Highlights
-
•
34% of subjects in treatment had problems filling their buprenorphine prescription.
-
•
Few (8/51) subjects in treatment reported using illicit buprenorphine to get high.
-
•
Subjects with problems filling prescriptions were more likely to report illicit use.
Keywords: Opioid use disorder, Buprenorphine, Diversion, Naloxone
Abstract
Background
While barriers to accessing buprenorphine (BUP) therapy have been well described, little is known about pharmacy-related barriers. The objective of this study was to estimate the prevalence of patient-reported problems filling BUP prescriptions and determine whether these problems were associated with illicit use of BUP. The secondary objectives included identifying motivations for illicit BUP use and the prevalence of naloxone acquisition among patients prescribed BUP.
Methods
Between July 2019 and March 2020, 139 participants receiving treatment for an opioid use disorder (OUD) at two sites within a rurally-located health system, completed an anonymous 33-item survey. A multivariable model was used to assess the association between pharmacy-related problems filling BUP prescriptions and illicit substance use.
Results
More than a third of participants reported having problems filling their BUP prescription (34.1%, n = 47) with the most commonly reported problems being insufficient pharmacy stock of BUP (37.8%, n = 17), pharmacist refusal to dispense BUP (37.8%, n = 17), and insurance problems (34.0%, n = 16). Of those who reported illicit BUP use (41.5%, n = 56), the most common motivations were to avoid/ease withdrawal symptoms (n = 39), prevent/reduce cravings (n = 39), maintain abstinence (n = 30), and treat pain (n = 19). In the multivariable model, participants who reported a pharmacy-related problems were significantly more likely to use illicitly obtained BUP (OR=8.93, 95% CI: 3.12, 25.52, p < 0.0001).
Conclusion
Efforts to improve BUP access have primarily focused on increasing the number of clinicians waivered to prescribe; however, challenges persist with BUP dispensing and coordinated efforts may be needed to systematically reduce pharmacy-related barriers.
1. Introduction
Buprenorphine (BUP) is an effective medication for opioid use disorder (MOUD) and it is the most commonly prescribed MOUD in the United States (U.S.) (Substance Abuse and Mental Health Services Administration, 2022). While BUP access has increased in recent years (Olfson et al., 2020), treatment barriers persist. These barriers include the requirement of an X-waivered practitioner, limited treatment availability in rural communities, inadequate reimbursement from private and public insurers, and provider stigma (Haffajee et al., 2018; Andrilla et al., 2017; Cooper et al., 2020; Leece et al., 2019). In rural areas, these barriers are more apparent and are confounded by low health literacy, lack of rural providers, and lack of transportation (Cooper et al., 2020; Andrilla et al., 2017). While provider- and individual-level barriers to BUP access have been described (Walley et al., 2008; Roman et al., 2011), little is known about patient-reported pharmacy barriers to receiving BUP prescriptions.
Pharmacies play an important role in dispensing BUP prescriptions to treat opioid use disorder (OUD) and providing naloxone to prevent overdose deaths. In the U.S., approximately 90% of individuals live within 5 miles of a community pharmacy (National Association of Chain Drug Stores, 2021). Although geographical accessibility of pharmacies should improve access to prescription medications, pharmacists may choose not to stock BUP and/or engage in other practices that deter patients from filling BUP prescriptions at their pharmacy. The majority of the evidence on pharmacy-related barriers to BUP and naloxone access are anecdotal reports from community pharmacists. Commonly reported pharmacy barriers to BUP access include refusal to accept new BUP patients, refusal to fill legitimate BUP prescriptions, and insurance delays (e.g., prior authorizations, too soon to refill) (Cooper et al., 2020; Chaar et al., 2013; Thornton et al., 2017; Kazerouni et al., 2020). Patients receiving BUP may also encounter barriers accessing naloxone. The classification of naloxone as a prescription, rather than over-the-counter (OTC), medication and the variability in state-level naloxone access laws and their implementation contribute to patients’ inability to access naloxone from pharmacies (Evoy et al., 2021). Pharmacists have also described lack of training, time constraints, cost for patients, and inadequate reimbursement as barriers to dispensing naloxone (Rudolph et al., 2018; Bakhireva et al., 2017; Spivey et al., 2020; Martino et al., 2020). Inadequate stocking and requirement of patient identification are pharmacy barriers to accessing BUP and naloxone (Pollini et al., 2022; Thornton et al., 2017). The existing research on pharmacy barriers to MOUD and naloxone are mostly from the provider perspective and less is known about patient-reported barriers.
West Virginia (WV), like many states across the U.S., has implemented legislation making it easier for individuals to obtain naloxone and individuals can receive it directly from pharmacies without a prescription (via standing orders and other regulatory mechanisms). However, rates of naloxone dispensing are lowest in rural counties and only 20.4% of community pharmacists surveyed in WV felt comfortable dispensing naloxone without a prescription (Thornton et al., 2017; Guy et al., 2019). Federal initiatives, such as the Comprehensive Addiction and Recovery Act (CARA), the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act, and the 2021 Buprenorphine Practice Guidelines (U.S. Department of Health and Human Services, 2021), have increased the number of BUP prescribers (Substance Abuse and Mental Health Services Administration, 2022; Andrilla and Patterson, 2022). These efforts should translate to increased BUP prescriptions. However, it is unclear whether pharmacies are willing or able to accommodate the increased volume of BUP prescriptions.
Pharmacists who are hesitant to fill BUP prescriptions are often concerned about diversion or misuse (Cooper et al., 2020), and it is unclear whether this reflects anticipated or realized concerns. It is particularly important to understand that the inability to access BUP treatment was determined to be the strongest predictor of diverted BUP use (Lofwall and Havens, 2012). Research suggests that the motivations for using illicit BUP vary widely and mainly include pain management and self-treatment of addiction, especially in the event of insufficient supplies of illicit opioids or prescribed BUP. (Lofwall and Walsh, 2014; Schuman-Olivier et al., 2010; Cicero et al., 2018; Moratti et al., 2010; Silverstein et al., 2020; Tofighi et al., 2019). This study will be the first to examine patient-reported barriers to filling BUP prescriptions and to determine whether such problems are associated with illicit BUP use. In addition to examining BUP access, this study will examine access to and patients’ perspectives on how to improve access to addiction services.
2. Methods
2.1. Participants
Patients receiving outpatient BUP treatment or inpatient residential treatment for an OUD from a rurally-located health system, between July 2019 and March 2020, were approached about study participation. Patients were eligible to complete an anonymous 33-item survey if they had received at least 3 BUP prescriptions in the past 12 months. A study team member approached patients waiting for group therapy to determine interest in completing the survey and data was not captured on patients who declined to participate. The survey was briefly explained to the patients; they were informed that their survey responses were confidential and would not be shared with the clinical staff, and participation was voluntary.
2.2. Measures
The survey instrument consisted of 33-items and took approximately 5 to 15 min to complete. As there is no established instrument on pharmacy-related problems encountered when filling a BUP prescription, several questions were developed for this study. Demographic characteristics included age, state of residence, gender, and type of insurance (public, private, uninsured). The survey assessed frequency and duration of BUP prescription, and type of BUP product dispensed. Differences in the duration of BUP prescriptions reflect the outpatient BUP programs phased approach whereby the frequency of treatment sessions progressively declines as patients build consecutive days of abstinence and increased levels of functioning (Winstanley et al. 2020). Participants were asked to indicate which pharmacies they filled most of their prescriptions at, which pharmacies they filled their BUP prescriptions at, and at which pharmacies they had tried but were unable to fill their BUP prescriptions. Options included six national chain pharmacies, five local independent pharmacies, and health-system associated pharmacies.
Participants were asked if they had ever had any problems filling their BUP prescriptions. Those who responded ‘yes’ were asked to specify what problem(s) they have had (insufficient pharmacy stock, insurance issues, pharmacy refusal, and other) and how frequently those problems had occurred over the last 12 months (Never, 1–2, 3–4, 5–6, 7–8, 9–11, 12 or more, or every time). Participants were asked if they had ever had to go without their prescribed BUP because they could not get their prescriptions filled at a pharmacy. Those who responded ‘yes’ were asked to report the number of times it had occurred over the past 12 months and number of days they usually had to go without prescribed BUP because of a pharmacy-related issue. Participants were asked to report if they had to wait more than 24 h for their prescription to be filled and the reason(s) for any delays. Participants were then asked to report if they always filled the entire quantity of their BUP prescription and reason(s) they were not able to do so.
The questions regarding past year illicit BUP use were based on published studies and captured any prior BUP experience ("Did you use buprenorphine before ever using a pain pill?"), use of illicit BUP (“In the past 12 months, have you taken buprenorphine that was not prescribed to you?”), and extent of exposure to illicit BUP (“In the past 12 months, how many times have you gotten buprenorphine off the streets or from someone you know?”) (Monico et al., 2015). The information collected on illicit BUP use included specific product name and route of administration with modifications to include cost per dose and drug source (Monico et al., 2015; Cicero et al., 2011; Kenney et al., 2017). Reasons for illicit BUP use were evaluated by combining motivations from several previous studies. Eleven of the 19 included motivations were from a survey on prescribed and non-prescribed BUP use, sources and reasons for diverted BUP use, routes of administration, and treatment barriers (Cicero et al., 2018). Two items were adapted from the Buprenorphine Beliefs and Behaviors Questionnaire (BBBQ) (Schuman-Olivier et al., 2010). Given Lofwall and colleagues (2012) research suggesting that patients may try illicit BUP before engaging in formal therapy, we added two new response options, including “I did not know where or how to get treatment” and “I was not able to get treatment due to lack of transportation, childcare, or insurance”. An additional motivation was included to determine if patients used illicit BUP to “try the medication before starting treatment of their own” (Monico et al., 2015). The remaining three motivations included pharmacy-related barriers which had been discussed by research and clinical staff (pharmacist refusal, prescription cost, and had a prescription but ran out of medication early).
Participants were also queried regarding any prior naloxone access and how it was obtained (with or without a prescription or from a community/health program). Pharmacy satisfaction was assessed by asking participants to report their perception of the pharmacy team's actions and attitudes while filling their BUP prescription. Participants were also asked their preference about alternate therapy delivery methods, including receiving BUP at their treatment facility, starting BUP under the supervision of a pharmacist, and online/mail-order BUP treatment. The survey concluded with three open-ended questions to assess other problems accessing addiction services and recommendations to improve BUP access, reduce overdose deaths, and to support recovery.
2.3. Analysis
Frequencies and means were used to describe the sample characteristics, pharmacy related problems, and motivations for illicit BUP use. To determine whether illicit BUP use was associated with pharmacy-related barriers, a multivariable logistic regression model was used. The model controlled for age, sex, the frequency of BUP prescription, number of years taking BUP and whether they reported using other prescription medications without a prescription in the previous 30 days. Open-ended responses were categorized based on common themes agreed upon by the study team. The study was approved by the WVU Institutional Review Board.
3. Results
3.1. Demographic characteristics and buprenorphine prescriptions
A total of 139 participants completed the study. The mean subject age was 37.8 years (SD = 9.50). More than half (56.4%) were female and the vast majority (97.1%) resided in WV. The majority had public insurance (78.8%), 15.9% had private insurance and 5.3% of participants were uninsured. Prescription frequency varied with 33.8% receiving a prescription monthly, 20.1% receiving a prescription bi-weekly, 42.4% receiving a prescription weekly, and 3.6% receiving a prescription more than once a week. The duration of enrollment in BUP therapy among participants ranged from 10 days to 13 years; the mean length of BUP therapy was 3.1 years (SD= 3.1).
3.2. Access to buprenorphine and naloxone
Participants reported having filled their BUP prescription at a health system outpatient pharmacy (35.8%), national chain pharmacy (35.8%), and local independent pharmacy (8.8%); 19.7% reported using more than one type of pharmacy. Only 16% of participants filled their BUP prescription at a different pharmacy from where they filled most of their other prescriptions. Most participants indicated BUP dispensing at the same pharmacy every time (84.0%). Few participants (6.5%, n = 9) felt their pharmacy did not treat them in a similar fashion as other patients or that the pharmacy staff appeared hesitant to dispense their BUP prescription (4.3%, n = 6). Nearly half (46.3%) of participants reported no prior receipt or attempts to access a prescription for naloxone. Only six participants were unable to obtain naloxone after trying to get it. Among the 48 participants who reported obtaining naloxone from a pharmacy, only 1 did so without a prescription despite state-mandated naloxone dispensing for any patients prescribed opioids.
3.3. Pharmacy related barriers
More than a third of the participants reported having problems filling their BUP prescription (34.1%, n = 47). Among these participants, commonly reported BUP dispensing issues included insufficient or unavailable pharmacy stock of BUP (36.2%, n = 17), pharmacist refusal to dispense BUP (36.2%, n = 17), and insurance-related obstacles (e.g., prior authorization requirements, need for patient reenrollment; 34.0%, n = 16). One participant reported that “we live in a small town and the [pharmacy name] does not carry Suboxone® in stock”. Among participants reporting BUP dispensing issues, more than half (57.8%, n = 26) reported facing such issues about 1–2 times in the past 12 months. Twenty-seven participants (19.7%) reported having to go without BUP due to a pharmacy-related barrier and, on average, they went 5.0 days (SD = 5.1) without their prescribed BUP. Nearly one-fourth of the participants (26.6%, n = 37) reported not being able to receive their BUP within 24 h of prescription drop-off at the pharmacy at least once in the past year. Most participants (83.2%) received the entire quantity of their BUP prescriptions regularly. Several participants reported difficulty obtaining the entire prescribed quantity of BUP, with one participant describing that it was due to “lack of money for the whole thing or because pharmacy only had so many”. Two participants reported not filling their prescription in their hometown. One participant who had their BUP prescription refused by the pharmacist reported that their pharmacy “only filled RX for certain doctors”.
3.4. Illicit buprenorphine use and motivations
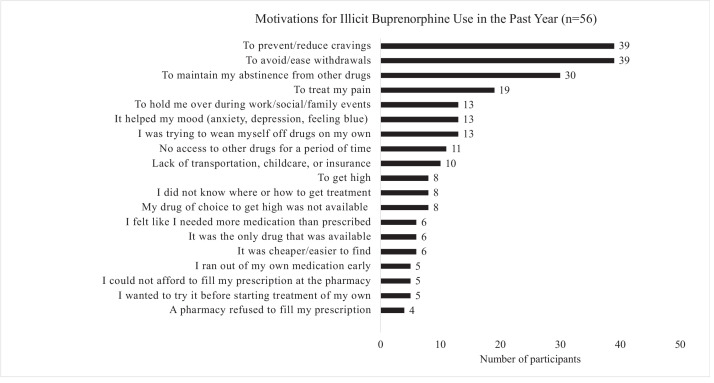
A minority of participants (11.9%, n = 16) reported having used BUP before having ever used opioid analgesics or heroin. Less than half (41.5%, n = 56) of participants indicated that they had used illicit BUP in the past 12 months. The number of times that patients had used illicit BUP ranged from 1 to 1000 times in the past 12 months (mode=8.5), with 39.4% of those endorsing illicit BUP reporting use within the last 30 days. Suboxone films were the most commonly utilized form of illicit BUP and the most commonly reported route of administration was sublingual (55.9%, n = 21). Illicit BUP was most commonly bought from another person (75%, n = 42) as opposed to obtained for free (25.0%, n = 14). Among those who reported illicit BUP use, the most common motivations were to quell withdrawal symptoms (76.5%, n = 39), cravings (76.5%, n = 39), maintain abstinence from other illicit opioids (58.8%, n = 30), and/or treat pain symptoms (37.3%, n = 19). Motivations for illicit BUP use are summarized in Fig. 1.
Fig. 1.
Motivations for illicit buprenorphine use in the past year (n = 56).
3.5. Open-ended responses
Twenty-nine participants reported other challenges to accessing addiction services they encountered in the past year. The challenges faced by participants included experiencing stigma (n = 6), lack of transportation (n = 4), pharmacy-related problems (n = 4), difficulty finding treatment (n = 3), long wait times (n = 3) and other problems (e.g., needing treatment for co-occurring disorders). One participant who experienced stigma reported that “[pharmacy name] refused to fill the prescription (threw it back at me with a dirty look)”. Other participants described their experience of stigma as “I was always treated like less than human”, “nobody wants to help us addicts”, and “doctors not caring about their patients”. Sixty-eight participants provided suggestions for improving BUP access, including the need for more addiction treatment facilities/programs (n = 40). Other recommendations for improving BUP treatment included ease and convenience of treatment (e.g., ease to get an appointment, fewer transportation challenges) (n = 12), decreasing out-of-pocket costs of treatment (n = 10), providing patient and community education on BUP treatment (n = 9), avoiding rigid clinical protocols (n = 4), reducing stigma (n = 2), and other suggestions (n = 4). One participant suggested “make treatment available online or at the pharmacy” and another recommended “vending machines”. Nearly identical themes emerged in response to what could be done in the state to reduce overdose deaths and help people achieve recovery (78 participants responded to this question). The majority of participants restated the need to expand treatment programs (n = 39) and other themes emerged including the need to increase access to naloxone (n = 6) and the need for harm reduction services (n = 2). For example, one participant stated “faster entry into treatment (less wait time)” and another noted the need for “better monitoring of patients and medication; better monitoring of dose given and taken”.
3.6. Multivariable model results
Participants reporting problems filling their BUP prescription in the past year were significantly more likely to report illicit BUP use in the past year (OR=8.93, 95% CI: 3.12, 25.52, p < 0.0001). Similarly, participants who reported using other medications without a prescription in the past month were more likely to report illicit BUP use in the past year (OR=6.46, 95% CI: 2.14, 19.56, p < 0.001).
4. Discussion
While many communities or treatment programs have anecdotally reported that their patients have problems filling their BUP prescriptions, the extent and details of these problems has been unknown. This study found that a third of participants encountered problems at the pharmacy, sometimes due to their insurance, when filling their BUP prescriptions in the past year. This study found that participants who reported pharmacy-related barriers to BUP dispensing were 8.9 times more likely to report past year illicit BUP use. This finding is consistent with prior literature reporting an association between BUP diversion and barriers to treatment access (Fox et al., 2015; Bazazi et al., 2011; Tofighi et al., 2019). Individuals reporting the illicit use of BUP often prefer to use legally prescribed BUP and decreased illicit BUP use when being prescribed BUP by a provider (Cicero et al., 2018; Schuman-Olivier et al., 2010). Paradoxically, regulations to prevent BUP diversion and misuse may decrease access to treatment and hence inadvertently cause some individuals to seek BUP from alternative sources.
Pharmacist refusal to fill BUP prescriptions has been documented previously, with some pharmacists expressing fear of legal repercussions and negative attitudes toward BUP (Cooper et al., 2020; Textor et al., 2022; Muzyk et al., 2019). If pharmacists have concerns about the veracity of a BUP prescription, they may not fill it out of fears that the questionable prescription could trigger a DEA investigation that could result in a loss of their license and/or limit their ability to obtain controlled substances (Cooper et al., 2020; Textor et al., 2022). It is unclear whether the veracity of the prescription is questionable due to how the patient presents in the pharmacy or due to the prescriber. In response to efforts to monitor and regulate the distribution of prescription opioid analgesics, wholesalers enforce supply ratios that would prohibit unexpected increases in pharmacy orders of controlled substances. Hence, if a community has newly X-waivered providers that are able to substantially increase BUP treatment access, it is possible that the local pharmacies could see their BUP orders restricted by wholesalers. Policymakers may want to consider recommending that wholesalers exclude BUP when calculating these ratios.
Participants who reported pharmacy-related issues filling their BUP prescription had to go without their medication for an average of 5 days. Participants reported pharmacy-related problems associated with their insurance, including prior authorizations and “refill too soon” rejections. Prior authorizations for BUP delay treatment for acute withdrawal symptoms and cravings while placing considerable burden on providers (Beetham, 2019). Although laws vary in terms of when a controlled medication can be refilled, insurance companies may impose stricter guidelines. These limits require patients to make multiple trips to a pharmacy, which are confounded in rural areas due to lack of transportation and significant travel time (Chan et al., 2006). Insufficient or unavailable stock of BUP is another largely uncontrollable issue at pharmacies, with some pharmacies choosing not to stock BUP. This can be harmful to patient care because BUP is a maintenance medication and is most effective when used regularly, therefore, the inability to get BUP may trigger a relapse (Ronquest et al., 2018). Since BUP is classified as a controlled substance, pharmacies may be less likely to partially fill the prescription, which may force patients to go without BUP. To remedy this, pharmacies may provide minimum days’ supply of BUP until they receive the remaining quantity or dispense the remainder of their stock. Patients who had to go to the pharmacy weekly for BUP prescriptions were 3.4 times more likely to engage in illicit BUP use. Since those receiving weekly BUP prescriptions are likely to be patients who recently initiated treatment, illicit BUP use may occur more frequently in the early stages of recovery. This issue may also be attributed to strict enforcement of early medication refills that can vary based on state laws and insurance policies. Additionally, it is unclear whether insufficient pharmacy supplies of BUP reported by participants were accurate. Prior studies have found that some pharmacists may falsely inform patients and prescribers that they did not stock BUP to avoid filling prescriptions that they believed to be suspicious (Textor et al., 2022).
An approach to alleviate pharmacy-related barriers is to provide BUP at office visits instead of pharmacies, which has shown to increase treatment retention rates, improve health outcomes, and increase patient satisfaction (Khan et al., 2021; Kolb and Reuth, 2021). Pharmacies integrated into office-based opioid treatment (OBOT) programs allow patients to receive BUP and naloxone from pharmacists trained in OUD care during clinic visits. This clinical workflow can overcome the inconvenience, long waiting times, and transportation challenges, hence providing opportunities for patients to receive optimal care. Low-threshold BUP treatment could also address patient-reported barriers by offering same-day treatment, harm reduction approaches, flexible program requirements, and availability in non-traditional settings (Jakubowski and Fox, 2020). Consistent with previous studies of community pharmacists, participants in this study reported being stigmatized by pharmacy staff (Trull et al., 2021; Cooper et al., 2020; Chaar et al., 2013; Werremeyer et al., 2021). In North Dakota, a training program implemented in community pharmacies was effective in positively changing pharmacists’ perceptions about opioid misuse or overdose (Eukel et al., 2019). More research is needed on training programs and other strategies to reduce pharmacists’ stigma towards patients with OUD.
Several studies have identified motivations for illicit BUP use, but few have included those currently in BUP treatment or in rural areas. Consistent with previous findings (Schuman-Olivier et al., 2010; Cicero et al., 2018; Chilcoat et al., 2019), the majority of participants in this study reported using illicit BUP as a form of self-treatment to prevent drug cravings and to ease withdrawal symptoms, whereas a much smaller proportion of participants used illicit BUP to experience euphoric effects. Alarm has been raised about increasing BUP diversion over the past several years; however, an increase in raw numbers may not be proportionate to the increased number of people now being treated with BUP. In fact, a recent national survey reported a decrease in BUP misuse between 2015 and 2019 among patients prescribed BUP (Han et al. 2021). In a March 2022 press release, the DEA reported doing outreach with pharmacists to express their support for MOUD (DEA, 2022). During this same time there were anecdotal reports in WV that the DEA told pharmacists that they would investigate BUP prescriptions like other controlled drugs and that treatment programs were struggling to find pharmacies in their community willing to fill their patients’ BUP prescriptions. There is a significant need to ensure local and federal coordination of efforts to ensure that valid BUP prescriptions can be easily filled in community pharmacies.
Patients receiving BUP are particularly susceptible to opioid overdose after a period of abstinence (Strang et al., 2003) and should be provided with opioid overdose education and naloxone (Department of Health and Human Services, 2018). Despite the implementation of state-mandated naloxone standing orders in pharmacies in WV, only one participant received naloxone from a pharmacy without a written prescription. This finding highlights unanticipated systems-, pharmacy-, and patient-level barriers limiting the provision of pharmacy-based naloxone dispensing. Low adoption of prescription-free naloxone has been documented in other states and has been attributed to a lack of knowledge of naloxone dispensing guidelines, insufficient pharmacy staff training, lack of administrative and clinical staff support to offset already overburdened pharmacy staff, lack of physician and/or patient acceptability for receiving naloxone, and pharmacy staff stigma towards patients with substance use disorders (Evoy et al., 2018; Tofighi et al., 2021). This suggests a need for training and education, organizational support, and payment for pharmacists’ services to maximize the role of community pharmacists in OUD care.
There are several limitations to this study. The questions regarding pharmacy-related barriers and the use of illicit BUP were framed within the past year and did not account for lifetime prevalence. This may have led to an underrepresentation of these issues as participants may be more likely to experience these issues when initiating OUD therapy. Survey non-response rates were not measured in this study; therefore, it is unclear whether non-response bias occurred. The study was conducted at two sites within one health system and it is unknown whether these results would generalize to other clinical settings. Since the open-ended responses provided by study participants were brief and without much context, additional qualitative research is warranted to further explore patients’ experiences and perceptions of these issues.
5. Conclusion
Although work has been done to expand access to BUP, patients encounter problems at the pharmacy when filling their BUP prescriptions, which may increase the risk of relapse and contribute to illicit BUP use. Local, state and federal coordination may be required to address these barriers to ensure timely access to this life-saving medication.
Role of funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Dr. Choo's doctoral studies are supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942–05. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
CRediT authorship contribution statement
Erin L. Winstanley: Visualization, Conceptualization, Writing – review & editing, Methodology. Emily P. Thacker: Writing – review & editing, Conceptualization, Methodology. Lyn Yuen Choo: Writing – review & editing, Conceptualization, Methodology. Laura R. Lander: Conceptualization, Writing – review & editing. James H. Berry: Writing – review & editing, Conceptualization. Babak Tofighi: Writing – review & editing, Conceptualization.
Declaration of Competing Interest
No conflicts declared.
References
- Andrilla C.H.A., Patterson D.G. Tracking the geographic distribution and growth of clinicians with a DEA waiver to prescribe buprenorphine to treat opioid use disorder. J. Rural Health. 2022;38(1):87–92. doi: 10.1111/jrh.12569. [DOI] [PubMed] [Google Scholar]
- Andrilla C.H.A., Coulthard C., Larson E.H. Barriers rural physicians face prescribing buprenorphine for opioid use disorders. Ann. Fam. Med. 2017;15:359–362. doi: 10.1370/afm.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakhireva L.N., Bautista A., Cano S., Shrestha S., Bachyrycz A.M., Cruz T.H. Barriers and facilitators to dispensing of intranasal naloxone by pharmacists. Subst. Abus. 2017;39(3):331–341. doi: 10.1080/08897077.2017.1391924. [DOI] [PubMed] [Google Scholar]
- Bazazi A.R., Yokell M., Fu J.J., Rich J.D., Zaller N.D. Illicit use of buprenorphine/naloxone among injecting and noninjecting opioid users. J. Addict. Med. 2011;5(3):175–180. doi: 10.1097/ADM.0b013e3182034e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beetham T. Buprenorphine prior authorization removal: low hanging fruit in the opioid epidemic fight. Harv. Public Health Rev. 2019;25:1–5. [Google Scholar]
- Chaar B.B., Wang H., Day C.A., Hanrahan J.R., Winstock A.R., Fois R. Factors influencing pharmacy services in opioid substitution treatment. Drug Alcohol Rev. 2013;32(4):426–434. doi: 10.1111/dar.12032. [DOI] [PubMed] [Google Scholar]
- Chan L., Hart L.G., Goodman D.C. Geographic access to health care for rural medicare beneficiaries. J. Rural Health. 2006;22(2):140–146. doi: 10.1111/j.1748-0361.2006.00022.x. [DOI] [PubMed] [Google Scholar]
- Chilcoat H.D., Amick H.R., Sherwood M.R., Dunn K.E. Buprenorphine in the United States: motives for abuse, misuse, and diversion. J. Subst. Abuse Treat. 2019;104:148–157. doi: 10.1016/j.jsat.2019.07.005. [DOI] [PubMed] [Google Scholar]
- Guy, G.P. Jr, Haegerich, T.M., Evans, M.E., Losby, J.L., Young, R., Jones, C.M., 2019. Vital Signs: Pharmacy-Based Naloxone Dispensing - United States, 2012-2018. MMWR Morb Mortal Wkly Rep. 68 (31), 679–686. doi: 10.15585/mmwr.mm6831e1. PMID: 31393863; PMCID: PMC6687198. [DOI] [PMC free article] [PubMed]
- Cicero T.J., Ellis M.S., Chilcoat H.D. Understanding the use of diverted buprenorphine. Drug Alcohol Depend. 2018;193:117–123. doi: 10.1016/j.drugalcdep.2018.09.007. [DOI] [PubMed] [Google Scholar]
- Cicero T.J., Ellis M.S., Paradis A., Ortbal Z. Role of key informants and direct patient interviews in epidemiological studies of substance abuse. Pharmacoepidemiol. Drug Saf. 2011;20(3):308–312. doi: 10.1002/pds.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H.L., Cloud D.H., Freeman P.R., Fadanelli M., Green T., Van Meter C., Beane S., Ibragimov U., Young A.M. Buprenorphine dispensing in an epicenter of the U.S. opioid epidemic: a case study of the rural risk environment in appalachian kentucky. Int. J. Drug Policy. 2020;85 doi: 10.1016/j.drugpo.2020.102701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DEA Press release on March 23, 2022 https://www.dea.gov/press-releases/2022/03/23/deas-commitment-expanding-access-medication-assisted-treatment.
- Department of Health and Human Services, 2018. U.S. surgeon general's advisory on naloxone and opioid overdose. https://www.hhs.gov/surgeongeneral/reports-and-publications/addiction-and-substance-misuse/advisory-on-naloxone/index.html (Accessed May 19, 2022).
- Eukel H.N., Skoy E., Werremeyer A., Burck S., Strand M. Changes in pharmacists' perceptions after a training in opioid misuse and accidental overdose prevention. J. Contin. Educ. Health. Prof. 2019;39(1):7–12. doi: 10.1097/CEH.0000000000000233. [DOI] [PubMed] [Google Scholar]
- Evoy K.E., Hill L.G., Groff L., Mazin L., Carlson C.C., Reveles K.R. Naloxone accessibility without a prescriber encounter under standing orders at community pharmacy chains in Texas. JAMA. 2018;320(18):1934. doi: 10.1001/jama.2018.15892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evoy K.E., Hill L.G., Davis C.S. Considering the potential benefits of over-the-counter naloxone. Integr. Pharm. Res. Pract. 2021;10:13–21. doi: 10.2147/IPRP.S244709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox A.D., Chamberlain A., Sohler N.L., Frost T., Cunningham C.O. Illicit buprenorphine use, interest in and access to buprenorphine treatment among syringe exchange participants. J. Subst. Abuse Treat. 2015;48(1):112–116. doi: 10.1016/j.jsat.2014.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haffajee R.L., Bohnert A.S.B., Lagisetty P.A. Policy pathways to address provider workforce barriers to buprenorphine treatment. Am. J. Prev. Med. 2018;54(6 Suppl 3):S230–S242. doi: 10.1016/j.amepre.2017.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B., Jones C.M., Einstein E.B., Compton W.M. Trends in and characteristics of buprenorphine misuse among adults in the US. JAMA Netw. Open. 2021;4(10) doi: 10.1001/jamanetworkopen.2021.29409. Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakubowski A., Fox A. Defining low-threshold buprenorphine treatment. J. Addict. Med. 2020;14(2):95–98. doi: 10.1097/ADM.0000000000000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazerouni N.J., Irwin A.N., Levander X.A., Geddes J., Johnston K., Gostanian C.J., Mayfield B.S., Montgomery B.T., Graalum DC, Hartung DM D.C., Hartung D.M. Pharmacy-related buprenorphine access barriers: An audit of pharmacies in counties with a high opioid overdose burden. Drug Alcohol Depend. 2021;224:108–729. doi: 10.1016/j.drugalcdep.2021.108729. [DOI] [PubMed] [Google Scholar]
- Kenney S.R., Anderson B.J., Bailey G.L., Stein M.D. The relationship between diversion-related attitudes and sharing and selling buprenorphine. J. Subst. Abuse Treat. 2017;78:43–47. doi: 10.1016/j.jsat.2017.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A., Khan Q., Kolb E. Supportive alternate site provision of buprenorphine: overcoming barriers and improving patient outcomes. J. Subst. Abuse Treat. 2021;123 doi: 10.1016/j.jsat.2020.108256. [DOI] [PubMed] [Google Scholar]
- Kolb E., Rueth M. Patient satisfaction with clinic-based medication pick up: addressing pharmacy-level challenges to buprenorphine access. J. Opioid Manag. 2021;17(7):77–86. doi: 10.5055/jom.2021.0645. [DOI] [PubMed] [Google Scholar]
- Leece P., Khorasheh T., Corace K., Strike C., Bayoumi A.M., Taha S., Marks E., Pach B., Ahamad K., Grennell E., Holowaty M., Manson H., Straus S.E. Barriers and facilitators to buprenorphine use for opioid agonist treatment: protocol for a scoping review. BMJ Open. 2019;9(12):32285. doi: 10.1136/bmjopen-2019-032285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofwall M.R., Havens J.R. Inability to access buprenorphine treatment as a risk factor for using diverted buprenorphine. Drug Alcohol Depend. 2012;126(3):379–383. doi: 10.1016/j.drugalcdep.2012.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofwall, M.R., Walsh, S.L., 2014. A review of buprenorphine diversion and misuse: the current evidence base and experiences from around the world. J. Addict. Med. 8 (5), 315–326. doi: 10.1097/ADM.0000000000000045. PMID: 25221984; PMCID: PMC4177012. [DOI] [PMC free article] [PubMed]
- Martino J.G., Smith S.R., Rafie S., Rafie S., Marienfeld C. Physician and pharmacist: attitudes, facilitators, and barriers to prescribing naloxone for home rescue. Am. J. Addict. 2020;29(1):65–72. doi: 10.1111/ajad.12982. [DOI] [PubMed] [Google Scholar]
- Monico L.B., Mitchell S.G., Gryczynski J., Schwartz R.P., O'Grady K.E., Olsen Y.K., Jaffe J.H. Prior experience with non-prescribed buprenorphine: role in treatment entry and retention. J. Subst. Abuse Treat. 2015;57:57–62. doi: 10.1016/j.jsat.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moratti E., Kashanpour H., Lombardelli T., Maisto M. Intravenous misuse of buprenorphine: characteristics and extent among patients undergoing drug maintenance therapy. Clin. Drug Investig. 2010;30(Suppl 1):3–11. doi: 10.2165/11536020-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Muzyk A., Smothers Z.P.W., Collins K., MacEachern M., Wu L.T. Pharmacists' attitudes toward dispensing naloxone and medications for opioid use disorder: a scoping review of the literature. Subst. Abus. 2019;40(4):476–483. doi: 10.1080/08897077.2019.1616349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of Chain Drug Stores, 2021. New NACDS report demonstrates how leveraging the expertise and accessibility of pharmacists will help support broader healthcare transformation to advance quality and value. https://www.nacds.org/news/new-nacds-report-demonstrates-how-leveraging-the-expertise-and-accessibility-of-pharmacists-will-help-support-broader-healthcare-transformation-to-advance-quality-and-value/(Accessed April 25, 2022)
- Olfson M., Zhang V.S., Schoenbaum M., King M. Trends in buprenorphine treatment in the United States, 2009-2018. JAMA. 2020;323(3):276–277. doi: 10.1001/jama.2019.18913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollini, R.A., Ozga, J.E., Joyce, R., Xuan, Z., Walley, A.Y., 2022. Limited access to pharmacy-based naloxone in West Virginia: Results from a statewide purchase trial. Drug Alcohol Depend. 231:109259. doi: 10.1016/j.drugalcdep.2021.109259. Epub 2021 Dec 31. PMID: 34998246; PMCID: PMC8810724. [DOI] [PMC free article] [PubMed]
- Roman P.M., Abraham A.J., Knudsen H.K. Using medication-assisted treatment for substance use disorders: evidence of barriers and facilitators of implementation. Addict. Behav. 2011;36:584–589. doi: 10.1016/j.addbeh.2011.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronquest N., Willson T., Montejano L., Nadipelli V., Wollschlaeger B. Relationship between buprenorphine adherence and relapse, health care utilization and costs in privately and publicly insured patients with opioid use disorder. Subst. Abuse Rehabil. 2018;Vol. 9:59–78. doi: 10.2147/SAR.S150253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph S.E., Branham A.R., Rhodes L.A., Hayes H.H., Moose J.S., Marciniak M.W. Identifying barriers to dispensing naloxone: a survey of community pharmacists in North Carolina. J. Am. Pharm. Assoc. 2018;58(4S):S55–S58. doi: 10.1016/j.japh.2018.04.025. e3. [DOI] [PubMed] [Google Scholar]
- Schuman-Olivier Z., Albanese M., Nelson S.E., Roland L., Puopolo F., Klinker L., Shaffer H.J. Self-treatment: illicit buprenorphine use by opioid-dependent treatment seekers. J. Subst. Abuse Treat. 2010;39(1):41–50. doi: 10.1016/j.jsat.2010.03.014. [DOI] [PubMed] [Google Scholar]
- Silverstein S.M., Daniulaityte R., Miller S.C., Martins S.S., Carlson R.G. On my own terms: motivations for self-treating opioid-use disorder with non-prescribed buprenorphine. Drug Alcohol Depend. 2020;210 doi: 10.1016/j.drugalcdep.2020.107958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spivey C.A., Wilder A., Chisholm-Burns M.A., Stallworth S., Wheeler J. Evaluation of naloxone access, pricing, and barriers to dispensing in Tennessee retail community pharmacies. J. Am. Pharm. Assoc.: JAPhA. 2020;60(5) doi: 10.1016/j.japh.2020.01.030. , 694–701.e1. [DOI] [PubMed] [Google Scholar]
- Strang J., McCambridge J., Best D., Beswick T., Bearn J., Rees S., Gossop M. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326(7396):959–960. doi: 10.1136/bmj.326.7396.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2022. Buprenorphine. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/buprenorphine (Accessed May 6, 2022).
- Thornton J.D., Lyvers E., Scott V.G.G., Dwibedi N. Pharmacists' readiness to provide naloxone in community pharmacies in West Virginia. J. Am. Pharm. Assoc. 2017;57(2S):S12–S18. doi: 10.1016/j.japh.2016.12.070. (Wash. DC)e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Textor L., Ventricelli D., Aronowitz S.V. Red flags' and 'red tape': telehealth and pharmacy-level barriers to buprenorphine in the United States. Int. J. Drug Policy. 2022;105 doi: 10.1016/j.drugpo.2022.103703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi B., Lekas H.M., Williams S.Z., Martino D., Blau C., Lewis C.F. Rural and small metro area naloxone-dispensing pharmacists' attitudes, experiences, and support for a frontline public health pharmacy role to increase naloxone uptake in New York State, 2019. J. Subst. Abuse Treat. 2021;129 doi: 10.1016/j.jsat.2021.108372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi B., Williams A.R., Chemi C., Suhail-Sindhu S., Dickson V., Lee J.D. Patient barriers and facilitators to medications for opioid use disorder in primary care. Subst. Use Misuse. 2019;54(14):2409–2419. doi: 10.1080/10826084.2019.1653324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull G., Major E., Harless C., Zule W., Ostrach B., Carpenter D. Rural community pharmacist willingness to dispense suboxone® - a secret shopper investigation in South-Central appalachia. Explor. Res. Clin. Soc. Pharm. 2021;4 doi: 10.1016/j.rcsop.2021.100082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2021. Practice guidelines for the administration of buprenorphine for treating opioid use disorder. https://www.federalregister.gov/documents/2021/04/28/2021-08961/practice-guidelines-for-the-administration-of-buprenorphine-for-treating-opioid-use-disorder (Accessed May 17, 2022)
- Walley A.Y., Alperen J.K., Cheng D.M., Botticelli M., Castro-Donlan C., Samet J.H., Alford D.P. Office-based management of opioid dependence with buprenorphine: clinical practices and barriers. J. Gen. Intern. Med. 2008;23(9):1393–1398. doi: 10.1007/s11606-008-0686-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werremeyer A., Mosher S., Eukel H., Skoy E., Steig J., Frenzel O., Strand M.A. Pharmacists' stigma toward patients engaged in opioid misuse: when "social distance" does not mean disease prevention. Subst. Abus. 2021;42(4):919–926. doi: 10.1080/08897077.2021.1900988. [DOI] [PubMed] [Google Scholar]
- Winstanley E.L., Lander L.R., Berry J.H., Mahoney J.J., Zheng W., Herschler J., Marshalek P., Sayres S., Mason J., Haut M.W. West Virginia's model of buprenorphine expansion: preliminary results. J. Subst. Abuse Treat. 2020;108:40–47. doi: 10.1016/j.jsat.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]