Abstract
Background:
Guideline based hypertension management is integral to the prevention of stroke. We examine trends in antihypertensive medications prescribed after stroke and assess how well a prescribers’ blood pressure medication choice adheres to clinical practice guidelines (Prescribers’-Choice Adherence).
Methods:
The Florida Stroke registry (FSR) utilizes statewide data prospectively collected for all acute stroke admissions. Based on established guidelines we defined optimal Prescribers’-Choice Adherence using the following hierarchy of rules: 1) use of an angiotensin inhibitor (ACEI) or angiotensin receptor blocker (ARB) as first-line antihypertensive among diabetics; 2) use of thiazide-type diuretics or calcium channel blockers (CCB) among African-American patients; 3) use of beta-adrenergic blockers (BB) among patients with compelling cardiac indication (CCI) 4) use of thiazide, ACEI/ARB or CCB class as first-line in all others; 5) BB should be avoided as first line unless CCI.
RESULTS:
A total of 372,254 cases from January 2010 to March 2020 are in FSR with a diagnosis of acute ischemic, hemorrhagic stroke, transient ischemic attack or subarachnoid hemorrhage; 265,409 with complete data were included in the final analysis. Mean age 70 +/−14 years, 50% female, index stroke subtype of 74% acute ischemic stroke and 11% intracerebral hemorrhage. Prescribers’-Choice Adherence to each specific rule ranged from 48-74% which is below quality standards of 85%. There were race-ethnic disparities with only 49% Prescribers choice Adherence for African Americans patients.
Conclusion:
This large dataset demonstrates consistently low rates of Prescribers’-Choice Adherence over 10 years. There is an opportunity for quality improvement in hypertensive management after stroke.
Keywords: Hypertension, stroke, beta blockers, race, ethnicity, disparities, blood pressure, Florida, Stroke registry
Introduction:
Hypertension (HTN) is the single most important modifiable stroke risk factor accounting for 36% of the population attributable stroke risk 1. It is an independent and major driver of both primary and secondary stroke recurrence in the population, with known race-ethnic differences in its rate of control and medication compliance2–4. Adequate control of blood pressure (BP) reduces the risk of stroke by 30% 5-7.Several clinical trials3, 4, 8-10 have revealed – and subsequent guidelines11-15 have recommended – specific medications based on compelling indications that not only optimizes BP control but also prioritizes mortality and morbidity benefits of specific agents. In the Post Stroke Setting, the recommended first-line antihypertensives are thiazide diuretics, angiotensin-converting enzyme inhibitors (ACEIs), or angiotensin receptor blockers (ARBs), and with more targeted therapy made in consideration of a patient’s medical comorbidities or race and/or ethnicity13, 16-19. Beta Blockers are no longer considered first line therapy in the post stroke setting except in the case of a compelling cardiac indication (CCI)13, 16, 20.
The choice of antihypertensive medications based on the compelling indications for vascular comorbidities has been supported by clinical practice guidelines since the 6th Joint National Commission on hypertension and affirmed by recent clinical practice guidelines. Currently there are no post stroke quality measures that facilitate implementation of Prescribers’-Choice Adherence for secondary prevention of stroke. We examine the contemporary trends in choice of antihypertension medications post stroke and introduce a novel concept of Prescribers’-Choice Adherence to clinical practice guidelines. We hypothesized that if guideline recommendations are fully implemented then Prescribers’-Choice Adherence would be >80% for each compelling indication. Further we examined the impact of social determinants of health on Prescribers’-Choice Adherence Rules and race-ethnic variabilities.
Methods:
Setting:
All patients admitted with a stroke diagnosis to a Florida Stroke Registry (FSR) participating January 2010 through to April 2020 were included for this study. FSR is a statewide data repository which collects data from 168 voluntarily participating stroke hospital that utilize the American Heart Association “Get with the Guidelines- Stroke (GWTG-S)” database. The FSR has previously demonstrated racial ethnic and sex disparities in acute stroke care 21, 22 and details of the FSR are previously described21, 23. In brief, each FSR hospital has specialized abstractors who submit data on all stroke cases to the GWTG-S form. Included in the standard GWTG-S data collection system the FSR also reports several questions regarding self-reported race ethnicity such as African Americans, Caucasian Americans (non-Hispanic white, NHW), and Hispanic. The “Blood Pressure (BP) Medication use Questionnaire” allows collection of information regarding the number and class of antihypertensive medications prescribed. It includes specific fields to identify if no antihypertensives were prescribed or whether these medications were contraindicated.
Population:
Patients admitted to a participating FSR hospital and a discharge diagnosis of acute ischemic stroke, acute intracerebral hemorrhage (ICH), transient ischemic attack (TIA), or subarachnoid hemorrhage (SAH) and with complete “Blood Pressure (BP) Medication use Questionnaire” between January 2010 and March 2020 were included in this analysis. For the decade analyzed, 121 hospitals with 372,254 stroke admissions were voluntarily participating in the FSR. Inclusion criteria: final diagnosis of acute stroke of either subtype, available race ethnicity data, completed BP medications list. Patients with incomplete records or records containing conflicting information regarding antihypertensive medications prescribed were excluded (n=106, 845) from the final analysis. Examples of conflicting information included the simultaneous selection of both “none” OR “medications contraindicated” AND “a specific antihypertensive medication” for the same patient in the same form. Please see the Consort diagram and the major resources table in supplemental materials.
Definition of Prescribers’-Choice Adherence:
In 1997, the Sixth Report of the Joint National Committee (JNC) on Prevention, Detection, Evaluation and Treatment of High Blood Pressure15 established recommendations for first-line therapy based on race-ethnicity and medical comorbidities. The term “a compelling medical indication” was first introduced in the JNC6 based on multiple randomized trials that demonstrated benefit of one or more class of drugs based on patients’ medical comorbidities. While stroke was not specifically listed as a compelling indication, the included meta-analysis demonstrated that high dose diuretics and ACEI were preferred for stroke prevention and while beta blockers were potentially harmful. The recommendations for stroke as a compelling indication was include in the JNC Seventh guideline and have been reaffirmed with subsequent iterations of the JNC (Eighth Reports)12-14, 16, 17, 19 and the 2020 International Society of Hypertension Global Hypertension Practice Guidelines13 with the recommendation for BP medication choice (Prescribers’-Choice Adherence) after stroke specifically incorporated. Based on this body of knowledge, we designed 5 simple hierarchical rules that can be used to determine Prescribers’-Choice Adherence:
use of an angiotensin inhibitor (ACEI) or angiotensin receptor blocker (ARB) as first-line in diabetics irrespective of race15.
use of thiazide-type diuretics or calcium channel blockers (CCB) among African-American patients (AA), as they had a superior response to treatment 24 and morbidity and mortality benefits 15.
use of Beta-adrenergic blockers (BB) among patients with coronary artery disease, myocardial infarction, atrial fibrillation or other compelling cardiac indication (CCI) irrespective of race ethnic origins15 as it conferred a mortality benefit
use of thiazide, ACEI/ARB or CCB class for all others not included in rules 1-3 above 15,
BB should be avoided as first line unless CCI.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting checklist. We collected baseline demographic information, insurance status, past medical history and other variables of interest including: final clinical diagnosis related to stroke; stroke etiology for acute ischemic stroke based on the Trial of ORG10172 in Acute Stroke Treatment (TOAST) classification25; medication list prior to stroke admission; antihypertensive medications at discharge; discharge disposition; and modified Rankin score(mRS) at discharge;
Statistical Analysis
Summary statistics were provided for each variable. Chi-squared and Kruskal-Wallis tests were used to determine differences in demographic and stroke characteristics. Univariate statistics were summarized using N and percentages for categorical variables; means and standard deviations were used for continuous variables. Statistical significance was accepted for p values less than 0.001 and with a > 2% difference between groups. Those variables with positive associations were included in a multivariate model to determine independent associations. We conducted multi-level logistic regression with generalized estimating equations to determine whether independent associations. Odds ratios and 95% confidence intervals were calculated to determine differences in Prescribers’-Choice Adherence vs Non-Prescribers’ Choice Adherence.
Most variables had fewer than 5% missing values. Those cases with missing data were not different from the overall cohort. All statistical analyses were performed with SAS version 9.4 (Copyright © 2021 by SAS Institute Inc., Cary, NC, USA). The statistical team and first author had full access to all the data and take responsibility for the data integrity and data analysis.
Data availability
As FSR utilizes data from American Heart Association (AHA) Get With The Guidelines-Stroke (GWTG-S), data-sharing agreements require an application process for other researchers to access data. Researchers can submit proposals at www.heart.org/qualityresearch to be considered by the GWTG-S and TCSD-S steering committees.
Analytic requests of the data are subject to approval by the FSR publication committee and aggregate, blinded data may be shared by the corresponding author upon written request from any qualified investigator.
Results:
There were 265,409 cases included in the final analysis, mean age 70.6 +/−14.7 years, 50.3% female NHW 68.6%, AA 17.6%, Hispanic 13.8%. The index stroke subtype consisted of 74% acute ischemic stroke, 11% intracerebral hemorrhage and 4% subarachnoid hemorrhage. Antihypertensive medications at discharge were prescribed in 70% of cases; 19% had a contraindicated and 10% were prescribed lifestyle modifications.
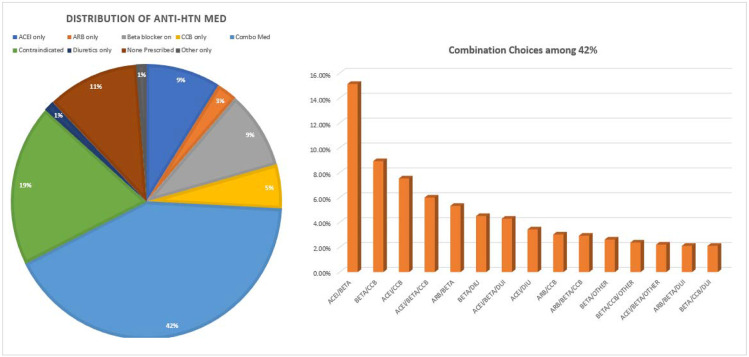
Figure 1 outlines contemporary antihypertensive medications prescribed in our cohort with 42% receiving combination therapy, with 39% of patients receiving one or another monotherapy. The most prescribed antihypertensive medication in the poststroke setting was beta blocker 38% either alone or in combination (also in Figure 1). Guideline preferred Prescribers’-Choice Adherence combination post stroke – ACEI and diuretics-was only used in 3% of cases. Diuretic monotherapy was prescribed in 1% of cases.
Figure 1. Discharge hypertensive medications among the FSR patients.
FSR: Florida Stroke Registry; ACEI: angiotensin converting enzyme inhibitor class of medications.
ARB: angiotensin receptor blocker medications; BB: beta adrenergic receptor blockers; CCB: calcium channel blockers; Other*: all other classes of Anti-HTN Medication such as vasodilators; Combination therapy: more than one class of anti-HTN medications.
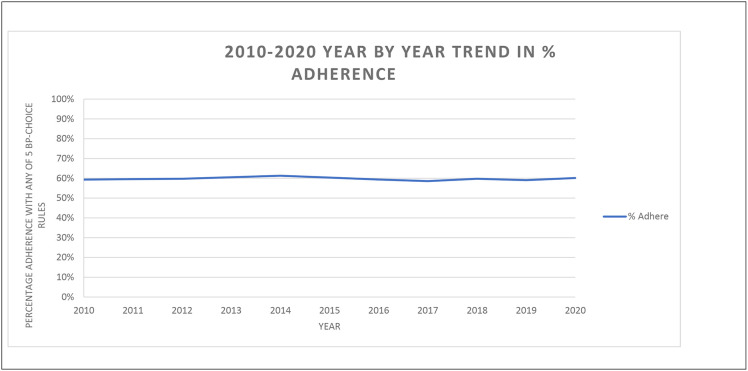
Table 1 summarizes the study population demographics, and characteristics based on Prescribers’-Choice Adherence vs. Non-Prescribers’-Choice Adherence Overall adherence to each specific post stroke Prescribers’-Choice Adherence rule was low ranging from 48 to 74% with an overall adherence to any of the five Prescribers’-Choice Adherence rules being only 60%. Table 2 Describes each Prescribers’-Choice Adherence Rule, its supporting evidence, and the results of this cohort relative to the benchmark threshold of 80% adherence. We selected a threshold of 80% as a more lenient goal than the GWTG recommended 85% for quality indicators. his trend did not vary by year from 2010-2020 (see figure 2) and continues to be consistently low over the past decade.
Table 1:
Study Population Demographics with characteristics Non-Prescriber’s-Choice Adherent vs Prescriber’s-Choice Adherence Cohorts
| Variables | Overall n= 265,409 |
Non-Prescribers’-Choice Adherent n=106,899 |
Prescribers’- Choice Adherent n=158,510 |
|
|---|---|---|---|---|
| Age, Mean (std), y | 70.6 (14.7) | 70.7 (15.3) | 70.6 (14.3) | |
| Sex, female | 50.3% | 50.0% | 50.4% | |
| Race/Ethnicity | ||||
| White | 68.6% | 66.3% | 70.1% | |
| African American (AA) | 17.6% | 20.7% | 15.5% | |
| Hispanic | 13.8% | 13.0% | 14.36% | |
| Stroke Type: | Acute Ischemic Stroke | 73.7% | 73.6% | 73.8% |
| Transient Ischemic Attack | 10.9% | 10.8% | 11% | |
| Subarachnoid Hemorrhage | 3.9% | 3.9% | 3.9% | |
| Intracerebral hemorrhage | 11.3% | 11.6% | 11.1% | |
| Acute Ischemic Stroke Etiology (TOAST Criteria) | ||||
| Cardio embolism | 7.5% | 8.2% | 7.0% | |
| Cryptogenic | 8.8% | 8.8% | 8.8% | |
| Large Vessel Atherosclerosis | 5.7% | 5.9% | 6.9% | |
| Small vessel occlusion | 6.4% | 5.6% | 6.9% | |
| Stroke of Other determined | 1.0% | 1.1% | 1% | |
| Unknown | 70.5% | 70.4% | 70.6% | |
| Insurance, % | ||||
| Private | 38.2% | 37.5% | 38.6% | |
| Medicare | 44.2% | 45% | 43.5% | |
| Medicaid | 5.0% | 5.1% | 5.0% | |
| Self-pay | 10.4% | 10.0% | 10.9% | |
| Diabetes | 31.8% | 37.6% | 27.8% | |
| Atrial Fibrillation/Flutter | 18.3% | 23.5% | 14.9% | |
| Prior Stroke or TIA | 29.4% | 30.1% | 28.9% | |
| Discharged Home | 48.4% | 44.2% | 51.3% | |
| Modified Rankin Scale at discharge | ||||
| mRS 0-2 | 43.4% | 39.7% | 45.8% | |
| mRS 3-5 | 51.3% | 50.9% | 51.5% | |
| mRS 6 | 5.4% | 9.3% | 2.7% | |
Table 2:
Evidence for Prescribers-Choice Adherence rules and percentage adherence to each rule.
| Prescribers-Choice Adherence Rules* |
LOE | HTN Guideline |
2006 Secondary Stroke Prevention Guideline |
2011 Secondary Stroke Prevention Guideline |
2014 Secondary Stroke Prevention Guideline |
Threshold | % Prescribers- Choice Adherence |
|---|---|---|---|---|---|---|---|
| Use ACEi or ARB in Diabetes | A | JNC 6 1997 - present | ✔ | ✔ | ✔ | 80% | 53.4% |
| AA use of diuretic or CCB | A | JNC 7 2003-Present | Silent Endorses JNC7 | Silent Endorses 2011 Primary Stroke | Silent Endorses 2011 Primary Stroke | 80% | 48.5% |
| Use of diuretic, ACEi/ARB or CCB | A | JNC 7 2003-Present | ✔ | ✔ | ✔ | 80% | 74.4% |
| BB in compelling Cardiac Indication | A | JNC 6 1997 - present | Silent Endorses JNC7 | ✔ | ✔ | 80% | 52% |
| % Failed to avoid BB without Compelling | A | JNC 6 1997 - present | Silent Endorses JNC7 | Silent Endorses 2011 Primary Stroke | Silent Endorses 2011 Primary Stroke | <5% | 20% |
| Any 1 of 5 Rules Combined | A | ✔ | ✔ | ✔ | ✔ | 80% | 59.7% |
| GP-Koch Rules |
This is different from compliance as it focused on the preserver’s choice of antihypertensive agents rather than patient’s ability to consistently take the medication; BP-Choice Adherence: Blood Pressure medication Choice Adherence to Clinical Practice Guidelines as derived from the Sixth Joint National Commission on Hypertension and the ISH 2020 HTN Guidelines; JNC: Joint National Commission on Hypertension; AA: African Americans; ACEi: Angiotensin Enzyme Inhibitors; ARB: Angiotensin Receptor Blockers; BB: Beta Blockers; CCB: Calcium Channel Blockers.
Figure 2: Trends in adherence to any of the 5 Prescribers’-Choice Adherence rules over the course of 10 years.
Non-Prescribers’-Choice Adherence was most prevalent among the following demographics: African American race (20.7% vs. 15.5% p <0.001). diabetes (37.5% vs 27.8% p <0.001), atrial fibrillation (23.5% vs14.9% p <0.001) and prior stroke or TIA 51.3% vs 44.2% p <0.001). Hispanics in the FSR were more likely to have Prescribers-Choice Adherent (13% vs 14% p < 0.001). One in 5 patients were prescribed a beta blocker without a CCI and were considered non-Prescribers’-Choice Adherence. ACE-I/ARBs were not used as first line in 46.6% of diabetics, 47% of cases with a compelling cardiac indication were not prescribed a b-blocker. Among African American cases, 51.5% were not prescribed diuretic or calcium channel blocker as first line therapy.
Ischemic stroke subtypes were not associated with an increased likelihood of Prescribers’-Choice Adherence. When these associations were further assessed in a predictive model that controlled for age, gender, race, insurance, diabetes, and atrial fibrillation, Hispanic had higher odds of being Prescribers’-Choice Adherence, (OR 1.05, 95%CI 1.02, 1.09 p< 0.002), while lower odds of being Prescribers’-Choice adherent was noted for those with atrial fibrillation (OR 0.53 95%CI 0.54, 0.56 p< 0.001) and diabetes mellitus (OR 0.65, 95%CI 0.61, 0.68 p< 0.001).
Discussion:
A prescriber’s ability to choose medications as recommended by anti-hypertensive guidelines is influenced by multiple factors. Our study highlights real-world challenges to adhering to Prescribers’-Choice Adherence rules after stroke. Prescribers’-Choice Adherence remained low (48-70%) over the course of a decade despite level A evidence, strong recommendations from multiple clinical practice guidelines and several years to facilitate adoption. The rates have been consistently low since 2010, suggesting that current prescribing practices are likely to continue unchanged unless specific antihypertensive prescribing quality measures are implemented.
Principal Findings:
This study goes beyond the question of whether antihypertensive medications are prescribed and specifically explores if the prescribed medications provide evidence-based benefits based on each patient’s medical comorbidities, with an algorithm of preferred agents based on medical comorbidities and evidence-based recommendations crafted from mortality and morbidity benefits. By describing, testing, and standardizing these simple rules, other large datasets or quality indicators can follow this paradigm to evaluate on a more granular level this important question of Prescribers’-Choice Adherence. There has been debate about whether the choice of antihypertensive medications matters, but rather only that the blood pressure goal is achieved. There is now new data from the SPRINT trial26 demonstrating that drug class influences outcomes post stroke with protective effects seen with thiazide type diuretics and angiotensin receptor blockers but a potential for harm with Beta blockers in this setting.
We demonstrate that applying these Prescribers’-Choice Adherence Rules is feasible and could be used as new quality measures to improve compliance with post stroke guideline recommendations, for secondary stroke prevention. The use of quality measures to improve clinical practice is well accepted, and their benefits demonstrated by several programs such as the national American Heart Association GWTG-S quality improvement program which showed improved adherence to during hospitalization and after discharge27-30. These quality measures are now accepted as the standard of care by certifying organizations such as The Joint Commission and payers such as the Centers for Medicare and Medicaid. Among the various post stroke quality indicators in practice, the threshold for successful adherence is typically 85% compliance or higher. In our study Prescribers’-Choice Adherence was assessed at a more lenient target of 80% adherence but our findings noted even lower adherence.
Common post stroke quality metrics related to medication use for secondary stroke prevention which are tracked by stroke centers and reported to certifying organizations include: the use of antithrombotic prior to discharge, use of anticoagulation for atrial fibrillation, and statin therapy at discharge. However, there are no post stroke quality measures for blood pressure management, even though 70% of post stroke patients are hypertensive. While most patients are prescribed an antihypertensive medication, including 70% of patients in our cohort, full adherence to guidelines-recommended treatment as defined by the Prescribers’-Choice Adherence is suboptimal. Deciding when to start antihypertensive medications and tailoring the choice of antihypertensive medication during hospitalization is often difficult. In addition, there may be insufficient time during acute hospitalization to modify a regimen that may have been appropriate in the acute setting or during intensive care.
There is significant of evidence for hypertension management in stroke, McGurgan etal31 provides a critical review of the plethora of evidence and highlight the challenges of adherence to guidelines. Our study offers innovative guideline-based rules as an easy tool for clinicians to consider when prescribing post stroke antihypertensive medications. The proposed Prescribers’-Choice Adherence Rules are presented in a hierarchical algorithm, prioritizing the patient’s medical comorbidities, making it easy for clinicians to follow and potentially makes this clinical variability in the choice of medications easier to codify for quality measures.
Disparities
We found that African Americans had a lower odd of having the Prescribers’-Choice Adherence to guidelines-based BP medications after stroke with 1 in 2 patients not prescribed guideline based first choice agents. This is consistent with prior work17, 23, 24, 32-35 on race ethnic disparities in hypertension and stroke management such as the REGARDS32 study. This disparity persisted even after controlling for insurance type, age, and other medical comorbidities and not related to patient compliance to medication but rather a prescriber’s choice of antihypertensive medication after a stroke. The reason for this is likely multifactorial and can’t be gleaned from this study. The data regarding optimal choice of antihypertensive medication among AA patients 13, 32, 35, 36 and specifically diuretics as first-line in AA patients is not readily accepted37. Some clinicians cite the low rates (4-13%) of AA patient enrollment in clinical trials. Additionally, there may be some distrust of the antihypertensive guidelines as it relates to race and/or the debate surrounding the JNC 8 guidelines16, 19. Whether or not this contributes to this disparity in Prescribers’-Choice Adherence cannot be assessed in this observational study but highlights an area for future research. For example, should the social construct of race really influence the choice of antihypertensive medication? Should the antihypertensive guidelines be updated to address this area?
It is noteworthy that beta blockers were the most prescribed antihypertensive medications, despite evidence of potential for harm without the strong benefit of secondary stroke prevention18, 30, 38. The reason for this preference in using beta blockers post stroke cannot be gleaned from this observational analysis. Additionally, the guideline-preferred combination of anti-hypertensive medications ACE inhibitors and diuretics are used very infrequently. By using the Prescribers’-Choice Adherence Rules as quality measures, tracking, and assessing these measures prospectively, we may better delineate the cause of this variability with Prescribers’-Choice Adherence and presents an opportunity for future research or quality interventions.
Strengthens and Limitations
An important strength of this analysis is the large cohort sample size with less than 5% missingness. Those cases with incomplete data were not demographically different from the final cohort. The data could be generalizable outside of Florida due to large sample from many institutions and large geographical area with a diverse cohort of patients which can policymakers and stroke centers. Our study has a diverse cohort with 17% of cases African American, 19% Hispanic which is powerful for assessing disparities in race ethnic associations. The longevity of the FSR provides an unparalleled view of post stroke anti-hypertensive prescribing practices over the course of 10 years.
One possible explanation for our findings is that prescribers may choose not to start blood pressure medications during the acute admission because of risk of hypotension and worsening infarct in the acute setting primarily among patients with intracranial stenosis. However, this is unlikely to be a primary driver of prescribing practices; as there’s no difference in blood pressure guidelines adherence among patients with transient ischemic attack or based on acute ischemic stroke etiology subtype. Another possible explanation is that hospitalizations after stroke may have a short length of stay so home medications, medications from the emergency department or intensive care unit are continued until discharge.
A limitation of our deidentified and aggregated, hospital-based dataset is that we are unable to discern readmission rates, long term BP control, recent changes in baseline home medications, duration of treatment, recurrent stroke or long-term outcomes for these cases. Moreover, we could not assess whether medication use was influenced by in-hospital events or medication adverse effects e.g. a myocardial infarct during hospitalization would lead to the use of a BB; renal injury with an ACEI would lead to discontinuation of that medication prior to discharge. However, in this is a large cohort these potential confounding cases are likely to be the exception rather than the norm.
Perspectives:
In this large, hospital-based Florida Stroke Registry we have demonstrated race ethnic disparities in Prescribers’-Choice Adherence to antihypertensive guidelines-based treatments in real world acute stroke cases. There is suboptimal adherence to hypertension management guidelines with at least 30– 40% of cases not guideline adherent. This represents a quality improvement opportunity for future research into limitations of guideline implementation, future quality improvement projects and educational interventions to address this public health disparity and can inform local policy implementation. Future studies will assess the impact of Prescribers’-Choice Adherence of Stroke outcomes such as 30-day or 90-day Stroke readmission and stroke recurrence and create interventions to improve evidence-based antihypertensive management. Future studies should also assess the impact of the Sars-COV 2 pandemic on Prescribers’-Choice Adherence with a focus on race ethnic disparities.
Novelty and Relevance:
What is new:
We define 5 Post Stroke Prescribers’-Choice Adherence Rules and determine prescribers’ choice of evidence-based and guideline recommended antihypertensive management after stroke.
What is relevant:
Prescribers’-Choice Adherence remains low (48-70%) with no significant improvement over the course of a decade.
50% of African Americans do not receive Prescribers’-Choice Adherence first line medication options
One in 5 persons receive may have received a BB without a compelling cardiac indication
Clinical Implications:
The proposed Prescribers’-Choice Adherence Rules are presented in a hierarchical algorithm, prioritizing the patient’s medical comorbidities, making it easy for clinicians to follow and potentially makes this clinical variability in the choice of medications easier to codify for quality measures.
Acknowledgements:
We would like to acknowledge the leadership and support of the Florida Stroke Registry (FSR), particularly the FSR’s executive and publication committees as well as each of the participating FSR hospitals and their staff.
Study Funded by the National Institute of Health (NIH)/National Institute of Neurological Disorders (NINDS) through the Stroke Prevention and Intervention Research Program (SPIRP) cooperative grant (Grant Number: U54NS081763) and the Florida Department of Health. Sources of Funding: Funding: This study is funded by the state of Florida DOH; NIMHD: R01MD012467
Non-Standard Abbreviations and Acronyms:
- BP
Blood Pressure
- FSR
Florida Stroke Registry
- HTN
Hypertension
- JNC
Joint National Committee
- CCI
compelling cardiac indication
Prescribers-Choice Adherence:
non-Prescribers’-Choice Adherence
Footnotes
Financial Disclosures
Dr. Sacco - recipient and the primary investigator of the SPIRP cooperative grant from the NIH/NINDs (Grant Number: U54NS081763) and the recipient of the FSR Grant (COHAN-A1 R2)
Dr. Rundek - recipient of the women’s supplement from the NIH, Office of Research on Women’s Health and receives salary support from the SPIRP cooperative grant from the NIH/NINDS (Grant Number: U54NS081763-01S1).
Dr. Romano - receives research salary support from the FSR COHAN-A1 R2 contract
Dr. Asdaghi-receives research salary support from the FSR COHAN-A1 R2 contract
Dr. Koch - receives research salary support from the FSR COHAN-A1 R2 contract
Dr. Alkhachroum is supported by an institutional KL2 Career Development Award from the Miami CTSI NCATS (Grant Number: UL1TR002736).
Statistical Analysis conducted by Hao Ying MSc, Bustillo, Antonio MSPH and Lili Zhou;
References
- 1.O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the interstroke study): A case-control study. Lancet. 2010;376:112–123 [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: A report from the american heart association. Circulation. 2019;139:e56–e528 [DOI] [PubMed] [Google Scholar]
- 3.Katsanos AH, Filippatou A, Manios E, Deftereos S, Parissis J, Frogoudaki A, et al. Blood pressure reduction and secondary stroke prevention: A systematic review and metaregression analysis of randomized clinical trials. Hypertension. 2017;69:171–179 [DOI] [PubMed] [Google Scholar]
- 4.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2224–2260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anti-hypertensive VACSGo, Agents. Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm hg. Jama. 1967;202:1028–1034 [PubMed] [Google Scholar]
- 6.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the systolic hypertension in the elderly program (shep). Shep cooperative research group. Jama. 1991;265:3255–3264 [PubMed] [Google Scholar]
- 7.Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: Principal results of the hypertension optimal treatment (hot) randomised trial. Hot study group. Lancet. 1998;351:1755–1762 [DOI] [PubMed] [Google Scholar]
- 8.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2020 update: A report from the american heart association. Circulation. 2020;141:e139–e596 [DOI] [PubMed] [Google Scholar]
- 9.Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The antihypertensive and lipid-lowering treatment to prevent heart attack trial (allhat). Jama. 2002;288:2981–2997 [DOI] [PubMed] [Google Scholar]
- 10.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: Ukpds 38. Uk prospective diabetes study group. Bmj. 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 11.Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, et al. Guidelines for the prevention of stroke in women: A statement for healthcare professionals from the american heart association/american stroke association. Stroke. 2014;45:1545–1588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. Jama. 2003;289:2560–2572 [DOI] [PubMed] [Google Scholar]
- 13.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–1357 [DOI] [PubMed] [Google Scholar]
- 14.Whitworth JA, Chalmers J. World health organisation-international society of hypertension (who/ish) hypertension guidelines. Clin Exp Hypertens. 2004;26:747–752 [DOI] [PubMed] [Google Scholar]
- 15.The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Archives of Internal Medicine. 1997;157:2413–2446 [DOI] [PubMed] [Google Scholar]
- 16.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (jnc 8). Jama. 2014;311:507–520 [DOI] [PubMed] [Google Scholar]
- 17.Flack JM, Sica DA, Bakris G, Brown AL, Ferdinand KC, Grimm RH Jr., et al. Management of high blood pressure in blacks: An update of the international society on hypertension in blacks consensus statement. Hypertension. 2010;56:780–800 [DOI] [PubMed] [Google Scholar]
- 18.Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. 2018;71:1269–1324 [DOI] [PubMed] [Google Scholar]
- 19.Wright JT Jr., Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm hg in patients aged 60 years or older: The minority view. Ann Intern Med. 2014;160:499–503 [DOI] [PubMed] [Google Scholar]
- 20.Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the anglo-scandinavian cardiac outcomes trial-blood pressure lowering arm (ascot-bpla): A multicentre randomised controlled trial. Lancet. 2005;366:895–906 [DOI] [PubMed] [Google Scholar]
- 21.Sacco RL, Gardener H, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM, et al. Racial-ethnic disparities in acute stroke care in the florida-puerto rico collaboration to reduce stroke disparities study. J Am Heart Assoc. 2017;6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Asdaghi N, Romano JG, Wang K, Ciliberti-Vargas MA, Koch S, Gardener H, et al. Sex disparities in ischemic stroke care: Fl-pr cresd study (florida-puerto rico collaboration to reduce stroke disparities). Stroke. 2016;47:2618–2626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gardener H, Leifheit EC, Lichtman JH, Wang K, Wang Y, Gutierrez CM, et al. Race-ethnic disparities in 30-day readmission after stroke among medicare beneficiaries in the florida stroke registry. J Stroke Cerebrovasc Dis. 2019;28:104399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beckie TM. Ethnic and racial disparities in hypertension management among women. Semin Perinatol. 2017;41:278–286 [DOI] [PubMed] [Google Scholar]
- 25.Adams HP Jr., Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. Toast. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24:35–41 [DOI] [PubMed] [Google Scholar]
- 26.DeCarolis DD, Gravely A, Olney CM, Ishani A. Impact of antihypertensive drug class on outcomes in the sprint. Hypertension. 2022:Hypertensionaha12118369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song S, Fonarow GC, Olson DM, Liang L, Schulte PJ, Hernandez AF, et al. Association of get with the guidelines-stroke program participation and clinical outcomes for medicare beneficiaries with ischemic stroke. Stroke. 2016;47:1294–1302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smaha LA. The american heart association get with the guidelines program. Am Heart J. 2004;148:S46–48 [DOI] [PubMed] [Google Scholar]
- 29.Ziaeian B, Xu H, Matsouaka RA, Xian Y, Khan Y, Schwamm LS, et al. Us surveillance of acute ischemic stroke patient characteristics, care quality, and outcomes for 2019. Stroke. 2022;53:3386–3393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Program. NHBPE. The sixth report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Bethesda (MD): National Heart, Lung, and Blood Institute; 1997. [Google Scholar]
- 31.McGurgan IJ, Kelly PJ, Turan TN, Rothwell PM. Long-term secondary prevention: Management of blood pressure after a transient ischemic attack or stroke. Stroke. 2022:Strokeaha121035851 [DOI] [PubMed] [Google Scholar]
- 32.Akinyelure OP, Jaeger BC, Moore TL, Hubbard D, Oparil S, Howard VJ, et al. Racial differences in blood pressure control following stroke: The regards study. Stroke. 2021:Strokeaha120033108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aggarwal R, Chiu N, Wadhera RK, Moran AE, Raber I, Shen C, et al. Racial/ethnic disparities in hypertension prevalence, awareness, treatment, and control in the united states, 2013 to 2018. Hypertension. 2021:Hypertensionaha12117570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carson AP, Howard G, Burke GL, Shea S, Levitan EB, Muntner P. Ethnic differences in hypertension incidence among middle-aged and older adults: The multi-ethnic study of atherosclerosis. Hypertension. 2011;57:1101–1107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferdinand KC, Yadav K, Nasser SA, Clayton-Jeter HD, Lewin J, Cryer DR, et al. Disparities in hypertension and cardiovascular disease in blacks: The critical role of medication adherence. J Clin Hypertens (Greenwich). 2017;19:1015–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koch S, Elkind MS, Testai FD, Brown WM, Martini S, Sheth KN, et al. Racial-ethnic disparities in acute blood pressure after intracerebral hemorrhage. Neurology. 2016;87:786–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shepherd S. Commentary: First do no harm. Let’s eradicate the inherent racism in medicine. Chicago Tribune. 2020 [Google Scholar]
- 38.Chan WV, Pearson TA, Bennett GC, Cushman WC, Gaziano TA, Gorman PN, et al. Acc/aha special report: Clinical practice guideline implementation strategies: A summary of systematic reviews by the nhlbi implementation science work group: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;69:1076–1092 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
As FSR utilizes data from American Heart Association (AHA) Get With The Guidelines-Stroke (GWTG-S), data-sharing agreements require an application process for other researchers to access data. Researchers can submit proposals at www.heart.org/qualityresearch to be considered by the GWTG-S and TCSD-S steering committees.
Analytic requests of the data are subject to approval by the FSR publication committee and aggregate, blinded data may be shared by the corresponding author upon written request from any qualified investigator.