Abstract
Objective:
We examined the relationship between self-neglect and risk for subsequent elder abuse report to social services agency.
Method:
Population-based cohort study conducted Chicago. Primary predictor was elder self-neglect at baseline without concurrent elder abuse. Cox proportional hazard models were used to assess independent associations of elder self-neglect with the risk of subsequent elder abuse using time-varying covariate analyses.
Results:
Of 10,333 participants, 1,460 were reported for self-neglect and 180 were reported for elder abuse. The median time from self-neglect to elder abuse was 3.5 years. In multivariable analyses, elder self-neglect was associated with increased risk for subsequent elder abuse (odds ratio, OR, 1.75[1.18–2.59]). Elder self-neglect was also associated with increased risk for subsequent caregiver neglect (OR, 2.09[1.24–3.52]), financial exploitation (OR, 1.73[1.01–2.95]), and multiple forms of elder abuse (HR, 2.06[1.22–3.48]).
Conclusion:
Elder self-neglect report is associated with increased risk for subsequent elder abuse report to social services agency.
Keywords: self-neglect report, elder abuse report, aging, elderly, population-based study
Introduction
Elder self-neglect and elder abuse are serious, common, and underrecognized public health issues, with an estimated 3 to 5 million cases in the United States (National Research Council, 2003; Government Accountability Office, 2011). According to the National Center on Elder Abuse, self-neglect is defined “… as the behavior of an elderly person that threatens his/her own health and safety.” Elder abuse is an act referring to any knowing, intentional, or negligent act by a caregiver or any other person that causes harm or a serious risk of harm to a vulnerable adult (National Center on Elder Abuse Website, 2006).
Data from social service agencies suggest that elder self-neglect and elder abuse reports are rising and that elder self-neglect accounts for more cases than all of the elder abuse cases combined (Teaster, 2002). This trend is particularly alarming as literature suggests that both elder self-neglect and elder abuse are associated with adverse health outcomes (Dong, Mendes de Leon, & Evans, 2009; Dong, Simon, & Evans, 2012a, 2012b; Dong et al., 2009, 2011). However, the temporal relations between elder self-neglect and elder abuse remain unclear.
Both elder self-neglect and elder abuse are reported and investigated by the same adult protective services but are often considered as drastically different entities by health care professionals, social services agencies, law enforcement agencies, and judiciary systems (Dong & Simon, 2011). While elder abuse often elicits emotions of a violation of fundamental human rights of the victims against the perpetrators, elder self-neglect is more difficult to understand, quantify, and intervene. There have been a number of conceptual frameworks postulated for the syndrome of elder self-neglect and elder abuse (Choi, Kim, & Asseff, 2009; Dyer, Goodwin, Pickens-Pace, Burnett, & Kelly, 2007; Orem, 1991; Longres, 1995; National Research Council, 2003). However, to our knowledge none has attempted to recognize the complex interactions and bidirectionality between elder self-neglect and elder abuse. This is further exacerbated by the lack of systematic research to explore these relationships. Improved understanding of the potential bidirectional temporal relationships between elder self-neglect and elder abuse could significantly inform research, education, practice and policy at the local, state, and national level.
In this report, we followed a cohort of elder self-neglect cases without concurrent elder abuse at baseline in order to investigate: (a) the prospective association between elder self-neglect and subsequent risk for elder abuse reported to a social services agency in a large and sociodemographically diverse cohort; and (b) the prospective association between elder self-neglect and subsequent risk for specific subtypes of elder abuse in the same population.
Method
Design and Participants
The study population consists of participants in the Chicago Health and Aging Project (CHAP). CHAP is a prospective, population-based study of a geographically defined, urban, biracial community population, which is designed to identify risk factors for Alzheimer’s disease and other common chronic health problems in older age. Details of the CHAP study design have been described previously (Bienias, Beckett, Bennett, Wilson, & Evans, 2003).
Briefly, the study enrolled residents aged 65 years and older from adjacent neighborhoods on the south side of Chicago. In 1993, the study began with a complete census of the community area. The census identified 7,813 age-eligible residents, 6,158 (78.9%) of whom were enrolled between 1993 and 1997 as the “original cohort.” In 2000, CHAP began to enroll additional participants from the study community who had turned 65 since inception of the study as “successive age cohorts.” Data collection occurs in 3-year cycles, with each follow-up cycle (85% follow up) beginning after the conclusion of the previous cycle, which includes an in-person interview that comprised the assessment of health history, physical function, cognitive function, health behaviors, and psychosocial factors. Written informed consent was obtained from all participants and the study was approved by the Institutional Review Board at Rush University Medical Center.
Identification of Elder Self-Neglect and Elder Abuse
Reports of elder self-neglect or elder abuse to the state social services agencies can come from a variety of sources, including health care and legal professionals, community organizations, city workers (i.e., postal worker, utility worker, etc.), family members, or concerned neighbors or friends who have contact with seniors. Self-neglect generally manifests itself in an older person as a refusal or failure to provide himself/herself with adequate food, water, clothing, shelter, personal hygiene, medication (when indicated), and safety precautions. When a suspected elder self-neglect case is reported, home assessment is performed, in which the concerns for unmet personal health and safety needs are measured. Available information (Illinois Department on Aging, 1989) indicates good interrater reliability (κ ≥ 0.70) and internal consistency (Cronbach’s coefficient α = 0.95).
Types of elder abuse include physical abuse, sexual abuse, emotional abuse, confinement, caregiver neglect, deprivation, and financial exploitation. Physical abuse is defined as inflicting physical pain or injury upon an older adult. Sexual abuse is touching, fondling, intercourse, or any other sexual activity with an older adult, when the older adult is unable to understand, unwilling to consent, threatened, or physically forced. Emotional abuse involves verbal assaults, threat of abuse, harassment, or intimidation. Confinement is restraining or isolating an older adult, other than for medical reasons. Neglect is a caregiver’s failure to provide an older adult with life’s necessities, including, but not limited to, food, clothing, shelter, or medical care. The difference between caregiver neglect and self-neglect is the presence or the absence of a formal or informal caregiver (Illinois Department on Aging, 2008). Willful deprivation is defined as willfully denying an older adult medication, medical care, shelter, food, a therapeutic device, or other physical assistance. Financial exploitation includes the misuse, or withholding of an older adult’s resources by another, to the disadvantage of the elderly person or the profit or advantage of someone else. Details of the indicators of elder abuse have been previously described (Illinois Department on Aging, 2008). Substantiation of abuse is based on the number and type of elder abuse indicators seen by APS workers. APS workers use multiple indicators for each type of abuse from both subjective expressions from the older adults and/or objective assessment of wounds and evidence or any records.
Data Set Matching
We matched data from CHAP participants to reported elder self-neglect and elder abuse cases reported to the Illinois state social services agency, which serves as the protective agency. Matching was based on an algorithm that compared the following information: date of birth, sex, race, exact home address, zip codes, and the home phone number and was performed twice to increase accuracy. This resulted in CHAP participants who were matched the electronic statewide social service agency record. If a CHAP participant was found to be reported more than once, we selected the first report. For the present study, we only used self-neglect cases and abuse cases that were reported to social services agency after the baseline CHAP interview. From the initial dataset matching, we found 1,812 cases of reported self-neglect and 238 cases of reported elder abuse, of which 1,460 cases remained as self-neglect and 180 cases of elder abuse were included in study as we necessitated the elder abuse cases to occur after self-neglect cases.
Study Variables
Demographic variables include age (in years), sex, race, income and, education (years of education completed). Data on self-reported, physician-diagnosed medical conditions were collected for hypertension, diabetes mellitus, stroke, cardiovascular disease, hip fracture, and cancer. Cognitive function was assessed using the Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975), immediate and delayed recall of brief stories in the East Boston Memory Test, (Albert et al., 1991) and the Symbol Digit Modalities Test (Smith, 1984). To assess global cognitive function with minimal floor and ceiling artifacts, we constructed a summary measure for global cognition based on all four tests. Individual test scores were summarized by first transforming a person’s score on each individual test to a z-score and then averaging z-scores across tests to yield a composite score for global cognitive function.
Physical function was assessed by direct performance testing, an objective and detailed assessment of certain abilities (range 0–15; Guralnik et al., 1994). It assesses walking speed, tandem stands ability, and repeated chair stand ability. The Katz Activities of Daily Living (ADL) scale measures limitations in an individual’s ability to perform basic self-care tasks (Katz & Akpom, 1976). It consists of six items and an ADL score is created by adding the individual items (range 0–6).
Symptoms of depression were measured using a modified version (Kohout, Berkman, Evans, & Cornoni-Huntley, 1993) of the Center for the Epidemiological Study of Depression Scale (CES-D: range 0–10; Radloff, 1977). Social network was summarized as the total number of children, relatives, and friends seen at least monthly (Cornoni-Huntley, Brock, Ostfeld, Taylor, & Wallace, 1986). Social engagement was assessed by asking how often subjects participate in social activities outside of house; religious activities, museums, library, and senior centers.
Analytic Approach
Participants were divided into three groups: self-neglect report, elder abuse report, and neither. In this study, elder self-neglect and elder abuse report occurred throughout the study period. Thus, the groups were modeled as a time-varying covariate (Andersen & Gill, 1982) in a series of Cox proportional hazards models (Cox, 1972) to examine the association between self-neglect and subsequent elder abuse. In this study, we included cases of self-neglect, which had a baseline CHAP interview prior to the identification to the social services agency. At the time of self-neglect identification to social services agency, participants did not have concurrent elder abuse. In turn, elder self-neglect cases were followed over time, to examine their subsequent risk for elder abuse.
In the primary model (Model A), we tested the association of self-neglect with elder abuse after adjustment for cohort, age, sex, and race. In the second model (Model B), we added education and income. In the third model (Model C), we added health-related variables of medical comorbidities, global cognitive function, and physical performance testing. In the fourth model (Model D), we added psychosocial variables of interests: symptoms of depression, social network, and social engagement.
We further examined the association between elder self-neglect and subsequent elder abuse in three additional ways, each time repeating the models described above. First, we tested the interactions of self-neglect with all potential confounding factors of interest (i.e., self-neglect × medical conditions, self-neglect × depressive symptoms, etc.), with respect to elder abuse outcome. Next, we considered the association between elder self-neglect and specific subtypes of elder abuse. Finally, we considered the association between elder self-neglect and multiple forms of elder abuse. Odds ratio (OR) and 95% confidence intervals (CIs) are reported. All analyses used two-sided alternatives with p less than .05 considered significant. All analyses were done using SAS (SAS Institute Inc., 2004).
Results
Baseline Characteristics
The 10,333 CHAP participants had a mean age of 73.3 years at baseline (standard deviation [SD] = 7.1). About 39% were men, 63% were Black, and the average education was 12.2 years (SD = 3.6). A total of 1,460 subjects without a prior elder abuse report had a report of self-neglect. During the follow-up period, 180 older adults were also reported for elder abuse. Total per years experience for entire cohort was 81,247.9 and the total person years experience after self-neglect was 5,207.9. The mean person years for the entire cohort was 7.9 years and the mean person years after self-neglect was 3.5 years. Both elder self-neglect and elder abuse cases tended to be older, women, Black, and have lower income and education (Table 1).
Table 1.
Characteristics of the Study Population by Self-Neglect (SN) and Elder Abuse (EA)
| Neither N = 8,693 | SN (No EA) N = 1,460 | EA N = 180 | |
|---|---|---|---|
|
| |||
| Age (yrs) mean (SD) | 73.3 (7.2) | 73.6 (6.6) | 73.1 (6.0) |
| Men, number (%) | 3,480 (40.0) | 508 (34.8) | 43 (23.9) |
| Black, number (%) | 5,056 (58.2) | 1,277 (87.5) | 163 (90.6) |
| Education (yrs), mean (SD) | 12.4 (3.5) | 11.1 (3.4) | 10.9 (3.3) |
| Income (range 0–10), mean (SD) | 5.5 (2.5) | 4.0 (2.0) | 4.2 (1.9) |
| Medical conditions (range 0–8), number (%) | |||
| Heart disease | 1,125 (12.9) | 237 (16.3) | 26 (14.4) |
| Diabetes | 557 (6.4) | 178 (12.2) | 27 (15.0) |
| Cancer | 1,577 (18.2) | 266 (18.2) | 27 (15.0) |
| Hypertension | 4,352 (50.4) | 781 (53.8) | 92 (51.1) |
| Stroke | 784 (9.0) | 176 (12.1) | 22 (12.2) |
| Hip fracture | 296 (3.4) | 49 (3.4) | 4 (2.2) |
| MMSE (range, 0–30), mean (SD) | 26.2 (5.3) | 24.9 (5.3) | 24.9 (4.8) |
| Global cognition (range, −4.31 to 1.73), mean (SD) |
0.20 (0.83) | −0.09 (0.82) | −0.12 (0.77) |
| Katz ADL impairment (range, 0–6), mean (SD) | 0.3 (1.1) | 0.4 (1.2) | 0.4 (1.0) |
| Physical Performance (range, 0–15), mean (SD) | 10.3 (3.8) | 9.0 (3.8) | 8.9 (4.1) |
| CESD (range, 0–10), mean (SD) | 1.5 (1.9) | 1.9 (2.2) | 1.9 (2.4) |
| Social Network (range, 0–81), mean (SD) |
7.5 (6.4) | 6.9 (5.9) | 6.4 (5.4) |
| Social Participation (range, 0–8), mean (SD) | 2.4 (1.7) | 2.1 (1.6) | 2.1 (1.6) |
MMSE = mini-mental status examination. global cognition = z scores of MMSE, East Boston Memory Test, East Boston Delayed Recall, and Symbol Digit Modality Test; physical performance test = chair stand, tandem stand, and measured walk. CESD = Centers for Epidemiological Study of Depression.
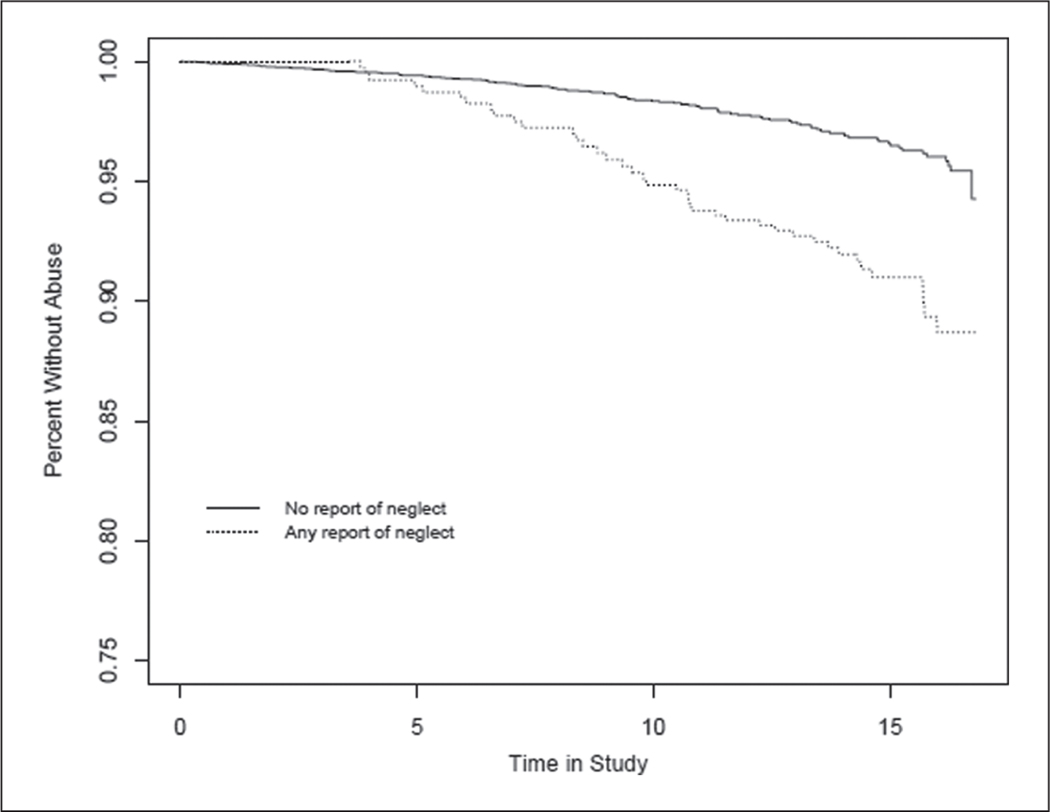
Elder Self-Neglect and Elder Abuse
In the core model (Table 2, Model A), elder self-neglect is associated with increased risk for subsequent elder abuse (OR, 2.01, 95% CI [1.38. 2.92]). Addition of socioeconomic status of education and income did not alter the degree of association (Model B). In Model C, we included health-related factors of medical conditions, cognitive function and physical function, elder self-neglect remains a significant predictor of subsequent elder abuse (OR, 1.75, 95% CI [1.18, 2.59]). In the fully adjusted analysis (Model D), reported self-neglect was associated with a significantly increased risk for subsequent elder abuse (OR, 1.75, 95% CI [1.18, 2.59]). A Kaplan–Meier survival curve was used to displace the proportion for elder abuse cases during the follow-up time of up to 14 years for those with and without elder self-neglect (Figure 1).
Table 2.
Association Between Self-Neglect and Subsequent Elder Abuse
| Odds Ratio (95% Confidence Interval) for Elder Abuse Outcome | ||||
|---|---|---|---|---|
|
|
||||
| Model A | Model B | Model C | Model D | |
|
| ||||
| Age | 1.06 (1.03–1.08) | 1.05 (1.02–1.08) | 1.02 (0.99–1.05) | 1.02 (0.99–1.05) |
| Sex | 0.56 (0.39–0.79) | 0.53 (0.37–0.77) | 0.57 (0.39–0.83) | 0.55 (0.38–0.81) |
| Race | 5.61 (3.37–9.34) | 4.89 (2.87–8.34) | 4.02 (2.29–7.05) | 3.98 (2.27–6.98) |
| Education | 0.94 (0.90–0.99) | 0.98 (0.93–1.03) | 0.98 (0.93–1.03) | |
| Income | 1.01 (0.93–1.09) | 1.05 (0.97–1.14) | 1.05 (0.97–1.14) | |
| Medical conditions | 1.12 (0.95–1.32) | 1.13 (0.96–1.33) | ||
| Cognitive function | 0.71 (0.56–0.92) | 0.73 (0.56–0.94) | ||
| Physical function | 0.92 (0.88–0.96) | 0.92 (0.88–0.97) | ||
| Depressive symptoms | 0.99 (0.93–1.07) | |||
| Social network |
0.98 (0.95–1.01) | |||
| Social engagement |
0.96 (0.86–1.07) | |||
| Predictor: Elder self-neglect | 2.01 (1.38–2.92) | 2.01 (1.38–2.93) | 1.75 (1.18–2.59) | 1.75 (1.18–2.59) |
Figure 1.
Kaplan–Meier survival curve for differences between those with and without elder self-neglect and subsequent elder abuse
X-axis: Years in the CHAP study
Y-axis: Percentage of CHAP participants without elder abuse
Note: Figure demonstrates that those with elder self-neglect compared to those without elder self-neglect are at greater risk to experience elder abuse in the study period.
In addition, we examined potential interactions of elder self-neglect and potential confounders (sociodemographic, socioeconomic, health-related, and psychosocial factors), with respect to the risk for subsequent elder abuse outcomes (Table 3). In the fully adjusted analyses, we did not find any significant interactions terms, suggesting that the significant association between self-neglect and risk for elder abuse was not mediated by these potential confounders.
Table 3.
Interactions Terms Between Sociodemographic, Socioeconomic, Health Related, and Psychosocial Factors and Self-Neglect (SN) and Elder Abuse Outcomes
| PE, SE | OR (95% CI) | p Value | |
|---|---|---|---|
|
| |||
| SN | 0.47 (0.22) | 1.59 (1.03–2.47) | 0.03 |
| Age | 0.03 (0.02) | 1.04 (1.00–1.07) | 0.04 |
| SN × age | −0.01 (0.03) | 0.99 (0.93–1/06) | 0.78 |
| SN | 0.43 (0.23) | 1.54 (0.99–2.40) | 0.06 |
| Sex | −0.56 (0.22) | 0.57 (0.37–0.88) | 0.01 |
| SN × sex | 0.29 (0.45) | 1.33 (0.55–3.23) | 0.52 |
| SN | 1.68 (0.65) | 5.39 (1.52–19.10) | 0.01 |
| Black | 1.51 (0.31) | 4.55 (2.46–8.41) | 0.00 |
| SN × Black | −1.26 (0.67) | 0.28 (0.08–1.05) | 0.06 |
| SN | 0.51 (0.21) | 1.66 (1.09–2.51) | 0.02 |
| Education | −0.02 (0.03) | 0.98 (0.93–1.05) | 0.48 |
| SN × education | 0.01 (0.06) | 1.01 (0.91–1.13) | 0.86 |
| SN | 0.53 (0.23) | 1.71 (1.09–2.65) | 0.02 |
| Income | 0.04 (0.05) | 1.04 (0.95–1.14) | 0.40 |
| SN × income | 0.16 (1.14) | 1.17 (0.13–10.99) | 0.88 |
| SN | 0.46 (0.31) | 1.58 (0.86–2.92) | 0.14 |
| Medical condition | 0.11 (0.09) | 1.12 (0.92–1.35) | 0.25 |
| SN × medical condition | 0.03 (0.20) | 1.03 (0.69–1.53) | 0.89 |
| SN | 0.49 (0.20) | 1.63 (1.09–2.44) | 0.01 |
| Cognition | −0.36 (0.14) | 0.69 (0.53–0.92) | 0.01 |
| SN × cognition | −0.03 (0.26) | 0.97 (0.57–1.62) | 0.90 |
| SN | 0.69 (0.47) | 1.99 (0.79–4.97) | 0.14 |
| Physical function | −0.07 (0.03) | 0.93 (0.88–0.98) | 0.01 |
| SN × physical function | −0.02 (0.05) | 0.97 (0.89–1.08) | 0.65 |
| SN | 0.78 (0.26) | 2.18 (1.32–3.60) | 0.01 |
| CESD | 0.02 (0.04) | 1.02 (0.94–1.11) | 0.56 |
| SN × CESD | −0.15 (0.09) | 0.86 (0.72–1.03) | 0.10 |
| SN | 0.72 (0.31) | 2.05 (1.11–3.78) | 0.02 |
| Social network | −0.01 (0.02) | 0.99 (0.96–1.02) | 0.51 |
| SN × social network | −0.04 (0.04) | 0.97 (0.89–1.04) | 0.38 |
| SN | 0.48 (0.34) | 1.61 (0.83–3.11) | 0.16 |
| Social engagement | −0.03 (0.06) | 0.97 (0.86–1.09) | 0.58 |
| SN × social engagement | 0.01 (0.12) | 1.01 (0.79–1.28) | 0.95 |
Note: CESD = Centers for Epidemiological Study of Depression.
Moreover, we examined the association between elder self-neglect and specific subtypes of subsequent elder abuse; namely physical abuse, psychological abuse, caregiver neglect, and financial exploitation (Table 4). In the fully adjusted model (Model D), elder self-neglect was associated with increased risk for subsequent financial exploitation (OR, 1.73, 95% CI [1.01, 2.95]) and caregiver neglect (OR, 2.09, 95% CI [1.24, 3.52]). Finally, we found that elder self-neglect was associated with increased risk for multiple forms of elder abuse (OR, 2.06, 95% CI [1.22, 3.48]; Model D).
Table 4.
Association Between Self-Neglect and Specific Subtypes of Subsequent Elder Abuse
| Models |
OR (95% confidence interval) for elder abuse outcomes |
|||||
|---|---|---|---|---|---|---|
| Specific Subtypes of Elder Abuse |
Multiple forms of elder abuse |
|||||
| Physical (n = 31 ) | Psychological (n = 70) | Financial (n = 105) | Caregiver Neglect (n = 88) | 1 Type | 2 or more types | |
|
| ||||||
| A | 1.49 (0.54–4.09) | 1.56 (0.81 –3.02) | 1.98 (1.21–3.28) | 2.27 (1.36–3.77) | 1.83 (1.07–3.16) | 2.21 (1.31–3.72) |
| B | 1.51 (0.55–4.17) | 1.55 (0.81 –2.99) | 2.01 (1.21–3.32) | 2.26 (1.36–3.77) | 1.86 (1.08–3.21) | 2.19 (1.30–3.70) |
| C | 1.32 (0.48–3.63) | 1.45 (0.75–2.80) | 1.97 (1.19–3.26) | 2.07 (1.23–3.48) | 1.45 (0.79–2.64) | 2.08 (1.23–3.51) |
| D | 1.35 (0.49–3.69) | 1.44 (0.74–2.78) | 1.73 (1.01–2.95) | 2.09 (1.24–3.52) | 1.47 (0.81–2.67) | 2.06 (1.22–3.48) |
A = age, sex, race. B = A + education, income. C = B + medical conditions, cognitive function and physical function. D = C + depressive symptoms, social network, and social engagement.
Discussion
Our study suggests that elder self-neglect to a social services agency was associated with a significant increased risk for subsequent elder abuse in a community-dwelling population of older adults. In addition, elder self-neglect was associated with increased risk for financial exploitation and caregiver neglect. Moreover, elder self-neglect was associated with increased risk for multiple forms of elder abuse.
Contribution to Existing Literature
Elder self-neglect and elder abuse reports are often initiated based on significant concerns for an older person’s welfare, health, and safety, perhaps to levels that suggest that there may be strong concerns for the older person’s well-being. However, in-part due to the lack of a responsible perpetrator and paucity of research, elder self-neglect is often perceived as a distinctly different syndrome, than that of elder abuse. Despite the proportion of elder self-neglect being greater than all other forms of elder abuse cases combined, elder self-neglect received relatively very little attention by health care professionals, social services agencies, and policy makers.
Our findings extend the prior body of work by demonstrating that the prospective relationship between elder self-neglect and subsequent elder abuse and providing systematic data on the significant relationship between two important geriatric syndromes. These findings may have direct implications for health care professionals and social services agencies to promote early identification of self-neglect and elder abuse. It would also prompt targeted interventions after the discovery of self-neglect to monitor the subsequent risk for elder abuse by others. In addition, this study is the first to demonstrate that the significant relationship between elder self-neglect and risk for elder abuse is not mediating by sociodemographic, socioeconomic, health-related. and psychosocial factors. This further suggests that elder self-neglect is an independent predictor for elder abuse. Moreover, our study is the first to suggest that elder self-neglect is associated with increased risk for subsequent financial exploitation and caregiver neglect by other perpetrators as well as predisposition to suffer multiple forms of elder abuse. This information will enable relevant aging disciplines to provide more targeted services and monitoring to prevent specific forms elder abuse among those with self-neglect in the community populations.
Possible Mechanisms
The mechanisms between elder self-neglect and elder abuse requires further investigation. We considered differences in sociodemographic and socioeconomic factors among groups but the adjustment for these factors did not substantially change the associations. In our analyses in Table 2, we noticed that race was highly associated with increased risk for elder abuse. Prior studies have suggested that prevalence of elder abuse is significantly higher among African American populations (Beach, Schulz, Castle, & Rosen, 2010; Laumann, Leitsch, & Waite, 2008). Future studies are needed to quantify the role of race in the relationship between self-neglect and elder abuse. In addition, we considered a comprehensive series of health-related characteristics including medical conditions, physical function, and cognitive function. But adjustment for these factors did not substantially alter the association. We also considered several psychosocial characteristics such as depressive symptoms, limited social networks, and social engagement. But again, adjustment for these factors did not change the results.
Clinical experience suggests that those who self-neglect often may not recognize or refuse to recognize the dangers of their self-neglectful behaviors and often only encounter the emergency health care system after a catastrophic event has occurred. Case reports (Clark, Mankikar, & Gray, 1975; Cornwall, 1981; Macmillan & Shaw, 1966; Ortiz, Lamdan, Johnson, & Korbage, 2009; Roe, 1977) often describe self-neglectors presenting to the health care system with organ failure, severe nutritional deficiencies, metabolic abnormalities, and undiagnosed advanced cancer. This may in turn trigger the need to identify potential family caregivers to facilitate discharge planning and power of attorney for personal and financial responsibilities. In addition, it is possible that a responsible caregiver was not identified at the time of initial self-neglect cases when in fact it could be caregiver neglect. Although this potential misclassification is possible, we believe that this is less likely, as the trained case workers could have most likely identified potential elder abuse. Moreover, it is possible that the new caregiver may not have the adequate resources and skills to meet the needs of the care recipients, which in turn could increase the proclivity toward elder abuse, as a result of caregiver stress, burnout, and/or depression. Future studies are needed to quantify these relationships
Mechanisms for self-neglect to be specifically at higher risk for financial exploitation remain unclear. It is conceivable that those who self-neglect may be more socially isolated with limited support, which may exacerbate their vulnerability to be exploited by potential perpetrators. However, in our interaction term analyses, we did not find such association as a potential mediating factor. Future studies are needed to gather more comprehensive information on social well-being to further explore these findings. In addition, it is possible that there are differential characteristics among those who accepted versus refused interventions at the point of self-neglect cases being identified. This would predispose certain older adults to be victimized by others.
Study Limitations
Several limitations of this study should be considered. First, both self-neglect and elder abuse are underreported and the rate of underreporting is unclear from the current literature. This may underestimate the degree of association in our findings. Second, our study could have detection bias, for which once an elderly is reported to social services agency; it could lead to the increased likelihood that further elder abuse will be detected. In addition, we do have ability identify participants with previous self-reported self-neglect and elder abuse prior to encounter with social services agency, which could bias the categorization of the participants. Future study is needed to explore the success and resolution process of the social service agency. Third, we did not have information as to if the CHAP participant were relocated out of state; or the reasons for the nonsubstantiated cases of elder abuse; or ability to delineate the detailed mechanism between self-neglect and elder abuse, especially with respect to socioeconomic status and trajectories of cognitive function. Fourth, we did not have detailed information on the perpetrators or any available in-depth information about potential caregiver stress, burden, and substance abuse history which would have contributed to subsequent elder abuse. Fifth, the study did not have any information on the social services agencies’ or health care professional’s intervention as the result of elder self-neglect and elder abuse report.
Conclusion
In sum, both self-neglect and elder abuse are common but underrecognized and poorly understood geriatric syndromes. Like other geriatric syndromes that are the result of the complex interactions among a variety of medical, psychological and social risk factors, self-neglect and elder abuse are likely to develop and progress slowly over time (Dong, 2005). Our findings contribute to an improved understanding of the temporal relationships between elder self-neglect and elder abuse. As the baby boomer population increases rapidly, elder self-neglect and elder abuse will likely increase over time and come to the attention of the health care, social services, and legal systems. This could have important implications as it will likely place significantly higher burdens on the existing system dealing with older adults who self-neglect with respect to the subsequent risk for elder abuse.
Future studies are needed to elucidate the causal mechanisms between elder self-neglect and elder abuse. Studies are also needed to examine the role of potential perpetrator and sociocultural context of the abusive relationships.
Future longitudinal studies are also needed to quantify specific phenotypes of elder self-neglect and other protective factors with respect to risk for elder abuse in community populations. Improved understanding of these relations may be useful not only in informing future research efforts of elder self-neglect and elder abuse in racially/ethnically diverse populations but also in developing relevant clinical, social, and policy guidelines for the treatment and prevention of self-neglect and elder abuse.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by National Institute on Aging grant (R01 AG042318, R01 MD006173, R01 AG11101 & RC4 AG039085), Paul B. Beeson Award in Aging (K23 AG030944), The Starr Foundation, John A. Hartford Foundation and The Atlantic Philanthropies.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Reference
- Albert M, Smith LA, Scherr PA, Taylor JO, Evans DA, & Funkenstein HH (1991). Use of brief cognitive tests to identify individuals in the community with clinically diagnosed Alzheimer’s disease. International Journal of Neuroscience, 57, 167–178. [DOI] [PubMed] [Google Scholar]
- Andersen PK, & Gill RD (1982). Cox’s regression model counting process: A large sample study. Annals of Statistics, 10, 1100–1120. [Google Scholar]
- Beach SR, Schulz R, Castle NG, & Rosen J. (2010). Financial exploitation and psychological mistreatment among older adults: Differences between African Americans and non-African Americans in a population-based survey. The Gerontologist, 50, 744–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bienias JL, Beckett LA, Bennett DA, Wilson RS, & Evans DA (2003). Design of the Chicago Health and Aging Project (CHAP). Journal of Alzheimers Disease, 5, 349–355. [DOI] [PubMed] [Google Scholar]
- Choi NG, Kim J, & Asseff J. (2009). Self-neglect and neglect of vulnerable older adults: Reexamination of etiology. Journal of Gerontological Social Work, 52, 171–187. [DOI] [PubMed] [Google Scholar]
- Clark AN, Mankikar GD, & Gray I. (1975). Diogenes syndrome. A clinical study of gross neglect. Lancet, 1, 366–368. [DOI] [PubMed] [Google Scholar]
- Cornoni-Huntley J, Brock DB, Ostfeld A, Taylor JO, & Wallace RB (1986). Established populations for epidemiological studies of the elderly resource data book (Rep. No. NIH Publication No. 86–2443). Washington, DC: US Department of Health and Human Services. [Google Scholar]
- Cornwall JV (1981). Filth, squalor and lice. Self neglect in the elderly. Nursing Mirror, 153, 48–49. [PubMed] [Google Scholar]
- Cox DR (1972). Regression models and life tables. Journal of Royal Statistics Society B, 34, 187–220. [Google Scholar]
- Dong X. (2005). Medical implications of elder abuse and neglect. Clinics in Geriatric Medicine, 21, 293–313. [DOI] [PubMed] [Google Scholar]
- Dong X, Mendes de Leon CF, & Evans DA (2009). Is greater self-neglect severity associated with lower levels of physical function? Journal of Aging and Health, 21, 596–610. [DOI] [PubMed] [Google Scholar]
- Dong X, & Simon MA (2011). Enhancing national policy and programs to address elder abuse. Journal of the American Medical Association, 305, 2460–2461. [DOI] [PubMed] [Google Scholar]
- Dong X, Simon MA, & Evans DA (2012a). Prospective study of the elder self-neglect and emergency department use in a community population. American Journal of Emergency Medicine, 30, 553–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, Simon MA, & Evans D. (2012b). Elder self-neglect and hospitalization: Findings from the Chicago health and aging project. Journal of the American Geriatrics Society, 60, 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, Simon MA, Fulmer T, Mendes de Leon CF, Hebert LE, Beck T, … Evans DA (2011). A Prospective population-based study of differences in elder self-neglect and mortality between Black and White older adults. Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 66(6), 695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, Simon M, Fulmer T, Mendes de Leon C, Beck T, Hebert L, … Evans DA (2009). Elder self-neglect and abuse and mortality risk in a community-dwelling population. Journal of the American Medical Association, 302, 517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer CB, Goodwin JS, Pickens-Pace S, Burnett J, & Kelly PA (2007). Self-neglect among the elderly: A model based on more than 500 patients seen by a geriatric medicine team. American Journal of Public Health, 97, 1671–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, & McHugh PR (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatry Research, 12, 189–198. [DOI] [PubMed] [Google Scholar]
- Government Accountability Office. (2011). Elder Justice: Stronger federal leadership could enhance national response to elder abuse. Retrieved from http://aging.senate.gov/events/hr230kb2.pdf
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, … Wallace RB (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49, M85–M94. [DOI] [PubMed] [Google Scholar]
- Illinois Department on Aging. (1989). Determination of need revision final report volume I. Springfield, IL: Author. [Google Scholar]
- Illinois Department on Aging. (2008). Elder abuse and neglect program: Standard and procedures manual. Retrieved from http://www.aging.state.il.us/eps/content/EAStandards&Procedures0208.pdf
- Katz S, & Akpom CA (1976). A measure of primary sociobiological functions. International Journal of Health Services, 6, 493–508. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, & Cornoni-Huntley J. (1993). Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. Journal of Aging and Health, 5, 179–193. [DOI] [PubMed] [Google Scholar]
- Laumann EO, Leitsch SA, & Waite LJ (2008). Elder mistreatment in the United States: Prevalence estimates from a nationally representative study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 63, S248–S254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longres JF (1995). Self-neglect among the elderly. Journal of Elder Abuse and Neglect, 7, 87–105. [Google Scholar]
- Macmillan D, & Shaw P. (1966). Senile breakdown in standards of personal and environmental cleanliness. British Medical Journal, 2, 1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center on ELder Abuse Website (2006). NCEA: The basics. Retrieved from http://elderabusecenter.org/pdf/research/apsreport030703.pdf
- National Research Council. (2003). Elder mistreatment: Abuse, neglect and exploitation in an aging America. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Orem DE (1991). Nursing: Concepts of practice (4th ed.). St Louis, MO: Mosby. [Google Scholar]
- Ortiz N, Lamdan R, Johnson S, & Korbage A. (2009). Caregiver status: A potential risk factor for extreme self-neglect. Psychosomatics, 50, 166–168. [DOI] [PubMed] [Google Scholar]
- Radloff L. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measure, 1, 385–401. [Google Scholar]
- Roe PF (1977). Self-neglect. Age and Ageing, 6, 192–194. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. (2004). SAS OnlineDoc, Version 9.1.3. Cary, NC: SAS Institute Inc. [Google Scholar]
- Smith A. (1984). Symbol digit modalities test manual-revised. Los Angeles, CA: Western Psychological. [Google Scholar]
- Teaster PB (2002). A response to abuse of vulnerable adults: The 2000 survey of state adult protective service. Retrieved from http://www.ncea.aoa.gov/ncearoot/Main_Site/pdf/research/apsreport030703.pdf [Google Scholar]