Abstract
Background:
The impact of a physically demanding occupation on clinical outcomes after anterior cruciate ligament (ACL) reconstruction (ACLR) is largely unknown.
Purpose/Hypothesis:
The purpose of this study was to assess the influence of occupation on 12-month outcomes after ACLR in male patients. It was hypothesized that patients undertaking manual work would not only have better functional outcomes in terms of strength and range of motion but also higher rates of joint effusion and greater anterior knee laxity.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
From an initial cohort of 1829 patients, we identified 372 eligible patients aged 18 to 30 years who underwent primary ACLR between 2014 and 2017. Based on a preoperative self-assessment, 2 groups were established: patients engaged in heavy manual occupations and those engaged in low-impact occupations. Data were collected from a prospective database including effusion, knee range of motion (using side-to-side difference), anterior knee laxity, limb symmetry index for single hop and triple hop, International Knee Documentation Committee (IKDC) subjective score, and complications up to 12 months. Because of the significantly lower rate of female patients undertaking heavy manual occupations compared to low-impact occupations (12.5% and 40.0%, respectively), data analysis was focused on male patients. Outcome variables were assessed for normality, and statistical comparisons were made between the heavy manual and low-impact groups using either an independent-samples t test or the Mann-Whitney U test.
Results:
Of 230 male patients, 98 were included in the heavy manual occupation group, and 132 were included in the low-impact occupation group. Patients in the heavy manual occupation group were significantly younger than those in the low-impact occupation group (mean age, 24.1 vs 25.9 years, respectively; P < .005). There was a greater range of active and passive knee flexion in the heavy manual occupation group than in the low-impact occupation group (mean active, 3.38° vs 5.33°, respectively [P = .021]; mean passive, 2.76° vs 5.00°, respectively [P = .005]). There was no difference in effusion, anterior knee laxity, limb symmetry index, IKDC score, return-to-sport rate, or graft rupture rate at 12 months.
Conclusion:
At 12 months after primary ACLR, male patients engaged in heavy manual occupations had a greater range of knee flexion, with no difference in the effusion rate or anterior knee laxity, compared with those engaged in low-impact occupations.
Keywords: occupation, heavy manual work, anterior cruciate ligament (ACL) reconstruction, clinical outcomes, knee
There is an increasing incidence of anterior cruciate ligament (ACL) reconstruction (ACLR) being performed across all age groups, with a significant upward trend in young patients. 22,30,41 Surgery is typically indicated in younger athletes, those with persistent symptoms of instability, and patients who participate in high-demand recreational and occupational activities. 31,33 Patient satisfaction after ACLR is highly correlated with achieving symptom-free return of function, including activities of daily living, sport participation, and work-related tasks. 21
Return to sport after ACLR is often the main goal for young active patients and has been the focus of a large number of studies, which have explored the factors that impact this objective. 11,38 However, return to a high-demand occupation is also a common objective in this patient population, and working in a high-demand occupation has been judged to be a relative indication for ACLR in a survey of orthopaedic surgeons. 14 In contrast to sport participation, there is a relative paucity of literature about the effect of a high-demand occupation on outcomes after ACLR. Noyes et al 25 highlighted the importance of understanding the effect that occupation has on the knee, and consequently, an occupation component was incorporated in the Cincinnati Knee Rating System. 5 In addition to this, there has been significant work done in relation to biomechanical loading as a risk factor for knee abnormalities, with rates significantly increased with certain high-demand occupational factors such as heavy lifting, kneeling, and crawling. 1,4,12,13,35 It is reasonable to hypothesize that loads encountered during heavy manual work may place significant stress on the ACL-reconstructed knee, and as such, it is important to understand whether these activities affect outcomes after ACLR.
Pouderoux et al 28 assessed joint laxity and graft compliance during the first postoperative year and found that there was a gradual increase in both, suggesting a period of relative weakness of the graft between 1 and 9 months, with it taking greater than 9 months to stabilize. Patients are more likely to try to return to work earlier in their recovery if there are financial implications to a prolonged time away from work. 17 This is more readily achievable in patients with a low-impact occupation, and there are more challenges with heavy manual roles. 15 For high-demand occupations, this potentially puts significant stress on the ACL-reconstructed knee, and this may have an effect on recovery.
There is no consensus as to when patients should return to high-demand work after ACLR. 15,24,34,36,40 The reported time to return to full heavy manual duties after ACLR varies, with average times ranging from 3 to 8 months. 15,24,34,36,40 This generally constitutes a period of rehabilitation, during which loading is being increased, and is also a time when the graft is undergoing remodeling and is potentially vulnerable to repetitive trauma. 7,20,27 A manual job is likely to require more time, with intensive loads placed on the knee, and be a less controlled environment than a rehabilitation program.
The aim of this study was to assess the influence of occupation type on 12-month outcomes after ACLR. We hypothesized that heavy manual workers would not only have better functional outcomes in terms of strength and range of motion compared to sedentary workers but also greater anterior knee laxity and higher rates of joint effusion because of greater demands on the recovering knee.
Methods
Patient Selection
This study was a retrospective review of prospectively collected data obtained from an audit database at a private metropolitan orthopaedic knee clinic. A total of 1829 patients who underwent ACLR between 2014 and 2017 were identified from the database. The inclusion criteria for this study were patients aged 18 to 30 years who underwent primary ACLR using a hamstring tendon autograft (n = 1266). Patients were excluded based on the following criteria: not in the workforce at the time of surgery (eg, students, retired, or unemployed) (n = 558), no data on occupation (n = 115), previous contralateral ACL injury (n = 71), multiligamentous knee surgery (n = 12), and concomitant lateral extra-articular tenodesis (n = 5). Meniscal and chondral injuries and previous arthroscopic surgery on the contralateral knee were not exclusion criteria. There were thus 505 patients who satisfied the eligibility criteria. Of these, 133 did not attend a 12-month postoperative review, leaving an eligible cohort of 372 patients (Figure 1). Human research ethics committee approval was obtained for this study.
Figure 1.
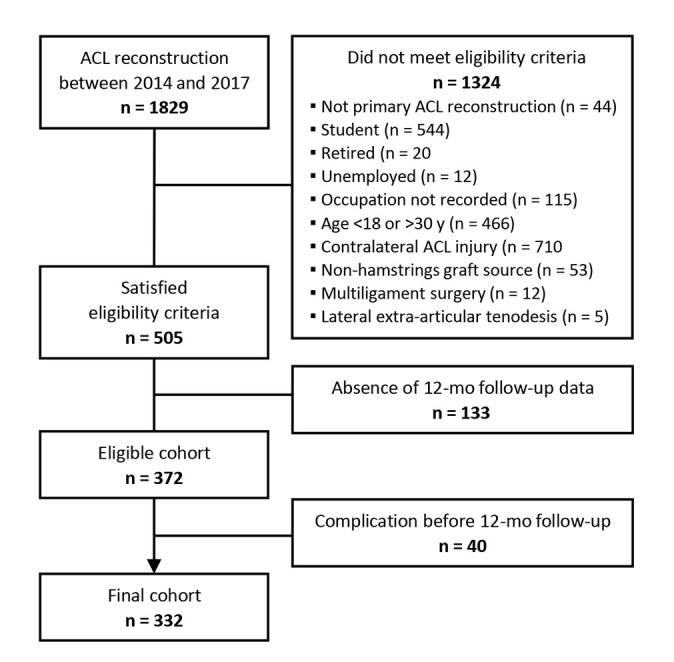
Flowchart of identified patients. ACL, anterior cruciate ligament.
Surgery and Rehabilitation
All patients underwent arthroscopically assisted single-bundle ACLR using a hamstring tendon autograft. All surgical procedures were performed by 1 of 4 fellowship-trained knee surgeons with a minimum of 10 years of experience. Suspensory fixation was used on the femoral side and interference screw fixation on the tibial side in all cases. The femoral tunnel was drilled via the anteromedial portal. Weightbearing as tolerated was allowed from the first postoperative day. All patients were encouraged to achieve full knee extension and regain quadriceps control early postoperatively. No braces or splints were used. The recommended time frame for return to work was 2 weeks for office-based work and up to 3 to 4 months for full heavy manual duties.
Data Collection
Information obtained from the database included demographic data (sex and age at the time of surgery), injury and surgical details, and return-to-sport rates at 12 months. All patients were asked to self-assess the physical demands of their occupation in a preoperative questionnaire, selecting from the discrete options of (1) heavy manual (majority of work involving lifting, climbing, kneeling, and repetitive heavy loads), (2) light manual (active occupation without repetitive heavy loads), (3) nonmanual but involving walking (requiring standing for prolonged periods and walking but no lifting or climbing), (4) nonmanual (sedentary occupation based outside of an office setting), (5) office (sedentary occupation based in an office setting), and (6) domestic (unpaid home duties). These categories were not defined by job title but rather self-determined based on the patient’s perception of his work type. There were 2 groups, heavy manual and low impact, established. The heavy manual group consisted of participants who selected option 1 on the preoperative questionnaire, and the low-impact group comprised those who selected options 2 through 6.
At 12 months postoperatively, patients completed the International Knee Documentation Committee (IKDC) subjective knee form 19 and underwent a physical assessment with a trained clinical assessor. The presence of knee effusion was assessed using the bulge test and quantified as none, small, moderate, or large. Range of motion was assessed using a goniometer with 60-cm arms. This included standing knee flexion as well as active and passive knee flexion measured in the lateral decubitus position, expressed as a side-to-side difference. Extension deficit was calculated based on the heel-height difference with the patient prone, as described by Sachs et al. 29 A KT-1000 arthrometer was used to quantify the side-to-side difference in anterior tibial translation, measured at both 67 and 134 N. The limb symmetry index (LSI) was calculated for the single and triple crossover hop for distance tests. Medical records were also reviewed to confirm any complications such as graft ruptures and infections or identify those who failed to complete the 12-month follow-up because of subsequent surgery on the ipsilateral knee or a contralateral ACL injury.
Statistical Analysis
All outcome variables were assessed for normality, and statistical comparisons were made between the heavy manual and low-impact occupation groups using either an independent-samples t test or the Mann-Whitney U test. When significant differences between the groups were identified, analysis of covariance was also performed, with age as the covariate, to determine whether the difference in age between groups was a contributing factor. Effect sizes (Cohen d) were calculated, with 0.2 indicating a small effect, 0.5 indicating a moderate effect, and 0.8 indicating a large effect. Significance was set at P < .05. All statistical analyses were performed using SPSS 27 (IBM Corp).
Results
Complete preoperative data were available on all patients. Of the 372 eligible patients, 40 sustained a complication (graft rupture, return to surgery, or infection) or contralateral ACL injury before 12 months and therefore did not complete a 12-month clinical review (Table 1). The final cohort for analysis consisted of 332 patients, with 112 undertaking a heavy manual occupation and 220 undertaking a low-impact occupation (Table 2).
Table 1.
Complications and Contralateral ACL Injuries Before 12 Months a
| Overall (n = 372) | Heavy Manual Occupation (n = 127) | Low-Impact Occupation (n = 245) | |
|---|---|---|---|
| Graft rupture | 19 (5.1) | 6 (4.7) | 13 (5.3) |
| Contralateral ACL injury | 2 (0.5) | 1 (0.8) | 1 (0.4) |
| Return to surgery | |||
| Meniscal lesion | 7 (1.9) | 3 (2.4) | 4 (1.6) |
| Cyclops lesion causing extension deficit | 9 (2.4) | 4 (3.2) | 5 (2.0) |
| Chondroplasty | 1 (0.3) | 0 (0.0) | 1 (0.4) |
| Infection | 2 (0.5) | 1 (0.8) | 1 (0.4) |
a Data are reported as n (%). ACL, anterior cruciate ligament.
Table 2.
Patient Demographics a
| Heavy Manual Occupation (n = 112) | Low-Impact Occupation (n = 220) | P Value | |
|---|---|---|---|
| Age at surgery, y | 24.3 ± 3.2 | 25.8 ± 3.2 | <.001 |
| Sex | <.001 | ||
| Male | 98 (87.5) | 132 (60.0) | |
| Female | 14 (12.5) | 88 (40.0) | |
| Body mass index, kg/m2 | 26.0 ± 3.8 | 25.0 ± 3.5 | N/S |
| Returned to sport at 12 mo | |||
| No | 38 (33.9) | 77 (35.0) | |
| Yes | 71 (63.4) | 139 (63.2) | |
| Nonsporting | 3 (2.7) | 4 (1.8) |
a Data are reported as mean ± SD or n (%). Boldface P values indicate a statistically significant difference between groups (P < .05).
Although we identified both male and female patients for eligibility, there were only 14 women of 112 patients (12.5%) in the heavy manual occupation group. This rate was significantly lower (P < .05) than the 40.0% (88/220) proportion of female representation in the low-impact occupation group (Table 2). In addition, patients in the heavy manual occupation group were significantly younger than those in the low-impact occupation group. There was no significant difference in body mass index between the 2 groups (Table 2).
As there were so few female participants involved in heavy manual work, the decision was made to split the cohort and analyze the male and female participants separately to minimize the effect of sex as a potential confounder. There was only 1 statistically significant difference in the female cohort, which was a greater passive flexion range in the low-impact occupation group (P = .023) (Appendix Table A1). The Results and Discussion sections will focus on the male cohort, which had good representation in both heavy manual and low-impact occupations.
Of 230 male patients, 98 were included in the heavy manual occupation group and 132 were included in the low-impact occupation group. Patients in the heavy manual occupation group were significantly younger than those in the low-impact occupation group (P < .005) (Table 3). Meniscal and chondral lesions found at index surgery are displayed in Table 3.
Table 3.
Demographics and Follow-up Information for Male Participants a
| Heavy Manual Occupation (n = 98) | Low-Impact Occupation (n = 132) | P Value | |
|---|---|---|---|
| Age at surgery, y | 24.1 ± 3.3 | 25.9 ± 3.2 | <.005 |
| Body mass index, kg/m2 | 26.0 ± 3.7 | 26.0 ± 3.0 | N/S |
| Medial meniscal injury and treatment | 23 (23.5) | 38 (28.8) | N/S |
| Stable tear, no surgery | 2 (2.0) | 5 (3.8) | N/S |
| Partial meniscectomy | 11 (11.2) | 23 (17.4) | N/S |
| Meniscal repair | 10 (10.2) | 10 (7.6) | N/S |
| Lateral meniscal injury and treatment | 44 (44.9) | 52 (39.4) | N/S |
| Stable tear, no surgery | 14 (14.3) | 19 (14.4) | N/S |
| Partial meniscectomy | 27 (27.6) | 30 (22.7) | N/S |
| Meniscal repair | 3 (3.1) | 3 (2.3) | N/S |
| Chondral lesion | 27 (27.6) | 43 (32.6) | N/S |
| Patella | 8 (8.2) | 5 (3.8) | N/S |
| Trochlear groove | 0 (0.0) | 3 (2.3) | N/S |
| Medial femoral condyle | 10 (10.2) | 16 (12.1) | N/S |
| Medial tibial plateau | 2 (2.0) | 3 (2.3) | N/S |
| Lateral femoral condyle | 3 (3.1) | 10 (7.6) | N/S |
| Lateral tibial plateau | 4 (4.1) | 6 (4.5) | N/S |
| Returned to sport at 12 mo | |||
| No | 35 (35.7) | 39 (29.5) | N/S |
| Yes | 60 (61.2) | 90 (68.2) | N/S |
| Training | 29 (29.6) | 43 (32.6) | N/S |
| Lower level | 8 (8.2) | 18 (13.6) | N/S |
| Same or higher level | 23 (23.5) | 29 (22.0) | N/S |
| Nonsporting | 3 (3.1) | 3 (2.3) | N/S |
a Data are reported as mean ± SD or n (%).
There was a higher proportion of high-level competitive and professional athletes in the heavy manual occupation group compared with the low-impact occupation group (n = 76 [77.6%] and n = 54 [40.9%], respectively). The return-to-sport rate at 12 months was slightly higher in the low-impact occupation group compared with that in the heavy manual occupation group (n = 90 [68.2%] and n = 60 [61.2%], respectively) (Table 3). For patients who returned to sport, the rates of return to preinjury levels were similar between the groups (Table 3).
There was no difference in the IKDC subjective score at 12 months between the 2 male groups (Table 4). Effusion rates were low and not significantly different between the 2 groups (Table 4). At 12 months, active and passive knee flexion deficits were significantly less in the heavy manual group compared with the low-impact group (Table 4). These remained significant when age was accounted for (active: P = .021; passive: P = .005), although the effect sizes for the differences were small to moderate (d = 0.3 and 0.4, respectively). The knee extension deficit was not significantly different between the heavy manual and low-impact groups (Table 4). There was no difference in anterior knee laxity between the 2 groups at either 67 or 134 N (Table 4). There was a mean side-to-side difference of <2 mm at 134 N. Both groups had LSIs averaging >90% for both the single and triple hops for distance. While the LSI for single hop was significantly better for the heavy manual group at 12 months (P = .031), when age was accounted for, this difference was no longer significant (P = .375) (Table 4).
Table 4.
Clinical Outcomes for Male Participants at 12 Months a
| Heavy Manual Occupation (n = 98) | Low-Impact Occupation (n = 132) | P Value | Cohen d | |
|---|---|---|---|---|
| IKDC score | 83.87 ± 13.00 | 84.78 ± 12.34 | .553 | |
| Effusion | .204 | |||
| No | 83 (84.7) | 103 (78.0) | ||
| Yes | 15 (15.3) | 29 (22.0) | ||
| Side-to-side difference with KT-1000 arthrometer | ||||
| 67 N | 0.70 ± 1.51 | 0.45 ± 1.51 | .365 | |
| 134 N | 1.08 ± 2.26 | 1.36 ± 2.49 | .219 | |
| Extension deficit | 1.47 ± 2.66 | 0.90 ± 2.51 | .241 | |
| Standing flexion difference, deg | 4.48 ± 6.57 | 4.84 ± 7.81 | .759 | |
| Active flexion difference, deg | 3.38 ± 5.99 | 5.33 ± 5.60 | .021 | 0.338 |
| Passive flexion difference, deg | 2.76 ± 5.90 | 5.00 ± 5.66 | .005 | 0.390 |
| Limb symmetry index, b % | ||||
| Single hop | 99.23 ± 10.37 | 96.31 ± 11.23 | .031 | 0.269 |
| Triple hop | 100.30 ± 14.53 | 97.28 ± 10.25 | .078 |
a Data are reported as mean ± SD or n (%). IKDC, International Knee Documentation Committee. Cohen d was only reported for those with a significant finding.
b The limb symmetry index showed moderate negative skewness and kurtosis (leptokurtic); however, transformation of the data did not normalize the distribution and given sample size of over 50 per group. This was not felt to affect the validity of performing analysis of covariance. 6
Discussion
The key finding of this study is that heavy manual occupations did not adversely affect the clinical outcome after ACLR, with both the heavy manual and low-impact groups achieving overall good clinical outcomes at 12 months. We report good strength in both groups, with a mean LSI for single hop of 99.23% in the heavy manual group and 96.31% in the low-impact group (P = .031), and no significant differences in the IKDC score (mean, 83.87 vs 84.78, respectively; P = .553). Importantly, the heavy manual group did not have an increased rate of effusion (15.3% vs 22.0%, respectively; P = .204) or greater anterior knee laxity (at 134 N: 1.08 vs 1.36, respectively; P = .219) than the low-impact group.
We did, however, find statistically significant differences in range of motion, with greater passive and active flexion in the heavy manual group. The improvement in flexion range detected in our cohort was small (<3°) and therefore unlikely to be clinically relevant, as both groups achieved an overall good range of motion. This finding may reflect that heavy manual workers may often be required to perform activities with a flexed knee (kneeling, crawling, squatting), and at times, these activities may be associated with carrying loads. Although Kocher et al 21 showed that the range of motion subscore of the IKDC score was significantly associated with patient satisfaction, they found the most powerful correlations between patient satisfaction and outcomes were subjective measures of function such as walking, squatting, and ascending or descending stairs without symptoms, which were positively associated with satisfaction after ACLR.
A premature return to high-demand activities and overly aggressive rehabilitation have been postulated as causes of graft laxity and failure after ACLR. 20 Heijne and Werner 16 compared the early and late introduction of open kinetic chain (OKC) quadriceps exercises after ACLR with a hamstring tendon autograft and found an increase in anterior knee laxity with OKC exercises introduced at 4 weeks postoperatively compared to a standard rehabilitation protocol. A review looking at ACL strain during weightbearing and nonweightbearing exercises identified that squatting forward with the heels off the ground, rising from kneeling, and stair climbing all increase strain and force on the ACL, similar to OKC knee extension exercises. 9 These are all activities that might be encountered in heavy manual occupations.
Increased rates of effusion have been reported in patients with higher demands placed on the knee both preoperatively and postoperatively. 18,23 Hughes et al 18 looked at blood flow restriction resistance training that utilized light external loads compared to traditional heavy load resistance training. They found greater rates of effusion and pain in the heavy load resistance training group. 18 In addition, a study looking at the role of postoperative bracing after ACLR showed that a high preinjury Tegner activity level was predictive of increased knee effusion at 3 and 12 months. 23
Our hypothesis was that anterior knee laxity would be greater in the heavy manual group because of the demands of manual labor on the ACL-reconstructed knee. However, despite having a greater range of motion, there was no increased laxity in the heavy manual group. Our hypothesis for the development and presence of effusion was based on a similar logic, but again, the heavy manual group did not demonstrate an increased frequency of effusion. This contrasts with the findings of Lindstrom et al, 23 who reported that patients with higher preoperative Tegner scores had higher rates of effusion at 3 and 12 months.
The IKDC subjective score was high in both groups, with a mean of 83.87 in the heavy manual group and 84.78 in the low-impact group (P = .553). Patient-reported outcome scores after ACLR in the literature are variable. 2,10,15,38,39 The MOON group examined a prospective cohort of 2340 patients who underwent ACLR, looking at modifiable predictors of clinical outcomes with a 2-year follow-up rate of 85%, and reported a median IKDC score of 75 at 2 years across all age groups. 32 Both the heavy manual and low-impact groups in our study demonstrated high IKDC scores at 12 months, with means of 84 and 85, respectively. This may reflect the fact that they were both young male groups, with both male sex and younger age having been previously associated with better subjective outcome scores. 37
The general advice given to patients in our cohort with high-demand occupations was that they could return to full duties at 3 to 4 months. Return-to-work time frames in the literature are variable. 15,24,34,36,40 A study by Obermeier et al 26 analyzed the achievement of functional milestones and demonstrated a mean return-to-work time of 2 weeks for medium/heavy occupations with an upper range of 3 months. This is significantly less time than most studies, but that study was limited by small numbers and the grouping of medium with heavy demand. 26 In contrast, Wexler et al 40 looked at ACLR in patients with workers’ compensation claims in which participants were not allowed to return to heavy-demand occupations until 4 to 6 months postoperatively, with all patients ultimately returning to work and 91% at the same or higher level than before the injury.
Although it was not a primary aim to investigate the association of occupation and return to sport, the 12-month return-to-sport rates were similar between the groups, with a slightly higher rate seen in the low-impact group. Overall, this is consistent with previous literature regarding return-to-sport rates at 12 months, acknowledging that it is an early time point at which to assess the return-to-sport rate and may not reflect the final return-to-sport rate. 3,11 Importantly, it is reassuring that despite participating in high-demand activities, the heavy manual group seemed to be achieving the goals of ACLR, such as being relatively symptom free, clinically stable, and able to participate in activities of daily living, work, and sport.
There were no differences in early graft rupture rates at 12 months between the groups. The graft rupture rate was 5.1% for the entire cohort. This is consistent with reported graft rupture rates at 12 months after ACLR with a hamstring tendon autograft for the age range of our cohort. 33 Further follow-up would be required to determine the longer term graft rupture rate after more patients have returned to higher demand sports.
Limitations
Our study has limitations because of its retrospective design and the nature of the questions asked at routine follow-up. Patients were not given specific parameters as to how to define their occupational demand. The challenge of categorizing work demands is a well-recognized issue in the occupational literature. 13,25 The use of occupational categories rather than job titles is preferred because of the high variation of occupational exposure patterns seen within the same occupation. 8,13 However, the use of self-reporting measures can lead to bias, as patients have the potential to either overestimate or underestimate the demands of their occupation or the performance of their work. In addition to this, we do not have an overall picture of the amount of loads being placed on the knee in each occupational group. It is possible that patients in either group who participated in high-level activities, such as sport, outside of work may have had superior outcomes, irrespective of their occupation. Although our study analyzed prospectively collected data, it was a retrospective analysis. We acknowledge that this creates an inherent weakness in terms of subtle baseline between-group differences. Because of the low number of female participants involved in heavy manual work in our cohort, we did not have a sufficient sample size to provide a meaningful assessment of the effects of heavy manual work in this subgroup of patients. These limitations highlight the need for a prospective study specifically designed to further assess the impact of return to work on clinical outcomes and to address these potential confounders.
Conclusion
Despite potentially increased demands on the recovering reconstructed knee, heavy manual workers fared just as well as low-impact workers with respect to subjective and objective clinical outcomes. Male patients engaged in heavy manual occupations had a slightly greater range of knee flexion but no difference in the effusion rate or in anterior knee laxity. These findings are reassuring and help to guide discussions between treating practitioners and patients engaged in heavy manual occupations.
APPENDIX
Appendix Table A1.
Clinical Outcomes for Female Participants at 12 Months a
| Heavy Manual Occupation (n = 14) | Low-Impact Occupation (n = 88) | P Value | Cohen d | |
|---|---|---|---|---|
| IKDC score | 85.37 ± 11.78 | 80.85 ± 14.16 | .249 | |
| Effusion | N/S | |||
| No | 12 (85.7) | 78 (88.6) | ||
| Yes | 2 (14.3) | 10 (11.4) | ||
| Side-to-side difference with KT-1000 arthrometer | ||||
| 67 N | 0.43 ± 1.87 | 0.70 ± 1.81 | .520 | |
| 134 N | 1.29 ± 2.34 | 1.78 ± 2.98 | .468 | |
| Extension deficit | –0.21 ± 3.34 | 1.22 ± 2.12 | .056 | |
| Standing flexion difference, deg | 6.50 ± 8.01 | 8.48 ± 8.56 | .316 | |
| Active flexion difference, deg | 8.07 ± 6.08 | 5.02 ± 5.77 | .074 | |
| Passive flexion difference, deg | 4.86 ± 4.13 | 2.49 ± 5.67 | .023 | 0.431 |
| Limb symmetry index, % | ||||
| Single hop | 92.84 ± 12.66 | 91.19 ± 12.92 | .586 | |
| Triple hop | 94.11 ± 11.06 | 93.01 ± 10.55 | .923 |
a Data are reported as mean ± SD or n (%). IKDC, International Knee Documentation Committee. Cohen d only reported for statistically significant findings.
Footnotes
Final revision submitted June 10, 2022; accepted August 7, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: T.S.W. has received research support from Smith & Nephew, consulting fees from Medacta, speaking fees from Medacta and Smith & Nephew, and royalties from Medacta. J.A.F. has received consulting fees from Smith & Nephew and is a paid associate editor for The Orthopaedic Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from La Trobe University (No. HEC19205).
References
- 1. Amin S, Goggins J, Nui J, et al. Occupation-related squatting, kneeling, and heavy lifting and the knee joint: a magnetic resonance imaging-based study in men. J Rheumatol. 2008;35(8):1645–1649. [PMC free article] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2011;39(3):538–543. [DOI] [PubMed] [Google Scholar]
- 4. Baker P. Knee disorders in the general population and their relation to occupation. Occup Environ Med. 2003;60(10):794–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati Knee Rating System in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am J Sports Med. 1999;27(4):402–416. [DOI] [PubMed] [Google Scholar]
- 6. Bedwell S. Applied Multivariate Statistics for the Social Sciences: Analyses with SAS and IBM’s SPSS by Keenan A. Pituch & James P. Stevens [review]. Psychologist. 2016. [Google Scholar]
- 7. Claes S, Verdonk P, Forsyth R, Bellemans J. The “ligamentization” process in anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(11):2476–2483. [DOI] [PubMed] [Google Scholar]
- 8. Eng A, ‘t Mannetje A, McLean D, et al. Gender differences in occupational exposure patterns. Occup Environ Med. 2011;68(12):888–894. [DOI] [PubMed] [Google Scholar]
- 9. Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. ACL strain and tensile forces for weight bearing and non–weight-bearing exercises after ACL reconstruction: a guide to exercise selection. J Orthop Sports Phys Ther. 2012;42(3):208–220. [DOI] [PubMed] [Google Scholar]
- 10. Failla MJ, Logerstedt DS, Grindem H, et al. Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction? Am J Sports Med. 2016;44(10):2608–2614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Feller J, Webster KE. Return to sport following anterior cruciate ligament reconstruction. Int Orthop. 2013;37(2):285–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Franklin J, Ingvarsson T, Englund M, Lohmander S. Association between occupation and knee and hip replacement due to osteoarthritis: a case-control study. Arthritis Res Ther. 2010;12(3):R102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fransen M, Agaliotis M, Bridgett L, Mackey MG. Hip and knee pain: role of occupational factors. Best Pract Res Clin Rheumatol. 2011;25(1):81–101. [DOI] [PubMed] [Google Scholar]
- 14. Grevnerts HT, Fältström A, Sonesson S, et al. Activity demands and instability are the most important factors for recommending to treat ACL injuries with reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2401–2409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Groot JAM, Jonkers FJ, Kievit AJ, Kuijer PPFM, Hoozemans MJM. Beneficial and limiting factors for return to work following anterior cruciate ligament reconstruction: a retrospective cohort study. Arch Orthop Trauma Surg. 2017;137(2):155–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):402–414. [DOI] [PubMed] [Google Scholar]
- 17. Hoorntje A, Kuijer PPFM, Van Ginneken BT, et al. Predictors of return to work after high tibial osteotomy: the importance of being a breadwinner. Orthop J Sports Med. 2019;7(12):232596711989005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hughes L, Rosenblatt B, Haddad F, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK National Health Service randomised controlled trial. Sports Med. 2019;49(11):1787–1805. [DOI] [PubMed] [Google Scholar]
- 19. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 20. Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):199–217. [DOI] [PubMed] [Google Scholar]
- 21. Kocher MS, Steadman JR, Briggs K, et al. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84(9):1560–1572. [DOI] [PubMed] [Google Scholar]
- 22. Lekkas C, Clarnette R, Graves SE, et al. Feasibility of establishing an Australian ACL registry: a pilot study by the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1510–1516. [DOI] [PubMed] [Google Scholar]
- 23. Lindstrom M, Wredmark T, Wretling ML, Henriksson M, Fellander-Tsai L. Post-operative bracing after ACL reconstruction has no effect on knee joint effusion: a prospective, randomized study. Knee. 2015;22(6):559–564. [DOI] [PubMed] [Google Scholar]
- 24. Minzlaff P, Heidt T, Feucht MJ, et al. Patient satisfaction with health is substantially improved following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):582–588. [DOI] [PubMed] [Google Scholar]
- 25. Noyes FR, Mooar LA, Barber SD. The assessment of work-related activities and limitations in knee disorders. Am J Sports Med. 1991;19(2):178–188. [DOI] [PubMed] [Google Scholar]
- 26. Obermeier MC, Sikka RS, Tompkins M, et al. Examination of early functional recovery after ACL reconstruction: functional milestone achievement and self-reported function. Sports Health. 2018;10(4):345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pauzenberger L, Syre S, Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: a systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29(10):1712–1721. [DOI] [PubMed] [Google Scholar]
- 28. Pouderoux T, Muller B, Robert H. Joint laxity and graft compliance increase during the first year following ACL reconstruction with short hamstring tendon grafts. Knee Surg Sports Traumatol Arthrosc. 2020;28(6):1979–1988. [DOI] [PubMed] [Google Scholar]
- 29. Sachs RA, Daniel DM, Stone ML, Garfein RF. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17(6):760–765. [DOI] [PubMed] [Google Scholar]
- 30. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction. Am J Sports Med. 2016;44(6):1502–1507. [DOI] [PubMed] [Google Scholar]
- 31. Smith TO, Davies L, Hing CB. Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):304–311. [DOI] [PubMed] [Google Scholar]
- 32. Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Spindler KP, Parker RD, Andrish JT, et al. Prognosis and predictors of ACL reconstructions using the MOON cohort: a model for comparative effectiveness studies. J Orthop Res. 2013;31(1):2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tiftikci U, Serbest S, Kilinc CY, Karabicak GÖ, Vergili Ö. Return to work in miners following anterior cruciate ligament reconstruction. Pan Afr Med J. 2015;22:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Verbeek J, Mischke C, Robinson R, et al. Occupational exposure to knee loading and the risk of osteoarthritis of the knee: a systematic review and a dose-response meta-analysis. Saf Health Work. 2017;8(2):130–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. von Essen C, McCallum S, Barenius B, Eriksson K. Acute reconstruction results in less sick-leave days and as such fewer indirect costs to the individual and society compared to delayed reconstruction for ACL injuries. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2044–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Webster KE, Feller JA. Younger patients and men achieve higher outcome scores than older patients and women after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2017;475(10):2472–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Webster KE, McPherson AL, Hewett TE, Feller JA. Factors associated with a return to preinjury level of sport performance after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2019;47(11):2557–2562. [DOI] [PubMed] [Google Scholar]
- 39. Werner JL, Burland JP, Mattacola CG, et al. Decision to return to sport participation after anterior cruciate ligament reconstruction, part II: self-reported and functional performance outcomes. J Athl Train. 2018;53(5):464–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wexler G, Bach BR, Bush-Joseph CA, et al. Outcomes of anterior cruciate ligament reconstruction in patients with workers’ compensation claims. Arthroscopy. 2000;16(1):49–58. [DOI] [PubMed] [Google Scholar]
- 41. Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med J Aust. 2018;208(8):354–358. [DOI] [PubMed] [Google Scholar]


