Abstract
Background/Aim: Prior immune-checkpoint inhibitors, weekly paclitaxel-cetuximab was one of the few options for platinum-ineligible patients with recurrent/ metastatic squamous cell carcinoma of the head and neck (R/M-SCCHN). This real-world study analyzed the long-term outcomes of this regimen.
Patients and Methods: A multicenter, retrospective, observational, cross-sectional, chart review study was realized in nine hospitals of the Galician Group of Head and Neck Cancer. Eligible population was adult platinum-ineligible patients with R/M SCCHN (unfit to, or after progressing following EXTREME or other platinum-based regimens) that received weekly paclitaxel plus cetuximab regimen as first- or second-line (1L or 2L) between January 2009 and December 2014. The efficacy was evaluated (1L-2L) in regards to overall survival (OS) and progression-free survival (PFS), and safety was assessed as the incidence of adverse events (AEs).
Results: Seventy-five R/M-SCCHN patients received the scheme (1L, n=50; 2L: n=25). The mean age of the patients was 59 years (1L, 59.5 years; 2L, 59.2 years), 90% were male (1L, 96%; 2L, 79%), 55% were smokers (1L, 60.4%; 2L, 45.8%), and 61% presented ECOG performance status (PS) 1 (1L, 54%; 2L, 62.5%). Median OS [interquartile range (IQR)] was 8.85 (4.22-40.96) months. Median PFS (IQR) was 8.5 (3.93-12.55) (1L) and 8.8 (5.62-16.91) (2L) months. Disease control rate was 60% (1L) and 85% (2L). Weekly paclitaxel-cetuximab was well tolerated in 1L/2L (cutaneous-toxicity, mucositis, neuropathy; mainly Grade 1-2). No grade 4 AEs were notified in 2L.
Conclusion: Weekly paclitaxel-cetuximab is an active and well tolerated therapeutical option in platinum-ineligible or after platinum regimens in R/M-SCCHN patients.
Keywords: Cetuximab-paclitaxel, first- and second-line of treatment, recurrent/metastatic squamous cell carcinoma of the head and neck, real world data, non-candidates to platinum
Squamous cell carcinoma of the head and neck (SCCHN) occupies the sixth position in the ranking of common cancer diseases, with 890,000 new cases and 450,000 deaths in 2018 (1). Many patients with SCCHN present advanced locoregional disease (stage III/IV) and more than 50% have recurrence or metastatic (R/M) disease in the following 3 years (2,3). The prognosis of R/M SCCHN is poor with a median overall survival (OS) of about 10-12 months (4).
Until the emergence of immune checkpoint inhibitors, the EXTREME regimen (Cetuximab added to chemotherapy consisting of fluorouracil plus platinum) was the first-line standard of care for inoperable R/M SCCHN (5,6). Not all patients were candidates for this scheme due to different toxicities (gastrointestinal, renal, neurological), mainly related to high dose of platinum, which make it not a suitable alternative for unfit patients (generally with poor physical condition), and logistic problems due to scheme itself (7).
The population of patients not candidates to platinum [comorbidities, early progression after radical radio-chemotherapy in locally advanced disease, poor ECOG performance status (PS) or progression after a first line (1L) with platinum] were poorly represented in the scientific literature. There was no standard treatment for this population at the time this study was conducted.
In Spain, the regimen commonly used for R/M SCCHN patients who were not candidates to standard treatment (EXTREME chemotherapy) was the one reported by Hitt et al. (8). It consists of weekly paclitaxel plus cetuximab and has shown activity [overall response rate (ORR) of 54% and disease control rate (DCR) of 80%] and well tolerance (8). Moreover, this scheme has been used for patients who presented a primary progression during or following the EXTREME treatment and lacked a standard treatment (8,9).
Nowadays, the weekly paclitaxel plus cetuximab treatment is gaining importance as a possible second-line (2L) therapy in patients that progress to 1L combination of immunotherapy and platinum based-chemotherapy.
To increase the real-world evidence of the weekly scheme of paclitaxel plus cetuximab in R/M SCCHN patients not eligible for the platinum scheme [unfit patients or with progression disease (PD) after platinum-based chemotherapy] we carried out a chart review study. This study was designed to investigate the long-term outcomes (activity and tolerance) of weekly paclitaxel plus cetuximab; additionally, we discuss our results in comparison with previously published data regarding this scheme and the EXTREME regimen (7), considering that the populations are not comparable.
Patients and Methods
Study design. This is a multicenter, retrospective, observational, cross-sectional, chart review study carried out in nine hospitals belonging to the Galician Group of Head and Neck (GGCC, for its acronym in Spanish) from the northwest of Spain (Galicia).
Investigators screened their medical records to identify the eligible population: adult platinum-ineligible patients with R/M SCCHN (unfit to, or after progressing following treatment with EXTREME or other platinum-based regimens) that received the weekly paclitaxel plus cetuximab regimen as 1L or 2L between January 2009 and December 2014.
Demographic and clinical data were collected retrospectively from the electronic patient records (from January 2015 to June 2015) and analyzed in October 2020.
Treatment. The treatment regimen consisted of cetuximab 500 mg/m2 administered initially intravenously (IV) over 2 h, followed by weekly doses of 250 mg/m2 over 1 h and paclitaxel 80 mg/m2 administered weekly over 1 h after cetuximab infusion. It was administered in platinum-ineligible patients, as 1L in unfit patients to platinum-based regimen (EXTREME or other schemes) and as 2L in patients progressing after a platinum-based chemotherapy. Treatment was administered until PD, unacceptable toxicity, or patient/physician decision. All patients received prophylactic dexamethasone (10 mg IV) and diphenhydramine (50 mg IV) before cetuximab, and cimetidine (300 mg IV) or ranitidine (50 mg IV) before paclitaxel.
Variables. Tumor response was assessed after the start of treatment until PD, using investigator assessment based on computed tomography (CT) scan or magnetic resonance imaging (MRI), according to RECIST criteria (10).
OS was as the time from treatment initiation until death, and progression-free survival (PFS) in 1L and 2L was considered the time from the first cycle of therapy until progression. The follow-up time for OS and PFS, regardless of the line of therapy (1L or 2L), was defined as time from the diagnosis until the last visit.
Safety. The incidence of adverse events (AEs) was evaluated using the Common Terminology Criteria for Adverse Events (CTCAE) version 5.0.
Statistical analysis. Variables were described using summary statistics, such as counts, mean, standard deviation (SD), median, minimum, maximum, and 25th and 75th percentiles for continuous variables and counts and percentages for categorical variables.
The Kaplan–Meier method was used to estimate survival, and the log-rank method was used to compare survival curves. A proportional hazards model was also fitted to evaluate the possible effect of variables on risks.
Data management and statistical analysis was carried out with STATA 17 (Stata Statistical Software Release 17, StataCorp LLC, College Station, TX, USA).
Results
Patients. We identified and included in the study 75 R/M SCCHN patients who had received weekly paclitaxel plus cetuximab regimen: 50 patients were ineligible to receive platinum-based chemotherapy (EXTREME or other schemes) and received the treatment in 1L, and 25 patients had progressed following a platinum-based chemotherapy and received the treatment in 2L.
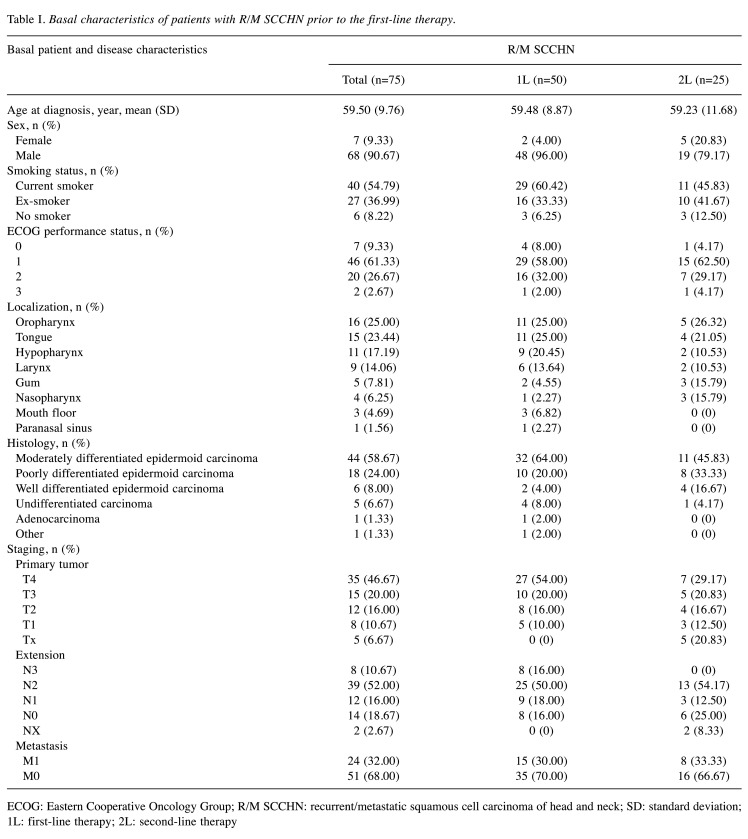
Overall, the mean age of the included patients was 59 years (1L, 59.5 years; 2L, 59.2 years), 90% were male (1L, 96%; 2L, 79%), 55% were smokers (1L, 60.4%; 2L, 45.8%), and 61% presented ECOG PS 1 (1L, 54%; 2L, 62.5%). The demographic characteristics of the population [overall and stratified by the line they received the weekly paclitaxel plus cetuximab regimen (1L or 2L)] are summarized in Table I.
Table I. Basal characteristics of patients with R/M SCCHN prior to the first-line therapy.
ECOG: Eastern Cooperative Oncology Group; R/M SCCHN: recurrent/metastatic squamous cell carcinoma of head and neck; SD: standard deviation; 1L: first-line therapy; 2L: second-line therapy
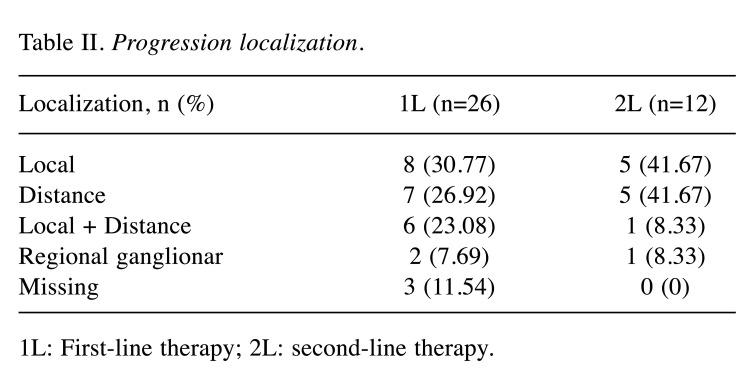
Efficacy. Around 50% of the patients progressed to weekly paclitaxel plus cetuximab in each line (26/50 patients in 1L and 12/25 patients in 2L). In both lines, local progression was the most common, followed by distant progression. Progression localization in both lines is summarized in Table II.
Table II. Progression localization.
1L: First-line therapy; 2L: second-line therapy.
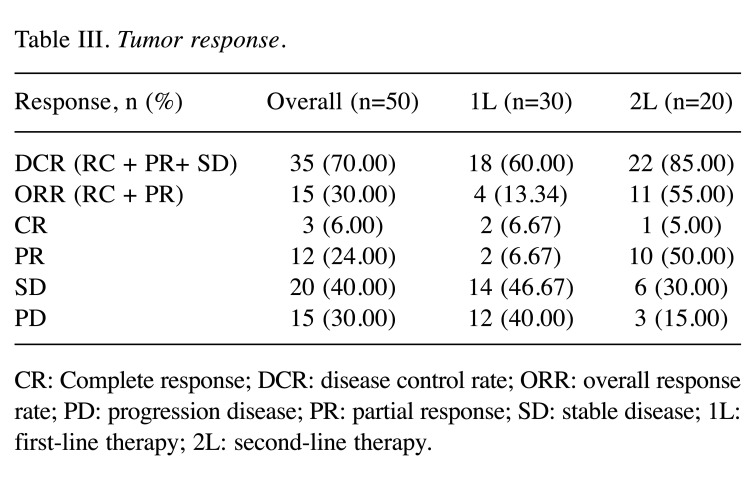
In the overall population, the median OS was 8.85 months (IQR=4.22-40.96 months) (Figure 1A), with an ORR of 30.0%, complete response (CR) rate of 6.0%, and partial response (PR) rate of 24.0%; the DCR was 70.0% (Table III).
Figure 1. Overall survival with weekly paclitaxel plus cetuximab. A) in overall population; B) in patients receiving the scheme as first line (1L) and C) in patients receiving the scheme as second line (2L).
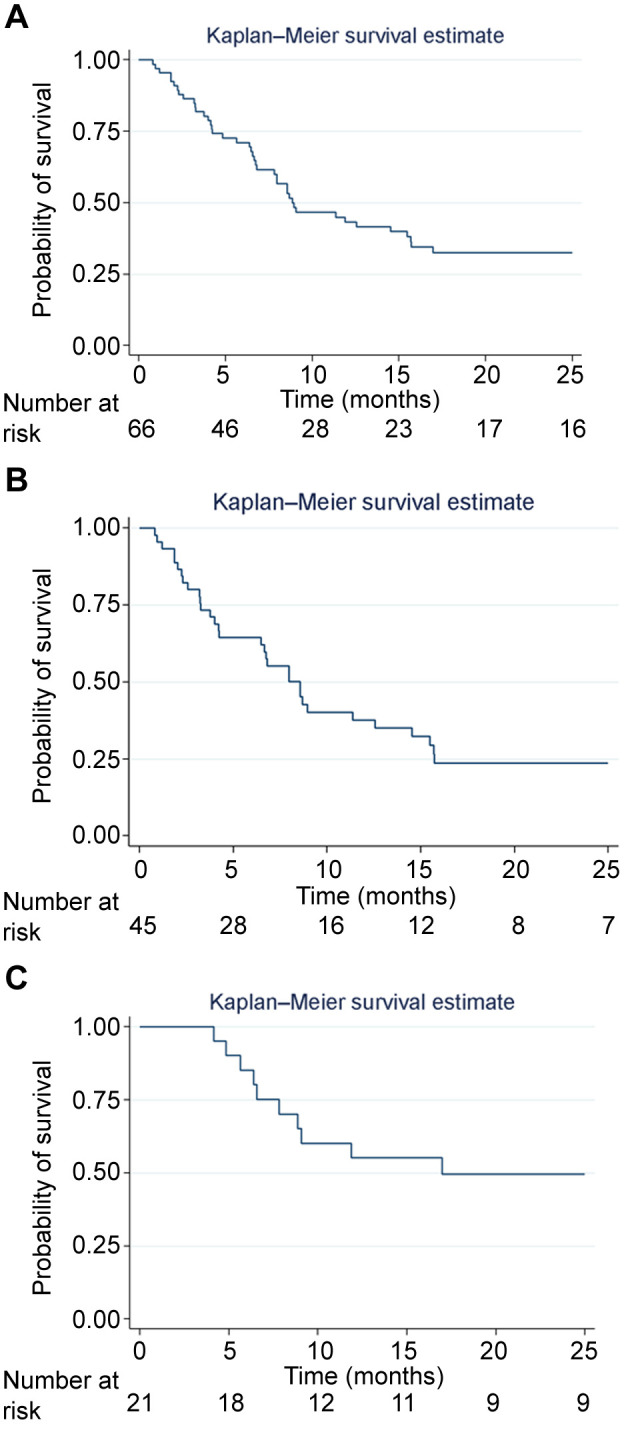
Table III. Tumor response.
CR: Complete response; DCR: disease control rate; ORR: overall response rate; PD: progression disease; PR: partial response; SD: stable disease; 1L: first-line therapy; 2L: second-line therapy.
In patients receiving weekly paclitaxel plus cetuximab in 1L, the ORR was 13.4%, with a CR rate of 6.7%, a PR rate of 6.7%, and a DCR rate of 60% (Table III); 20 patients were not evaluable due to comorbidities, treatment toxicity, and poor status, or they did not receive enough treatment to be evaluated (first response assessment). The median PFS (1L) was 8.55 months (IQR=3.93-12.55 months) (Figure 2A), with a median OS of 8.55 months (IQR=3.26-15.71 months) (Figure 1B).
Figure 2. Progression-free survival with weekly paclitaxel plus cetuximab A) in first line and B) in second line.
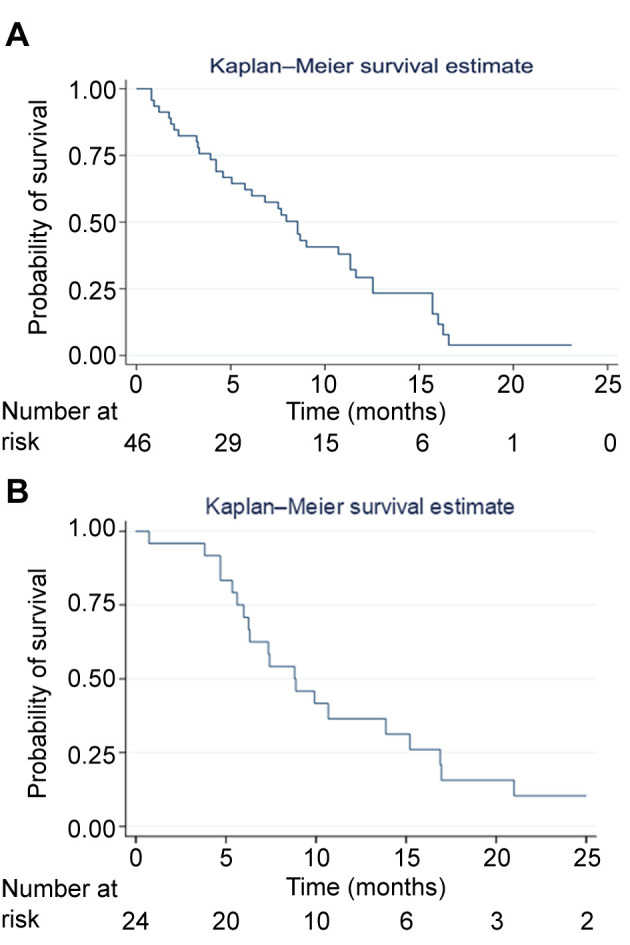
In patients treated with weekly paclitaxel plus cetuximab in 2L (5 patients were not evaluable), the ORR was 55.0%, with a CR rate of 5.0%, a PR rate of 50.0% and a DCR of 85.0% (Table III). The median PFS (2L) was 8.82 months (IQR=5.62-16.91 months) (Figure 2B), with a median OS of 16.97 months (IQR=7.82-47.32 months) (Figure 1C).
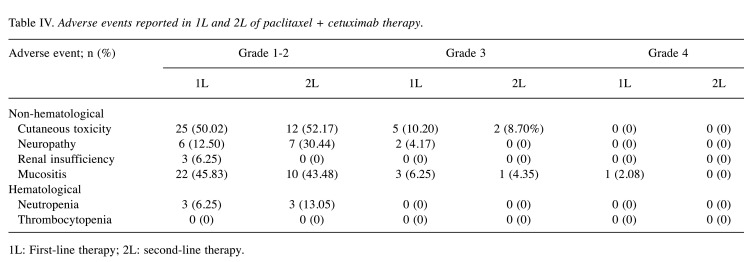
Safety. The list of AEs is shown in Table IV. Grade 1-2 AEs were reported with paclitaxel + cetuximab in both lines (1L and 2L). The most common AE was mucositis, followed by cutaneous toxicity and neuropathy.
Table IV. Adverse events reported in 1L and 2L of paclitaxel + cetuximab therapy.
1L: First-line therapy; 2L: second-line therapy.
All the hematological AEs reported were grade 1-2; all of them were neutropenia (range=2.08-8.70%) both in 1L and 2L. There were no events of thrombocytopenia.
Regarding grade 3-4 AEs, the most common were mucositis and cutaneous toxicity, which were reported in both lines (1L and 2L). Mucositis (2.08%) was the only grade 4 AE described; it was reported in 1L of paclitaxel + cetuximab. No grade 4 AEs were notified in 2L.
Discussion
The results of this study showed that the combination of weekly paclitaxel plus cetuximab is an active therapeutical option in R/M SCCHN as 1L in ineligible (unfit and poor prognosis) patients for the EXTREME standard therapy and other platinum-based regimens, and in 2L in patients who had progressed during 1L platinum-based chemotherapy. These results are interesting because they add to the evidence about this scheme (11,12) in this category of patients for whom very few treatment options were eligible at the time (9). Nowadays, this combination has regained value as 2L following 1L immunotherapy as monotherapy or in combination with platinum-containing schemes or after a platinum treatment. We present the results of our previous daily clinical practice in unfit and poor prognosis patients with the intention of providing external validity to this scheme.
Our study showed a median global OS of 8.85 months, with a median PFS of 8.5 in 1L. Our results in 1L are better than those presented in similar populations receiving the same regimen (weekly paclitaxel plus cetuximab) as 1L treatment (5,7,8); it doubled the PFS (5,8) with similar OS outcomes (8). Obviously, these studies are not completely comparable. In the phase II trial carried out by Hitt et al. in 2012 (8) this treatment was assessed as 1L in R/M SCCHN patients non-candidates for platinum or who had received platinum-containing chemotherapy as part of an induction, concomitant or adjuvant treatment if it was completed >6 months before study entry (34.7% of the overall population). The Karnofsky PS was between 70%-80% in 61% of patients. The efficacy outcomes showed a PFS of 4.2 months, an OS of 8.1 months, and a DCR of 80% (8). One of the reasons that could explain our longer PFS and OS compared with these results is that our study was conducted in a different period of time, when more knowledge (AEs management, treatment dose management, etc.) was available regarding this scheme. Although in our study the patients in 1L were platinum-naïve, their poor prognostic profile and comorbidities led to a lower survival compared to patients eligible for standard therapy as shown by our high rate of non-evaluable patients with regard to the response in 1L.
Other retrospective studies based on this scheme include the one carried out by Jimenez et al. in 2013 (12). This study included R/M SCCHN patients treated with weekly paclitaxel plus cetuximab and showed a median of PFS of 5.4 months and OS of 9.1 months. In the case of the retrospective study reported by Bernard et al. in 2017 (11), the results were similar to ours although with a more fit population (69.6% of patients had received platinum-containing >6 months before study entry). Another more recent retrospective study carried out by Fushimi et al. in 2020 (13) showed slightly worse outcomes than ours (median PFS of 5.7 months, and OS of 11.8 months, DCR of 73%) with an older population but with better ECOG PS.
However, in the study of Motai et al. (5) in 2021, carried out in the immunotherapy era, data of R/M SCCHN patients treated with weekly paclitaxel plus cetuximab versus EXTREME regimen (only in 1L setting) were collected retrospectively. Similar results were observed in both schemes. In this study the age of the population (1L) was slightly higher (+8 years in both arms) than that of the population analyzed in our study (mean 59.5 years) and may be because of this age difference their survival results were a little worse than ours. The 1-year OS rate for paclitaxel plus cetuximab reported by Motai et al. (5) was 34% (95%CI=14.5–22.1), being slightly higher in the platinum-refractory vs. platinum-intolerant patients (39.5% vs. 33.3%). The opposite was observed for the 1-year PFS rate, which was higher in platinum-intolerant patients (22.2% vs. 13.6% in platinum-refractory patients). Jimenez et al. (12) treated R/M SCCHN patients with weekly paclitaxel plus cetuximab and showed that the patient platinum status (refractory or sensitive) did not influence PFS and OS (no differences in survival rates). This showed that weekly paclitaxel plus cetuximab has a comparable impact on survival in R/M SCCHN patients in which platinum is not indicated (5) and moreover, this scheme is active regardless of the platinum status (12).
Despite our survival results (OS, PFS) are better than those previously published with the same scheme (paclitaxel plus cetuximab), our tumor responses in 1L [ORR (13.3%) and DCR (60.0%)] were slightly lower than those previously published with paclitaxel plus cetuximab (7-9,11,12) and the EXTREME scheme (6,9,14). Despite the low ORR found in our study, the scheme of weekly paclitaxel plus cetuximab showed disease control, as improved PFS was obtained. Furthermore, this scheme provides clinical benefits in a high percentage of patients even though these patients being unfit and presented poor prognosis, and it was similar to those that received the standard treatment.
Regarding the weekly paclitaxel plus cetuximab as 2L treatment, it is interesting to note that the observed PFS was the same regardless the line of therapy [PFS (median) 1L, 8.55 months or PFS (median) 2L, 8.82 months] and better (double) than the PFS of those patients who progressed in the EXTREME scheme as previously published (7,8,15). It could be because weekly paclitaxel plus cetuximab is an active scheme despite prior exposure to platinum, as revealed by Jimenez et al. (12).
In concordance with the previously published results reported with paclitaxel plus cetuximab (15,16), the tumor response we observed in 2L in patients who progressed in the EXTREME therapy or in other schemes based on platinum in 1L was better than that in 1L (platinum ineligible patients), showing ORR of 55.0% and DCR of 85.0%. Both tumor response and PFS achieved in 2L treatment are relevant outcomes because patients who achieve a response (PR or SD) have better clinical benefit regarding survival and quality of life (17), corroborating the suitability of this scheme administrated as 2L in patients progressing in the immunotherapy and platinum based-chemotherapy.
Regarding the positioning of weekly paclitaxel plus cetuximab as a 2L scheme in the immunotherapy era, Suzuki et al. (18) published in 2021 a study using this regimen in eighteen R/M HNSCC patients after progression following immune checkpoint inhibitor (ICI) therapy. This study showed a median PFS and OS of 3.8 months and 9.6 months, respectively (18). In this sense, Sato et al. (19) in a retrospective study in patients with R/M head and neck cancer showed that the sequential treatment with anti-PD-1 therapy followed by paclitaxel-based chemotherapy could be a good strategy to maximize the efficacy of chemotherapy in this type of patients. They found a significant difference in the ORR between paclitaxel plus cetuximab administered before and after nivolumab [17% vs. 70% (p=0.027)]. Similarly, TTP was significantly longer after nivolumab than before nivolumab (7.4 months; 4.9 months, p=0.020). These results are interesting because these patients are the ones that we will encounter in the immediate future and suggest an optimized sequence strategy.
The safety profile of the weekly paclitaxel plus cetuximab regimen we observed was as expected (5,7-9,15,20,21). It was well tolerated with most of the AEs reported being grade 1-2. Mucositis, cutaneous toxicity (both related to cetuximab) (22) and neuropathy were the main AEs (grade 1-3); only mucositis was grade 4 (in 1L). Neutropenia was the only hematological AE observed; all cases were grade 1-2 (<10%).
Due to its well tolerance, that our results corroborate, the weekly paclitaxel plus cetuximab scheme has been considered as a good option for fragile patients who present alimentary problems and poor general condition (16). Therefore, it entails an optimal option for patients progressing to platinum combination or/and immunotherapy in which there are few therapeutic options after 1L.
The safety of weekly paclitaxel plus cetuximab scheme has not been compared with that of other schemes, our results show that it is better tolerated from the standard of care (EXTREME) (5,6) of chemotherapy in R/M HNSCC patients and should be considered as an option for patients in whom the potential toxicity of current standard regimens may be a limiting factor.
Our results suggest the weekly paclitaxel plus cetuximab regimen as the best salvage therapy option (4,23). This is also because there is no established standard 2L therapy, as the treatment is mainly palliative (24) and these patients have very poor prognosis with a low response rate and short survival (25). Paclitaxel and cetuximab have also been shown to maintain high efficacy and acceptable safety for R/M HNSCC that progressed after immune checkpoint inhibitor therapy (18).
Limitations. The main limitation of the study is the scarce evidence regarding the use of this regimen in the historic context in which it was applicable. Furthermore, the study is retrospective with a small patient population.
Another important limitation is that at the time the data were collected there was no available immunotherapy. Therefore, the results are not exactly extrapolable to the current treatment situation where there are regimens that include immunotherapy in 1L or schemes based on immunotherapy in 2L.
Conclusion
Our study supports the use of weekly paclitaxel plus cetuximab as first-line treatment in unfit (not candidates to platinum) and poor prognosis R/M-SCCHN patients showing similar disease control than standard treatment and competitive survival outcomes. Moreover, weekly paclitaxel plus cetuximab is an attractive option in second-line owing to its good efficacy outcomes in R/M-SCCHN patients who relapse after platinum-based chemotherapy and/or immunotherapy. The safety profile is well tolerated and manageable; this makes this scheme a renewed therapeutical option for these different groups of patients.
Conflicts of Interest
The Authors declare that there are no conflicts of interest regarding the publication of this article.
Authors’ Contributions
Aguín S, and Medina A were the guarantors, and designed the study and drafted of the manuscript; Carral A, Covela M, Iglesias I, García Gómez J, Pena C, Costa M, García Arroyo R, Huidobro G and Vilches Simo R participated in the acquisition, analysis, and interpretation of the data; Aguín S and Medina A revised the article critically for important intellectual content and written the final versions of the manuscript.
Acknowledgements
The Authors thank Jorge Ruiz (Mixestat, Barcelona) and Sergio Alonso-Orgaz and Pilar López (Lidesec, Madrid) for their assistance in data analysis, visualization and writing and editing the manuscript. Medical writing was funded by Merck, S. L.U.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–1953. doi: 10.1002/ijc.31937. [DOI] [PubMed] [Google Scholar]
- 2.Adelstein DJ, Li Y, Adams GL, Wagner H Jr, Kish JA, Ensley JF, Schuller DE, Forastiere AA. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol. 2003;21(1):92–98. doi: 10.1200/JCO.2003.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, Peters G, Lee DJ, Leaf A, Ensley J, Cooper J. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med. 2003;349(22):2091–2098. doi: 10.1056/NEJMoa031317. [DOI] [PubMed] [Google Scholar]
- 4.Sacco AG, Cohen EE. Current treatment options for recurrent or metastatic head and neck squamous cell carcinoma. J Clin Oncol. 2015;33(29):3305–3313. doi: 10.1200/JCO.2015.62.0963. [DOI] [PubMed] [Google Scholar]
- 5.Motai R, Sawabe M, Kadowaki S, Sasaki E, Nishikawa D, Suzuki H, Beppu S, Terada H, Hanai N. Clinical impact of weekly paclitaxel plus cetuximab is comparable to the EXTREME regimen for recurrent/metastatic head and neck squamous cell carcinoma. Int J Clin Oncol. 2021;26(7):1188–1195. doi: 10.1007/s10147-021-01907-x. [DOI] [PubMed] [Google Scholar]
- 6.Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, Erfan J, Zabolotnyy D, Kienzer HR, Cupissol D, Peyrade F, Benasso M, Vynnychenko I, De Raucourt D, Bokemeyer C, Schueler A, Amellal N, Hitt R. Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med. 2008;359(11):1116–1127. doi: 10.1056/NEJMoa0802656. [DOI] [PubMed] [Google Scholar]
- 7.Nakano K, Marshall S, Taira S, Sato Y, Tomomatsu J, Sasaki T, Shimbashi W, Fukushima H, Yonekawa H, Mitani H, Kawabata K, Takahashi S. A comparison of weekly paclitaxel and cetuximab with the EXTREME regimen in the treatment of recurrent/metastatic squamous cell head and neck carcinoma. Oral Oncol. 2017;73:21–26. doi: 10.1016/j.oraloncology.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 8.Hitt R, Irigoyen A, Cortes-Funes H, Grau JJ, García-Sáenz JA, Cruz-Hernandez JJ, Spanish Head and Neck Cancer Cooperative Group (TTCC) Phase II study of the combination of cetuximab and weekly paclitaxel in the first-line treatment of patients with recurrent and/or metastatic squamous cell carcinoma of head and neck. Ann Oncol. 2012;23(4):1016–1022. doi: 10.1093/annonc/mdr367. [DOI] [PubMed] [Google Scholar]
- 9.Enokida T, Okano S, Fujisawa T, Ueda Y, Uozumi S, Tahara M. Paclitaxel plus cetuximab as 1st line chemotherapy in platinum-based chemoradiotherapy-refractory patients with squamous cell carcinoma of the head and neck. Front Oncol. 2018;8:339. doi: 10.3389/fonc.2018.00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bogaerts J, Ford R, Sargent D, Schwartz LH, Rubinstein L, Lacombe D, Eisenhauer E, Verweij J, Therasse P, RECIST Working Party Individual patient data analysis to assess modifications to the RECIST criteria. Eur J Cancer. 2009;45(2):248–260. doi: 10.1016/j.ejca.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 11.Bernad IP, Trufero JM, Urquizu LC, Pazo Cid RA, de Miguel AC, Agustin MJ, Lanzuela M, Antón A. Activity of weekly paclitaxel-cetuximab chemotherapy in unselected patients with recurrent/metastatic head and neck squamous cell carcinoma: prognostic factors. Clin Transl Oncol. 2017;19(6):769–776. doi: 10.1007/s12094-016-1604-z. [DOI] [PubMed] [Google Scholar]
- 12.Jiménez B, Trigo JM, Pajares BI, Sáez MI, Quero C, Navarro V, Llácer C, Medina L, Rueda A, Alba E. Efficacy and safety of weekly paclitaxel combined with cetuximab in the treatment of pretreated recurrent/metastatic head and neck cancer patients. Oral Oncol. 2013;49(2):182–185. doi: 10.1016/j.oraloncology.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Fushimi C, Baba D, Masubuchi T, Yamazaki M, Kitani Y, Kitajima T, Tanaka J, Hanyu K, Tanaka N, Miura K, Tada Y. Weekly cetuximab and paclitaxel for recurrent or metastatic head and neck squamous cell carcinoma. In Vivo. 2020;34(5):2653–2657. doi: 10.21873/invivo.12084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Mello RA, Gerós S, Alves MP, Moreira F, Avezedo I, Dinis J. Cetuximab plus platinum-based chemotherapy in head and neck squamous cell carcinoma: a retrospective study in a single comprehensive European cancer institution. PLoS One. 2014;9(2):e86697. doi: 10.1371/journal.pone.0086697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Péron J, Ceruse P, Lavergne E, Buiret G, Pham BN, Chabaud S, Favier B, Girodet D, Zrounba P, Ramade A, Fayette J. Paclitaxel and cetuximab combination efficiency after the failure of a platinum-based chemotherapy in recurrent/metastatic head and neck squamous cell carcinoma. Anticancer Drugs. 2012;23(9):996–1001. doi: 10.1097/CAD.0b013e32835507e5. [DOI] [PubMed] [Google Scholar]
- 16.Sosa AE, Grau JJ, Feliz L, Pereira V, Alcaraz D, Muñoz-García C, Caballero M. Outcome of patients treated with palliative weekly paclitaxel plus cetuximab in recurrent head and neck cancer after failure of platinum-based therapy. Eur Arch Otorhinolaryngol. 2014;271(2):373–378. doi: 10.1007/s00405-013-2537-6. [DOI] [PubMed] [Google Scholar]
- 17.Constenla DO, Hill ME, A’Hern RP, Henk JM, Rhys-Evans P, Breach N, Archer D, Gore ME. Chemotherapy for symptom control in recurrent squamous cell carcinoma of the head and neck. Ann Oncol. 1997;8(5):445–449. doi: 10.1023/a:1008203613364. [DOI] [PubMed] [Google Scholar]
- 18.Suzuki S, Toyoma S, Kawasaki Y, Koizumi K, Iikawa N, Shiina K, Endo T, Abe T, Kouga T, Yamada T. Clinical outcomes of cetuximab and paclitaxel after progression on immune checkpoint inhibitors in recurrent or metastatic head and neck squamous cell carcinoma. Medicina (Kaunas) 2021;57(11):1151. doi: 10.3390/medicina57111151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sato Y, Fukuda N, Fujiwara YU, Wang X, Urasaki T, Ohmoto A, Nakano K, Ono M, Tomomatsu J, Mitani H, Takahashi S. Efficacy of paclitaxel-based chemotherapy after progression on nivolumab for head and neck cancer. In Vivo. 2021;35(2):1211–1215. doi: 10.21873/invivo.12371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Okada T, Okamoto I, Sato H, Ito T, Miyake K, Tsukahara K. Efficacy and safety of paclitaxel combined with cetuximab for head and neck squamous cell carcinoma. In Vivo. 2021;35(2):1253–1259. doi: 10.21873/invivo.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sparano JA, Wang M, Martino S, Jones V, Perez EA, Saphner T, Wolff AC, Sledge GW Jr, Wood WC, Davidson NE. Weekly paclitaxel in the adjuvant treatment of breast cancer. N Engl J Med. 2008;358(16):1663–1671. doi: 10.1056/NEJMoa0707056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taberna M, Oliva M, Mesía R. Cetuximab-Containing Combinations in Locally Advanced and Recurrent or Metastatic Head and Neck Squamous Cell Carcinoma. Front Oncol. 2019;9:383. doi: 10.3389/fonc.2019.00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cramer JD, Burtness B, Ferris RL. Immunotherapy for head and neck cancer: Recent advances and future directions. Oral Oncol. 2019;99:104460. doi: 10.1016/j.oraloncology.2019.104460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Büntzel J, Micke O. Second-line chemotherapy in head and neck cancer: what should we expect. Expert Rev Anticancer Ther. 2009;9(3):269–273. doi: 10.1586/14737140.9.3.269. [DOI] [PubMed] [Google Scholar]
- 25.León X, Hitt R, Constenla M, Rocca A, Stupp R, Kovács AF, Amellal N, Bessa EH, Bourhis J. A retrospective analysis of the outcome of patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck refractory to a platinum-based chemotherapy. Clin Oncol (R Coll Radiol) 2005;17(6):418–424. doi: 10.1016/j.clon.2005.02.014. [DOI] [PubMed] [Google Scholar]