Highlights
-
•
Crisis Intervention Team trainings offer opportunities to address stigma
-
•
Knowledge of communication strategies was found to be correlated with lower levels of substance use stigma
-
•
Increased self-efficacy post-training was associated with lower levels of mental illness and substance use stigma
-
•
Awareness of community resources was related to decreased mental illness and substance use stigma after training
-
•
Additional training content on bias and substance use disorders may be beneficial
Keywords: CIT, Crisis intervention team, Stigma, Mental illness, Substance use, law enforcement
Abstract
Limited empirical data and research exists about stigmatizing attitudes and perceptions held by law enforcement officers towards persons with mental illness and substance use issues. Pre- and post-training survey data from 92 law enforcement personnel who attended a 40-hour Crisis Intervention Team (CIT) training was used to investigate training-related changes in mental illness stigma and substance use stigma. Training participant's mean age was 38.35 ± 9.50 years, majority white non-Hispanic race/ethnicity (84.2%), male gender (65.2%), and reported job category as road patrol (86.9%). Pre-training, 76.1% endorsed at least one stigmatizing attitude towards people with mental illness, and 83.7% held a stigmatizing attitude towards those with substance use problems. Poisson regression revealed that working road patrol (RR=0.49, p<0.05), awareness of community resources (RR=0.66, p<0.05), and higher levels of self-efficacy (RR=0.92, p<0.05) were associated with lower mental illness stigma pre-training. Knowledge of communication strategies (RR=0.65, p<0.05) was associated with lower pre-training substance use stigma. Post-training, improvement in knowledge of community resources and increases in self-efficacy were significantly associated with decreases in both mental illness and substance use stigma. These findings highlight the existence of stigma related to both mental illness and substance use pre-training suggesting the need for implicit and explicit bias training prior to the start of active law enforcement duty. These data are consistent with prior reports indicating CIT trainings as a path to address mental illness and substance use stigma. Further research on effects of stigmatizing attitudes and additional stigma-specific training content is warranted.
1. Introduction
In general, prejudices and stereotypes have been shown to be a contributor to negative attitudes and behaviors towards persons with mental illness (Corrigan et al., 2009; Amodio and Swencionis, 2018), and stigmatizing attitudes have been shown to influence interactions between law enforcement and persons with mental illness (Compton et al., 2006; Godschalx, 1984; Laniyou and Goff, 2021). Interactions between individuals with mental illness and substance use disorders and law enforcement are common. A systematic review of 21 studies conducted by Livingston (2016) indicated that one in four people with mental disorders have histories of law enforcement involvement and police arrests. In that same review, data from 48 studies suggested that one in ten individuals has had police involvement in their pathway to mental health care (Livingston, 2016). Individual officers’ attitudes and beliefs, including stigma, affect their dispositions in confrontations with individuals with mental illness and can determine how these interactions are managed (Ritter et al., 2010; Tribolet-Hardy et al., 2015; Watson and Angell, 2007; Watson et al., 2004). Further, it has also been shown that an individual's race and ethnicity is also a risk factor for experiences of aggression from law enforcement (Kulesza et al., 2016; Hartman & Golub, 1999).
Given the recent attention of excessive use of force by some law enforcement officers when engaging individuals experiencing a mental health crisis, it is imperative that federal, state, and local government agencies support and engage in policies, practices, and programs that address bias and stigma, especially towards persons with mental health and substance use issues and those who may belong to racial and ethnic groups. Trainings that help front-line police officers identify signs of psychological distress and employ de-escalation practices can reduce stressful interactions and potentially decrease the use of lethal force used by officers, and can tools modify attitudes, build mental health literacy (Hansson and Markstrom, 2014) among law enforcement personnel. One such training adopted and implemented by law enforcement agencies across the United States, is the Crisis Intervention Team (CIT) training model (Watson et al., 2008).
1.1. Overview of CIT
The CIT training model was developed in 1988 in Memphis, Tennessee, in response to a critical incident in which a Memphis police officer fatally shot a man who suffered from mental illness and substance abuse (Hassell, 2020). A basic tenet of the CIT model suggests that if police officers knew more about serious mental illnesses (e.g., schizophrenia), their interactions with individuals with such an illness could be improved. Thus, the individual who is need of mental health support could be diverted from the criminal justice system and triaged to mental health care (Demir et al., 2009). The best‐known component of the model is the 40‐hour training designed to provide officers with knowledge and skills to intervene with individuals safely and effectively in a crisis and link them to mental health care (Watson et al., 2017a). The elements of the 40-hour didactic and interactive training generally include content related to communication and de-escalation strategies, legal issues, signs and symptoms of mental illness, recovery and treatment approaches, suicide risk assessment and intervention, drug and alcohol problems, and a collaborative exercise involving consumers of mental health services or their family members. Of note, while there is variation in how the CIT training is implemented across the United States, the format of the program generally does not plainly include a module on implicit bias or stigma despite evidence of the positive impact of anti-stigma training on officer's attitudes and behavior (Hansson and Markstrom, 2014).
1.2. CIT training impact and stigma
Previous research on CIT impact has shown a reduction in stigmatizing attitudes in police officers who received mental health training (Compton et al., 2006, 2017; Godschalx, 1984; Hansson and Markstrom, 2014). Stigmatizing attitudes of police officers can interfere with appropriate de-escalation approaches, strategies to avoid excessive force, and effectively transporting the persons in mental health crisis to an appropriate psychiatric or healthcare facility rather than arresting and/or incarcerating them (Ellis, 2014). Studies indicate that police officers who received any type of mental health training demonstrated an improvement in attitudes, reduction in stigma, and decreased use of force in a hypothetical mental health crisis encounter (Bonfine et al., 2014; Compton et al., 2006, 2008a, 2008b; Compton et al., 2011; Ellis, 2014; Godschlax, 1984; Morabito et al., 2012). For example, Compton et al. (2014) compared knowledge, attitudes, and skills of 251 CIT-trained officers with 335 non-CIT trained officers and found that CIT-trained officers reported greater knowledge about mental illnesses and their treatments, better attitudes, greater self-efficacy when interacting with someone with psychosis or suicidality, less stigma towards mental illness, better de-escalation decisions; and better referral decisions (Compton et al., 2014; Watson and Compton, 2019). Similarly, Hanafi et al. (2008) evaluated officers’ perceptions after the completion of a CIT program and found that officers perceived themselves as possessing greater knowledge of mental illnesses and greater confidence in managing situations involving people with mental illness.
Law enforcement officers often face numerous challenges when interacting with individuals with mental illness and substance use concerns whereby the use of traditional police tactics, such as verbal commands, verbal and/or physical force, and others, may escalate a situation or cause further distress for individuals experiencing acute symptoms (Desmarais et al., 2014; Engel et al., 2000; Watson et al., 2008;). The fear of injury or lack of understanding of mental illness and substance use may create tension between officers and individuals with mental illness, which may exacerbate an already tense encounter (Kerr et al., 2010). Stigma around substance use disorder has important implications for how law enforcement may perceive and predict the behavior of individuals who use drugs (Kruis et al., 2020; Lowder et al., 2019; Wagner et al., 2016).
Previous research has indicated that police officers tend to have negative and punitive attitudes about drug use and drug users as well as feeling pessimistic about the effectiveness of law enforcement strategies combating drug offenses (Jorgensen, 2018; Moore and Palmiotto, 1997). Some evidence also suggests that there are also differences in attitudes toward drugs based on age, race, and assignment where younger officers and patrol officers are more likely to hold punitive “get tough” attitudes, whereas minorities and police managers are less likely to hold such punitive attitudes, with the latter worrying about the unintended consequences of punitive practices being counterproductive (Beyer et al., 2002; Moore and Palmiotto, 1997). A more recent study examining stigma toward persons using opioids showed that officers held a relatively high level of stigma toward this vulnerable population as measured by perceptions of dangerousness, blame, and social distance (Kruis et al., 2020). This same study indicated that officer rank, support for the disease model of addiction, and beliefs about the demographic characteristics of a substance-using person were significantly associated with stigma among officers. Given that over 50% of jail and prison inmates meet the criteria for substance use disorder (Peters et al., 2015), understanding stigma related to substance misuse and receiving training on assessing and interacting with a person using drugs and alcohol is critical (Corrigan et al., 2009).
1.3. Current study
The purpose of this exploratory study was to: 1) examine associations of CIT trainee characteristics, knowledge, and self-efficacy with stigmatizing attitudes and 2) document the level of pre- and post-training stigmatizing attitudes towards mental illness and substance use. We used a pre- and post-training survey design to investigate stigma related to mental illness stigma and substance use and explored if CIT training was associated with a decrease in stigmatizing attitudes toward and perceptions of mental illness and substance use. To our knowledge, this is the first study to explore knowledge and attitudes related to both mental illness and substance use stigma among CIT- trained law enforcement. As CIT continues to serve as a model for training and enhancing first responder skills, research is needed to assess the potential impact of this educational program on reducing stigma. To reduce law enforcement's violent interactions with persons with mental health and substance use issues, it is imperative that they receive training to address stigma and explore their own biases (Demir et al., 2009). We hope this study illuminates the valuable role of CIT and encourages further investigation into behavior change related to stigma reduction among law enforcement.
2. Methods
2.1. Data collection
Data were collected via evaluation surveys administered to law enforcement trainees on the first (pre-training survey) and final (post-training survey) days of a five-session, 40-hour CIT training. CIT Training sessions were held between February and November 2019 in five non-urban counties in New York state. Prior to survey administration, each participant was assigned a unique identifier allowing for pre- and post-training survey data linkage. The surveys were developed through leveraging the expertise of CIT trainers and state collaborators as well as the research evaluation team at Nathan S. Kline Institute for Psychiatric Research (NKI). The instrument was then pilot tested for face and content validity among a cohort of twenty law enforcement CIT trainees in October 2018. Items in the surveys as well as general feedback from pilot study participants informed the discussion among the research team in evaluating the usefulness of the tool. The structure of the surveys was deemed appropriate. Minor changes were made to format the length of the survey (e.g., deleting some questions due to redundancy in language and refining items to better address key concepts related to the subject matter). All study procedures were approved by the NKI Institutional Review Board.
The pre-training survey ascertained information related to trainee sociodemographic and job characteristics, as well as their knowledge, self-efficacy, attitudes, and perceptions related to people with mental illness and substance use problems. To assess CIT training-related changes, the post-training survey also included questions related to knowledge, self-efficacy, attitudes, and perceptions. In this analysis, we are interested in exploring the associations between law enforcement trainee stigmatizing attitudes and perceptions, and sociodemographic and job-related characteristics, knowledge, and self-efficacy.
Predictors of interest. Demographic and job-related characteristics included age (in years), gender (male, female), race (white, non-white), law enforcement position (road patrol, or dispatch/ corrections/ other), years of service (less than 5 years, 5 to 14 years, 15 years or more), as well as an indicator for whether they had attended a police academy training mental health training (yes, no). Knowledge items assessed trainee ability to identify symptoms of psychosis and suicidal thoughts; ability to describe communication strategies and appropriate actions to take in dealing with a person in crisis; and awareness of community resources to assist in crisis situations. An indicator variable was used to identify trainees who displayed knowledge in each area (yes, no). Self-efficacy was measured as the sum of 12 items, which asked trainees to rate their confidence in recognizing signs of distress and utilizing skills to assist persons in distress (e.g., de-escalation, communication techniques). Each item was scored using a five-point Likert-scale (1 or strongly disagree to 5 or strongly agree) with higher sum score values representing greater levels of self-efficacy. For analysis of post-training stigma, change in trainee knowledge and self-efficacy were included as predictors. To measure improved knowledge in the four areas of interest, i.e., communication strategies, community resources, symptoms of psychosis, and indicators of suicidal thoughts, indicator variables were created to identify trainees with improved knowledge in each area (yes, no). With respect to self-efficacy, a variable measuring change in self-efficacy (post-training score – pre-training score) was utilized.
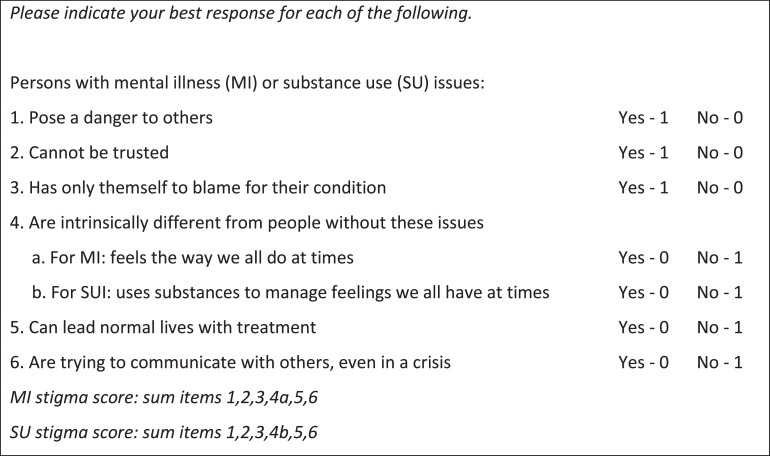
Mental illness and substance use stigma. Our analysis focused on two outcomes, stigmatizing attitudes towards individuals with (1) mental illness (MI) and (2) substance use (SU) issues. We measured MI and SU stigma separately. We would have liked to develop or adapt a tool specifically for examining stigma among the law enforcement workforce to include in this study; however, very few studies exist evaluating stigmatizing attitudes and beliefs around mental illness and substance use held by law enforcement officers. For our comparison between mental illness stigma and substance use stigma, we used parallel items and similar wording in the scales. Finally, we aimed to assess stigma given the specific context in which law enforcement interacts with persons with mental health and substance use issues (e.g., in a crisis, and in the community). Taking these factors into consideration, and leveraging existing literature on stigma, we developed a very brief 6-item scale to assess each of these key domains that are associated with stigma towards persons with MI/SU: being dangerous, not trustworthy, blameworthy, othered, and uncontrollable (see Fig. 1). To quantify the stigma, we computed a count of the number of discriminatory stereotypes endorsed by the trainee (Cronbach's alpha=0.7, range: 1–6).
Fig. 1.
Brief measure of stigmatizing attitudes and perceptions toward people with mental illness or substance use issues.
2.2. Analysis plan
First, we examined the distribution of study variables using frequencies and percentages or mean values and standard deviations, as appropriate. Second, we estimated crude or unadjusted associations between study measures (i.e., gender, age, years in service, law enforcement role, previous CIT training, knowledge, and self-efficacy) and pre-training MI and SU stigma using simple scaled Poisson regression modeling. Study measures meeting criteria of p<0.10 in crude association, were included in an initial multivariable or adjusted scaled Poisson regression model. From this initial adjusted model, a final adjusted model was constructed by retaining only measures maintaining p<0.10 in from the initial adjusted model. Coefficient estimates from scaled Poisson regression models are exponentiated and interpreted as rate ratios (RRs). Ratio estimates below 1 indicate decreased endorsement stigmatizing attitudes while estimates above 1 indicate increased endorsement of stigmatizing attitudes.
To explore the impact of the CIT training on MI and SU stigma, we assessed pre-post training changes in MI and SU sum score. First, using dependent samples t-test, we examined whether trainee pre-training mean MI and SU stigma scores were significantly different from their post-training scores. Then, we computed a difference score to quantify the pre-post change in stigma score (post-training score – pre-training score) for both MI and SU stigma; trainees with decreased stigmatizing attitudes had negative difference scores. To appropriately model the difference scores (which could be negative or positive), we used linear regression to explore associations between study measures and the difference scores among trainees who exhibited pre-training stigma (score>0). Study measures meeting criteria of p<0.10 in crude models were retained in an initial multivariable model. As above, only measures with p<0.10 in initial multivariable or adjusted modeling were retained in a final multivariable or adjusted model. We confirmed the proposed model building procedure and model fit by comparing Akaike information criteria (AIC) statistics from models for each outcome; models with the lowest AIC are preferred. Poisson and linear regression model assumptions were checked and confirmed to be reasonable; all analyses were conducted using SAS v9.4.
3. Results
A total of 92 law enforcement personnel attended the training. Table 1 provides a summary of trainee sociodemographic and job-related characteristics as well as pre-training knowledge, self-efficacy, and MI and SU stigma. Participants reported a mean age of 38.4 ± 9.5 years. Most participants identified as male (65.2%) and white race (84.8%). Roughly 87% of participants held a position related to road patrol in the police/sheriff's department, while about 13% of participants identified their role as dispatch and corrections. Participants’ years of service in law enforcement ranged from 1.5 to 30 years with an average of 11.6 years. Many trainees (92.4%) responded to having previous educational training pertaining to mental health. With respect to knowledge, among the 92 participants, 23.9% (n = 22) responded that they were able to describe communication skills; 75% (n = 69) were aware of community resources; 40% (n = 37) were able to identify typical symptoms of psychosis; 38% (n = 35) and were able identify indicators of suicidal thoughts.
Table 1.
Distribution of demographic characteristics and pre-training knowledge, self-efficacy, and stigma among CIT trainees in 5 New York State counties, 2019.
| Measures | Distribution, n (%) |
|---|---|
| All | 92 (100.0) |
| Gender | |
| Male | 60 (65.2) |
| Female | 32 (34.8) |
| Race | |
| White | 78 (84.8) |
| Non-White | 14 (15.2) |
| Age (years), mean (SD) | 38.3 (9.5) |
| Range | 23–59 |
| Law enforcement role | |
| Police/Sheriff (road patrol) | 80 (87.0) |
| Dispatch/corrections/other | 12 (13.0) |
| Years of service (years), mean (SD) | 11.60 (8.4) |
| Less than 5 years | 31 (33.7) |
| 5–14 years | 26 (28.3) |
| 15 years or more | 35 (38.0) |
| Previous mental health-related training | |
| Yes | 85 (92.4) |
| No | 7 (7.6) |
| Pre-training knowledge | |
| Describe communication strategies | 22 (23.9) |
| Awareness of community resources | 69 (75.0) |
| Identify typical symptoms of psychosis | 37 (40.2) |
| Identify indicators of suicidal thoughts | 35 (38.0) |
| Self-efficacy score, mean (SD) | |
| Pre-training | 14.6 (2.4) |
| Post-training | 17.5 (2.0) |
| Mental illness stigma | |
| Count, mean (SD) | |
| Pre-training | 1.7 (1.5) |
| Post-training | 1.0 (1.1) |
| Endorse at least one stigmatizing attitude | |
| Pre-training | 70 (76.1) |
| Post-training | 56 (60.9) |
| Substance use stigma | |
| Count, mean (SD) | |
| Pre-training | 2.4 (1.8) |
| Post-training | 1.4 (1.5) |
| Endorse at least one stigmatizing attitude | |
| Pre-training | 77 (83.7) |
| Post-training | 56 (60.9) |
The mean level of pre-training self-efficacy in the sample was 14.6 ± 2.4, which increased to 17.5 ± 2.0 at post-training. At pre-training, over three in four (n = 70, 76.1%) trainees endorsed at least one stigmatizing attitude related to MI, and fewer (n = 56, 60.9%) endorsed at least one stigmatizing attitude at post-training. The mean number of MI stigma items endorsed at pre-training (1.7 ± 1.5) decreased at post-training (1.0 ± 1.1; Paired t(91)=3.99, p = 0.0001). Over one-half (n = 48, 52.2%) of trainees had decreased levels of MI stigma post-training. SU stigma was endorsed at a higher rate pre training with over 80% of trainees reporting having at least one stigmatizing attitude (n = 77, 83.7%); this decreased post-training to 60.9% (n = 56) endorsing at least one SU stigma item. The mean number of SU stigma items endorsed pre-training was 2.4 ± 1.7. This decreased significantly to 1.4 ± 1.5 SU stigma items endorsed post-training (Paired t(91)=5.88, p<0.0001). Nearly two-thirds (n = 58, 63.0%) of trainees had decreased levels of SU stigma post-training.
3.1. Correlates of pre-training mental illness and substance use stigma
In Table 2, estimates from the scaled Poisson regression models for pre-training MI and SU stigma are provided. Road patrol assignment, being aware of community resources, and self-reported self-efficacy level were significantly associated with pre-training MI stigma in crude models at a 5% level of significance (p<0.05). Officers with a road patrol job role (Crude RR=0.49, p<0.05) reported lower MI stigma counts when compared to trainees in non-patrol roles; trainees aware of community resources pre-training had lower MI stigma scores compared to those who were not aware of community resources (Crude RR=0.66, p<0.05); trainees scoring higher on self-efficacy were found to endorse fewer stigmatizing attitudes related to MI (Crude RR=0.92, p<0.05). Having previous educational training was marginally significant (p<0.10), such that those who underwent previous educational training pertaining to mental health reported lower MI stigma counts when compared to those with no prior training. As such, having previous educational training, road patrol assignment, being aware of community resources, and self-reported self-efficacy level were included in an initial adjusted model for pre-training MI stigma (results not shown). From the initial adjusted analysis, having a road patrol officer role and having previous educational training were the only covariates that met criteria (p<0.10) to be included in a final adjusted model. Results from the final adjusted model, presented in Table 2, showed that with officers endorsing MI stigma items at a rate 50% lower than those working in dispatch, corrections, or other roles (Adj RR=0.50, p<0.05).
Table 2.
Results for crude and adjusted scaled Poisson regression of pre-training mental illness and substance use stigma count among CIT trainees in 5 New York State counties, 2019.a.
| Measures | Mental Illness Stigma |
Substance Use Stigma |
||
|---|---|---|---|---|
| Crude RR (95% CI) | Adj. RR (95% CI) | Crude RR (95% CI) | Adj. RR (95% CI) | |
| Gender | ||||
| Male | 0.82 (0.55 – 1.21) | 0.84 (0.60 – 1.18) | ||
| Female | ref | ref | ||
| Race | ||||
| White | 1.45 (0.79 – 2.68) | 1.30 (0.79 – 2.13) | ||
| Non-White | ref | ref | ||
| Age (years) | 0.99 (0.97 – 1.02) | 1.00 (0.98 – 1.01) | ||
| Law enforcement role | ||||
| Road patrol | 0.49 (0.32 – 0.76)⁎⁎ | 0.50 (0.32 – 0.77)⁎⁎ | 0.68 (0.45 – 1.04)* | 0.66 (0.44 – 1.00)⁎⁎ |
| Dispatch/corrections/other | ref | ref | ||
| Years of service | ||||
| Less than 5 years | ref | ref | ||
| 5–14 years | 1.24 (0.75 – 2.06) | 1.03 (0.67 – 1.58) | ||
| 15 years or more | 1.30 (0.81 – 2.08) | 1.16 (0.79 – 1.71) | ||
| Previous mental health-related training | 0.58 (0.33 – 1.05)* | 0.60 (0.34 – 1.04)* | 0.93 (0.51 – 1.70) | |
| Pre-training Knowledge | ||||
| Describe communication strategies | 0.82 (0.51 – 1.33) | 0.65 (0.42 – 0.99)⁎⁎ | – | |
| Awareness of community resources | 0.66 (0.44 – 0.98)⁎⁎ | – | 0.75 (0.53 – 1.07) | |
| Identify typical symptoms of psychosis | 0.84 (0.56 – 1.25) | 0.75 (0.53 – 1.05)* | 0.73 (0.52, 1.03)* | |
| Identify indicators of suicidal thoughts | 0.72 (0.50 – 1.13) | 0.77 (0.55 – 1.09) | ||
| Self-efficacy | 0.92 (0.85 – 0.99)⁎⁎ | – | 0.94 (0.88 – 1.01)* | – |
Notes:.
No. of observations, n = 92.
p<0.10,.
p<0.05.
With respect to pre-training SU stigma (see Table 2), knowledge of communication strategies was a statistically significant predictor of pre-training SU stigma in crude analysis. Law enforcement trainees with pre-training knowledge of communication strategies had lower rates of endorsing stigmatizing attitudes related to SU when compared to those who had less knowledge about communication strategies (Crude RR=0.65, p<0.05). Law enforcement job role, having pre-training knowledge of symptoms of psychosis, and trainee self-efficacy were found to be marginally associated with pre-training SU stigma, such that, being in road patrol role, having knowledge about symptoms of psychosis, and higher levels of self-efficacy trended toward lower endorsement of stigmatizing items about SU (p<0.10). Law enforcement job role, having pre-training knowledge of symptoms of psychosis, trainee self-efficacy, and pre-training knowledge of communication strategies were included in an initial multivariable model for pre-training SU stigma (results not shown). From the initial adjusted analysis, having a road patrol officer role and having pre-training knowledge of symptoms of psychosis met criteria (p<0.10) to be included in a final adjusted model. Only law enforcement job role was identified as a significant correlate of SU stigma in the final adjusted model at a 5% level of significance; road patrol officers exhibited lower pre-training SU stigma as compared to dispatch, corrections, or other officers (Adj RR=0.66, p<0.05).
3.2. Post-training change in mental illness and substance use stigma
Table 3 presents slope estimates for MI and SU stigma difference scores on sociodemographic characteristics, improved knowledge (post training), and change in self-efficacy (post training) among trainees exhibiting stigma pre training. Results found significant crude associations at the p<0.05 level such that trainees with 15 or more years of service experienced an average 0.87-unit decrease in MI stigma as compared to those with less than 5 years of service. Improved knowledge about community resources (Crude slope=−0.91, p<0.05) and self-efficacy (Crude slope=−0.15, p<0.05) post training was associated with decreased MI stigma. Increased age and improved knowledge about identifying indicators of suicidal thoughts were marginally associated with decreased MI stigma (p<0.10). When included together in an initial multivariable model including age, improved knowledge about identifying indicators of suicidal thoughts, years of service, improved post-training knowledge about community resources, and increased self-efficacy post-training, the latter two retained significance at a 10% level of significance. Results from the final model showed that only self-efficacy was significantly associated with decreased MI stigma at a 5% level of significance such that increased self-efficacy post-training was associated with decreased MI stigma post training (Adj. slope=−0.12, p<0.05). In terms of post-training decreases in SU stigma, results from the crude regression model indicated that improved knowledge about community resources and indicators of suicidal thoughts were both associated with decreases in the mean SU stigma count of 0.87 and 1.29 items, respectively. Increased post-training self-efficacy was also associated with significant decreases in SU stigma (Crude slope=−0.16, p<0.05). Only improved knowledge of community resources and increased post-training self-efficacy were retained from the initial adjusted model for inclusion in a final adjusted model. In the final adjusted linear regression model with improved knowledge about community resources, post-training improved self-efficacy was significantly associated with decreased SU stigma (Adj. slope=−0.13, p<0.05).
Table 3.
Results for crude and adjusted linear regression of post-training change in mental illness and substance use stigma among CIT trainees endorsing stigmatizing attitudes prior to training in 5 New York State counties, 2019.
| Measures | Mental Illness Stigmaa |
Substance Use Stigmab |
||
|---|---|---|---|---|
| Crude β (95% CI) | Adj. β (95% CI) | Crude β (95% CI) | Adj. β (95% CI) | |
| Gender | ||||
| Male | 0.12 (−0.60, 0.83) | 0.35 (−0.39, 1.09) | ||
| Female | ref | ref | ||
| Race | ||||
| White | −0.05 (−1.08, 0.98) | −0.60 (−1.57, 0.36) | ||
| Non-White | ref | ref | ||
| Age (years) | −0.03 (−0.05, 0.01)* | – | −0.01 (−0.05, 0.03) | |
| Law enforcement role | ||||
| Road patrol | 0.50 (−0.45, 1.43) | −0.31 (−1.28, 0.66) | ||
| Dispatch/corrections/other | ref | ref | ||
| Years of service | ||||
| Less than 5 years | ref | ref | ||
| 5–14 years | −0.76 (−1.62, 0.09)* | – | −0.28 (−1.18, 0.62) | |
| 15 years or more | −0.87 (−1.65, −0.08)⁎⁎ | – | −0.34 (−1.17, 1.04) | |
| Previous mental health-related training | 0.74 (−0.40, 1.88) | 0.26 (−0.97, 1.49) | ||
| Improved knowledge post-training | ||||
| Describe communication strategies | 0.41 (−0.35, 1.17) | 0.38 (−0.38, 1.14) | ||
| Awareness of community resources | −0.91 (−1.68, −0.15)⁎⁎ | −0.74 (−1.50, 0.01)* | −0.87 (−1.67, −0.08)⁎⁎ | −0.71 (−1.51, 0.08)* |
| Identify typical symptoms of psychosis | −0.20 (−1.04, 0.64) | −0.21 (−1.11, 0.68) | ||
| Identify indicators of suicidal thoughts | −0.67 (−1.48, 0.13)* | – | −1.29 (−2.14, −0.44)⁎⁎ | – |
| Post-training change in self-efficacy | −0.15 (−0.26, −0.03)⁎⁎ | −0.12 (−0.24, −0.00)⁎⁎ | −0.16 (−0.29, −0.02)⁎⁎ | −0.13 (−0.26, −0.02)⁎⁎ |
Notes:.
No. of observations, n = 70.
No. of observations, n = 77.
p<0.10.
p<0.05.
4. Discussion
Prior research has summarized positive effects of CIT training (Rogers et al., 2019; Watson and Compton, 2019), and have shown CIT programs to be effective at reducing unnecessary arrests, minimizing the use of force, and increasing referrals to psychiatric facilities (Bower and Petit, 2001; Compton et al., 2006, 2008c; Steadman et al., 2000). While our data also demonstrated an encouraging decrease in stigmatizing attitudes after the final day of training, and factors associated with this decrease, stigmatizing attitudes did not entirely diminish, and the impact on practice remains unknown.
Findings from this study, revealed, as previous studies have, that CIT training does have an impact on attitudes and perceptions of mental illness. Our results indicate stigmatizing attitudes related to mental illness and substance use among law enforcement officers prior to CIT training, and a decrease for some trainees afterwards. We observed a decrease in mental illness stigma among officers assigned to road patrol compared to those working in dispatch or corrections. This finding may indicate that officers with exposure and contact to individuals with mental illness in the community may have more familiarity and awareness of the challenges faced by this population, and in turn, may hold fewer stigmatizing views. Corrigan et al. (2002) found that contact with individuals with mental illness may reduce stigma, as both familiarity and compassion can have an important effect on bias. Conversely, while officers working in corrections also have contact with persons with mental illness, the context of incarceration and criminalization may inhibit compassion and foster stigmatizing attitudes. This plausible explanation warrants further study that includes observation of real-world follow-up data collected in these various work settings and documenting officer attitudes, experiences and practices.
Awareness of community resources also emerged as an important factor related to a decrease in stigma related to mental illness, and stigma related to substance use. Awareness of community resources is essential for providing localized care and potential diversion from arrest and the criminal justice system. Trainees who may have been aware of resources in their community to address the needs of the population may also have an ability to recognize signs and symptoms of mental illness based on knowledge about the resources in their community such as mental health providers, emergency services or mental health advocates. Further, awareness of community resources can also contribute to police officers’ capability to navigate the behavioral health services system and thus, enhance their self-efficacy that was found to decrease mental health and substance use stigma. Mapping Workshops, another component of the CIT program, brings together law enforcement and community members to identity community-responsive strategies to divert people away from the criminal justice system, can support integration and collaboration with localized assets in the community, which may further assist law enforcement in addressing the needs of those with mental illness and diverting them from jail.
In this analysis, we found increasing levels of self-efficacy associated with a decrease in stigma related to mental illness and substance use. Self-efficacy, the belief in one's own capacity to execute behaviors necessary to produce specific attainments (Bandura, 1977), has been explored in several service delivery professions and has been found to predict their behavior and motivation to persevere in a challenging situation (Love et al., 2021). In support of our findings, Bahora et al. (2008) found preliminary evidence of CIT enhanced self-efficacy when interacting with individuals with depression, cocaine dependence, schizophrenia, and alcohol dependence, and reduced social distance, many of which are the sources of stigma regarding individuals with these conditions. While there is a body of literature suggesting that self-efficacy may be protective and lead to more positive outcomes (Bahora et al., 2008; Compton et al., 2006; Ellis, 2014; Godfredson et al., 2010; Hanafi et al., 2008; Wells and Schafer, 2006), it may also lead to overconfidence and negative performance in some cases (Moores and Chang, 2009). Given historical and present-day events highlighting disproportionate use of excessive force by law enforcement when contending with members in the community experiencing a mental health crisis (Cojean et al., 2020; Kleider et al., 2010; Morabito et al., 2012) (including those with prior CIT training), it is likely additional and specialized training is warranted (Amodio and Swencionis, 2018; Boxer et al., 2021; Lai et al., 2014).
Crises are critical timepoints for intervention and treatment, and providing the appropriate level of intervention, including peer support and crisis respite, can result in positive outcomes for the individual and their family—and in safer communities (Steadman and Morrissette, 2016). Further, for a more fully comprehensive response, several other elements beyond police training and community assets should be considered: avoiding police involvement when it is not needed or appropriate, offering police community-based alternatives to jail, prioritizing behavioral health workers over police as first respondents in crisis events involving persons with mental health and substance use issues, offering some type of transportation from the encounter to the treatment setting when necessary, and providing respite options for individuals in crisis and their families (Steadman and Morrisette, 2016).
As CIT programs are lauded for their potential to reduce unnecessary arrests, to intervene with consumers more effectively without the use of force, and to obtain appropriate interventions for consumers (Lord et al., 2011), our study aims to further support the existing body of literature recognizing the use of communication, empathy, and de-escalation strategies to divert individuals in mental health crisis away from the criminal justice system. While existing research on CIT training to date has shown some measurable positive effects on officer-level outcomes (Compton et al., 2006; Ritter et al., 2010; Watson et al., 2008), further investigations are warranted given the limited body of literature examining the impact of CIT training on stigmatizing attitudes and beliefs held by officers. A review by Krameddine and Silverstone (2015) proposed four key concepts to evaluate effectiveness of law-enforcement trainings: 1) provide officers with training that is emotionally and intellectually engaging; 2) evaluate trainings across jurisdictions using consistent outcome; 3) assess behavior change in addition to changes; and 4) conduct repeated trainings to optimize effects of both skills acquired and memory retention (Krameddine and Silverstone, 2015). Adopting such practices in appraising the CIT program overall may help further our understanding of the long-term impact of stigma on police practice, including that related to mental illness, substance use, and those at the intersection of both conditions.
4.1. Limitations
There were several limitations to this study. First, the study is only a snapshot of officers that participated in the CIT program within a 10-month period in 2019 and among those who were employed in one of the five specific counties where CIT training was available at the time of the study. As such, the study sample of participants were from a select number of counties within a geographic region, thereby limiting the generalizability of the findings. Given the wide diversity in the law enforcement workforce, and the way CIT in implemented within certain regions, it would be critical to examine differences between law enforcement personnel at a regional level.
Second, our study did not determine the exact program components that may contribute to successful training outcomes measures for CIT such as behavioral change and impact of interactions over the longer term. Because research on the effectiveness of CIT continues to produce inconsistent findings, it is possible that focusing on certain categories of attitudes and program components could be more cost- efficient and more effective at addressing stigma (Haigh et al., 2020). Due to the variability in program components, there is a range of outcomes indicating that CIT has no effect in some jurisdictions and a medium effect in others (Canada et al., 2020; Taheri et al., 2016; Watson and Wood, 2017b). Standardizing the content and implementation of the CIT training can support greater scalability and replicability.
Additionally, our study did not measure any longitudinal outcomes of the training related to self-efficacy and/or knowledge. Our measures of stigma for mental illness and substance use captured participants self-perceived knowledge of content and are not a reflection of the items correctly answered in the evaluation. While our findings are consistent with earlier work in this area, it is unknown if improved self-efficacy or knowledge gained as a result CIT training will translate into real world practice. These data do not provide evidence of the impact of existing MH trainings on stigmatizing attitudes among law enforcement personnel. As such, we cannot determine whether officer behavior changed because of the training. This further supports that increasing awareness and understanding of mental illness does not necessarily translate into decreased stigma, and additional efforts to understand this are needed. Further research and evaluation on the impact of CIT on long-term behavior change is critically needed.
Finally, we did not measure whether and to what extent stigma of mental illness and of substance use intersects with race and ethnicity and given that minoritized consumers are more likely to experience aggression from law enforcement, this is an important topic that demands investigation (Kulesza et al., 2016; Hartman & Golub, 1999).
5. Conclusion
This study documents an immediate positive impact on beliefs, stigmatizing attitudes, and feelings of self-efficacy following a 40-hour CIT training. Our study highlights that increased knowledge of community resources and improved/higher self-efficacy was associated with less stigma and as such, it appears that participation in CIT training may further decrease stigma. However, the extent to which this impact extends into practice in the field, if at all, is unknown. Given the inequities in police response to community crisis events involving mental illness and/or substance use, it is likely that CIT training accompanied with ongoing training is warranted. Targeted funding to support educational programs to address stigma and bias among law enforcement is also needed to support these additional efforts. Overall, it is important to recognize that broad uptake of CIT deployment both nationally and internationally, and the municipal investment in the 40-hour CIT core curriculum suggests widespread commitment to better police training and increased community collaboration.
While CIT can serve as a conduit for addressing both explicit and implicit stigma through training and experiential learning, the process of exploring one's own biases should begin earlier, perhaps as a compulsory in-service training when one enters the academy. The need to expand training efforts to include mental illness and substance use-related stigma emerged in this study, which indicated that more specialized curriculum and content related to implicit bias, stigma and behavioral and psychological aspects of substance use disorders may be beneficial. Learning new skills and gaining knowledge through interactive and self-reflective training on implicit and explicit bias can support improved engagement of all persons with compassion, and particularly those with mental health and/or substance use problems. Successfully deescalating potentially precarious and aggressive interactions with individuals in crisis is paramount to an officer's ability to safely perform their jobs, decrease fatalities, and further build trust in the communities in which they serve.
Contibuting authors
Gilbert A. Nick - Conceptualization of the study, investigation, data analysis, and writing-original draft preparation
Sharifa Williams- Conceptualization of the study, investigation, data analysis, and writing-original draft preparation
Helen-Maria Lekas- Conceptualization of the study, investigation, and writing-original draft preparation
Kerstin Pahl- Conceptualization of the study, investigation, writing-reviewing and editing
Chloe Blau- Conceptualization of the study, investigation, writing-reviewing, and editing
Don Kamin- Conceptualization of the study, investigation, data analysis, and writing-original draft preparation
Crystal Lewis Conceptualization of the study, investigation, data analysis, and writing-original draft preparation
Role of funding source
Nothing Declared.
Conflicts of interest
None of the authors have any conflicts declared.
Acknowledgements
None
References
- Amodio D.M., Swencionis J.K. Proactive control of implicit bias: a theoretical model and implications for behavior change. J. Pers. Soc. Psychol. 2018;115(2):255–275. doi: 10.1037/pspi0000128. [DOI] [PubMed] [Google Scholar]
- Bahora, M., Hanafi, S., Chien, V.H., & Compton, M.T. (2008). Preliminary evidence of effects of crisis intervention team training on self-efficacy and social distance. Administration and Policy in Mental Health, 35(3), 159–167. https://doi.org/10.1007/s10488-007-0153-8 [DOI] [PubMed]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Beyer L., Crofts N., Reid G. Drug offending and Criminal Justice responses: practitioners’ Perspectives. Int. J. Drug Policy. 2002;13:203–211. doi: 10.1016/S0955-3959(02)00063-4. [DOI] [Google Scholar]
- Bonfine N., Ritter C., Munetz M.R. Police officer perceptions of the impact of Crisis Intervention Team (CIT) programs. Int. J. Law Psychiatry. 2014;37(4):341–350. doi: 10.1016/j.ijlp.2014.02.004. [DOI] [PubMed] [Google Scholar]
- Bower D., Pettit G. The Albuquerque Police Department's Crisis Intervention Team: a Report Card. FBI Law Enforce. Bull. 2001 https://corpora.tika.apache.org/base/docs/govdocs1/106/106725.pdf [Google Scholar]
- Boxer P., Brunson R.K., Gaylord-Harden N., Kahn K., Patton D.U., Richardson J., Rivera L.M., Smith Lee J.R., Staller M.S., Krahé B., Dubow E.F., Parrott D., Algrim K. Addressing the inappropriate use of force by police in the United States and beyond: a behavioral and social science perspective. Aggress. Behav. 2021;47(5):502–512. doi: 10.1002/ab.21970. [DOI] [PubMed] [Google Scholar]
- Canada K.E., Watson A.C., O'Kelley S. Utilizing Crisis Intervention Teams in Prison to Improve Officer Knowledge, Stigmatizing Attitudes, and Perception of Response Options. Crim. Justice Behav. 2020:1–2. doi: 10.1177/0093854820942274. [DOI] [Google Scholar]
- Cojean S., Combalbert N., Taillandier-Schmitt A. Psychological and sociological factors influencing police officers' decisions to use force: a systematic literature review. Int. J. Law Psychiatry. 2020;70 doi: 10.1016/j.ijlp.2020.101569. [DOI] [PubMed] [Google Scholar]
- Compton M.T., Esterberg M.L., McGee R., Kotwicki R.J., Oliva J.R. Brief reports: crisis intervention team training: changes in knowledge, attitudes, and stigma related to schizophrenia. Psychiatr. Serv. 2006;57(8):1199–1202. doi: 10.1176/ps.2006.57.8.1199. https://ps.psychiatryonline.org/doi/full/10.1176/ps.2006.57.8.1199 [DOI] [PubMed] [Google Scholar]
- Compton M.T., Bahora M., Watson A.C., Olivia J.R. A comprehensive review of extant research on crisis intervention team (CIT) programs. J. Am. Acad. Psychiatry Law. 2008;36:47–55. http://jaapl.org/content/36/1/47 [PubMed] [Google Scholar]
- Compton M.T., Chien V.H. Factors related to knowledge retention after crisis intervention team training for police officers. Psychiatr. Serv. 2008;59(9):1049–1051. doi: 10.1176/ps.2008.59.9.1049. [DOI] [PubMed] [Google Scholar]
- Compton M.T., Esterberg M.L., Broussard B. Causes of schizophrenia reported by Urban African American lay community members. Compr. Psychiatry. 2008;49(1):87–93. doi: 10.1016/j.comppsych.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Compton M., Demir, Neubert B., Broussard B., McGriff J., Morgan R., Oliva J. Use of force preferences and perceived effectiveness of actions among crisis intervention team police officers and non-CIT officers in an escalating psychiatric crisis involving a subject with schizophrenia. Schizophr. Bull. 2011;37:737–745. doi: 10.1093/schbul/sbp146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton, M.T., Bakeman, R., Broussard, B., Hankerson-Dyson, D., Husbands, L., Krishan, S., Stewart-Hutto, T., D'Orio, B.M., Oliva, J.R., Thompson, N.J., & Watson, A.C. (2014). The police-based crisis intervention team (CIT) model: I. Effects on officers' knowledge, attitudes, and skills. Psychiatr. Serv., 65(4), 517–522. https://doi.org/10.1176/appi.ps.201300107 [DOI] [PMC free article] [PubMed]
- Compton M.T., Bakeman R., Broussard B., D'Orio B., Watson A. Police officers' volunteering for (rather than being assigned to) Crisis Intervention Team (CIT) training: evidence for a beneficial self-selection effect. Behav. Sci. Law. 2017;35(5–6):470–479. doi: 10.1002/bsl.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P.W., Kuwabara S.A., O'Shaughnessy J. The public stigma of mental illness and drug addiction: findings from a stratified random sample. J. Social Work. 2009;9(2):139 147. doi: 10.1177/1468017308101818. [DOI] [Google Scholar]
- Corrigan P., Rowan D., Green A., Lundin R., River P., Uphoff-Wasowski K., Kubiak M. Challenging two mental illness stigmas: personal responsibility and dangerousness. Schizophr. Bull. 2002;28:293–309. doi: 10.1093/oxfordjournals.schbul.a006939. [DOI] [PubMed] [Google Scholar]
- Demir B., Broussard B., Goulding S.M., Compton M.T. Beliefs about Causes of Schizophrenia among Police Officers Before and After Crisis Intervention Team Training. Community Ment. Health J. 2009;45:385–392. doi: 10.1007/s10597-009-9194-7. [DOI] [PubMed] [Google Scholar]
- Desmarais S.L., Van Dorn R.A., Johnson K.L., Grimm K.J., Douglas K.S., Swartz M.S. Community violence perpetration and victimization among adults with mental illnesses. Am. J. Public Health. 2014;104(12):2342–2349. doi: 10.2105/AJPH.2013.301680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis H.A. Effects of a Crisis Intervention Team (CIT) training program upon police officers before and after Crisis Intervention Team training. Arch. Psychiatr. Nurs. 2014;28(1):10–16. doi: 10.1016/j.apnu.2013.10.003. [DOI] [PubMed] [Google Scholar]
- Engel R.S., Sobol J.J., Worden R.E. Further exploration of the demeanor hypothesis: the interaction effects of suspects' characteristics and demeanor on police behavior. Justice Q. 2000;17(2):235–258. doi: 10.1080/07418820000096311. [DOI] [Google Scholar]
- Godfredson J.W., Ogloff J.R.P., Thomas S.D.M., Luebbers S. Police discretion and encounters with people experiencing mental illness: the significant factors. Crim. Justice Behav. 2010;37(12):1392–1405. doi: 10.1177/0093854810383662. [DOI] [Google Scholar]
- Godschalx S.M. Effect of a Mental Health Educational Program Upon Police Officers. Res. Nurs. Health. 1984;7:111–117. doi: 10.1002/nur.4770070207. [DOI] [PubMed] [Google Scholar]
- Haigh C.B., Kringen A.L., Kringen J.A. Mental illness stigma: limitations of crisis intervention team training. Crim. Justice Policy Rev. 2020;31(1):42–57. doi: 10.1177/0887403418804871. [DOI] [Google Scholar]
- Hassell K.D. The impact of Crisis Intervention Team Training for police. Int. J. Police Sci. Manage. 2020;22(2):159–170. doi: 10.1177/1461355720909404. [DOI] [Google Scholar]
- Hanafi S., Bahora M., Demir B.N., Compton M.T. Incorporating Crisis Intervention Team (CIT) knowledge and skills into the daily work of police officers: a focus group study. Community Ment. Health J. 2008;44(6):427–432. doi: 10.1007/s10597-008-9145-8. [DOI] [PubMed] [Google Scholar]
- Hansson L., Markström U. The effectiveness of an anti-stigma intervention in a basic police officer training programme: a controlled study. BMC Psychiatry. 2014;14:55. doi: 10.1186/1471-244X-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorgensen C. Badges and Bongs: police Officers’ Attitudes Toward Drugs. Criminol. Criminal Justice. 2018;8(4):1–17. doi: 10.1177/2158244018805357. [DOI] [Google Scholar]
- Kerr A.N., Morabito M., Watson A.C. Police Encounters, Mental Illness and Injury: an Exploratory Investigation. J. Police Crisis Negot.: Int. J. 2010;10:116–132. doi: 10.1080/15332581003757198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleider H.M., Parrott D.J., King T.Z. Shooting behaviour: how working memory and negative emotionality influence police officer shoot decisions. Appl. Cogn. Psychol. 2010;24:707–717. doi: 10.1002/acp.1580. [DOI] [Google Scholar]
- Krameddine Y.I., Silverstone P.H. How to improve interactions between police and the mentally ill. Front. Psychiatry. 2015;5 doi: 10.3389/fpsyt.2014.00186. Article 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruis N.E., Choi J., Donohue R.H. Police officers, stigma, and the opioid epidemic. Int. J. Police Sci. Manage. 2020;22(4):393–406. doi: 10.1177/1461355720962524. [DOI] [Google Scholar]
- Lai C.K., Marini M., Lehr S.A., Cerruti C., Shin J.E., Joy-Gaba J.A., Ho A.K., Teachman B.A., Wojcik S.P., Koleva S.P., Frazier R.S., Heiphetz L., Chen E.E., Turner R.N., Haidt J., Kesebir S., Hawkins C.B., Schaefer H.S., Rubichi S., Sartori G., Nosek B.A. Reducing implicit racial preferences: I. a comparative investigation of 17 interventions. J. Exp. Psychol. Gen. 2014;143(4):1765–1785. doi: 10.1037/a0036260. [DOI] [PubMed] [Google Scholar]
- Laniyou A., Goff P.A. Measuring disparities in police use of force and injury among persons with serious mental illness. BMC Psychiatry. 2021;21(1):500. doi: 10.1186/s12888-021-03510-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston J. Contact Between Police and People with Mental Disorders: a Review of Rates. Psychiatr. Serv. 2016;67(8):850–857. doi: 10.1176/appi.ps.201500312. [DOI] [PubMed] [Google Scholar]
- Lord V.B., Bjerregaard B., Blevins K.R., Whisman H. Factors Influencing the Responses of Crisis Intervention Team–Certified Law Enforcement Officers. Police Q. 2011;14(4):388–406. doi: 10.1177/1098611111423743. [DOI] [Google Scholar]
- Love A.M.A., Usher E.L., Toland M.D., et al. Measuring police officer self-efficacy for working with individuals with autism spectrum disorder. J. Autism Dev. Disord. 2021;51:1331–1345. doi: 10.1007/s10803-020-04613-1. [DOI] [PubMed] [Google Scholar]
- Lowder E.M., Ray B.R., Gruenewald J.A. Criminal Justice Professionals’ Attitudes Toward Mental Illness and Substance Use. Community Ment. Health J. 2019;55:428–439. doi: 10.1007/s10597-019-00370-3. [DOI] [PubMed] [Google Scholar]
- Moores T.T., Chang J.C.J. Self-efficacy, overconfidence, and the negative effect on subsequent performance: a field study. Inf. Manage. 2009;46(2):69–76. doi: 10.1016/j.im.2008.11.006. [DOI] [Google Scholar]
- Moore R.H., Palmiotto M.J. Drug policies: a study of the opinions of local law enforcement patrol officers about various policy alternatives. J. Police Criminol. Psychol. 1997;12:32–38. doi: 10.1007/BF02813809. 1997. [DOI] [Google Scholar]
- Morabito M.S., Kerr A.N., Watson A., Draine J., Ottati V., Angell B. Crisis intervention teams and people with mental illness exploring the factors that influence the use of force. Crime Delinquency. 2012;58:57–77. doi: 10.1177/0011128710372456. [DOI] [Google Scholar]
- Peters R.H., Wexler H.K., Lurigio A.J. Co-occurring substance use and mental disorders in the criminal justice system: a new frontier of clinical practice and research. Psychiatr. Rehabil. J. 2015;38(1):1–6. doi: 10.1037/prj0000135. [DOI] [PubMed] [Google Scholar]
- Ritter C., Teller J.L.S., Munetz M.R., Bonfine N. Crisis Intervention Team (CIT) training: selection effects and long-term changes in perceptions of mental illness and community preparedness. J. Police Crisis Negot. 2010;10:133–152. doi: 10.1080/15332581003756992. [DOI] [Google Scholar]
- Rogers M.S., McNiel D.E., Binder R.L. Effectiveness of Police Crisis Intervention Training Programs. J. Am. Acad. Psychiatry Law. 2019;47(4):414–421. doi: 10.29158/JAAPL.003863-19. [DOI] [PubMed] [Google Scholar]
- Steadman H.J., Deane M.W., Borum R., Morrissey J.P. Comparing outcomes of major models of police responses to mental health emergencies. Psychiatr. Serv. 2000;51(5):645–649. doi: 10.1176/appi.ps.51.5.645. [DOI] [PubMed] [Google Scholar]
- Steadman H.J., Morrissette D. Police responses to persons with mental illness: going beyond CIT training. Psychiatr. Serv. 2016;67(10):1054–1056. doi: 10.1176/appi.ps.201600348. [DOI] [PubMed] [Google Scholar]
- Taheri S.A. Do crisis intervention teams reduce arrests and improve officer safety? A systematic review and meta-analysis. Crim. Justice Policy Rev. 2016;27(1):76–96. doi: 10.1177/0887403414556289. [DOI] [Google Scholar]
- Tribolet-Hardy F., Kesic D., Thomas S.D.M. Police management of mental health crisis situations in the community: status quo, current gaps and future directions. Policing Soc. 2015;25:294–307. doi: 10.1080/10439463.2013.865737. [DOI] [Google Scholar]
- Wagner K.D., Bovet L.J., Haynes B., Joshua A., Davidson P.J. Training law enforcement to respond to opioid overdose with naloxone: impact on knowledge, attitudes, and interactions with community members. Drug Alcohol Depend. 2016;165:22–28. doi: 10.1016/j.drugalcdep.2016.05.008. [DOI] [PubMed] [Google Scholar]
- Watson A.C., Corrigan P.W., Ottati V. Police officers’ attitudes toward and decisions about persons with mental illness. Psychiatr. Serv. 2004;55:49–53. doi: 10.1176/appi.ps.55.1.49. [DOI] [PubMed] [Google Scholar]
- Watson A.C., Angell B. Applying procedural justice theory to law enforcement's response to persons with mental illness. Psychiatr. Serv. 2007;58:787–793. doi: 10.1176/ps.2007.58.6.787. [DOI] [PubMed] [Google Scholar]
- Watson A.C., Morabito M.S., Draine J., Ottati V. Improving police response to persons with mental illness: a multi-level conceptualization of CIT. Int. J. Law Psychiatry. 2008;31(4):359–368. doi: 10.1016/j.ijlp.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson A.C., Compton M.T., Draine J.N. The crisis intervention team (CIT) model: an evidence-based policing practice? Behav. Sci. Law. 2017;35(56):431–441. doi: 10.1002/bsl.2304. [DOI] [PubMed] [Google Scholar]
- Watson A.C., Wood J.D. Everyday police work during mental health encounters: a study of call resolutions in Chicago and their implications for diversion. Behav. Sci. Law. 2017;35(5–6):442–455. doi: 10.1002/bsl.2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson A.C., Compton M.T. What research on crisis intervention teams tells us and what we need to ask. J. Am. Acad. Psychiatry Law. 2019;47(4):422–426. doi: 10.29158/JAAPL.003894-19. [DOI] [PubMed] [Google Scholar]
- Wells W., Schafer J.A. Officer perceptions of police responses to persons with a mental illness. Policing: Int. J. Police Strategies Manage. 2006;29(4):578–601. doi: 10.1108/13639510610711556. [DOI] [Google Scholar]