats. Lab Anim Sci 40:603–607. [PubMed] [Google Scholar]
- 356.Percy DH, Williams KL, Bond SJ, MacInnes JI. 1990. Characteristics of Parker’s rat coronavirus (PRC) replicated in L-2 cells. Arch Virol 112:195–202. 10.1007/BF01323164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Perico L, Benigni A, Casiraghi F, Ng LFP, Renia L, Remuzzi G. 2021. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat Rev Nephrol 17:46–64. 10.1038/s41581-020-00357-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Perlman S, Dandekar AA. 2005. Immunopathogenesis of coronavirus infections: Implications for SARS. Nat Rev Immunol 5:917–927. 10.1038/nri1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Perpiñán D, López C. 2008. Clinical aspects of systemic granulomatous inflammatory syndrome in ferrets (Mustela putorius furo). Vet Rec 162:180–183. 10.1136/vr.162.6.180. [DOI] [PubMed] [Google Scholar]
- 360.Peterson EH, Hymas TA. 1951. Antibiotics in the Treatment of an Unfamiliar Turkey Disease. Poult Sci 30:466–468. 10.3382/ps.0300466. [DOI] [Google Scholar]
- 361.Pratelli A, Martella V, Decaro N, Tinelli A, Camero M, Cirone F, Elia G, Cavalli A, Corrente M, Greco G, Buonavoglia D, Gentile M, Tempesta M, Buonavoglia C. 2003. Genetic diversity of a canine coronavirus detected in pups with diarrhoea in Italy. J Virol Methods 110:9–17. 10.1016/S0166-0934(03)00081-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Priestnall SL. 2020. Canine respiratory coronavirus: A naturally occurring model of COVID-19? Vet Pathol 57:467–471. 10.1177/0300985820926485. [DOI] [PubMed] [Google Scholar]
- 363.Priestnall SL, Mitchell JA, Walker CA, Erles K, Brownlie J. 2014. New and emerging pathogens in canine infectious respiratory disease. Vet Pathol 51:492–504. 10.1177/0300985813511130. [DOI] [PubMed] [Google Scholar]
- 364.Pritchard GC. 1987. Transmissible gastroenteritis in endemically infected breeding herds of pigs in East Anglia, 1981-85. Vet Rec 120:226–230. 10.1136/vr.120.10.226. [DOI] [PubMed] [Google Scholar]
- 365.PruttonJ SW, Barnum S, Pusterla N. 2019. Evaluation of safety, humoral immune response and faecal shedding in horses inoculated with a modified-live bovine coronavirus vaccination. Equine Vet Educ. 10.1111/eve.13175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Pullium JK, Homberger FR, Benjamin KA, Dillehay DL, Huerkamp MJ. 2003. Confirmed persistent mouse hepatitis virus infection and transmission by mice with a targeted null mutation of tumor necrosis factor to sentinel mice, using short-term exposure. Comp Med 53:439–443. [PubMed] [Google Scholar]
- 367.Pusterla N, James K, Mapes S, Bain F. 2019. Frequency of molecular detection of equine coronavirus in faeces and nasal secretions in 277 horses with acute onset of fever. Vet Rec 184:385. 10.1136/vr.104919. [DOI] [PubMed] [Google Scholar]
- 368.Pusterla N, Mapes S, Wademan C, White A, Ball R, Sapp K, Burns P, Ormond C, Butterworth K, Bartol J, Magdesian KG. 2013. Emerging outbreaks associated with equine coronavirus in adult horses. Vet Microbiol 162:228–231. 10.1016/j.vetmic.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Pusterla N, Vin R, Leutenegger CM, Mittel LD, Divers TJ. 2018. Enteric coronavirus infection in adult horses. Vet J 231:13–18. 10.1016/j.tvjl.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Raj VS, Mou H, Smits SL, Dekkers DHW, Müller MA, Dijkman R, Muth D, Demmers JAA, Zaki A, Fouchier RAM, Thiel V, Drosten C, Rottier PJM, Osterhaus ADME, Bosch BJ, Haagmans BL. 2013. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature 495:251–254. 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Rempel JD, Murray SJ, Meisner J, Buchmeier MJ. 2004. Differential regulation of innate and adaptive immune responses in viral encephalitis. Virology 318:381–392. 10.1016/j.virol.2003.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Reusken CB, Farag EA, Jonges M, Godeke GJ, El-Sayed AM, Pas SD, Raj VS, Mohran KA, Moussa HA, Ghobashy H, Alhajri F, Ibrahim AK, Bosch BJ, Pasha SK, Al-Romaihi HE, Al-Thani M, Al-Marri SA, Al Hajri MM, Haagmans BL, Koopmans MP. 2014. Middle East respiratory syndrome coronavirus (MERS-CoV) RNA and neutralising antibodies in milk collected according to local customs from dromedary camels, Qatar, April 2014. Euro Surveill 19:20829. 10.2807/1560-7917.ES2014.19.23.20829. [DOI] [PubMed] [Google Scholar]
- 373.Rocha CB, Fornells L, Rojas M, Libetal M, Manchego A, Pezo D, Santos N. 2018. Molecular epidemiology of coronavirus in faeces of Brazilian calves and Peruvian camelid herds. J Infect Dev Ctries 12:37–42. 10.3855/jidc.9528. [DOI] [PubMed] [Google Scholar]
- 374.Roe CK, Alexander TJ. 1958. A Disease of Nursing Pigs Previously Unreported in Ontario. Can J Comp Med Vet Sci 22:305–307. [PMC free article] [PubMed] [Google Scholar]
- 375.Rohaim MA, El Naggar RF, Clayton E, Munir M. 2021. Structural and functional insights into non-structural proteins of coronaviruses. Microb Pathog 150:104641. 10.1016/j.micpath.2020.104641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Rojas M, Manchego A, Rocha CB, Fornells LA, Silva RC, Mendes GS, Dias HG, Sandoval N, Pezo D, Santos N. 2016. Outbreak of diarrhea among preweaning alpacas (Vicugna pacos) in the southern Peruvian highland. J Infect Dev Ctries 10:269–274. 10.3855/jidc.7398. [DOI] [PubMed] [Google Scholar]
- 377.Russell RG, Brian DA, Lenhard A, Potgieter LN, Gillespie D, Clapp NK. 1985. Coronavirus-like particles and Campylobacter in marmosets with diarrhea and colitis. Dig Dis Sci 30:72S–77S. 10.1007/BF01296981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Ryan KA, Bewley KR, Fotheringham SA, Slack GS, Brown P, Hall Y, Wand NI, Marriott AC, Cavell BE, Tree JA, Allen L, Aram MJ, Bean TJ, Brunt E, Buttigieg KR, Carter DP, Cobb R, Coombes NS, Findlay-Wilson SJ, Godwin KJ, Gooch KE, Gouriet J, Halkerston R, Harris DJ, Hender TH, Humphries HE, Hunter L, Ho CMK, Kennard CL, Leung S, Longet S, Ngabo D, Osman KL, Paterson J, Penn EJ, Pullan ST, Rayner E, Skinner O, Steeds K, Taylor I, Tipton T, Thomas S, Turner C, Watson RJ, Wiblin NR, Charlton S, Hallis B, Hiscox JA, Funnell S, Dennis MJ, Whittaker CJ, Catton MG, Druce J, Salguero FJ, Carroll MW. 2021. Dose-dependent response to infection with SARS-CoV-2 in the ferret model and evidence of protective immunity. Nat Commun 12:81. 10.1038/s41467-020-20439-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Rydyznski Moderbacher C, Ramirez SI, Dan JM, Grifoni A, Hastie KM, Weiskopf D, Belanger S, Abbott RK, Kim C, Choi J, Kato Y, Crotty EG, Kim C, Rawlings SA, Mateus J, Tse LPV, Frazier A, Baric R, Peters B, Greenbaum J, Ollmann Saphire E, Smith DM, Sette A, Crotty S. 2020. Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity. Cell 183:996–1012. 10.1016/j.cell.2020.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Saad M, Omrani AS, Baig K, Bahloul A, Elzein F, Matin MA, Selim MA, Al Mutairi M, Al Nakhli D, Al Aidaroos AY, Al Sherbeeni N, Al-Khashan HI, Memish ZA, Albarrak AM. 2014. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis 29:301–306. 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Saif L. 2004. Animal Coronaviruses: Lessons for SARS, p 84–99. In: Knobler S, Mahmoud A, Lemon S, Mack A, Sivitz L, Oberholtzer K, editors. Learning from SARS: Preparing for the next disease outbreak: Workshop summary. Washington (DC: ): The National Academy Press. [PubMed] [Google Scholar]
- 382.Saif L. 2007. Coronaviruses of domestic livestock and poultry: Interspecies transmission, pathogenesis, and immunity, p 279–298. In: Perlman S, Gallagher T, Snijder EJ, editors. Nidoviruses.Washington (DC): ASM Press. [Google Scholar]
- 383.Saif LJ. 2004. Animal coronavirus vaccines: lessons for SARS. Dev Biol (Basel) 119:129–140. [PubMed] [Google Scholar]
- 384.Saif LJ. 2010. Bovine respiratory coronavirus. Vet Clin North Am Food Anim Pract 26:349–364. 10.1016/j.cvfa.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Saif YM, Guy JS, Day JM, Cattoli G, Hayhow CS. 2019. Viral enteric infections, p 401–445. In: Swayne DE, Boulianne M, Logue CM, McDougald LR, Nair V, Suarez DL, de Wit S, Grimes T, Johnson D, Kromm M, Prajitno TY, Rubinoff I, Zavala G, editors. Diseases of poultry, 14th edition. Hoboken (NJ: ): Wiley & Sons. [Google Scholar]
- 386.Sarkar L, Putchala RK, Safiriyu AA, Das Sarma J. 2020. Azadirachta indica A. Juss ameliorates mouse hepatitis virus-induced neuroinflammatory demyelination by modulating cell-to-cell fusion in an experimental animal model of multiple sclerosis. Front Cell Neurosci 14:116. 10.3389/fncel.2020.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Schaefer E, Harms C, Viner M, Barnum S, Pusterla N. 2018. Investigation of an experimental infection model of equine coronavirus in adult horses. J Vet Intern Med 32:2099–2104. 10.1111/jvim.15318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Scherk MA, Ford RB, Gaskell RM, Hartmann K, Hurley KF, Lappin MR, Levy JK, Little SE, Nordone SK, Sparkes AH. 2013. 2013 AAFP feline vaccination advisory panel report. J Feline Med Surg 15:785–808. 10.1177/1098612X13500429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Schlenstedt D, Barnikol H, Plonait H. 1969. [Vomiting and distress in suckling pigs (short clinical report)]. [Article in German]. Dtsch Tierarztl Wochenschr 76:694–695. [PubMed] [Google Scholar]
- 390.Schoeman D, Fielding BC. 2019. Coronavirus envelope protein: Current knowledge. Virol J 16:69. 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Schultze B, Herrler G. 1992. Bovine coronavirus uses N-acetyl-9-O-acetylneuraminic acid as a receptor determinant to initiate the infection of cultured cells. J Gen Virol 73:901–906. 10.1099/0022-1317-73-4-901. [DOI] [PubMed] [Google Scholar]
- 392.Schultze B, Krempl C, Ballesteros ML, Shaw L, Schauer R, Enjuanes L, Herrler G. 1996. Transmissible gastroenteritis coronavirus, but not the related porcine respiratory coronavirus, has a sialic acid (N-glycolylneuraminic acid) binding activity. J Virol 70:5634–5637. 10.1128/jvi.70.8.5634-5637.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Schunk MK, Percy DH, Rosendal S. 1995. Effect of time of exposure to rat coronavirus and Mycoplasma pulmonis on respiratory tract lesions in the Wistar rat. Can J Vet Res 59:60–66. [PMC free article] [PubMed] [Google Scholar]
- 394.Schwegmann-Weßels C, Herrler G. 2006. Sialic acids as receptor determinants for coronaviruses. Glycoconj J 23:51–58. 10.1007/s10719-006-5437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Schwegmann-Weßels C, Herrler G. 2006. Transmissible gastroenteritis virus infection: A vanishing specter. Dtsch Tierarztl Wochenschr 113:157–159. [PubMed] [Google Scholar]
- 396.See RH, Petric M, Lawrence DJ, Mok CPY, Rowe T, Zitzow LA, Karunakaran KP, Voss TG, Brunham RC, Gauldie J, Finlay BB, Roper RL. 2008. Severe acute respiratory syndrome vaccine efficacy in ferrets: Whole killed virus and adenovirus-vectored vaccines. J Gen Virol 89:2136–2146. 10.1099/vir.0.2008/001891-0. [DOI] [PubMed] [Google Scholar]
- 397.Shi J, Wen Z, Zhong G, Yang H, Wang C, Huang B, Liu R, He X, Shuai L, Sun Z, Zhao Y, Liu P, Liang L, Cui P, Wang J, Zhang X, Guan Y, Tan W, Wu G, Chen H, Bu Z. 2020. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science 368:1016–1020. 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Shi Z, Hu Z. 2008. A review of studies on animal reservoirs of the SARS coronavirus. Virus Res 133:74–87. 10.1016/j.virusres.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Shirato K, Maejima M, Islam MT, Miyazaki A, Kawase M, Matsuyama S, Taguchi F. 2016. Porcine aminopeptidase N is not a cellular receptor of porcine epidemic diarrhea virus, but promotes its infectivity via aminopeptidase activity. J Gen Virol 97:2528–2539. 10.1099/jgv.0.000563. [DOI] [PubMed] [Google Scholar]
- 400.Shriner SA, Ellis JW, Root JJ, Roug A, Stopak SR, Wiscomb GW, Zierenberg JR, Ip HS, Torchetti MK, DeLiberto TD. 2021. SARS-CoV-2 exposure in escaped mink, Utah, USA. Emerg Infect Dis 27:988–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Sirinarumitr T, Paul PS, Halbur PG, Kluge JP. 1997. An overview of immunological and genetic methods for detecting swine coronaviruses, transmissible gastroenteritis virus, and porcine respiratory coronavirus in tissues. Adv Exp Med Biol 412:37–46. 10.1007/978-1-4899-1828-4_4. [DOI] [PubMed] [Google Scholar]
- 402.Small JD, Aurelian L, Squire RA, Strandberg JD, Melby EC, Jr, Turner TB, Newman B. 1979. Rabbit cardiomyopathy associated with a virus antigenically related to human coronavirus strain 229E. Am J Pathol 95:709–729. [PMC free article] [PubMed] [Google Scholar]
- 403.Small JD, Woods RD. 1987. Relatedness of rabbit coronavirus to other coronaviruses. Adv Exp Med Biol 218:521–527. 10.1007/978-1-4684-1280-2_68. [DOI] [PubMed] [Google Scholar]
- 404.Smith GC, Lester TL, Heberling RL, Kalter SS. 1982. Coronavirus-like particles in nonhuman primate feces. Arch Virol 72:105–111. 10.1007/BF01314455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Snijder EJ, Bredenbeek PJ, Dobbe JC, Thiel V, Ziebuhr J, Poon LL, Guan Y, Rozanov M, Spaan WJ, Gorbalenya AE. 2003. Unique and conserved features of genome and proteome of SARS-coronavirus, an early split-off from the coronavirus group 2 lineage. J Mol Biol 331:991–1004. 10.1016/S0022-2836(03)00865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Song D, Zhou X, Peng Q, Chen Y, Zhang F, Huang T, Zhang T, Li A, Huang D, Wu Q, He H, Tang Y. 2015. Newly emerged porcine deltacoronavirus associated with diarrhoea in swine in China: Identification, prevalence and full-length genome sequence analysis. Transbound Emerg Dis 62:575–580. 10.1111/tbed.12399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Song HD, Tu CC, Zhang GW, Wang SY, Zheng K, Lei LC, Chen QX, Gao YW, Zhou HQ, Xiang H, Zheng HJ, Chern SW, Cheng F, Pan CM, Xuan H, Chen SJ, Luo HM, Zhou DH, Liu YF, He JF, Qin PZ, Li LH, Ren YQ, Liang WJ, Yu YD, Anderson L, Wang M, Xu RH, Wu XW, Zheng HY, Chen JD, Liang G, Gao Y, Liao M, Fang L, Jiang LY, Li H, Chen F, Di B, He LJ, Lin JY, Tong S, Kong X, Du L, Hao P, Tang H, Bernini A, Yu XJ, Spiga O, Guo ZM, Pan HY, He WZ, Manuguerra JC, Fontanet A, Danchin A, Niccolai N, Li YX, Wu CI, Zhao GP. 2005. Cross-host evolution of severe acute respiratory syndrome coronavirus in palm civet and human. Proc Natl Acad Sci USA 102:2430–2435. 10.1073/pnas.0409608102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Spackman D, Cameron IR. 1983. Isolation of infectious bronchitis virus from pheasants. Vet Rec 113:354–355. 10.1136/vr.113.15.354. [DOI] [PubMed] [Google Scholar]
- 409.Stair EL, Rhodes MB, White RG, Mebus CA. 1972. Neonatal calf diarrhea: Purification and electron microscopy of a coronavirus-like agent. Am J Vet Res 33:1147–1156. [PubMed] [Google Scholar]
- 410.Stavisky J, Pinchbeck GL, German AJ, Dawson S, Gaskell RM, Ryvar R, Radford AD. 2010. Prevalence of canine enteric coronavirus in a cross-sectional survey of dogs presenting at veterinary practices. Vet Microbiol 140:18–24. 10.1016/j.vetmic.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Stephenson N, Swift P, Moeller RB, Worth SJ, Foley J. 2013. Feline infectious peritonitis in a mountain lion (Puma concolor), California, USA. J Wildl Dis 49:408–412. 10.7589/2012-08-210. [DOI] [PubMed] [Google Scholar]
- 412.Stodola JK, Dubois G, Le Coupanec A, Desforges M, Talbot PJ. 2018. The OC43 human coronavirus envelope protein is critical for infectious virus production and propagation in neuronal cells and is a determinant of neurovirulence and CNS pathology. Virology 515:134–149. 10.1016/j.virol.2017.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Stohlman SA, Lai MM. 1979. Phosphoproteins of murine hepatitis viruses. J Virol 32:672–675. 10.1128/jvi.32.2.672-675.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Stokstad M, Klem TB, Myrmel M, Oma VS, Toftaker I, Østerås O, Nødtvedt A. 2020. Using biosecurity measures to combat respiratory disease in cattle: The Norwegian control program for bovine respiratory syncytial virus and bovine coronavirus. Front Vet Sci 7:167. 10.3389/fvets.2020.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Stone AES, Brummet GO, Carozza EM, Kass PH, Petersen EP, Sykes J, Westman ME. 2020. 2020 AAHA/AAFP Feline Vaccination Guidelines. J Feline Med Surg 22:813–830. 10.1177/1098612X20941784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Storz J, Lin X, Purdy CW, Chouljenko VN, Kousoulas KG, Enright FM, Gilmore WC, Briggs RE, Loan RW. 2000. Coronavirus and Pasteurella infections in bovine shipping fever pneumonia and Evans’ criteria for causation. J Clin Microbiol 38:3291–3298. 10.1128/JCM.38.9.3291-3298.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Stout AE, André NM, Jaimes JA, Millet JK, Whittaker GR. 2020. Coronaviruses in cats and other companion animals: Where does SARS-CoV-2/COVID-19 fit? Vet Microbiol 247:108777. 10.1016/j.vetmic.2020.108777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Sturman LS, Holmes KV, Behnke J. 1980. Isolation of coronavirus envelope glycoproteins and interaction with the viral nucleocapsid. J Virol 33:449–462. 10.1128/jvi.33.1.449-462.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Su S, Du L, Jiang S. 2021. Learning from the past: Development of safe and effective COVID-19 vaccines. Nat Rev Microbiol 19:211–219. 10.1038/s41579-020-00462-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, Liu W, Bi Y, Gao GF. 2016. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol 24:490–502. 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Sueyoshi M, Tsuda T, Yamazaki K, Yoshida K, Nakazawa M, Sato K, Minami T, Iwashita K, Watanabe M, Suzuki Y, Mori M. 1995. An immunohistochemical investigation of porcine epidemic diarrhoea. J Comp Pathol 113:59–67. 10.1016/S0021-9975(05)80069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Sun N, Grzybicki D, Castro RF, Murphy S, Perlman S. 1995. Activation of astrocytes in the spinal cord of mice chronically infected with a neurotropic coronavirus. Virology 213:482–493. 10.1006/viro.1995.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Szczepanski A, Owczarek K, Bzowska M, Gula K, Drebot I, Ochman M, Maksym B, Rajfur Z, Mitchell JA, Pyrc K .2019. Canine respiratory coronavirus, bovine coronavirus, and human coronavirus OC43: Receptors and attachment factors. Viruses 11:328. 10.3390/v11040328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Taguchi F, Hirai-Yuki A. 2012. Mouse hepatitis virus receptor as a determinant of the mouse susceptibility to MHV infection. Front Microbiol 3:68. 10.3389/fmicb.2012.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Tai W, He L, Zhang X, Pu J, Voronin D, Jiang S, Zhou Y, Du L. 2020. Characterization of the receptor-binding domain (RBD) of 2019 novel coronavirus: implication for development of RBD protein as a viral attachment inhibitor and vaccine. Cell Mol Immunol 17:613–620. 10.1038/s41423-020-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, Silva J, Mao T, Oh JE, Tokuyama M, Lu P, Venkataraman A, Park A, Liu F, Meir A, Sun J, Wang EY, Casanovas-Massana A, Wyllie AL, Vogels CBF, Earnest R, Lapidus S, Ott IM, Moore AJ, Shaw A, Fournier JB, Odio CD, Farhadian S, Dela Cruz C, Grubaugh ND, Schulz WL, Ring AM, Ko AI, Omer SB, Iwasaki A. 2020. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature 588:315–320. 10.1038/s41586-020-2700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Tao Y, Shi M, Chommanard C, Queen K, Zhang J, Markotter W, Kuzmin IV, Holmes EC, Tong S. 2017. Surveillance of bat coronaviruses in Kenya identifies relatives of human coronaviruses NL63 and 229E and their recombination history. J Virol 91:e01953-16. 10.1128/JVI.01953-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 428.Tarbert DK, Bolin LL, Stout AE, Schaefer DMW, Ruby RE, Rodriguez-Ramos Fernandez J, Duhamel GE, Whittaker GR, de Matos R. 2020. Persistent infection and pancytopenia associated with ferret systemic coronaviral disease in a domestic ferret. J Vet Diagn Invest 32:616–620. 10.1177/1040638720937105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Tekes G, Thiel HJ. 2016. Feline coronaviruses: Pathogenesis of feline infectious peritonitis, p 193–218. In: Ziebuhr J, editor. Coronaviruses. Advances in virus research, vol 96. Cambridge (MA): Academic Press. 10.1016/bs.aivir.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Tennant BJ, Gaskell RM, Kelly DF, Carter SD, Gaskell CJ. 1991. Canine coronavirus infection in the dog following oronasal inoculation. Res Vet Sci 51:11–18. 10.1016/0034-5288(91)90023-H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Terada Y, Minami S, Noguchi K, Mahmoud HY, Shimoda H, Mochizuki M, Une Y, Maeda K. 2014. Genetic characterization of coronaviruses from domestic ferrets, Japan. Emerg Infect Dis 20:284–287. 10.3201/eid2002.130543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Thoms M, Buschauer R, Ameismeier M, Koepke L, Denk T, Hirschenberger M, Kratzat H, Hayn M, Mackens-Kiani T, Cheng J, Straub JH, Stürzel CM, Fröhlich T, Berninghausen O, Becker T, Kirchhoff F, Sparrer KMJ, Beckmann R. 2020. Structural basis for translational shutdown and immune evasion by the Nsp1 protein of SARS-CoV-2. Science 369:1249–1255. 10.1126/science.abc8665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Tizard IR. 2020. Vaccination against coronaviruses in domestic animals. Vaccine 38:5123–5130. 10.1016/j.vaccine.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Toffan A, Catania S, Salviato A, De Battisti C, Vascellari M, Toson M, Capua I, Cattoli G. 2012. Experimental infection of poults and guinea fowl with genetically distinct avian astroviruses. Avian Pathol 41:429–435. 10.1080/03079457.2012.704980. [DOI] [PubMed] [Google Scholar]
- 435.Tohya Y, Narayanan K, Kamitani W, Huang C, Lokugamage K, Makino S. 2009. Suppression of host gene expression by nsp1 proteins of group 2 bat coronaviruses. J Virol 83:5282–5288. 10.1128/JVI.02485-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Tooze J, Tooze S, Warren G. 1984. Replication of coronavirus MHV-A59 in sac- cells: Determination of the first site of budding of progeny virions. Eur J Cell Biol 33:281–293. [PubMed] [Google Scholar]
- 437.Tresnan DB, Levis R, Holmes KV. 1996. Feline aminopeptidase N serves as a receptor for feline, canine, porcine, and human coronaviruses in serogroup I. J Virol 70:8669–8674. 10.1128/jvi.70.12.8669-8674.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Tseng C-T, Sbrana E, Iwata-Yoshikawa N, Newman PC, Garron T, Atmar RL, Peters CJ, Couch RB. 2012. Immunization with SARS coronavirus vaccines leads to pulmonary immunopathology on challenge with the SARS virus. PLoS One 7:e35421. 10.1371/journal.pone.0035421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439.Tsunemitsu H, el-Kanawati ZR, Smith DR, Reed HH, Saif LJ. 1995. Isolation of coronaviruses antigenically indistinguishable from bovine coronavirus from wild ruminants with diarrhea. J Clin Microbiol 33:3264–3269. 10.1128/jcm.33.12.3264-3269.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Tyrrell DA, Almeida JD. 1967. Direct electron-microscopy of organ culture for the detection and characterization of viruses. Arch GesamteVirusforsch 22:417–425. 10.1007/BF01242962. [DOI] [PubMed] [Google Scholar]
- 441.Tyrrell DA, Bynoe ML. 1965. Cultivation of a novel type of common-cold virus in organ cultures. BMJ 1:1467–1470. 10.1136/bmj.1.5448.1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Underdahl NR, Mebus CA, Torres-Medina A. 1975. Recovery of transmissible gastroenteritis virus from chronically infected experimental pigs. Am J Vet Res 36:1473–1476. [PubMed] [Google Scholar]
- 443.US Food and Drug Administration. [Internet]. 2021. Emergency use authorization: COVID drugs. [Cited 15 March 2021]. Available at: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization#coviddrugs.
- 444.US Food and Drug Administration. [Internet]. 2021. Moderna COVID-19 Vaccine. [Cited 15 March 2021]. Available at: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/moderna-covid-19-vaccine.
- 445.US Food and Drug Administration. [Internet]. 2021. Pfizer-BioNTech COVID-19 Vaccine. [Cited 15 March 2021]. Available at: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine.
- 446.van der Hoek L. 2007. Human coronaviruses: What do they cause? AntivirTher 12:651–658. 10.1177/135965350701200S01.1. [DOI] [PubMed] [Google Scholar]
- 447.van der Hoek L, Pyrc K, Jebbink MF, Vermeulen-Oost W, Berkhout RJ, Wolthers KC, Wertheim-van Dillen PM, Kaandorp J, Spaargaren J, Berkhout B. 2004. Identification of a new human coronavirus. Nat Med 10:368–373. 10.1038/nm1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.van der Hoek L, Sure K, Ihorst G, Stang A, Pyrc K, Jebbink MF, Petersen G, Forster J, Berkhout B, Uberla K. 2006. Human coronavirus NL63 infection is associated with croup. Adv Exp Med Biol 581:485–491. 10.1007/978-0-387-33012-9_86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449.Van Cott JL, Brim TA, Simkins RA, Saif LJ. 1993. Isotype-specific antibody-secreting cells to transmissible gastroenteritis virus and porcine respiratory coronavirus in gut- and bronchus-associated lymphoid tissues of suckling pigs. J Immunol 150:3990–4000. [PubMed] [Google Scholar]
- 450.Vennema H, de Groot RJ, Harbour DA, Dalderup M, Gruffydd-Jones T, Horzinek MC, Spaan WJ. 1990. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J Virol 64:1407–1409. 10.1128/jvi.64.3.1407-1409.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.Vijaykrishna D, Smith GJD, Zhang JX, Peiris JSM, Chen H, Guan Y. 2007. Evolutionary insights into the ecology of coronaviruses. J Virol 81:4012–4020. 10.1128/JVI.02605-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Vijgen L, Keyaerts E, Lemey P, Moës E, Li S, Vandamme AM, Van Ranst M. 2005. Circulation of genetically distinct contemporary human coronavirus OC43 strains. Virology 337:85–92. 10.1016/j.virol.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Virelizier JL, Virelizier AM, Allison AC. 1976. The role of circulating interferon in the modifications of immune responsiveness by mouse hepatitis virus (MHV-3). J Immunol 117:748–753. [PubMed] [Google Scholar]
- 454.Vlasova AN, Halpin R, Wang S, Ghedin E, Spiro DJ, Saif LJ. 2011. Molecular characterization of a new species in the genus Alphacoronavirus associated with mink epizootic catarrhal gastroenteritis. J Gen Virol 92:1369–1379. 10.1099/vir.0.025353-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Vlasova AN, Marthaler D, Wang Q, Culhane MR, Rossow KD, Rovira A, Collins J, Saif LJ. 2014. Distinct characteristics and complex evolution of PEDV strains, North America, May 2013-February 2014. Emerg Infect Dis 20:1620–1628. 10.3201/eid2010.140491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Wang L, Junker D, Collisson EW. 1993. Evidence of natural recombination within the S1 gene of infectious bronchitis virus. Virology 192:710–716. 10.1006/viro.1993.1093. [DOI] [PubMed] [Google Scholar]
- 457.Wang L, Maddox C, Terio K, Lanka S, Fredrickson R, Novick B, Parry C, McClain A, Ross K. 2020. Detection and characterization of new coronavirus in bottlenose dolphin, United States, 2019. Emerg Infect Dis 26:1610–1612. 10.3201/eid2607.200093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Wang W, Lin XD, Guo WP, Zhou RH, Wang MR, Wang CQ, Ge S, Mei SH, Li MH, Shi M, Holmes EC, Zhang YZ. 2015. Discovery, diversity and evolution of novel coronaviruses sampled from rodents in China. Virology 474:19–27. 10.1016/j.virol.2014.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Wang W, Lin XD, Zhang HL, Wang MR, Guan XQ, Holmes EC, Zhang YZ. 2020. Extensive genetic diversity and host range of rodent-borne coronaviruses. Virus Evol 6:veaa078. 10.1093/ve/veaa078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Wang X, Li C, Guo D, Wang X, Wei S, Geng Y, Wang E, Wang Z, Zhao X, Su M, Liu Q, Zhang S, Feng L, Sun D. 2016. Co-circulation of canine coronavirus I and IIa/b with high prevalence and genetic diversity in Heilongjiang Province, Northeast China. PLoS One 11:e0146975. 10.1371/journal.pone.0146975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Wang X, Yan W, Lu Y, Chen T, Sun Y, Qin X, Zhang J, Han M, Guo W, Wang H, Wu D, Xi D, Luo X, Ning Q. 2012. CD4-CD8-T cells contribute to the persistence of viral hepatitis by striking a delicate balance in immune modulation. Cell Immunol 280:76–84. 10.1016/j.cellimm.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Wang Y, Tu X, Humphrey C, McClure H, Jiang X, Qin C, Glass RI, Jiang B. 2007. Detection of viral agents in fecal specimens of monkeys with diarrhea. J Med Primatol 36:101–107. 10.1111/j.1600-0684.2006.00167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Watsa M. 2020. Rigorous wildlife disease surveillance. Science 369:145–147. 10.1126/science.abc0017. [DOI] [PubMed] [Google Scholar]
- 464.Weingartl HM, Derbyshire JB. 1994. Evidence for a putative second receptor for porcine transmissible gastroenteritis virus on the villous enterocytes of newborn pigs. J Virol 68:7253–7259. 10.1128/jvi.68.11.7253-7259.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Weir EC, Jacoby RO, Paturzo FX, Johnson EA. 1990. Infection of SDAV-immune rats with SDAV and rat coronavirus. Lab Anim Sci 40:363–366. [PubMed] [Google Scholar]
- 466.Weir EC, Jacoby RO, Paturzo FX, Johnson EA, Ardito RB. 1990. Persistence of sialodacryoadenitis virus in athymic rats. Lab Anim Sci 40:138–143. [PubMed] [Google Scholar]
- 467.Weiss SR, Leibowitz JL. 2011. Coronavirus pathogenesis. Adv Virus Res 81:85–164. 10.1016/B978-0-12-385885-6.00009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Werdin RE, Sorensen DK, Stewart WC. 1976. Porcine encephalomyelitis caused by hemagglutinating encephalomyelitis virus. J Am Vet Med Assoc 168:240–246. [PubMed] [Google Scholar]
- 469.Wertheim JO, Chu DKW, Peiris JSM, Kosakovsky Pond SL, Poon LLM. 2013. A case for the ancient origin of coronaviruses. J Virol 87:7039–7045. 10.1128/JVI.03273-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Wesley RD, Lager KM. 2003. Increased litter survival rates, reduced clinical illness and better lactogenic immunity against TGEV in gilts that were primed as neonates with porcine respiratory coronavirus (PRCV). Vet Microbiol 95:175–186. 10.1016/S0378-1135(03)00150-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Whitehead CE, Anderson DE. 2006. Neonatal diarrhea in llamas and alpacas. Small Rumin Res 61:207–215. 10.1016/j.smallrumres.2005.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Whitworth KM, Rowland RRR, Petrovan V, Sheahan M, Cino-Ozuna AG, Fang Y, Hesse R, Mileham A, Samuel MS, Wells KD, Prather RS. 2019. Resistance to coronavirus infection in amino peptidase N-deficient pigs. Transgenic Res 28:21–32. 10.1007/s11248-018-0100-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Wilk AJ, Lee MJ, Wei B, Parks B, Pi R, Martínez-Colón GJ, Ranganath T, Zhao NQ, Taylor S, Becker W, Jimenez-Morales D, Blomkalns AL, O’Hara R, Ashley EA, Nadeau KC, Yang S, Holmes S, Rabinovitch M, Rogers AJ, Greenleaf WJ, Blish CA. 2021. Multi-omic profiling reveals widespread dysregulation of innate immunity and hematopoiesis in COVID-19. J Exp Med 218:e20210582. 10.1084/jem.20210582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Wille M, Holmes EC. 2020. Wild birds as reservoirs for diverse and abundant gamma- and deltacoronaviruses. FEMS Microbiol Rev 44:631–644. 10.1093/femsre/fuaa026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Williams BH, Kiupel M, West KH, Raymond JT, Grant CK, Glickman LT. 2000. Coronavirus-associated epizootic catarrhal enteritis in ferrets. J Am Vet Med Assoc 217:526–530. 10.2460/javma.2000.217.526. [DOI] [PubMed] [Google Scholar]
- 476.Williams RK, Jiang GS, Holmes KV. 1991. Receptor for mouse hepatitis virus is a member of the carcinoembryonic antigen family of glycoproteins. Proc Natl Acad Sci USA 88:5533–5536. 10.1073/pnas.88.13.5533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, Curtis HJ, Mehrkar A, Evans D, Inglesby P, Cockburn J, McDonald HI, MacKenna B, Tomlinson L, Douglas IJ, Rentsch CT, Mathur R, Wong AYS, Grieve R, Harrison D, Forbes H, Schultze A, Croker R, Parry J, Hester F, Harper S, Perera R, Evans SJW, Smeeth L, Goldacre B. 2020. Factors associated with COVID-19-related death using OpenSAFELY. Nature 584:430–436. 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 478.Winter C, Herrler G, Neumann U. 2008. Infection of the tracheal epithelium by infectious bronchitis virus is sialic acid dependent. Microbes Infect 10:367–373. 10.1016/j.micinf.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Wise AG, Kiupel M, Garner MM, Clark AK, Maes RK. 2010. Comparative sequence analysis of the distal one-third of the genomes of a systemic and an enteric ferret coronavirus. Virus Res 149:42–50. 10.1016/j.virusres.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Wise AG, Kiupel M, Maes RK. 2006. Molecular characterization of a novel coronavirus associated with epizootic catarrhal enteritis (ECE) in ferrets. Virology 349:164–174. 10.1016/j.virol.2006.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 481.Wojcinski ZW, Percy DH. 1986. Sialodacryoadenitis virus-associated lesions in the lower respiratory tract of rats. Vet Pathol 23:278–286. 10.1177/030098588602300308. [DOI] [PubMed] [Google Scholar]
- 482.Wong CK, Lam CW, Wu AK, Ip WK, Lee NL, Chan IH, Lit LC, Hui DS, Chan MH, Chung SS, Sung JJ. 2004. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol 136:95–103. 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Woo PC, Lau SK, Chu CM, Chan KH, Tsoi HW, Huang Y, Wong BH, Poon RW, Cai JJ, Luk WK, Poon LL, Wong SS, Guan Y, Peiris JS, Yuen KY. 2005. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J Virol 79:884–895. 10.1128/JVI.79.2.884-895.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Woo PC, Lau SK, Huang Y, Tsoi HW, Chan KH, Yuen KY. 2005. Phylogenetic and recombination analysis of coronavirus HKU1, a novel coronavirus from patients with pneumonia. Arch Virol 150:2299–2311. 10.1007/s00705-005-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485.Woo PC, Lau SK, Lam CS, Tsang AK, Hui SW, Fan RY, Martelli P, Yuen KY. 2014. Discovery of a novel bottlenose dolphin coronavirus reveals a distinct species of marine mammal coronavirus in Gammacoronavirus. J Virol 88:1318–1331. 10.1128/JVI.02351-13. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 486.Woo PC, Lau SK, Li KS, Tsang AK, Yuen KY. 2012. Genetic relatedness of the novel human group C betacoronavirus to Tylonycteris bat coronavirus HKU4 and Pipistrellus bat coronavirus HKU5. Emerg Microbes Infect 1:e35. 10.1038/emi.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 487.Woo PCY, Lau SKP, Lam CSF, Lau CCY, Tsang AKL, Lau JHN, Bai R, Teng JLL, Tsang CCC, Wang M, Zheng B-J, Chan K-H, Yuen K-Y. 2012. Discovery of seven novel mammalian and avian coronaviruses in the genus deltacoronavirus supports bat coronaviruses as the gene source of alphacoronavirus and betacoronavirus and avian coronaviruses as the gene source of gammacoronavirus and deltacoronavirus. J Virol 86:3995–4008. 10.1128/JVI.06540-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 488.Wood EN. 1977. An apparently new syndrome of porcine epidemic diarrhoea. Vet Rec 100:243–244. 10.1136/vr.100.12.243. [DOI] [PubMed] [Google Scholar]
- 489.Woods RD. 1997. Development of PCR-based techniques to identify porcine transmissible gastroenteritis coronavirus isolates. Can J Vet Res 61:167–172. [PMC free article] [PubMed] [Google Scholar]
- 490.World Health Organization. [Internet]. 2022. Middle East respiratory syndrome coronavirus (MERS-CoV). [Cited 28 March 2022]. Available at: https://www.who.int/health-topics/middle-east-respiratory-syndrome-coronavirus-mers#tab=tab_1.
- 491.World Health Organization. [Internet]. 2021. COVID-19 vaccine tracker and landscape. [Cited 25 September 2021]. Available at: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 492.Xia L, Yang Y, Wang J, Jing Y, Yang Q. 2018. Impact of TGEV infection on the pig small intestine. Virol J 15:102. 10.1186/s12985-018-1012-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Xu Y. 2020. Genetic diversity and potential recombination between ferret coronaviruses from European and American lineages. J Infect 80:350–371. 10.1016/j.jinf.2020.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494.Xydakis MS, Albers MW, Holbrook EH, Lyon DM, Shih RY, Frasnelli JA, Pagenstecher A, Kupke A, Enquist LW, Perlman S. 2021. Post-viral effects of COVID-19 in the olfactory system and their implications. Lancet Neurol 20:753–761. 10.1016/S1474-4422(21)00182-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495.Yeager CL, Ashmun RA, Williams RK, Cardellichio CB, Shapiro LH, Look AT, Holmes KV. 1992. Human aminopeptidase N is a receptor for human coronavirus 229E. Nature 357:420–422. 10.1038/357420a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Yen YT, Liao F, Hsiao CH, Kao CL, Chen YC, Wu-Hsieh BA. 2006. Modeling the early events of severe acute respiratory syndrome coronavirus infection in vitro. J Virol 80:2684–2693. 10.1128/JVI.80.6.2684-2693.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Yin L, Chen J, Li L, Guo S, Xue M, Zhang J, Liu X, Feng L, Liu P. 2020. Aminopeptidase N expression, not interferon responses, determines the intestinal segmental tropism of porcine deltacoronavirus. J Virol 94:e00480-20. 10.1128/JVI.00480-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 498.Yoo D, Pei Y, Christie N, Cooper M. 2000. Primary structure of the sialodacryoadenitis virus genome: sequence of the structural-protein region and its application for differential diagnosis. Clin Diagn Lab Immunol 7:568–573. 10.1128/CDLI.7.4.568-573.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 499.Yu J, Sreenivasan C, Uprety T, Gao R, Huang C, Lee EJ, Lawson S, Nelson J, Christopher-Hennings J, Kaushik RS, Nelson E, Diel DG, Hause BM, Li F, Wang D. 2021. Piglet immunization with a spike subunit vaccine enhances disease by porcine epidemic diarrhea virus. NPJ Vaccines 6:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 500.Yuan S, Balaji S, Lomakin IB, Xiong Y. 2021. Coronavirus Nsp1: Immune response suppression and protein expression inhibition. Front Microbiol 12:752214. 10.3389/fmicb.2021.752214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 501.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. 2012. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med 367:1814–1820. 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 502.Zarnke RL, Evermann J, Hoef JMV, McNay ME, Boertje RD, Gardner CL, Adams LG, Dale BW, Burch J. 2001. Serologic survey for canine coronavirus in wolves from Alaska. J Wildl Dis 37:740–745. 10.7589/0090-3558-37.4.740. [DOI] [PubMed] [Google Scholar]
- 503.Zeng Q, Langereis MA, van Vliet AL, Huizinga EG, de Groot RJ. 2008. Structure of coronavirus hemagglutinin-esterase offers insight into corona and influenza virus evolution. Proc Natl Acad Sci USA 105:9065–9069. 10.1073/pnas.0800502105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 504.Zhang J. 2016. Porcine deltacoronavirus: Overview of infection dynamics, diagnostic methods, prevalence and genetic evolution. Virus Res 226:71–84. 10.1016/j.virusres.2016.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 505.Zhang J, Guy JS, Snijder EJ, Denniston DA, Timoney PJ, Balasuriya UB. 2007. Genomic characterization of equine coronavirus. Virology 369:92–104. 10.1016/j.virol.2007.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Zhang XM, Kousoulas KG, Storz J. 1992. The hemagglutinin/esterase gene of human coronavirus strain OC43: phylogenetic relationships to bovine and murine coronaviruses and influenza C virus. Virology 186:318–323. 10.1016/0042-6822(92)90089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 507.Zhao Z, Zhang F, Xu M, Huang K, Zhong W, Cai W, Yin Z, Huang S, Deng Z, Wei M, Xiong J, Hawkey PM. 2003. Description and clinical treatment of an early outbreak of severe acute respiratory syndrome (SARS) in Guangzhou, PR China. J Med Microbiol 52:715–720. 10.1099/jmm.0.05320-0. [DOI] [PubMed] [Google Scholar]
- 508.Zhou H, Chen Y, Zhang S, Niu P, Qin K, Jia W, Huang B, Zhang S, Lan J, Zhang L, Tan W, Wang X. 2019. Structural definition of a neutralization epitope on the N-terminal domain of MERS-CoV spike glycoprotein. Nat Commun 10:3068. 10.1038/s41467-019-10897-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 509.Zhou P, Fan H, Lan T, Yang X-L, Shi W-F, Zhang W, Zhu Y, Zhang Y-W, Xie Q-M, Mani S, Zheng X-S, Li B, Li J-M, Guo H, Pei G-Q, An X-P, Chen J-W, Zhou L, Mai K-J, Wu Z-X, Li D, Anderson DE, Zhang L-B, Li S-Y, Mi Z-Q, He T-T, Cong F, Guo P-J, Huang R, Luo Y, Liu X-L, Chen J, Huang Y, Sun Q, Zhang X-L-L, Wang Y-Y, Xing S-Z, Chen Y-S, Sun Y, Li J, Daszak P, Wang L-F, Shi Z-L, Tong Y-G, Ma J-Y. 2018. Fatal swine acute diarrhoea syndrome caused by an HKU2-related coronavirus of bat origin. Nature 556:255–258. 10.1038/s41586-018-0010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W, Si H-R, Zhu Y, Li B, Huang C-L, Chen H-D, Chen J, Luo Y, Guo H, Jiang R-D, Liu M-Q, Chen Y, Shen X-R, Wang X, Zheng X-S, Zhao K, Chen Q-J, Deng F, Liu L-L, Yan B, Zhan F-X, Wang Y-Y, Xiao G-F, Shi Z-L. 2020. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270–273. 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Zhou R, To KK, Wong YC, Liu L, Zhou B, Li X, Huang H, Mo Y, Luk TY, Lau TT, Yeung P, Chan WM, Wu AK, Lung KC, Tsang OT, Leung WS, Hung IF, Yuen KY, Chen Z. 2020. Acute SARS-CoV-2 infection impairs dendritic cell and T cell responses. Immunity 53:864–877. 10.1016/j.immuni.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Ziebuhr J, Snijder EJ, Gorbalenya AE. 2000. Virus-encoded proteinases and proteolytic processing in the Nidovirales. J Gen Virol 81:853–879. 10.1099/0022-1317-81-4-853. [DOI] [PubMed] [Google Scholar]